Summary
Background
Preterm birth is the leading cause of death in children younger than 5 years worldwide. Although preterm survival rates have increased in high-income countries, preterm newborns still die because of a lack of adequate newborn care in many low-income and middle-income countries. We estimated global, regional, and national rates of preterm birth in 2014, with trends over time for some selected countries.
Methods
We systematically searched for data on preterm birth for 194 WHO Member States from 1990 to 2014 in databases of national civil registration and vital statistics (CRVS). We also searched for population-representative surveys and research studies for countries with no or limited CRVS data. For 38 countries with high-quality data for preterm births in 2014, data are reported directly. For countries with at least three data points between 1990 and 2014, we used a linear mixed regression model to estimate preterm birth rates. We also calculated regional and global estimates of preterm birth for 2014.
Findings
We identified 1241 data points across 107 countries. The estimated global preterm birth rate for 2014 was 10·6% (uncertainty interval 9·0–12·0), equating to an estimated 14·84 million (12·65 million–16·73 million) live preterm births in 2014. 12· 0 million (81·1%) of these preterm births occurred in Asia and sub-Saharan Africa. Regional preterm birth rates for 2014 ranged from 13·4% (6·3–30·9) in North Africa to 8·7% (6·3–13·3) in Europe. India, China, Nigeria, Bangladesh, and Indonesia accounted for 57·9 million (41×4%) of 139·9 million livebirths and 6·6 million (44×6%) of preterm births globally in 2014. Of the 38 countries with high-quality data, preterm birth rates have increased since 2000 in 26 countries and decreased in 12 countries. Globally, we estimated that the preterm birth rate was 9×8% (8×3–10×9) in 2000, and 10×6% (9×0–12×0) in 2014.
Interpretation
Preterm birth remains a crucial issue in child mortality and improving quality of maternal and newborn care. To better understand the epidemiology of preterm birth, the quality and volume of data needs to be improved, including standardisation of definitions, measurement, and reporting.
Funding
WHO and the March of Dimes.
Introduction
WHO defines preterm birth as all births before 37 completed weeks of gestation, or fewer than 259 days from the first date of a woman's last menstrual period.1 Complications of preterm birth were the leading cause of death in children younger than 5 years of age globally in 2016, accounting for approximately 16% of all deaths, and 35% of deaths among newborn babies.2
Preterm neonates who survive are at greater risk of a range of short-term and long-term morbidities. Common complications of preterm birth are high rates of respiratory distress syndrome, bronchopulmonary dysplasia, necrotising enterocolitis, sepsis, periventricular leucomalacia, seizures, intraventricular haemorrhage, cerebral palsy, infections, feeding difficulties, hypoxic ischaemic encephalopathy, and visual and hearing problems.3, 4, 5, 6, 7, 8, 9, 10, 11 Preterm birth is associated with significant costs to health systems, and families of preterm newborns often experience considerable psychological and financial hardship.12, 13, 14, 15 Although the risks of mortality and morbidity are much higher in early gestation (<34 weeks), late preterm birth (34<37 weeks) occurs more often, and newborn babies born late preterm have significantly higher risks of adverse outcomes than babies born at term.6, 16 The 37 week cutoff for preterm birth is somewhat arbitrary, as early term births (37 and 38 weeks) have higher rates of adverse outcomes than full term gestations (39 and 40 weeks).17 Preterm births can be classified as spontaneous (due to spontaneous preterm labour or preterm prelabour rupture of membranes) or provider-initiated (caesarean or labour induction, for a maternal or fetal indication).18 Although many sociodemographic, nutritional, biological, and environmental factors can increase the risk of spontaneous preterm birth, the cause is not fully understood.18, 19
Research in context.
Evidence before the study
Complications of preterm birth are the leading cause of death in children younger than 5 years of age. However, data for the prevalence of preterm birth are not routinely collected or reported in many countries. Previous global estimates reported that preterm birth affected approximately one in 10 livebirths worldwide in 2010. As part of WHO's commitment to addressing preterm birth within the framework of the Global Strategy for Women's, Children's and Adolescents' Health and the Every Newborn Action Plan, we developed global, regional, and national estimates of preterm birth for 2014, and estimates of changes over time for selected countries.
Added value of this study
Our study shows that an estimated 10·6% of livebirths worldwide were preterm in 2014. Of the 14·84 million babies born preterm in 2014, more than 80% were born in south Asia and sub-Saharan Africa. Data from selected high-income and high-middle-income countries suggest that rates of preterm birth are increasing.
Implications of all the available evidence
There is a clear need to improve the quality and volume of data for preterm birth, including standardisation of definitions, measurement, and reporting of preterm birth rates. Improved prevention and management of preterm birth is crucial to reducing associated mortality and morbidity in newborn babies. Greater investments are required to improve the quality of care for pregnant women and newborn babies (including those born preterm), as well as research on new interventions to identify, prevent, and manage the consequences of preterm birth globally.
Addressing the global burden of preterm birth is crucial to achieving Sustainable Development Goal 3 (ensure healthy lives and promote wellbeing for all at all ages) and for reducing preterm-related neonatal and child mortality. Estimates of the global burden of preterm birth are needed to understand the global epidemiology of this condition because data are sparse and incomplete in many countries. They allow health system stakeholders, policies, and programmes to be better informed, enabling more precise targeting of interventions. Estimates can also raise awareness of preterm birth as a global public health issue, and can help mobilise resources for research and maternal and child health programmes. Previous estimates of preterm birth have been developed for 2005 and 2010.20, 21 WHO has committed to providing updated analyses of global levels and trends of preterm birth every 3–5 years. The aim of this study was to estimate national, regional, and global preterm births between 1990 and 2014.
Methods
Study design
We did a systematic review for data on preterm birth in databases of national civil registration and vital statistics, supplemented with population-representative surveys and research studies. For countries without high-quality data on preterm birth for 2014, we used a regression model to estimate preterm birth rates. We also calculated regional and global estimates of preterm birth for 2014.
Methodological details for this study are available in the protocol.22 The preterm birth rate (based on the WHO definition1) was the primary outcome, defined as the number of liveborn preterm births (ie, a singleton or multiple livebirth before 37 completed weeks of gestation) divided by the number of livebirths.
We identified and extracted available data on preterm birth for the 194 Member States of WHO23 for 1990 to 2014 (inclusive). The preferred data source was civil registration and vital statistics (CRVS) data. However, data for preterm birth are often not available in national CRVS systems, and not all countries have a CRVS system.24 Thus, in countries where no or limited CRVS preterm birth data were reported, we searched for research studies (whether representative of the national population or not) and population-representative household surveys.
We classified WHO Member States into three groups (A, B, or C) to guide data extraction, based on the availability of CRVS preterm birth data and the estimated coverage of births captured by the national CRVS system (appendix pp 5–7).25 Group A countries were those with an estimated CRVS birth registration coverage of more than 80%, and CRVS preterm birth data available for at least 50% of the years from 1990 to 2014. Group B countries were those with coverage from 60% to 80%, CRVS preterm birth data available for less than 50% of years, or both. Group C countries were those with less than 60% birth registration coverage (or unknown), no available CRVS data for preterm birth, or both. For group A countries, we used CRVS data only. For group B and C countries, we used any available CRVS data and sought additional data from research studies and population-representative household surveys. All searches were done without language restrictions.
To identify CRVS data, we searched all online databases of national ministries of health and national statistical offices for all WHO Member States using search terms related to births or preterm birth in the relevant language.26 We did a first search in January, 2016, and an updated search in May, 2017. For group B and C countries, we also searched the online repositories of Demographic and Health Surveys27 and Reproductive Health Surveys28 for all survey reports with data for preterm birth. We also conducted a systematic review, searching MEDLINE, Embase, Popline, Global Index Medicus, CINAHL, PsychInfo, and the Cochrane Central Register of Controlled Trials for articles with data for preterm birth (appendix pp 8–17). Given the large population in China (where national data on preterm birth are not reported), we also searched Sinomed, a Chinese language database, restricted to the six most highly cited medical journals.
Data eligibility
We included reports providing preterm birth data for 1990 to 2014 with at least 500 births.22 Reports using definitions similar to our primary outcome (such as those reporting preterm birth in all births, in singletons only, or with minor exclusions for selected subpopulations) were also eligible. We included reports using livebirths or all births (ie, livebirths and stillbirths), regardless of the definition used. The Intergrowth-21st multicentre cohort study reported that 3% of healthy, low-risk women experienced a preterm birth and spontaneous onset of labour.29 Hence, we excluded data points in which less than 3% of births were preterm on the basis of biological implausibility.
We excluded case-control studies, studies with insufficient information (such as conference abstracts), or those in which preterm birth data were available only for high-risk subpopulations (eg, women with specific medical or obstetric complications, women or newborn babies using specialty services, or selected socio-demographic subgroups). If multiple reports originated from the same dataset, we used the report providing the most comprehensive information. We excluded articles in which the midpoint of data collection was before 1990, or in which the year of data collection was not reported. We also excluded some reports for reasons that were not prespecified: reports in which gestational age was reported using months only, and several population-representative surveys that lacked a clear operational definition of preterm birth or that relied on maternal recall.
Data collection and management
We developed a study manual of operations to standardise all screening and extraction procedures, which was used to train all participating reviewers in an in-person workshop. An eligibility checklist was used to screen reports. Each CRVS report and population-representative survey report were reviewed independently for inclusion by two reviewers. For the systematic review, all recovered citations were merged and duplications removed, and all titles and abstracts were screened by two reviewers independently using the Covidence platform. Full texts of potentially eligible articles were reviewed independently for inclusion by two reviewers. Disagreements were resolved through discussion or a third reviewer.
We developed a customised online database (OpenClinica) for data extraction. Extracted data included: country, data source, design, time period, range of gestational age used, method of assessment of gestational age, and data for preterm birth. We also extracted any data on prespecified gestational age subgroups (<28 weeks, 28<32 weeks, 32<37 weeks). CRVS data were extracted by two reviewers, with results compared and disagreements resolved by a third reviewer. Data from population-representative surveys and research studies were extracted by one reviewer, with a 10% random sample extracted by a second reviewer and compared for quality control. A midpoint year was assigned to each data point. Additional quality checks were done for on all outlier data points. There was considerable heterogeneity in how preterm birth was defined and measured; some reports provided multiple indicators (eg, preterm birth reported in livebirths; in livebirths and stillbirths; in singletons only; in multiples only). We extracted characteristics and data for all available preterm birth indicators and developed a hierarchy of indicators based on proximity to the WHO definition to assign a primary indicator for each data point (appendix p 18).
We also created a database of candidate predictors of preterm birth to use in our models, based on potential risk factors and covariates identified in previous estimates of preterm births.22 Data were extracted from the most recent published national estimates of these predictors from the pertinent United Nations sources (appendix pp 19–20). In the event of missing years of data, interpolation was applied.
Statistical models
We modelled preterm birth rates using a multilevel (region, country, and preterm birth rates) linear mixed regression model, with correlated random country-specific intercepts and time slopes; a regional random intercept was also applied. Inclusion of covariates was based on the deviance information criterion and significance and inspection at country level. Covariates included in the final model were: (1) Human Development Index, (2) low birthweight proportion, (3) definition of preterm used in data source, (4) birth population used (livebirths or all births), (5) whether singleton or multiple births were included, or both, and (6) data source. We did statistical regression analyses in Stata (version 14.2) based on the full dataset (1241 data points from 107 countries). We estimated the logit transform of the preterm birth data using a linear Bayesian model (bayesmh command in Stata):
for the i:th year, j:th country, k:th region, and the l:th observation. The random component αj is the correlated country intercept and the random component βj is the time slopes, γk is the regional dummy intercept, δ1 is the Human Development Index (continuous) slope, δ2 is the low birthweight (continuous) proportion slope, δ3 is the coefficient of the categorical variable for preterm definition (0 if ≤36 weeks, 1 if <36 weeks, 2 if ≤37 weeks), δ4 is the coefficient of the categorical variable for population (0 if livebirths, 1 if all births, 2 if not defined), δ5 is the coefficient of the plurality dummy (0 if singleton and multiple, 1 if other or not defined), δ6 is the coefficient of the data source dummy (0 if CRVS, 1 if research study or household survey), and εijkl is a normally distributed residual.
In the regression models, we used the United Nations Statistics Division (M49) regional groupings (merging Latin America and North America into one region, and sub-Saharan Africa and North Africa into one region).30 We did not apply weights for study sample size because of differences in sample sizes between studies and CRVS data. We used Markov Chain Monte Carlo to simulate the posterior distribution. We used three chains, each with a sample size of 10 000 draws, following a burn-in of 10 000 draws, for a total of 30 000 posterior draws. The technical details and syntax (including distribution of priors) are shown in the appendix (pp 21–24).
To estimate preterm birth rates at global and regional level, we generated predictions for all country-years from the estimated model parameters. To properly reflect uncertainty around estimates for countries without data, random intercepts and slopes for these countries were simulated from the posterior means and covariance of country intercepts and slopes for countries with data. From this procedure, we had 30 000 sets of model parameter values for the model for each country.
When predicting preterm birth rates from the model, the dummy variables, δ3, δ4, δ5, and δ6, were all set to 0, which was the preferred level for these four variables (appendix 21–24). The predicted preterm birth rates per year in each country were then weighted into global and regional estimates, based on the estimated total number of livebirths per country per year. Uncertainty intervals (UI) were constructed from the weighted 2nd and 98th percentiles of the posterior samples (30 000 replicates). The estimated numbers of preterm births were calculated as the product of the preterm birth rate and the yearly total livebirths.31 We used United Nations Development Programme estimates of livebirths (1990–2014) rather than country estimates because we needed comparable data across all countries. Consequently, we excluded 11 countries without a United Nations Development Programme estimate of livebirths from the analysis. Regional estimates were weighted to a global estimate based on the regional livebirth population. We also estimated the contribution of different preterm birth definitions (<28 weeks, 28 to <32 weeks, 32 to <37 weeks) and of multiple births to the overall preterm birth rates. We conducted an official country consultation with WHO Member States in July, 2017, for review of the methods and provision of potentially eligible additional data. Additional data were received from four countries that were eligible for inclusion.
Presentation of results
Global and regional estimates of preterm birth rate for 2014 are based on model predictions for 183 countries. For the 38 group A countries, the data for 2014 are reported directly without modelling and without UIs. If data for 2014 were not available, the predicted preterm birth rates for 2014 (extrapolated from available data) are provided. Trends in preterm birth rates from 2000 to 2014 were also estimated for group A countries. For group B and C countries with three or more data points (of any type) available for 1990 to 2014, we present the predicted preterm birth rates with UIs for 2014. For group B and group C countries with fewer than three data points, we do not present a country-specific estimate because of concerns regarding the reliability of national estimates for which no or few country data are available. In these countries, the corresponding regional estimate is provided to guide stakeholders.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the Article. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Our website searches and online country consultation identified 882 CRVS data points for 55 countries. The literature search identified 33 599 citations, of which 5863 were duplicates. A further 26 511 citations were excluded after screening the titles and abstracts. We conducted full text review of 1225 papers, excluding 119 duplicates and a further 799 that were ineligible. After extraction, 47 data points were excluded because the preterm birth rate was less than 3%, or the study population was ineligible. The search of Demographic and Health Surveys and Reproductive Health Surveys databases identified 357 reports, of which we included five reports (five data points). The final database included 1241 data points for 107 countries (appendix pp 25–37).
In total, 882 (71·1%) of 1241 data points were from CRVS (table 1). Only 10·9% of all CRVS data came from Asia, and there were no CRVS data from Africa. European and North American countries accounted for 636 (51·2%) of all data points; 1123 (90·5%) were from high-income or upper-middle-income countries. Of the 183 countries with a United Nations Development Programme estimate of livebirths, no data were identified for 76 countries (table 1, appendix pp 5–7). 268 (74·7%) of 359 included studies (whether research studies or population-representative surveys) were facility-based. Across all data points, the method used to ascertain gestational age was generally not reported (929 data points; 74·9%). The use of ultrasound or best obstetric estimate for gestational age estimation was explicitly stated in only 197 (15·9%) of all data points. Only 414 (33·3%) data points reported preterm birth as a proportion of livebirths, including singletons and multiple births (ie, the WHO definition).
Table 1.
Sources of data
| Number of countries | Number of countries with a least one data point | CRVS data points | Research study or survey data points | All data points | |
|---|---|---|---|---|---|
| Asia | 47 | 31 | 96 (10·9%) | 221 (61·6%) | 317 (25·5%) |
| Europe | 39 | 35 | 535 (60·7%) | 52 (14·5%) | 587 (47·3%) |
| Latin America and the Caribbean | 31 | 18 | 153 (17·3%) | 30 (8·4%) | 183 (14·7%) |
| North America | 2 | 2 | 49 (5·6%) | 0 (0·0%) | 49 (3·9%) |
| Northern Africa | 6 | 4 | 0 (0·0%) | 6 (1·7%) | 6 (0·5%) |
| Oceania | 10 | 3 | 49 (5·6%) | 1 (0·3%) | 50 (4·0%) |
| Sub-Saharan Africa | 48 | 14 | 0 (0%) | 49 (13·6%) | 49 (3·9%) |
| Total | 183 | 107 | 882 (100%) | 359 (100%) | 1241 (100%) |
Data are n (%). Regions are based on the United Nations Standard Country or Area Codes for Statistical Use (M49) major regional groups. Countries includes WHO Member States with a United Nations Development Programme estimate of livebirths for 2014. CRVS=civil registration and vital statistics.
The estimated global preterm birth rate for 2014 was 10·6% (UI 9·0–12·0). Of the 139·95 million livebirths in 2014, an estimated 14·84 million were preterm (UI 12·65 million–16·73 million; table 2). The estimated regional preterm birth rates for 2014 ranged from 13·4% (UI 6·3–30·9) in North Africa to 8×7% (UI 6·3–13·3) in Europe (table 2), although there were few data available from North Africa. Asian and sub-Saharan African countries accounted for 110 395 283 (78·9%) livebirths and 12 030 083 (81·1%) preterm births globally in 2014.
Table 2.
Estimated preterm birth rates and numbers of preterm births in 2014
| Estimated preterm birth rate*(%, UI) | UNDP estimated number of livebirths | Proportion of global livebirths (%) | Estimated number of preterm births (n, UI) | Proportion of global preterm births (%) | |
|---|---|---|---|---|---|
| Asia | 10·4% (8·7–11·9) | 75 441 991 | 53·9% | 7 847 643 (6 579 297–8 987 184) | 52·9% |
| Europe | 8·7% (6·3–13·3) | 7 927 034 | 5·7% | 690 931 (497 738–1 051 737) | 4·7% |
| Latin America and the Caribbean | 9·8% (8·6–11·3) | 10 814 139 | 7·7% | 1 062 800 (931 611–1 220 105) | 7·2% |
| North America | 11·2% (9·5–13·2) | 4 394 185 | 3·1% | 491 297 (416 479–578 367) | 3·3% |
| North Africa | 13·4% (6·3–30·9) | 5 771 560 | 4·1% | 773 687 (365 845–1 782 375) | 5·2% |
| Oceania | 10·0% (7·9–12·7) | 643 749 | 0·5% | 64 227 (50 706–81 961) | 0·4% |
| Sub-Saharan Africa | 12·0% (8·6–16·7) | 34 953 292 | 25·0% | 4 182 440 (2 994 834–5 838 104) | 28·2% |
| Global | 10·6% (9·0–12·0) | 139 945 950 | 100·0% | 14 835 606 (12 654 938–16 728 926) | 100·0% |
Regions are based on the United Nations Standard Country or Area Codes for Statistical Use (M49) major regional groups. UI=uncertainty interval. UNDP=United Nations Development Programme.
Preterm births per 100 livebirths.
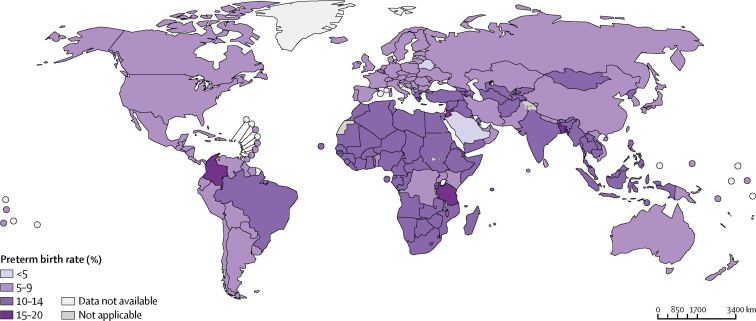
National data for preterm birth rates for 2014 were reported directly for 29 countries; we estimated rates for 2014 for a further 51 countries. For the remaining 103 countries, we present the corresponding regional estimate (Figure 1, Figure 2, appendix pp 38–39). The highest estimated national rate for 2014 was 19·1% (UI 13·2–26·2) in Bangladesh. The top five countries for number of preterm births (India, China, Nigeria, Bangladesh, and Indonesia) accounted for an estimated 57 945 623 (41·4%) of 139 945 950 livebirths and for 6 622 621 (44·6%) of 14 835 606 preterm births globally in 2014 (table 3).
Figure 1.
Estimated preterm birth rates in 2014
Figure 2.
Estimated numbers of preterm births in 2014
Table 3.
Top ten countries for number of preterm births in 2014
| Estimated number of preterm births (UI) | Estimated number of livebirths | Estimated proportion of global livebirths (%) | Preterm birth rate (%, UI) | Proportion of global preterm births (%) | |
|---|---|---|---|---|---|
| India* | 3 519 947 (2 872 618–4 165 975) | 25 860 462 | 18·5% | 13·6 (11·1–16·1) | 23·4% |
| China* | 1 168 126 (978 578–1 333 121) | 16 826 493 | 12·0% | 6·9 (5·8–7·9) | 7·8% |
| Nigeria* | 803 178 (563 907–1 107 550) | 7 033 430 | 5·0% | 11·4 (8·0–15·7) | 5·3% |
| Bangladesh* | 603 698 (416 079–825 413) | 3 152 549 | 2·3% | 19·1 (13·2–26·2) | 4·0% |
| Indonesia† | 527 672 (442 389–604 295) | 5 072 689 | 3·6% | 10·4 (8·7–11·9) | 3·5% |
| Pakistan* | 454 104 (300 768–645 911) | 5 415 657 | 3·9% | 8·4 (5·6–11·9) | 3·0% |
| USA‡ | 383 257 (NA–NA) | 4 008 329 | 2·9% | 9·6 (NA–NA) | 2·6% |
| Ethiopia† | 376 730 (269 757–525 862) | 3 148 388 | 2·2% | 12·0 (8·6–16·7) | 2·5% |
| Brazil‡ | 339 239 (NA–NA) | 3 035 148 | 2·2% | 11·2 (NA–NA) | 2·3% |
| Tanzania* | 336 025 (131 167–676 648) | 2 025 593 | 1·4% | 16·6 (6·5–33·4) | 2·2% |
UI=uncertainty interval.
Preterm births based on modelled national estimates.
Preterm births based on modelled regional estimates.
Preterm births based on directly reported data.
National trends for 2000–14 were estimated for the 38 group A countries, as were regional and global trends (appendix p 40). The preterm birth rate increased over this period for 26 countries (ranging from an absolute difference of +7·9% in Chile to +0·06% in Austria), while it decreased in 12 countries (ranging from an absolute difference of −0·04% in Czech Republic, to −3·7% in Bahrain). Globally, the preterm birth rate was 9×8% (UI 8×3–10×9) in 2000, and 10×6% (9×0–12×0) in 2014). The decrease in sub-Saharan Africa (13·1% in 2000, to 12·0% in 2014) should be interpreted with caution, given the wide, overlapping UIs and the paucity of data from this region.
Data on gestational age subgroups were available from 67 countries (table 4). Globally, 84·7% (UI 83·2–86·1%) of preterm births occurred in the late preterm period (32<37 weeks), ranging from 81·2% (UI 77·7–84·7) in Latin America and the Caribbean to 85·9% (UI 84·4–87·3) in Asia. Based on 50 data points from six countries (where preterm birth was reported separately for singleton births alone, and singleton and multiple births) an estimated 20·0% (UI 19·0–21·0) of the preterm birth rate was attributable to multiple births.
Table 4.
Preterm births by gestational age in 2014
|
Global |
Regional |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Data points (n) | Proportion (UI) | Asia |
Europe |
Latin America and the Caribbean |
North America |
North Africa |
Oceania |
Sub-Saharan Africa |
||||||||
| Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | Data points (n) | Proportion (UI) | |||
| <28 weeks | 553 | 4·1% (3·5–4·7) | 49 | 3·4% (2·8–4·0) | 351 | 5·1% (4·9–5·3) | 70 | 8·9% (5·1–12·8) | 25 | 6·8% (6·3–7·2) | 2 | 3·3% (1·6–5·1) | 45 | 5·6% (2·7–8·6) | 11 | 3·3% (1·6–5·1) |
| 28 to <32 weeks | 555 | 11·3% (10·2–12·4) | 50 | 10·8% (9·6–12·1) | 352 | 10·9% (10·3–11·6) | 70 | 9·8% (9·2–10·4) | 25 | 10·7% (10·4–10·9) | 2 | 12·8% (9·3–16·4) | 45 | 12·0% (6·0–18·0) | 11 | 12·8% (9·3–16·4) |
| 32 to <37 weeks | 553 | 84·7% (83·2–86·1) | 50 | 85·9% (84·4–87·3) | 350 | 84·5% (84·1–84·8) | 70 | 81·2% (77·7–84·7) | 25 | 82·6% (82·1–83·0) | 2 | 83·8% (79·1–88·5) | 45 | 82·4% (79·3–85·4) | 11 | 83·8% (79·1–88·5) |
UI=uncertainty interval.
Discussion
We found that preterm birth affected an estimated 10·6% of livebirths globally in 2014, equating to 14·84 million liveborn preterm newborn babies. Nearly 85% of preterm births occur in the late preterm period, and more than 80% occurred in Asia and sub-Saharan Africa.
There are several methodological challenges that confound estimation of preterm birth rates. In general, the later in pregnancy an estimate of gestational age is made, the greater is the uncertainty of that estimate.32 Ultrasound early in pregnancy for measurement of fetal crown–rump length is considered the gold standard for assessment of gestational age, with an accuracy of around ±5–7 days.32, 33 Less accurate methods, such as last menstrual period, symphysis–fundal height measurement, postnatal examination of the baby, or use of birthweight, are often used, particularly in low-income and middle-income countries where access to early antenatal ultrasound is poor or absent, and may be incorrect by 4 weeks or more.
The method of assessment of gestational age can affect population preterm birth rates, exemplified by changes in preterm birth reporting in the USA. From 2014, the USA has used the obstetric estimate of gestational age primarily for preterm birth reporting, rather than the last menstrual period method. Estimation based on last menstrual period gives higher preterm birth rates than obstetric estimates (although trends are similar).34 Consequently, the 2014 North American regional estimate (11·3%, UI 9·6–13·2) is driven by historical data from the USA based on last menstrual period, and is higher than the obstetric estimate of the US national rate for 2014 (9·6%). Most reports included in this study did not provide sufficient information on the method used to assess gestational age, which prevented its use in the model. The impact of assessment method on preterm birth rates and international comparisons is probably substantial; however, ensuring good quality antenatal care for all women throughout pregnancy is necessary to improve the quality of population data for gestational age data. WHO recommends antenatal ultrasound (before 24 weeks) for all pregnant women.35 Implementation of this recommendation in low-income and middle-income countries—as part of coordinated efforts to improve the quality of maternal and newborn care—could improve estimation of gestational age and changes in preterm birth rates.
Despite our extensive searches, data on preterm births were available disproportionately from high-income countries (where monitoring systems are generally more robust and antenatal ultrasound is more often used). Most countries do not report national CRVS data on preterm births, and there is no international indicator to assess CRVS coverage for preterm births specifically (our country classification used CRVS coverage for births as a proxy). Definitions differed between countries, including the definitions of fetal viability and preterm birth. ICD-10 does not advise a lower gestational age limit for fetal viability, rather advising use of “signs of life” to define a livebirth.36 In practice, definitions of livebirth may include thresholds for birthweight or gestational age. A lower threshold for fetal viability will capture more preterm births than would a higher threshold. Preterm data from Colombia, for example, used a preterm birth definition of less than 38 weeks' gestation, contributing to reported preterm birth rates of 18–19% in recent years. Other variations included the denominator population used to report preterm births, and whether certain exclusions were applied or not (such as excluding newborn babies with congenital malformations or multiple births). These differences can have varying effects on the preterm birth rate, and confound international comparisons.
Data for preterm births can be of variable quality, subject to misclassification and incompleteness. Preterm births can be misclassified as term births (or vice versa), and the misclassification of livebirths, stillbirths, and neonatal deaths can directly affect reporting of preterm birth in liveborns.37 Inclusion of stillbirths increases the overall preterm birth rate, particularly in low-income countries where stillbirth rates are high.38 Although model adjustments for differences in the definitions used in different countries can partly mitigate this, we were unable to adjust for all factors because of a lack of data, particularly on misclassification, heaping, and method of ascertainment of gestational age. International variations in preterm birth rates to some extent reflect differences in the definitions used rather than epidemiological differences and should be interpreted with caution. Modelling preterm birth using estimated covariates of other conditions can further increase uncertainty. The analysis of gestational age subgroups and contribution of multiple births are based only on a subset of the database for which those variables were available (disproportionately from high-income countries) and might thus be biased.
The use of non-population-representative data (such as research studies) is a limitation. In many low-income and middle-income countries, only small, facility-based research studies with limited information were available to inform estimation. These studies were often done in high-level hospitals in urban centres and are largely not nationally representative. This shortcoming is reflected in the greater uncertainty for estimates in lower-income countries. We advocate caution when interpreting national estimates that are based on research study data only (including Bangladesh, China, India, Nigeria, and Pakistan, which are all in the top ten countries for estimated number of preterm births). It is likely that estimates would change if higher-quality data were available. Mixing large CRVS datasets with data from research studies is not ideal. Hence, more population-representative studies (such as household surveys and large cohort studies), particularly from low-income and middle-income countries, are needed. These studies should use standardised, prospective measurement of gestational age (using reliable methods) from early pregnancy onwards.
Although we found that preterm birth rates are increasing in some high-income countries, caution is warranted in interpreting trends. The number of data points increased over time, and concomitant trends in model covariates could also be playing a part. Changes in preterm birth definitions, reductions in thresholds of viability, and improvements in CRVS coverage and birth registration might also contribute to apparent increases in preterm birth rates. The variation between regions in the proportion of preterm births less than 28 weeks' gestation suggests regional differences in viability; however, there were insufficient data in some regions to draw firm conclusions from this subanalysis. We were unable to report on spontaneous versus provider-initiated preterm birth rates because of a lack of data; however, the increasing use of obstetric interventions appears to be increasing preterm birth rates (particularly late preterm births) in some high-income countries.39 Although around 85% of preterm births occurred in the late preterm period, gestational age distributions might be subject to issues of heaping, similar to birthweight.40
More and better data on preterm birth would help address these limitations. We support the continued calls41, 42, 43 for improvements in birth registration (including gestational age assessment); they are critical for a range of health and social reasons, as well as to improve understanding of preterm birth epidemiology. Relatively simple measures, such as using standard operational definitions and subgroups (eg, by gestational age, or spontaneous vs provider-initiated preterm births), in collection and reporting of data for preterm births are also of great value. Every baby counts—whether stillborn or liveborn, preterm or term—yet counting cannot occur without reliable civil registration data collection and reporting systems.44
Given the global burden of preterm birth and its contribution to neonatal and child mortality, greater investments are needed to improve the quality of care for all pregnant women and newborn babies (including preterm newborn babies), as well as improving collection and monitoring of data for preterm birth. WHO is committed to reducing the health problems and lives lost as a result of preterm birth within the framework of the Global Strategy for Women's, Children's and Adolescents' Health.45 This effort includes working with Member States to strengthen the availability and quality of data on preterm births, developing updated estimates, working with partners to research preterm births, and developing and implementing clinical guidelines and tools to improve the management of pregnant women at risk of preterm birth and the care of preterm babies.46, 47, 48 In addition, the Every Newborn Action Plan specifies coverage targets for key interventions (such as kangaroo mother care and use of oxygen) to improve outcomes for preterm babies by 2020.49 Improvements in monitoring and evaluation of preterm birth should be well integrated into relevant local and national health statistics infrastructure and could be linked to initiatives to improve quality of care.
More research is needed on the mechanisms of spontaneous preterm birth, so it can be better predicted and prevented.50 For example, metabolic markers for assessment of gestational age could improve recognition of preterm birth.51 However, further research is needed to develop preventive interventions that are safe, effective, and scalable in low-resource settings, where most preterm-associated child mortality occurs.
Two previous estimates (in 2005 and 2010) on the global burden of preterm birth have been published.20, 21 The present analysis includes a larger dataset and uses revised methods compared with the previous estimates. Our 2014 estimates supersede previously published estimates; findings of the estimates published in 2012 for the period 1990–2010 are therefore not directly comparable to these estimates for 1990–2014. That said, global and regional rates of preterm birth are broadly similar to previous reports for earlier years. Differences between these and earlier national estimates probably relate to the few data points for many countries—estimates are thus sensitive to the addition of new preterm or covariate data. The absence of national estimates for countries where no or few preterm data were available can present a challenge to stakeholders. Because of the uncertainty as to the causes of preterm birth itself, as well as the inherent methodological limitations of national estimates, we provided the relevant regional estimate as guidance for these countries.
Preterm birth is a crucial global health issue, which must be addressed to reduce neonatal and child mortality globally and reach the Sustainable Development Goals. Better recognition, prevention, and management of preterm birth require efforts to improve the quality of maternal and newborn care more broadly. To better understand the global epidemiology of preterm birth, the quality and volume of data needs to be strengthened, including standardisation in definitions, measurement, monitoring, and reporting. Further research on causes of preterm birth, better tools for measuring preterm birth, and new interventions to prevent and manage the consequences of preterm birth (particularly in low-resource settings) are also needed.
Acknowledgments
Acknowledgments
This study was financially supported by UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Department of Reproductive Health and Research, WHO. The March of Dimes funded a meeting of the Technical Advisory Group. This Article represents the views of the authors only, and not the views of their institutions. We thank Rajiv Bahl, Ana Pilar Betrán, Mercedes Bonet, Lynn Hampson, Dina Khan, Jorge Lopez Camelo, Mariela Pawluk, and Jamie Perin for their contributions. We also thank all members of the Technical Advisory Group: Shabina Ariff, Hannah Blencowe, Rogelio Gonzalez Perez, Tanya Guenther, Bo Jacobsson, Michael Kramer (chair), Gertrude Namazzi, Jeff Murray, Lisa Noguchi, Joe-Leigh Simpson, Dilys Walker, and Jennifer Zeitlin.
Contributors
JPV, SC, PL, and AMG had the idea for the study. All authors designed the study, collected and analysed data, and revised and approved the report. JPV and SC wrote the first draft of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths, Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56:247–253. [PubMed] [Google Scholar]
- 2.UN Inter-Agency Group for Child Mortality Estimation . United Nations Children's Fund; New York: 2017. Levels and trends in child mortality: Report 2017. [Google Scholar]
- 3.Kinney HC. The near-term (late preterm) human brain and risk for periventricular leukomalacia: a review. Semin Perinatol. 2006;30:81–88. doi: 10.1053/j.semperi.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Ramenghi LA. Late preterm babies and the risk of neurological damage. Acta Biomed. 2015;86(suppl 1):36–40. [PubMed] [Google Scholar]
- 5.Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;379:445–452. doi: 10.1016/S0140-6736(11)61577-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–269. doi: 10.1016/S0140-6736(08)60136-1. [DOI] [PubMed] [Google Scholar]
- 7.Araujo BF, Zatti H, Madi JM, Coelho MB, Olmi FB, Canabarro CT. Analysis of neonatal morbidity and mortality in late-preterm newborn infants. J Pediatr. 2012;88:259–266. doi: 10.2223/jped.2196. [DOI] [PubMed] [Google Scholar]
- 8.Platt MJ. Outcomes in preterm infants. Public Health. 2014;128:399–403. doi: 10.1016/j.puhe.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74(suppl 1):35–49. doi: 10.1038/pr.2013.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Dommelen P, Verkerk PH, van Straaten HL, Dutch Neonatal Intensive Care Unit Neonatal Hearing Screening Working Group J Pediatr. 2015;166:840–43 e1. [Google Scholar]
- 11.O'Connor AR, Wilson CM, Fielder AR. Ophthalmological problems associated with preterm birth. Eye. 2007;21:1254–1260. doi: 10.1038/sj.eye.6702838. [DOI] [PubMed] [Google Scholar]
- 12.Berard A, Le Tiec M, De Vera MA. Study of the costs and morbidities of late-preterm birth. Arch Dis Child Fetal Neonatal Ed. 2012;97:F329–F334. doi: 10.1136/fetalneonatal-2011-300969. [DOI] [PubMed] [Google Scholar]
- 13.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281:799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korvenranta E, Lehtonen L, Rautava L. Impact of very preterm birth on health care costs at five years of age. Pediatrics. 2010;125:e1109–e1114. doi: 10.1542/peds.2009-2882. [DOI] [PubMed] [Google Scholar]
- 15.Petrou S, Abangma G, Johnson S, Wolke D, Marlow N. Costs and health utilities associated with extremely preterm birth: evidence from the EPICure study. Value Health. 2009;12:1124–1134. doi: 10.1111/j.1524-4733.2009.00580.x. [DOI] [PubMed] [Google Scholar]
- 16.Teune MJ, Bakhuizen S, Gyamfi Bannerman C. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011;205:374 e1–374 e9. doi: 10.1016/j.ajog.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 17.ACOG Committee Opinion No 579: definition of term pregnancy. Obstet Gynecol. 2013;122:1139–1140. doi: 10.1097/01.AOG.0000437385.88715.4a. [DOI] [PubMed] [Google Scholar]
- 18.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muglia LJ, Katz M. The enigma of spontaneous preterm birth. N Engl J Med. 2010;362:529–535. doi: 10.1056/NEJMra0904308. [DOI] [PubMed] [Google Scholar]
- 20.Blencowe H, Cousens S, Oestergaard MZ. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 21.Beck S, Wojdyla D, Say L. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–38. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vogel JP, Chawanpaiboon S, Watananirun K. Global, regional and national levels and trends of preterm birth rates for 1990 to 2014: protocol for development of World Health Organization estimates. Reprod Health. 2016;13:76. doi: 10.1186/s12978-016-0193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO Countries. 2017. http://www.who.int/countries/en/
- 24.Mikkelsen L, Phillips DE, AbouZahr C. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386:1395–1406. doi: 10.1016/S0140-6736(15)60171-4. [DOI] [PubMed] [Google Scholar]
- 25.WHO . World Health Organization; Geneva: 2015. World Health Statistics 2015.http://www.who.int/gho/publications/world_health_statistics/2015/en/ [Google Scholar]
- 26.UN The United Nations Statistics Division. https://unstats.un.org/home/nso_sites/
- 27.The DHS Program Demographic and Health Surveys. http://dhsprogram.com/
- 28.CDC Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion Reproductive Health Surveys. https://www.cdc.gov/reproductivehealth/global/tools/surveys.htm
- 29.Papageorghiou AT, Ohuma EO, Altman DG. International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet. 2014;384:869–879. doi: 10.1016/S0140-6736(14)61490-2. [DOI] [PubMed] [Google Scholar]
- 30.UN Statistics Division Methodology—standard country or area codes for statistical use (M49) https://unstats.un.org/unsd/methodology/m49/
- 31.UNDP World Population Prospects. 2017. http://esa.un.org/wpp/
- 32.Lynch CD, Zhang J. The research implications of the selection of a gestational age estimation method. Paediatr Perinat Epidemiol. 2007;21(suppl 2):86–96. doi: 10.1111/j.1365-3016.2007.00865.x. [DOI] [PubMed] [Google Scholar]
- 33.Committee on Obstetric Practice. the American Institute of Ultrasound in Medicine. the Society for Maternal-Fetal Medicine Committee opinion No 700: methods for estimating the due date. Obstet Gynecol. 2017;129:e150–e154. doi: 10.1097/AOG.0000000000002046. [DOI] [PubMed] [Google Scholar]
- 34.Hamilton B, Martin J, Osterman M. US Department of Health and Human Services; Atlanta, GA: 2015. National vital statistics reports. Births: preliminary data for 2015. [PubMed] [Google Scholar]
- 35.WHO WHO recommendations on antenatal care for a positive pregnancy experience. 2016. http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf [PubMed]
- 36.WHO . World Health Organization; Geneva: 2004. ICD-10: International Statistical Classification of Diseases and Related Health Problems-Instruction Manual. [Google Scholar]
- 37.Liu L, Kalter HD, Chu Y. Understanding misclassification between neonatal deaths and stillbirths: empirical evidence from Malawi. PLoS One. 2016;11:e0168743. doi: 10.1371/journal.pone.0168743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morisaki N, Ganchimeg T, Vogel JP. Impact of stillbirths on international comparisons of preterm birth rates: a secondary analysis of the WHO multi-country survey of Maternal and Newborn Health. BJOG. 2017;124:1346–1354. doi: 10.1111/1471-0528.14548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richards JL, Kramer MS, Deb-Rinker P. Temporal trends in late preterm and early term birth rates in 6 high-income countries in North America and Europe and association with clinician-initiated obstetric interventions. JAMA. 2016;316:410–419. doi: 10.1001/jama.2016.9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Channon AA, Padmadas SS, McDonald JW. Measuring birth weight in developing countries: does the method of reporting in retrospective surveys matter? Matern Child Health J. 2011;15:12–18. doi: 10.1007/s10995-009-0553-3. [DOI] [PubMed] [Google Scholar]
- 41.United Nations Children's Fund . UNICEF; New York, NY: 2013. A passport to protection: a guide to birth registration programming. [Google Scholar]
- 42.World Bank. WHO . World Bank Group; Washington, DC: 2014. Global civil registration and vital statistics: scaling up investment plan 2015–2024. [Google Scholar]
- 43.WHO. Civil registration and vital statistics 2013: challenges, best practice and design principles for modern systems. Geneva, Switzerland; 2013.
- 44.WHO Making every baby count: audit and review of stillbirths and neonatal deaths. 2016. http://www.who.int/maternal_child_adolescent/documents/stillbirth-neonatal-death-review/en/
- 45.WHO Promoting health through the life-course. 2016. http://www.who.int/life-course/partners/global-strategy/en/
- 46.WHO Preterm birth. Fact sheet: reviewed November 2016. http://www.who.int/news-room/fact-sheets/detail/preterm-birth
- 47.Tuncalp, Were WM, MacLennan C. Quality of care for pregnant women and newborns-the WHO vision. BJOG. 2015;122:1045–1049. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.WHO WHO recommendations on interventions to improve preterm birth outcomes. http://apps.who.int/iris/bitstream/10665/183037/1/9789241508988_eng.pdf [PubMed]
- 49.WHO. UNICEF . World Health Organization; Geneva: 2014. Every Newborn: an action plan to end preventable deaths. [Google Scholar]
- 50.Lopez Bernal A. Overview. Preterm labour: mechanisms and management. BMC Pregnancy Childbirth. 2007;7(suppl 1):S2. doi: 10.1186/1471-2393-7-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.D'Silva AM, Hyett JA, Coorssen JR. Proteomic analysis of first trimester maternal serum to identify candidate biomarkers potentially predictive of spontaneous preterm birth. J Proteomics. 2018;178:31–42. doi: 10.1016/j.jprot.2018.02.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.