Abstract
Switzerland has not yet reached the measles vaccination coverage of 95 percent that is recommended by the World Health Organization to achieve herd immunity. Within the overall objective of informing effective ways to promote the combined Measles, Mumps, Rubella (MMR) vaccination in Switzerland, the aim of this study was to identify predictors of parents’ intention to adhere to official MMR vaccination recommendations. Between October 2012 and January 2013, we surveyed 554 parents of middle school students aged 13 to 15 in Ticino, Switzerland. Guided by Protection Motivation Theory (PMT), the survey covered predictors related to threat and coping appraisal with regards to measles and the MMR vaccine, MMR-related social attitudes and social norms, past experience with the disease and the vaccine, and information sources in the MMR vaccine context. Data were analyzed using Structural Equation Modelling. Among central PMT concepts describing people’s threat and coping appraisal, only response (vaccination) efficacy showed to be directly related to parents’ intention to adhere to MMR vaccination recommendations (B = .39, p < .001). In addition, social attitudes (B = .38, p < .001) were a direct predictor. Furthermore, social attitudes, social norms, knowing somebody who experienced MMR vaccination side effects, and having sought MMR information from public health institutions, all indirectly predicted parents’ intention to adhere to MMR recommendations by activating different threat and coping appraisal mechanisms. To conclude, future communication measures from public health institutions should highlight the altruistic aspect (herd immunity) of the immunization practice as well as present evidence on the high effectiveness of the vaccination in reducing the risk at both the individual and collective levels of getting infected with measles.
Keywords: MMR, Childhood vaccination, Protection Motivation Theory, Parents, Switzerland
Highlights
-
•
Switzerland has not yet reached the 95% MMR vaccination coverage goal set by the WHO.
-
•
PMT allows to study parents’ intentions to follow MMR vaccination recommendations.
-
•
Perceived efficacy of the MMR vaccine is the strongest direct predictor of intentions.
-
•
Pro-social attitudes in favor of herd immunity also directly and indirectly predict intentions.
-
•
Doctors and public health institutions should highlight these aspects.
1. Introduction
As most European countries, Switzerland aims at achieving the goal set by the World Health Organization (WHO) to eliminate measles by 2020 (World Health Organization, 2016). However, although the WHO recommends a 95 percent vaccination coverage (World Health Organization, 2009), to date only 87 percent of 2-year-old children living in Switzerland have received the necessary two doses of a measles vaccine such as Measles Mumps Rubella (MMR) (Swiss Federal Office of Public Health, 2018a). Sub-optimal MMR coverage resulted in a number of measles outbreaks in Switzerland in the last two decades (Lang, 2007, Swiss Federal Office of Public Health, 2018a). The number of measles cases doubled between 2015 and 2016 from 35 to 71 cases annually. While 17 cases were registered between January and April 2018, 2017 was marked by as many as 105 new cases. Between late December 2016 and early February 2017, 22 cases of measles occurred in the Italian-speaking part of Switzerland, mostly among adults, making Ticino and Grigioni the two Cantons with the highest incidence in this period (Swiss Federal Office of Public Health, 2017a).
Given the continuous struggle to achieve the WHO-set goal, it is most important to identify the factors that influence parents’ attitudes towards childhood vaccination in general and their decision for or against the MMR vaccination in particular. Theory-based empirical research and interventions are preferential if not imperative for successful health behavior promotion (Lippke & Ziegelmann, 2008). Theories allow to synthesize and generalize complex processes beyond a specific context. They further allow to formulate intervention recommendations for public health organizations concerned with measles vaccine communication measures and campaigns in Switzerland and abroad.
The aim of the present paper is to understand what predicts parents’ intention to adhere to official MMR vaccination recommendations in Switzerland; this aim is to be reached by applying the Protection Motivation Theory (PMT), originally developed by Rogers (1975), in the context of the MMR vaccination.
1.1. Theoretical background
PMT has been applied to different health-related behaviors including vaccination (for a meta-analysis see Floyd, Prentice-Dunn, & Rogers, 2000; Milne, Sheeran, & Orbell, 2000). The theory has established social cognitive determinants in common with other behavioral theories including the Health Belief Model (HBM), Theory of Reasoned Action and Theory of Planned Behavior (TPB), Social Cognitive Theory as well as Health Action Process Approach (Lippke & Ziegelmann, 2008). For example, PMT shares with the HBM (Smith et al., 2011) and social theories of risk (for an overview see Casiday, 2007) the notion that the intention to adopt a protective behavior (e.g. vaccinating) results from perceiving a given threat (e.g. disease) and desiring to avoid the negative outcomes of such a threat (Floyd et al., 2000). The strength of PMT lies in the fact that it takes into account people’s threat perceptions in terms of severity of and vulnerability towards experiencing an advert event, and the costs (e.g., personal resources) involved in avoiding it. While the first cognitive mechanism presents a threat appraisal, the second, related to response costs, presents a coping appraisal. A revised version of PTM (Maddux & Rogers, 1983) also considers people’s belief in their own capacities in engaging in a specific behavior (self-efficacy) as it has been found to be crucial in triggering “motivational, cognitive and affective processes” (Floyd et al., 2000). In addition, the theory takes into account efficacy beliefs related to the behavior itself and the outcomes it brings (response efficacy). According to the PMT, efficacy beliefs and perceived response costs constitute people’s coping appraisal. Furthermore, both threat and coping appraisal determine people’s motivation (or intention) to protect themselves from experiencing an advert event. As such, PMT combines core concepts of risk perception theories (e.g., HBM) and behavioral action theories (e.g., TPB).
PMT has been furthermore extended to include information sources, intrapersonal characteristics, and prior experiences associated with threat and coping appraisal (Floyd et al., 2000, Milne et al., 2000, Rogers, 1983). This way, the revised PMT applies a more holistic approach towards the understanding of behavioral intentions by incorporating contextual factors related to the living environment, information sources, and social norms as additional determinants of health-related behaviors, especially relevant in the context of vaccination as shown in a comprehensive framework by Betsch, Böhm, and Chapman (2015). Information sources cover informal and formal sources as well as interpersonal contacts and media coverage. Intrapersonal characteristics include, among others, social attitudes and perceived social norms with regards to threat and coping appraisal as well as the behavioral intention. Eventually, prior experiences with the (health) context are said to determine risk and severity perceptions as well as efficacy beliefs in relation to a specific (health) behavior. In the present paper, the extended version of PMT is used to better understand potential predictors of parents’ intention to adhere to official MMR vaccination recommendations in Switzerland.
1.2. The context of the MMR vaccination
PMT was successful in predicting hepatitis B vaccination intention and behavior among an adult population (Liu et al., 2016). However, MMR vaccination differs from hepatitis B vaccination inasmuch as it requires parents to make a vaccination decision for their child, which implies different cognitive mechanisms and the responsibility over another individual (Meszaros et al., 1996). Compared to other widely accepted childhood vaccinations such as diphtheria, tetanus, pertussis (DTaP), the measles containing MMR vaccination has been heavily doubted in the general public after the Lancet published an article in 1998 linking the MMR vaccine to autism. Although the article was later retracted by the journal editors (see also Rao & Andrade, 2011), it set off a highly-publicized controversy about the safety of the MMR vaccine potentially influencing parents’ MMR vaccination decision (Lewis and Speers, 2003, Smith et al., 2008).
The fluctuation in MMR vaccination rates over the last decades hints towards changes in parents’ perceptions of their child’s susceptibility towards negative MMR vaccination side effects. The severity of these effects, i.e., autism, has changed their intentions to follow (inter-)national MMR vaccination recommendations. While MMR coverage rates among children born in affluent countries like Switzerland before the late 1990s are generally high (Sansonetti, 2018, World Health Organization, 2018), they only increased slightly among younger children since the early 2000s and rates at two doses are generally low (37% between 1999 and 2003) (Swiss Federal Office of Public Health, 2018b).
As such, much research to date has focused on parents of young children and their intention to comply with the MMR vaccination schedule (e.g., Fadda, Depping, & Schulz, 2015b; Flynn & Ogden, 2004; Gellatly, McVittie, & Tiliopoulos, 2005). The schedule foresees two doses of a measles vaccine such as MMR by the age of two in most European countries including Switzerland (Swiss Federal Office of Public Health, 2017b). If older children, adolescents, or adults have missed a dose or two, they are highly recommended to receive the MMR vaccine at any age to be sufficiently protected (Swiss Federal Office of Public Health, 2018b). If they are still underage, parents need to make the vaccination decision for them. However, less is known about the vaccination intention of parents with children born at the advent of the controversy, that is between 1997 and 1999. These parents were asked to make a decision for their child at the time when insecurity among the general public was high and public health efforts alleviating the negative publicity of the MMR vaccination were not yet widely diffused. Therefore, the present study is concerned with factors that predict the intention of parents of adolescents to adhere to official MMR vaccination recommendations in Switzerland making use of PMT.
1.3. PMT and the MMR vaccination
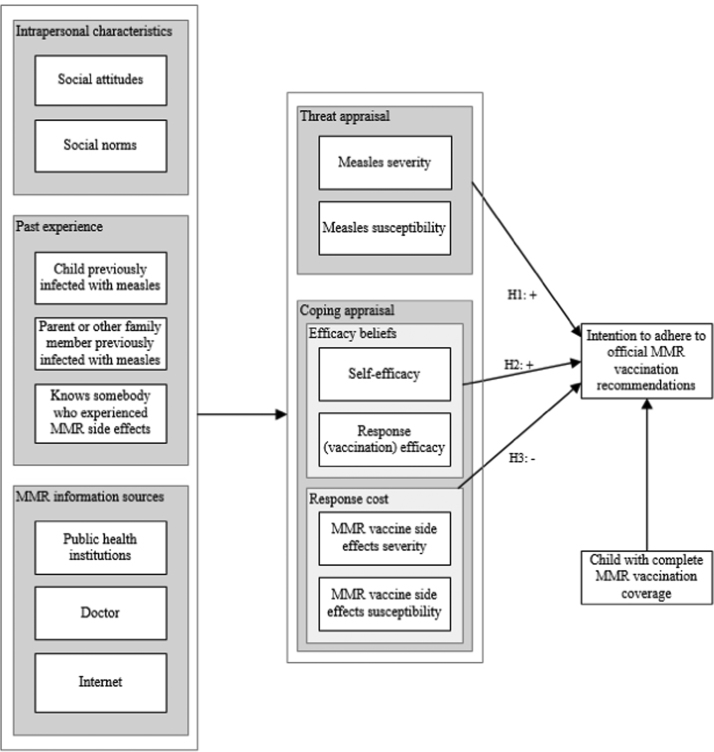
In the context of the MMR vaccination, the core concepts of the threat appraisal within PMT include parents’ perceived severity of measles and the belief that their child is susceptible towards the disease. Perceived disease severity and susceptibility are considered to be positively associated with the behavioral intention to disease avoidance (Brewer et al., 2007). This leads us to the following hypothesis:
H1
The higher the perceived severity of and susceptibility to measles, the higher parents’ intention to follow official MMR vaccination recommendations.
Coping appraisal, which is the evaluation of the adaptive response to the threat, is composed by efficacy variables (self-efficacy and response efficacy) and response costs (Rogers, 1975). More recently, self-efficacy has received attention in the MMR vaccination decision-making context as a sub-dimension of psychological empowerment (Fadda, Galimberti, Carraro, & Schulz, 2016). In the context of the MMR vaccination, perceived response efficacy describes parents’ belief in the effectiveness of the vaccination in protecting their children from the disease. Strong positive correlations with intention and vaccination status were found in previous studies for the perceived effectiveness of vaccination (Bennett and Smith, 1992, Meszaros et al., 1996, Pareek and Pattison, 2000). Likewise, self-efficacy and perceived behavioral control (the equivalent of self-efficacy) were found to be significant positive predictors of preventive health behavioral intention (Maddux & Rogers, 1983), and vaccination in particular (Britt, Hatten, & Chappuis, 2014). Based on these findings, we hypothesize that:
H2
The higher parents’ perceived self-efficacy and response efficacy, the higher their intention to follow official MMR vaccination recommendations.
On the other hand, response costs are any costs associated with performing the adaptive coping response (Rogers, 1975). They may include negative outcomes that can be experienced by an individual because of adopting the protective measure suggested (e.g., side effects after the inoculation of the vaccine). Regarding the severity of the risks attached to the vaccine, research found that parents who delayed and refused vaccines were significantly less likely to believe that vaccines are safe (Betsch and Sachse, 2012, Gust et al., 2008, Smith et al., 2011, Thorpe et al., 2012) and more likely to believe that vaccination is unhealthy (Flynn & Ogden, 2004). In a similar fashion, Bennett and Smith found that those who did not vaccinate their children had significantly more concern over their child experiencing long-term health problems as a result of the vaccination than respondents who fully or partially vaccinated their children (Bennett & Smith, 1992). The importance attached to the risk of adverse reactions also plays a role in predicting vaccination status (Gellatly et al., 2005), so does the number of reported vaccine concerns (Wheeler & Buttenheim, 2013). In light of these findings, we formulate the following hypothesis:
H3
The higher parents’ perceived severity of and susceptibility to MMR vaccine side effects, the lower their intention to follow official MMR vaccination recommendations.
Concerning intra- and interpersonal characteristics beyond the core concepts related to threat and coping appraisal within PMT, the present study takes into account parents’ social attitudes and norms with regards to the MMR vaccination (Bennett and Smith, 1992, Betsch et al., 2017, Brown et al., 2011, Skea et al., 2008), their past experiences, which include any direct experiences with measles or MMR vaccination side effects as well as indirect experiences, that is, knowing somebody (including their child) who was previously inflected with measles or experienced negative MMR vaccination side effects (Freeman & Freed, 1999). Past behavior in relation to the MMR vaccination is accounted for by directly linking parents’ prior decision to vaccinate their adolescent child against measles to their behavioral intentions to follow MMR vaccination recommendations, which are particularly crucial for this age group given that adolescents and young adults are, in some countries, the most vulnerable group in terms of susceptibility to measles (Filia et al., 2017, Kimura and Nishiyama, 2007, Rathi et al., 2017). Eventually, formal and informal online and offline information sources on the disease and the vaccination are taken into account as they may have differential effects on parents’ threat and coping appraisal and their subsequent behavioral intention to adhere to official MMR vaccination recommendations (Betsch and Sachse, 2012, Fadda et al., 2015a, Jones et al., 2012, Lewis and Speers, 2003).
All factors and derived hypotheses of the extended PMT model are summarized in Fig. 1. Using Structural Equation Modelling, we aim to identify which of these factors are linked to parents’ intention to adhere to official MMR vaccination recommendations while controlling for their past MMR vaccination decision. By doing this, we are able to formulate intervention recommendations for MMR vaccine communication measures and campaigns in Switzerland.
Fig. 1.
Hypothesized extended PMT model applied to the context of the MMR vaccination.
2. Methods
2.1. Recruitment and procedure
Survey and MMR coverage data were collected between October 2012 and January 2013. All parents of adolescents attending the third year of obligatory middle school in Ticino (N=3,249) received a letter from the Cantonal Office of Public Health in Ticino in which they were asked to provide the children with their vaccination card. Together with the letter, parents received an invitation to participate in a survey on parents’ attitudes towards childhood vaccination conducted by [name of the institution omitted for blind review]. Parents who agreed to participate in the study (n=891) filled out an enclosed response card which asked them to provide their informed consent and indicate details for their preferred form of contact (regular mail, e-mail or phone). Adolescents brought both the vaccination and response cards to school, where certified school doctors checked the vaccination status and specified on the back of the response card whether the adolescent was not at all vaccinated (0 dose), under-vaccinated (1 dose) or fully vaccinated (2 doses) against MMR. All completed response cards were forwarded to [name of the institution omitted for blind review]. Based on their preferred form of contact, parents received a standardized self-administered questionnaire. Parents were contacted up to two times by letter or telephone and up to three times by email to increase the response rate. Once parents’ responses were collected and matched to adolescents’ MMR vaccination coverage data, personal contact details were deleted to obtain an anonymized dataset for further analyses. The procedure was approved by the ethics committee of Canton Ticino.
2.2. Measures
Unless otherwise noted, the following measures were assessed on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree).
2.2.1. Intention to adhere to official MMR recommendations
Intention was measured with a single item (“I follow official recommendations regarding MMR vaccination”; Mean (M) = 5.50, Standard Deviation (SD) = 1.68).
2.2.2. Threat appraisal
Measles severity was assessed with a single item (“Measles is an infective disease that can have severe consequences for one’s health”; M = 6.08, SD = 1.33).
Likewise, measles susceptibility was assessed with a single item (“If my child wasn’t vaccinated against measles, he would be likely to suffer from the disease during the course of his life”; M = 5.43, SD = 1.64).
2.2.3. Coping appraisal
Self-efficacy was measured with three items adapted from the competence dimension of the Psychological Empowerment Scale (Spreitzer, 1995). These were “I am confident about my ability to decide regarding the MMR vaccination of my child”, “I have the necessary skills to decide whether to vaccinate my child against measles”, “I trust my ability to make decisions regarding the MMR vaccination of my child”. They were averaged to create a compound score; M = 5.12, SD = 1.55, α = .82.
Response (vaccination) efficacy was measured with three items adapted from Brown and colleagues’ scale (Brown et al., 2011) on attitudinal predictors of MMR vaccine acceptance (“The vaccination against measles is not efficient enough for fighting the disease”, “It is possible to prevent measles by vaccinating during childhood” and “Only pharmaceutical companies can profit from the MMR vaccination”). Two items were reverse coded before calculating an average compound score; M = 5.84, SD = 1.15, α = .55.
Response costs were measured as MMR vaccine side-effects susceptibility (“It is likely that my child will have side-effects from MMR vaccine”; M = 3.85, SD = 1.79) and MMR vaccine side-effects severity (“The side-effects of MMR vaccine can be severe”; M = 4.07, SD = 1.82).
2.2.4. Intrapersonal characteristics
Social attitudes were assessed with a single item (“The vaccination of my child helps to prevent the diffusion of measles in the population”; M = 6.22, SD = 1.39.).
Similarly, social norms were measured with a single item describing injunctive norms (“Most parents I know vaccinate their children against measles”; M = 5.65, SD = 1.50).
2.2.5. Past experience
Past experience with measles and MMR side effects was measured with a binary response format where 1 indicated “yes, parent had made the experience” and 0 “no, parent had not made it”. The questionnaire differentiated between one’s own child having previously been infected with measles (7%), parents or somebody else in the family having previously been infected with measles (53%), and parents knowing somebody who experienced MMR side effects (5%).
2.2.6. MMR information sources
Information sources were assessed by asking if parents had actively sought information about MMR vaccination (coded as 1) or not (coded as 0) from public health institutions such as the Cantonal office of public health (3%), doctors (29%), and the Internet (15%).
2.2.7. Socio-demographics
In addition, the questionnaire assessed parents’ age, highest educational attainment, and nationality. Information on children’s age and MMR vaccination coverage were also available.
3. Results
3.1. Sample
The final sample consisted of 554 out of 891 (62%) parents with valid survey data. Of 554 parents, 253 (46%) opted for a paper-and-pencil questionnaire and a prepaid self-addressed envelope, 276 (50%) for a link to an online questionnaire, and 25 (4%) for a computer assisted telephone interview. In the majority of cases (88%), the mother answered the survey confirming her central role in the care of and decisions regarding the health of their offspring. Among respondents, the modal level of highest educational attainment was apprenticeship or professional school (n = 246; 44%), in 149 cases (27%) respondents held a university degree. Four in five adolescents (80%) had at least one parent with Swiss nationality, 91 (16%) had at least one parent with a European Union nationality and in 18 cases (3%) the family had a Non-European origin. According to recent census data (Federal Statistical Office, 2018), the distribution of educational level and nationality in our sample reflects that of the Ticino population in the corresponding age group, although the percentage of people with a university degree in our sample was slightly higher than the one in the general population. Children’s age ranged between 13 and 15 years, and 11.3% did not have the recommended two doses of the MMR vaccine. Table 1 summarizes socio-demographic characteristics divided for each parent and the child.
Table 1.
Sample characteristics (n=554).
| Mother |
Father |
Child |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Highest educational attainment | ||||||
| Obligatory school | 58 | 10.5 | 38 | 6.9 | ||
| Apprenticeship/professional school | 245 | 44.2 | 247 | 44.6 | ||
| High school | 149 | 26.9 | 81 | 14.6 | ||
| University of applied sciences | 38 | 6.9 | 59 | 10.6 | ||
| University | 56 | 10.1 | 84 | 15.2 | ||
| No answer | 8 | 1.4 | 45 | 8.1 | ||
| Nationality | ||||||
| Swiss | 403 | 72.8 | 310 | 56.0 | ||
| Other European | 113 | 20.4 | 128 | 23.1 | ||
| Non-European | 28 | 5.1 | 19 | 3.4 | ||
| No answer | 10 | 1.8 | 97 | 17.5 | ||
| MMR coverage | ||||||
| No dose | 49 | 8.8 | ||||
| 1 dose | 14 | 2.5 | ||||
| 2 doses | 491 | 88.6 | ||||
| M | SD | M | SD | M | SD | |
| Age | 45.9 | 4.5 | 48.6 | 5.6 | 13.1 | 0.4 |
3.2. Preliminary results
Data were analysed in SPSS© v.23 and AMOS© v.22. First, data were evaluated for missingness and normal distribution of continuous variables. The number of missing values at the univariate level was minimal and never exceeded 2 percent of the overall sample. Furthermore, data were missing at random. The model was run on a dataset with imputed values for missing data using an Expectation Maximization algorithm implemented in SPSS. Examination of skewness and kurtosis at the univariate level revealed somewhat troublesome kurtosis values for social attitude (K = 4.65) and perceived severity of measles (K = 2.28). In addition, Mardia’s test pointed towards multivariate non-normality. Thus, the model was run on 2,000 Bootstrap replications. Table 2 provides a correlation matrix with bivariate relationships among all factors of the model.
Table 2.
Bivariate correlations among concepts of PMT model.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Intention to adhere | .225** | .181** | .054 | .435** | −.126** | −.117* | .445** | .220** | −.157** | −.087* | −.107* | .060 | .019 | .022 | .153** |
| 2 Measles severity | .318** | .180** | .325** | .058 | .026 | .379** | .218** | −.049 | −.019 | .047 | .064 | .124** | .042 | .083 | |
| 3 Measles susceptibility | .172** | .269** | .008 | .133** | .222** | .123** | .047 | .064 | .028 | .048 | .072 | .044 | .094* | ||
| 4 Self-efficacy | .151** | .032 | .025 | .201** | .108** | −.030 | .059 | −.001 | .037 | .128** | .091* | .013 | |||
| 5 Response efficacy | −.158** | −.150** | .444** | .290** | −.141** | −.030 | −.084* | .099* | .144** | .118* | .086* | ||||
| 6 MMR vaccine side effects severity | .464** | −.089* | −.081 | −.014 | .029 | .143** | .031 | .034 | −.033 | −.102* | |||||
| 7 MMR vaccine side effects susceptibility | −.082 | −.054 | −.034 | .033 | .137** | .096* | .040 | −.085* | −.094* | ||||||
| 8 Social attitudes | .335** | −.151** | −.018 | −.030 | −.011 | .086* | .079 | .056 | |||||||
| 9 Social norms | .051 | −.062 | .022 | −.006 | −.001 | .013 | .001 | ||||||||
| 10 Child infected with measles | .208** | .103* | −.047 | −.060 | .007 | −.086* | |||||||||
| 11 Other family member infected with measles | .101** | .058 | .096* | −.017 | −.006 | ||||||||||
| 12 Knowing somebody with MMR side effects | .142** | .087* | .042 | −.072 | |||||||||||
| 13 MMR information from public health institution | .119** | .085* | −.056 | ||||||||||||
| 14 MMR information from doctor | .319** | .017 | |||||||||||||
| 15 MMR information from Internet | −.021 | ||||||||||||||
| 16 complete MMR vaccination coverage |
Note: n=554; coefficients based on 2,000 Bootstrap replications with 95% confidence interval
p < .05
p < .01
3.3. Primary results
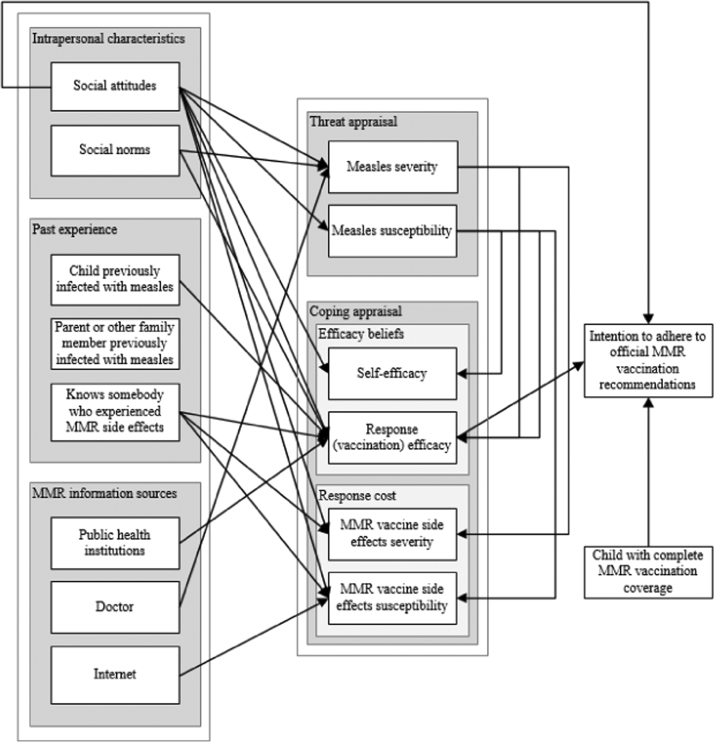
The hypothesized PMT model in Fig. 1 was evaluated with Structural Equation Modelling, which allows to test for mediation effects. As such, it is a suitable technique for testing the extended PMT as it estimates path coefficients for all relationships at the same time (Kline, 2015). Absolute and comparative goodness of fit indices for the initial hypothesized model pointed towards a bad model fit: Bollen-Stine p < .001, RSMEA = .101, p value for the test of close fit < .001, CFI = .870. Modification indices above 4 indicated an additional direct path from social attitudes to adhere to MMR recommendations, and from threat appraisal components to coping appraisal components. After adding these theoretically meaningful modifications, model fit indices improved and an acceptable model fit was achieved: Bollen-Stine p = .054, RSMEA = .041, p value for the test of close fit = .720, CFI = .985.
Table 3 and Fig. 2 summarize the results for the extended PMT model, whose predictors explain 28 percent of variance in parents’ intention to adhere to official MMR vaccination recommendations as the final outcome variable. The results will be described by focusing on significant direct and indirect relationships with intention as the final outcome variable. Concerning the central PMT concepts related to threat and coping appraisal, only response (vaccination) efficacy showed to be significantly positively related to parents’ intention to adhere (B = .40, p < .001) (H2 partly confirmed). More precisely, a one point increase on the 7-point response efficacy scale led to a .40-point increase on the 7-point intention to adhere scale. None of the other concepts describing parents’ threat and coping appraisal proved to be significant predictors of their intention to follow MMR vaccination recommendations (H1 and H3 not confirmed). Instead, intention was directly positively associated with children’s MMR coverage (B = .54, p = .004), meaning that, on average, parents of children who received the two MMR vaccine doses in the past reported .54 points higher intentions to follow the official MMR vaccination schedule. When it comes to antecedents of the central PMT model, intention was directly positively related to respondents’ social attitudes (B = .38, p < .001), that is, their willingness to vaccinate one’s child to help contain the diffusion of measles in the population. Response efficacy, in turn, was significantly associated with the two intrapersonal characteristics, social attitudes (B = .24, p < .001) and social norms (B = .12, p < .001), past experience, that is, having a child who experienced measles (B = −.40, p = .020) and knowing somebody who experienced MMR vaccine side effects (B = −.52, p = .006), as well as having sought information on the MMR vaccine from public health institutions (B = .54, p = .019). In addition, response efficacy as one component of coping appraisal was significantly positively associated with both threat appraisal components, that is, measles severity (B = .11, p = .002) and measles susceptibility (B = .10, p < .001).
Table 3.
Unstandardized and standardized direct, indirect and total effects on intention to adhere to official MMR vaccination recommendations and threat and coping appraisal components.
| B | Beta | p | |
|---|---|---|---|
| Direct effect on intention | |||
| Measles severity (H1) | .012 | .010 | .810 |
| Measles susceptibility (H1) | .041 | .039 | .318 |
| Self-efficacy (H2) | −.063 | −.058 | .119 |
| Response efficacy (H2) | .399 | .273 | <.001 |
| MMR vaccine side effects severity (H3) | −.027 | −.029 | .477 |
| MMR vaccine side effects susceptibility (H3) | −.030 | −.032 | .446 |
| Complete MMR coverage | .544 | – | .004 |
| MI: Social attitudes | .381 | .313 | <.001 |
| Direct effect on measles severity | |||
| Social attitudes | .329 | .342 | <.001 |
| Social norms | .090 | .101 | .015 |
| Child previously infected with measles | .037 | – | .864 |
| Parent or other family member previously infected with measles | −.068 | – | .526 |
| Knows somebody who experienced MMR side effects | .267 | – | .267 |
| MMR information from public health institutions | .403 | – | .164 |
| MMR information from doctor | .279 | – | .023 |
| MMR information from Internet | −.089 | – | .560 |
| Direct effect on measles susceptibility | |||
| Social attitudes | .252 | .213 | <.001 |
| Social norms | .056 | .051 | .245 |
| Child previously infected with measles | .462 | – | .102 |
| Parent or other family member previously infected with measles | .157 | – | .260 |
| Knows somebody who experienced MMR side effects | .082 | – | .792 |
| MMR information from public health institutions | .390 | – | .299 |
| MMR information from doctor | .162 | – | .310 |
| MMR information from Internet | .036 | – | .855 |
| Direct effect on self-efficacy | |||
| Social attitudes | .135 | .120 | .011 |
| Social norms | .044 | .042 | .337 |
| Child previously infected with measles | −.124 | – | .642 |
| Parent or other family member previously infected with measles | .179 | – | .174 |
| Knows somebody who experienced MMR side effects | −.138 | – | .639 |
| MMR information from public health institutions | .118 | – | .741 |
| MMR information from doctor | .269 | – | .075 |
| MMR information from Internet | .212 | – | .258 |
| MI: Measles severity | .093 | .080 | .082 |
| MI: Measles susceptibility | .098 | .103 | .018 |
| Direct effect on response (vaccination) efficacy | |||
| Social attitudes | .240 | .288 | <.001 |
| Social norms | .120 | .156 | <.001 |
| Child previously infected with measles | −.403 | – | .020 |
| Parent or other family member previously infected with measles | −.010 | – | .903 |
| Knows somebody who experienced MMR side effects | −.524 | – | .006 |
| MMR information from public health institutions | .542 | – | .019 |
| MMR information from doctor | .175 | – | .073 |
| MMR information from Internet | .184 | – | .130 |
| MI: Measles severity | .105 | .121 | .002 |
| MI: Measles susceptibility | .101 | .143 | <.001 |
| Direct effect on MMR vaccine side effects severity | |||
| Social attitudes | −.137 | −.104 | .028 |
| Social norms | −.082 | −.067 | .133 |
| Child previously infected with measles | −.268 | – | .398 |
| Parent or other family member previously infected with measles | .056 | – | .722 |
| Knows somebody who experienced MMR side effects | 1.137 | – | .001 |
| MMR information from public health institutions | .011 | – | .980 |
| MMR information from doctor | .115 | – | .521 |
| MMR information from Internet | −.212 | – | .341 |
| MI: Measles severity | .134 | .098 | .017 |
| Direct effect on MMR vaccine side effects susceptibility | |||
| Social attitudes | −.137 | −.106 | .019 |
| Social norms | −.041 | −.034 | .437 |
| Child previously infected with measles | −.452 | – | .144 |
| Parent or other family member previously infected with measles | .032 | – | .833 |
| Knows somebody who experienced MMR side effects | 1.024 | – | .003 |
| MMR information from public health institutions | .677 | – | .099 |
| MMR information from doctor | .193 | – | .267 |
| MMR information from Internet | −.542 | – | .012 |
| MI: Measles susceptibility | .170 | .155 | <.001 |
| Indirect effect on intention | |||
| Social attitudes | .127 | .105 | .001 |
| Social norms | .056 | .050 | .001 |
| Child previously infected with measles | −.098 | −.015 | .344 |
| Parent or other family member previously infected with measles | −.010 | −.003 | .762 |
| Knows somebody who experienced MMR side effects | −.244 | −.032 | .015 |
| MMR information from public health institutions | .234 | .025 | .036 |
| MMR information from doctor | .068 | .018 | .163 |
| MMR information from Internet | .080 | .017 | .133 |
| Measles severity | −.003 | −.002 | .069 |
| Measles susceptibility | −.001 | −.001 | .054 |
| Total effect on intention | |||
| Social attitudes | .508 | .418 | .001 |
| Correlations among disturbance terms of | r | p | |
| Measles severity and measles susceptibility | .251 | <.001 | |
| Self-efficacy and response efficacy | .012 | <.001 | |
| MMR vaccine side effects severity and MMR vaccine side effects susceptibility | .449 | <.001 | |
| Self-efficacy and MMR vaccine side effects severity | .043 | <.001 | |
| Self-efficacy and MMR vaccine side effects susceptibility | .023 | <.001 | |
| Response efficacy and MMR vaccine side effects severity | −.144 | <.001 | |
| Response efficacy and MMR vaccine side effects susceptibility | −.168 | <.001 | |
| Explained variance of | R2 | ||
| Intention | .283 | ||
| Measles severity | .168 | ||
| Measles susceptibility | .066 | ||
| Self-efficacy | .080 | ||
| Response efficacy | .297 | ||
| MMR vaccine side effects severity | .043 | ||
| MMR vaccine side effects susceptibility | .068 |
Note: n = 554; coefficients based on 2000 Bootstrap replications with 95% confidence interval; MI denotes non-hypothesized effects based on modification indices > 4.
Fig. 2.
Final extended PMT model applied to the context of the MMR vaccination (only significant paths are shown).
We also looked at the indirect and total effects that result from the mediations summarized in Table 3. Examination of the bias corrected significance level indicated that intention was indirectly positively associated with social attitudes (B = .13, p = .001), social norms (B = −.06, p = .001), and having sought MMR information from public health institutions (B = .23, p = .036), while it was indirectly negatively related to knowing somebody who experienced MMR side effects (B = -.24, p = .015). Eventually, the total effect, combining the direct and indirect effects, of social attitudes on intention to adhere to official MMR vaccination recommendations turned out to be significant (B = .51, p = .001).
4. Discussion
The aim of this study was to apply Protection Motivation Theory (PMT) in the context of childhood vaccination and to identify which predictors included in the theory are likely to influence parents’ intention to adhere to official recommendation regarding the MMR vaccination in Canton Ticino in Italian-speaking Switzerland. In particular, we focused on parents of adolescents, as MMR vaccination coverage among adolescents born at the advent of the MMR controversy has not yet reached the WHO goal. Survey responses from parents of 554 adolescents aged 13 to 15 revealed that the perceived efficacy of the MMR vaccination was the only significant predictor among the concepts that represent the core components of PMT, i.e., threat and coping appraisal. In general, this is in line with other studies’ findings showing that not all PMT variables are able to predict a given behavior with the same strength (Floyd et al., 2000, Ho, 1998, Milne et al., 2000). A meta-analysis of the literature on PMT found that, generally, coping appraisal concepts have stronger relationships with the adaptive behavior or related intention, compared to threat appraisal concepts (Floyd et al., 2000). Our findings confirm that parents’ perception that vaccination is efficient in protecting their children from a target disease is positively associated with parents’ intention to vaccinate their children or with children’s vaccination status (Bennett and Smith, 1992, Chen, 2015, Fall et al., 2018, Lee and Kim, 2015, Meszaros et al., 1996, Pareek and Pattison, 2000). This finding is also confirmed by different attempts to apply PMT to other health domains. Hsieh and colleagues found that response efficacy was one of the strongest predictors of individuals’ behavioral intention for personal health records among all PMT variables (Hsieh, Kuo, Wang, Chuang, & Tsai, 2016), while Cox and colleagues’ study revealed that, together with self-efficacy, response efficacy was the most important antecedent of the intention to consume functional foods or supplements among middle-aged consumers (Cox, Koster, & Russell, 2004).
Despite the fact that we did not find a direct relationship between the threat appraisal pathway and the intention to adhere to official MMR vaccination recommendations, our results reinforce the idea that threat and coping appraisals are, within the PMT model, two intimately intertwined constructs: Perceived severity of and susceptibility to measles were significantly linked to efficacy beliefs and perceived response costs. Likewise, other studies have shown that individuals tend to make their vaccination decision by comparing the perceived benefits that can derive from vaccinating against the perceived risks which can result from contracting a target disease (Chen, 2015, Heininger, 2009).
It is not surprising that, within the extended version of the PMT model, pro-social attitudes result to be positively and significantly associated not only with the perceived efficacy of the vaccination but also with the intention to follow official vaccination recommendations. Previous studies already reported on the supportive role of parents’ belief in the benefit of vaccinating to protect other members of society, especially those more at risk, in their vaccination decision-making (Betsch et al., 2017, Chapman et al., 2012, Hershey et al., 1994, Shim et al., 2012, Skea et al., 2008). While it might be too simplistic to frame the vaccination decision as a mere form of altruism or free-riding, our results suggest that parents not only worry about the health of their own child when making a vaccination decision, but also about the health of other children, and they understand the potential risk of free-riding when vaccination coverage is insufficient. In the context with a high vaccination uptake (such as the one captured by our study), individuals are more likely to avoid free-riding if they believe in the benefits and efficacy of immunization (Betsch et al., 2013, Buttenheim and Asch, 2013, Ibuka et al., 2014). Thus, the indirect relationship between pro-social attitude and vaccination intention within the PMT model, as mediated by the perceived response efficacy, becomes even more central. This highlights the importance of communicating the benefits of vaccination even among populations where vaccination uptake is relatively high but not saturated (Buttenheim & Asch, 2013).
Furthermore, the finding that perceived vaccination efficacy mediated the relationship between social norms, past experience (having a child who previously had measles and knowing someone who suffered from MMR vaccine side effects), and MMR information sources (having actively sought information about the MMR vaccination from public health institutions) on the one side, and intention to adhere to official MMR recommendations on the other side, suggests that parents’ behavioral intentions are not a direct consequence of intra- and interpersonal characteristics, but that the latter activate a process where parents critically evaluate the efficacy of the MMR vaccine. In line with Roger’s (1975) suggestion that, when confronted with a threat, individuals activate a threat appraisal first and a coping appraisal subsequently, our analyses revealed that parents’ evaluation of the efficacy of the MMR vaccine are, among others, a direct consequence of parents’ perceived severity of measles and the perceived likelihood that their children will get this highly infectious disease throughout their course of life. While other studies also found that social norms, past experiences (with vaccination and diseases), and information sources can play a role on the immunization intention (Oraby et al., 2014, Quinn et al., 2017, Tabacchi et al., 2017, Wells and Bauch, 2012), our study emphasizes the central role of the perceived efficacy of the vaccination to prevent a target disease as a (partial) mediator between intrapersonal, experience-related, and information source-related factors and the intentional outcome of the PMT model. MMR information acquired through the Internet did not have any effects on the intention to vaccinate. This could be due to the fact that only 15 percent of our sample reported to have searched for information from the Internet, or it could be explained by a social desirability bias that would lead our participants to not report having obtained information from the Internet.
Furthermore, it is noteworthy that negative past experiences with measles did not increase parents’ threat appraisal, nor were related to parents’ perceived self-efficacy when it comes to making a decision about the MMR vaccination of their children. Interestingly, having a child that previously had measles was significantly negatively related to perceived response efficacy. This finding underscores that, among all coping appraisal concepts of PMT, response efficacy is the most stable over the years as parents of children who previously suffered from measles most likely did not believe in the response (vaccination) efficacy in the past and, hence, did not get their children vaccinated against the disease, which increases the likelihood of measles contagion. It can be speculated that those children who previously contracted measles despite being vaccinated against the disease, represent the 3 percent of cases in which two doses of the MMR vaccine are not efficient in protecting from contracting measles (Centers for Disease Control and Prevention, 2018). Consequently, these parents do not believe that the MMR vaccination is efficient, and they have no further intentions to follow the official MMR vaccination schedule. Emphasizing the high effectiveness of the MMR vaccination (97% of the population is protected with two doses, 93% with only one; Centers for Disease Control and Prevention, 2018) could be a successful strategy to promote vaccination especially in those communities where individuals that have been infected by measles despite having been vaccinated.
Finally, research has shown that the sources individuals employ to collect information on vaccination play a crucial role on their vaccination decision-making, attitudes and behavior, with positive outcomes when the sources are medical professionals or other trusted sources (Fadda et al., 2015a, Fadda et al., 2015b, Jones et al., 2012, Kennedy et al., 2011). Notably, a recent meta-analysis highlighted the importance of the type of information and information source for individuals’ immunization outcome, showing that when the information source or the advice from general or other health practitioners are lacking or inadequate, this leads to a significantly lower vaccination acceptance (Tabacchi et al., 2016). Our findings support past evidence as they highlight the importance of public health institutions in emphasizing the efficacy of the MMR vaccination as well as the role of doctors and other healthcare providers in elucidating the seriousness of measles for children’s health, that eventually contribute to parents’ intention to follow MMR vaccination recommendations. This is of utmost relevance considering the press coverage and other sources of information about measles and the MMR vaccination, which parents not only actively seek out but to which they are also passively exposed in an omnipresent media environment and which include conflicting standpoints on the seriousness of measles and side effects of the MMR vaccination (Begg et al., 1998, Lewis and Speers, 2003). That said, our participants’ reports stress the importance of the accuracy of information from health practitioners and institutions (which should correctly describe the benefit of the vaccination in terms of its efficacy) to be successful in promoting vaccination acceptance within the ecosystem of PMT. Parents seem to be aware of the implications of recent studies’ findings that some healthcare professionals advise against immunization (Paterson et al., 2016). Our results underline the importance of assessing the accuracy of the information regardless of the source it comes from.
4.1. Implications of the finding
The results of this study have a number of implications at both theoretical and practical levels. In terms of theory, as previously discussed, our results indicate that the extended version of the PMT (including intrapersonal characteristics, past experience, and information sources) has a higher predictive and explanatory power than the PMT with its core components of threat and coping appraisal. Although the present study did not compare the two models systematically, the strong direct and indirect effect of pro-social attitudes is only one reason to believe that we need to consider factors beyond risk perception and efficacy beliefs in order to understand parents’ intentions to follow MMR vaccination recommendations. This should not be surprising since the vaccination decision is, to parents, an important and complex decision, where multiple factors are taken into account to make the best choice for their children (Forster et al., 2016).
At a practical level, concerning health communication and public health interventions, our findings help formulating message contents and selecting adequate message channels. Regarding the message, the strong and significant relationships between pro-social attitudes, response (vaccination) efficacy and intention to adhere to official MMR vaccination recommendations should be taken into account when designing communication strategies and campaigns in the area under study. The content of vaccination promotion messages should present evidence on the high effectiveness of the MMR vaccination in reducing the risk of getting infected with the disease both at the individual and, even more importantly, at the community levels, rather than the health risks that follow from the target disease(s) (see also Hobson-West, 2003). As for the message channels, future efforts should highlight the benefits of searching vaccination-related information through health institutions, who should promptly answer parents’ questions and elucidate their doubts (May, 2005).
4.2. Study limitations
Our findings should be interpreted in the light of several study limitations. First of all, participation in the study was voluntary and parents were recruited in collaboration with the Cantonal Office of Public Health. It is likely that parents who agreed to participate in the study are mainly those who have high regards for local public health institutions, their recommendations and activities in the context of childhood vaccinations. In a future study on this topic, a more neutral form of recruitment should be applied to minimize potential selection bias. By implementing three modes of data collection (online questionnaire, postal questionnaire, and telephone interview), we aimed to increase participation rate and reduce systematic bias. However, the use of different assessment modes has also its limitations as participants may differ in their responses due to different perceptions of anonymity and a social desirability bias introduced by the presence of an interviewer. We conducted one-way ANOVAs with Tukey’s post-hoc test to evaluate if the different survey modes had an impact on participants’ self-reports. This was not the case, except for response efficacy, where online responses (M = 5.99, SD = 1.11) significantly differed from postal responses (M = 5.64, SD = 1.17), and for information search on the Internet, where online responses (M = .20, SD = .40) were significantly different from phone responses (M = .00, SD = .00). The latter difference can be explained by the fact that parents who opted for the phone survey probably rarely or never use the Internet in general and as an information source. In fact, these parents have not sought online MMR information at all. The difference in participants’ evaluation of MMR vaccination response efficacy was somewhat surprising since both online and postal survey provided the same level of anonymity so that a discriminating systematic bias (e.g., social desirability bias) can be excluded. Another limitation is linked to the measurement of concepts. We used single items to assess many components of the PMT model. Operationalizing the key concepts in a different way and with more items would increase the predictive validity of our study results. However, multi-item indicators in this study context face the challenge of good reliability. For example, Cronbach’s alpha for our multi-item indicator of response efficacy was below the standard threshold and similar alpha levels have been found in other studies with measures on attitudes and beliefs in the context of measles and the MMR vaccination (Brown et al., 2011). Furthermore, the decisive dependent variable, agreeing to the statement that one follows official MMR vaccination recommendations, is not necessarily understood as a proclamation of what one intends to do; it can as well be understood as a reporting about past behavior. In fact, parents whose children received full MMR vaccination coverage were significantly more likely to adhere to official MMR vaccination guidelines than parents whose children received no or only one dose of the vaccine. However, it is most important to understand what supports and – on the other hand – prevents parents from getting their now adolescent child vaccinated against measles, especially with regards to parents whose children did not receive full MMR coverage by the age of 13 to 15.
Furthermore, research on the MMR vaccination should move a step forward and include studies looking at similarities and differences in the factors that predict parents’ intention to follow MMR vaccination recommendations by comparing parents of very young children, being the primary target group of MMR vaccination campaigns and interventions, with parents of adolescent children. If differences in the predictive factors exists, these should be addressed in targeted campaigns and interventions to improve MMR vaccination status in all age groups.
A final limitation regards the generalizability of our finding. As mentioned earlier, our sample composition largely reflects that of the general Ticino population in the relevant age group and we can therefore safely assume that they provide a good snapshot of the dynamics of the population. However, it must be acknowledged that some of the peculiarities of Ticino might limit the generalizability of our results to other socio-cultural contexts. For instance, it might be hypothesized that social attitudes would play a more marginal role in more individualistic contexts (Schulz, Nakamoto, Brinberg, & Haes, 2006). Further research is therefore needed to investigate the role of the different concepts of the PMT in predicting the intention to follow official MMR vaccination recommendations and, eventually, the decision for vaccination in different socio-cultural contexts.
5. Conclusions
The present study gave useful insights on the factors that underlie parents’ intention to adhere to official MMR vaccination recommendation in a Swiss Canton with a high measles incidence, using Protection Motivation Theory. Our results underline the importance of vaccination efficacy and social attitudes, i.e., the belief that the MMR vaccine helps protecting one’s child and that vaccinating one’s child also protects other children, as positive predictors of the intention to adhere to official MMR vaccination recommendations in the Italian-speaking part of Switzerland. Hence, future efforts in view of the goal of measles elimination in the Swiss population by the end of 2020 should include campaigns and other public health strategies targeted at parents, highlighting the altruistic aspect of vaccinating and the high effectiveness of the immunization practice. This is particularly difficult, yet crucial in persuading parents with negative measles experiences to decide for the MMR vaccination when it comes to protect younger siblings and/or advocating for the MMR vaccination when advising parents of toddlers or parents-to-be. Furthermore, official information through public health institutions should be promoted. In light of current suboptimal measles vaccine coverage, future studies could evaluate past measles vaccine campaigns conducted in Switzerland, by means of verifying the presence of the PMT concepts and their practical application in the intervention.
Conflict of interest
None declared.
Funding
The study was funded by the Swiss National Science Foundation (Grant no. 147333). The Public Health Office of the Canton Ticino collaborated in the recruitment of the participants and collected MMR vaccination coverage data.
Contributor Information
Anne-Linda Camerini, Email: anne.linda.camerini@usi.ch.
Nicola Diviani, Email: nicola.diviani@unilu.ch.
Marta Fadda, Email: marta.fadda@hest.ethz.ch.
Peter J. Schulz, Email: peter.schulz@usi.ch.
References
- Begg N., Ramsay M., White J., Bozoky Z. Media dents confidence in MMR vaccine. BMJ. 1998;316(7130):561. [Google Scholar]
- Bennett P., Smith C. Parents attitudinal and social influences on childhood vaccination. Health Education Research. 1992;7(3):341–348. doi: 10.1093/her/7.3.341. [DOI] [PubMed] [Google Scholar]
- Betsch C., Böhm R., Chapman G.B. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights from the Behavioral and Brain Sciences. 2015;2(1):61–73. [Google Scholar]
- Betsch C., Böhm R., Korn L. Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychology. 2013;32(9):978–985. doi: 10.1037/a0031590. [DOI] [PubMed] [Google Scholar]
- Betsch C., Böhm R., Korn L., Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nature Human Behaviour. 2017;1:0056. [Google Scholar]
- Betsch C., Sachse K. Dr. Jekyll or Mr. Hyde? (How) the Internet influences vaccination decisions: Recent evidence and tentative guidelines for online vaccine communication. Vaccine. 2012;30(25):3723–3726. doi: 10.1016/j.vaccine.2012.03.078. [DOI] [PubMed] [Google Scholar]
- Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Britt R.K., Hatten K.N., Chappuis S.O. Perceived behavioral control, intention to get vaccinated, and usage of online information about the human papillomavirus vaccine. Health Psychology and Behavioral Medicine. 2014;2(1):52–65. doi: 10.1080/21642850.2013.869175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K.F., Shanley R., Cowley N.A.L., van Wijgerden J., Toff P., Falconer M., Sevdalis N. Attitudinal and demographic predictors of measles, mumps and rubella (MMR) vaccine acceptance: Development and validation of an evidence-based measurement instrument. Vaccine. 2011;29(8):1700–1709. doi: 10.1016/j.vaccine.2010.12.030. [DOI] [PubMed] [Google Scholar]
- Buttenheim A.M., Asch D.A. Making vaccine refusal less of a free ride. Human Vaccines Immunotherapeutics. 2013;9(12):2674–2675. doi: 10.4161/hv.26676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casiday R.E. Children’s health and the social theory of risk: Insights from the British measles, mumps and rubella (MMR) controversy. Social Science Medicine. 2007;65(5):1059–1070. doi: 10.1016/j.socscimed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2018). MMR Vaccination | What You Should Know | Measles, Mumps, Rubella | CDC. Retrieved June 18, 2018, from 〈https://www.cdc.gov/vaccines/vpd/mmr/public/index.html〉.
- Chapman G.B., Li M., Vietri J., Ibuka Y., Thomas D., Yoon H., Galvani A.P. Using Game Theory to examine incentives in influenza vaccination behavior. Psychological Science. 2012;23(9):1008–1015. doi: 10.1177/0956797612437606. [DOI] [PubMed] [Google Scholar]
- Chen N.T.N. Predicting vaccination intention and benefit and risk perceptions: The incorporation of affect, trust, and television influence in a dual-mode model. Risk Analysis. 2015;35(7):1268–1280. doi: 10.1111/risa.12348. [DOI] [PubMed] [Google Scholar]
- Cox D.N., Koster A., Russell C.G. Predicting intentions to consume functional foods and supplements to offset memory loss using an adaptation of protection motivation theory. Appetite. 2004;43(1):55–64. doi: 10.1016/j.appet.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Fadda M., Allam A., Schulz P.J. Arguments and sources on Italian online forums on childhood vaccinations: Results of a content analysis. Vaccine. 2015;33(51):7152–7159. doi: 10.1016/j.vaccine.2015.11.007. [DOI] [PubMed] [Google Scholar]
- Fadda M., Depping M.K., Schulz P.J. Adressing issues of vaccination literacy and psychological empowerment in the measles-mumpls-rubella (MMR) vaccination decision-making: A qualitative study. BMC Public Health. 2015;15(1):836. doi: 10.1186/s12889-015-2200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadda M., Galimberti E., Carraro V., Schulz P.J. What are parents' perspectives on psychological empowerment in the MMR vaccination decision? A focus group study. BMJ Open. 2016;6(4):e010773. doi: 10.1136/bmjopen-2015-010773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fall E., Izaute M., Chakroun-Baggioni N. How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention? A longitudinal study among university students. Psychology Health. 2018;33(6):746–764. doi: 10.1080/08870446.2017.1401623. [DOI] [PubMed] [Google Scholar]
- Federal Statistical Office (2018). Results. Retrieved October 15, 2018, from 〈https://www.bfs.admin.ch/bfs/en/home/statistiken/bevoelkerung/erhebungen/se/ergebnisse.html〉.
- Filia A., Bella A., Manso M.D., Baggieri M., Magurano F., Rota M.C. Ongoing outbreak with well over 4,000 measles cases in Italy from January to end August 2017 − what is making elimination so difficult? Eurosurveillance. 2017;22(37):30614. doi: 10.2807/1560-7917.ES.2017.22.37.30614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd D.L., Prentice-Dunn S., Rogers R.W. A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology. 2000;30(2):407–429. [Google Scholar]
- Flynn M., Ogden J. Predicting uptake of MMR vaccination: A prospective questionnaire study. British Journal of General Practice. 2004;54(504):526–530. [PMC free article] [PubMed] [Google Scholar]
- Forster A.S., Rockliffe L., Chorley A.J., Marlow L.A.V., Bedford H., Smith S.G., Waller J. A qualitative systematic review of factors influencing parents' vaccination decision-making in the United Kingdom. SSM - Population Health. 2016;2:603–612. doi: 10.1016/j.ssmph.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman V.A., Freed G.L. Parental knowledge, attitudes, and demand regarding a vaccine to prevent varicella. American Journal of Preventive Medicine. 1999;17(2):153–155. doi: 10.1016/s0749-3797(99)00063-x. [DOI] [PubMed] [Google Scholar]
- Gellatly J., McVittie C., Tiliopoulos N. Predicting parents' decisions on MMR immunisation: A mixed method investigation. Family Practice. 2005;22(6):658–662. doi: 10.1093/fampra/cmi066. [DOI] [PubMed] [Google Scholar]
- Gust D.A., Darling N., Kennedy A., Schwartz B. Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics. 2008;122(4):718–725. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- Heininger U. A risk-benefit analysis of vaccination. Vaccine. 2009;27(Suppl 6) doi: 10.1016/j.vaccine.2009.10.010. (G9–G12) [DOI] [PubMed] [Google Scholar]
- Hershey J.C., Asch D.A., Thumasathit T., Meszaros J., Waters V.V. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organizational Behavior and Human Decision Processes. 1994;59(2):177–187. [Google Scholar]
- Ho R. The intention to give up smoking: Disease versus social dimensions. The Journal of Social Psychology. 1998;138(3):368–380. doi: 10.1080/00224549809600389. [DOI] [PubMed] [Google Scholar]
- Hobson-West P. Understanding vaccination resistance: Moving beyond risk. Health, Risk Society. 2003;5(3):273–283. [Google Scholar]
- Hsieh H.-L., Kuo Y.-M., Wang S.-R., Chuang B.-K., Tsai C.-H. A study of personal health record user’s behavioral model based on the PMT and UTAUT integrative perspective. International Journal of Environmental Research and Public Health. 2016;14(1):8. doi: 10.3390/ijerph14010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibuka Y., Li M., Chapman G.B., Galvani A.P. Free-riding behavior in vaccination decisions: An experimental study. PLOS ONE. 2014;9(3):e94066. doi: 10.1371/journal.pone.0087164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.M., Omer S.B., Bednarczyk R.A., Halsey N.A., Moulton L.H., Salmon D.A. Parents' source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Advances in Preventive Medicine. 2012;2012:e932741. doi: 10.1155/2012/932741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A., Basket M., Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: Results from the 2009 HealthStyles Survey. Pediatrics, 2011 doi: 10.1542/peds.2010-1722N. (peds.2010-1722N) [DOI] [PubMed] [Google Scholar]
- Kimura H., Nishiyama Y. Measles outbreak in adolescents. Japan Medical Association Journal. 2007;50(5):3. [Google Scholar]
- Kline R.B. Principles and Practice of Structural Equation Modeling. Fourth Edition. Guilford Publications; 2015. [Google Scholar]
- Lang, P. (2007). Vaccination Status of Children in Switzerland. University of Basel. Retrieved June 18, 2018 from 〈http://edoc.unibas.ch/699/1/DissB_8139.pdf〉.
- Lee H.O., Kim S. Linking health information seeking to behavioral outcomes: Antecedents and outcomes of childhood vaccination information seeking in South Korea. Journal of Health Communication. 2015;20(3):285–296. doi: 10.1080/10810730.2014.927035. [DOI] [PubMed] [Google Scholar]
- Lewis J., Speers T. Misleading media reporting? The MMR story. Nature Reviews Immunology. 2003;3(11):913–918. doi: 10.1038/nri1228. [DOI] [PubMed] [Google Scholar]
- Lippke S., Ziegelmann J.P. Theory-based health behavior change: Developing, testing, and applying theories for evidence-based interventions. Applied Psychology. 2008;57(4):698–716. [Google Scholar]
- Liu R., Li Y., Wangen K.R., Maitland E., Nicholas S., Wang J. Analysis of hepatitis B vaccination behavior and vaccination willingness among migrant workers from rural China based on protection motivation theory. Human Vaccines Immunotherapeutics. 2016;12(5):1155–1163. doi: 10.1080/21645515.2015.1123358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux J.E., Rogers R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology. 1983;19(5):469–479. [Google Scholar]
- May T. Public communication, risk perception, and the viability of preventive vaccination against communicable diseases. Bioethics. 2005;19(4):407–421. doi: 10.1111/j.1467-8519.2005.00452.x. [DOI] [PubMed] [Google Scholar]
- Meszaros J.R., Asch D.A., Baron J., Hershey J.C., Kunreuther H., Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. Journal of Clinical Epidemiology. 1996;49(6):697–703. doi: 10.1016/0895-4356(96)00007-8. [DOI] [PubMed] [Google Scholar]
- Milne S., Sheeran P., Orbell S. Prediction and intervention in health-related behavior: A meta-analytic review of Protection Motivation Theory. Journal of Applied Social Psychology. 2000;30(1):106–143. [Google Scholar]
- Oraby T., Thampi V., Bauch C.T. The influence of social norms on the dynamics of vaccinating behaviour for paediatric infectious diseases. Proceedings of the Royal Society B: Biological Sciences. 2014;281(1780):20133172. doi: 10.1098/rspb.2013.3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pareek M., Pattison H.M. The two-dose measles, mumps, and rubella (MMR) immunisation schedule: Factors affecting maternal intention to vaccinate. British Journal of General Practice. 2000;50(461):969–971. [PMC free article] [PubMed] [Google Scholar]
- Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- Quinn S.C., Hilyard K.M., Jamison A.M., An J., Hancock G.R., Musa D., Freimuth V.S. The influence of social norms on flu vaccination among African American and White adults. Health Education Research. 2017;32(6):473–486. doi: 10.1093/her/cyx070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao T.S.S., Andrade C. The MMR vaccine and autism: Sensation, refutation, retraction, and fraud. Indian Journal of Psychiatry. 2011;53(2):95–96. doi: 10.4103/0019-5545.82529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathi P., Narendra V., Sathiya V., Kini S., Kumar A., Sana N., Kamath V.G. Measles outbreak in the adolescent population - Matter of concern? Journal of Clinical and Diagnostic Research: JCDR. 2017;11(8):LC20–LC23. doi: 10.7860/JCDR/2017/28619.10488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R.W. A Protection Motivation Theory of fear appeals and attitude change. The Journal of Psychology. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Rogers R.W. Cognitive and physiological processes in fear appeals and attitude change: A revised Theory of Protection Motivation. In: Cacioppo B.L., Petty L.L., editors. Social Psychophysiology: A Sourcebook. Guilford; London, UK: 1983. pp. 153–176. [Google Scholar]
- Sansonetti P.J. Measles 2018: A tale of two anniversaries. EMBO Molecular Medicine. 2018;10(5):e9176. doi: 10.15252/emmm.201809176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz P.J., Nakamoto K., Brinberg D., Haes J. More than nation and knowledge: Cultural micro-diversity and organ donation in Switzerland. Patient Education and Counseling. 2006;64(1–3):294–302. doi: 10.1016/j.pec.2006.03.009. [DOI] [PubMed] [Google Scholar]
- Shim E., Chapman G.B., Townsend J.P., Galvani A.P. The influence of altruism on influenza vaccination decisions. Journal of The Royal Society Interface. 2012;9(74):2234–2243. doi: 10.1098/rsif.2012.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skea Z.C., Entwistle V.A., Watt I., Russell E. ‘Avoiding harm to others' considerations in relation to parental measles, mumps and rubella (MMR) vaccination discussions – An analysis of an online chat forum. Social Science Medicine. 2008;67(9):1382–1390. doi: 10.1016/j.socscimed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Smith M.J., Ellenberg S.S., Bell L.M., Rubin D.M. Media coverage of the measles-mumps-rubella vaccine and autism controversy and its relationship to MMR immunization rates in the United States. Pediatrics. 2008;121(4):e836–e843. doi: 10.1542/peds.2007-1760. [DOI] [PubMed] [Google Scholar]
- Smith P.J., Humiston S.G., Marcuse E.K., Zhao Z., Dorell C.G., Howes C., Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Reports. 2011;126(2_suppl):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spreitzer G.M. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Academy of Management Journal. 1995;38(5):1442–1465. [Google Scholar]
- Swiss Federal Office of Public Health. (2017a). Masern - Lagebericht Schweiz. Retrieved May 19, 2017, from 〈https://www.bag.admin.ch/bag/de/home/themen/mensch-gesundheit/uebertragbare-krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/masern-lagebericht-schweiz.html〉.
- Swiss Federal Office of Public Health. (2017b). Masern, Mumps, Röteln. Retrieved June 13, 2018, from 〈https://www.bag.admin.ch/bag/de/home/service/publikationen/broschueren/publikationen-uebertragbare-krankheiten/masern-mumps-roeteln.html〉.
- Swiss Federal Office of Public Health. (2018a). Masern - Lagebericht Schweiz. Retrieved June 13, 2018, from 〈https://www.bag.admin.ch/bag/de/home/themen/mensch-gesundheit/uebertragbare-krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/masern-lagebericht-schweiz.html〉.
- Swiss Federal Office of Public Health. (2018b). Measles. Retrieved September 28, 2018, from 〈https://www.bag.admin.ch/bag/en/home/krankheiten/krankheiten-im-ueberblick/masern.html〉.
- Tabacchi G., Costantino C., Cracchiolo M., Ferro A., Marchese V., Napoli G., Casuccio A. Information sources and knowledge on vaccination in a population from southern Italy: The ESCULAPIO project. Human Vaccines Immunotherapeutics. 2017;13(2) doi: 10.1080/21645515.2017.1264733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabacchi G., Costantino C., Napoli G., Marchese V., Cracchiolo M., Casuccio A., Vitale F. Determinants of European parents' decision on the vaccination of their children against measles, mumps and rubella: A systematic review and meta-analysis. Human Vaccines Immunotherapeutics. 2016;12(7) doi: 10.1080/21645515.2016.1151990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe E.L., Zimmerman R.K., Steinhart J.D., Lewis K.N., Michaels M.G. Homeschooling parents' practices and beliefs about childhood immunizations. Vaccine. 2012;30(6):1149–1153. doi: 10.1016/j.vaccine.2011.12.019. [DOI] [PubMed] [Google Scholar]
- Wells C.R., Bauch C.T. The impact of personal experiences with infection and vaccination on behaviour–incidence dynamics of seasonal influenza. Epidemics. 2012;4(3):139–151. doi: 10.1016/j.epidem.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Wheeler M., Buttenheim A.M. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Human Vaccines Immunotherapeutics. 2013;9(8):1782–1789. doi: 10.4161/hv.25959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Measles vaccines: WHO position paper. Weekly Epidemiological Record. 2009;84(35):349–360. [Google Scholar]
- World Health Organization (2016). WHO | Measles. Retrieved May 19, 2017, from 〈http://www.who.int/immunization/diseases/measles/en/〉.
- World Health Organization (2018). WHO | Data, statistics and graphics. Retrieved June 13, 2018, from 〈http://www.who.int/immunization/monitoring_surveillance/data/en/〉.