Abstract
Between 5% and 10% of people with psychosis will die by suicide, a rate which is 20–75 times higher than the general population. This risk is even greater in those not taking antipsychotic medication. We examined whether negative appraisals of psychotic experiences and negative metacognitive beliefs about losing mental control mediated a relationship between psychotic symptoms and suicidal ideation in this group. Participants were diagnosed with schizophrenia spectrum disorders, antipsychotic-free for 6 months at baseline, and were participating in an 18-month randomized controlled trial of cognitive therapy vs treatment as usual. We conducted a series of mediation analyses with bootstrapping on baseline (N = 68), follow-up data (9–18 mo; n = 49), and longitudinal data (n = 47). Concurrent general symptoms were directly associated with suicidal ideation at baseline, and concurrent negative symptoms were directly associated with suicidal ideation at 9–18 months. Concurrent positive, negative, general, and overall symptoms were each indirectly associated with suicidal ideation via negative appraisals and/or negative metacognitive beliefs, at baseline and 9–18 months, except for negative symptoms at baseline. Controlling for baseline suicidal ideation and treatment allocation, baseline general symptoms were indirectly associated with later suicidal ideation, via baseline negative appraisals and negative metacognitive beliefs. Baseline negative metacognitive beliefs also had a direct association with later suicidal ideation. These findings suggest the clinical assessment of suicidal ideation in psychosis may be enhanced by considering metacognitive beliefs about the probability and consequences of losing mental control.
Keywords: psychosis, schizophrenia, suicide, antipsychotic medication, appraisals, metacognitive beliefs
Introduction
Estimates of suicide rates among individuals diagnosed with schizophrenia spectrum disorders range from 5% to 10%, making it a leading cause of premature death in this population.1–3 Nonuse of antipsychotics is thought to increase this risk further, with one large observational study reporting a 37 times greater risk of suicide in inpatients who were not taking antipsychotics.4 Given antipsychotics have their strongest effects on the positive symptoms of psychosis,5 it is plausible that individuals not taking this medication may have greater positive symptom severity than those who do—and that this accounts for their increased suicide risk.
However, the evidence on the contribution of positive symptoms to suicide risk remains unclear. One meta-analysis suggested they were associated with a lower risk;3 one found no association6 whereas another found they were associated with a higher risk.7 Although this inconsistency may reflect methodological differences, the absence of a robust relationship may indicate the presence of underlying mechanisms that have yet to be fully accounted for. As predicted by cognitive theories,8,9 several studies have found that the way a person interprets or “appraises” their psychotic experiences may be more important than symptom severity for predicting suicidal behavior.10,11 Importantly, one review found that people with psychosis who die by suicide were more likely to have “fears of mental disintegration” than matched controls.3
This latter finding suggests “metacognition”12,13 may be important for understanding their suicidality. Whereas cognition refers to knowledge and appraisals of the external world, metacognition refers to knowledge and beliefs relating to the structure and integrity of the self, and ones own cognitive processes. Although the distinction between metacognition and cognition has been debated,13 Moritz and Lysaker13 review how it has been usefully applied in psychosis to understanding the psychological mechanisms implicated in (a) awareness of cognitive biases,14 such as the “jumping to conclusions” bias15,16; (b) concepts of self and others, including perceived self-integration17; and (c) negative metacognitive beliefs about the uncontrollability and danger of worry and rumination.18 In relation to the latter, high levels of negative metacognitive beliefs are associated with psychotic symptom severity and chronicity,19–22 and changing these beliefs may lead to improvements in psychotic symptoms.23–26 Although worry and rumination are associated with suicidality in various populations27–29 and although a cross-sectional study (N = 1920) found that rumination was associated with increased suicidality in people with schizophrenia,30 negative metacognitive beliefs have not featured prominently in theoretical accounts of their increased suicide risk.31
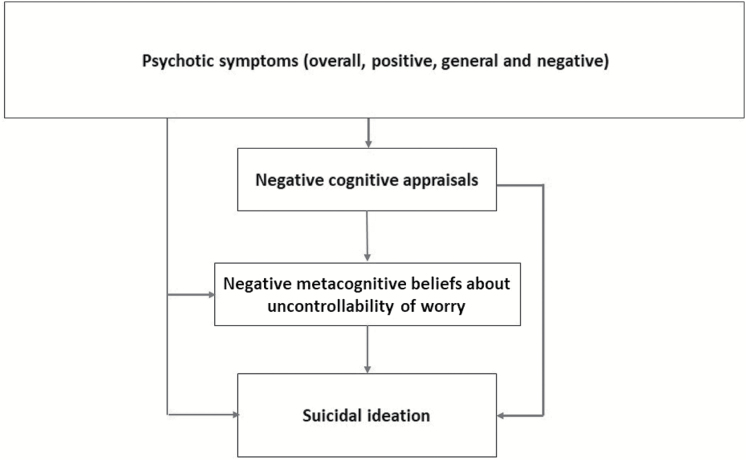
In this study, we set out to test a metacognitive model of suicidal ideation in this group (see figure 1).32 We focused on recent suicidal ideation (past 2 wk) because of its strong relationship to dying from suicide in psychosis (OR = 30, 95% CI = 12, 73)3 and we focused on those who have been antipsychotic-free for an extended period of time, because they are considered to be at particularly high risk of suicide.4 The model we tested is a version of a model of psychosis-related distress we developed for a recent case series of metacognitive therapy (MCT),23 but adapted to explain suicidality. According to this, a person may have suicidal thoughts because of an increase in the severity and negative content of their psychotic symptoms, which may in turn activate cognitive appraisals involving defeat and hopelessness (eg, “I am powerless to influence or control my experiences”).11 However, the effect of symptoms and symptom appraisals on suicidal ideation will be magnified by negative “metacognitive” beliefs about the uncontrollability and danger of worry (eg, “My worrying thoughts persist, no matter how I try to stop them,” “My worrying could make me go mad”). The emergence of suicidal ideation can be conceptualized as not only a response to symptoms and related perceptions of defeat and entrapment, but also as attempts at cognitive control, motivated by worry about the uncontrollability and danger of worry itself.
Fig. 1.
Metacognitive model of suicidal ideation in psychosis.
To test the model, we examined whether negative cognitive appraisals and negative metacognitive beliefs mediate the relationship between psychotic symptoms (overall, positive, negative, or general) and suicidal ideation at baseline (mo 0) and at follow-up (mo 9–18). We then examined whether their initial cognitive appraisals and metacognitive beliefs mediated the relationship between initial symptom severity and future suicidal ideation.
Methods
Study Design, Participants, and Procedures
This study is a secondary analysis of baseline and 9–18 month data obtained from the ACTION randomized controlled trial (RCT), a pilot trial designed to assess the effects of cognitive therapy in individuals with a schizophrenia spectrum diagnosis not receiving antipsychotic medication for at least 6 months.32 The trial was approved by the UK NHS National Research Ethics Service (09/H1014/53) and conducted in 2 sites (Manchester and Newcastle) between 2010 and 2013 (see protocol33 for further information).
Measures
Symptoms: Positive and Negative Syndrome Scale.
The Positive and Negative Syndrome Scale (PANSS)34 is a 30-item interview-based measure developed to assess the following symptom subscales associated with schizophrenia: General Psychopathology (16 items), Negative Symptom Scale (7 items), and Positive Symptom Scale (7 items). Symptoms in the preceding week are assessed using a 1- to 7-point Likert scale.
Cognitive Appraisals: Personal Beliefs About Experiences Questionnaire.
The Personal Beliefs about Experiences Questionnaire (PBEQ) is a revised version of the Personal Beliefs about Illness Questionnaire (PBIQ),35,36 and is designed to measure cognitive appraisals about psychotic experiences. Rating of the 13 items is on a 4-point Likert-type scale, which ranges from “strongly disagree” to “strongly agree.” Factor analysis suggests the PBEQ measures 3 specific domains of cognitions: Negative Appraisal of Experience (5 items), External Shame (2 items), and Internal Shame/Defectiveness (6 items).37 The PBEQ was also shown to have adequate internal reliability and validity. The Negative Appraisal of Experience subscale, which assesses the respondent’s negative appraisals and expectations of their own psychotic experiences, was used in this analysis. Items include “I am powerless to influence or control my experiences” and “My experiences frighten me.”
Negative Metacognitive Beliefs: The Metacognitions Questionnaire-30.
The Metacognitions Question naire-30 (MCQ-30)38 is a 30-item self-report questionnaire, which measures individual metacognitive beliefs and processes, grouped under 5 different subscales: positive beliefs about worrying, negative beliefs about uncontrollability and danger of worry, cognitive confidence, beliefs about the need to control thoughts, and cognitive self-consciousness. Items are scored on a 4-point Likert-type scale with 1 representing “I do not agree” and 4 representing “I agree very much.” The MCQ-30 has good internal consistency, validity, and reliability.38 We used the “Negative beliefs about uncontrollability and dangerousness of thoughts” subscale in the current analysis. This assesses negative metacognitive appraisals and expectations about worrying and thinking. Items include “My worrying could make me go mad” and “My worrying is dangerous for me.”
The Beck Depression Inventory for Primary Care.
The Beck Depression Inventory for Primary Care (BDI-PC)39 is a self-report questionnaire that measures depression severity. In this analysis, responses to item 7 (item 9 in the full BDI-2) were used to measure suicidal ideation. This item requires participants to select which of 4 statements best describe their experiences over the preceding 2 weeks. The statements are “I don’t have any thoughts of killing myself” (score of 0), “I have thoughts of killing myself, but I would not carry them out” (score of 1), “I would like to kill myself” (score of 2), and “I would kill myself if I had the chance” (score of 3). Responses correlate highly with the Beck Scale of Suicidal Ideation (r = .56–.58),40 and individuals scoring ≥2 on this item were 6.9 times more likely to commit suicide than those scoring <2.41
Statistical Analyses.
Mediation analyses were conducted to concurrently test the direct effect of psychotic symptoms (overall, positive, negative, or general) on suicidal ideation, and their hypothesized indirect effects through cognitive appraisals and metacognitive beliefs, at the 2 time points when we assessed each variable. To minimize the loss of power introduced by missing data at follow-up, we combined into one group those who had full datasets at either 9 months (n = 39) or 18 months (n = 10). To assess the risk of bias introducing by missing data, we tested for differences in baseline characteristics between the full baseline sample (N = 68) and those for whom we had full baseline and full follow-up data (n = 47). We also ran all baseline mediation analyses in both samples and covaried for the follow-up assessment time point (9 or 18 mo).
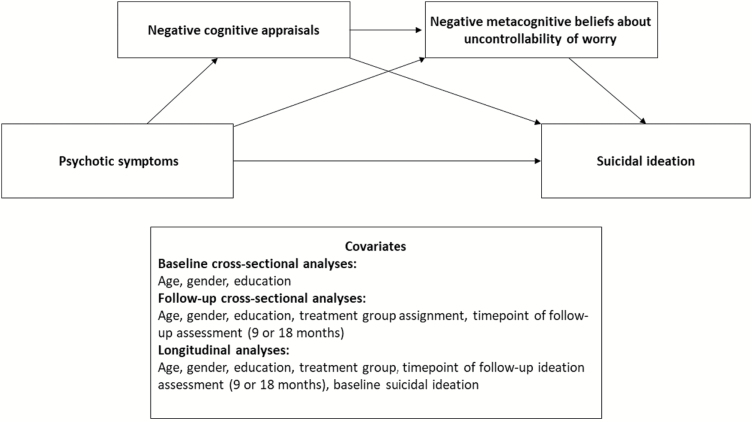
We tested a model whereby, after controlling for participant differences in age, gender, years of education, group allocation (follow-up analysis only), and the point when suicidal ideation was assessed (follow-up analysis only), psychotic symptoms activate negative cognitive appraisals, which then activate negative metacognitive beliefs, which in turn activates greater suicidal ideation (figure 1). All mediation analyses were performed using Model 6 of the PROCESS42 macro for the IBM Statistical Package for Social Sciences (SPSS) (see figure 2). This macro is based on a logistic regression-based path analytic framework and uses bootstrapping to determine the magnitude and significance of the direct (unmediated) and indirect (mediated) effects.43 Bootstrapping is a nonparametric approach that can be applied to smaller sample sizes and nonnormal data.44 All models were conducted with bias-corrected confidence intervals based on 5000 samples. In line with previous studies,45–48 suicidal ideation scores were treated as a continuous variable in all analyses.
Fig. 2.
General mediation model tested (ie, PROCESS Model 6).
We used linear regression to explore the potential prospective association between psychotic symptoms, metacognitive beliefs, and suicidal ideation over time. This analysis focuses on the residual variance in suicidal ideation once baseline levels are accounted for. For the linear regression model, suicidal ideation at 9–18 months was first regressed onto symptoms (positive, negative, and general) and covariates (same as 9–18 mo cross-sectional analysis, but with the addition of baseline suicidal ideation). We then examined whether models also incorporating (a) baseline negative cognitive appraisals and (b) baseline negative metacognitive beliefs helped to explain additional variance.
We then tested whether cognitive appraisals and negative metacognitive beliefs at baseline mediated a relationship between psychotic symptoms at baseline and suicidal ideation at 9–18 months, using the same covariates for the linear regression. For this, the baseline value of each symptom category was the independent variable, the mediating variables of interest were baseline appraisals and metacognitive beliefs, and the dependent variable was suicidal ideation at 9–18 months. We also examined the effect of symptom categories with and without other symptom categories as covariates.
For all mediation analyses, the unstandardized direct effect (UDE) or indirect effect (UIE), and the completely standardized indirect effects (CSE) were calculated as measures of effect size. The UDE and UIE represent the unit change in the dependent variable per unit change in the independent, whether direct (unmediated; UDE) or indirect (mediated; UIE). The CSE represents the proportion of standard deviation change in the dependent variable per 1 SD unit change in the independent variable, occuring through change in the mediator. Cohen’s guidelines for interpreting standardized mean differences can therefore be applied to the CSE to provide an approximate appraisal of the magnitude of the dependent variable change (0.2 = small, 0.5 = moderate, 0.8 = large),49 per a large (1 SD) change in the independent variable. Cohen’s criteria were also used to interpret correlations (0.1 = small, 0.3 = moderate, 0.5 = large).
Results
Participant Characteristics
The mean age of the full sample (N = 68) was 31 (SD = 12.75). Just under half (n = 31, 46%) were female (table 1). Overall, 60% (n = 41) of these participants reported suicidal ideation at trial entry; 50% (n = 34) reported having mild suicidal ideation whereas 10% (n = 7) reported severe to very severe ideation involving intent. There were no significant differences in demographics, symptom severity, suicidal ideation, negative cognitive appraisals, or negative metacognitive beliefs between the full sample, and those who provided full data at baseline and 9–18 months (all Ps > .1).
Table 1.
Participant Characteristics
| All | 9–18 mo completers | ||
|---|---|---|---|
| Variable | 0 mo (N = 68) | 0 mo (n = 47–49) | 9–18 mo (n = 49) |
| Age, mean (SD), y | 31.28 (12.75) | 29.92 (11.18) | |
| Gender (female), n (%) | 31 (46) | 23 (47) | |
| Years of education, mean (SD) | 12.59 (3.03) | 12.31 (2.86) | |
| MCQ-30: “Negative Beliefs About Uncontrollability and Danger” subscale, mean (SD) | 17.28 (4.82) | 16.98 (4.55)a | 15.87 (4.70) |
| PBEQ: “Negative Appraisals of Experiences” subscale, mean (SD) | 14.09 (3.16) | 14.22 (3.16)b | 12.92 (3.78) |
| PANSS: positive symptoms, mean (SD) | 20.99 (4.89) | 20.29 (4.30) | 16.63 (6.21) |
| PANSS: negative symptoms, mean (SD) | 14.75 (4.52) | 14.73 (4.90) | 13.90 (4.48) |
| PANSS: general symptoms, mean (SD) | 36.69 (7.54) | 36.02 (7.36) | 31.98 (9.34) |
| PANSS: total symptoms, mean (SD) | 72.43 (13.77) | 71.04 (13.41) | 62.51 (17.44) |
| BDI-7: suicidal ideation, mean (SD) | 0.74 (0.73) | 0.73 (0.81) | 0.53 (0.71) |
| BDI-7: suicidal ideation (no ideation), n (%) | 27 (40) | 22 (45) | 28 (57) |
| BDI-7: suicidal ideation (mild), n (%) | 34 (50) | 20 (41) | 17 (35) |
| BDI-7: suicidal ideation (moderate to severe), n (%) | 5 (7.4) | 5 (10) | 3 (6) |
| BDI-7: suicidal ideation (severe), n (%) | 2 (3) | 2 (4) | 1 (2) |
Note: SD, standard deviation; MCQ-30, Metacognition Questionnaire-30; PBEQ, Personal Beliefs About Experiences Questionnaire; PANSS, Positive and Negative Syndrome Scale; BDI-7, Beck Depression Inventory-7.
a N = 48.
b N = 47.
Correlations
No correlation was observed between suicidal ideation and negative symptoms at baseline, but a moderate correlation (r = .30) was evident at 9–18 months (table 2). At baseline, moderate correlations were observed between suicidal ideation and positive and overall symptoms for the sample with 9–18-month data. These associations were large at 9–18 months (r = .47–.51). Large correlations (r = .43–.57) between suicidal ideation and negative cognitive appraisals, negative metacognitive beliefs, and general symptoms were also observed at both baseline (both samples) and 9–18 months.
Table 2.
Correlations Between Variables (Pearson’s r, 2-tailed)
| Time point (mo) | N | Age | Education | MCQ negative beliefs | PBEQ negative appraisals | Positive symptoms | Negative symptoms | General symptoms | Overall symptoms | |
|---|---|---|---|---|---|---|---|---|---|---|
| Education | 0 | 68 | −.02 | |||||||
| 0 | 49 | −.17 | ||||||||
| 9–18 | 49 | −.17 | ||||||||
| MCQ negative beliefs | 0 | 68 | −.08 | .10 | ||||||
| 0 | 48 | −.14 | −.08 | |||||||
| 9–18 | 49 | .02 | −.12 | |||||||
| PBEQ negative appraisals | 0 | 68 | −.17 | −.01 | .59** | |||||
| 0 | 47 | −.04 | −.10 | .58** | ||||||
| 9–18 | 49 | .12 | −.10 | .72** | ||||||
| Positive symptoms | 0 | 68 | .20 | −.05 | .16 | .17 | ||||
| 0 | 47–49 | .08a | −.06a | .30 b* | .29 c* | |||||
| 9–18 | 49 | .23 | −.24 | .64** | .58** | |||||
| Negative symptoms | 0 | 68 | −.12 | −.21 | −.02 | .13 | .25* | |||
| 0 | 47–49 | −.16a | −.23a | .05b | .13c | .27a | ||||
| 9–18 | 49 | .06 | −.13 | .15 | .31* | .39** | ||||
| General symptoms | 0 | 68 | −.03 | −.04 | .37** | .42** | .60** | .49** | ||
| 0 | 47–49 | −.15a | −.03a | .40 b** | .43 c** | .59 a** | .48 a** | |||
| 9–18 | 49 | .19 | −.04 | .63** | .58** | .78** | .56** | |||
| Overall symptoms | 0 | 68 | .01 | −.11 | .25* | .33** | .77** | .68** | .92** | |
| 0 | 47–49 | −.12a | −.12a | .33 b* | .38 c** | .74 a** | .72 a** | .91 a** | ||
| 9–18 | 49 | .20 | −.14 | .60** | .59** | .87** | .69** | .96** | ||
| BDI-7 suicidal ideation | 0 | 68 | −.01 | −.02 | .43** | .51** | .25* | .00 | .45** | .34** |
| 0 | 47–49 | −.02a | −.02a | .46 b** | .51 c** | .36 a* | −.02a | .45 a** | .36 a* | |
| 9–18 | 49 | .11 | −.07 | .57** | .47** | .50** | .30* | .47** | .51** |
Note: Abbreviations are explained in the first footnote to Table 1.
aN = 49.
b N = 48.
c N = 47.
*P < .05; ** P < .01. All significant results (P < .05) are highlighted in bold.
Cross-sectional Analyses
Baseline.
All results in the full sample (reported here) were replicated in those with full baseline and follow-up data (supplementary table S1). Total symptoms were related to suicidal ideation through the negative cognitive appraisals alone (CSE = 0.13, 95% CI = 0.04, 0.25) and the combined negative cognitive appraisals and negative metacognitive beliefs pathways (CSE = 0.03, 95% CI = −0.00, 0.11). No direct (unmediated) effect was observed. The same pattern was observed for positive symptoms. Overall, the effects suggest a 1 SD increase in overall or positive symptoms were indirectly associated with small increases in suicidal ideation (CSEs = 0.12–0.18), with approximately 70% of the indirect effects accounted for by the negative cognitive appraisals alone pathway, and 20% by the combined negative cognitive appraisals and negative metacognitive beliefs pathway. Negative symptoms did not have a direct or indirect relationship with suicidal ideation. General symptoms had both a direct effect on suicidal ideation, suggesting a 0.03 unit increase in suicidal ideation scores for each unit increase in general symptoms (UDE 0.03, SE 0.012, P < .05) and an indirect (mediated) effect (CSE = 0.19, 95% CI = 0.09, 0.34), suggesting that for a 1 SD increase in general symptoms, there was an additional 0.19 SD increase in suicidal ideation. As with total and positive symptoms, approximately 70% of this was accounted for by negative cognitive appraisals (CSE = 0.14, 95% CI = 0.05, 0.26).
The indirect effect of positive symptoms was not robust to controlling for negative and general symptoms. However, both the direct and indirect effects of general symptoms remained significant after controlling for positive and negative symptoms. Although the overall indirect effect was marginally smaller (CSE = 0.17, 95% CI = 0.06, 0.31), the proportion explained by negative cognitive appraisals was larger (80%) in this analysis.
9–18 Months
No direct effect of total symptom severity on suicidal ideation was observed at 9–18 months; however, this had an indirect effect through the combined pathway of negative cognitive appraisals and negative metacognitive beliefs (CSE = 0.10, 95% CI = −0.00, 0.29) (supplementary table S3). For a 1 SD increase in total symptoms, there was an overall 0.27 SD (95% CI = 0.06, 0.26) indirect increase in suicidal ideation. The combined appraisals and negative metacognitive beliefs pathway accounted for approximately 37% of this effect. There was also no direct effect of positive symptoms. Although they had a significant indirect effect on suicidal ideation, with a 1 SD increase in positive symptoms indirectly associated with a 0.31 SD (95% CI = 0.04, 0.61) increase in suicidal ideation, no one individual pathway was significant. The relative contributions of each individual pathway to this effect was similar to that for total symptoms. Negative symptoms had a direct effect on suicidal ideation at this time point, but no indirect effect. For each unit increase in negative symptoms, there was a 0.043 unit increase in suicidal ideation (SE = 0.021, P < .05). As with total and positive symptoms, general symptoms were not directly associated with suicidal ideation. As with total symptoms, general symptoms had an indirect effect on suicidal ideation via the combined appraisals and metacognitive beliefs pathway (CSE = 0.10, 95% CI = 0.01, 0.30). The effect sizes and relative contribution of individual pathways were similar to those for total and positive symptoms.
When we entered other symptom categories as covariates in the analyses of positive, negative, and general symptoms, the indirect effects for positive symptoms were no longer significant and the analysis of negative symptoms remained unchanged. General symptoms continued to not have a direct effect after controlling for positive and negative symptoms. The indirect effect remained significant; however, the contribution of the individual pathways changed, and the total indirect effect fell from a 0.32 SD (95% CI = 0.09, 0.58) change in suicidal ideation per 1 SD change in general symptoms to a 0.22 SD (95% CI = 0.04, 0.45) change. The contribution of negative metacognitive beliefs to this effect increased from a nonsignificant 49% to a significant 70% (CSE = 0.16, 95% CI = 0.01, 0.43), and the contribution of the combined appraisals and metacognitive beliefs pathway fell from a significant 31% to a nonsignificant 24%.
Longitudinal Analyses
Multiple Linear Regression.
Baseline psychotic symptoms and suicidal ideation, together with covariates, accounted for 54% of the variance in suicidal ideation at 9–18 months (supplementary table S2). Adding baseline negative cognitive appraisals to the model did not account for additional variance; however, adding negative metacognitive beliefs accounted for a further 5% (P < .05). An effect of female gender also emerged; this was associated with a significant reduction in BDI suicidal ideation scores (0.4 point, P < .05).
Mediation Analysis
No direct effects of baseline symptoms on suicidal ideation at 9–18 months were observed (table 3). There were also no indirect effects of baseline negative or positive symptoms. Baseline total symptoms and general symptoms, however, had indirect effects on suicidal ideation at follow-up via the combined appraisals and metacognitive beliefs pathway. A 1 SD increase in baseline overall symptoms and baseline general symptoms accounted for a 0.03 SD (95% CI = 0.00, 0.12) and 0.04 SD (95% CI = 0.00, 0.14) increase in suicidal ideation at 9–18 months via this pathway, respectively.
Table 3.
Results of Longitudinal Mediation Analyses
| Model (all n = 47) | Predictor | Suicidal ideation in 9- or 18-mo completers | ||
|---|---|---|---|---|
| Unstandardized coefficients (SE) | Completely standardized coefficients (95% CI) | |||
| Overall symptoms | Control variables | Age (baseline), y | 0.010 (0.008) | — |
| Gender (fixed) | −0.325 (0.170)* | — | ||
| Education (baseline) | −0.013 (0.029) | — | ||
| Treatment allocation | −0.082 (0.168) | — | ||
| Suicidal ideation at mo 0 | 0.515 (0.122)*** | — | ||
| 9- or 18-mo data | 0.299 (0.200) | — | ||
| Independent variables | Overall symptoms at mo 0 (direct effect) | 0.001 (0.007) | — | |
| Negative cognitive appraisals at mo 0 | −0.022 (0.034) | — | ||
| Negative metacognitive beliefs at mo 0 | 0.043 (0.023)* | — | ||
| R2 | 0.562*** | |||
| Bootstrap indirect effects of | Overall symptoms > Negative cognitive appraisals | −0.001 (0.002) 95% CI (−0.007, 0.001) |
−0.022 (−0.049, 0.253) | |
| Overall symptoms > Negative metacognitive beliefs | 0.002 (0.003) 95% CI (−0.001, 0.011) |
0.038 (−0.029, 0.235) | ||
| Overall symptoms > Negative cognitive appraisals > Negative metacognitive beliefs |
0.001** (0.001) 95% CI (0.000, 0.006) |
0.028** (0.000, 0.120) | ||
| Total indirect effect | 0.002 (0.003) 95% CI (−0.002, 0.012) |
0.045 (−0.049, 0.253) | ||
| Positive symptoms | Control variables | Age (baseline), y | 0.010 (0.008) | — |
| Gender (fixed) | −0.354** (0.167)a | — | ||
| Education (baseline) | −0.014 (0.029) | — | ||
| Treatment allocation | −0.067 (0.166) | — | ||
| Suicidal ideation at mo 0 | 0.538*** (0.121)a | — | ||
| 9- or 18-mo data | 0.308 (0.196) | — | ||
| Independent variables | Positive symptoms at mo 0 (direct effect) | −0.012 (0.020) | — | |
| Negative cognitive appraisals at mo 0 | −0.020 (0.034) | — | ||
| Negative metacognitive beliefs at mo 0 | 0.045* (0.023)a | — | ||
| R2 | 0.566**a | — | ||
| Bootstrap indirect effects of | Positive symptoms > Negative cognitive appraisals | −0.002 (0.004) 95% CI (−0.017, 0.002) |
−0.013 (−0.135, 0.018) | |
| Positive symptoms > Negative metacognitive beliefs | 0.005 (0.009) 95% CI (−0.005, 0.032) |
0.041 (−0.040, 0.231) | ||
| Positive symptoms > Negative cognitive appraisals > Negative metacognitive beliefs | 0.002 (0.004) 95% CI (−0.002, 0.014) |
0.019 (−0.013, 0.105) | ||
| Total indirect effect | 0.006 (0.009) 95% CI (−0.017, 0.002) |
0.048 (−0.054, 0.236) | ||
| Negative symptoms | Control variables | Age (baseline), y | 0.011 (0.007) | — |
| Gender (fixed) | −0.322* (0.161)a | — | ||
| Education (baseline) | −0.005 (0.029) | — | ||
| Treatment allocation | −0.125 (0.167) | — | ||
| Suicidal ideation at mo 0 | 0.522*** (0.115)a | — | ||
| 9- or 18-mo data | 0.269 (0.194) | — | ||
| Independent variables | Negative symptoms at mo 0 (direct effect) | 0.022 (0.017) | — | |
| Negative cognitive appraisals at mo 0 | −0.024 (0.033) | — | ||
| Negative metacognitive beliefs at mo 0 | 0.044* (0.022)a | — | ||
| R2 | 0.580**a | — | ||
| Bootstrap indirect effects of | Negative symptoms > Negative cognitive appraisals | −0.001 (0.006) 95% CI (−0.015, 0.002) |
−0.009 (−0.118, 0.016) | |
| Negative symptoms > Negative metacognitive beliefs | −0.001 (0.006) 95% CI (−0.014, 0.011) |
−0.013 (−0.125, 0.079) | ||
| Negative symptoms > Negative cognitive appraisals > Negative metacognitive beliefs | 0.001 (0.003) 95% CI (−0.002, 0.011) |
0.011 (−0.018, 0.016) | ||
| Total indirect effect | −0.001 (0.006) 95% CI (−0.012, 0.014) |
−0.010 (−0.111, 0.105) | ||
| General symptoms | Control variables | Age (baseline), y | 0.009 (0.008) | — |
| Gender (fixed) | −0.347* (0.173)a | — | ||
| Education (baseline) | −0.014 (0.029) | — | ||
| Treatment allocation | −0.075 (0.166) | — | ||
| Suicidal ideation at mo 0 | 0.531*** (0.125)a | — | ||
| 9- or 18-mo data | 0.318 (0.203) | — | ||
| Independent variables | General symptoms at mo 0 (direct effect) | −0.004 (0.014) | — | |
| Negative cognitive appraisals at mo 0 | −0.020 (0.034) | — | ||
| Negative metacognitive beliefs at mo 0 | 0.044* (0.023)a | — | ||
| R2 | 0.562**a | — | ||
| Bootstrap indirect effects of | General symptoms > Negative cognitive appraisals | −0.002 (0.004) 95% CI (−0.015, 0.003) |
−0.025 (−0.171, 0.035) | |
| General symptoms > Negative metacognitive beliefs | 0.005 (0.006) 95% CI (−0.001, 0.023) |
0.061 (−0.019, 0.248) | ||
| General symptoms > Negative cognitive appraisals > Negative metacognitive beliefs |
0.003** (0.002)a 95% CI (0.000, 0.013) |
0.035** (0.004, 0.141) | ||
| Total indirect effect | 0.006 (0.007)a 95% CI (−0.031, 0.024) |
0.071 (−0.044, 0.279) | ||
Note: Exact P values for completely standardized indirect effects not available. Significance (P < .05) inferred when 95% confidence intervals exclude zero.
aRemained or became significant (P < .05) after entering other symptom groups as covariates.
*P < .1, **P < .05, ***P < .01.All significant results (P < .05) are highlighted in bold.
The analyses for general, positive, and negative symptoms were largely unaffected by controlling for other symptom categories, although a significant direct effect of baseline negative metacognitive beliefs (UDE = 0.051, SE = 0.023, P = .03) emerged in the general symptoms analysis and, as with the linear regression, a significant association between suicidal ideation and female gender emerged in each analysis, with a similar effect size.
Discussion
We tested a metacognitive model of suicidal ideation in people with psychosis not taking antipsychotic medication, a group considered to be at particularly high risk of suicide.3,4 We tested whether psychotic symptoms may contribute to increased suicidal ideation not only directly, but also indirectly via appraisals of symptoms and metacognitive beliefs about the probability and consequences of losing mental control.23,24
We found no evidence that positive or total symptom severity has a direct effect on suicidal ideation in this group. Only concurrent general symptoms had a direct effect at baseline, and only concurrent negative symptoms had a direct effect at follow-up. Concurrent general symptoms also had an indirect effect on baseline suicidal ideation, mediated by negative cognitive appraisals. This was robust to controlling for other symptom categories. However no indirect effect of negative symptoms was found, and the indirect effect of positive symptoms was not robust to controlling for general and negative symptoms. At 9–18 months, a similar pattern emerged. However, negative metacognitive beliefs played a more significant role at this point, which suggests the psychological mechanisms involved in suicidal ideation in psychosis may change over time in this group. They either formed part of the indirect pathway, mediating the mediating effect of negative cognitive appraisals (positive symptoms and general symptoms), or were a sole mediator (general symptoms controlling for positive and negative symptoms). Again, the pathway linking general symptoms and suicidal ideation was the only indirect pathway robust to controlling for other symptom categories.
The longitudinal analyses are relevant to interpreting these findings. No direct effect of baseline general symptoms on later suicidal ideation was evident, but it had an indirect effect through concurrently measured negative cognitive appraisals and negative metacognitive beliefs. Although this indirect pathway explained only a very small amount of future suicidal ideation, both the linear regression and the mediation analyses (general symptoms, controlling for negative and positive symptoms) suggested a 1-point increase in baseline negative metacognitive beliefs may directly account for a 0.05-point increase in suicidal ideation at 9–18 months, which corresponds to a 0.5-point increase on the BDI suicide item (scored 0–3) per 10-point increase in negative metacognitive beliefs (scored 6–24). Notably, these beliefs did not predict concurrent suicidal ideation at baseline. If further research confirms these findings, high negative metacognitive beliefs at baseline may be a useful predictor of later increases in suicidal ideation in people with psychosis who are not currently taking antipsychotic medication, both directly and as a mediator of early general symptoms.
Limitations
We used a single-item measure of suicidal ideation; however, Desseilles et al.50, in a study of 281 suicide attempters, concluded the single suicide item represented a valid approach to assess suicidal ideation, a finding replicated by Brown and colleagues51 in a sample of 5319 patients. Endorsing suicidal ideation on the BDI item also has important implications for clinical risk assessment.51 The BDI data were treated as interval for the analyses. This is in line with previous studies,45–48 and dichotomizing the data for logistic regression would incur a substantial loss of statistical power.52,53 There is debate over the best way to conceptualize questionnaire data,54 but we encourage attempts to replicate these findings using full-scale measures (eg, the Beck Scale for Suicidal Ideation55). Evidence suggests the PANSS may have a 5-factor structure.56,57 We used the traditional 3-factor structure,34 because this is widely used and interpretable by clinicians.58 Although a larger sample would have greater power to detect smaller effects with greater precision, in-depth psychological studies of people with psychosis who are antipsychotic-free are rare, partly because few people with psychosis are not taking antipsychotics. Finally, the analyses tested a theoretically driven model, but alternative ordering of the variables is also plausible. Causal claims await the results of randomized controlled “interventionist-causal” trials,59 where the effect of selectively reduce negative metacognitive beliefs on suicidality can be assessed.
Implications
Consistent with previous findings, that fears of mental disintegration are strongly associated with suicide in psychosis,3 our results suggest that the way people appraise their symptoms and their consequences, including whether they heighten concerns about losing mental control, may partly determine whether they lead to thoughts of suicide. RCTs of interventions that either address negative metacognitive beliefs, such as MCT,18 or directly enhance self-integration, such as Metacognitive Reflection and Insight Therapy60 and Cognitive Analytic Therapy,61,62 may be warranted to examine their effect on suicidality. Overall, our findings emphasize the importance of clinicians promoting a recovery-focused and appropriately optimistic outlook when working with people with psychosis, taking care to avoid providing information that might heighten negative illness appraisals and/or fears of losing mental control.
Funding
This is a secondary analysis of a trial funded by the National Institute for Health Research under its Research for Patient Benefit program (Grant reference number PB-PG-1208-18053).
Supplementary Material
Acknowledgments
We would like to thank Professor Anthony P Morrison (ACTION Trial Principal Investigator), Dr Melissa Pyle (ACTION Trial Manager), and the ACTION Trial research team. Dr Turkington receives royalties from books he has published on cognitive therapy, has received fees for delivering workshops on cognitive therapy, and has received lecture fees from pharmaceutical companies. Dr Hutton, Ms Di Rienzo, Ms Spencer, and Dr Taylor declare they have no conflicts of interest. The views expressed are those of the authors and not necessarily those of the UK National Health Service, the National Institute for Health Research, or the Department of Health.
References
- 1. Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull. 1990;16:571–589. [DOI] [PubMed] [Google Scholar]
- 2. Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005;62:247–253. [DOI] [PubMed] [Google Scholar]
- 3. Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9–20. [DOI] [PubMed] [Google Scholar]
- 4. Tiihonen J, Wahlbeck K, Lönnqvist J, et al. Effectiveness of antipsychotic treatments in a nationwide cohort of patients in community care after first hospitalisation due to schizophrenia and schizoaffective disorder: observational follow-up study. BMJ. 2006;333:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–962. [DOI] [PubMed] [Google Scholar]
- 6. Cassidy RM, Yang F, Kapczinski F, Passos IC. Risk factors for suicidality in patients with schizophrenia: a systematic review, meta-analysis, and meta-regression of 96 studies. Schizophr Bull. 2018;44:787–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang X, Fox KR, Ribeiro JD, Franklin JC. Psychosis as a risk factor for suicidal thoughts and behaviors: a meta-analysis of longitudinal studies. Psychol Med. 2018;48:765–776. [DOI] [PubMed] [Google Scholar]
- 8. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 9. Morrison AP. The interpretation of intrusions in psychosis: an integrative cognitive approach to psychotic symptoms. Behav Cogn Psychother. 2001;29(03):257–276. [Google Scholar]
- 10. Fialko L, Freeman D, Bebbington PE, et al. Understanding suicidal ideation in psychosis: findings from the Psychological Prevention of Relapse in Psychosis (PRP) trial. Acta Psychiatr Scand. 2006;114:177–186. [DOI] [PubMed] [Google Scholar]
- 11. Taylor PJ, Gooding PA, Wood AM, Johnson J, Pratt D, Tarrier N. Defeat and entrapment in schizophrenia: the relationship with suicidal ideation and positive psychotic symptoms. Psychiatry Res. 2010;178:244–248. [DOI] [PubMed] [Google Scholar]
- 12. Flavell JH. Metacognition and cognitive monitoring: a new area of cognitive-developmental inquiry. Am Psychol. 1979;34:906–911. [Google Scholar]
- 13. Moritz S, Lysaker PH. Metacognition—What did James H. Flavell really say and the implications for the conceptualization and design of metacognitive interventions [published online ahead of print June 12, 2018]. Schizophr Res. doi: 10.1016/j.schres.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 14. Moritz S, Andreou C, Schneider BC, et al. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin Psychol Rev. 2014;34:358–366. [DOI] [PubMed] [Google Scholar]
- 15. Huq SF, Garety PA, Hemsley DR. Probabilistic judgements in deluded and non-deluded subjects. Q J Exp Psychol A. 1988;40:801–812. [DOI] [PubMed] [Google Scholar]
- 16. Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the “jumping to conclusions” reasoning bias: a systematic review and meta-analysis. Schizophr Bull. 2016;42:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lysaker PH, Lyskaker JT.. Schizophrenia and the Fate of the Self. Oxford: Oxford University Press; 2008. [Google Scholar]
- 18. Wells A. Metacognitive therapy: cognition applied to regulating cognition. Behav Cogn Psychother. 2008;36(6):651–658. [Google Scholar]
- 19. Chan CC, Spencer CC, West C, Viegas C, Bedwell JS. Metacognitive processes in psychometrically defined schizotypy. Psychiatry Res. 2015;230:279–286. [DOI] [PubMed] [Google Scholar]
- 20. Sellers R, Varese F, Wells A, Morrison AP. A meta-analysis of metacognitive beliefs as implicated in the self-regulatory executive function model in clinical psychosis. Schizophr Res. 2017;179:75–84. [DOI] [PubMed] [Google Scholar]
- 21. Austin SF, Mors O, Nordentoft M, et al. Schizophrenia and metacognition: an investigation of course of illness and metacognitive beliefs within a first episode psychosis. Cognit Ther Res. 2015;39(1):61–69. [Google Scholar]
- 22. Morrison AP, Wells A. A comparison of metacognitions in patients with hallucinations, delusions, panic disorder, and non-patient controls. Behav Res Ther. 2003;41:251–256. [DOI] [PubMed] [Google Scholar]
- 23. Hutton P, Morrison AP, Wardle M, Wells A. Metacognitive therapy in treatment-resistant psychosis: a multiple-baseline study. Behav Cogn Psychother. 2014;42:166–185. [DOI] [PubMed] [Google Scholar]
- 24. Morrison AP, Pyle M, Chapman N, French P, Parker SK, Wells A. Metacognitive therapy in people with a schizophrenia spectrum diagnosis and medication resistant symptoms: a feasibility study. J Behav Ther Exp Psychiatry. 2014;45:280–284. [DOI] [PubMed] [Google Scholar]
- 25. Foster C, Startup H, Potts L, Freeman D. A randomised controlled trial of a worry intervention for individuals with persistent persecutory delusions. J Behav Ther Exp Psychiatry. 2010;41:45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freeman D, Dunn G, Startup H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry. 2015;2(4):305–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kerkhof A, van Spijker B. Worrying and rumination as proximal risk factors for suicidal behaviour. In: O’Connor R, Platt S, Gordon J, eds. International Handbook of Suicide Prevention. Chichester, UK: Wiley Blackwell; 2011. [Google Scholar]
- 28. Rogers ML, Joiner TE. Rumination, suicidal ideation, and suicide attempts: a meta-analytic review. Rev Gen Psychol. 2017;21(2):132–142. [Google Scholar]
- 29. O’Connor RC, Kirtley OJ. The integrated motivational-volitional model of suicidal behaviour. Philos Trans R Soc B Biol Sci. 2018;373(1754). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ahrens B, Linden M. Is there a suicidality syndrome independent of specific major psychiatric disorder? Results of a split half multiple regression analysis. Acta Psychiatr Scand. 1996;94:79–86. [DOI] [PubMed] [Google Scholar]
- 31. Bolton C, Gooding P, Kapur N, Barrowclough C, Tarrier N. Developing psychological perspectives of suicidal behaviour and risk in people with a diagnosis of schizophrenia: we know they kill themselves but do we understand why?Clin Psychol Rev. 2007;27:511–536. [DOI] [PubMed] [Google Scholar]
- 32. Morrison AP, Turkington D, Pyle M, et al. Cognitive therapy for people with schizophrenia spectrum disorders not taking antipsychotic drugs: a single-blind randomised controlled trial. Lancet. 2014;383(9926):1395–1403. [DOI] [PubMed] [Google Scholar]
- 33. Morrison AP, Wardle M, Hutton P, et al. Assessing cognitive therapy instead of neuroleptics: rationale, study design and sample characteristics of the ACTION trial. Psychos Psychol Soc Integr Approaches. 2013;5(1):82–92. [Google Scholar]
- 34. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 35. Birchwood M, Mason R, MacMillan F, Healy J. Depression, demoralization and control over psychotic illness: a comparison of depressed and non-depressed patients with a chronic psychosis. Psychol Med. 1993;23:387–395. [DOI] [PubMed] [Google Scholar]
- 36. Pyle M, Stewart SL, French P, et al. Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Interv Psychiatry. 2015;9:133–140. [DOI] [PubMed] [Google Scholar]
- 37. Taylor PJ, Pyle M, Schwannauer M, Hutton P, Morrison A. Confirming the structure of negative beliefs about psychosis and bipolar disorder: a confirmatory factor analysis study of the Personal Beliefs about Experience Questionnaire and Personal Beliefs about Illness Questionnaire. Br J Clin Psychol. 2015;54:361–377. [DOI] [PubMed] [Google Scholar]
- 38. Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: properties of the MCQ-30. Behav Res Ther. 2004;42:385–396. [DOI] [PubMed] [Google Scholar]
- 39. Beck AT, Guth D, Steer RA, Ball R. Screening for major depression disorders in medical inpatients with the beck depression inventory for primary care. Behav Res Ther. 1997;35(8):785–791. [DOI] [PubMed] [Google Scholar]
- 40. Beck A, Steer R.. Manual for the Beck Scale for Suicidal Ideation. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- 41. Brown GK. A Review of Suicide Assessment Mesaures for Intervention Research With Adults and Older Adults. Bethesda, MD: National Institute of Mental Health; 2000. [Google Scholar]
- 42. Hayes A. Introduction to Mediation, Moderation, and Conditional Process Analysis. New York, NY: Guilford; 2013. doi:978-1-60918-230-4 [Google Scholar]
- 43. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. [DOI] [PubMed] [Google Scholar]
- 44. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. [DOI] [PubMed] [Google Scholar]
- 45. Näslund J, Hieronymus F, Lisinski A, Nilsson S, Eriksson E. Effects of selective serotonin reuptake inhibitors on rating-scale-assessed suicidality in adults with depression. Br J Psychiatry. 2018;212:148–154. [DOI] [PubMed] [Google Scholar]
- 46. Teismann T, Forkmann T, Brailovskaia J, Siegmann P, Glaesmer H, Margraf J. Positive mental health moderates the association between depression and suicide ideation: a longitudinal study. Int J Clin Heal Psychol. 2017;18(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schmidt SJ, Schultze-Lutter F, Bendall S, et al. Mediators linking childhood adversities and trauma to suicidality in individuals at risk for psychosis. Front Psychiatry. 2017;8:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Brown LA, Contractor A, Benhamou K. Posttraumatic stress disorder clusters and suicidal ideation. Psychiatry Res. 2018;270:238–245. [DOI] [PubMed] [Google Scholar]
- 49. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York, NY: Lawrence Erlbaum Associates; 1988. doi: 10.1234/12345678 [DOI] [Google Scholar]
- 50. Desseilles M, Perroud N, Guillaume S, et al. Is it valid to measure suicidal ideation by depression rating scales?J Affect Disord. 2012;136:398–404. [DOI] [PubMed] [Google Scholar]
- 51. Green KL, Brown GK, Jager-Hyman S, Cha J, Steer RA, Beck AT. The Predictive validity of the beck depression inventory suicide item. J Clin Psychiatry. 2015;76:1683–1686. [DOI] [PubMed] [Google Scholar]
- 52. Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Purgato M, Barbui C. Dichotomizing rating scale scores in psychiatry: a bad idea?Epidemiol Psychiatr Sci. 2013;22:17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Allen I, Seaman C. Likert scales and data analyses. Qual Prog. 2007. doi: 10.1111/j.1365-2929.2004.02012.x [DOI] [Google Scholar]
- 55. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. [DOI] [PubMed] [Google Scholar]
- 56. van der Gaag M, Cuijpers A, Hoffman T, et al. The five-factor model of the Positive and Negative Syndrome Scale I: confirmatory factor analysis fails to confirm 25 published five-factor solutions. Schizophr Res. 2006;85:273–279. [DOI] [PubMed] [Google Scholar]
- 57. van der Gaag M, Hoffman T, Remijsen M, et al. The five-factor model of the Positive and Negative Syndrome Scale II: a ten-fold cross-validation of a revised model. Schizophr Res. 2006;85(1–3):280–287. [DOI] [PubMed] [Google Scholar]
- 58. Leucht S, Leucht C, Huhn M, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–942. [DOI] [PubMed] [Google Scholar]
- 59. Kendler KS, Campbell J. Interventionist causal models in psychiatry: repositioning the mind-body problem. Psychol Med. 2009;39(6):881–887. doi: 10.1017/S0033291708004467. [DOI] [PubMed] [Google Scholar]
- 60. Lysaker PH, Klion R.. Recovery, Meaning-Making, and Severe Mental Illness: A Comprehensive Guide to Metacognitive Reflection and Insight Therapy. New York, NY: Routledge; 2017. [Google Scholar]
- 61. Taylor PJ, Perry A, Hutton P, Seddon C, Tan R. Curiosity and the CAT: considering cognitive analytic therapy as an intervention for psychosis. Psychosis. 2015;7(3):276–278. [Google Scholar]
- 62. Taylor PJ, Perry A, Hutton P, et al. Cognitive analytic therapy for psychosis: a case series [published online ahead of print May 2, 2018]. Psychol Psychother Theory Res Pract. doi: 10.1111/papt.12183 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.