Abstract
Psychotic disorders often have been linked with violence. However, studies have shown that people with a psychotic disorder are more often victim than perpetrator of violence. The objective of this meta-analysis was to review prevalence rates for different types of victimization and to identify risk factors associated with victimization. Based on a search in MEDLINE, PsycINFO, and Web of Science, 27 studies were found with samples consisting of adults with a psychotic disorder and possible victimization occurring during adulthood and data on “violent victimization,” “sexual victimization,” “non-violent victimization,” and/or “victimization not otherwise specified.” The median prevalence rate for violent victimization was 20%, for sexual victimization 20%, nonviolent victimization 19%, and for victimization not otherwise specified 19%. Victimization rates were approximately 4–6 times higher than in the general community. Meta-analyses showed the following significant risk factors: delusion (OR = 1.69), hallucinations (OR = 1.70), manic symptoms (OR = 1.66), drugs (OR = 1.90) or alcohol abuse (OR = 2.05), perpetration of a crime (OR = 4.33), unemployment (OR = 1.31), and homelessness (OR = 2.49). Other risk factors like previous victimization, impaired social functioning, personality disorder, and living in a disadvantaged neighborhood were found only in 1 or 2 studies. Based on the results, we conclude that, depending on the examined time period, 1 in 5 (assessment period ≤3 y) or 1 in 3 (assessment period entire adulthood) people with a psychotic disorder was victim of a crime. Clinical, behavioral, and sociodemographic factors were significantly associated with victimization, as well as previous victimization. Prospective research into risk factors is needed to capture causal trajectories of victimization.
Keywords: schizophrenia, mental illness, victim, trauma, violence, meta-analysis
Introduction
People with a psychotic disorder are often perceived as dangerous and regularly associated with violent behavior by the public.1,2 Although in some situations, psychotic symptoms are significantly associated with violent behavior,3 the majority of people with psychosis never expresses violent behavior.4 In reality, people with severe mental illness are more commonly victim than perpetrator of violence.5 Compared with the general population, victimization rates for people with a severe mental illness are found to be 2 to more than a hundred times higher.6 It is apparent that victimization prevalence rates vary widely between studies, partly due to methodological differences, especially questionnaire design and interview mode, and/or differences in sample characteristics.6,7 Nevertheless, the picture that emerges from the literature is altogether grim: there is a high risk of victimization for people with a psychotic disorder.8,9
Why do people with a psychotic disorder have an increased risk of becoming victimized? The Lifestyle and Routine Activity Theory (L-RAT), which is an integration of the routine activity and the lifestyle-exposure theory,10,11 provides a theoretical framework for the elevated victimization risks.12 According to L-RAT, there are 3 important elements for a criminal event to occur: there has to be a motivated offender, a suitable target, and lack of a capable guardian.10 In line with this reasoning, routine activities and/or lifestyles that exposes people to high-risk places and people, during times when there is a lack of security or social guardianship to prevent the crime, increase the risk of becoming a victim, especially when one is an attractive target.11,13 Target attractiveness depends on the characteristics of the victim that may arouse the offenders’ anger or for instance the expectation that the victim will not be resistant to an attack.14
In addition, it has been suggested that clinical factors such as positive symptoms could make people with psychotic disorders more vulnerable to victimization.15,16 The same holds for other clinical factors, such as dysfunctional personality traits,17 which are frequently present in this population. Maybe these clinical factors contribute to the attractiveness of this group of people as a target. For instance, some symptoms may arouse anger in a potential offender or people may seem less resistant to an attack. Behavior that stems from addiction, which is more common in people with a psychotic disorder, is also related to victimization.18 as they expose substance abusers to dangerous situations with potential offenders. In addition, L-RAT stresses the role of sociodemographic factors that can play a role in victimization when they increase proximity to offenders, and target attractiveness and decrease the chances for adequate guardianship.19,20 For instance, people with a psychotic disorder are more likely to live in socially disorganized neighborhoods with higher crime rates,21 and have a greater risk of being single, homeless, and/or unemployed, compared with the general population.22 Also, victimological research has shown that negative life events such as previous victimization23 increase victimization risk either because the former victims still carry known risk characteristics, or because previous involvement in victimization has increased one’s vulnerability. The phenomenon of revictimization is known to be most pronounced among high-risk groups.24
Although these risk analyses confirm that people with psychosis may for various reasons have a greater possibility to be confronted with violence, to date, no comprehensive review of both prevalence rates and risk factors for this group is available. The objective of this study is to review the prevalence rates for violent, nonviolent, and sexual victimization because these rates have been reported to be higher in people with a psychotic disorder than in people from the general population. We have chosen to narrow down the focus on adulthood victimization because psychosis is rare in children, and the type and context of victimization as well as potential risk factors can be different during childhood.13 For example, childhood victimization is related to factors such as family stress, young maternal age, large family size, and poverty.25,26 It is likely that because people age and become more independent of their family, other factors could play a role. We expect that clinical, behavioral, sociodemographic factors and negative life experiences that can be related to the L-RAT (in which a suitable target get exposed to a motived offender in the absence of capable guardians), will be associated with victimization.
Methods
Search Strategy and Procedure
A search was performed in 3 bibliographic databases: MEDLINE, PsycINFO, and Web of Science. The following terms were applied: victimization, victimization or victim* in combination with schizophrenia, schizophreniform, psychosis, psychoses, or psychotic. Hits were independently reviewed by B.V. and S.N. A secondary search of reference lists was performed. Abstracts and full texts were screened to determine whether inclusion criteria were met. In case of inconsistency between raters, consensus was reached through discussion.
Inclusion and Exclusion Criteria
Studies were included if: (1) all participants were 18 years or older and had a diagnosis in the psychosis spectrum according to DSM-5, DSM-IV, DSM-III-R, or ICD criteria, (2) prevalence rates or risk factors of victimization were reported, (3) victimization took place during adulthood, (4) the time frame over which victimization was measured was mentioned, and (5) published in English in a peer reviewed journal. In case of missing information, the corresponding author was contacted. In case of multiple publications on a single data set, the paper with the largest sample size or the longest examined time frame was included.
Categorization of Victimization, Prevalence Rates, and Risk Factors
In this article, victimization is defined as an event in which an individual is the target of a criminal act by another individual.27 For the purpose of this review, 4 categories of victimization were distinguished based on frequently used victimization types although some overlap could not be avoided. “Violent victimization” consists of crimes that involve physical violence, threats with a weapon, robbery, mugging, assault, and sexual victimization. When studies reported results for sexual offences such as forced sexual penetration, sexual touch without consent, or sexual harassment, these were placed in the category “sexual victimization.” “Nonviolent victimization” contains crimes without physical contact including threats, theft of property or money, burglary, identity theft, and fraud. Studies that did not differentiate between victimization types, or that gave a total score based on more than 1 type were placed in a fourth category, “victimization not otherwise specified (NOS).” Because victimization chance inevitably increases with time, studies were arranged by the length of the examined time frame.
The risk factors are divided into 4 categories. First is the “clinical risk factors”; this is a broad category as we want to explore all possible clinical characteristics that are associated with victimization. The category consists of positive, negative, and general symptoms; comorbidity; affect related symptoms; treatment-related factors; and diagnosis. Apart from this we categorized the following 3 risk factors that are not specific for psychosis based on examination of previous victimization studies23,28: behavioral risk factors like substance abuse and being a perpetrator of a crime; sociodemographic risk factors, such as age, gender, ethnicity, education level, living situation, income, and social contacts; and as a fourth category, “negative life experiences” such as previous victimization and childhood abuse.
Quality Appraisal
The quality of the included studies was assessed with the Newcastle-Ottawa Quality Assessment Scale for Observational Non-randomized Studies.29 A modified version for cross-sectional studies was used. A total of 10 points could be allocated to the following categories: selection (representative of the sample, sample size, nonrespondents, and ascertainment), comparability (controlled for confounding factors), and outcome (assessment and statistics). Studies that scored above the median were considered high-quality studies.30 All studies were assessed by the authors B.V. and S.N.
Meta-analysis of the Risk Factors
Risk factors that were addressed by 3 or more studies were included in a meta-analysis. For the purpose of this analysis victimization was considered to be a dichotomous variable, and ORs were used as an effect size.31 A random effects model was chosen because we expected systematic heterogeneity among studies due to differences in the definition of victimization, methodology, and sample characteristics.32 When frequencies were reported, the Mantel-Haenszel (M-H) method recommended by Cochrane collaboration was used.33 With no frequencies available, or combined continuous and categorical independent variables, the generic Inverse Variance (IV) method with LogOR and SE was used,34 and OR and CIs 95% were converted to logORs and their SE. In case of reported t test, first Cohen’s d was calculated using software developed by Wilson (2001) and subsequently converted to log-transformed ORs and SE.35 In case of more than 1 OR for a single risk factor, the subcategories were divided into 2 groups and a new OR was calculated. Heterogeneity between studies was measured using Higgins I2. Heterogeneity around 25%, 50%, and 75% was interpreted as low, moderate, and high values, respectively.33 The meta-analyses were performed with Review Manager 5.3 (version 5.3.5) developed by the Cochrane collaboration.36 ORs ranging from 1.0 to 1.5 were considered as a weak association, OR between 1.6 and 2.5 as moderate, and ORs between 2.6 and 9.9 as strong.37
Publication Bias and Sensitivity Analysis
When more than 10 studies were available for 1 risk factor, possible publication bias was evaluated by examination of funnel plots.38 A sensitivity analysis was performed by repeating the meta-analyses while excluding all the studies one by one. If this had a considerable effect on heterogeneity or level of significance, the study was removed from the final analysis. This was based on consensus of the authors B.V., J.B., and G.P.
Results
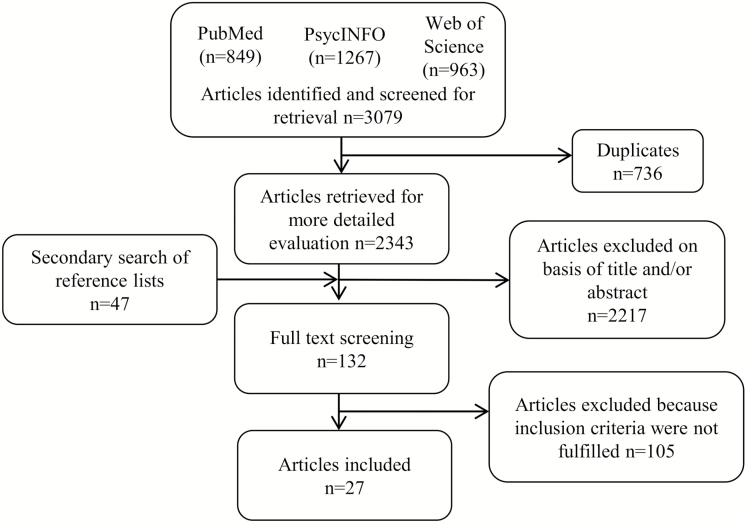
The search and cross-reference check yielded 3126 records (figure 1), of which 27 studies fulfilled the inclusion criteria and were included. Of these 27 studies, 26 studies reported prevalence rates and 19 studies addressed potential risk factors. Because Fortugno et al39 presented different results for an English, and European sample, outcomes of the two samples were included separately. Twenty-four studies were published after 2000, with 15 published in the past decade (2007 to June 2017).
Fig. 1.
Summary of study selection.
Ten studies were performed in the United States, 12 in Europe, 3 in Australia, 1 in New Zealand, 1 in Taiwan, and 1 in Nigeria. With the exception of 4 studies, which included only female patients, more male patients were included (mean 61%). The mean age was 38 years and the examined time frame ranged from 1 month to the entire adulthood. The 1-year time frame was most common, applied in 12 studies. Assessments were done with (structured) interviews or self-report questionnaires. Only 3 studies applied the same assessment method, the Lehman Quality of Life Interview.15,16,40
Prevalence Rates
The victimization prevalence rate varies widely, partly due to variation in length of the examined time period (table 1). In studies with time frames of maximum 3 years, the median prevalence rates for the victimization categories showed a higher degree of similarity. Within this time frame, 20% of the participants reported violent victimization (k = 13, range 4–51), 19% nonviolent victimization (k = 7, range 8–23), and 19% of the participants reported victimization in the not otherwise specified (NOS) category (k = 10, range 8–43). Sexual victimization in the previous year was assessed by 2 studies and reported by 15% and 24% of the participants. When entire adulthood was examined, violent victimization had the highest median prevalence rate with 66% (k = 4, range 42–82). Nonviolent victimization had a prevalence rate of 39% (k = 1), and sexual victimization 27% (k = 6, range 15–59).
Table 1.
Victimization Prevalence Rates for People With a Psychotic Disorder
| Study | Country | Sample | Male | Mean Age (SD) | Victimization NOS |
Violent Victimization | Sexual Victimization | Nonviolent Victimization | Examined Time Period | Assessment Method |
|---|---|---|---|---|---|---|---|---|---|---|
| Ascher-Svanum et al, 2006 |
United States | 1906 in- and outpatients | 61% | 41 (11) | 11% | —1 | — | — | 1 mo | Structured interview (victim of crime yes/ no) |
| Carter et al, 2011 | United States | 1635 in- and outpatients | 61% | 42 (11) | 11% | — | — | — | 1 mo | Schizophrenia Care and Assessment Program Health Questionnaire1 |
| Fitzgerald et al, 2005 | Australia | 347 patients | 62% | 34 (10) | 13% | 4% | — | 11% | 1 mo | LQLI2 |
| Crisanti et al, 2014 | United States | 507 outpatients | 63% | 42 | — | 10% | — | 9% | 6 mo | Quality of Live Interview- Very Brief QOLI-VB2 |
| Swanson et al, 2006 | United States | 1354 in- and outpatients | 74% | 41 | 20% | — | — | — | 6 mo | MacArthur community violence interview |
| Afe et al, 2017 | Nigeria | 79 outpatients | 0% | 38 (3) | — | 51% | 24% | — | 1 y | Intimate partner violence questionnaire3 |
| Bengtsson-Tops., 2012 | Sweden | 174 outpatients | 43% | 46 | — | 20% physical | 15% sexual | 21% threats | 1 y | Composite Abuse Scale questionnaire |
| Brunette et al, 1998 | United States | 172 patients4 | 78% | 33 (8) | — | 20% | — | 20% | 1 y | LQLI2 |
| Chapple et al, 2004 | Australia | 962 patients | 60% | 40 | 18% | — | — | — | 1 y | Victim of violence? |
| De Mooij et al, 2015 | Netherlands | 188 in- and outpatients | 63% | 49 (10) | — | 22% | — | 23% | 1 y | Dutch version of Integral Safety/ Security Monitor (Integrale Veiligheidsmonitor IVM) |
| Fortugno et al, 2013 | United Kingdom | 383 inpatients5 | 72% | 36 (11) | — | 38% | — | — | 1 y | MANSA Victim of physical violence? Yes/no |
| Fortugno et al, 2013 | Europe6 | 543 inpatients5 | 49% | 40 (12) | — | 28% | — | — | 1 y | MANSA |
| Goodman et al, 2001 | United States | 527 in- and outpatients | 69% | 41 (10) | — | 33% | — | — | 1 y | Revised Conflict Tactics Scale (CTS2)7 |
| Hiday et al, 2002 | United States | 153 outpatients | ? | ? | 31% | — | — | — | 1 y | Interview2 |
| Hsu et al, 2009 | Taiwan | 92 in-and outpatients | 46% | 37 (12) | 8% | — | — | — | 1 y | Taiwan Crime Victimization Survey8 |
| Morgan et al, 2015 | Australia | 1825 patients | 60% | ? | 39% | 16% | — | — | 1 y | Based on Australian Crime and Safety Survey |
| Silver et al, 2005 | New Zealand | 38 in- and outpatients | ? | 21 | — | 57.9% | 13.2% | 44.7% threat 15.8% attempted |
1 y | Have you been a victim of physical assault or sexual assault?9 |
| Dean et al, 2007 | England | 632 in- and outpatients10 | 57% | 38 (12) | — | 23% | — | — | 2 y | LQLP11 |
| Schomerus et al, 2008 | United Kingdom, France, Germany | 1204 patients | 62% | 41 (11) | — | 10% | — | 19% | 2.5 y | LQLI1 |
| Brekke et al 2001 | United States | 172 outpatients12 | 74% | 33 (7) | 38% | — | — | — | 3 y | Community Adjustment Form, semistructured interview13 |
| Horsselenberg et al 2016 | Netherlands | 102 outpatients | 75% | 39 (11) | 43% | — | — | — | 3 y | IVM |
| Honkonen et al, 2004 | Finland | 666 patients | 54% | 38 (10) | — | 6% | — | 8% property crime 1% drug-related 1% other crime |
3 y | Interview |
| Bebbington et al, 2011 | England | 38 participants | 38% | ? | — | — | 32%14 23%15 16%16 |
— | After the age of 16 | Computer-assisted self- completion interview |
| Darves-Bornoz et al, 1995 | France | 64 in- and outpatients | 0% | 34 | — | — | 22% | — | After the age of 16 | Semistructured questionnaire Were you a victim of rape? |
| Bengtsson-Tops., 2012 | Sweden | 174 outpatients | 43% | 46 | — | 51% physical | 32% sexual | 39% threats | Adulthood | Composite Abuse Scale questionnaire |
| Gearon et al, 2003 | United States | 54 outpatients17 | 0% | 41 (7) | — | 82% physical assault 54% robbed18 46% life threatened18 |
59% sexual abuse | — | Adulthood | Traumatic Life Events Questionnaire |
| Hacioglu Yildirim, et al, 2014 | Turkey | 70 inpatients | 0% | 39 (9) | — | 81% physical abuse | 24% sexual abuse 29% sexual harassment |
— | Adulthood | Traumatic Experiences Checklist |
| Hardy et al (2016) | United Kingdom | 228 in- and outpatients10 | 72% | 38 (11) | — | 42% | 15% | — | Adulthood | THQ Sexual and physical abuse |
Note: LQLP, Lancashire Quality of Life Profile; LQLI, Lehman Quality of Life Interview; MANSA, Manchester Short Assessment for quality of life; THQ, Trauma History Questionnaire.
1Study did not assess this victimization category.
2Violent crime (eg, assault, rape, mugging, or robbery) and nonviolent crime (eg, theft or being cheated).
3Physical abuse, sexual assault by partner/husband.
4Inclusion criteria: diagnosis of alcohol and drug use disorder in the past 6 months.
5Included only involuntary admitted patients.
6Czech republic, Germany, Lithuania, Poland, Slovakia, and Sweden.
7Physical assault (any assault, ranging from grabbing, pushing, or shoving to using a knife or gun) and sexual assault (forced or threatened oral, anal, or vaginal intercourse).
8Theft, assault robbery, mugging, kidnapping, intimidation, rape or sexual assault, fraud, and identity theft.
9Physical assault (eg, hitting, kicking, biting, choking, arm twisting, pushing, using a weapon) sexual assault (attempted or completed vaginal, oral, or anal intercourse)
10Exclusion criteria: primary substance misuse.
11Assaulted, beaten, molested, or otherwise a victim of violence (with physical contact).
12Exclusion criteria: current diagnosis of substance dependence.
13Robbery, assault, property offense, rape, or other.
14Talked to you in a sexual way that made you feel uncomfortable?
15Touching in a sexual way without your consent?
16Sexual intercourse without your consent?
17Inclusion criteria: illicit drug abuse or dependence in the past 3 months.
18With weapon.
Meta-analysis of the Risk Factors Associated With Victimization
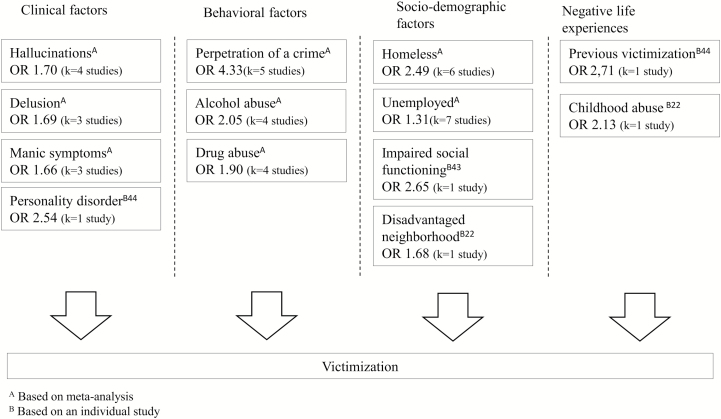
Table 2 shows the results of the meta-analyses and figure 2 shows a model of some of the important significant risk factors. Seventeen “sociodemographic” factors and 58 “clinical” factors were examined. Twenty-four potential risk factors were eligible for meta-analyses. One study15 could not be included in the meta-analysis because there was insufficient available statistical information. Forest plots of the meta-analyses can be found in the supplementary material. No test for publication bias was performed, due to an insufficient number of studies. Due to the moderate and high heterogeneity between studies, funnel plots could be misleading.41 The quality assessment showed that 4 studies were of low quality (median = 5, range = 3–7, see supplementary material) due to a small sample size or limited representativeness (eg, only females, exclusion of substance misuse and inclusion of comorbid substance abuse) of the sample. Sensitivity analysis showed that exclusion of low-quality studies in the meta-analysis revealed no substantial differences in ORs. Only 1 low-quality study by Hacioglu et al42 had a considerable effect on heterogeneity (I2 61% vs I2 0) of the education level analysis, and was for this reason excluded from this meta-analysis.
Table 2.
Meta-analysis of the risk factors associated with victimization
| Risk factors | Studies k | Victimized N | Total N | Random OR (95% CI) | Z | I2 (%) | p |
|---|---|---|---|---|---|---|---|
| Clinical factors | |||||||
| Higher overall symptoms score | 3 | 248 | 1474 | 1.03 (0.98–1.08) | 1.11 | 86 | 0.27 |
| Longer duration/worse outcome | 8 | 967 | 6219 | 1.19 (0.88–1.63) | 1.12 | 64 | 0.26 |
| Lower global functioning | 3 | 383 | 2841 | 1.11 (0.85–1.44) | 0.75 | 42 | 0.46 |
| Higher positive symptoms score | 4 | 370 | 1916 | 1.23 (0.97–1.55) | 1.74 | 87 | 0.08 |
| Delusion | 3 | 344 | 1678 | 1.69 (1.16–2.46) | 2.76 | 60 | < 0.01 |
| Hallucinations | 4 | 437 | 2466 | 1.70 (1.41–2.06) | 5.51 | 0 | < 0.001 |
| Higher negative symptoms score | 4 | 370 | 1915 | 0.95 (0.75–2.34) | 0.60 | 49 | 0.55 |
| Higher manic symptoms score | 3 | 587 | 2725 | 1.66 (1.27–2.17) | 3.73 | 73 | < 0.001 |
| Higher depression score | 4 | 633 | 3071 | 1.29 (0.89–1.86) | 1.36 | 88 | 0.17 |
| Past hospitalization | 3 | 326 | 1233 | 1.06 (0.70–1.59) | 0.26 | 44 | 0.79 |
| Type of psychotic diagnosis | 3 | 492 | 2803 | 1.01 (0.62–1.66) | 0.04 | 78 | 0.97 |
| Lower age of onset/age at first admission | 5 | 586 | 3543 | 1.38 (0.97–1.97) | 1.79 | 83 | 0.07 |
| Behavioral related factors | |||||||
| Drug abuse or dependence | 4 | 529 | 3461 | 1.90 (1.16–3.12) | 2.53 | 71 | 0.01 |
| Alcohol abuse or dependence | 4 | 523 | 3450 | 2.05 (1.17–3.56) | 2.53 | 71 | 0.01 |
| Perpetration of a crime | 5 | 693 | 4426 | 4.33 (2.53–7.41) | 5.34 | 81 | < 0.001 |
| Socio-demographic factors | |||||||
| Younger age | 9 | 1058 | 5484 | 1.02 (0.96–1.08) | 0.51 | 83 | 0.51 |
| Lower education level | 4 | 529 | 3473 | 0.98 (0.85–1.13) | 0.30 | 0 | 0.76 |
| Ethnicity | 3 | 492 | 2803 | 1.32 (0.91–1.92) | 1.46 | 35 | 0.14 |
| Unemployed | 7 | 853 | 3845 | 1.31 (1.04–1.64) | 2.32 | 23 | 0.02 |
| Less income | 4 | 423 | 2960 | 1.49 (0.83–2.67) | 1.35 | 76 | 0.19 |
| Homeless | 6 | 934 | 5417 | 2.49 (2.00–3.08) | 8.28 | 6 | < 0.01 |
| Living alone | 3 | 339 | 618 | 1.23 (0.90–1.68) | 1.30 | 0 | 0.19 |
| Marital status single | 5 | 586 | 3539 | 1.29 (0.85–1.95) | 1.21 | 56 | 0.22 |
| Gender female | 9 | 1111 | 5029 | 1.02 (0.80–1.30) | 0.17 | 59 | 0.87 |
Fig. 2.
Risk factors of victimization.
Clinical Factors
Overall Symptoms and Chronicity.
The meta-analysis showed no significant association between victimization and chronicity or worse outcome. Six studies found a trend or a significant association with longer duration of the illness, whereas in 2 studies shorter duration was significantly related to victimization. Furthermore, there was no association between higher overall symptoms score and victimization. Two studies found such an association only on bivariate level. There was also no association found between global functioning and victimization, neither in this meta-analysis, nor in the 3 studies separately.
Positive Symptoms.
One study found an association on bivariate level between general level of positive symptoms and victimization. However, meta-analysis showed only a weak, insignificant association (P =.08). Meta-analysis showed a moderate relationship with hallucination (OR = 1.70, P ≤ .001), as was the case on bivariate level in 2 of the individual studies. Furthermore, a meta-analysis showed a significant association between delusion and victimization (OR = 1.69, P ≤ .01). Two studies found a significant relationship on bivariate level.
Negative Symptoms.
The meta-analysis regarding negative symptoms showed no significant association between negative symptoms and victimization. Only one study found a significant association between negative symptoms and lower victimization prevalence rate.
Affect-Related Symptoms.
Three studies revealed a significant relationship between manic symptoms and victimization, with 2 on multivariate level. Accordingly, meta-analysis revealed that this association was moderate (OR = 1.66, P ≤ .01). Meta-analysis showed no significant association between victimization and depression. One study found a significant association on bivariate level.22
Treatment Related.
No significant association was found between past hospitalization and victimization, neither in this meta-analysis, nor in the individual studies.
Diagnosis.
Meta-analysis did not show a significant association between type of psychotic disorder and victimization. One study found that people with schizophrenia reported less victimization compared with other psychotic disorders, but only in bivariate analysis.
Age of Onset.
Results showed a weak, insignificant association between lower age of onset and victimization (P = .07). Lower age of onset or younger age at first admission was associated with victimization in three studies (2 on bivariate level and 1 on multivariate level).
Behavioral Factors
Alcohol and Drugs.
Meta-analysis showed that both drug and alcohol misuse or abuse were moderately associated with victimization (OR = 1.90, P = .01 and OR = 2.05, P = .01, respectively). Three studies found a significant association between drug abuse and victimization. Two studies found a significant association between alcohol abuse and victimization.
Perpetrator of a Crime.
Five studies revealed that perpetration of a crime (eg, being assaultive, arrested, or perpetrator of a crime) was strongly associated with victimization (OR = 4.33, P ≤ .01). All five studies showed a significant relationship between perpetration and victimization.
Sociodemographic Factors
Age.
Meta-analysis did not show a relationship between age and victimization. In 4 studies younger people reported more victimization. Four studies found no significant relationship. In one study, younger age was associated with higher risk for sexual abuse and lower risk for physical abuse.42
Education Level.
Results did not show a relationship between education level and victimization. Neither the meta-analysis nor the individual studies found this.
Ethnicity.
Meta-analysis did not reveal a significant relationship between victimization and ethnicity. Two studies did not find an association for ethnicity. One study found an association on bivariate level but not on multivariate level.22
Employment and Income.
Meta-analysis showed that unemployment was weakly associated with victimization (OR = 1.31, P = .02). Two studies found a significant relation with unemployment or not having meaningful daily activities. Meta-analysis of 4 studies showed no significant association with poor financial situation or less income. In 1 study a significant relationship was found but not in the 3 other studies.
Living Situation.
Meta-analysis of 6 studies showed a moderate relationship between homelessness and victimization (OR = 2.49, P ≤ .01). Four studies found a significant relationship, but in the 2 samples of Fortugno et al39 this association did not reach significance. There was no association found between living alone and victimization, neither in the meta-analysis, nor in 1 of the 3 included studies separately.
Being Single.
Meta-analysis of 5 studies did not reveal a relationship between being single and victimization. In 2 studies not having a romantic partner was associated with victimization, in 3 others this was not the case.
Gender.
Meta-analysis did not show a significant association between violent victimization and gender. In one study, women were more often victim of violent victimization and in another study men. The other 7 studies did not find a significant difference.
Review of the 4 Risk Factors: Categories Associated With Victimization
Supplementary material provides an overview of possible risk factors that were addressed by 1 or 2 studies. The following clinical factors were significantly associated with victimization: lower satisfaction of basic needs, higher satisfaction of social needs,16 hostility,16,42 unusual thought content, grandiosity, conceptual disorganization, excitement,16 higher disorganization score,43 higher emotional withdrawal, higher blunted affect score,42 higher general symptoms score,16 higher difficulty in delaying gratification score,42 personality disorder,22,44 higher affective lability score, higher anger score,42 higher anxiety score,22,42 higher depression score, deliberate self-harm, suicidal ideation,22 higher posttraumatic stress disorder score,45 and medication nonadherence.46 Behavioral factors that were significantly associated with victimization were: been in jail at least 1 night in the past 6 months,16 and nonviolent conviction.44 Sociodemographic factors that were associated with victimization were not having a disability pension,47 living in a disadvantaged neighborhood,22 impaired social and occupational functioning,43 not living with family,48 less than daily contact with family,44 less than 1 social contact a month was associated with less victimization,16 having an intimate relationship shorter than 10 years was associated with intimate partner violence,49 and gender with females reporting less nonviolent victimization and more sexual victimization.9 Negative life experiences that were significantly associated with victimization were previous victimization44 and childhood abuse.22
Discussion
The 27 studies on victimization in people with psychosis that were reviewed provided evidence for an increased risk for this group. Especially individuals who have symptoms and/or show behavior that impairs social functioning, and people who have a lifestyle that exposes them to potential offenders are at risk.
Prevalence Rate
The objective of this study was to review victimization prevalence rates and examine risk factors associated with victimization in people with a psychotic disorder. When victimization was examined over a short period (≤3 years) approximately 1 in 5 patients reported violent, nonviolent, sexual, or NOS crime. When victimization was examined during entire adulthood, 2 out of 3 people were found to have been a victim of violent victimization, followed by nonviolent victimization (39%), while the median prevalence rate of sexual victimization increased to 27%.
None of the studies used a matched control group that lived in the same area. However, some studies did mention the average prevalence rate for victimization for the entire country, during the time of the study. In these studies victimization rates were approximately between 4 and 6 times higher in people with a psychotic disorder, than for people in the general community.9,22,44
The broad range of prevalence rates between studies can be explained by the differences between study methodologies, such as the definition of victimization, reference period, and assessment method that were used. In some studies, people were only asked whether they had been a victim of a crime. A more extensive questionnaire is likely to be more sensitive, because specific questions prompt a better recall of incidents. Secondly, studies differ in sample characteristics. For example, a study that only included patients with substance abuse or dependence reported higher victimization prevalence rates.45 Finally, prevalence rates should be understood in the demographic context of the country. For example, Finland has lower crime rates than many other countries, and patients reported less victimization accordingly.47
Clinical Factors Associated With Victimization
Symptoms.
The included studies show that the associations between severity of illness, chronicity of the illness, global functioning, overall symptoms score, or general symptoms score and victimization are inconsistent. This is unexpected because most of the literature suggests a bidirectional relationship between victimization and symptoms. Where some individual studies show that psychotic symptoms are significantly associated with an increased victimization risk in adulthood,5,16,44 there is also an increasing evidence from large population-based studies that trauma plays a role in the development of psychotic symptoms.50–53 Even though causality is unclear, more significant associations in individual studies and the meta-analyses were expected due to the cross-sectional design of the studies. It is possible that when symptoms increase, the victimization risk is moderated by protective factors. For example, people could avoid social situations when they are not feeling well or their social support system becomes more protective and shields them from dangerous situations. Another possibility is that only specific symptoms are affected or responsible for the increase in victimization risk.
Meta-analysis shows a weak association between victimization and positive symptoms, particularly for delusion and hallucinations, but only when no other variables were controlled for. Because neither the exact time between victimization and symptom measurement was reported, nor the severity of the positive symptoms right before the victimization, the nature of this association remains unclear. However, it is likely that an increase in positive symptoms has a negative impact on social interactions and when the time between the victimization and assessment of positive symptoms is shorter, the association will be stronger.
Total level of negative symptoms was not associated with victimization. This confirms earlier studies, in which negative symptoms were not regarded as a risk factor because these symptoms lead to less social contacts (including violent contacts).54 However, in one of the studies,42 emotional withdrawal and blunted affect were significantly associated with sexual harassment of female patients. It should be noted, however, that it may be possible that these symptoms were a consequence of victimization, rather than a cause. This could also be the case for anxiety,22,42 which was increased in patients who were victimized, whereas depression scores were not. Furthermore, our meta-analysis showed an association between comorbid cluster B personality disorder and victimization.22,44 It is plausible that difficulties in interpersonal relationships, in these cases caused by maladaptive personality traits, make people more vulnerable to victimization.
Social Functioning.
Impaired social functioning was significantly associated with victimization in people with a psychotic disorder43 and may be an important risk factor in victimization. The idea is that impaired social functioning may restrain the development of a good social support system and enhance the chances of having conflicting relationships and behaving inadequately in a potentially dangerous social situation or lacking sufficient social guardianship from intimates or bystanders. However, this is speculation as this was not directly investigated by the included studies. Some indication was found that guardianship indeed can protect people from becoming a victim, because patients who had daily family contact,44 who lived with family,48 and who had a partner16,44 were less likely to report victimization. In addition, studies also show that problematic and even violent relationships are not uncommon in the lives of people with a psychotic disorder. Violence often occurs in the victim’s own home and is often committed by perpetrators from the victim’s own social network.9,55 This result indicates that people with a psychotic disorder sometimes have problematic relationships, which brings them in proximity to potential offenders.
The mechanisms underlying the relationship between social functioning and victimization were not addressed in the included studies. However, other studies show that deficits in social cognition are commonly found in people with a psychotic disorder,56 and are significantly associated with lower social functioning.57,58 People may become victimized because they do not recognize potentially dangerous social cues,59 miss cues that a social contract is violated, and fail to anticipate that their behavior can cause interpersonal problems or to remove themselves in time from a potentially dangerous situation.60 In victimological risk models, this would be subsumed under lack of security or self-protection.
Emotion Regulation and Aggressive Behavior.
Emotion dysregulation can have an impact on social interactions, as people experience and respond in a maladaptive (sometimes aggressive) way to emotional states.61 People may end up in a conflict in which they ultimately become victimized. Indeed, we found that patients who had higher scores on anger, affective lability, difficulty in delaying gratification score,42 deliberate self-harm, and suicidal ideation22 reported more victimization. Similarly, this could explain why manic symptoms were significantly associated with victimization. Manic episodes may lead to higher activity levels, impaired judgment, and reduced self-control, which place people in high-risk social situations.39
Treatment.
Type of treatment was not associated with victimization,16,44,47 nor was past hospitalization, time in hospital, and number of admissions.16,42 As such no evidence was found for the suggestion that involuntary admitted patients report more victimization because they have more conflicts, nor that treatment can protect people of becoming victimized.62This is in contrast to a study by Hiday et al,62 who found that people with a severe mental illness who were committed to outpatient treatment were significantly less likely to report violent victimization, compared with patient who did not receive this treatment. The authors suggest that the treatment improves medication adherence and reduces substance abuse and therefore protects people.
Behavioral Risk Factors
Substance abuse is another common problem in people with a psychotic disorder and is significantly associated with victimization. Those who abused or were dependent on alcohol or drugs had twice the odds to report victimization. Substance abuse itself, as well as the interaction with people (eg, drug dealers) that are involved, could increase victimization risk. Possibly provocative or aggressive behavior and socially inadequate reactions may underlie the strong association between victimization and perpetration of a crime, as offenders were 4.3 times more likely to report victimization compared with non-offenders.
Sociodemographic Risk Factors
As expected from theory, sociodemographic factors that are related to a risky lifestyle and/or deprived circumstances were significantly associated with victimization. First, patients that were unemployed had 1.3 times the odds of reporting victimization compared with those with a job. Unemployment or a lack of significant daily activities could create an incentive to become involved in risky situations or increase proximity to potential offender through routine activities such as hanging around in public spaces. Especially patients who are not receiving a disability pension seem to be at higher risk.47 Not having an income puts people in a dependent position leading to victimization.
Secondly, this article confirms that living in a disadvantaged neighborhood was significantly associated with victimization.22 The influence of the living situation was even more apparent for homeless people, who were 2.5 times as likely to become victim of a crime compared with peers with a roof over their head. Living on the streets or in these neighborhoods makes people and their possessions more vulnerable and brings them in close proximity to the offender population.
In contrast to studies in the general population, in which the victimization rate tends to be the highest during adolescence and young adulthood, declining as people age,63 our meta-analysis showed no significant association between age and victimization. The main explanation seems the relative high mean age (38 years) in the studies. It is plausible that also the period examined was a confounding factor. Older people might have reported more victimization when entire adulthood is examined, while young people will experience more victimization when the previous year is assessed.
Also contrary to people in the general population, for patients with psychosis, victimization was not associated with lower education level or ethnicity. And where in the general population males have in most countries a higher risk to become victim of a violent crime.64 in psychosis no such gender differences were found or results were inconsistent. The narrowing of the gender gap can be explained by the increased risk of intimate partner violence.49 In addition, Khalifeh and Dean65 suggest that severe mental illness could lead to a loss of meaningful social roles and impact behavior patterns, which lead to a less distinct gender pattern with respect to risk domains (eg, proximity to offenders, absence of a suitable guardian). Women with psychosis did report more sexual victimization during adulthood than men.9 This is in line with studies among the general population.
Negative Life Experiences Associated With Victimization
The complex causal relation between symptoms and victimization is again apparent in the high number of people (28%–40%) experiencing revictimization44,45,66 within 2 years. Additionally, 45% of the people who had been victimized reported childhood abuse.22 Possibly the risk factors that made people vulnerable in the first place persist or increase after the first victimization and enhance the chance of revictimization. An example of the latter would be that mental stress resulting from victimization may cause acting out provoking revictimization.
Limitations and Implications for Research and Treatment
The heterogeneity between studies in our review limits comparison and adequate interpretation of results. To make studies more homogenous in the future, it is advised to use the same and preferably an extensive victimization survey (see prevalence rates) and examine similar time periods of at least 1 year to capture rare incidents. More research is needed to confirm this.
In all studies, victimization measures were based on self-report, which is unfortunately more apt to be influenced by memory or reporting bias.39 However, self-report is more adequate especially for this group than police reports because people with a psychotic disorder are less likely to have an official police report of the victimization.67 Another limitation is the absence of a neighborhood matched control group. Although results revealed that the victimization prevalence is high, it is unknown how much higher these rates are compared with the general population that lives in the same neighborhood or circumstances. In addition, most studies were performed in high-income Western countries and findings cannot be generalized as such to patients in other parts of the world. It is difficult to say how prevalence rates would be in these countries as there is little information available on this topic. It possibly depends on factors such as crime rate of a country, the status of people with a mental disorder, and availability or quality of mental health care. In future research, the influence of country characteristics should be studied to confirm these hypotheses.
To gain a better understanding of why people are victimized more information is needed on lifestyle and related routine activities, type of incidents, the context (eg, where was it, who was the offender), and the process of cause and effect.68 To gain knowledge on risk factors, it is important to investigate mediating and moderating factors that influence victimization risk. For example, childhood abuse may be a common cause for adulthood victimization and risk factors such as hallucinations and substance abuse. Another example is that victimization risk is possibly moderated by social withdrawal or avoidance, as this could limit social contacts and possible conflicts. Because of the cross-sectional nature of most studies, it is unclear whether potential risk factors were (already) present at the time of the victimization. In the future, a prospective design should be utilized to investigate the risk factors and to capture causal trajectories of victimization.
To prevent victimization, intervention programs should be developed targeting the risk factors. In the Netherlands, for example, a body-oriented resilience training has been developed and is currently under evaluation, with the aim to decrease victimization risk in people with a psychotic disorder (De Vries et al, in preparation).69 Of special importance seems the detection of victimization experiences by clinicians, subsequent referrals to police and/or available services for crime victims, and interventions to mitigate traumatic stress and prevent revictimization.
Conclusions
Every year approximately 1 in 5 individuals with a psychotic disorder becomes victimized. However, not every patient has the same risk of becoming a victim. Clinical factors such as hallucinations, delusions, manic symptoms, and a personality disorder may increase target attractiveness. The offender may see someone with many symptoms as an easy target, or they may provoke anger or aggression more easily in potential offenders. People whose social functioning is impaired face additional risks because they may not be able to develop a social network that protects them and because they may have difficulty to detect social threats in time. Substance abuse and criminal behavior may also increase the victimization risk as this not only provokes potential offenders, it also brings people in close proximity to possible offenders. The demographic factors such as homelessness, unemployment, and living in a disadvantaged neighborhood possibly affect lifestyles that are associated with victimization as these factors could expose people to high-risk places and people when no capable guardian is around to prevent the crime. Where meta-analysis only highlights bivariate associations, L-RAT in this way helps to see how the different risk factors are mutually related, suggesting that there is a small group of patients who have a high risk of becoming victimized. More prospective research is needed to capture the causal trajectories of victimization and investigate mediating or moderating factors that protect or increase the victimization risk.
Supplementary Material
Acknowledgments
This study is financed by the Netherlands Organization for Scientific Research (now; 432-12-807) as part of the research program “Geweld tegen psychatrische patienten” (Violence against psychiatric patients).
Conflicts of Interest: The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Vilhauer RP. Depictions of auditory verbal hallucinations in news media. Int J Soc Psychiatry. 2015;61:58–63. [DOI] [PubMed] [Google Scholar]
- 2. Clement S, Foster N. Newspaper reporting on schizophrenia: a content analysis of five national newspapers at two time points. Schizophr Res. 2008;98:178–183. [DOI] [PubMed] [Google Scholar]
- 3. Coid JW, Ullrich S, Bebbington P, Fazel S, Keers R. Paranoid ideation and violence: meta-analysis of individual subject data of 7 population surveys. Schizophr Bull. 2016;42:907–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hiday VA. Putting community risk in perspective: a look at correlations, causes and controls. Int J Law Psychiatry. 2006;29:316–331. [DOI] [PubMed] [Google Scholar]
- 5. Brekke JS, Prindle C, Bae SW, Long JD. Risks for individuals with schizophrenia who are living in the community. Psychiatr Serv. 2001;52:1358–1366. [DOI] [PubMed] [Google Scholar]
- 6. Maniglio R. Severe mental illness and criminal victimization: a systematic review. Acta Psychiatr Scand. 2009;119:180–191. [DOI] [PubMed] [Google Scholar]
- 7. Meijwaard SC, Kikkert M, de Mooij LD et al. . Risk of criminal victimisation in outpatients with common mental health disorders. PLoS One. 2015;10:e0128508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marley JA, Buila S. Crimes against people with mental illness: types, perpetrators, and influencing factors. Soc Work. 2001;46:115–124. [DOI] [PubMed] [Google Scholar]
- 9. Bengtsson-Tops A, Ehliasson K. Victimization in individuals suffering from psychosis: a Swedish cross-sectional study. J Psychiatr Ment Health Nurs. 2012;19:23–30. [DOI] [PubMed] [Google Scholar]
- 10. Cohen LE, Felson M. Social change and crime rate trends: a routine activity approach. Am Sociol Rev. 1979;44:588–608. [Google Scholar]
- 11. Hindelang MJ, Gottfredson MR, Garofalo J.. Victims of Personal Crime : An Empirical Foundation for a Theory of Personal Victimization. Cambridge, MA: Ballinger Publ; 1978. [Google Scholar]
- 12. McNeeley S. Lifestyle-routine activities and crime events. J Contemp Crim Justice. 2015;31:30–52. [Google Scholar]
- 13. van Dijk J. The criminal victimization of children and women in international perspective. In: Kury H, Redo S, Shea E, eds. Women and Children as Victims and Offenders: Background, Prevention, Reintegration. Vol 1 Switzerland: Springer; 2016:405–427. [Google Scholar]
- 14. Finkelhor D, Asdigian NL. Risk factors for youth victimization: beyond a lifestyles/routine activities theory approach. Violence Vict. 1996;11:3–19. [PubMed] [Google Scholar]
- 15. Schomerus G, Heider D, Angermeyer MC et al. . Urban residence, victimhood and the appraisal of personal safety in people with schizophrenia: results from the European Schizophrenia Cohort (EuroSC). Psychol Med. 2008;38:591–597. [DOI] [PubMed] [Google Scholar]
- 16. Fitzgerald PB, de Castella AR, Filia KM, Filia SL, Benitez J, Kulkarni J. Victimization of patients with schizophrenia and related disorders. Aust N Z J Psychiatry. 2005;39:169–174. [DOI] [PubMed] [Google Scholar]
- 17. Walsh E, Moran P, Scott C et al. . Prevalence of violent victimisation in severe mental illness. Br J Psychiatry. 2003;183:233–238. [DOI] [PubMed] [Google Scholar]
- 18. Dolan MC, Castle D, McGregor K. Criminally violent victimisation in schizophrenia spectrum disorders: the relationship to symptoms and substance abuse. BMC Public Health. 2012;12:445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Spano R, Freilich JD. An assessment of the empirical validity and conceptualization of individual level multivariate studies of lifestyle/routine activities theory published from 1995 to 2005. J Crim Justice. 2009;37:305–314. [Google Scholar]
- 20. Bunch J, Clay-Warner J, Lei M-K. Demographic characteristics and victimization risk: testing the mediating effects of routine activities. Crime Delinq. 2015;61:1181–1205. [Google Scholar]
- 21. Lögdberg B, Nilsson LL, Levander MT, Levander S. Schizophrenia, neighbourhood, and crime. Acta Psychiatr Scand. 2004;110:92–97. [DOI] [PubMed] [Google Scholar]
- 22. Morgan VA, Morgan F, Galletly C, Valuri G, Shah S, Jablensky A. Sociodemographic, clinical and childhood correlates of adult violent victimisation in a large, national survey sample of people with psychotic disorders. Soc Psychiatry Psychiatr Epidemiol. 2016;51:269–279. [DOI] [PubMed] [Google Scholar]
- 23. Amstadter AB, Elwood LS, Begle AM et al. . Predictors of physical assault: findings from the national survey of adolescents. Addict Behav. 2013;36:814–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Farrell G, Pease K. Once bitten, twice bitten: repeat victimisation and its implications for crime prevention. Police Res Group, Crime Prev Unit Pap. 1993;46:38 http://hdl.handle.net/2134/2149\nhttp://core.ac.uk/download/pdf/67259.pdf [Google Scholar]
- 25. Levey EJ, Gelaye B, Bain P et al. . A systematic review of randomized controlled trials of interventions designed to decrease child abuse in high-risk families. Child Abuse Negl. 2017;65:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wu SS, Ma CX, Carter RL et al. . Risk factors for infant maltreatment: a population-based study. Child Abuse Negl. 2004;28:1253–1264. [DOI] [PubMed] [Google Scholar]
- 27. Bjs. Bureau of justice statistics https://www.bjs.gov/content/pub/html/cvus/definitions.cfm. Accessed July 3, 2017.
- 28. Vézina J, Hébert M. Risk factors for victimization in romantic relationships of young women: a review of empirical studies and implications for prevention. Trauma Violence Abuse. 2007;8:33–66. [DOI] [PubMed] [Google Scholar]
- 29.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed July 10, 2017.
- 30. Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–1060. [DOI] [PubMed] [Google Scholar]
- 31. Lettell JH, Corcoran J, Pillai V. Systematic Reviews and Meta-analysis. New York, NY; Oxford University Press;2008.
- 32. Field AP, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63:665–694. [DOI] [PubMed] [Google Scholar]
- 33. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cleophas TJ, Zwinderman AH.. Statistics Applied to Clinical Studies. Vol 53 Intergovernmental Panel on Climate Change. Dordrecht: Springer Netherlands; 2012. [Google Scholar]
- 35. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Meta-regression. In: Introduction to Meta-Analysis. Chichester, UK: John Wiley & Sons, Ltd; 2009:187–203. [Google Scholar]
- 36. Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. [Google Scholar]
- 37. Rosenthal JA. Qualitative descriptors of strength of association and effect size. J Soc Serv Res. 1996;21:37–59. [Google Scholar]
- 38. Sterne JA, Sutton AJ, Ioannidis JP et al. . Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 39. Fortugno F, Katsakou C, Bremner S et al. . Symptoms associated with victimization in patients with schizophrenia and related disorders. PLoS One. 2013;8:e58142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brunette M, Drake RE. Gender differences in homeless persons with schizophrenia and substance abuse. Community Ment Health J. 1998;34:627–642. [DOI] [PubMed] [Google Scholar]
- 41. Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006;333:597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hacioglu Yildirim M, Yildirim EA, Kaser M et al. . The relationship between adulthood traumatic experiences and psychotic symptoms in female patients with schizophrenia. Compr Psychiatry. 2014;55:1847–1854. [DOI] [PubMed] [Google Scholar]
- 43. Chapple B, Chant D, Nolan P, Cardy S, Whiteford H, McGrath J. Correlates of victimisation amongst people with psychosis. Soc Psychiatry Psychiatr Epidemiol. 2004;39:836–840. [DOI] [PubMed] [Google Scholar]
- 44. Dean K, Moran P, Fahy T et al. . Predictors of violent victimization amongst those with psychosis. Acta Psychiatr Scand. 2007;116:345–353. [DOI] [PubMed] [Google Scholar]
- 45. Gearon JS, Kaltman SI, Brown C, Bellack AS. Traumatic life events and PTSD among women with substance use disorders and schizophrenia. Psychiatr Serv. 2003;54:523–528. [DOI] [PubMed] [Google Scholar]
- 46. Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67:453–460. [DOI] [PubMed] [Google Scholar]
- 47. Honkonen T, Henriksson M, Koivisto AM, Stengård E, Salokangas RK. Violent victimization in schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2004;39:606–612. [DOI] [PubMed] [Google Scholar]
- 48. Brekke JS, Mathiesen SG. Effects of parental involvement on the functioning of noninstitutionalized adults with schizophrenia. Psychiatr Serv. 1995;46:1149–1155. [DOI] [PubMed] [Google Scholar]
- 49. Afe TO, Emedoh TC, Ogunsemi OO, Adegohun AA. Socio-demographic characteristics, partner characteristics, socioeconomic variables, and intimate partner violence in women with schizophrenia in South-South Nigeria. J Health Care Poor Underserved. 2017;28:707–720. [DOI] [PubMed] [Google Scholar]
- 50. Bebbington PE, Bhugra D, Brugha T et al. . Psychosis, victimisation and childhood disadvantage: evidence from the second British national survey of psychiatric morbidity. Br J Psychiatry. 2004;185:220–226. [DOI] [PubMed] [Google Scholar]
- 51. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? a study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Velikonja T, Fisher HL, Mason O, Johnson S. Childhood trauma and schizotypy: a systematic literature review. Psychol Med. 2015;45:947–963. [DOI] [PubMed] [Google Scholar]
- 53. Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Swanson JW, Swartz MS, Van Dorn RA et al. . A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63:490–499. [DOI] [PubMed] [Google Scholar]
- 55. Kageyama M, Yokoyama K, Nagata S et al. . Rate of family violence among patients with schizophrenia in Japan. Asia-Pacific J Public Heal. 2015;27:652–660. [DOI] [PubMed] [Google Scholar]
- 56. Savla GN, Vella L, Armstrong CC, Penn DL, Twamley EW. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical evidence. Schizophr Bull. 2013;39:979–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Addington J, Girard TA, Christensen BK, Addington D. Social cognition mediates illness-related and cognitive influences on social function in patients with schizophrenia-spectrum disorders. J Psychiatry Neurosci. 2010;35:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roberts DL, Combs DR, Willoughby M et al. . A randomized, controlled trial of social cognition and interaction training (SCIT) for outpatients with schizophrenia spectrum disorders. Br J Clin Psychol. 2014;53:281–298. [DOI] [PubMed] [Google Scholar]
- 59. Huang J, Xu T, Chan RCK. Do patients with schizophrenia have a general or specific deficit in the perception of social threat? A meta-analytic study. Psychiatry Res. 2011;185:1–8. [DOI] [PubMed] [Google Scholar]
- 60. DePrince AP. Social cognition and revictimization risk. J Trauma Dissociation. 2005;6:125–141. [DOI] [PubMed] [Google Scholar]
- 61. Donahue JJ, Goranson AC, McClure KS, Van Male LM. Emotion dysregulation, negative affect, and aggression: a moderated, multiple mediator analysis. Pers Individ Dif. 2014;70:23–28. [Google Scholar]
- 62. Hiday V, Swartz M, Swanson J, Borum R, Wagner R. Impact of victimization on outpatient commitment among people with severe mental illness. Am J Psychiatry. 2002;159:1403–1411. [DOI] [PubMed] [Google Scholar]
- 63. Menard S, Covey HC. Age and gender variations in the victimization-offending relationship in a national sample, ages 11–88. Vict Offender. 2016;11:355–372. [Google Scholar]
- 64. Brennan IR, Moore SC, Shepherd JP. Risk factors for violent victimisation and injury from six years of the British crime survey. Int Rev Vict. 2010;17:209–229. [Google Scholar]
- 65. Khalifeh H, Dean K. Gender and violence against people with severe mental illness. Int Rev Psychiatry. 2010;22:535–546. [DOI] [PubMed] [Google Scholar]
- 66. Teasdale B, Daigle LE, Ballard E. Trajectories of recurring victimization among people with major mental disorders. J Interpers Violence. 2014;29:987–1005. [DOI] [PubMed] [Google Scholar]
- 67. Short TBR, Thomas S, Luebbers S, Mullen P, Ogloff JRP. A case-linkage study of crime victimisation in schizophrenia-spectrum disorders over a period of deinstitutionalisation. BMC Psychiatry. 2013;66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Siesling M, Habraken JM, Bongers IL, van Weeghel J. Victimisation of persons with severe mental illness: a qualitative study. J Ment Heal. In press. [Google Scholar]
- 69. van der Stouwe EC, de Vries B, Aleman A et al. . BEATVIC, a body-oriented resilience training with elements of kickboxing for individuals with a psychotic disorder: study protocol of a multi-center RCT. BMC Psychiatry. 2016;16:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.