Abstract
Purpose
Flexible flatfoot (FFF) is a widespread condition in juvenile patients. If symptomatic, FFF can require surgical treatment. The calcaneo-stop procedure has shown excellent clinical and radiographic outcomes and low rates of complications. The aim of the present study was to assess the sport practice of young athletes affected by FFF having undergone the calcaneo-stop procedure.
Methods
Between 2008 and 2016, 68 sport practitioners were bilaterally treated by the calcaneo-stop procedure, for a total of 136 FFF cases. Clinical evaluation, including the American Orthopedic Foot and Ankle Score (AOFAS), the Yoo et al score and The Foot & Ankle Disability Index (FADI) and FADI Sport scores were assessed. Radiographic evaluation was based on measurement of talar declination, Costa-Bertani’s angle and calcaneal pitch.
Results
Mean follow-up was 57.6 months (sd 16.8). The AOFAS score mean increased from 79.3 (sd 5.7) to 97.3 (sd 4.5) three years after surgery. The Yoo score improved from 3.1 (sd 1.0) preoperatively to 11.7 (sd 0.6) three years after surgery. The FADI Sport subscale mean improved from 74.1 (sd 10.4) preoperatively to 95.9 (sd 4.9) three years after surgery.
Costa-Bertani’s angle decreased from 156.1° (sd 4.2°) to 135.8° (sd 7.3°) at three years postoperatively; mean talar declination angle decreased from 44.2° (sd 6.3°) to 30.6° (sd 3.2°) at three years postoperatively and mean calcaneal pitch increased from 12.6° (sd 2.3°) to 16.3° (sd 1.3°) at three years postoperatively.
Conclusion
Adolescent patients who underwent the calcaneo-stop procedure reported satisfactory outcomes in terms of clinical and radiological evaluations. Moreover, our results showed an improvement of sport activity levels, with patients recovering sports activity within three months of surgery and without limitation in the execution of preferred activities.
Level of Evidence:
IV
Keywords: flexible flatfoot, symptomatic feet, sport practice, calcaneo-stop, young athletes
Introduction
Flexible flatfoot is the most common paediatric condition,1 it is physiological until ten years old and is clinically characterized by the loss of medial longitudinal arch and heel valgus.2 It is defined as ‘flexible’ if the medial arch is restored performing the Jack and the Tip Toe tests and the heel alignment is restored when standing on tiptoe.3
Juvenile flexible flatfoot is characterized by anatomical features including: heel valgus, subtalar joint subluxation with talus intra-rotation and plantar flexion and mid-tarsal joint abduction with navicular dorsal-subluxation. Tightness of the Achilles’ tendon could also be associated with these features.4
Despite a high prevalence of flexible flatfoot in children and adolescents, only a small proportion of cases are symptomatic with pain, fatigue and disability.5
Conservative treatment is preferred in most of cases with satisfying results; only in rare, selected, symptomatic and conservative-treatment-refractory cases is surgical treatment proposed. Surgical options described are: soft-tissue tensioning, arthroereisis, osteotomy and arthrodesis.5 Arthroereisis is a widespread option of treatment of flexible flatfoot in children. Nowadays, it is performed as subtalar extra-articular (SESA or calcaneo-stop) or with a subtalar intra-articular implant. Several authors have reported on the validity, efficacy, safety and mini-invasiveness of the arthroereisis techniques.6–9
The practise of sport has an important role to play in the improvement of mental and physical development, protects children from obesity and promotes additional health benefits.10 Young sport practitioners have a better quality of life,11 better brain cortical excitability12 and have enhanced long-term neural adaptation mechanisms and increased visuo-spatial abilities.13
The aim of this study was to assess the practise of sports in patients affected by FFF who have undergone the calcaneo-stop procedure.
Patients and methods
Eligibility criteria
Between 2008 and 2016, 326 flexible flatfeet in 216 patients were treated with the calcaneo-stop procedure at our institution.14 According to inclusion and exclusion criteria, 91 patients were eligible; during the investigation, 23 were lost at follow-up and excluded. A total of 68 treated patients were retrospectively reviewed and included in the present study.
Inclusion criteria were: (a) skeletal immaturity with growth cartilage visible on preoperative foot radiographs; (b) symptomatic flexible flatfoot deformity (pain, function and limitations and/or skin lesions) not responsive to conservative treatment;15 (c) surgical treatment with calcaneo-stop procedure; (d) bilateral treatment; and (e) all patients had participated in sports at a recreational or occasional level preoperatively, for at least three hours every week.
Exclusion criteria include those patients diagnosed with neurological or neuromuscular disorders, congenital or post-traumatic flatfoot, diabetes or immunological diseases.
All patients provided an informed consent to participate in the present investigation. This study was carried out according to the guidelines for Good Clinical Practice and the Declaration of Helsinki.
The cohort of 68 patients (136 feet) consisted of 38 male (55.9%) and 30 female (44.1%) patients and the mean age at time of surgery was 12.7 years (9 to 15). Practised sports were: soccer in 21 (30.9%) patients, basket in 18 (26.5%), volley in 13 (19.1%), swimming in ten (14.7%), tennis in four (5.9%) and cycling in two (2.9%).
Surgical technique
The calcaneo-stop procedure for correction of an idiopathic flexible flatfoot was indicated in patients who experienced pain during or after exercise, postural fatigue and failure of conservative treatment.16 All the patients under general anaesthesia were placed supine and with the foot in the internal rotation position. An incision of 2 cm was made under the skin on the lateral aspect of the sinus tarsi. Drilling with a 3.2-mm drill bit was performed vertically into the calcaneus from the superior to the inferior aspect opposite to the sinus tarsi after reduction of the subtalar eversion. A 4.5-mm cortical, stainless, self-tapping screw (8-mm head) with a length of 30 mm to 35 mm (the calcaneal-stop screw) (Synthes LCP, Bettlach, Switzerland) was inserted, such that the screw head impinged against the lateral aspect of the talus, preventing eversion at the subtalar joint. The dorsiflexion of the foot was evaluated with the knee extended, once appropriate placement of the screw had been radiographically verified in the neutral position.
Sport activities return, follow-up and screw removal protocol
Within three days of the surgery, weight-bearing is allowed. All patients were subjected to the rehabilitation protocol, consisting of proprioceptive exercises and stretching, avoiding running and jumping for the subsequent two months. After four to six weeks, patients undertook clinical and radiographic follow-up. After two months postoperatively, each patient was encouraged to practise their favourite sporting activity. The calcaneo-stop screw was removed at least three years from surgery.
Clinical and radiographic assessment
Clinical and functional outcomes of all patients were evaluated, before surgery, at one and three years after surgery, using the American Orthopedic Foot and Ankle Society (AOFAS) Ankle–Hindfoot score,17 Yoo et al’s clinical criteria,18 the Oxford Ankle Foot Questionnaire for Children (OxAFQ-C)19 and the Foot & Ankle Disability Index (FADI) and FADI Sport scores.20 The AOFAS Ankle– Hindfoot score consists of nine items under three different categories, i.e. pain (40 points), functional aspect (50 points) and alignment (ten points), totalling 100 points. Items on pain and functional limitation are answered by the patient, while the alignment items are answered by an examiner. The Yoo et al criteria assign 0 to 3 points for the following parameters: pain or callus, forefoot abduction, longitudinal arch and hindfoot valgus. Outcomes were considered satisfactory if final score is 8 or more. The OxAFQ-C is a self-reported health status measure questionnaire used to measure subjective well-being for child patients (aged five to 16 years) affected by foot and ankle conditions using issues that are considered important to children. The OxAFQ-C consists of four domains, Physical (six items, 24 points), School and Play (four items, 16 points), Emotional (four items, 16 points) and Footwear (one item, four points), for a total of 15 items. Domain scores can be transformed to a percentage scale (0% to 100%) to aid interpretation. The FADI is a region-specific self-reporting scale of function and includes 34 items divided into two subscales, the first (FADI) consisting of 26 items about activities of daily living (ADL) and pain and the second (FADI Sport) consisting of eight items about sports activities. Each item is scored on a five-point Likert scale (4 to 0) and, thereafter, the results are converted into percentages. Higher scores represent higher levels of function for each subscale. The ADL and sports subscales are scored separately.
For each patient, we recorded the times and the hours per week of sport practices before and one and three years after surgery; each sport was classified using Mitchell criteria.21
The Mitchell classific ation of sport relates individual competitive sports to the two general types of exercise: dynamic and static. Each sport is categorized by the level of intensity (low, medium, high) of dynamic or static exercise generally required to perform that sport during competition. It also recognizes those sports that pose significant risk due to bodily collision, either because of the probability of hard impact between competitors or between a competitor and an object, projectile or the ground.
All patients underwent anteroposterior (AP) and lateral weight-bearing foot radiograph preoperatively and at one and three years postoperatively. For each single patient, measurements of Kite’s angle, Costa-Bertani’s angle, talar declination and calcaneal pitch16 were assessed in a randomly chosen foot (Fig. 1). Kite’s angle is the angle between the longitudinal axis of the calcaneus and talus. Costa-Bertani’s angle is the angle between the line formed from the lower point of the medial sesamoid to the lower point of the talonavicular joint, and the line formed between the lower point of the talonavicular joint and the lower point of the posterior calcaneal tuberosity. The talar declination angle is the angle between the collum tali axis (originating from the centre of the body of the talus and extending through the bisection of the talar neck and head) and a horizontal line extending from the plantar surface of the calcaneus to the plantar surface of the fifth metatarsal head. The calcaneal pitch is the angle between the lines extending from the inferior portion of the calcaneocuboid joint to the same horizontal line along the plantar aspect of the calcaneus to the plantar surface of the fifth metatarsal head.
Fig. 1.
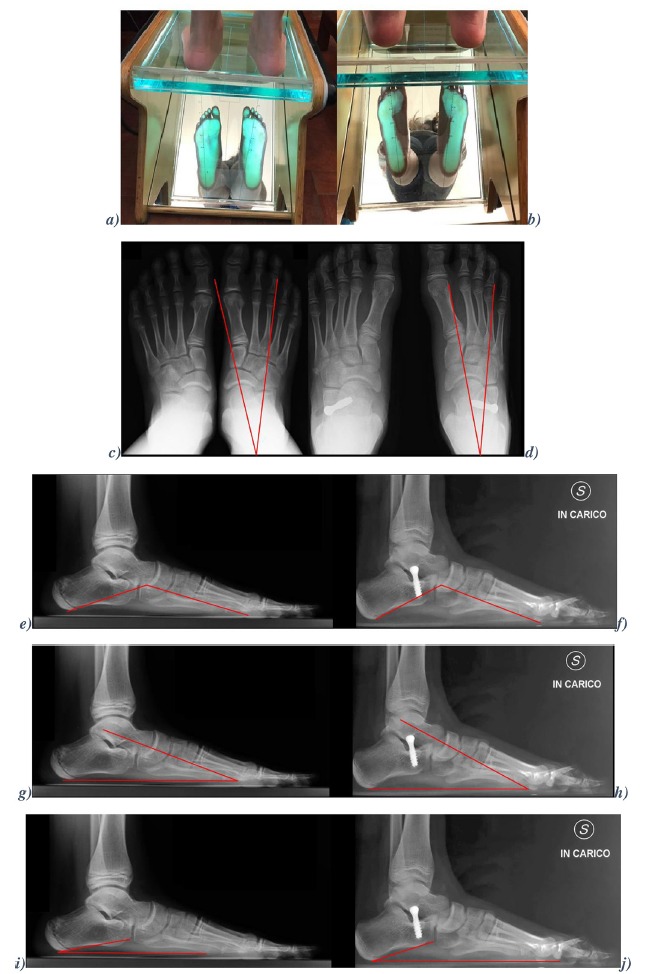
Clinical and radiological evaluation of an 11-year-old patient: footprint before surgery (a) and two years postoperatively (b); Kite’s angle (c,d), Costa-Bertani’s angle (e, f), talar declination (g,h) and calcaneal pitch (i,j) before surgery (left) and after two years (right).
Statistical analysis
Continuous data are presented as means and standard deviations, as appropriate. The analysis of variance test and Tukey–Kramer method were used to compare the clinical assessment and radiographic measurements preoperatively and at one and three years postoperatively. The Pearson Rho correlation coefficient was used to study the influence the weekly hours of sport practice on the increase of FADI Sport values. Finally, chi-squared tests were used to compare the types of sports practiced preoperatively and at one year and three years after surgery. The selected threshold for statistical significance was p < 0.05. All statistical analyses were performed using the 2016 GraphPad Software (GraphPad Inc, San Diego, California).
Results
Mean follow-up was 57.6 months (sd 16.8); 15 to 96). Heel valgus decreased from 130 feet (95.6%) preoperatively to 14 feet (10.3%) at final follow-up; normal footprint was recorded in 114 feet (83.8%). Following AOFAS (F2,201 = 287.51; p < 0.0001), Yoo et al (F2,201 = 2627.00; p < 0.0001), OxAFQ-C (F2,201 = 210.60; p < 0.0001), FADI (F2,201 = 372.62; p < 0.0001) and FADI Sport (F2,201= 189.32; p < 0.0001) scoring criteria, all the patients were recorded with an improvement and the maintenance of clinical outcomes (Table 1) at one and three years postoperatively (p < 0.0001). Significant statistical differences were found in the AOFAS pain category at one and three years after the surgery (Fig. 2) According to the AOFAS and Yoo et al criteria, at one-year postoperatively the heel alignment was corrected in 134 of 136 feet (98.6%) and improved in the rest of the cases (1.4%). Above 97% of the patients (132 feet) were satisfied with the treatment. All radiographic assessments; Kite’s angle (F2,201 = 203.02; p < 0.0001), Costa-Bertani’s angle (F2,201 = 210.41; p < 0.0001), talar declination (F2,201 = 213.30; p <0.0001) and calcaneal pitch (F2,201 = 368.79; p < 0.0001), were enhanced one year from the surgery (p < 0.0001) and the values were maintained at three years postoperatively (Table 2) (p < 0.0001).
Table 1.
Clinical assessment, following American Orthopedic Foot and Ankle Score (AOFAS), Yoo et al, Oxford Ankle Foot Questionnaire for Children (OxAF-C), The Foot & Ankle Disability Index (FADI) and FADI Sport scores. All presented as mean and sd (range). The p-values in the table are based on ANOVA test e Tukey test.
| AOFAS | Yoo et al | OxAFC | FADI | FADI Sport | |
|---|---|---|---|---|---|
| Preoperatively | 79.3 sd 5.7 (69.0 to 85.0) | 3.1 sd 1.0 (2 to 4) | 88.5 sd 4.5 (80.0 to 93.0) | 76.1 sd 7.5 (62.5 to 81.7) | 74.1 sd 10.4 (50 to 81.2) |
| p-value pre- versus postoperatively | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 |
| One-year postoperatively | 96.4 sd 4.5 (79 to 100) | 11.4 sd 0.7 (9 to 12) | 97.5 sd 2.5 (88.3 to 100) | 96.4 sd 4.4 (79.8 to 100) | 95.1 sd 5.7 (78.1 to 100) |
| p-value one year versus three years postoperatively | p > 0.05 | p > 0.05 | p > 0.05 | p > 0.05 | p > 0.05 |
| Three-years postoperatively | 97.3 sd 4.5 (90 to 100) | 11.7 sd 0.6 (9 to 12) | 98.6 sd 1.8 (93.3 to 100) | 98.3 sd 2.7 (94.2 to 100) | 95.9 sd 4.9 (78.1 to 100) |
| p-value pre- versus three years postoperatively | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 |
Fig. 2.
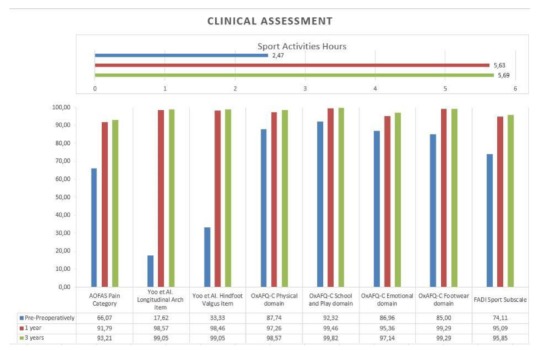
Clinical assessment following American Orthopedic Foot and Ankle Score (AOFAS) score, Yoo et al score (%), Oxford Ankle Foot Questionnaire for Children (OxAFQ-C) score (%), The Foot & Ankle Disability Index (FADI) and FADI Sport (%) subscale and hours of sport activities.
Table 2.
Radiological assessment, following Kite’s angle, Costa-Bertani’s Angle, talar declination and calcaneal inclination. All presented as mean and sd (range). The p-values in the table are based on ANOVA test e Tukey test.
| Kite’s angle (°) | Costa-Bertani’s angle (°) | Talar declination (°) | Calcaneal inclination (°) | |
|---|---|---|---|---|
| Preoperatively | 30.5 sd 1.3 (30 to 32) | 156.1 sd 4.2 (150 to 160) | 44.2 sd 6.3 (35 to 55) | 12.6 sd 2.3 (11 to 15) |
| p-value pre- versus postoperatively | p < 0.001 | p < 0.0001 | p < 0.0001 | p < 0.0001 |
| One-year postoperatively | 24.4 sd 2.1 (22 to 29) | 135.3 sd 8.1 (125 to 148) | 29.6 sd 3.7 (26 to 34) | 16.9 sd 1.7 (15 to 18) |
| p-value one year versus three years postoperatively | p > 0.05 | p > 0.05 | p > 0.05 | p > 0.05 |
| Three-years postoperatively | 24.6 sd 2.4 (22 to 30) | 135.8 sd 7.3 (125 to 149) | 30.6 sd 3.2 (26 to 34) | 16.3 sd 1.3 (15 to 18) |
| p-value pre- versus three years postoperatively | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 |
The mean level of sports activities per week before the surgery was 2.5 hours (sd 0.8; 1 to 3) and increased to 5.6 hours (sd 1.1; 1 to 7) at one year (p < 0.001) and to 5.7 hours (sd 1.2; 1 to 7) three years after the surgery (p < 0.001). No correlation between the weekly hours of sport practice and the increase of FADI Sport values were found one year after the surgery (r = 0.0092) and at the three-years follow-up (r = 0.0065). Following the Mitchell criteria, no significant statistical differences were found between the types of sports practiced (Table 3). In all, 37 patients started to practise sport activities regularly, increasing to 119.35% after the surgery (Table 3). Minor complications were encountered in 17 patients (12.5%); five patients (3.7%) had pain at surgical scar, four (2.9%) had local symptoms at the incision, three (1.2%) had screw loosening and four (2.9%) had superficial infections. In one case (0.73%) screw breakage was reported.
Table 3.
Types of sport following Mitchell criteria preoperatively and at one-year and three-years postoperatively. The p-values in the table are based on Chi-squared test.
| Type of sport | IA | IB | IC | IIA | IIB | IIC | IIIA | IIIB | IIIC | NO |
|---|---|---|---|---|---|---|---|---|---|---|
| Preoperatively | 0 | 6 | 11 | 0 | 0 | 10 | 0 | 2 | 2 | 37 |
| One-year postoperatively | 0 | 11 | 28 | 0 | 0 | 24 | 0 | 3 | 2 | 0 |
| Three-years postoperatively | 0 | 10 | 27 | 0 | 0 | 26 | 0 | 4 | 1 | 0 |
| p-value pre- versus one-year postoperatively | p > 0.05 | |||||||||
| p-value one-year versus three-years postoperatively | p > 0.05 | |||||||||
| p-value pre- versus three-years postoperatively | p > 0.05 |
NO, number of patients stopping sports due to flatfoot
In all, 11 patients (22 feet) removed the screw at skeletal maturity; four patients (eight feet) removed screw before the skeletal maturity for persistent pain, screw loosening or breakage, with presence of lysis around the screw in three feet.
In all, 65 patients (95.6%) were able to practise their sport, while three (4.4%) preferred to practise no-weight-bearing sports.
Discussion
Several authors have reported the outcomes after the return to sport activities in flexible flatfoot children having been treated with different surgical techniques,16,22 but, as far as we are aware, no previously published studies have investigated the outcomes of the calcaneo-stop procedure in the treatment of juvenile flatfoot in young athletes. The main inclusion criterion in the present study was sport practise for at least one hour three times a week. In this study, clinical outcomes and sports activities were assessed in children with symptomatic flatfoot before and after calcaneo-stop procedure; only patients with bilateral involvement were enrolled, since the sport performance and the functional outcomes may be influenced by both feet. Overall, we found that patients restored their preoperative level of sport activity within one year of surgery in terms of frequency and duration. All clinical and radiological assessments measured preoperatively and one and three years postoperatively improved (p < 0.0001). All patients were able to return to sports and recreational activities, and just in a few cases minimal pain and symptoms were reported. One year from surgery, we recorded a decrease of painful symptoms, an increase in the ability to perform daily activities and the emotional sphere-related score, and also, an improvement in the sports performance of greater than 21% (Fig. 2).
The mean sport activities time incresead from 2.5 hours to 5.6 hours one-year postoperatively and to 5.7 hours three years later: this could be explained by analyzing the questonnaries data. Decrease of pain and fatigue could increase the hours spent in sport practice. The orthosis removal after the surgery allows the patient to choose more efficient and comfortable sport footwear. A better body awareness, a removal of minor deformity functional impact, less flatfoot-related embarrassment and the possibility of socializing through sport could influence the calcaneo-stop treated patients’ emotional sphere improving through social interactions. An enhancement of mean sport practice time and of sport activities values were noted, but no correlations were demonstrated. We can deduce that a quantitative improvement of the sport practice following the calcaneo-stop procedure can be related to improvement in the quality of sport activities.
Arthroereisis procedures were applied to limit subtalar joint movement and improve the weight-bearing position of the foot, using a movement-blocking implant into the sinus tarsi.23 The calcaneo-stop procedure is a widely performed, studied, effectiveness-proved procedure,14,24 considered simple, reliable and minimally invasive for the treatment of paediatric flexible flatfoot, because it allows the alignment of the talus and calcaneus, restoring a proper foot arch.15 As several authors reported, SESA is indicated in children and adolescents with idiopathic flexible flatfeet presenting with any clinical disorder (pain, fatigue, inability to practice sports, falls, low limbs or back pain) refractory to non-surgical treatment.1,3,15,25 Operative correction of flexible flatfoot is performed with the aim of reducing symptoms rather than to correct the foot shape deformity.8 All mentioned symptoms could impact on the patients’ quality of life25 but our results showed, coherently with the literature, patient satisfaction and improvement of all examined clinical and radiographic parameters.
Rate of minor complications was 12.5%. Miller,26 at surgical removal of arthroereisis implant, revealed erosion of the cartilage on the anterior leading edge of the talus. In this series, eight cases of mobilization of screw reported lysis and erosion of talus at implant removal. Recent studies have reported complication rates of 3.5% to 11%, including inappropriate implantation in asymptomatic physiologic flatfeet, malpositioning of screw, overcorrection and implant aseptic loosening, breakage or degradation of biomaterials and biologic problems, adverse reactions, infection, persistent pain and osteonecrosis of the talus and peroneal spasm.27–29
Limitations of this study were: its retrospective nature, the lack of a control group, the mid-term follow-up, bias in clinical and radiographic evaluation and lack of objectively measurable parameters.
Conclusion
Adolescent patients who underwent the calcaneo-stop procedure report satisfactory clinical and radiographic outcomes. Advantages of this technique have been confirmed regarding symptom relief, short time for functional restoration and reduced invasiveness. Moreover, our results showed an early improvement and the long-term maintenance of sport activity levels, without limitation in the execution of preferred activities, confirming the effectiveness of the studied treatment.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical Statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained for all individual participants included in the study.
ICMJE Conflict of Interest Statement
Each author certifies that he/she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Yontar NS, Ogut T, Guven MF, et al. Surgical treatment results for flexible flatfoot in adolescents. Acta Orthop Traumatol Turc 2016;50:655–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pourghasem M, Kamali N, Farsi M, Soltanpour N. Prevalence of flatfoot among school students and its relationship with BMI. Acta Orthop Traumatol Turc 2016;50:554–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carr JB II, Yang S, Lather LA. Pediatric pes planus: a state-of-the-art review. Pediatrics 2016;137:e20151230. [DOI] [PubMed] [Google Scholar]
- 4.Ford SE, Scannell BP. Pediatric flatfoot: pearls and pitfalls. Foot Ankle Clin 2017;22:643–656. [DOI] [PubMed] [Google Scholar]
- 5.Dare DM, Dodwell ER. Pediatric flatfoot: cause, epidemiology, assessment, and treatment. Curr Opin Pediatr 2014;26:93–100. [DOI] [PubMed] [Google Scholar]
- 6.Costa FP, Costa G, Carvalho MS, et al. Long-term outcomes of the calcaneo-stop procedure in the treatment of flexible flatfoot in children: a retrospective study. Acta Med Port 2017;30:541–545. [DOI] [PubMed] [Google Scholar]
- 7.Kwon JY, Myerson MS. Management of the flexible flat foot in the child: a focus on the use of osteotomies for correction. Foot Ankle Clin 2010;15:309–322. [DOI] [PubMed] [Google Scholar]
- 8.Jerosch J, Schunck J, Abdel-Aziz H. The stop screw technique—a simple and reliable method in treating flexible flatfoot in children. Foot Ankle Surg 2009;15:174–178. [DOI] [PubMed] [Google Scholar]
- 9.Burutaran JM. El calcaneo-stop para el tratiamento del valgo de talon infantile. Chir Del Piede 1979;3:319–322. [Google Scholar]
- 10.Coledam DHC, Ferraiol PF. Engagement in physical education classes and health among young people: does sports practice matter? A cross-sectional study. Sao Paulo Med J 2017;135:548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Päivärinne V, Kautiainen H, Heinonen A, Kiviranta I. Relations between subdomains of physical activity, sedentary lifestyle and quality of life in young adult men. Scand J Med Sci Sports. 2018;28;1389–1396. [DOI] [PubMed] [Google Scholar]
- 12.Monda V, Valenzano A, Moscatelli F, et al. Primary motor cortex excitability in karate athletes: a transcranial magnetic stimulation study. Front Physiol 2017;8:695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bianco V, Berchicci M, Perri RL, Quinzi F, Di Russo F. Exercise-related cognitive effects on sensory-motor control in athletes and drummers compared to non-athletes and other musicians. Neuroscience 2017;360:39–47. [DOI] [PubMed] [Google Scholar]
- 14.De Pellegrin M, Moharamzadeh D, Strobl WM, et al. Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop 2014;8:479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pavone V, Costarella L, Testa G, et al. Calcaneo-stop procedure in the treatment of the juvenile symptomatic flatfoot. J Foot Ankle Surg 2013;52:444–447. [DOI] [PubMed] [Google Scholar]
- 16.Martinelli N, Bianchi A, Martinkevich P, et al. Return to sport activities after subtalar arthroereisis for correction of pediatric flexible flatfoot. J Pediatr Orthop B 2018;27:82–87. [DOI] [PubMed] [Google Scholar]
- 17.Leigheb M, Janicka P, Andorno S, et al. Italian translation, cultural adaptation and validation of the ‘American Orthopaedic Foot and Ankle Society’s (AOFAS) ankle-hindfoot scale’. Acta Biomed 2016;87:38–45. [PubMed] [Google Scholar]
- 18.Yoo WJ, Chung CY, Choi IH, Cho TJ, Kim DH. Calcaneal lengthening for the planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop 2005;25:781–785. [DOI] [PubMed] [Google Scholar]
- 19.Morris C, Doll HA, Wainwright A, Theologis T, Fitzpatrick R. The Oxford ankle foot questionnaire for children: scaling, reliability and validity. J Bone Joint Surg [Br] 2008;90-B:1451–1456. [DOI] [PubMed] [Google Scholar]
- 20.Martin RL, Burdett RG, Irrgang JJ. Development of the Foot and Ankle Disability Index (FADI). J Orthop Sports Phys Ther 1999;29:A32–A33. [Google Scholar]
- 21.Mitchell JH, Haskell W, Snell P, Van Camp SP. Task Force 8: classification of sports. J Am Coll Cardiol 2005;45:1364–1367. [DOI] [PubMed] [Google Scholar]
- 22.Usuelli FG, Di Silvestri CA, D’Ambrosi R, Maccario C, Tan EW. Return to sport activities after medial displacement calcaneal osteotomy and flexor digitorum longus transfer. Knee Surg Sports Traumatol Arthrosc 2018;26:892–896. [DOI] [PubMed] [Google Scholar]
- 23.Das SP, Das PB, Ganesh S, Sahu MC. Effectiveness of surgically treated symptomatic plano-valgus deformity by the calcaneo stop procedure according to radiological, functional and gait parameters. J Taibah Univ Sci 2017;12:102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giannini S, Cadossi M, Mazzotti A, et al. Bioabsorbable calcaneo-stop implant for the treatment of flexible flatfoot: a retrospective cohort study at a minimum follow-up of 4 Years. J Foot Ankle Surg 2017;56:776–782. [DOI] [PubMed] [Google Scholar]
- 25.Kothari A, Dixon PC, Stebbins J, Zavatsky AB, Theologis T. The relationship between quality of life and foot function in children with flexible flatfeet. Gait Posture 2015;41:786–790. [DOI] [PubMed] [Google Scholar]
- 26.Miller SJ. Collapsing pes valgo planus (flexible flatfoot) In: Levy LA, Hetherington VJ, Bakotic BW, eds. Principles and Practice of Podiatric Medicine. Brooklandville: Data Trace Publishing Company, 2006:1–35. [Google Scholar]
- 27.Gutiérrez PR, Lara MH. Giannini prosthesis for flatfoot. Foot Ankle Int 2005;26:918–926. [DOI] [PubMed] [Google Scholar]
- 28.Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int 2005;26:336–346. [DOI] [PubMed] [Google Scholar]
- 29.Saxena A, Nguyen A. Preliminary radiographic findings and sizing implications on patients undergoing bioabsorbable subtalar arthroereisis. J Foot Ankle Surg 2007;46:175–180. [DOI] [PubMed] [Google Scholar]


