Abstract
Purpose
We assessed the pattern of relapse as well as the correlation between the number of casts required for correction and Pirani and Dimeglio scores at presentation, and age at presentation. We hypothesized that the Ponseti method would be effective in treatment of relapsed clubfoot as well.
Methods
We evaluated 115 idiopathic clubfeet in 79 children presenting with relapse following treatment by the Ponseti method. The mean age was 33.8 months with mean follow-up of 24 months. All patients were assessed for various patterns of relapsed deformities. Quantification of deformities was done using the Pirani and Dimeglio scores. All relapsed feet were treated by a repeat Ponseti protocol.
Results
Non-compliance to a foot abduction brace was observed to be the main contributing factor in relapse, in 99 clubfeet (86%). Combination of three static deformities (equinus, varus and adduction) together was observed most commonly (38.3% feet). Overall, relapse of equinus deformity was noted most commonly followed by adduction. A painless plantigrade foot was obtained in all 115 feet with a mean of five casts. In all, 71 feet (61.7%) underwent percutaneous tenotomy. A total of 15 feet (13%) required tibialis anterior tendon transfer. Re-relapse rate in group 1 was 21% compared with 12.6% in group 2 and overall 16.5%.
Conclusion
We conclude that the Ponseti method is effective and the preferred initial treatment modality for relapsed clubfeet. Surgical intervention should be reserved for residual deformity only after a fair trial of Ponseti cast treatment. Regular follow-up and strict adherence to brace protocol may reduce future relapse rates. Further research is required to identify high-risk feet and develop individualized bracing protocol.
Level of evidence:
IV
Keywords: relapse, clubfoot, Ponseti, Dimeglio scoring, re-relapse
Introduction
A relapsed clubfoot is defined as recurrence of any component of deformity after a complete correction of clubfoot.1,2 Regardless of the mode of treatment, the clubfoot has an inherent and stubborn tendency to relapse.1 Although the Ponseti method has now been established as the treatment of choice for idiopathic clubfoot, even this method has not solved the problem of relapse completely. Relapse following the Ponseti method is very common and has been reported even upto rates of 56% by various authors.3–6 Not only the aetiology of relapsed clubfoot is elusive, the satisfactory treatment of such feet is still obscure. Various methods ranging from recasting to soft-tissue releases and bony osteotomies to external fixators have been described in isolation or combination. None of the methods dealing with relapses are universally acceptable and each has its own drawbacks. We have evaluated a series of 115 idiopathic clubfeet in 79 children presenting with relapse after Ponseti method.
The aim of our study was to assess the effectiveness of a repeat of the Ponseti method in treatment of clubfeet relapsed following the Ponseti method and its limitations. Further we assessed not only the pattern of relapse, but also any correlation between the number of casts required for correction and Pirani and Dimeglio scores at presentation, and age at presentation of relapse. We hypothesized that the Ponseti method would be effective in treatment of relapsed clubfoot as well.
Materials and methods
Institutional Ethical committee approval was obtained before the initiation of the study. A prospective study was carried out between July 2012 and June 2015 at our tertiary care institute. During this study period there were a total of 617 children with 817 idiopathic clubfeet registered at our clubfoot clinic. Relapse was defined as return to casting or surgery after documented correction of the initial deformity and initiation of bracing. A total of 125 idiopathic clubfeet in 85 children presenting with relapse were included in the study. Out of these, 25 children with 41 clubfeet were referred relapse cases from other institutes.
All the children included were treated previously by the Ponseti method. Syndromic clubfeet, neurogenic clubfeet and post-surgical relapses were excluded. Informed consent was taken for treatment and study from parents after explaining the nature of disease and mode of treatment.
A detailed history was taken from parents regarding the onset of deformity, history of treatment and general examination to rule out syndromic clubfoot. We relied on the parents’ report with regard to the use of a brace, as objective measures of brace compliance were not available.7, 8 We considered it as non-compliance (NC) when the foot abduction brace (FAB) was not used for at least ten hours a day, as suggested by Morcuende et al.9 Quantification of deformities was done using the Pirani and Dimeglio scores.10,11 All patients were assessed for pattern of relapse of static deformities i.e. equinus (E), varus (V), adduction (A), cavus (C) as well as for dynamic supination (D). We also observed the age at presentation, change in scores, number of casts required and amount of ankle dorsiflexion achieved.
All relapsed feet were treated by a repeat Ponseti casting. All patients underwent weekly cast application in our day-care clinic using Ponseti’s classical two hand technique. The initial stretching for two to three minutes was done before every cast application as the soft-tissue in elder children and relapsed cases was less yielding. All of the casts were applied under the supervision of the senior author (AM). Percutaneous tenotomy (PCT) of the tendo-Achilles, if required, was done mostly under local anaesthesia. Post-tenotomy casts were removed at three weeks. Tibialis anterior tendon transfer (TATT) was done in children older than three years with D where the third cuneiform showed ossification. TATT was done under general anaesthesia by the modified Garceau’s procedure, as described by Ponseti.1,12 To maintain the achieved correction, a Steenbeek FAB was given to all, excepting patients who underwent TATT. In non-ambulatory children (who had not started walking at the time of relapse), FAB was applied for 23 hours a day for the first three months and sleep and nap time (12 to 14 hours/day) until the age of five years was recommended. In ambulatory patients below five years, FAB was given only for night and nap time until the age of five years. For children older than five years at presentation, the braces were advised for night time for only about three to six months. No special footwear was given for day time.13 Patients were followed-up every six weeks for the first six months and then every three months.
The quantitative variables were expressed as mean and sd and compared between pre- and post-treatment follow-up using the paired t-test. Also, the relation between the Pirani and Dimeglio score and age at presentation with number of casts required was evaluated using Pearson’s correlation coefficient. Statistical analysis was performed using SPSS version 21.0 software (IBM; Armonk, New York) and a p-value < 0.05 was considered statistically significant.
Results
A total of 125 idiopathic clubfeet (85 children) that had relapsed after Ponseti management were included in the study. Six children (ten feet) were lost to follow-up. A total of 115 idiopathic clubfeet (79 children) with a minimum of 12 months follow-up were available for final assessment. The mean age at presentation was 33.8 months (7 to 100). The male to female ratio was 3.4:1. At relapse, 43 children had unilateral involvement (54.4%). In unilateral cases, the right foot was involved twice as many times as the left foot. The mean follow-up was 24 months (12 to 36). We divided children into two categories: age group (group 1 – age less than two years and group 2– age two or more years). and deformity group (group A – less than three deformities and group B – three or more deformities) (Table 1).
Table 1.
Cohort of our study
| Study cohort | ||
|---|---|---|
| Total children | 79 | |
| Boys | 61 | |
| Girls | 18 | |
| Total feet | 115 | |
| Age | < 2 yrs (group 1) | 52 (45.2%) (feet) |
| ≥ 2 yrs (group 2) | 63 (54.8%) | |
| Bilateral feet | 36 children | |
| Unilateral | Right | 31 |
| Left | 12 | |
| Initial Dimeglio (at relapse) | I (Mild) | 2 (feet) |
| II (Moderate) | 89 | |
| III (Severe) | 24 | |
| IV (Very severe) | 0 | |
| FAB | N | 16 (feet) |
| NC | 99 | |
| Previous treatment method | Ponseti in all (100%) | |
| Previous surgery | None | 7 (feet) |
| PCT | 102 | |
| PCT+TATT* | 6 |
six feet had primary relapse following previous TATT. On checking records, we noted all of them underwent this procedure at an outside institute between two and three years of age
FAB, foot abduction brace; N, FAB compliant feet; NC, non-compliance; PCT, percutaneous tenotomy; TATT, tibialis anterior tendon transfer
NC to FAB was observed in 99 clubfeet (86%). We noticed that the relapse of deformities occurred either singularly or more commonly in various combinations (Table 2). The most common relapse pattern observed was a combination of three deformities (E, A and V in 38% feet). In group 2, 78% of feet had three or more deformities whereas group 1 had only 40% of feet in this category (p <0.001).
Table 2.
Various combinations of deformities observed with number of feet involved
| Deformity | Feet (n) | Total (n) |
|---|---|---|
| Patients with relapse of only one deformity: | ||
| E | 17 | 20 |
| A | 2 | |
| D | 1 | |
| Patients with relapse of combination of two deformities: | ||
| EA | 8 | 17 |
| EV | 6 | |
| EC | 2 | |
| ED | 1 | |
| Patients with relapse of combination of three deformities: | ||
| EAV | 40 | 51 |
| EAD | 9 | |
| VCD | 2 | |
| Patients with relapse of combination of more than three deformities: | ||
| EVAC | 14 | 19 |
| EVAD | 4 | |
| EVACD | 1 | |
| Patients with relapse as loss of correction achieved rather than frank deformity (Pirani score ≥ 1/difficulty in squatting): | ||
| n/a | n/a | 8 |
E, equinus; V, varus; A, adduction; C, cavus; D, dynamic supination
However, overall, the relapse of E deformity was noted most in 102 clubfeet (89%). Deformity A was noted as the second most common deformity, involving 78 (67.8%) clubfeet. V and C involved 67 (58.3%) and 19 (16.5%) clubfeet respectively but were never observed as a singular deformity.
At presentation, D was noted in 18 (15.6%) clubfeet. Among these, ten feet required TATT.
Five more feet required TATT in which D was not appreciable at the time of presentation due to combination of severe deformities. But when feet became plantigrade after cast treatment, D became evident and required TATT. So, in our study of 115 clubfeet, 15 feet in total underwent TATT. Post treatment, D was corrected in all patients.
The mean values of Pirani and Dimeglio scores, E and casts applied in relation to deformities and age are shown in Tables 3, 4, 5. We noted a positive correlation between age at presentation with relapse and initial Dimeglio score (p = 0.012), E (p = 0.087) and casts applied (p = 0.000); but a negative correlation with initial Pirani score (p = 0.224).
Table 3.
Mean values of Pirani and Dimeglio scores, equinus (pre and post) and casts applied
| 95% confidence interval for mean | ||||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | sd | Standard error | Lower bound | Upper bound | Minimum | Maximum | |
| Initial Pirani | 115 | 2.409 | 0.8825 | 0.0823 | 2.246 | 2.572 | 1.0 | 4.5 |
| Final Pirani | 115 | .02 | 0.131 | 0.012 | 0.00 | 0.04 | 0 | 1 |
| Change in Pirani scores | 115 | 2.3913 | 0.90025 | 0.08395 | 2.2250 | 2.5576 | 1.00 | 4.50 |
| Initial Dimeglio | 115 | 7.92 | 2.086 | 0.195 | 7.54 | 8.31 | 4 | 14 |
| Final Dimeglio | 115 | 1.89 | 1.310 | 0.122 | 1.65 | 2.13 | 0 | 5 |
| Change in Dimeglio scores | 115 | 6.0348 | 1.99090 | 0.18565 | 5.6670 | 6.4026 | 1.00 | 11.00 |
| Equinus (pre) | 115 | 9.62 | 9.855 | 0.919 | 7.80 | 11.44 | −5 | 48 |
| Equinus (post) (DF achieved) | 115 | 17.86 | 5.655 | 0.527 | 16.82 | 18.91 | 5 | 24 |
| Change in equinus | 115 | 8.2435 | 11.85852 | 1.10581 | 6.0529 | 10.4341 | −43.00 | 27.00 |
| Casts applied | 115 | 5.0261 | 2.12941 | 0.19857 | 4.6327 | 5.4195 | 1.00 | 12.00 |
| Follow-up (mths) | 79 | 23.82 | 6.261 | 0.704 | 22.42 | 25.23 | 12 | 36 |
DF, dorsiflexion
Table 4.
Mean values of Pirani and Dimeglio scores, equinus (pre and post) and casts applied in age group
| Age | n | Mean | sd | p-value | |
|---|---|---|---|---|---|
| Initial Pirani | Group 1 (age < 2 yrs) | 52 | 2.519 | 0.8854 | 0.224 |
| Group 2 (age > 2 yrs) | 63 | 2.317 | 0.8767 | ||
| Final Pirani | Group 1 (age < 2 yrs) | 52 | 0.00 | 0.000 | 0.198 |
| Group 2 (age > 2 yrs) | 63 | 0.03 | 0.177 | ||
| Change in Pirani scores | Group 1 (age < 2 yrs) | 52 | 2.5192 | 0.88540 | 0.167 |
| Group 2 (age > 2 yrs) | 63 | 2.2857 | 0.90569 | ||
| Initial Dimeglio | Group 1 (age < 2 yrs) | 52 | 7.38 | 1.952 | 0.012 |
| Group 2 (age > 2 yrs) | 63 | 8.37 | 2.105 | ||
| Final Dimeglio | Group 1 (age < 2 yrs) | 52 | 1.06 | 1.110 | 0.000 |
| Group 2 (age > 2 yrs) | 63 | 2.57 | 1.043 | ||
| Change in Dimeglio scores | Group 1 (age < 2 yrs) | 52 | 6.3269 | 1.71179 | 0.154 |
| Group 2 (age > 2 yrs) | 63 | 5.7937 | 2.17877 | ||
| Equinus (pre) | Group 1 (age < 2 yrs) | 52 | 7.885 | 8.9851 | 0.087 |
| Group 2 (age > 2 yrs) | 63 | 11.048 | 10.3712 | ||
| Equinus (post) | Group 1 (age < 2 yrs) | 52 | −20.481 | 2.8731 | 0.000 |
| Group 2 (age > 2 yrs) | 63 | −15.698 | 6.4424 | ||
| Change in equinus (pre-post) | Group 1 (age < 2 yrs) | 52 | 28.3654 | 9.48069 | 0.428 |
| Group 2 (age > 2 yrs) | 63 | 26.7460 | 11.87566 | ||
| Casts applied | Group 1 (age < 2 yrs) | 52 | 4.00 | 1.469 | 0.000 |
| Group 2 (age > 2 yrs) | 63 | 5.87 | 2.225 |
Table 5.
Mean values of Pirani and Dimeglio scores, equinus (pre and post) and casts applied in deformity group
| Deformity | n | Mean | sd | p-value | |
|---|---|---|---|---|---|
| Age (months) | Group A* | 33 | 23.24 | 15.678 | 0.000 |
| Group B* | 46 | 41.35 | 22.968 | ||
| Initial Pirani | Group A* | 45 | 1.800 | 0.6342 | 0.000 |
| Group B* | 70 | 2.800 | 0.7958 | ||
| Final Pirani | Group A* | 45 | 0.00 | 0.000 | 0.257 |
| Group B* | 70 | 0.03 | 0.168 | ||
| Change in Pirani scores | Group A* | 45 | 1.8000 | 0.63425 | 0.000 |
| Group B* | 70 | 2.7714 | 0.84135 | ||
| Initial Dimeglio | Group A* | 45 | 6.00 | 1.128 | 0.000 |
| Group B* | 70 | 9.16 | 1.557 | ||
| Final Dimeglio | Group A* | 45 | 1.22 | 1.363 | 0.000 |
| Group B* | 70 | 2.31 | 1.084 | ||
| Change in Dimeglio scores | Group A* | 45 | 4.7778 | 1.75666 | 0.000 |
| Group B* | 70 | 6.8429 | 1.69941 | ||
| Equinus (pre) | Group A* | 45 | 5.222 | 5.2175 | 0.000 |
| Group B* | 70 | 12.443 | 11.0632 | ||
| Equinus (post) | Group A* | 45 | −18.000 | 5.4062 | 0.834 |
| Group B* | 70 | −17.771 | 5.8463 | ||
| Change in Equinus (pre-post) | Group A* | 45 | 23.2222 | 7.12514 | 0.001 |
| Group B* | 70 | 30.2143 | 11.93569 | ||
| Casts applied | Group A* | 45 | 4.04 | 1.461 | 0.000 |
| Group B* | 70 | 5.66 | 2.258 |
Group A (less than three deformities); group B (three or more deformities)
On analyzing groups 1 and 2, we noted a lower mean initial Pirani score in group 2 despite higher Dimeglio score and E. However, p-values were not significant. The final Pirani score was also not significant between these two groups, but a p-value which was significant in the final Dimeglio score and DF was achieved. Also, changes in scores were not significant between groups 1 and 2. A statistically significant highest mean change in scores and E was noted in subgroup 1B (age less than two years and with three or more deformities).
The mean number of casts applied was 5.03 (1 to 12). Group 1 patients required fewer casts to regain correction (four versus 5.9, p < 0.05). Casts applied had statistically significant positive correlation with initial Dimeglio score, E and age; but not with initial Pirani score. The mean time taken for treatment was eight weeks.
The pre-treatment mean E was 9.6° (−5° to 48°). The mean dorsiflexion achieved was 17.8° (5° to 24°). The mean DF achieved in group 1 was 20° compared with 15° in group 2 with a p-value < 0.05.
In 44 feet (38.3%), complete correction was achieved with casting only. 75% of these feet (33) were in group 1. In the remaining 71 feet (61.7%) PCT was also required, whereas TATT was added to PCT in 15 feet (13%). Three feet belonging to group 2 required percutaneous plantar fasciotomy for ‘C’ correction. This was done under general anaesthesia at the time of PCT.
Thus, all 115 feet (100%) were corrected by the Ponseti treatment protocol. None of the feet required capsular release or osseous procedures. Figures 1 and 2 show some of our results.
Fig. 1.

(a) Deformity at presentation - from front; (b) cavus at presentation; (c) deformity at presentation - both feet.
Fig. 2.
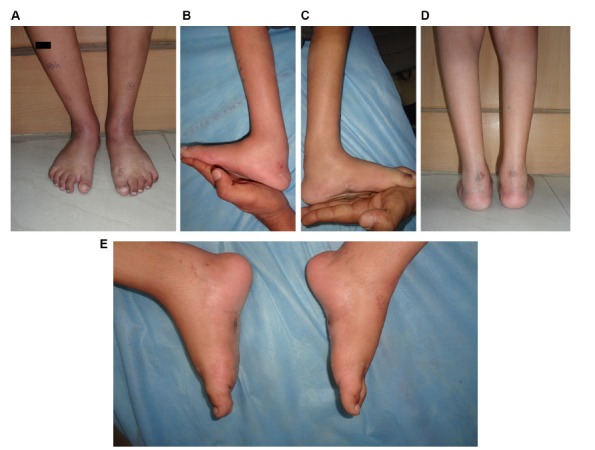
(a) Correction achieved - from front; (b) dorsiflexion achieved - right foot; (c) dorsiflexion achieved - left foot; (d) correction of heel varus; (e) correction of cavus.
In all, 19 feet (16.5%) relapsed again. Eleven of these feet were in group 1. NC to FAB was found in all. E was the only deformity to re-relapse in all 19 feet. These re-relapse cases were managed again in a similar way with the Ponseti method and are currently under follow-up.
Three feet developed plaster sores over the talar head region which was managed by sterile dressing and gentle casting with extra padding. One foot developed wound infection on the sole at the button site after TATT. This was managed by antiseptic dressing and button removal at three weeks post-surgery.
Discussion
With a large number of clubfoot cases, there is an obvious load of relapse cases, especially in developing countries. Long-term studies of surgical procedures have shown poor results with complications like painful feet, arthritis, stiffness of the ankle and subtalar joint and residual deformity.14–16 Relapses after soft-tissue releases and osteotomies are further difficult to treat as they result in rigid foot due to extensive scarring after surgery.17 The Ponseti method is essentially a conservative method, which has shown more than 90% successful long-term results in idiopathic clubfoot.1,18–20 It seemed interesting and judicious to evaluate the role and efficacy of the Ponseti method in the management of relapsed clubfoot (previous Ponseti treatment) which formed the basis of our study. Also, this is one of the preliminary attempts to study pattern of relapse in clubfeet treated by the Ponseti method.
In the literature, there is no consensus on the definition of ‘non-compliance’ to FAB.7–9 But most authors agree on the fact that NC to FAB is the single most significant risk factor for relapse.1,7–9,21,22 Reported NC ranges from 0% to 51%.7,20–22
NC to FAB was observed in 99 clubfeet (86%). Among relapse feet with NC to FAB, 66% had more than three deformities. Thus, NC to FAB was not only associated with increased chances of relapse, but also with increased severity of deformity (p < 0.05). Mahan et al23 reported that relapse in patients aged less than two years was more related to NC than relapse in patients aged two or more years. In our study, NC was similar in both groups 1 and 2.
Bhaskar and Patni24 suggested a classification for relapse. However, they did not describe various combinations of deformities that could relapse. They used various surgical procedures including abductor hallucis release, posterior release and osteotomies (Table 6).
Table 6.
Comparison with various published studies
| Refaie al27 | Prem et al26 | Bhaskar and Patni24 | Our study | ||
|---|---|---|---|---|---|
| Study group | Idiopathic (Ponseti + post-surgical relapse) | Idiopathic (post-surgical + post-Ilizarov relapse) | Idiopathic, post-Ponseti relapse | Idiopathic, post-Ponseti relapse | |
| Type of study | Retrospective case series | Retrospective | Prospective | Prospective | |
| Number of feet | 19 (9 post-Ponseti) | 19 | 164 | 115 | |
| Mean age (range) | 8 yrs (2 to 6) | 5 yrs (2 to 8) | 48 mths (24 to 72) | 33.8 mths (7 to 100) | |
| Mean Pirani score | Pre | NA | NA | NA | 2.4 |
| Post | NA | NA | NA | .02 | |
| Mean Dimeglio score | Pre | NA | NA (all at least grade III Dimeglio) | NA | 7.92 |
| Post | NA | NA | NA | 1.89 | |
| Mean casts applied (range) | Cast for consolidation for 4 to 6 wks | Consolidation cast for 6 wks | NA | 5.03 (1 to 12) | |
| NC to FAB in relapse cases | NA | NA | 89% | 86% | |
| Average time taken for treatment | 11 wks | 22 wks | NA | 8 wks | |
| Average dorsiflexion | NA | NA (only 1 foot had dorsiflexion > 10°) | NA | 17.9° | |
| Re-relapses | 15.8% | 5.3% | NA | 16.5% | |
| Soft-tissue procedures |
|
None |
|
|
|
| Osseous procedures |
|
None |
|
None | |
| Complications | 36 minor complications including 4 flat topped-talus |
|
NA |
|
|
| Braces/special shoes |
|
|
|
FAB only | |
| Mean follow-up(range) | 4.5 yrs (2 to 6) | 6.9 yrs (5 to 10) | 24 mths (12 to 28) | 24 mths (12 to 36) |
NA, not available; NC, non-compliance; FAB, foot abduction brace; PCT, percutaneous tenotomy; TATT, tibialis anterior tendon transfer; FAO, foot abducation orthosis; AFO, ankle foot orthosis; CTEV, congenital telipes equino varus
We observed relapse of E most commonly (89% feet), and this was more severe in feet with a combination of deformities (p < 0.05). This may probably be due to the relapse of E first in most cases, with other deformities added later. Eight feet from group 1 had no frank deformity but had a Pirani score ≥ 1 and presented with difficulty in squatting or loss of previous dorsiflexion to neutral. We included these in our study as early relapse cases as we believe this would progress to a fixed E (grade Ia of Bhaskar and Patni24). Also, a relapse of V or C deformity alone was never noticed. Thus, loss of dorsiflexion can be seen as the earliest sign of relapse.
We included D as a relapse because we believe that it signifies muscle imbalance in the foot and may progress to severe static deformities, if not addressed timely.
Contrary to earlier reports1,25 we found that the relapse of forefoot A was as common as relapse of hind foot deformities. Bhaskar and Patni24 also described similar findings. They noted that dynamic forefoot A or in-toeing was the most common relapse pattern after treatment by the Ponseti technique.
We described various patterns and combinations of deformities that have rarely been described in literature. We observed 14 possible combinations of deformities. However, distribution of feet was skewed with one combination (EAV) contributing to more than one-third of feet with relapse. A larger study should be able to describe deformities/combination patterns which are more prone to recurrences and are difficult to treat. This may help us in guiding/modifying treatment and bracing protocols.
We acknowledge that in any study design it is difficult to pinpoint when a relapse first began to happen. It is a very likely possibility that some children had relapse before two years of age but reported it after two years of age. It may suggest some cases of relapse with multiple deformities presented very late after relapse. The upper age limit for bracing was set somewhat arbitrarily. After observing relapses even after the age of six years, bracing protocol needs a re-evaluation. Further research is required to develop an individualized bracing schedule at least in some selected cases.
A review of the literature revealed relapses managed by Ilizarov with or without soft-tissue/bony procedures. Results from Prem et al26 and Refai et al27 are summarized in a comparison in Table 6.
Utukuri et al28 studied patient-based outcomes after Ilizarov surgery in 26 resistant clubfeet (all had previously undergone surgery). Mean age was nine years with a mean follow-up of 47 months. The total time taken was around 23 weeks. They noted a 65% recurrence rate. They described better functional results in spite of a poor surgical outcome. All Ilizarov procedures require at least two general anaesthesia procedures in each case (adding further to cost of frame).
A painless plantigrade foot was obtained in all 115 feet with casting and/or minimal surgery as per Ponseti protocol with a mean of 5.02 casts. Children in group 1 achieved statistically significant higher DF with fewer number of casts (p < 0.05). Children and parents were satisfied with the final results as they were able to wear normal footwear and carry out most of the functions. Our results are better than studies with surgical and fixator treatment for post-Ponseti relapses in terms of very few complications, less treatment time taken, no capsular release or osseous procedures needed and supple feet with better final scores and higher DF (Table 6).
We recommend use of the Dimeglio score, as relapse cases may score less on Pirani despite stubborn deformity. Many of these children lack deep posterior and medial crease. Initial Pirani score had a negative correlation with age at relapse. Also, improvement in the 20-point Dimeglio score is a better indicator for correction achieved between consecutive casts, as the Pirani score may remain unchanged.
Younger age at TATT has been found to be a risk factor for recurrence.6,29 We noted that six feet presenting with primary relapse had a history of TATT. On checking records, all of them underwent this procedure at an outside institute between two to three years of age. We did not perform TATT in children under the age of three years. In this study, none of our patients who underwent TATT at our institute re-relapsed until last follow-up.
The re-relapse rate in group 1 was 21% compared with 12.6% in group 2 and overall 16.5%. Mahan et al23 also reported higher a recurrence rate at age less than two years. A higher re-relapse rate should be anticipated in a longer follow-up but these re-relapses after Ponseti treatment are less stiff and can be managed again with the Ponseti protocol. Also, prophylactic TATT can be considered in children above three years of age. However, further study would be required to validate its role.
There are a few limitations to this study. A larger study group and longer follow-up from multiple centres is desirable to validate results of repeat Ponseti method in relapse. Also, we recorded recall-based NC to FAB. A total of 25 children with 41 clubfeet included in this study underwent first treatment elsewhere. It is often difficult to distinguish incomplete correction from true relapses. Final outcome assessment based on functional scoring was not used in this study.
Despite these shortcomings, our study describes rarely described patterns and combinations of deformities that relapse following use of the Ponseti technique and achieved correction by repeat Ponseti.
We conclude that the Ponseti method should be the preferred initial treatment modality even for relapsed idiopathic clubfeet. Surgical intervention should be reserved for residual deformity only after the fair trial of Ponseti treatment. It would be a good cost-effective method especially in developing countries with a high occurrence of clubfoot and scarce resources. Strict adherence to brace protocol and good communication between doctor and parents may reduce future incidences of relapse. Further research is required to identify high risk feet and develop individualized bracing protocols.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
OA Licence Text
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Ethical Statement
Ethical approval: Institutional Ethical Committee approval was obtained prior to the initiation of the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ICMJE Conflict of Interest Statement
The authors declare no potential conflicts of interest.
References
- 1.Ponseti IV. Congenital clubfoot: fundamentals of treatment. 1st ed. Oxford: Oxford University Press, 1996:61–97. [Google Scholar]
- 2.Goriainov V, Judd J, Uglow M. Does the Pirani score predict relapse in clubfoot? J Child Orthop 2010;4:439–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owen RM, Kembhavi G. A critical review of interventions for clubfoot in low and middle-income countries: effectiveness and contextual influences. J Pediatr Orthop B 2012;21:59–67. [DOI] [PubMed] [Google Scholar]
- 4.Ponseti IV. Relapsing clubfoot: causes, prevention, and treatment. Iowa Orthop J 2002;22:55–56. [PMC free article] [PubMed] [Google Scholar]
- 5.Chu A, Lehman WB. Persistent clubfoot deformity following treatment by the Ponseti method. J Pediatr Orthop B 2012;21:40–46. [DOI] [PubMed] [Google Scholar]
- 6.Masrouha KZ, Morcuende JA. Relapse after tibialis anterior tendon transfer in idiopathic clubfoot treated by the Ponseti method. J Pediatr Orthop 2012;32:81–84. [DOI] [PubMed] [Google Scholar]
- 7.Abdelgawad AA, Lehman WB, van Bosse HJ, Scher DM, Sala DA. Treatment of idiopathic clubfoot using the Ponseti method: minimum 2-year follow-up. J Pediatr Orthop B 2007;16:98–105. [DOI] [PubMed] [Google Scholar]
- 8.Avilucea FR, Szalay EA, Bosch PP, Sweet KR, Schwend RM. Effect of cultural factors on outcome of Ponseti treatment of clubfeet in rural America. J Bone Joint Surg[Am] 2009;91-A:530–540. [DOI] [PubMed] [Google Scholar]
- 9.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics 2004;113:376–380. [DOI] [PubMed] [Google Scholar]
- 10.Pirani S, Outerbridge H, Moran M, Sawatsky BJ. A method of evaluating the virgin clubfoot with substantial interobserver reliability. Vol 71 Miami, Florida: POSNA, 1995:99. [Google Scholar]
- 11.Diméglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B 1995;4:129–136. [DOI] [PubMed] [Google Scholar]
- 12.Garceau GJ. Anterior tibial tendon transposition in recurrent congenital club-foot. J Bone Joint Surg [Am] 1940;22-A:932–936. [PubMed] [Google Scholar]
- 13.Mehtani A, Prakash J, Vijay V, Kumar N, Sinha A. Modified Ponseti technique for management of neglected Clubfeet. J Pediatr Orthop B 2018;27: 61–66. [DOI] [PubMed] [Google Scholar]
- 14.Aronson J, Puskarich CL. Deformity and disability from treated clubfoot. J Pediatr Orthop 1990;10:109–119. [PubMed] [Google Scholar]
- 15.Dobbs MB, Nunley R, Schoenecker PL. Long-term follow-up of patients with clubfeet treated with extensive soft-tissue release. J Bone Joint Surg [Am] 2006;88-A:986–996. [DOI] [PubMed] [Google Scholar]
- 16.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg [Am] 2003;85-A:1286–1294. [DOI] [PubMed] [Google Scholar]
- 17.van Bosse HJ. Treatment of the neglected and relapsed clubfoot. Clin Podiatr Med Surg 2013;30:513–530. [DOI] [PubMed] [Google Scholar]
- 18.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg [Am] 1980;62-A:23–31. [PubMed] [Google Scholar]
- 19.Ponseti IV, Smoley EN. Congenital club foot: the results of treatment. J Bone Joint Surg [Am] 1963;45-A:261–344. [Google Scholar]
- 20.Bor N, Coplan JA,. Herzenberg JE.Ponseti treatment for idiopathic clubfoot: minimum 5-year followup. Clin Orthop Relat Res 2009;467:1263–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dobbs MB, Rudzki JR, Purcell DB, et al. . Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg [Am] 2004;86-A:22–27. [DOI] [PubMed] [Google Scholar]
- 22.Zhao D, Liu J, Zhao L, Wu Z. Relapse of clubfoot after treatment with the Ponseti method and the function of the foot abduction orthosis. Clin Orthop Surg 2014;6:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahan ST, Spencer SA, May CJ, Prete VI, Kasser JR. Clubfoot relapse: does presentation differ based on age at initial relapse? J Child Orthop 2017;11:367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhaskar A, Patni P. Classification of relapse pattern in clubfoot treated with Ponseti technique. Indian J Orthop 2013;47:370–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dietz FR. Treatment of a recurrent clubfoot deformity after initial correction with the Ponseti technique. Instr Course Lect 2006;55:625–629. [PubMed] [Google Scholar]
- 26.Prem H, Zenios M, Farrell R, Day JB. Soft tissue Ilizarov correction of congenital talipes equinovarus—5 to 10 years postsurgery. J Pediatr Orthop 2007;27: 220–224. [DOI] [PubMed] [Google Scholar]
- 27.Refai MA, Song S-H, Song H-R. Does short-term application of an Ilizarov frame with transfixion pins correct relapsed clubfoot in children? Clin Orthop Relat Res 2012;470:1992–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Utukuri MM, Ramachandran M, Hartley J, Hill RA. Patient-based outcomes after Ilizarov surgery in resistant clubfeet. J Pediatr Orthop B 2006;15:278–284. [DOI] [PubMed] [Google Scholar]
- 29.Luckett MR, Hosseinzadeh P, Ashley PA, et al. . Factors predictive of second recurrence in clubfeet treated by ponseti casting. J Pediatr Orthop 2015;35:303–306. [DOI] [PubMed] [Google Scholar]


