Abstract
Background:
The relationship between injury risk (IR) in age groups and periods around peak height velocity (PHV) remains unclear. PHV is defined as the moment of the largest increase in body height.
Purpose:
To investigate injury risk and injury burden as functions of growth velocity (periods around PHV) and chronological age groupings (under 12 years [U12] to U19) in talented youth male soccer players.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A total of 170 players from the youth academy of a Dutch soccer club (highest professional league: Eredivisie) were observed for 1 to 3 seasons. Injuries, exposure, PHV age, and chronological age were registered. The injury incidence density (IID) and injury burden per 1000 hours of soccer participation, with 95% CIs, were calculated for 5 PHV periods and 7 age groups. These were compared with the overall cohort results using incidence ratios (IRs) and burden ratios (BRs) with 95% CIs.
Results:
The mean age at PHV was 14.4 ± 0.65 years (range, 12.8-16.5 years). The mean IID for the total cohort was 8.34 injuries per 1000 hours (95% CI, 7.71-9.02). Compared with the overall mean, a significantly higher IID was found for PHV period 4+5 (IR, 1.31 [95% CI, 1.00-1.71]; P = .049) and for the U15 group (IR, 1.49 [95% CI, 1.24-1.79]; P < .001). The overall injury burden was 58.37 injury days per 1000 hours (95% CI, 56.66-60.13). In PHV period 4+5, the injury burden was significantly higher (BR, 1.53 [95% CI, 1.39-1.68]; P < .001) when compared with the overall mean. Also, compared with the overall mean, the injury burden was higher in the U16 (BR, 1.48 [95% CI, 1.39-1.58]; P < .001), U15 (BR, 1.28 [95% CI, 1.19-1.38]; P < .001), and U17 groups (BR, 1.21 [95% CI, 1.13-1.31]; P < .001).
Conclusion:
Talented young soccer players were more prone to injuries during the 6 months after PHV (31% above overall mean) as well as in the U15 group (49% above overall mean). Based on the higher injury burden in the U16 (48%), U15 (28%), and U17 (21%) groups, we suggest that research on injury risk factors and preventive measures should primarily target these age groups. Additional interventions based on PHV may be of limited value from a screening perspective. Further research is needed on the interaction between age groups and PHV periods.
Keywords: peak height velocity, age group, chronological age, biological age, injury incidence density, injury burden
Young soccer players in most organized leagues are classified per team based on their chronological age, usually with a threshold set at January 1. For example, if a player was 16 years old on January 1, 2018, he or she is considered part of the under 16 (U16) age group for the 2018-2019 season. Peak height velocity (PHV) defines the moment of the largest increase in body height.12,15 As the velocity of growth differs between players, biological differences are likely to occur within teams. The differences in height and weight can imply differences in physical capacity.
Periods around PHV have been associated with an increased injury risk.13,23,24 A decrease in flexibility and bone density during the growth spurt may result in increased vulnerability of the skeletal system.2–4,10,22 Boys between 12 and 16 years of age can grow up to 12 cm per year.15 Adolescent “clumsiness” due to the quick increase in the length of arms and legs relative to the trunk may result in physical impairments and lower performance during this period.3 Furthermore, increased training loads and match congestion in youth soccer academies are associated with an increased injury incidence in this group of athletes.9 A recent review suggested that both an increased load and height gain augmented the risk of sustaining an injury.16
The injury incidence density (IID) in academy soccer players (2.0-19.4 injuries per 1000 hours of soccer participation) is higher than that in male professional players (2.5-9.4).16 In both groups, the IID in training (1.4-5.8 and 3.7-11.1, respectively) is lower than in matches (8.7-65.9 and 9.5-48.7, respectively).16 Recent studies in English soccer academies (age groups of U11-U18) and Qatari youth players (U9-U18) have reported 1.3 and 1.5 injuries per player per season, respectively.13 Time loss per injury was significantly higher in the U14 and U15 groups when compared with the U11 to U13 groups and the U16 group,13 whereas the number of injuries was significantly higher in the U15 group (2.7 per player per season) compared with the U13 (1.3 per player per season) and U14 groups (1.7 per player per season).13 Older academy players (U17-U19) were at a higher risk to sustain a severe injury when compared with younger players (U9-U16).20 However, these studies13,16,20 did not report on exposure and thus lack an estimate of the injury risk.
In Dutch academy soccer players, a higher IID of acute injuries was found in the period from 6 months before PHV to 6 months after PHV when compared with the year before this period.23 Another study found more overuse injuries present in the period from 1 year before PHV to 1 year after PHV and more time loss due to acute injuries from 1 year after PHV.23
The little information available, derived from different cohorts, age groups, and study designs, as well as the contrary outcomes, warrants new studies on this topic.13,23,24 Our aim in the current study was to investigate the associations between the injury risk and injury burden with both height increase (periods around PHV) and chronological age groupings (U12-U19) in talented youth male soccer players.
Methods
In this study, we observed 170 academy soccer players of a professional Dutch Premier League club who played in the U12 to U19 groups during the seasons 2013-2014 and/or 2014-2015 and/or 2015-2016. Players were included when they (1) played in the academy for at least 1 full season to a maximum of 3 seasons, (2) had at least 1 PHV measurement taken, (3) had complete injury registration over the season(s) during the study, and (4) had training and match exposure registration over the season(s) during the study.
As data for this study were routinely collected in the academy program, players were not exposed to an extra burden of measurements or activities. At the start of the study, the Dutch Central Committee on Research Involving Human Subjects (CCMO) confirmed that no ethical approval was needed, as stated in the Dutch Medical Research Involving Human Subjects Act (WMO). Parents gave their written informed consent to use the anonymized data for scientific purposes. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement was used to report the findings of this study.26
Measurements and Procedures
Body weight was measured with a weight scale (Seca 700; Seca) with 50-g increments. This scale was calibrated every 3 months. Body height was assessed with a verified measuring rod (Seca 220; Seca). Players stood upright with their head positioned in the Frankfort horizontal plane. They were barefoot while wearing underwear and soccer shorts, with their feet positioned together.15 Standing and sitting height were registered in 0.5-cm increments. For sitting height, the maximum distance from the top to the buttocks was measured while the player was sitting on a standard 50-cm box with his hands on the upper legs, looking straightforward and holding his breath after deeply inhaling. All measurements were taken in the afternoon between 3:00 PM and 5:00 PM before a training session. An experienced (>4 years) assessor performed all PHV measurements.
Peak Height Velocity
The age at PHV was calculated according to the algorithm of Mirwald et al15 (R 2 = 0.92, standard error of the estimate = 0.49):
where A is the standing height (cm), B is the sitting height (cm), C is the chronological age (years), and D is the weight (kg).
When more than 1 PHV measurement was obtained, the measurement of the date closest to the estimated age of PHV was used to attain the most reliable estimate of PHV.15
PHV Periods
To allow the comparison of IID in different PHV periods with previous findings13,23,24 and clinical observations from the Athletic Skills Model (ASM),27 we identified 6 periods. The pre-PHV periods were PHV 1 (>12 months before PHV), PHV 2 (6-12 months before PHV), and PHV 3 (<6 months before PHV). The post-PHV periods were PHV 4 (<3 months after PHV), PHV 5 (3-6 months after PHV), and PHV 6 (>6 months after PHV). The combination of PHV periods 4 and 5 was used to compare equally long periods of 6 months before (PHV 2 and 3) and after (PHV 4+5) PHV. We compared periods both individually and in combinations according to van der Sluis et al23,24 and the ASM27 (Table 1).
TABLE 1.
Classification of PHV Periods in Other Studies/Models and Those in the Current Studya
| Pre-PHV | Post-PHV | ||||||
| >12 mo | 6-12 mo | <6 mo | <3 mo | 3-6 mo | 7-12 mo | >12 mo | |
| Materne et al13 | 1 | 2 | 3 | ||||
| van der Sluis et al23,24 | 1 | 2 | 3 | ||||
| ASM27 | 1 | 2 | 3 | ||||
| Current study | PHV 1 | PHV 2 | PHV 3 | PHV 4+5 | PHV 6 | ||
a1, time before PHV period; 2, defined period around PHV; 3, time after PHV period; ASM, Athletic Skills Model; PHV, peak height velocity.
Age Groups
Team formation at the soccer academy is based on chronological age, per year, ranging from U12 to U19. Players aged 17 and 18 years play in the U19 group (there is no separate U18 group).
Injury Registration
All players had to contact the club’s medical staff in case of an injury. According to the consensus statement on injury reporting in soccer,7 an injury was defined as any physical complaint resulting from a soccer match or training that prevented a player from taking full part in future soccer training or match play. The sports medicine physician and/or sports physical therapist performed all diagnoses and registered them according to the Orchard Sports Injury Classification System.19 The location (body region), type (medical or tissue diagnosis), and character (acute/overuse) of the injury were coded according to a standard list. The dates of injury and return to sport (defined as the moment of full re-participation in training and/or match play) were recorded.
Injury severity was defined as the number of days that a player was unable to participate fully in training or match play as a result of the injury. This was categorized as minimal (1-3 days), mild (4-7 days), moderate (8-28 days), or severe (>28 days).19 Whether injuries were growth specific (ie, apophysitis) could not be retrieved from the data.
Exposure
Exposure was registered in minutes by the trainer/coach. Match exposure was registered at an individual level. Training exposure was registered at a team level. Missed training exposure as a result of injury was recorded. Individual exposure was calculated as ((match exposure + training exposure) – missed training exposure) for every player per age group and every individual PHV period.
Statistical Analysis
All descriptive variables (age at PHV, chronological age, and duration of injury) were assessed for normality (Shapiro-Wilk test). Normally distributed data are reported as mean ± SD and range when applicable. Nonnormally distributed data are reported as median with interquartile range (IQR). Descriptive data on sustained injuries (total, acute, and overuse) and their body location and severity (duration and days of time loss) are presented as counts and percentages. Statistical analyses were performed with SPSS 22.0 (IBM).
The primary outcome measure was IID,25 which was calculated per subgroup (for all separate and combined PHV periods and age groups as ((number of injuries/hours of exposure) × 1000). To compare the injury risk between groups, the incidence ratio (IR) was calculated as the chance of sustaining an injury and compared with the chance found in the total group according to the following formula: (IID subgroup)/(IID total group). For IID and IR, 95% CIs were calculated. When the 95% CI of an IR did not pass the “1” value, the IIDs were considered different between groups. For example, an IR of 1.25 indicates that the chance of sustaining an injury in that specific subgroup is 25% higher than in the total group. In case of an IR of 0.70, this chance is 30% lower.25 P values were calculated using Z scores (lowest 95% CI value of IR/highest 95% CI value of IR). The alpha level for statistical significance was set at .05.
The secondary outcome measure was injury burden. Because of the skewed distribution, we used the median to calculate the injury burden (number of injuries × median number of time-loss days per injury) per 1000 hours of soccer exposure.1 To compare the injury burden of subgroups with the overall injury burden, the burden ratio (BR) and 95% CI were calculated similar to the IR for the IID. Again, Z scores were used to calculate P values.
Results
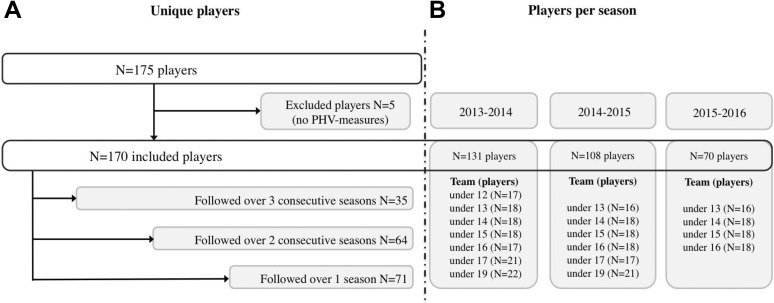
The original cohort consisted of 175 soccer players. Of these, 5 players were excluded because they had no PHV measurement taken as a result of illness or an in-season transfer to another club. Of the remaining 170 players, 35 were observed over 3 seasons, 64 over 2 seasons, and 71 over 1 season. The U13 to U16 groups were observed over 3 seasons, U17 and U19 groups over 2 seasons, and U12 group over 1 season (Figure 1).
Figure 1.
(A) Flowchart of inclusion and exclusion and numbers of observed players over consecutive seasons. (B) Numbers of observed players per season and per team. PHV, peak height velocity.
The mean age at PHV was 14.4 ± 0.65 years (range, 12.8-16.5 years). The biological age of players within a single team could be 3 years apart (highest/lowest), with the largest variance found in the U15 group (3.1 years). Of all 170 players, 148 (87.1%) together sustained a total of 620 injuries (range, 1-19 injuries per player), of which 468 (75.5%) were acute and 152 (24.5%) were overuse injuries (Table 2). The total group sustained a mean of 2.0 injuries per player per season. Most injuries (n = 528, 85.2%) concerned the lower extremity, of which 393 (74.4%) were acute and 135 (25.6%) were overuse injuries. The most prevalent locations for acute injuries were the ankle (n = 114, 24.3%), thigh (n = 95, 20.2%), knee (n = 64, 13.6%), and hip/groin (n = 45, 10.4%). For overuse injuries, the hip/groin (n = 57, 37.5%) and knee (n = 39, 25.7%) were the most common locations. Among the 468 acute injuries were 207 strains, 170 sprains, and 27 fractures.
TABLE 2.
Injuries by Location, Type, and Severity
| Injury Type, n (%) | Severity,a n | ||||||
|---|---|---|---|---|---|---|---|
| Location | Total, n (%) | Acute | Overuse | 1-3 d | 4-7 d | 8-28 d | >28 d |
| Head/spine/belly/pelvis | |||||||
| Head/face | 11 (1.8) | 11 (2.4) | 0 (0.0) | 3 | 2 | 5 | 1 |
| Neck/cervical spine | 2 (0.3) | 2 (0.4) | 0 (0.0) | 1 | 0 | 1 | 0 |
| Sternum/ribs/thoracic spine | 4 (0.6) | 3 (0.6) | 1 (0.1) | 2 | 0 | 2 | 0 |
| Belly | 2 (0.3) | 1 (0.2) | 1 (0.1) | 0 | 1 | 1 | 0 |
| Lumbar spine/pelvic | 40 (6.5) | 25 (5.3) | 15 (9.9) | 13 | 11 | 10 | 6 |
| Subtotal | 59 (9.5) | 42 (8.9) | 17 (11.2) | 19 | 14 | 19 | 7 |
| Upper extremity | |||||||
| Shoulder/clavicle | 8 (1.3) | 8 (1.5) | 0 (0.0) | 5 | 1 | 1 | 1 |
| Upper arm | 1 (0.2) | 1 (0.2) | 0 (0.0) | 1 | 0 | 0 | 0 |
| Elbow | 4 (0.6) | 4 (0.9) | 0 (0.0) | 0 | 2 | 1 | 1 |
| Forearm | 4 (0.6) | 4 (0.9) | 0 (0.0) | 0 | 1 | 2 | 1 |
| Wrist | 11 (1.8) | 11 (2.4) | 0 (0.0) | 3 | 1 | 6 | 1 |
| Hand/finger/thumb | 5 (0.8) | 5 (1.1) | 0 (0.0) | 4 | 0 | 1 | 0 |
| Subtotal | 33 (5.3) | 33 (7.0) | 0 (0.0) | 13 | 5 | 11 | 4 |
| Lower extremity | |||||||
| Hip/groin | 102 (16.5) | 45 (10.4) | 57 (37.5) | 31 | 23 | 35 | 13 |
| Thigh | 106 (17.1) | 95 (20.2) | 11 (7.2) | 31 | 23 | 36 | 16 |
| Knee | 103 (16.6) | 64 (13.6) | 39 (25.7) | 29 | 15 | 36 | 23 |
| Lower leg/Achilles tendon | 55 (8.9) | 44 (9.4) | 11 (7.2) | 21 | 9 | 24 | 1 |
| Ankle | 121 (19.5) | 114 (24.3) | 7 (4.6) | 47 | 20 | 32 | 22 |
| Foot/toe | 41 (6.6) | 31 (6.6) | 10 (6.6) | 10 | 7 | 15 | 9 |
| Subtotal | 528 (85.2) | 393 (84.5) | 135 (88.8) | 169 | 97 | 178 | 84 |
| Total | 620 (100.0) | 468 (100.0) | 152 (100.0) | 201 | 116 | 208 | 95 |
aDefined as the number of days that a player was unable to participate fully in training or match play as a result of the injury.
The most prevalent injuries were bruises (n = 174, 28.1%), muscle injuries (n = 173, 27.9%), tendon injuries (n = 81, 13.1%), ligament injuries (n = 78, 12.6%), and fractures/other bone injuries (n = 56, 9.1%). The injury duration was not normally distributed. The mean duration was 16.8 ± 30.8 days, and the median was 7.0 days (IQR, 15; range, 1-371 days).
Injury Incidence Density
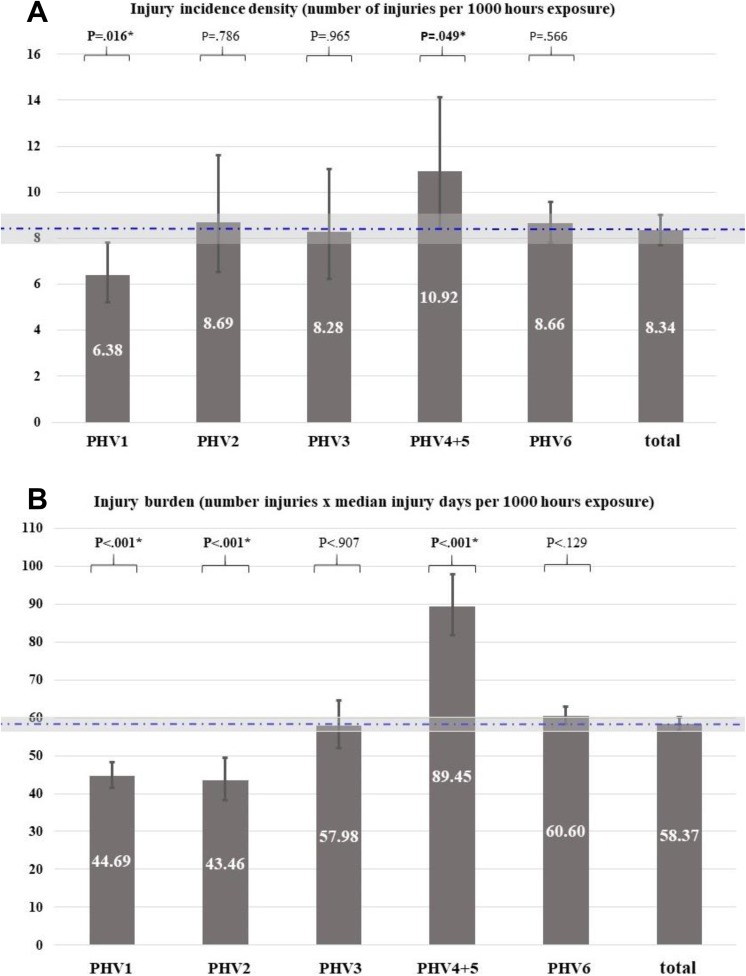
The overall mean IID was 8.34 injuries per 1000 hours of soccer exposure (95% CI, 7.71-9.02). For acute injuries, the IID was 6.29 (95% CI, 5.75-6.89) and for overuse injuries it was 2.04 (95% CI, 1.74-2.40). Compared with the overall IID, the IID in PHV period 4+5 (6 months after PHV) was significantly higher (IR, 1.31 [95% CI, 1.00-1.71]; P = .049) (Table 3 and Figure 2A), and the IID in PHV period 1 was significantly lower (IR, 0.77 [95% CI, 0.62-0.95]; P = .016). The IID for PHV periods 2, 3, and 6 were not significantly different when compared with the overall mean (Table 3).
TABLE 3.
IID, IR, Injury Burden, and BR by PHV Period According to the Classification of the Current Study, van der Sluis et al,23,24 and the ASM27 a
| Classification per Current Study | ||||||||
|---|---|---|---|---|---|---|---|---|
| Pre-PHV | Post-PHV | |||||||
| Total | PHV 1 (>12 mo to PHV) |
PHV 2 (6-12 mo to PHV) |
PHV 3 (<6 mo to PHV) |
PHV 4+5 (<3 to 6 mo after PHV) |
PHV 6 (>6 mo after PHV) |
|||
| IID (95% CI) | 8.34 (7.71-9.02) | 6.38 (5.22-7.81) | 8.69 (6.51-11.60) | 8.28 (6.22-11.02) | 10.92 (8.44-14.13) | 8.66 (7.82-9.58) | ||
| IR (95% CI) | 1.00 | 0.77 (0.62-0.95) | 1.04 (0.77-1.41) | 0.99 (0.74-1.34) | 1.31 (1.00-1.71) | 1.04 (0.91-1.18) | ||
| P value | .016b | .786 | .965 | .049b | .566 | |||
| Injury burden (95% CI) | 58.37 (56.66-60.13) | 44.69 (41.42-48.22) | 43.46 (38.19-49.46) | 57.98 (52.04-64.60) | 89.45 (81.76-97.87) | 60.60 (58.32-62.97) | ||
| BR (95% CI) | 1.00 | 0.77 (0.71-0.83) | 0.74 (0.65-0.85) | 0.99 (0.89-1.11) | 1.53 (1.39-1.68) | 1.04 (0.99-1.09) | ||
| P value | <.001b | <.001b | .907 | <.001b | .129 | |||
| Classification per van der Sluis et al23,24 | ||||||||
|
Total |
PHV 1-2 (>6 mo to PHV) |
PHV 3-5 (6 mo before–6 mo after PHV) | PHV 6 (>6 mo after PHV) |
|||||
| IID (95% CI) | 8.34 (7.71-9.02) | 6.99 (5.93-8.24) | 9.56 (7.89-11.57) | 8.66 (7.82-9.58) | ||||
| IR (95% CI) | 1.00 | 0.84 (0.70-1.01) | 1.15 (0.93-1.41) | 1.04 (0.91-1.18) | ||||
| P value | .059 | .195 | .566 | |||||
| Injury burden (95% CI) | 58.37 (56.66-60.13) | 44.37 (41.55-47.37) | 73.19 (68.30-78.43) | 60.60 (58.32-62.97) | ||||
| BR (95% CI) | 1.00 | 0.76 (0.70-0.82) | 1.25 (1.16-1.36) | 1.04 (0.98-1.10) | ||||
| P value | <.001b | <.001b | .174 | |||||
| Classification per the ASM | ||||||||
|
Total |
PHV 1 (>12 mo to PHV) |
PHV 2-4 (12 mo before–3 mo after PHV) |
PHV 5-6 (>3 mo after PHV) |
|||||
| IID (95% CI) | 8.34 (7.71-9.02) | 6.38 (5.22-7.81) | 9.09 (7.62-10.85) | 8.75 (7.93-9.65) | ||||
| IR (95% CI) | 1.00 | 0.77 (0.62-0.95) | 1.09 (0.90-1.32) | 1.05 (0.93-1.19) | ||||
| P value | .015 | .382 | .451 | |||||
| Injury burden (95% CI) | 58.37 (56.66-60.13) | 44.69 (41.42-48.22) | 55.71 (51.88-59.84) | 63.08 (60.82-65.42) | ||||
| BR (95% CI) | 1.00 | 0.77 (0.70-0.83) | 0.95 (0.88-1.04) | 1.08 (1.03-1.14) | ||||
| P value | <.001b | .260 | .004b | |||||
aASM, Athletic Skills Model; BR, burden ratio; IID, injury incidence density; IR, incidence ratio; PHV, peak height velocity.
bStatistically significant difference (P < .05) compared with the value for the total cohort in the current study for injury risk (top set) and injury burden (bottom set).
Figure 2.
(A) Injury incidence density (IID) and (B) injury burden for different peak height velocity (PHV) periods compared with the mean of the total cohort. (B) Injury burden (number of injuries × median injury days per 1000 hours of exposure). The boxes and whiskers depict the IID and injury burden and their 95% CI per PHV group. The horizontal dotted line and gray bar depict the mean IID and injury burden and their 95% CI. *Statistically significant difference (P < .05) compared with the value for the total cohort.
A comparison of PHV periods according to van der Sluis et al23,24 showed no significant differences in the injury risk for their PHV periods compared with the overall mean. According to the ASM classification, the IID in PHV period 1 was significantly lower than that in the total group (IR, 0.77 [95% CI, 0.62-0.95]; P < .016) (Figure 2A).
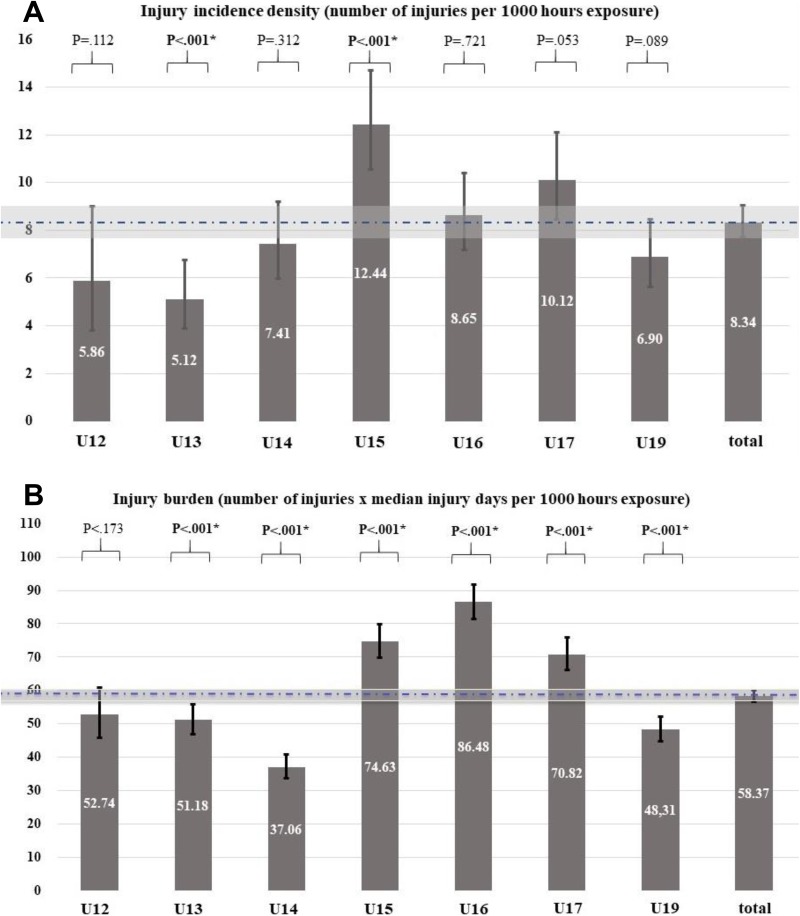
The IID in the U15 group was higher (IR, 1.49 [95% CI, 1.24-1.79]; P < .001) than that for the total group (Table 4 and Figure 3A). In the U17 group, we observed a trend toward a higher IID (IR, 1.21 [95% CI, 1.00-1.48]; P = .053). In the U13 group, a lower IID was found (IR, 0.61 [95% CI, 0.46-0.82]; P < .001) when compared with the total group (Table 4 and Figure 3A).
TABLE 4.
IID, IR, Injury Burden, and BR by Age Groupa
| Total | U12 | U13 | U14 | U15 | U16 | U17 | U19 | |
|---|---|---|---|---|---|---|---|---|
| Injury duration, median (range), d | 7.0 (1-371) | 9.0 (1-59) | 10.0 (1-110) | 5.0 (1-371) | 6.0 (1-143) | 10.0 (1-295) | 7.0 (1-277) | 7.0 (1-158) |
| Injuries per player per season | 2.0 | 1.2 | 1.0 | 1.6 | 2.6 | 2.1 | 3.1 | 2.2 |
| Exposure time, h | 74,358 | 3583 | 9965 | 11,332 | 11,175 | 13,066 | 11,761 | 13,475 |
| IID (95% CI) | 8.34 (7.71-9.02) | 5.86 (3.82-8.99) | 5.12 (3.89-6.73) | 7.41 (5.99-9.18) | 12.44 (10.53-14.69) | 8.65 (7.19-10.40) | 10.12 (8.45-12.11) | 6.90 (5.63-8.46) |
| IR (95% CI) | 1.00 | 0.70 (0.45-1.09) | 0.61 (0.46-0.82) | 0.89 (0.71-1.12) | 1.49 (1.24-1.79) | 1.04 (0.85-1.27) | 1.21 (1.00-1.48) | 0.83 (0.67-1.03) |
| P value | .112 | <.001b | .312 | <.001b | .721 | .053 | .089 | |
| Injury burden (95% CI) | 58.37 (56.66-60.13) | 52.74 (45.74-60.83) | 51.18 (46.92-55.82) | 37.06 (33.68-40.78) | 74.63 (69.74-79.87) | 86.48 (81.58-91.67) | 70.82 (66.17-75.80) | 48.31 (44.74-52.17) |
| BR (95% CI) | 1.00 | 0.90 (0.78-1.05) | 0.88 (0.80-0.96) | 0.63 (0.57-0.70) | 1.28 (1.19-1.38) | 1.48 (1.39-1.58) | 1.21 (1.13-1.31) | 0.83 (0.76-0.90) |
| P value | .173 | <.001b | <.001b | <.001b | <.001b | <.001b | <.001b |
aBR, burden ratio; IID, injury incidence density; IR, incidence ratio; U12, under 12 (U13, under 13; etc).
bStatistically significant difference (P < .05) compared with the value for the total cohort in the current study for injury risk (top set) and injury burden (bottom set).
Figure 3.
(A) Injury incidence density (IID) and (B) injury burden for different age groups compared with the mean of the total cohort. (B) Injury burden (number of injuries × median injury days per 1000 hours of exposure). The boxes and whiskers depict the IID and injury burden and their 95% CI per age group. The horizontal dotted line and gray bar depict the mean IID and injury burden and their 95% CI. U12, under 12 (U13, under 13; etc). *Statistically significant difference (P < .05) compared with the value for the total cohort.
Injury Burden
The overall injury burden was 58.37 injury days per 1000 hours of soccer exposure (95% CI, 56.66-60.13). In PHV period 4+5, the injury burden was significantly higher (BR, 1.53 [95% CI, 1.39-1.68]; P < .001) when compared with the overall mean (Table 3 and Figure 2B). A comparison of age groups showed the highest injury burden in the U16 group (86.48 [95% CI, 81.58-91.67]), which was also significantly higher (BR, 1.48 [95% CI, 1.39-1.58]; P < .001). The injury burden in the U15 and U17 groups was also significantly higher compared to overall. This is in contrast to the significantly lower injury burden in the U13, U14, and U19 groups (Table 4 and Figure 3B).
A comparison of the injury risk in PHV periods with the overall mean according to van der Sluis et al23,24 showed a higher injury burden in PHV period 3-5 (BR, 1.25 [95% CI, 1.16-1.36]; P < .001). According to the ASM classification, the injury burden in PHV period 5-6 was significantly higher compared with overall (BR, 1.08 [95% CI, 1.03-1.14]; P = .004) (Table 3).
Discussion
Young, talented soccer players have a higher injury risk and injury burden during the first 6 months after their PHV when compared with the overall mean. Comparisons for age groups revealed that the injury risk in the U15 group was higher than the overall mean. Among age groups, the injury burden in the U16 group was highest, and the injury burden in the U15 and U17 groups was higher than the overall mean as well. These findings imply that for both age groups and PHV periods, differences exist regarding injury risk parameters. We discuss our findings below.
Injury Characteristics
Most injuries (85.2%) were located in the lower extremity, with the highest prevalence in the ankle (19.5%), thigh (17.1%), knee (16.6%), and hip/groin (16.5%) regions. This is in line with the study of Price et al,18 who reported percentages of 19%, 19%, 18%, and 13%, respectively. Strains and sprains were the most prevalent injury types in both our study and their study.16 The mean injury duration of 16.8 days is also comparable with previous reports (12.5-26.3 days).5,11 As we found that the injury duration data were nonnormally distributed (skewed to the right), we used the median (7.0 days) in our study.
Injury Risk and Injury Burden
The IID is the most commonly used outcome measure to describe the injury risk. The duration of an injury reflects the consequences for such an injury for both the player and the team. The injury burden was recently proposed by Bahr et al1 as an additional and relevant outcome measure. The question is whether 1 long-standing injury of 200 days has more impact than, for example, 10 separate injuries of 15 days. In the first situation, 1 player needs to be replaced, whereas 10 players need to be replaced in the second situation. Furthermore, because long-standing injuries occur less frequently, their impact on the injury burden and BR between groups will be high. We therefore propose the injury burden to be calculated as (median injury duration [in days] × number of injuries divided by exposure time [in days]) to avoid overestimation due to single injuries of long duration. In our study, compared with overall, both the IID and injury burden were higher in the first 6 months after PHV and in the U15 group. In the U16 and U17 groups, the IID was not significantly higher, but based on the higher injury burden, these groups should also be considered as having a higher injury risk.
Comparison With Previous Studies
The higher injury risk found for the U15 group in our study is in line with results from previous studies.13,20 However, a strict comparison is difficult, as these studies did not use exposure time in their risk comparisons. The higher injury risk that we found in the first 6 months after PHV is not in line with the higher risk period of 6 months before PHV to 6 months after PHV found by van der Sluis et al,24 nor with the period from 1 year before PHV to 1 year after PHV found by Materne et al.13 We followed an open cohort of 170 players (7 teams, U12-U19) up to a maximum of 3 seasons. Materne et al13 also followed an open cohort (n = 289, 10 teams, U9-U18) of Qatari academy players over 1 season, and van der Sluis et al23,24 followed a smaller closed cohort (N = 26) over 3 seasons. In a closed cohort, a possible bias could be that the players who completed the full 3 years had fewer injuries. The “survival of the fittest” phenomenon may result in bias of the less serious injuries. In our opinion, the open inflow and outflow of players during the follow-up in our study represent more adequately the true setting and situation of players in an academy over several years. Differences in study designs (open vs closed cohort, age, teams) and training methods between clubs and individual teams may have contributed to the differences observed between studies. Considering the mean age at PHV of 14.4 ± 0.65 years in our study, the high-risk period of the first 6 months after PHV seems to coincide with the higher risk of injury in the U15 group. Large longitudinal studies are needed to further investigate the interaction between age groups and PHV periods.22
Exposure and Athletic Load
The increased vulnerability in the identified groups may relate to the athletic loading volume (hours of sport per week).6,14,17 It is advocated that younger players not take part in sport regimens for more hours per week than their age is in years. We found that the players’ soccer exposure in the academy was lower in all teams than their chronological age. All teams trained 4 times per week and played 1 or 2 matches lasting 60 (U12 and U13), 70 (U14 and U15), 80 (U16 and U17), or 90 (U19) minutes. We acknowledge that the soccer (or any other) load outside the academy (ie, at home or school) was not registered. The training load between age groups could have differed in our study, but this was not registered at the individual level. Therefore, acute and chronic workload ratios as potential influencers could not be calculated.8 Furthermore, upon reaching PHV, players may experience reduced load tolerance. In this period, a comparable training volume due to a reduced load capacity could imply an increased training load for an individual player. Continuous registration of perceived training loads and the IID is needed to further investigate this assumption.
Practical and Scientific Applications
As obtaining PHV measurements is time (and thus budget) consuming, this may only be organized in academies of professional soccer clubs. However, the accuracy of the method of Mirwald et al15 should be taken into consideration when these measurements are obtained. The observed higher injury risk (U15) and injury burden (U15, U16, and U17) in certain age groups (85.2% located in the lower extremity) suggest that future research into the underlying causes for the increased risk and duration of injuries in these groups is warranted. Study designs should ideally include large cohorts, comparable PHV periods, and registration methods of exposure time and workload to enable comparisons and/or data pooling between studies.
Limitations
This study has its limitations. A possible interaction effect between the PHV periods and chronological age groups was not investigated. The mix of a cross-sectional and longitudinal design combined with an underpowered data did not allow further analysis of interaction effects. We only had data from 1 season for the U12 group and data from 2 seasons for the U17 and U19 groups, resulting in a lower representation of these age groups. Yet, we do not know if more data, obtained from a larger number of players in these age groups, would have affected the results of this study. In addition, the competitive nature of the sport increases with age in youth teams, which can lead to more injuries as well as more serious injuries in higher age groups.
Training exposure was calculated at the team level and corrected by subtracting missed exposure as a result of injury. Individual training exposure data would have improved the accuracy of risk estimates. The club and the resources available did not allow this.
Furthermore, we calculated the age at PHV according the method described by Mirwald et al.15 It should be acknowledged that this has lower accuracy than the Tanner-Whitehouse method, but a clear advantage is the lack of stochastic radiation effects occurring in case of repeated measures.21
In addition, we do not know whether the first injury in the study was the first injury of the player in question, and the underlying causes of injuries (recorded according to the Orchard Sports Injury Classification System classification) were not registered. We could not separate the growth-related injuries in the overuse injury group. It is therefore possible that first-year players in the academy have a greater chance of injuries because they have to adapt to new training and competition regimens (regarding volume, intensity, or rhythm).
Generalizability
Generalizing these findings to other sports or soccer populations is questionable. Geographical and cultural differences may result in differences between types and volumes of training, surface and weather conditions, and other athletic participation in free time or at school. Comparisons with other sports seem impossible because injury patterns may differ widely. We are unaware of any other existing data on the relationship between biological/chronological age and sport injury, except for those described in this study.13,23,24
Conclusion
There was a higher injury risk (31%) in young academy soccer players during a period of 6 months after the age of PHV. This increased risk (49%) also existed in the chronologically classified U15 group. Based on the higher injury burden in the U15 (28%), U16 (48%), and U17 (21%) groups, we suggest that research on injury risk factors and preventive measures should primarily target these age groups. Additional PHV measurements seem to be of limited value from a screening perspective. Studies on different soccer academies with similar data registration are warranted to further establish the relation and interaction between the injury risk and injury burden in periods of growth and aging.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Dutch Medical Research Involving Human Subjects Act (WMO) from the Dutch Central Committee on Research Involving Human Subjects (CCMO).
References
- 1. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. 2018;52(16):1018–1021. [DOI] [PubMed] [Google Scholar]
- 2. Blimkie CJ, Lefevre J, Beunen GP, Renson R, Dequeker J, Van Damme P. Fractures, physical activity, and growth velocity in adolescent Belgian boys. Med Sci Sports Exerc. 1993;25(7):801–808. [DOI] [PubMed] [Google Scholar]
- 3. Davies PL, Rose JD. Motor skills of typically developing adolescents: awkwardness or improvement? Phys Occup Ther Pediatr. 2000;20(1):19–42. [PubMed] [Google Scholar]
- 4. Difiori JP, Benjamin HJ, Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48:287–288. [DOI] [PubMed] [Google Scholar]
- 5. Elias SR. 10-year trend in USA Cup soccer injuries: 1988-1997. Med Sci Sports Exerc. 2001;33(3):359–367. [DOI] [PubMed] [Google Scholar]
- 6. Faude O, Rößler R, Junge A. Football injuries in children and adolescent players: are there clues for prevention? Sports Med. 2013;43(9):819–837. [DOI] [PubMed] [Google Scholar]
- 7. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med. 2006;40:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50(5):273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hawkins D, Metheny J. Overuse injuries in youth sports: biomechanical considerations. Med Sci Sports Exerc. 2001;33(10):1701–1707. [DOI] [PubMed] [Google Scholar]
- 10. Hirano A, Fukubayashi T, Ishii T, Ochiai N. Magnetic resonance imaging of Osgood-Schlatter disease: the course of the disease. Skeletal Radiol. 2002;31(6):334–342. [DOI] [PubMed] [Google Scholar]
- 11. Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. 2006;34(6):928–938. [DOI] [PubMed] [Google Scholar]
- 12. Malina RM. Maturity status and injury risk in youth soccer players. Clin J Sport Med. 2010;20(2):132. [DOI] [PubMed] [Google Scholar]
- 13. Materne O, Farooq A, Johnson A, Greig M, McNaughton L. Relationship between injuries and somatic maturation in highly trained youth soccer players In: Favero T, Drust B, Dawson B, eds. International Research in Science and Soccer II. Abingdon: Routledge; 2016:182–192. [Google Scholar]
- 14. McGuine TA, Post EG, Hetzel SJ, Brooks MA, Trigsted S, Bell DR. A prospective study on the effect of sport specialization on lower extremity injury rates in high school athletes. Am J Sports Med. 2017;45(12):2706–2712. [DOI] [PubMed] [Google Scholar]
- 15. Mirwald RL, Baxter-Jones AD, Bailey DA, Beunen GP. An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc. 2002;34(4):689–694. [DOI] [PubMed] [Google Scholar]
- 16. Pfirrmann D, Herbst M, Ingelfinger P, Simon P, Tug S. Analysis of injury incidences in male professional adult and elite youth soccer players: a systematic review. J Athl Train. 2016;51(5):410–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Post EG, Bell DR, Trigsted SM, et al. Association of competition volume, club sports, and sport specialization with sex and lower extremity injury history in high school athletes. Sports Health. 2017;9(6):518–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Price RJ, Hawkins RD, Hulse MA, Hodson A. The Football Association medical research programme: an audit of injuries in academy youth football. Br J Sports Med. 2004;38(4):466–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rae K, Orchard J. The Orchard Sports Injury Classification System (OSICS) version 10. Clin J Sport Med. 2007;17(3):201–204. [DOI] [PubMed] [Google Scholar]
- 20. Read PJ, Oliver JL, De Ste Croix MBA, Myer GD, Lloyd RS. An audit of injuries in six English professional soccer academies. J Sports Sci. 2018;36(13):1542–1548. [DOI] [PubMed] [Google Scholar]
- 21. Serinelli S, Panetta V, Pasqualetti P, Marchetti D. Accuracy of three age determination x-ray methods on the left hand-wrist: a systematic review and meta-analysis. Leg Med (Tokyo). 2011;13(3):120–133. [DOI] [PubMed] [Google Scholar]
- 22. Swain M, Kamper SJ, Maher CG, Broderick C, McKay D, Henschke N. Relationship between growth, maturation and musculoskeletal conditions in adolescents: a systematic review. Br J Sports Med. 2018;52(19):1246–1252. [DOI] [PubMed] [Google Scholar]
- 23. van der Sluis A, Elferink-Gemser MT, Brink MS, Visscher C. Importance of peak height velocity timing in terms of injuries in talented soccer players. Int J Sports Med. 2015;36(4):327–332. [DOI] [PubMed] [Google Scholar]
- 24. van der Sluis A, Elferink-Gemser MT, Coelho-E-Silva MJ, Nijboer JA, Brink MS, Visscher C. Sport injuries aligned to peak height velocity in talented pubertal soccer players. Int J Sports Med. 2014;35(4):351–355. [DOI] [PubMed] [Google Scholar]
- 25. Verhagen E, van Mechelen W, eds. Sports Injury Research. Oxford: Oxford University Press; 2010. [Google Scholar]
- 26. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. [DOI] [PubMed] [Google Scholar]
- 27. Wormhoudt R, Savelsbergh GJP, Teunissen JW, Davids K, eds. The Athletic Skills Model: Optimizing Talent Development Through Movement Education. Abingdon: Routledge; 2018. [Google Scholar]