Abstract
Background:
Prior to the annual National Football League (NFL) Draft, the top college football prospects are evaluated by medical personnel from each team at the NFL Scouting Combine. On the basis of these evaluations, each athlete is assigned an orthopaedic grade from the medical staff of each club, which aims to predict the impact of an athlete’s injury history on his ability to participate in the NFL.
Purpose:
(1) To identify clinical predictors of signs, symptoms, and subsequent professional participation associated with football-related injuries identified at the NFL Combine and (2) to assess the methodological quality of the evidence currently published.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. We reviewed all studies that examined musculoskeletal injuries identified among athletes at the NFL Combine and associated outcomes. Data on signs, symptoms, and subsequent NFL participation were collected, and the methodological quality of the studies was assessed.
Results:
Overall, 32 studies, including 30 injury-specific studies, met the inclusion criteria. Twenty studies analyzed data collected at the NFL Combine from 2009 and later. When compared with matched controls, athletes with a history of a cervical or lumbar spine injury, rotator cuff repair, superior labrum anterior-posterior repair, anterior cruciate ligament reconstruction, full-thickness chondral lesions of the knee, or Lisfranc injury played in significantly fewer games early in their NFL careers. Additionally, athletes with a history of a cervical or lumbar spine injury, rotator cuff repair, and navicular injury had decreased career lengths versus controls. Defensive players and linemen were found to have decreased participation in the NFL for several injuries, including prior meniscectomy, anterior cruciate ligament reconstruction, and shoulder instability. Career length follow-up, measures of athletic participation, and matching criteria were highly variable among studies.
Conclusion:
For medical professionals caring for professional football athletes, this information can help guide orthopaedic grading of prospects at the NFL Combine and counseling of athletes on the potential impact of prior injuries on their professional careers. For future studies, improvements in study methodology will provide greater insight into the efficacy of current treatments and areas that require further understanding.
Keywords: football, NFL, combine, injury, participation, career
Each offseason, the top college football prospects are invited to attend the National Football League (NFL) Scouting Combine. This weeklong event is held prior to the NFL Draft and allows the medical staff of each NFL club to collect medical histories, perform comprehensive physical examinations, and collect imaging modalities, including plain radiographs, magnetic resonance imaging (MRI), and computed tomography as indicated. Subsequently, the medical staff of each club assigns each player an orthopaedic grade, according to its own criteria, in an attempt to predict the impact of a given history on a player’s physical durability, career longevity, and participation in the NFL.5 This information often affects a player’s draft status, and up to 6% of players may even receive failing medical grades.4
Since 1987, databases have been formed containing the medical information of all players evaluated at the NFL Combine.4 Numerous retrospective studies based on these data have been published.1,4–6 In recent years, Provencher and colleagues have published several studies with NFL Combine data collected from 2009 to 2015, analyzing the association between specific prior injuries and outcomes in the NFL (draft position, games played, and games started during the first 2 NFL seasons).1,8,9,22,25,28,31,32,38 These studies enable team management, scouts, coaches, physicians, and athletic trainers to better understand the impact of a given injury on a player’s participation in the NFL. More important, even beyond the NFL, such information may (1) help athletes and medical professionals better understand the ability to return to sport at a high level, (2) guide treatment options, and (3) set appropriate expectations for both parties.6
The purpose of this systematic review was to critically evaluate the available literature on clinical predictors of outcomes relevant to musculoskeletal injuries reported or diagnosed at the NFL Scouting Combine. Specifically, we sought to (1) identify clinical predictors of signs, symptoms, and subsequent professional participation associated with football-related injuries identified at the NFL Combine and (2) assess the methodological quality of the currently published evidence.
Methods
A systematic review was conducted in July 2018 according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.20 PubMed (Medline), Embase, and the Cochrane library were searched with the terms “National Football League,” “NFL,” “combine,” “injury,” and surgery.” The search was limited to English-language articles. Titles and abstracts from these searches were independently reviewed by 2 authors (D.W., S.A.T), and full-text articles meeting the inclusion criteria were then obtained and reviewed. Additionally, the references of all included full-text articles were scanned for further eligible studies.
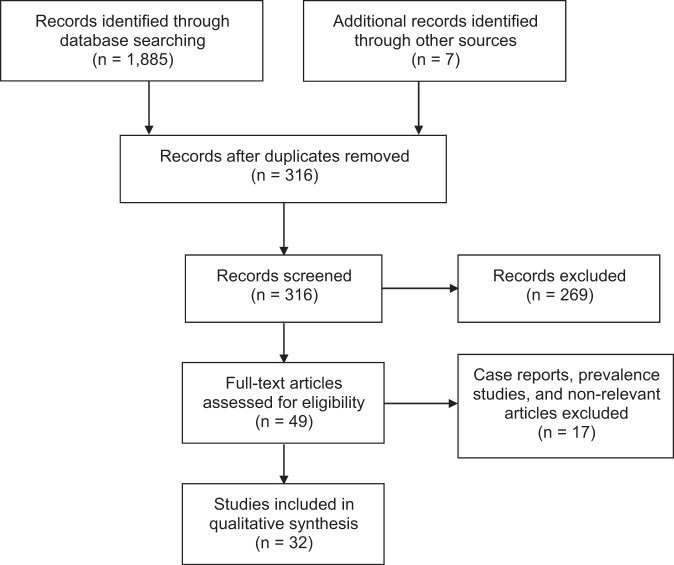
Inclusion criteria were established before data collection. Studies were included if they reported on musculoskeletal injuries identified among athletes at the NFL Combine and their association with clinical signs and symptoms and/or future participation in the NFL, including games played and career length. Studies were excluded if they (1) were case reports of 1 or only a few participants; (2) were epidemiologic studies that reported just the prevalence of specific injuries at the NFL Combine and did not evaluate for associations between injury and clinical signs, symptoms, or outcomes in the NFL; or (3) examined football-related injuries occurring after the NFL Combine. After elimination of duplicate articles among databases and screening of abstracts for relevance, 32 studies were analyzed (Figure 1). Thirty studies examined a cohort of athletes with a specific diagnosis or injury. All studies were retrospective, with the exception of 2 studies that prospectively collected data at the NFL Combine from a single year.2,12
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart of the literature search process.
Two authors (D.W., M.A.) extracted the data, which were then reviewed by the coauthors. Any disagreements in data were resolved by consensus or by arbitration of a third author (L.J.W.). The tabulated data included the injury or surgery, combine years studied, number of injuries and athletes, and level of evidence. Outcomes collected included draft status, game participation data, NFL career length, and clinical assessments derived from physical examination, imaging, and functional measures related to the specific injury.
The level of evidence of the selected studies was determined according to the criteria established by the Oxford Centre for Evidence-Based Medicine.39 As no randomized clinical trials were identified among the included studies, the MINORS criteria (methodological index for nonrandomized studies) were used to assess the methodological quality of the studies.36 This tool has 8 criteria to assess the methodological quality of noncomparative studies and 4 additional criteria for assessing the methodological quality of comparative studies. Each criterion is scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate), with the global ideal score being 16 for noncomparative studies and 24 for comparative studies.
Results
Data by Injury
Of the 32 studies, 30 were injury specific. There were 2 studies on cervical spine injuries,30,35 5 on foot injuries,7,23,25,37,38 1 on hand injuries,26 4 on hip/groin injuries,14,17,18,33 9 on knee injuries,2,8,9,13,21,22,24,31,32 3 on lumbar spine injuries,27,29,34 and 6 on shoulder injuries.10,11,15,16,19,28 No studies specifically examined injuries of the ankle, elbow, or long bones. Nineteen studies analyzed data collected at the NFL Combine from 2009 or later.∥ There were 22 level 3 studies (Table 1) and 8 level 4 studies (Table 2). Based on the MINORS criteria, the mean score for methodological quality of the level 3 studies was 16.4 (range, 13-19) out of a possible 24 points. The mean score for methodological quality of the level 4 studies was 10.8 (range, 7-13) out of a possible 16 points.
TABLE 1.
Summary of Injury-Specific NFL Combine Level 3 Retrospective Studiesa
| First Author | Injury/Surgery | Years | Injuries (Athletes), n | Methods | Results |
|---|---|---|---|---|---|
| Cervical spine | |||||
| Schroeder35 | Cervical spine diagnosis | 2003-2011 | 143 (143) | Study on athletes with a history of a cervical spine diagnosis Control group matched by age, position, year drafted, and round drafted Outcomes: draft status, years played, games played and started, performance |
Most common diagnoses: spondylosis, stenosis, cervical sprain/strain Athletes with cervical spine diagnosis were less likely to be drafted vs controls (P = .001) Athletes drafted who had a cervical spine diagnosis had decreased total games played (P = .01) but no significant differences in number of games started or performance score vs controls Athletes with cervical spine stenosis and those with prior cervical spine surgery demonstrated no difference in performance-based outcomes and no reports of neurological injury during their careers |
| Presciutti30 | Chronic stinger syndrome | 2005-2006 | 28 (28) | Study on athletes with cervical spine MRI Athletes with chronic stingers vs those without chronic stingers and age-matched nonathletes Outcomes: mean subaxial cervical space available for the cord (MSCSAC), mean subaxial cervical Torg ratio |
Athletes with chronic stingers had lower MSCSAC (4.5) vs those without chronic stingers (5.8; P < .01) and controls (6.7; P < .001) A critical value of 5.0 mm for the MSCSAC produced a sensitivity of 80% and a negative likelihood ratio of 0.23 for predicting chronic stingers MSCSAC more accurate than the classic Torg ratio |
| Foot | |||||
| Carreira7 | Jones fracture/fifth metatarsal diaphyseal stress fracture | 2004-2009 | 74 (68) | Study on athletes with a history of a Jones or proximal diaphyseal fifth metatarsal fracture Control group matched by draft status, player position, BMI, and medical grade Outcomes: games played and started, years played |
Among all fractures, 61% were Jones, 20% were proximal diaphyseal, and 19% were of indeterminate location No significant differences in mean games played/started, total years, and likelihood of being drafted between fracture and control groups |
| Tu37 | Jones fracture fixation | 2012-2015 | 41 (40) | Study on athletes who had undergone fixation of Jones fracture Control group with no history of Jones fracture fixation Outcomes: draft status, games played and started |
All fractures treated with intramedullary screw fixation with 92% complete union No athletes, including those with incomplete union, had any limitations in strength of ROM No significant differences between percentage drafted, games played, or games started between fracture and control groups |
| McHale25 | Lisfranc injury | 2009-2015 | 41 (41) | Study on athletes with a history of a Lisfranc injury Control group with no history of midfoot injury matched by position Outcomes: draft status and position, games played and started, NFL career length ≥2 y |
63% of injuries treated operatively Athletes treated surgically were more likely to go undrafted (P = .04) and had a worse draft position (P = .03) vs those treated nonoperatively Athletes with Lisfranc injury had worse draft position (P = .04) and fewer games played (P = .001) and started (P = .08) vs controls Athletes with >2-mm residual displacement on radiograph had worse outcomes across all measurements vs those with ≤2-mm displacement |
| Vopat38 | Navicular injury | 2009-2015 | 15 (14) | Study on athletes with a history of a navicular injury Control group matched by position and composed of players who missed <2 games in college and did not undergo previous surgery or have a documented injury Outcomes: draft status and position, games played and started, NFL career length ≥2 y |
11 overt navicular fractures, 3 stress reactions on MRI 8 athletes with navicular fracture underwent surgery Evidence of ipsilateral talonavicular arthritis in 75% of those with fracture vs 60% in the uninjured foot (P = .04) 57% of athletes with navicular injury were undrafted vs 31% of the control group (P = .001) 29% of athletes with navicular injury played ≥2 y vs 70% of the control group (P = .02) |
| Hip/groin | |||||
| Knapik14 | Athletic pubalgia repair | 2012-2015 | 55 (55) | Study on athletes who had undergone surgical repair for athletic pubalgia Control group without history of athletic pubalgia repair Outcomes: draft status, current NFL status, games played and started, positive pathology (pubic plate injury, rectus abdominis injury, adductor aponeurosis injury, or combination thereof) on postsurgical MRI |
No significant differences in games played/started, draft status, or current status between athletic pubalgia and control groups 53% of those with postsurgical MRI showed positive pelvic pathology No significant differences in games played/started, draft status, and current status between athletes with negative and positive MRI pathologies Offensive linemen (P = .005) and athletes who had surgery <1 y before NFL Combine (P = .03) were more likely to have positive pathology on MRI |
| Knapik17 | Hip arthroscopic surgery | 2012-2015 | 15 (14) | Study on athletes who had undergone hip arthroscopic surgery Control group with no history of hip arthroscopic surgery Outcomes: draft status, games played and started, current status |
Acetabular labral tearing was treated with repair alone (73%), debridement alone (7%), or repair and debridement (13%) in 93% of hips undergoing arthroscopic surgery Decompression for FAI was performed in 33% of hips No significant differences in draft status, current status, games played, or games started between surgical and control groups |
| Knee | |||||
| Keller13 | ACLR | 2010-2014 | NA (98) | Study on athletes with a history of ACLR Control group matched by age, size, and position Outcomes: 40-yd dash, vertical leap, broad jump, shuttle drill, 3-cone drill |
No significant differences in 40-yd dash times, vertical leap, broad jump, shuttle drill times, and 3-cone drill times between ACLR and control groups |
| Provencher31 | ACLR | 2009-2015 | NA (110) | Study on athletes with a history of ACLR Injury-free control group matched by position and draft class Outcomes: draft status, games played and started, snap percentage |
Athletes with prior ACLR were drafted lower (P = .019), played and started fewer games (P ≤ .003), and had lower snap percentage (P < .001) Defensive linemen, defensive backs, and linebackers were most affected positions |
| Provencher32 | Chondral injury | 2009-2015 | 124 (101) | Study on athletes with knee chondral injuries without history of prior knee surgery Injury-free drafted control group Outcomes: draft position, games played and started, snap percentage, position-specific performance metrics |
Patella (63%) and trochlea (34%) were most commonly affected Defensive linemen at highest risk for unrecognized injuries (P = .015) Athletes with untreated chondral injuries had lower draft position, played fewer games, and started fewer games than controls (P < .001) Subchondral bone edema and full-thickness cartilage injuries were associated with fewer games played (P = .003) |
| Chahla8 | Meniscectomy and chondral injury | 2009-2015 | 249 (247) | Study on athletes with chondral injury in the setting of prior meniscectomy Compared with injury-free control group matched by position Condition of the meniscus graded with modified ISAKOS scores Condition of the cartilage graded with ICRS scores Outcomes: draft position, games played and started, snap percentage |
287 players had a prior meniscectomy (206 lateral, 81 medial) Poorer meniscal score was associated with worse chondral pathology, especially in the lateral compartment Controls had greater number of games played and started and higher snap percentage vs those with prior meniscectomy of at least 10% volume Athletes with severe chondral lesions (ICRS grade 4) had significantly worse performance metrics vs controls |
| Logan22 | MCL injury | 2009-2015 | 337 (301) | Study on athletes with a history of MCL injury Injury-free control group Outcomes: draft position, games played and started, snap percentage |
55% had additional soft tissue injury (eg, meniscus, ACL, PCL) No significant differences in draft status/position, games played, or games started between athletes with MCL injury and controls Athletes with isolated MCL injury had better draft position (P = .034), proportion playing ≥2 NFL seasons (P = .022), games played (P = .014), and games started (P = .020) vs athletes with combined injuries |
| Chahla9 | Posterolateral corner injury | 2009-2015 | 23 (23) | Study on athletes with a history of posterolateral corner injury Inclusion criteria: positive clinical findings or previous surgery consistent with a posterolateral corner injury Compared with surgery-free control group matched by position Outcomes: varus stress physical examination, draft status, games played and started |
70% of injuries treated surgically, 30% were diagnosed on clinical examination 57% were combined injuries (with ACL, MCL, or PCL), all treated surgically 87% of injuries treated surgically were stable on examination, whereas none of the injuries managed nonoperatively were stable No significant differences in draft status, games played, or games started between posterolateral corner injury and control groups; athletes with surgically managed posterolateral corner injuries started fewer games than controls (P = .03) |
| Lumbar spine | |||||
| Moorman27 | Hyperconcavity of the lumbar vertebral end plates | 1992-1993 | 88 (88) | Study on linemen with radiographic evidence of hyperconcavity of lumbar vertebral end plates Control group of nonathletes matched by age Outcomes: incidence, association with lumbosacral spine symptoms |
Hyperconcavity present in 33% of linemen vs 8% in controls (P < .0001) Trend toward lower incidence of lumbosacral spine symptoms for those with hyperconcavity (P = .1839) When hyperconcavity was present, all 5 lumbosacral disk spaces were commonly affected |
| Paxton29 | Hyperconcavity of the lumbar vertebral end plates | 1992-1993 | 93 (93) | Study on linemen with radiographic evidence of hyperconcavity of the lumbar vertebral end plates Control group matched by year and round drafted, surgery and injury history Outcomes: percentage who played at least 1 NFL game, career length, games played and started |
No difference in likelihood of playing in NFL, years played, games played, or games started between athletes with lumbar spine hyperconcavity and controls No association between lumbar spine hyperconcavity and BMI |
| Schroeder34 | Lumbar spine diagnosis | 2003-2011 | 414 (414) | Study on athletes with a history of a lumbar spine diagnosis Control group matched by age, position, year and round drafted Outcomes: draft status, years played, games played and started, performance |
Most common diagnoses: degenerative spondylosis, herniated disc, spondylolysis with/without spondylolisthesis, strain Athletes without lumbar spine diagnosis were more likely to be drafted than those with a diagnosis (P < .001) Drafted athletes with preexisting lumbar spine injuries had decreased number of years played (P = .001), games played (P = .0001), and games started (P = .02) but not performance score (P = .013) vs controls Spondylolysis was associated with decreased career longevity (P < .05) |
| Shoulder | |||||
| Knapik16 | Bristow/Latarjet procedure | 2012-2015 | 10 (10) | Study on athletes who had undergone Bristow or Latarjet surgery Control group with history of isolated shoulder soft tissue repair without bony augmentation or fracture fixation Outcomes: draft status, games played and started, status after the athletes’ first NFL season |
70% had deficits in shoulder motion; 40% had evidence of mild glenohumeral arthritis 40% of athletes were drafted into NFL No significant risk of diminished participation with regard to games played and started vs controls 60% remained on active NFL roster after their first season |
| Knapik15 | Labral repair | 2012-2015 | 146 (132) | Study on athletes with a history of labral repair and MRI of the operative shoulder Control group with no history of labral repair Outcomes: association between primary labral repair location and presence and location of recurrent tearing, concomitant shoulder pathology, arthritis, draft status, games played and started |
32% of shoulders had recurrent labral tears on MRI Athletes with recurrent tears were more likely to have undergone bilateral labral repairs (P = .048) and possess concomitant shoulder pathology (P < .001) Recurrent labral tearing was more common in posterior labrum in the setting of prior posterior labral repair (P = .032) No significant differences in games played and games started between athletes who had undergone labral repair and controls No significant differences in chance of being drafted, games played, and games started between athletes with recurrent tearing and intact repairs |
| Murphy28 | Anterior labral injury | 2009-2015 | 226 (206) | Study on athletes with a history of an anterior labral injury Control group without history of surgery and >2 games missed in college Outcomes: draft status, games played and started, snap percentage |
72% had surgical intervention, 38% were treated nonoperatively No significant differences in draft status, games played, games started, or snap percentage vs controls Concomitant injury (eg, SLAP tear, glenoid bone loss, Hill-Sachs lesion) was associated with lower draft position (P = .003) |
| Gibbs11 | Rotator cuff tear | 2003-2011 | NA (49) | Study on athletes with a history of a rotator cuff tear Control group matched by age, position, year and round drafted Outcomes: draft status, years played, games played and started, performance score |
45% underwent surgical intervention, 55% treated nonoperatively Athletes with rotator cuff tear were less likely to be drafted vs controls (P = .002) Athletes who were drafted started fewer games (P = .02) and played fewer years (P = .04) and fewer games (P = .04) vs controls |
| Chambers10 | SLAP tears | 2003-2011 | NA (25) | Study on athletes reporting a history of a SLAP tear Control group with no documented shoulder pathology matched by position, age, and draft year and round Outcomes: draft success, games played and started |
SLAP repairs most performed in offensive linemen (32%) Drafted athletes with SLAP tears played fewer games (P = .049) and had fewer game starts (P = .036) vs controls |
aACL, anterior cruciate ligament; ACLR, ACL reconstruction; BMI, body mass index; FAI, femoroacetabular impingement; ICRS, International Cartilage Repair Society; ISAKOS, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine; MCL, medial collateral ligament; MRI, magnetic resonance imaging; NA, not available; NFL, National Football League; PCL, posterior cruciate ligament; ROM, range of motion; SLAP, superior labrum anterior-posterior.
TABLE 2.
Summary of Injury-Specific NFL Combine Level 4 Studies
| First Author | Injury/Surgery | Years | Injuries (Athletes), n | Methods | Results |
|---|---|---|---|---|---|
| Foot | |||||
| Low23 | Jones fracture | 1988-2002 | 86 (83) | Case series of athletes with a history of a Jones fracture Outcomes: radiographic union, complications |
53% of fractures were treated surgically; of these, 89% healed without complication and 7% developed nonunion 20% of fractures treated nonoperatively developed nonunion |
| Hand | |||||
| Moatshe26 | Scaphoid fracture | 2009-2015 | 56 (56) | Case series of athletes with a history of a scaphoid fracture Outcomes: clinical outcomes (ROM, pain, stiffness, grip strength, pinch test), complications |
76% treated with screw fixation, 4% treated with resection and fusion, 18% treated nonoperatively 72% had normal ROM of wrist, 93% reported no pain, 83% reported no stiffness; grip strength and pinch strength were 91% and 96% vs uninjured side 25% nonunion rate, 34% had degenerative changes, 15% had hardware complications |
| Hip/groin | |||||
| Larson18 | Hip or groin pain | 2009-2010 | 239 (125) | Case series of athletes with hip radiographs Outcomes: radiographic pathomorphology/abnormalities, radiographic predictors of athletic-related “hip” and “groin” symptoms |
87% had ≥1 finding on radiograph suggestive of cam- or pincer-type FAI 75 hips in the symptomatic group, 164 hips in the asymptomatic group Although the symptomatic group had greater prevalence of cam-type FAI (P = .009), combined-type FAI (P < .001), and osteitis pubis (P = .014), increased α angle (larger cam deformity) was the only independent predictor of groin pain (P = .01) FAI not correlated to BMI or player position |
| Rebolledo33 | Lower extremity and core muscle injuries | 2015 | 107 (107) | Case series of athletes with low vitamin D levels Outcomes: association between vitamin D levels and lower extremity muscle strain (adductor/groin, hamstring, hip flexor, quadriceps) or core muscle injuries |
59% of athletes with inadequate vitamin D levels, 10% with deficient levels Lower extremity or core muscle injury was present in 50% of athletes, which was associated with vitamin D levels (P = .03) African American race (P < .001) and positive injury history (P < .001) were associated with lower vitamin D levels No significant differences in age, BMI, or Functional Movement Screen scores among vitamin D groups |
| Knee | |||||
| Bedi2 | ACLR | 2012 | 34 (NA) | Case series of athletes measured for hip ROM Outcomes: association between reduction in hip ROM (internal rotation) and history of ACL injury |
Reduction of left hip internal rotation was associated with increased odds of ACL injury in either knee (P < .001) 30° reduction of left hip internal rotation was associated with 4.1- and 5.3-times-greater odds of ACL in the ipsilateral and contralateral limbs, respectively |
| Mall24 | ACLR | 2005-2009 | 137 (125) | Case series of athletes with a history of ACLR and radiographs/MRI Outcomes: association between graft obliquity and knee laxity on Lachman physical examination |
64% of knees had vertical grafts based on radiography and 35% based on MRI Knees with a sum score of ≤66 (sum of tibial and femoral tunnel positions on lateral radiograph), tibial tunnel ≤37% from anterior tibial plateau, and sagittal obliquity of ≤60° were less likely to have increased translation on Lachman examination than knees with higher corresponding values (P < .05) |
| Logan21 | PCL injury | 2009-2015 | 69 (69) | Case series of athletes with a history of PCL injury Inclusion criteria: positive clinical findings or previous surgery consistent with PCL injury Outcomes: posterior drawer physical examination, concomitant injuries identified on MRI, draft status, collegiate games missed |
Running back and offensive lineman were most common positions with PCL injuries (20% each) 16% treated surgically 52% of athletes had a grade II/III posterior drawer; athletes with grade III posterior drawer examination went undrafted Concomitant injuries: MCL (42%), ACL (12%), chondral (32%) |
| Shoulder | |||||
| LeBus19 | Latarjet procedure | 2009-2016 | 13 (13) | Case series of athletes who had undergone Latarjet procedure Outcomes: fixation type, hardware complications, bone block status, draft status, games played and started, total snaps, percentage of eligible snaps |
61% had 2-screw fixation, 39% had 1 screw 46% demonstrated hardware complications All athletes had evidence of degenerative changes on radiographs (77% mild, 8% moderate, 15% severe) 54% drafted; of these, no player participated in more than half of the plays during rookie season |
aACL, anterior cruciate ligament; ACLR, ACL reconstruction; BMI, body mass index; FAI, femoroacetabular impingement; MCL, medial collateral ligament; MRI, magnetic resonance imaging; NA, not available; NFL, National Football League; PCL, posterior cruciate ligament; ROM, range of motion.
Cervical and Lumbar Spine
Athletes with a cervical spine diagnosis (including spondylosis, stenosis, sprain/strain, herniated disc, and spine spasms) were less likely to be drafted, played fewer games (Table 3), and had decreased NFL career lengths (Table 4) as compared with controls. Those with a history of multiple stinger episodes were noted on MRI to have a lower mean subaxial cervical space available for the cord, with 5.0 mm reported as the critical value. Of note, players with a cervical sagittal canal diameter <10mm did not have any significant differences in games played or performance score compared with matched controls, and no neurological injury occurred during their careers.35
TABLE 3.
NFL Games Played Dataa
| Mean Games Played, n | ||||
|---|---|---|---|---|
| First Author | Injury/Surgery | Athletes With Injury | Controls | P |
| Schroeder35 | Cervical spine diagnosis | 42.1 | 55.6 | .01 |
| Schroeder34 | Lumbar spine diagnosis | 46.5 | 50.8 | <.01 |
| Lumbar spondylosis | 41 | 44.6 | .11 | |
| Lumbar herniated disc | 45.3 | 50 | .50 | |
| Spondylolysis with or without slip | 46.9 | 55.1 | .11 | |
| Paxton29 | Hyperconcavity of the lumbar vertebral end plates | 86 | 76 | .33 |
| Knapik15 | Shoulder labral repair | 7.04b | 2.8b | .38 |
| Murphy28 | Shoulder anterior labral injury | 14.3c | 15.3c | .39 |
| Knapik16 | Bristow/Latarjet procedure | 6.2b | 7.5b | .59 |
| Gibbs11 | Rotator cuff tear | 47.1 | 68.4 | .04 |
| Chambers10 | SLAP repair | 33.7 | 48.3 | .05 |
| Knapik14 | Athletic pubalgia repair | 17.2 | 17.6 | .87 |
| Knapik17 | Hip arthroscopic surgery | 10.9b | 11.0b | .96 |
| Provencher31 | ACL reconstruction | 9.2b | 7.4b | <.01 |
| Provencher32 | Knee chondral injury | 23.0c | 29.4c | <.01 |
| Logan22 | Knee MCL injury | 16c | 15c | .87 |
| Chahla9 | Posterolateral corner injury | 24c | 23.3c | .42 |
| Carreira7 | Jones fracture/fifth metatarsal diaphyseal stress fracture | 16.9 | 24.9 | .12 |
| Tu37 | Jones fracture fixation | 8.8b | 7.4b | .23 |
| McHale25 | Lisfranc injury | 16.9b | 23.3b | <.01 |
| Vopat38 | Navicular injury | 15.0c | 23.3c | .07 |
aBolded P values indicate statistically significant difference between groups (P < .05). ACL, anterior cruciate ligament; MCL, medial collateral ligament; NFL, National Football League; SLAP, superior labrum anterior-posterior.
bIn athletes’ first NFL season after the combine only.
cIn athletes’ first 2 NFL seasons after the combine only.
TABLE 4.
NFL Career Length Dataa
| Mean Years Played, n | ||||
|---|---|---|---|---|
| First Author | Injury/Surgery | Athletes With Injury | Controls | P |
| Schroeder35 | Cervical spine diagnosis | 3.7 | 4.6 | .01 |
| Schroeder34 | Lumbar spine diagnosis | 4.0 | 4.3 | <.01 |
| Lumbar spondylosis | 3.6 | 3.8 | .07 | |
| Lumbar herniated disc | 3.9 | 4.3 | .27 | |
| Spondylolysis with or without slip | 4.1 | 4.4 | .32 | |
| Paxton29 | Hyperconcavity of the lumbar vertebral end plates | 7.5 | 6.5 | .11 |
| Gibbs11 | Rotator cuff tear | 4.3 | 5.7 | .04 |
| Chambers10 | SLAP repair | 3.4 | 4.0 | .06 |
| Knapik14 | Athletic pubalgia repair | 1.5b | 1.6b | .52 |
aBolded P values indicate statistically significant difference between groups (P < .05). NFL, National Football League; SLAP, superior labrum anterior-posterior.
bData collected from maximum of 4 NFL seasons after the combine.
Athletes with a history of a lumbar spine diagnosis (including degenerative spondylosis, herniated disc, spondylolysis, and strain) were less likely to be drafted and had a decreased number of years played, games played, and games started. Radiographic evidence of hyperconcavity of the lumbar vertebral end plates (disk space expansion) in linemen was not associated with a significant difference in career length, games played, or games started as compared with controls.
Shoulder
Two studies demonstrated that athletes with labral injuries or those who had undergone labral repair of the shoulder did not have any significant differences in draft status, games played, games started, or snap percentage when compared with controls.15,28 Furthermore, athletes with evidence of recurrent labral tears on MRI did not have any significant differences in draft status, games played, or games started versus those with intact labral repairs. For athletes treated with bone block augmentation for shoulder instability, as many as 40% to 77% of athletes had evidence of glenohumeral arthritis on radiographs. Against controls, those who were drafted were not at significant risk for diminished participation with regard to games played or started in their first season in the NFL. In contrast, athletes with a history of a rotator cuff tear, of which 45% received operative treatment, were less likely to be drafted, played and started in fewer games, and played in fewer years versus controls. Finally, those treated with superior labrum anterior-posterior (SLAP) repair had no significant differences in draft status and performance scores as opposed to controls; however, they played and started in fewer games than healthy controls.
Hip and Pelvis
Athletes who had undergone athletic pubalgia repair or hip arthroscopic surgery did not have any significant differences in draft status, games played, or games started as compared with controls. Although the prevalence of cam- or combined-type femoroacetabular impingement and osteitis pubis was higher among symptomatic athletes, an increased alpha angle was the only independent predictor of athletic-related groin pain.
Knee
When compared with controls, athletes who had undergone anterior cruciate ligament (ACL) reconstruction were more likely to be picked lower in the draft, and they played and started fewer games in their first 2 NFL seasons. Chondral injuries of the knee were noted in 4.4% of athletes at the NFL Combine who had knee MRI because they reported prior injury or reported knee pain but had no known history of surgery; the patellofemoral joint was the most affected compartment. Athletes with chondral injuries, in the setting of no prior knee surgery or prior meniscectomy, played and started in fewer games versus controls. Specifically, subchondral bone edema and full-thickness chondral lesions were associated with fewer games played. Athletes with a history of medial collateral ligament injury or posterolateral corner knee injury did not have any significant differences in draft status, games played, or games started as opposed to respective controls.
Foot
A history of proximal fifth metatarsal fractures, including Jones fractures, was not associated with a difference in draft likelihood, games played, or games started, as compared with controls. In contrast, a history of Lisfranc or navicular injury was associated with worse draft position and fewer games played and started during the first 2 NFL seasons. In addition, a prior navicular injury was associated with significantly decreased probability of playing ≥2 years in the NFL.
Data by Position
Two level 3 studies specifically examined injuries identified at the NFL Combine and their impact on NFL participation by player position.1,6 Based on the MINORS criteria, the mean score for methodological quality of these studies was 17 (range, 16-18) out of a possible 24 points. NFL participation data by athlete position are summarized in Table 5. Game participation appears to be affected by injuries most in offensive and defensive linemen and defensive backs. Of note, spondylolisthesis was not significantly associated with a reduced percentage of athletes playing in the league or a shorter career length at any position.
TABLE 5.
NFL Participation Data by Athlete Positiona
| Position | Injury: Participation |
|---|---|
| Offense | |
| Offensive lineman | Shoulder instability: decreased chance of playing in NFL Rotator cuff tear: shorter playing career and fewer games played ACLR: decreased chance of playing in NFL, shorter playing career, and lower snap percentageb Meniscectomy: fewer games playedb and lower snap percentageb Ankle injury: fewer games playedb |
| Quarterback | Shoulder injury: fewer games playedb |
| Running back | Spondylolysis: decreased chance of playing in NFL Meniscectomy: fewer games playedb Chondral injury (knee): decreased fantasy scoreb |
| Tight end | Shoulder injury: fewer games playedb
Hand injury: fewer games playedb |
| Wide receiver | Shoulder instability: shorter playing career Meniscectomy: fewer games playedb Chondral injury (knee): decreased fantasy scoreb |
| Defense | |
| Defensive back | Cervical spine diagnosis: shorter playing career and fewer games played Lumbar spine diagnosis: shorter playing career, fewer games played, and lower performance score Hand injury: fewer games playedb ACLR: lower snap percentageb Meniscectomy: decreased chance of playing in NFL, shorter playing career, fewer games played,b and lower snap percentageb |
| Defensive lineman | Shoulder instability: decreased chance of playing in NFL and shorter playing career Rotator cuff tear: shorter playing career and fewer games played ACLR: decreased chance of playing in NFL, fewer games played,b and lower snap percentageb Meniscectomy: played fewer gamesb and lower snap percentageb Chondral injury (knee): decreased fantasy scoreb Ankle injury: fewer games playedb |
| Linebacker | ACLR: decreased chance of playing in NFL, fewer games played,b and lower snap percentageb
Meniscectomy: played fewer gamesb and lower snap percentageb Chondral injury (knee): decreased fantasy scoreb |
aACLR, anterior cruciate ligament reconstruction; NFL, National Football League.
bIn first 2 NFL seasons after the combine only.
Discussion
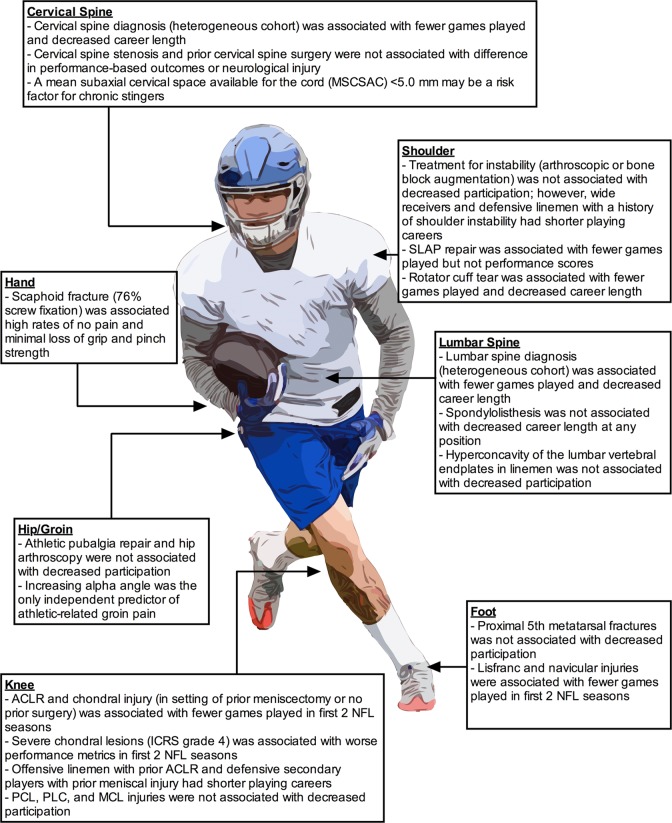
When compared with matched controls, athletes with a history of a cervical or lumbar spine injury, rotator cuff repair, SLAP repair, ACL reconstruction, full-thickness chondral lesions of the knee, or Lisfranc injury played in significantly fewer games early in their NFL careers. Additionally, athletes with a history of a cervical or lumbar spine injury, rotator cuff repair, or navicular injury had decreased career length versus controls. The potential impact of these injuries seems to vary by player position as well, with defensive players and offensive and defensive linemen having decreased participation in the NFL for several injuries, including prior meniscectomy, ACL reconstruction, and shoulder instability (Figure 2). Nevertheless, the available literature remains highly variable with regard to length of follow-up, matching criteria, measures of participation outcomes, and overall methodological quality.
Figure 2.
Summary of NFL participation data sorted by injury identified at the NFL Combine. ACLR, anterior cruciate ligament reconstruction; ICRS, International Cartilage Repair Society; MCL, medial collateral ligament; NFL, National Football League; PCL, posterior cruciate ligament; PLC, posterolateral corner; SLAP, superior labrum anterior-posterior.
Using NFL Combine data collected by 1 team from 1987 to 2000, Brophy et al5 examined the correlation between orthopaedic grade and career longevity in the NFL. Players with a high grade (no injury, minor injury, or successful surgical interventions) had a mean career of 42 games, as opposed to 34 games for players with a low grade (incomplete recovery and/or injury likely to recur) and 19 games for players with a failed grade. Thus, assigning orthopaedic grades to college football prospects based on their injury history has historically been a useful practice for predicting career longevity in the NFL. Of note, we found an increasing trend of likelihood of playing in the NFL for players treated with ACL reconstruction or shoulder stabilization over the study period, likely reflecting the improved understanding of these injuries and advancements in surgical technique and rehabilitation. As a result, over time, fewer players received failed grades at the combine.
Although recent NFL Combine studies have improved a medical professional’s ability to predict the impact of a prior injury on a player’s professional career, there is a dearth of studies examining athletes with a history of hand, elbow, long bone, and ankle injuries. Although hand and ankle injuries are among the most commonly identified injuries at the NFL Combine,1,4 this review found only 1 study on hand injuries and no studies on ankle injuries. Furthermore, while the lone hand study examined the clinical and radiographic outcomes of scaphoid fracture, it did not assess NFL participation metrics.26
Moreover, future studies utilizing more rigorous methodology would allow medical professionals to provide more accurate predictions of a prior injury’s impact on an athlete’s NFL career. Currently available studies on injuries of the cervical spine or lumbar spine classify all spine diagnoses together in their analyses, resulting in heterogeneous cohorts. These aggregated diagnoses, which included stinger, spondylosis, stenosis, spondylolysis, and sprain/strain, are all unique pathologies that have different symptoms and prognoses. Although the studies by Schroeder et al34,35 found that athletes with a cervical or lumbar spine diagnosis were less likely to be drafted and played in fewer games than controls, diagnoses of strain, scoliosis, and spasms were included in relatively fewer numbers when compared with the more severe diagnoses of spondylosis, spondylolysis, herniated disc, and stenosis. Future studies examining a more focused cohort of spine diagnoses are needed.
Additionally, measurement of draft status, games played and started, snap percentage, and game performance metrics are influenced by a multitude of factors (eg, player position, team needs, opponent game plan, depth chart), which can ultimately confound the results. Many currently available studies do not account for these factors. For instance, with regard to player position, drafted quarterbacks often do not play in any games during the first few years of their professional career, owing to their position on the depth chart, whereas kickers often go undrafted but are signed by teams and play during their rookie years. Several studies utilizing a matched control group did not match per player position.14,17,29,30,32,37 Some players are made inactive on game day despite being healthy and participating in practice. Therefore, measurement of games played or games started may not accurately represent the degree of professional athletic participation. Metrics such as athlete exposures, which accounts for practice participation, or days on the “physically unable to perform”–injured reserve list would better characterize athletic participation. Finally, missed time caused by reinjury to the previously injured anatomic area is more likely to be indicative of the impact of a specific prior injury on participation in the NFL.
Other limitations of this qualitative review are related to the level and availability of evidence reviewed. The majority of the studies reviewed were retrospective and used injury data that were self-reported or derived from scouting, introducing recall bias. Instead of using the NFL Injury Surveillance System, some studies used publicly accessible websites to collect participation and performance data, for which their accuracy or completeness cannot be verified. The majority of studies that measured participation or performance analyzed data within only the first 1 or 2 NFL years after the combine.1,8,9,22,25,28,31,32,38 Analysis of outcomes within the first 4 to 5 years, which is the length of the typical rookie contract, may be more valuable from an administrative perspective. The impact of injuries within an anatomic region may not be mutually exclusive to the same region; for instance, limited hip rotation and femoroacetabular impingement have been linked to risk of ACL injury.2,3 Finally, there is inherent selection bias in the analyzed studies, since athletes who were invited to the combine likely had successful outcomes after their injuries. These studies did not include athletes who were not invited to the combine but still made it to the professional level. Therefore, these findings cannot necessarily be extrapolated to the average collegiate football athlete, nor can they necessarily be extrapolated to high school or younger athletes, owing to the higher demands that are placed on the musculoskeletal system in the NFL.
Conclusion
NFL prospects with a history of a cervical or lumbar spine injury, rotator cuff repair, SLAP repair, ACL reconstruction, full-thickness chondral lesions of the knee, or Lisfranc injury played in significantly fewer games early in their NFL careers. Game participation was also dependent on player position, with defensive players and offensive and defensive linemen having decreased participation for several injuries. For medical professionals caring for professional football athletes, this information can help guide orthopaedic grading of prospects at the NFL Combine and counseling of athletes on the potential impact of prior injuries on their professional careers. For future studies, improvements in study methodology—including longer career follow-up, more accurate measures of athletic participation, more robust and consistent matching criteria, separate investigation of specific spine diagnoses, and prospective designs—will provide greater insight into the efficacy of current treatments and areas that require further understanding.
Acknowledgment
The authors thank Evan Pinkus for his assistance with Figure 2.
One or more of the authors has declared the following potential conflict of interest or source of funding: D.W. has received educational support from Smith & Nephew. R.F.W. receives royalties from Zimmer Biomet and Arthrex and hospitality payments from Stryker. S.A.R. receives royalties from Zimmer Biomet, honoraria from Fidia Pharmaceuticals, and nonconsulting payments from Smith & Nephew. S.A.T. has received educational support from Arthrex and Smith & Nephew, is a consultant for DePuy, and has received hospitality payments from Encore Medical and Exactech. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Beaulieu-Jones BR, Rossy WH, Sanchez G, et al. Epidemiology of injuries identified at the NFL Scouting Combine and their impact on performance in the National Football League: evaluation of 2203 athletes from 2009 to 2015. Orthop J Sports Med. 2017;5(7):2325967117708744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bedi A, Warren RF, Wojtys EM, et al. Restriction in hip internal rotation is associated with an increased risk of ACL injury. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):2024–2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boutris N, Byrne RA, Delgado DA, et al. Is there an association between noncontact anterior cruciate ligament injuries and decreased hip internal rotation or radiographic femoroacetabular impingement? A systematic review. Arthroscopy. 2018;34(3):943–950. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine—trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22–27. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Chehab EL, Barnes RP, Lyman S, Rodeo SA, Warren RF. Predictive value of orthopedic evaluation and injury history at the NFL combine. Med Sci Sports Exerc. 2008;40(8):1368–1372. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768–775. [DOI] [PubMed] [Google Scholar]
- 7. Carreira DS, Sandilands SM. Radiographic factors and effect of fifth metatarsal Jones and diaphyseal stress fractures on participation in the NFL. Foot Ankle Int. 2013;34(4):518–522. [DOI] [PubMed] [Google Scholar]
- 8. Chahla J, Cinque ME, Godin JA, et al. Meniscectomy and resultant articular cartilage lesions of the knee among prospective National Football League players: an imaging and performance analysis. Am J Sports Med. 2018;46(1):200–207. [DOI] [PubMed] [Google Scholar]
- 9. Chahla J, Kennedy NI, Cinque ME, et al. Posterolateral corner injuries of the knee at the National Football League Combine: an imaging and outcomes analysis. Arthroscopy. 2018;34(3):687–692. [DOI] [PubMed] [Google Scholar]
- 10. Chambers CC, Lynch TS, Gibbs DB, et al. Superior labrum anterior-posterior tears in the National Football League. Am J Sports Med. 2017;45(1):167–172. [DOI] [PubMed] [Google Scholar]
- 11. Gibbs DB, Lynch TS, Gombera MM, et al. Preexisting rotator cuff tears as a predictor of outcomes in National Football League athletes. Sports Health. 2016;8(3):250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33(8):1142–1146. [DOI] [PubMed] [Google Scholar]
- 13. Keller RA, Mehran N, Austin W, Marshall NE, Bastin K, Moutzouros V. Athletic performance at the NFL Scouting Combine after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(12):3022–3026. [DOI] [PubMed] [Google Scholar]
- 14. Knapik DM, Gebhart JJ, Nho SJ, Tanenbaum JE, Voos JE, Salata MJ. Prevalence of surgical repair for athletic pubalgia and impact on performance in football athletes participating in the National Football League Combine. Arthroscopy. 2017;33(5):1044–1049. [DOI] [PubMed] [Google Scholar]
- 15. Knapik DM, Gebhart JJ, Sheehan J, Tanenbaum JE, Salata MJ, Voos JE. Recurrent labral tearing on magnetic resonance imaging is not predictive of diminished participation among National Football League athletes. Arthroscopy. 2018;34(1):66–72. [DOI] [PubMed] [Google Scholar]
- 16. Knapik DM, Gillespie RJ, Salata MJ, Voos JE. Prevalence and impact of glenoid augmentation in American football athletes participating in the National Football League Scouting Combine. Orthop J Sports Med. 2017;5(8):2325967117722945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Knapik DM, Sheehan J, Nho SJ, Voos JE, Salata MJ. Prevalence and impact of hip arthroscopic surgery on future participation in elite American football athletes. Orthop J Sports Med. 2018;6(2):2325967117752307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Larson CM, Sikka RS, Sardelli MC, et al. Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate National Football League prospects. Arthroscopy. 2013;29(3):405–410. [DOI] [PubMed] [Google Scholar]
- 19. LeBus GF, Chahla J, Sanchez G, et al. The Latarjet procedure at the National Football League Scouting Combine: an imaging and performance analysis. Orthop J Sports Med. 2017;5(9):2325967117726045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. [DOI] [PubMed] [Google Scholar]
- 21. Logan CA, Beaulieu-Jones BR, Sanchez G, et al. Posterior cruciate ligament injuries of the knee at the National Football League Combine: an imaging and epidemiology study. Arthroscopy. 2018;34(3):681–686. [DOI] [PubMed] [Google Scholar]
- 22. Logan CA, Murphy CP, Sanchez A, et al. Medial collateral ligament injuries identified at the National Football League Scouting Combine: assessment of epidemiological characteristics, imaging findings, and initial career performance. Orthop J Sports Med. 2018;6(7):2325967118787182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Low K, Noblin JD, Browne JE, Barnthouse CD, Scott AR. Jones fractures in the elite football player. J Surg Orthop Adv. 2004;13(3):156–160. [PubMed] [Google Scholar]
- 24. Mall NA, Matava MJ, Wright RW, Brophy RH. Relation between anterior cruciate ligament graft obliquity and knee laxity in elite athletes at the National Football League Combine. Arthroscopy. 2012;28(8):1104–1113. [DOI] [PubMed] [Google Scholar]
- 25. McHale KJ, Vopat BG, Beaulieu-Jones BR, et al. Epidemiology and outcomes of Lisfranc injuries identified at the National Football League Scouting Combine. Am J Sports Med. 2017;45(8):1901–1908. [DOI] [PubMed] [Google Scholar]
- 26. Moatshe G, Godin JA, Chahla J, et al. Clinical and radiologic outcomes after scaphoid fracture: injury and treatment patterns in National Football League Combine athletes between 2009 and 2014. Arthroscopy. 2017;33(12):2154–2158. [DOI] [PubMed] [Google Scholar]
- 27. Moorman CT, 3rd, Johnson DC, Pavlov H, et al. Hyperconcavity of the lumbar vertebral endplates in the elite football lineman. Am J Sports Med. 2004;32(6):1434–1439. [DOI] [PubMed] [Google Scholar]
- 28. Murphy CP, Frangiamore SJ, Mannava S, et al. Effect of anterior glenoid labral tears and glenoid bone loss at the NFL Combine on future NFL performance. Orthop J Sports Med. 2018;6(7):2325967118784884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Paxton ES, Moorman CT, Chehab EL, Barnes RP, Warren RF, Brophy RH. Effect of hyperconcavity of the lumbar vertebral endplates on the playing careers of professional American football linemen. Am J Sports Med. 2010;38(11):2255–2258. [DOI] [PubMed] [Google Scholar]
- 30. Presciutti SM, DeLuca P, Marchetto P, Wilsey JT, Shaffrey C, Vaccaro AR. Mean subaxial space available for the cord index as a novel method of measuring cervical spine geometry to predict the chronic stinger syndrome in American football players. J Neurosurg Spine. 2009;11(3):264–271. [DOI] [PubMed] [Google Scholar]
- 31. Provencher MT, Bradley JP, Chahla J, et al. A history of anterior cruciate ligament reconstruction at the National Football League Combine results in inferior early National Football League career participation. Arthroscopy. 2018;34(8):2446–2453. [DOI] [PubMed] [Google Scholar]
- 32. Provencher MT, Chahla J, Cinque ME, et al. Symptomatic focal knee chondral injuries in National Football League Combine players are associated with poorer performance and less volume of play. Arthroscopy. 2018;34(3):671–677. [DOI] [PubMed] [Google Scholar]
- 33. Rebolledo BJ, Bernard JA, Werner BC, et al. The association of vitamin D status in lower extremity muscle strains and core muscle injuries at the National Football League Combine. Arthroscopy. 2018;34(4):1280–1285. [DOI] [PubMed] [Google Scholar]
- 34. Schroeder GD, Lynch TS, Gibbs DB, et al. Pre-existing lumbar spine diagnosis as a predictor of outcomes in National Football League athletes. Am J Sports Med. 2015;43(4):972–978. [DOI] [PubMed] [Google Scholar]
- 35. Schroeder GD, Lynch TS, Gibbs DB, et al. The impact of a cervical spine diagnosis on the careers of National Football League athletes. Spine (Phila Pa 1976). 2014;39(12):947–952. [DOI] [PubMed] [Google Scholar]
- 36. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 37. Tu LA, Knapik DM, Sheehan J, Salata MJ, Voos JE. Prevalence of Jones fracture repair and impact on short-term NFL participation. Foot Ankle Int. 2018;39(1):6–10. [DOI] [PubMed] [Google Scholar]
- 38. Vopat B, Beaulieu-Jones BR, Waryasz G, et al. Epidemiology of navicular injury at the NFL Combine and their impact on an athlete’s prospective NFL career. Orthop J Sports Med. 2017;5(8):2325967117723285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]