Abstract
The drug compliance and its associated factors were investigated among hypertensive patients attending the outpatient department of National Institute of Cardiovascular Disease (NICVD), Karachi, from September 2014 to March 2015. Data were collected retrospectively from 300 hypertensive patients taken treatment for >1 year. Half of the patients (51%) were >55 years of age with the predominance of males (52.70%). Most respondents (47%) had had ischemic heart disease (IHD), 30% had diabetes, 47% had both IHD and diabetes, while only a small number of subjects (18%) reporting no comorbidity. Most respondents (82%) reported that they took medicine regularly. Drug compliance was found significantly higher in males (55.70%) as compared with females (44.30%) (P = .025). Similarly, drug compliance was found significantly higher in patients who monitored their blood pressure (BP) regularly (59.30%) as compared with the patients who did not monitor their BP regularly (40.70%) (P = .001). Most respondents (46.30%) with hypertension (HTN) duration ≤5 years had significantly higher drug compliance as compared with the patients with HTN duration of 6 to 10 years and ≥11 years, that is, 33.30% and 20.30%, respectively (P = .018). In conclusion, the rate of drug adherence is not up to the mark in hypertensive patients, with high compliance reported in only half of the respondents.
Keywords: drug/medical use evaluation, adverse drug reactions reporting/monitoring, physician prescribing
Introduction
Hypertension (HTN) is the most prevalent disease worldwide. It is considered as one of the major modifiable risk factors and one of the most important public health problems.1 Chronically, elevation in blood pressure (BP) is associated with high risk of renal, cardiac, and brain damage as well as other medical conditions.2 Due to the morbidity, mortality, and high hospital costs associated with HTN, patient adherence to appropriate treatment is essential.3
The control of BP has a strong correlation to the medication of the patients. Factors such as the lack of knowledge about the disease or motivation to treat a chronic disease, low socioeconomic status, cultural aspects, ineffective relationship with health care team, and cost of medications negatively influence adherence to treatment and consequently quality of life.4 Other factors that may be associated are demographic, clinical, and behavioral factors, in addition to psychological and social factors.
It is clear that controlling of BP in real practice is impossible without proper adherence to the treatment which is not only challenging for the health care professionals but for the patients as well.5,6 In this context, this study sought to determine adherence to antihypertensive drug treatment and to identify factors which cause hurdles in maintaining the compliance of the antihypertensive drugs.
Materials and Methods
Study Design, Study Setting, and Duration
A cross-sectional study was carried out in the outpatient department of National Institute of Cardiovascular Disease (NICVD) from September 2014 to March 2015. We have included an age group of 18 years or older, with a known history of high BP and taking medication more than a year. Signed informed consent was taken from all patients before collection of the data, and the purpose and benefit of the study were explained. It was explained to the patients that inclusion in this study is not a compulsion, and disagreement would not compromise the treatment process which is a basic right.
Data Collection Procedure
The data were prospectively collected from 300 hypertensive patients taking antihypertensive medicines for more than 1 year through a semistructured questionnaire. All information regarding age, gender, systolic blood pressure (SBP), diastolic blood pressure (DBP), duration of HTN, comorbidities, and factors that interfere in adherence to the treatment like discontinuation of medication when symptoms were controlled, forgot to bring medicine when travel or leave home, cut back or stopped taking medicine without informing doctor due to worse feeling after it, and felt hassled about sticking to medicine plan were noted.
Statistical Analysis
All data were entered and analyzed on Statistical Package for Social Sciences (SPSS) version 21. Cleaning and coding of the data were done prior to the analysis. Frequency and percentages were computed for all the qualitative variables. The association between outcome variable (drug compliance) and associated risk factors was determined using the chi-square test. P ≤ .05 was taken as significant.
Results
Baseline characteristics of the patients are shown in Table 1. A majority of the patients (n = 246, 82%) reported taking regular medication for HTN. A large number of patients (n = 133, 44.30%) reported that most of the time they had difficulty in remembering to take medicine, whereas 131 (43.70%) patients never faced any difficulty in remembering. Thirty-one (10.3%) patients occasionally faced any difficulty in remembering to take the medicines, whereas only 5 (1.7%) patients reported that they faced difficulty in remembering to take the medicines all the time (Figure 1). Drug compliance was found significantly higher in males (n = 137, 55.70%) as compared with females (n = 109, 44.30%) (P = .025). Similarly, drug compliance was found significantly higher in the patients who monitored their BP regularly (n = 146, 59.30%) as compared with the patients who did not monitor their BP regularly (n = 100, 40.70%) (P = .001). There was no significant difference in the compliance between younger adults aged <55 years and older adults aged >55 years, with compliance rates being 44.4% and 55.6%, respectively.
Table 1.
Baseline Characteristics of the Patients (N = 300).
| n | % | |
|---|---|---|
| Age (years) | ||
| ≤55 | 147 | 49 |
| >55 | 153 | 51 |
| Gender | ||
| Male | 158 | 52.70 |
| Female | 142 | 47.30 |
| Systolic BP (mm/Hg) | ||
| 100-150 | 196 | 65.30 |
| 160-230 | 104 | 34.70 |
| Diastolic BP (mm/Hg) | ||
| 50-80 | 180 | 60 |
| 90-150 | 120 | 40 |
| Duration of HTN (years) | ||
| ≤5 | 148 | 49.30 |
| 6-10 | 99 | 33 |
| >10 | 53 | 17.70 |
| Monitoring BP | ||
| Yes | 159 | 53 |
| No | 141 | 47 |
| Comorbidities | ||
| Diabetes | 14 | 4.70 |
| IHD | 141 | 47 |
| Diabetes and IHD both | 91 | 30.30 |
| None | 54 | 18 |
| Taking prescribed medicine regularly | ||
| Yes | 246 | 82 |
| No | 54 | 18 |
| Drug therapy | ||
| Monotherapy | 134 | 44.70 |
| Polytherapy | 166 | 55.30 |
| Stopped taking medicine when symptoms were under control | ||
| Yes | 90 | 30 |
| No | 210 | 70 |
| Forgot to bring along your medicines when travel or leave home | ||
| Yes | 140 | 46.70 |
| No | 160 | 53.30 |
| Cut back or stopped taking medicine due to worse feeling after taking it, without informing doctor | ||
| Yes | 94 | 31.30 |
| No | 206 | 64.70 |
| Felt hassled about sticking to your medicine plan | ||
| Yes | 48 | 16 |
| No | 252 | 84 |
Note. BP = blood pressure; HTN = hypertension; IHD = ischemic heart disease.
Figure 1.
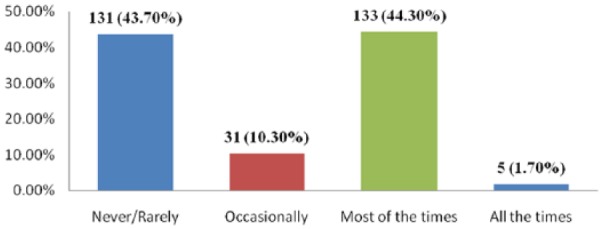
Difficulty in remembering to take all medicines.
A majority of the patients (n = 114, 46.30%) with duration of HTN ≤5 years had significantly higher drug compliance as compared with the patients with duration of HTN 6 to 10 years (n = 82, 33.30%) and ≥11 years (n = 50, 20.30%) (P = .018) (Table 2).
Table 2.
Factors Relating With Drug Compliance (N = 300).
| Taking medicines regularly |
|||||
|---|---|---|---|---|---|
| Yes |
No |
P valuea | |||
| n | % | n | % | ||
| Age (years) | |||||
| ≤55 | 123 | 50 | 24 | 44.40 | 0.460 |
| >55 | 123 | 50 | 30 | 55.60 | |
| Gender | |||||
| Male | 137 | 55.70 | 21 | 38.90 | .025* |
| Female | 109 | 44.30 | 33 | 61.10 | |
| Monitoring BP | |||||
| Yes | 146 | 59.30 | 13 | 24.10 | <0.001** |
| No | 100 | 40.70 | 41 | 75.90 | |
| Comorbidities | |||||
| Diabetes | 13 | 5.30 | 1 | 1.90 | 0.194 |
| IHD | 109 | 44.30 | 32 | 59.30 | |
| Diabetes and IHD both | 79 | 32.10 | 12 | 22.20 | |
| None | 45 | 18.30 | 9 | 1.00 | |
| Duration of HTN (years) | |||||
| ≤5 | 114 | 46.30 | 34 | 63 | .018* |
| 6-10 | 82 | 33.30 | 17 | 31.50 | |
| ≥11 | 50 | 20.30 | 3 | 5.60 | |
Note. BP = blood pressure; IHD = ischemic heart disease; HTN = hypertension.
Chi-square test applied.
p-value <0.05, **p-value <0.001.
Discussion
The findings of this study revealed that almost half of the respondents had good compliance with drug therapy. Similar results were found in a study in which it is reported that belief in the necessity of antihypertensive medication was high among the respondents and the majority believed that it was necessary to take antihypertensive medication even if one does not feel sick.7
The results indicate poor adherence to medication (53%) among patients when they travel or leave home. A possible reason for that could be linked to cultural norms in Pakistan, where people may not want to show that they have a particular medical condition when they are in the public by taking medication.
Thirty percent of the patients reported that they stop taking medicine when symptoms are under control without informing their doctor. They also reported to have cut back or stopped taking medicine due to worse feeling after resuming their medication without informing the doctor. These findings also provide a preliminary insight into the mechanism by which beliefs relating to medication might influence compliance. Some of these findings were similar to those reported in previous studies.8
It is reported that only about one-third of patients knew that HTN should ideally be treated for life, a majority believed that antihypertensive drugs should be used only where there are symptoms, while only a small number of patients believed that the treatment should be for a period of time and not for life.9 It is reported that almost all patients who were hypertensive before treatment became hypertensive again when treatment was stopped. This practice has resulted in high morbidity and mortality in this cohort.7
Our study indicates that male gender, BP monitoring, and duration of HTN more than 5 years were significant factors associated with higher drug compliance. Similar results were found in another study from Karachi, Pakistan; the adherence to antihypertensive drugs is estimated to be around 30% (95% confidence interval [CI]: 22.6%-42.3%). However, age and comorbidities were not significantly associated. Nonetheless, age cannot be discounted as a factor as we did not have the data to further stratify age greater than 65 years with the younger cohort of age below 45 years.10 In future studies, continuous data on age should be collected to run a regression analysis on age and adherence.
Al-Ramahi reported that younger age, living in a village compared with a city, evaluating health, forgetfulness, fear of getting used to medication, adverse effect, and dissatisfaction with treatment were significant factors association with lower levels of medication adherence.11 One central theme that runs through the collected data was the issue of socioeconomic status of the respondents. It is believed that financial hardship is a significant barrier to complying with treatment and is a contributory factor to noncompliance.12 Our study showed that males have a higher compliance as compared with females. A possible reason for this could be concordance, which means that men may have an understanding that as breadwinners they need to look after their health. A major limitation in our study was the lack of data on financial status of the patients. We recommend that further large-scale studies are needed focusing on ethnic, socioeconomic, educational, and psychological factors.
Conclusion
In conclusion, the rate of adherence is not up to the mark in hypertensive patients, with high compliance reported in only half of the respondents. The higher compliance rate was observed in male gender and patients with duration of HTN >11 years.
Acknowledgments
The authors acknowledge Dr. Sultana Habib for her support and guidance in the data collection process.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2004;365:217–223. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. The world health report 2002—reducing risks, promotinghealthy life. Stylus Publishing; 2002. [Google Scholar]
- 3. Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41:1178–1179. [DOI] [PubMed] [Google Scholar]
- 4. Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 5. Black HR, Elliott WJ, Neaton JD, et al. Baseline characteristics and early blood pressure control in the CONVINCE trial. Hypertension. 2001;37:12–18. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization. Adherence to long-term therapies: evidence for action; 2003.
- 7. Osamor PE, Owumi BE. Factors associated with treatment compliance in hypertension in southwest Nigeria. J Health Popul Nutr. 2011;29:619–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Benson J, Britten N. Patients’ decisions about whether or not to take antihypertensive drugs: qualitative study. BMJ. 2002;325:873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Familoni BO, Ogun SA, Aina AO. Knowledge and awareness of hypertension among patients with systemic hypertension. J Natl Med Assoc. 2004;96:620–624. [PMC free article] [PubMed] [Google Scholar]
- 10. Qureshi NN, Hatcher J, Chaturvedi N, Jafar TH. Effect of general practitioner education on adherence to antihypertensive drugs: cluster randomised controlled trial. BMJ. 2007;335(7628):1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Al-Ramahi R. Adherence to medications and associated factors: a cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Isezuo AS, Opera TC. Hypertension awareness among Nigerians in a Nigerian tertiary health institution. Sahel Med J. 2000;3:93–96. [Google Scholar]


