Abstract
Study Design:
A review of a prospective database.
Objectives:
Surgery for elderly patients is increasing yearly due to aging of society and the desire for higher quality of life. The goal of the study was to examine perioperative complications in spine surgery in such patients.
Methods:
A multicenter study of surgical details and perioperative complications was performed in 35 patients aged older than 90 years who underwent spinal surgery, based on a review of a prospective database. The frequency and severity of complications were assessed, and the effects of patient-specific and surgical factors were examined. Major complications were defined as those that were life threatening, required reoperation in the perioperative period or left a permanent injury. Ambulatory function before and after surgery was also analyzed.
Results:
Perioperative complications occurred in 19 of the 35 cases (54%), and included 11 cases of postoperative delirium, most of which occurred after cervical spine surgery. There were 8 major complications (23%), including cerebral infarction (n = 3), coronary heart disease (n = 3), pulmonary embolism (n = 1), and angina (n = 1). Preoperative motor deficit, operative time, estimated blood loss, and instrumented fusion were significantly associated with major complications. An improved postoperative ambulatory status occurred in 61% of cases, with no change in 33%, and worsening in 2 cases (6%).
Conclusions:
Timing of surgery before paralysis progression and reduced surgical invasiveness are important considerations in treatment of the very elderly. Improved outcomes can be obtained with better management of spine surgery for patients aged 90 years or older.
Keywords: complications, spine surgery, elderly patients, older than 90 years, multicenter study
Introduction
Japanese society is progressively aging and there are now 9.64 million people aged more than 80 years in Japan, accounting for 7.6% of the total population in 2014. This number is 1.5 times higher than 10 years ago, 2.4 times higher than 20 years ago, and 4.2 times higher than 30 years ago. In addition, 1.72 million people are more than 90 years of age, accounting for 1.4% of the population.1 The combination of an aging society and recent advances in surgical techniques and anesthesia have increased the demand for spinal surgery in elderly patients and has also increased surgeries performed for higher quality of life.
Many studies have reported perioperative complications in elderly patients, but generally the term “elderly” is accepted to mean a chronological age of 65 years.2–4 In contrast, there are only a few similar reports in very elderly patients,5–8 which normally means patients older than 80 years, and none have focused only on patients aged 90 years or older. Therefore, in this study, we performed a retrospective review of a prospective database of surgical details and perioperative complications in spine surgery for elderly patients aged 90 years or older. The frequency and severity of complications, patient and surgical factors, and ambulatory function before and after surgery were analyzed in the study.
Materials and Methods
From January 2008 to December 2013, data for 35 patients aged ≥90 years old who underwent spinal surgeries at 10 facilities associated with our group was examined in a retrospective study. The average follow-up period was 22 months (range 12-37 months). This study was approved by the Ethics Committee of our hospital (IRB No. 354-3). The characteristics of the patients are shown in Table 1. Fourteen patients were male and 21 were female. Age ranged from 90 to 98 years, with a mean of 91.3 years old. Preoperatively, nonsteroidal anti-inflammatory drugs were taken in 12 cases as a conservative approach to pain, and preoperative physiotherapy was performed in 6 cases with lumbar spinal stenosis. All cases were primary operations. The mean operative time was 87 minutes, mean estimated blood loss (EBL) was 120 mL, and there were 7 fusion surgeries with instrumentation (Table 1). Surgeries were performed with instrumentation of combined screws with hooks and ultra-high-molecular-weight polyethylene tape due to osteoporosis. Surgical lesions and diseases are shown in Table 2.
Table 1.
Characteristics of the 35 Cases in the Study.
| Item | Value |
|---|---|
| Demographics | |
| Age, years, mean (range) | 91.3 (90-98) |
| Gender, male/female, n | 14/21 |
| Previous spinal surgery, n | 0 |
| Body mass index, kg/m2, mean (range) | 21.3 (14-26) |
| Comorbidities, n (%) | |
| Hypertension | 14 (40) |
| Coronary heart disease | 9 (26) |
| Diabetes | 8 (23) |
| Cerebrovascular disease | 7 (20) |
| Preoperative motor loss (manual muscle test < 4) | 6 (17) |
| Operative factors | |
| Operative time, minutes, mean (range) | 87 (19-333) |
| Estimated blood loss, mL, mean (range) | 120 (10-800) |
| Fusion with instrumentation, n (%) | 7 (20) |
Table 2.
Surgical Lesions and Diseases in 35 Cases.
| Lesion and Disease | Number of Cases (%) |
|---|---|
| Lesion | |
| Cervical | 11 (31) |
| Thoracic | 9 (26) |
| Lumbar | 15 (43) |
| Disease | |
| Lumbar spinal stenosis | 11 (31) |
| Cervical spondylotic myelopathy | 10 (29) |
| Thoracic-lumbar compression fracture | 9 (26) |
| Chance fracture of diffuse idiopathic skeletal hyperostosis | 3 (9) |
| Meningioma | 1 (3) |
| Lumbar spinal spondylolisthesis | 1 (3) |
| Type of procedure | |
| Cervical laminoplasty | 10 (29) |
| Balloon kyphoplasty | 9 (26) |
| Lumbar decompression | 8 (23) |
| Posterior fusion | 6 (17) |
| Posterior lumbar interbody fusion | 1 (3) |
| Tumor excision | 1 (3) |
Ambulatory function preoperatively and 6 months postoperatively was rated on a 4-point scale (4, independent; 3, requiring a cane; 2, requiring a walker; and 1, wheelchair bound). Medical comorbidities were evaluated using the method described by Charlson et al9 (Table 3).
Table 3.
Summary of the Charlson Comorbidity Index.
| Comorbidity | Relative Weight Assignment |
|---|---|
| Metastatic solid tumor | 6 |
| Acquired immune deficiency syndrome (AIDS) | 6 |
| Moderate-to-severe liver disease | 3 |
| Hemiplegia | 2 |
| Moderate- to-severe renal failure | 2 |
| Diabetes with end organ damage | 2 |
| Neoplasia | 2 |
| Leukemia/lymphoma | 2 |
| Myocardial infarct | 1 |
| Congestive heart failure | 1 |
| Peripheral vascular disease | 1 |
| Cerebrovascular disease | 1 |
| Dementia | 1 |
| Chronic pulmonary disease | 1 |
| Connective tissue disease | 1 |
| Ulcer | 1 |
| Mild liver disease | 1 |
| Diabetes | 1 |
All adverse events and major complications that occurred within 3 months after surgery were defined as postoperative complications. Major complications were defined as those that were life threatening, required reoperation in the perioperative period, or left a permanent deficit, including cardiac, urinary and renal, and wound-related complications.10,11 To assess risk factors for postoperative complications, age, gender, body mass index (BMI), comorbidities, and operative factors were compared in patients with and without complications.
Differences between 2 groups were analyzed by Mann-Whitney U test or Student t test, and those among 3 groups were analyzed by Kruskal-Wallis test. All statistical analyses were conducted using SPSS version 22 for Windows (IBM Corp, Armonk, NY). P < .05 was considered to be significant in all analyses.
Results
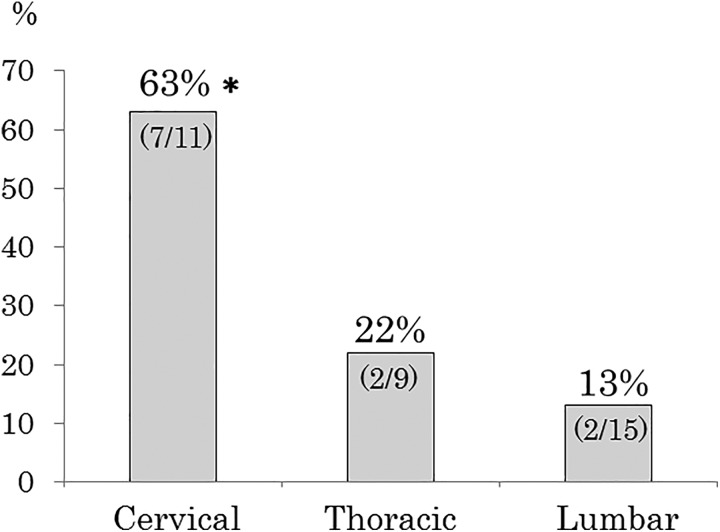
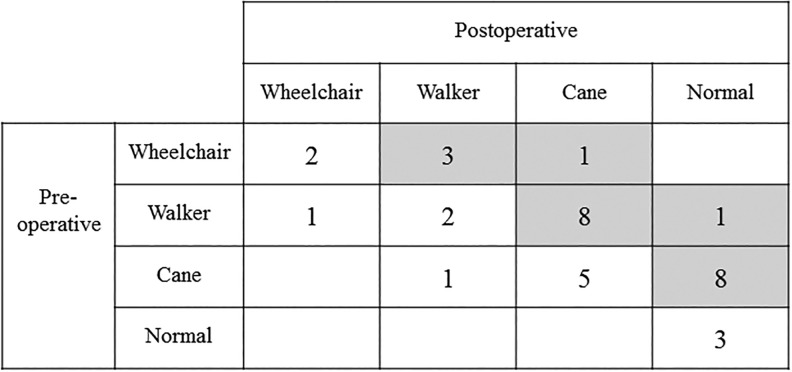
Postoperative complications occurred in 19 of the 35 cases (54%) and included 11 cases of postoperative delirium. Details are shown in Table 4. One of these patients died due to coronary heart disease on the second day after surgery. Delirium was significantly associated with cervical spine surgery (Figure 1), and delirium and preoperative motor loss also had a significant association (P < .05, Table 5). Of the 31 patients with preoperative gait disturbance requiring assistive devices, the status improved by at least 1 point on the ambulatory scale in 61%, was unchanged in 33%, and worsened by 1 point in 6% (Figure 2). Both cases with worsened gait had cerebral infarction postoperatively, and as a result hemiplegia remained and ambulatory status worsened.
Table 4.
Details of Perioperative Complications in 19 Patients.
| Complication | Number of Cases |
|---|---|
| Delirium | 11 |
| Major complications (n = 8) | |
| Cerebral infarction | 3 |
| Coronary heart disease | 3 |
| Pulmonary embolism | 1 |
| Angina | 1 |
Figure 1.
Rates of postoperative delirium in patients with different surgical lesions. *P < .05 versus thoracic or lumbar lesions.
Table 5.
Relationship Between Delirium and Preoperative Motor Loss.a
| Delirium (n = 11) | ||
|---|---|---|
| + | − | |
| Preoperative motor loss + | 67% (4/6) | 23% (7/29) |
a P < .05.
Figure 2.
Pre- and postoperative ambulatory status. The gray area shows an improved status after surgery.
A comparison of patients with and without a major complication is shown in Table 6. Preoperative motor deficit (P = .015), comorbidity index score (P = .075), operative time (P = .047), EBL (P = .048), and fusion surgery with instrumentation (P = .015) were all associated with major complications, and length of hospital stay was significantly longer for patients with major complications (P = .046).
Table 6.
Comparison of Background Data in Patients With and Without Major Complications.
| Item | With Major Complication (n = 8) | Without Major Complication (n = 27) | P |
|---|---|---|---|
| Demographics | |||
| Female, % (n) | 75 (5) | 56 (15) | NS |
| Body mass index, kg/m2, mean ± SD | 21.5 ± 4.4 | 21.2 ± 2.6 | NS |
| Comorbidities, % (n) | |||
| More than 1 comorbidity | 75 (5) | 59 (16) | NS |
| Hypertension | 25 (2) | 52 (14) | NS |
| Coronary heart disease | 38 (3) | 22 (6) | NS |
| Diabetes | 25 (2) | 22 (6) | NS |
| Cerebrovascular disease | 25 (2) | 19 (5) | NS |
| Preoperative motor loss (MMT < 4) | 50 (4) | 11 (3) | .015 |
| Comorbidity index score | 2.0 | 1.3 | .075 |
| Perioperative factors | |||
| Cervical lesion, % (n) | 25 (2) | 33 (9) | NS |
| Operative time, minutes, mean ± SD | 119 ± 40 | 80 ± 63 | .047 |
| Estimated blood loss, mL, mean ± SD | 257 ± 239 | 92 ± 121 | .048 |
| Fusion with instrumentation, % (n) | 50 (4) | 11 (3) | .015 |
| Perioperative outcome | |||
| Length of hospital stay, days,a mean ± SD | 51 ± 21 | 30 ± 20 | .046 |
| Death, % (n) | 13 (1) | 0 (0) | NS |
Abbreviation: MMT, manual muscle test; NS, not significant.
a Excluding 1 patient who died.
Discussion
Based on 2013 data in Japan, life expectancy at birth was 84 years for both sexes, which is the greatest longevity of any country worldwide.12 In 1990, this age was 79 years, and thus aging of society is progressing rapidly. In recent years, these changes have increased the demand for spinal surgery in elderly patients.7,8
Elderly patients older than 65 years have major postoperative complications at rates of 3% to 29%,12–20 and risk factors for these complications include increased age, comorbidities, blood loss, operative time, and number of levels.8,11,15,21 Studies in the very elderly, which generally indicates patients aged ≥80 years,5,7,8,22,23 have shown complication rates of 20% with length of intensive care unit stay as a risk factor23 and 26% without mortality in lumbar decompression surgery, which was concluded to be safe and effective.22 In the current report, which is the first to focus on patients aged 90 years or older, the rates of perioperative and major complications were 54% and 23%, respectively. In a previous multicenter study in Japan, Yone at al24 found a morbidity rate of 10.4% in more than 30 000 spinal surgeries in patients of all ages. Therefore, patients aged ≥90 years are at a higher risk for complications after spine surgery, with a rate 5.2 times higher than that for patients of all ages.
In our series, delirium was the most common among postoperative complications. Previous studies have also found that postoperative delirium occurs commonly in very elderly patients and is associated with a significant increase in mortality-related complications such as cerebrovascular disease, length of hospital stay, and admission to a long care facility.25–27 Postoperative delirium is characterized by acute onset with fluctuations in neuropsychiatric function, inattention, disorganized thinking, and altered levels of consciousness.28 The frequency of delirium after head and neck surgery is 17% to 36%,29–33 and delirium generally includes hallucinations, illusions, mental excitement, and disorientation. Delirium may also lead to fractures due to fall and discontinuous treatment due to intravenous drip removal. In our series of patients aged 90 or older, delirium occurred at a rate of 31%, which is consistent with previous reports, and was significantly associated with cervical surgery.
Preoperative motor deficit results in worsened ambulatory ability and causes a vulnerable condition of the spinal cord. This may lead to poorer postoperative recovery and a longer period of time in bed, which may then worsen the general condition. In our series, cases with preoperative motor deficit had a significantly higher complication rate. These results show that appropriate timing of surgery prior to worsening of paralysis is important for good recovery after surgery. The postoperative ambulatory score improved in 61% of cases and worsened in only 6%; therefore, improvement can be obtained with careful surgery and management in patients aged 90 years or older. In particular, cases with no muscle weakness or a slight motor deficit (manual muscle test ≥4) and few comorbidities (comorbidity index ≤1), have a reduced risk of complications and this might be an indication for surgery. A surgical plan with a short operative time and avoidance of implant use to reduce invasiveness may also help avoid postoperative complications.
There are several limitations in the study, including the small number of cases, exclusion of patients who could not undergo surgery due to a poor general condition, and the absence of long-term follow-up and information on long-term outcome. Despite these limitations, the results provide important information on morbidity and mortality after spinal surgery in very elderly patients.
In summary, the incidence of postoperative complications after spine surgery was 54% in very elderly patients aged 90 years or older. These complications were mostly delirium and were significantly associated with cervical lesions. The rate of major complications that were potentially life threatening and extended the hospitalization period was 23%. A preoperative motor deficit, operative time, EBL, and fusion surgery with instrumentation were significant risk factors for major complications. These findings indicate that timing of the surgical procedure prior to worsening of paralysis is an important consideration in surgery for very elderly patients, in addition to reduction of surgical invasiveness.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Statistics Bureau. The 64th Japan statistical yearbook 2015. http://www.stat.go.jp/english/data/nenkan/back64/index.htm. Accessed March 8, 2018.
- 2. Gorman M. Development and the rights of older people In: Randel EJ, German T, Ewing D, eds. The Ageing and Development Report: Poverty, Independence and the World’s Older People. London, England: Earthscan; 1999:3–21. [Google Scholar]
- 3. Roebuck J. When does “old age begin?”: the evolution of the English definition. J Soc Hist. 1979;12:416–428. [Google Scholar]
- 4. Thane P. History and the sociology of ageing. Soc Hist Med. 1989;2:93–96. [Google Scholar]
- 5. Bydon M, Abt NB, De la Garza-Ramos R, et al. Impact of age on short-term outcomes after lumbar fusion: an analysis of 1395 patients stratified by decade cohorts. Neurosurgery. 2015;77:347–353. [DOI] [PubMed] [Google Scholar]
- 6. Li G, Patil CG, Lad SP, Ho C, Tian W, Boakye M. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine (Phila Pa 1976). 2008;33:1250–1255. [DOI] [PubMed] [Google Scholar]
- 7. Sciubba DM, Scheer JK, Yurter A, et al. ; the International Spine Study Group (ISSG). Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J. 2016;25:2433–2441. [DOI] [PubMed] [Google Scholar]
- 8. Wang MY, Green BA, Shah S, Vanni S, Levi AD. Complications associated with lumbar stenosis surgery in patients older than 75 years of age. Neurosurg Focus. 2003;14:e7. [DOI] [PubMed] [Google Scholar]
- 9. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 10. Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J. 2003;3:496–501. [DOI] [PubMed] [Google Scholar]
- 11. Imagama S, Kawakami N, Tsuji T, et al. Perioperative complications and adverse events after lumbar spinal surgery: evaluation of 1012 operations at a single center. J Orthop Sci. 2011;16:510–515. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization. World health statistics 2015. http://www.who.int/gho/publications/world_health_statistics/EN_WHS2015_TOC.pdf. Accessed March 8, 2018.
- 13. Benz RJ, Ibrahim ZG, Afshar P, Garfin SR. Predicting complications in elderly patients undergoing lumbar decompression. Clin Orthop Relat Res. 2001;(384):116–121. [DOI] [PubMed] [Google Scholar]
- 14. Best NM, Sasso RC. Outpatient lumbar spine decompression in 233 patients 65 years of age or older. Spine (Phila Pa 1976). 2007;32:1135–1139. [DOI] [PubMed] [Google Scholar]
- 15. Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A(11):2089–2092. [DOI] [PubMed] [Google Scholar]
- 16. Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 17. Johnsson KE, Rosén I, Udén A. The natural course of lumbar spinal stenosis. Clin Orthop Relat Res. 1992;(279):82–86. [PubMed] [Google Scholar]
- 18. Katz JN, Lipson SJ, Larson MG, McInnes JM, Fossel AH, Liang MH. The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am. 1991;73:809–816. [PubMed] [Google Scholar]
- 19. Quigley MR, Kortyna R, Goodwin C, Maroon JC. Lumbar surgery in the elderly. Neurosurgery. 1992;30:672–674. [PubMed] [Google Scholar]
- 20. Smith EB, Hanigan WC. Surgical results and complications in elderly patients with benign lesions of the spinal canal. J Am Geriatr Soc. 1992;40:867–870. [DOI] [PubMed] [Google Scholar]
- 21. Cassinelli EH, Eubanks J, Vogt M, Furey C, Yoo J, Bohlman HH. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976). 2007;32:230–235. [DOI] [PubMed] [Google Scholar]
- 22. Galiano K, Obwegeser AA, Gabl MV, Bauer R, Twerdy K. Long-term outcome of laminectomy for spinal stenosis in octogenarians. Spine (Phila Pa 1976). 2005;30:332–335. [DOI] [PubMed] [Google Scholar]
- 23. Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976). 2006;31:99–103. [DOI] [PubMed] [Google Scholar]
- 24. Yone K, Imajo Y, Iguchi T, et al. Nationwide survey on complications of spine surgery in Japan. J Spine Res. 2013;4:462. [Google Scholar]
- 25. Gosselt AN, Slooter AJ, Boere PR, Zaal IJ. Risk factors for delirium after on-pump cardiac surgery: a systematic review. Crit Care. 2015;19:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kratz T, Heinrich M, Schlauß E, Diefenbacher A. Preventing postoperative delirium: a prospective intervention with psychogeriatric liaison on surgical wards in a general hospital. Dtsch Arztebl Int. 2015;112:289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mouchoux C, Rippert P, Duclos A, et al. Impact of a multifaceted program to prevent postoperative delirium in the elderly: the CONFUCIUS stepped wedge protocol. BMC Geriatr. 2011;11:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Montes DM. Postoperative delirium in head and neck cancer patients: a survey of oncologic oral and maxillofacial surgeon practices. J Oral Maxillofac Surg. 2014;72:2591–2600. [DOI] [PubMed] [Google Scholar]
- 29. Kunimatsu T, Misaki T, Hirose N, et al. Postoperative mental disorder following prolonged oral surgery. J Oral Sci. 2004;46:71–74. [DOI] [PubMed] [Google Scholar]
- 30. Shah S, Weed HG, He X, Agrawal A, Ozer E, Schuller DE. Alcohol-related predictors of delirium after major head and neck cancer surgery. Arch Otolaryngol Head Neck Surg. 2012;138:266–271. [DOI] [PubMed] [Google Scholar]
- 31. Shiiba M, Takei M, Nakatsuru M, et al. Clinical observations of postoperative delirium after surgery for oral carcinoma. Int J Oral Maxillofac Surg. 2009;38:661–665. [DOI] [PubMed] [Google Scholar]
- 32. Weed HG, Lutman CV, Young DC, Schuller DE. Preoperative identification of patients at risk for delirium after major head and neck cancer surgery. Laryngoscope. 1995;105:1066–1068. [DOI] [PubMed] [Google Scholar]
- 33. Yamagata K, Onizawa K, Yusa H, Wakatsuki T, Yanagawa T, Yoshida H. Risk factors for postoperative delirium in patients undergoing head and neck cancer surgery. Int J Oral Maxillofac Surg. 2005;34:33–36. [DOI] [PubMed] [Google Scholar]