Abstract
Study Design:
Retrospective analysis of prospectively collected data.
Objective:
The aim of the study was to compare the outcome of anterior cervical decompression and fusion (ACDF) with stand-alone tricortical iliac crest autograft versus stand-alone polyetheretherketone (PEEK) cage in cases of cervical spondylotic myelopathy.
Methods:
Prospectively collected data of 60 patients in each group were compared.
Results:
There was statistically significant improvement noted in postoperative Modified Japanese Orthopaedic Association (MJOA) follow-up scores with comparison pairs of preoperative versus 6 months, preoperative versus 1 year, and 3 months versus 6 months, 3 months versus 1 year in both groups. But improvements in MJOA scores were statistically insignificant between 6 months and 1 year (P = .0639) for the autograft group when compared with PEEK cage group (P = 0001). The mean loss of segmental lordosis on follow-up X-ray for the autograft group was (5.89 ± 2.90°), which was significantly higher (1.88 ± 2.77°) than the mean loss seen in the PEEK cage group (P = .01). This was most evident between 6 months and 1 year, resulting in plateauing of the improvement in MJOA score between 6 months to 1 year in the autograft group. While there was no statistical difference between fusion rates between the groups for 1 and 2 levels of ACDF, overall fusion rates were significantly better for 1-level ACDF (95.74%) when compared with 2-level ACDF (76.00%).
Conclusion:
ACDF with PEEK cage is the fusion technique of choice for cervical fusion with fewer complications and better functional recovery in the treatment of cervical spondylotic myelopathy.
Keywords: cervical myelopathy, ACDF, PEEK cage, cervical fusion, bone graft
Introduction
Degenerative cervical disease or cervical spondylosis refers to age-related degenerative changes within the cervical column. Approximately 25% of the individuals <40 years of age, 50% of individuals more than 40 years of age, and 85% of individuals over 60 years of age have some degree of disc degeneration.1 Cervical spondylotic myelopathy results due to degenerative changes in cervical spine leading to cervical stenosis and cord dysfunction. Anterior cervical decompression and fusion (ACDF) is the standard treatment option for the management of degenerative cervical spondylotic myelopathy with good short- and long-term outcome.2-4 The goal of surgery is to decompress the spinal cord and nerve roots while providing a stable spine and to restore segmental alignment. ACDF using iliac crest autograft still remains the gold standard with good functional outcome in these patients. But donor site morbidity remains a concern with the use of iliac crest autograft.5,6 Many artificial materials have been used, such as tantalum blocks, titanium, carbon fiber, and polyetheretherketone (PEEK), as interbody support in ACDF.7,8 PEEK cages have emerged as the implant of choice for interbody graft in ACDF. A recent Cochran review has suggested no functional or radiological difference or advantage of using an additional anterior plate for single- or double-level ACDF.8 Our institution also uses only stand-alone interbody graft for all cases of nontraumatic cervical fusion for 1- and 2-level ACDF. In spite of plethora of evidence in the literature, the choice of one graft material over another remains controversial. The aim of the study was to compare the functional and radiological outcomes of ACDF while using the 2 most popular interbody grafts, tricortical iliac crest autograft versus PEEK cage, in the management of cervical spondylotic myelopathy.
Material and Methods
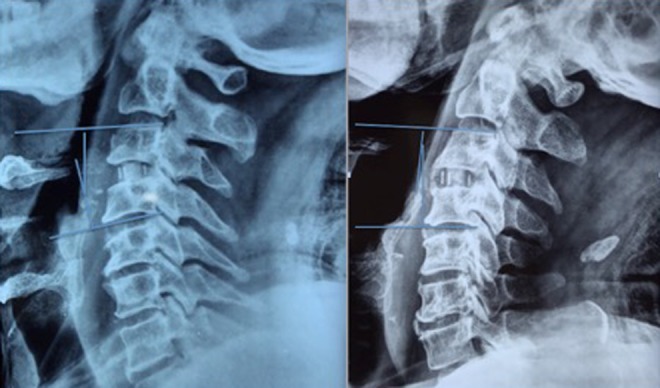
Prospectively collected data of all patients of cervical spondylotic myelopathy who underwent ACDF with stand-alone tricortical iliac crest autograft between December 2011 and December 2013 were directly compared with patients who underwent ACDF with stand-alone PEEK cages filled with ChronOS (synthetic β-tricalcium phosphate;DePuy Synthes) between January 2014 and March 2017. All the patients before December 2014 were operated using stand-alone tricortical iliac crest autograft, and from January 2014 onwards, our center started using stand-alone PEEK cages as interbody graft in ACDF to avoid graft site morbidity associated with autografts. Only patients who underwent 1 or 2 levels of ACDF and with more than 1-year follow-up were included in the study. Sixty cases from each group were finally included in the study design. All cases were operated using anterior approach under fluoroscopic guidance by a single team of experienced surgeons. Modified Japanese Orthopaedic Association (MJOA) scoring was done preoperatively and postoperatively at 3 months, at 6 months, and at 1 year to assess functional outcome for all the cases. Data was collected by direct observations as per the performance. Sequential follow-up radiographs of the cervical spine (anteroposterior, lateral and flexion extension) were done postoperatively, and at 3 months, 6 months, and 1-year follow-up to assess cervical spine alignment and fusion. Additional computed tomography scan was done in the PEEK cage group at 1-year follow-up to confirm fusion (Figure 1). Two authors blinded to clinical data did independent assessment on 2 separate occasion for fusion and graft subsidence based on the follow-up X-rays and computed tomography scans. Graft subsidence was further assessed by comparing the sequential follow-up X-rays. Fusion rate was assessed at 1-year follow-up based on <1 mm of motion between spinous proceeds on flexion extension X-rays by presence of bony trabeculae between bone end plates and by formation of bridging bone anterior or posterior to cage (PEEK) across the end plates.9,10 The association between 2 variables was done using χ2 test. Comparison of mean between 2 fusion groups was done with unpaired t test, and comparison of mean values of MJOA scores at different time intervals was done with repeated-measures ANOVA (analysis of variance), and multiple comparison within groups was done with Sidak test. P value less than .05 was considered significant.
Figure 1.

Good evidence of bony fusion on flexion extension view with <1 mm of motion between spinous proceeds of C5-C6 at 150% magnification.
Results
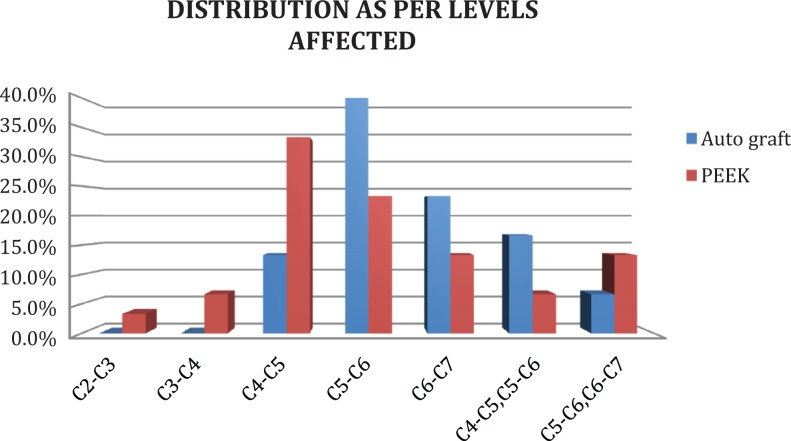
Most of patients in the study were in the age group of 40 to 59 years (n = 84, 70%). The mean age in the autograft group was 51.07 ± 9.39 years compared with 47.3 ± 9.3 years in the PEEK cage group (Table 1). Sixty percent of patients in both the groups were male (n = 36). In the autograft group, 36.7% (n = 22) presented with signs and symptoms of myelopathy alone and 63.3% (n = 38) presented with signs and symptoms of myelopathy and radiculopathy, while in the PEEK cage group this distribution was 30.0% (n = 18) and 70.0% (n = 42), respectively. The mean duration of symptoms in months till surgery in the autograft group was 3.63 ± 2.56 months, while in the PEEK cage group it was 4.3 ± 2.98 months. Difference of duration of symptoms in both groups was not statistically significant. A total of 78.3% (n = 94) of the patients was operated for single-level ACDF, while 21.7% (n = 26) underwent 2 levels of ACDF (Figure 2). The most common comorbidity was diabetes in 25 (21.00%) patients followed by hypertension in 23 (19.16%). Incidence of diabetes and hypertension was not different between the 2 groups (P = .67 and P = .63). History of smoking or use of tobacco was seen in 18 patients (15%). Incidence of smoking or use of tobacco was similar in both the groups.
Table 1.
Comparison of Results Between the 2 Groups.
| Autograft | PEEK Cage | P | |
|---|---|---|---|
| Age (years) | 51.07 ± 9.39 | 47.3 ± 9.3 | >.05 |
| Duration of symptoms (months) | 3.63 ± 2.56 | 4.3 ± 2.98 | >.05 |
| Smokers (number of patients) | 9 | 9 | >.05 |
| Preoperative MJOA score | 12.40 ± 3.68 | 10.83 ± 3.01 | >.05 |
| Intraoperative blood loss (mL) | 146.33 ± 63.19 | 133.17 ± 35.46 | >.05 |
| Anesthesia time (minutes) | 120.67 ± 31.94 | 116.00 ± 26.98 | >.05 |
| Loss of segmental lordosis on follow-up X-ray | 5.89 ± 2.90° | 1.88 ± 2.77° | <.05 |
| Perioperative complication in patients | 18 | 4 | <.05 |
Abbreviations: PEEK, polyetheretherketone; MJOA, Modified Japanese Orthopaedic Association.
Figure 2.
Distribution of cases as per levels affected.
The mean preoperative MJOA score in the autograft group was 12.40 ± 3.68, while in PEEK group it was 10.83 ± 3.01. The mean intraoperative blood loss in the autograft group was 146.33 ± 63.19 mL, while in PEEK group it was 133.17 ± 35.46 mL. The mean time taken for anesthesia was 120.67 ± 31.94 minutes in the autograft group, while it was 116.00 ± 26.98 minutes in the PEEK cage group. On statistical analysis, there was no significant difference between the 2 groups while comparing preoperative MJOA scores (P = .077), the mean intraoperative blood loss (P = .324), or the mean time taken for anesthesia (P = .543).
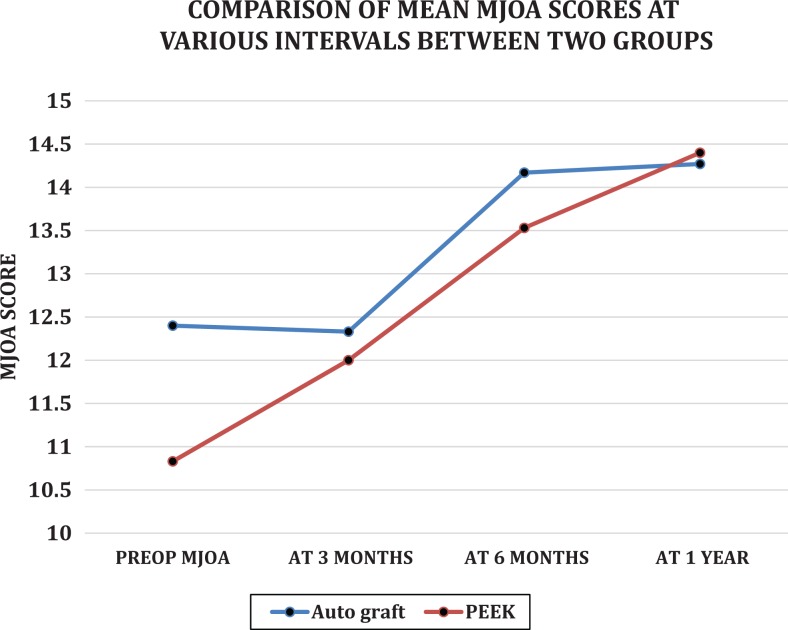
On comparisons of MJOA scores at various time intervals (see Tables 2 –5), there was statistically significant differences noted at various time intervals in postoperative MJOA scores at 3 months, 6 months, and 1 year. There was statistically significant difference noted with comparison pairs of preoperative versus 6 months, preoperative versus 1 year, and 3 months versus 6 months, 3 months versus 1 year. Similarly, on comparison of MJOA score at various time intervals among the PEEK cage cases, there was statistically significant difference noted at various time intervals in postoperative MJOA scores at 3 months, 6 months, and 1 year. There was statistically significant difference noted with comparison pairs of preoperative versus 3 months, preoperative versus 6 months, preoperative versus 1 year, 3 months versus 6 months, 3 months versus 1 year, and 6 months versus 1 year (Figure 3).
Table 2.
Comparison of MJOA Score at Various Time Intervals Among the Cases in the Autograft Group.
| Autograft | Mean | SD | P |
|---|---|---|---|
| Preoperative MJOA | 12.40 | 3.682 | .0001* |
| Postoperative MJOA at 3 months | 12.33 | 4.020 | |
| Postoperative MJOA at 6 months | 14.17 | 4.316 | |
| Postoperative MJOA at 1 year | 14.27 | 4.586 |
Abbreviation: MJOA, Modified Japanese Orthopaedic Association.
* Significant.
Table 3.
All Pairwise Multiple Comparison Procedures in the Autograft Group.
| Mean Difference | P | ||
|---|---|---|---|
| Preoperative MJOA | Postoperative MJOA at 3 months | 0.067 | .865 |
| Postoperative MJOA at 6 months | −1.767 | .0001* | |
| Postoperative MJOA at 1 year | −1.867 | .0001* | |
| At 3 months | Postoperative MJOA at 6 months | −1.833 | .0001* |
| Postoperative MJOA at 1 year | −1.933 | .0001* | |
| At 6 months | Postoperative MJOA at 1 year | −0.100 | .639 |
Abbreviation: MJOA, Modified Japanese Orthopaedic Association.
* Significant.
Table 4.
Comparison of MJOA Score at Various Time Intervals Among the Cases in the PEEK Cage Group.
| Autograft | Mean | SD | P |
|---|---|---|---|
| Preoperative MJOA | 10.83 | 3.018 | .0001* |
| Postoperative MJOA at 3 months | 12.00 | 3.107 | |
| Postoperative MJOA at 6 months | 13.53 | 3.235 | |
| Postoperative MJOA at 1 year | 14.40 | 3.410 |
Abbreviations: MJOA, Modified Japanese Orthopaedic Association; PEEK, polyetheretherketone.
* Significant.
Table 5.
All Pairwise Multiple Comparison Procedures in the PEEK Cage Group.
| Mean Difference | P | ||
|---|---|---|---|
| Preoperative MJOA | Postoperative MJOA at 3 months | −1.167 | .0001* |
| Postoperative MJOA at 6 months | −2.700 | .0001* | |
| Postoperative MJOA at 1 year | −3.567 | .0001* | |
| At 3 months | Postoperative MJOA at 6 months | −1.533 | .0001* |
| Postoperative MJOA at 1 year | −2.400 | .0001* | |
| At 6 months | Postoperative MJOA at 1 year | −.867 | .0001* |
Abbreviations: PEEK, polyetheretherketone; MJOA, Modified Japanese Orthopaedic Association.
* Significant.
Figure 3.
Graph showing the mean Modified Japanese Orthopaedic Association (MJOA) scores at various time intervals.
Among the 94 patients who underwent single-level noninstrumented ACDF, only 4 (4.25%) had pseudarthrosis. The fusion rate for single-level ACDF in our series was 95.74% (Figures 1 and 4). Among the 25 patients operated for 2-level noninstrumented ACDF, 6 patients (24.00%) had pseudarthrosis. The fusion rate for 2-level ACDF in our series was 76.00%. There was no significant difference in fusion rates of the PEEK cage group when compared with the autograft group. Both the groups showed better fusion for single-level ACDF. Both the groups showed graft subsidence and loss of segmental lordosis on follow-up X-rays. The mean loss of segmental lordosis on follow-up X-ray for the autograft group was 5.89 ± 2.90°, which was significantly higher (1.88 ± 2.77°) than the mean loss seen in the PEEK cage group (P = .01). Cage subsidence and loss of segmental lordosis was most obvious in the autograft group between 6 months and 1 year (Figures 5 and 6). Subsidence and loss of segmental lordosis was more in 2-level ACDF compared with 1-level ACDF.
Figure 4.

Confirmation of bony fusion between C5 and C6 by presence of bony trabeculae between bone and cage and by formation of bridging bone posterior to cage across the end plates on computed tomography scan.
Figure 5.

Graft subsidence and loss of segmental lordosis on follow-up X-rays for anterior cervical decompression and fusion C6-C7 with autograft.
Figure 6.
Graft subsidence and loss of segmental lordosis on follow-up X-rays for anterior cervical decompression and fusion C3-C4 with polyetheretherketone cage.
Residual severity of symptoms was studied at 1-year follow-up according to MJOA scorings (Table 6). Residual severity of mild grade was more in the PEEK group (56.7%) as compared with the autograft group (46.7%), while severe grade was less in the PEEK age group (13.3%) when compared with the autograft group (26.7%), but this difference was not statistically significant.
Table 6.
Comparison of Residual Severity of Function in Both the Groups.
| Residual Severity of Function | Groups | Total | ||
|---|---|---|---|---|
| Autograft | PEEK | |||
| Mild | Count | 28 | 34 | 62 |
| % | 46.7% | 56.7% | 51.7% | |
| Moderate | Count | 2 | 8 | 10 |
| % | 3.3% | 13.3% | 8.3% | |
| Severe | Count | 16 | 8 | 24 |
| % | 26.7% | 13.3% | 20.0% | |
| No | Count | 14 | 10 | 24 |
| % | 23.3% | 16.7% | 20.0% | |
| Total | Count | 60 | 60 | 120 |
| % | 100.0% | 100.0% | 100.0% | |
| χ2 = 0.08a; df = 1; P = .77 | ||||
Abbreviation: PEEK, polyetheretherketone.
a Using pooled data.
In our study, perioperative complications like dysphagia, hoarseness, and neck pain and graft subsidence were more in the autograft group. In the autograft group, 18 patients had perioperative complications compared with 4 patients in the PEEK cage group, and the most common perioperative complication was dysphagia in 11 patients while hoarseness was seen in 10 patients. Donor site complications like donor site pain was seen in 10 patients while donor site hematoma was seen in one patient. These complications were more commonly noted with 2-level ACDF when compared with 1-level ACDF.
Discussion
Treatment of cervical spondylotic myelopathy and ideal fusion technique continues to remain a mystery in spite of plethora of evidence in the literature. Even recent studies and Cochrane reviews have failed to establish the rational of using one fusion graft over others.11-14 We have conducted a comparative study to assess the functional and radiological outcome of cervical fusion with tricortical iliac crest autograft versus PEEK cage. In present study while the mean age and age distribution of patients was comparable in both groups, most of patients were seen in the age group of 40 to 59 years (n = 84, 70%). Incidence of comorbidities and smoking was comparable between the 2 groups. The mean intraoperative blood loss and duration of anesthesia was less in the PEEK cage group but there was no significant difference noted when compared with the autograft group (Table 1). The mean duration of symptoms in months till surgery was also comparable in both groups with no statistical difference. MJOA scores were used to compare the functional outcome in 2 fusion groups. The mean preoperative MJOA score in the autograft group was 12.40 ± 3.68, while in the PEEK group it was 10.83 ± 3.01. On statistical analysis, there was no significant difference between the 2 groups (P = .077). There was statistically significant improvement noted in postoperative MJOA scores at 6 months and 1 year in both the groups (P = .0001). On comparing MJOA scores with all pairwise multiple comparison procedures (least significant difference), there was statistically significant difference noted with comparison pairs of preoperative versus 6 months, preoperative versus 1 year, and 3 months versus 6 months, 3 months versus 1 year in both the groups. Improvement in MJOA scores was not statistically significant between 6 months and 1 year (P = .0639) in the autograft group. While there was statistically significant improvement noted with comparison pairs of MJOA score between 6 months and 1 year for PEEK cage group suggesting better recovery in this group between 6 months and 1 year (Figure 3). On comparing the fusion rates, there was no statistical difference between fusion rates between the groups for 1 and 2 levels of ACDF. Overall fusion rates were significantly better for 1-level ACDF (95.74%) when compared with 2-level ACDF (76.00%). Studies have suggested similar fusion rate for both the groups.15-18 Subsidence and loss of segmental lordosis was more in 2-level ACDF compared to 1-level ACDF. Other studies have also suggested that subsidence is associated with a greater number of levels.19
Graft subsidence and loss of segmental lordosis on follow-up X-rays was significant in the bone graft group and was most evident between 6-month and 1-year follow-up. This might explain the plateauing of the improvement in MJOA score between 6 months and 1 year (Figure 3) in this group due to loss of segmental lordosis secondary to graft subsidence. Various studies have suggested that restoration of cervical lordosis and alignment leads to better clinical outcome in ACDF.20 However, overall, the functional results in terms of improvement in postoperative MJOA scores at 1 year were comparable between the 2 groups. On comparison of residual severity of function at 1-year follow-up, there was no statistical difference between the groups (P = .77). Perioperative complications were significantly higher in the autograft group when compared with the PEEK cage group.
Limitations of the Study
This study was based on retrospective analysis of prospectively collected data. Thus, although all the cases were operated by a single team of experienced surgeons, factors like improvement in surgical skills with time could not be negated while comparing the 2 groups. A long-term follow-up study is required to substantiate our clinical findings.
Conclusion
Based on our study, use of tricortical iliac crest and PEEK cage as stand-alone interbody graft for ACDF results in good functional outcome with statistically significant improvement in postoperative MJOA scores in the management of cervical spondylotic myelopathy. Fusion rate for 1-level ACDF and 2-level ACDF is comparable for both fusion techniques. Graft subsidence and subsequent loss of segmental lordosis was more significant with bone graft, which resulted in plateauing of the improvement in MJOA score after 6 months. Perioperative complications related to donor site morbidity are common with autograft. ACDF with PEEK cage is effective and is the fusion technique of choice when compared with iliac crest autograft in the ACDF surgery for cervical spondylotic myelopathy with fewer perioperative complications and better functional recovery.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24. [DOI] [PubMed] [Google Scholar]
- 2. Fehlings MG, Arvin B. Surgical management of cervical degenerative disease: the evidence related to indications, impact, and outcome. J Neurosurg Spine. 2009;11:97–100. [DOI] [PubMed] [Google Scholar]
- 3. Matz PG, Holly LT, Groff MW, et al. Indications for anterior cervical decompression for treatment of cervical degenerative radiculopathy. J Neurosurg Spine. 2009;11:174–182. [DOI] [PubMed] [Google Scholar]
- 4. Liu X, Min S, Zhang H, Zhou Z, Wang H, Jin A. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis. Eur Spine J. 2014;23:362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sonntag VK, Han PP, Vishteh AG. Anterior cervical discectomy. Neurosurgery. 2001;49:909–912. [DOI] [PubMed] [Google Scholar]
- 6. Lied B, Sundseth J, Helseth E. Immediate (0-6 h), early (6-72 h) and late (>72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible. Acta Neurochir (Wien). 2008;150:111–118. [DOI] [PubMed] [Google Scholar]
- 7. Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine (Phila Pa 1976). 2000,25:2646–2654. [DOI] [PubMed] [Google Scholar]
- 8. Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51:1343–1349. [PubMed] [Google Scholar]
- 9. Rhee JM, Chapman JR, Norvell DC, Smith J, Sherry NA, Riew KD. Radiological determination of postoperative cervical fusion: a systematic review. Spine (Phila Pa 1976). 2015;40:974–991. [DOI] [PubMed] [Google Scholar]
- 10. Oshina M, Oshima Y, Tanaka S, Riew KD. Radiological fusion criteria of postoperative anterior cervical discectomy and fusion: a systematic review [published online February 11, 2018]. Global Spine J. doi:10.1177/2192568218755141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jacobs W, Willems PC, van Limbeek J, et al. Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database Syst Rev. 2011;(1):CD004958. [DOI] [PubMed] [Google Scholar]
- 12. Samartzis D, Shen FH, Matthews DK, Yoon ST, Goldberg EJ, An HS. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J. 2003;3:451–459. [DOI] [PubMed] [Google Scholar]
- 13. Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: a prospective randomized study. Neurosurgery. 2007;61:107–116. [DOI] [PubMed] [Google Scholar]
- 14. Samartzis D, Shen FH, Lyon C, Phillips M, Goldberg EJ, An HS. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J. 2004;4:636–643. [DOI] [PubMed] [Google Scholar]
- 15. Lofgren H, Engquist M, Hoffmann P, Sigstedt B, Vavruch L. Clinical and radiological evaluation of trabecular metal and the Smith-Robinson technique in anterior cervical fusion for degenerative disease: a prospective, randomized, controlled study with 2-year follow-up. Eur Spine J. 2010;19:464–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matge G. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir (Wien). 2002;144:539–554. [DOI] [PubMed] [Google Scholar]
- 17. Hao YJ, Yu L, Zhang Y, Wang LM, Li JZ. Surgical treatment of cervical vertebral hemangioma associated with adjacent cervical spondylotic myelopathy. Spine J. 2013;13:1774–1779. [DOI] [PubMed] [Google Scholar]
- 18. Wang X, Chen Y, Chen D, et al. Anterior decompression and interbody fusion with BAK/C for cervical disc degenerative disorders. J Spinal Disord Tech. 2009;22:240–245. [DOI] [PubMed] [Google Scholar]
- 19. Kao TH, Wu CH, Chou YC, Chen HT, Chen WH, Tsou HK. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg. 2014;134:1343–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hu X, Ohnmeiss DD, Zigler JE, Guyer RD, Lieberman IH. Restoration of cervical alignment is associated with improved clinical outcome after one and two level anterior cervical discectomy and fusion. Int J Spine Surg. 2015;9:61. [DOI] [PMC free article] [PubMed] [Google Scholar]