Abstract
Background
It is well established that migration and ethnic minority status are risk factors for psychotic disorders. Recent studies have aimed to determine if they are also associated with subclinical psychosis (psychotic-like experiences and schizotypal traits).
Aims
We aimed to determine to what extent migrant and ethnic minority groups are associated with higher risk of subclinical psychosis.
Method
We conducted a systematic review, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement, and examined findings by ethnicity, migrant status, outcomes of subclinical psychosis and host country. A meta-analysis was carried out with robust variance estimation where possible, to handle statistically dependent effect size estimates.
Results
We included 28 studies (19 studies on psychotic-like experiences and 9 studies on schizotypal traits) and found that ethnicity, but not migrant status, was associated with current and lifetime psychotic-like experiences. In the narrative analysis, we observed the effect of psychosocial risk factors on this association: Black ethnicity groups showed consistent increased prevalence of current and lifetime psychotic-like experiences compared with the reference population across countries.
Conclusions
More generalisable and standardised cohort studies of psychotic-like experiences and schizotypal traits in relation to migration/ethnicity are necessary to examine the effects of exposures and outcomes in different contexts, and to understand the underlying mechanisms of the association between subclinical psychosis and migrant and ethnic minority status.
Declaration of interest
None.
Keywords: Migrants, ethnic minorities, psychosis continuum, subclinical psychosis, psychotic-like experiences
It is well established that migration and ethnic minority status are risk factors for psychotic disorders.1 Recent studies have also investigated this association with regard to subclinical psychosis (i.e. psychotic-like experiences (PLE), isolated psychotic symptoms and schizotypal personality, suggesting that they are also risk factors for the extended psychosis phenotype).2,3 In a meta-analysis carried out by Linscott and van Os,4 lifetime PLE were associated with ethnic minority status in a non-adjusted analysis (odds ratio 1.3, 95% CI 1.2–1.9), but not with migrant status (odds ratio 0.8, 95% CI 0.3–1.8). However, it is still unclear to what extent specific ethnic groups have a higher risk of subclinical psychosis. Furthermore, no meta-analyses have investigated the association between ethnic minority or migration status and schizotypal traits.
The study of subclinical psychosis in a non-clinical population is based on the hypothesis of a psychosis continuum, where subclinical psychosis and psychotic disorders are continuously distributed in the general population and may share the same risk factors.5 This approach brings new perspectives, maximising statistical power and the possibility to detect confounders, modifiers, and biological and psychosocial factors underpinning the aetiology and development of psychotic disorders. Moreover, in migrant and ethnic minority populations, it provides additional advantages in avoiding specific methodological limits, such as differences in case ascertainement (mainly from barriers to mental healthcare access) and misdiagnoses caused by categorical standardised diagnosis. The investigation of subclinical psychosis is important to identify groups at higher risk of psychiatric disorders and therefore promote prevention and reduce treatment delay. For instance, individuals who report PLE have been shown to be more likely to attend their general practitioners for emotional problems.6 More recently, PLE in the general population have been associated with increased rates of mental health service use.7 Thus, higher rates of PLE in migrants and ethnic minorities could indicate the need for tailored policies and interventions to improve mental health for these subgroups, as in other relevant public health issues such as cancer screening and diabetes.
We conducted a systematic review and meta-analysis to further explore the association between ethnic minorities, migrant status and subclinical psychosis outcomes. In the narrative review, we described and compared the results according to adjustment variables related to psychosocial risk factors, because there is evidence that the risk of psychosis varies across different ethnic groups in different host countries, suggesting an influence of other risk factors for psychosis, such as psychological stress (e.g. trauma, social defeat or discrimination).8 We also considered the interpretation of results according to the host country, to better compare the prevalence between different ethnic and migrant groups in the same wider context.
Method
Eligibility criteria
Studies written in English were included if (a) they provided original data on subclinical psychosis (schizotypal traits and PLE, isolated hallucinations or delusional symptoms), (b) the study population was adult (aged >16 years) and the study was in a non-clinical setting and (c) they provided data allowing for comparison between a native reference population and migrants (first- and/or second-generation) and/or ethnic minority groups. Studies that used the same database were included if they provided different analysis (different adjustments or different migrant or ethnic groups studied). We excluded studies recruiting only older adults and those set in secondary or tertiary health services, prison or aged-care facilities. Qualitative studies were also excluded. The considered time period was from 1950 to July 2017.
Search strategy
The following search items were entered in several electronic databases (MEDLINE, PubMed, PsycINFO and ScienceDirect): [delusion OR delusional OR hallucination OR hallucinatory OR paranoia OR paranoid OR psychotic OR schizotypy OR schizotypal] AND [migrant OR migration OR ethnicity OR ethnic]. Authors were contacted if full texts or supplement material were not available online. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to conduct our systematic review and meta-analysis9 (Supplementary material 1 available at https://doi.org/10.1192/bjo.2018.68).
Data extraction
After the screening of titles and abstracts, A.T. and B.P. carefully read all the articles retrieved and selected those of interest for our systematic review and meta-analysis, and independently extracted the data needed for the calculations. Authors were contacted for additional data when necessary.
We extracted information regarding design (incidence, prevalence), country of study, setting (college students, general population, enlistees, etc.), age limits, gender, outcome (hallucinations, delusions or both for PLE; scores for schizotypal personality), diagnostic instrument, sample characteristics (ethnicity, migrant status, reference population) and sample size.
When available, we used odds ratios and 95% confidence intervals as the main result. To examine the relationship between unadjusted and adjusted odds ratios, we also extracted adjusted odds ratios and their adjustment factors. In the case of missing odds ratios, we extracted additional values such as P-values, percentages, s.e. and 95% confidence intervals. Finally, when quantitative data were not available or not adequate, we extracted the summary of findings.
Outcomes
PLE can be defined as delusional or hallucinatory experiences in non-clinical populations,5 although a consistent phenomenological definition is lacking in the literature. We included studies that defined PLE as the presence or absence of positive symptoms of psychosis (delusions, hallucinations or any), as assessed by standardised tools.
Schizotypal personality is a personality organisation with a vulnerability to psychosis.10 Thus, schizotypal traits are usually stable over time, unlike PLE.11 We included studies that quantitatively assessed schizotypal traits with standardised scales.
Quality assessment
Quality assessment of all studies was conducted with the scale proposed by Munn et al,12 developed to assess the quality of prevalence studies in systematic reviews, based on 10 criteria (sample representativeness, strategy for recruitment of participants, sample size, description of settings and participants, coverage of data analysis, objective standard criteria, measures reliability, statistical analysis, confounding factors and sub-population identification criteria). To better identify the level of the quality, we attributed values to the answers suggested by the authors, whereby ‘no’ was designated 0, ‘unclear/not applicable’ was designated 1 and ‘yes’ was designated as 2, resulting in a maximum possible score of 20. This quality assessment was done by A.T. and B.P. separately, and the discrepancies were subsequently addressed and discussed.
Data synthesis and analysis
A narrative synthesis was made for all retrieved studies by outcome and migrant status/ethnicity. In the PLE analyses, we also tried to describe the studies according to the assessment period (current or lifetime) and by outcome (delusions, hallucination or any PLE).
We then performed a meta-analysis where there was sufficient number of studies (at least two)13 providing raw data and taking into account the different outcomes in different migrant/ethnic groups. When there was more than one outcome by study (e.g. PLE, delusions or hallucinations), we preferred to include only results on any PLE, to avoid cumulate dependent effect sizes. We estimated pooled odds ratios and corresponding 95% confidence intervals by random effects meta-analysis to investigate the effect of ethnic minority groups on within- and between-study variability. The level of inconsistency between studies was assessed with the I2 statistic or τ2 (in robust variance estimation).14 To reduce heterogeneity between studies, sensitivity analyses were performed on study quality and use of a validated questionnaire/interview for lifetime and current PLE. To detect publication bias, funnel plots and Egger's test were done.15 Because most studies used more than one exposure (different ethnic groups), to handle statistically dependent effect sizes estimates, we performed a meta-analysis with robust variance estimation when it was possible (at least 10 effect sizes in the data-set).16 The meta-analysis was performed with the METAN and ROBUMETA packages for Stata version 14.2 (StataCorp).17
Results
Study identification
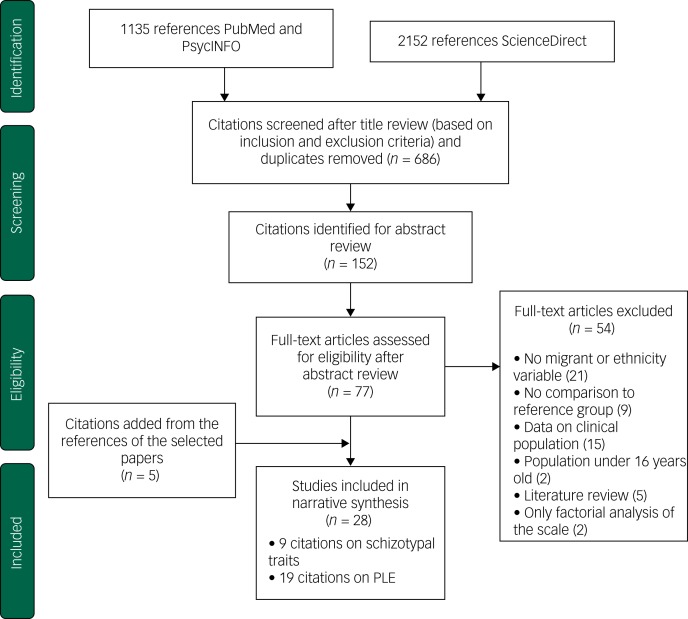
We found 686 potential citations. After reviewing the titles, 152 citations were selected for abstract review, based on our inclusion and exclusion criteria. We kept 77 citations for full manuscript review. Five studies were added based on the citations of considered studies. In the end, 28 studies met the inclusion criteria (Fig. 1).
Fig. 1.
Flow diagram (selection strategy) of selected studies.
PLE, psychotic-like experiences.
Study characteristics
Nineteen studies provided findings on PLE (Supplementary material 1), and nine studies provided findings on schizotypal traits (Table 1), published from 1977 to 2015. Twenty-six studies provided data on ethnicity and five provided data on migrant status. Ethnic groups varied across the countries where the studies were carried out. All citations selected concerned prevalence studies in non-clinical populations, although not all of them analysed data from the general population. This was the case for most studies on schizotypal traits (eight out of nine studies), which were conducted among college students. Regarding studies on PLE, one study was conducted among young male pre-enlistees for the National Service in Singapore,18 whereas the remaining studies were conducted in the general population. One study was conducted only among young adults (18–24 years of age).19 Three studies on PLE20–22 used data from the Collaborative Psychiatric Epidemiologic Surveys in the USA, which consists of three large national ethnic community surveys (in Latino, Black and Asian populations), using similar methods23 and the same data-set (16 423 participants). However, they adjusted for different correlates, which allowed us to compare differences in odds ratios as the result of the different adjustments made. The same reasoning was used for the inclusion of two studies in the UK that used the same data but analysed different risk factors.24,25 Inclusion criteria in studies on PLE were similar (at least one PLE endorsed) despite the different scales used. Eight studies used the Composite International Diagnostic Interview (CIDI)26 and seven studies used the Psychosis Screening Questionnaire (PSQ).27 With respect to studies on schizotypal traits, the Chapman scales28 and the Schizotypal Personality Questionnaire (SPQ)29 were used in seven of the nine studies. One study compared the reliability of 11 different scales,30 and one study31 used the Oxford–Liverpool Inventory of Feelings and Experience (O-LIFE) scale.32
Table 1.
Studies on schizotypal traits: characteristics and findings
| Author/year | Country | Instrument | N | Setting | Ethnic/migrant groups | Findings | Quality assesment |
|---|---|---|---|---|---|---|---|
| Kelley et al (1992)30 | USA | 11 scales | 316 | Male College students | White, Black, Asians | Overall effect of ethnicity (p < 0.001). Asians showed higher scores than White and Black. No differences between White and Black | 7 |
| Poreh et al (1994)47 | USA | Chapman | 852 | College students | Afro-American, European American | No statistically significant differences were found between African-American and European-American, except on the Perceptual Aberration Scale (p < 0.01) which seems mediated by the subjects' gender and socioeconomic background. | 12 |
| Chmielewski et al (1995)46 | USA | Chapman | 7691 | College students | Caucasian, African American, Asian American, Latino | Caucasian showed the lowest scores, Asian the highest for magical ideation and perceptual aberration, Blacks the highest scores of social anhedonia | 11 |
| Sharpley et al (1999)31 | UK | O-LIFE/ PDI | 12 | General population | African Caribbean | No effect of ethnicity in scores of O-LIFE. | 10 |
| Kwapil et al (2002)45 | USA | Chapman | 6137 | College students | Caucasian, African American | Higher scores in African American than in Caucasian, mainly in social and physical anhedonia | 15 |
| Schiffman et al (2004)50 | USA (Hawaii) | SPQ-B | 353 | College students | Caucasian, Asian, mixed ethnicity | No significant differences in total scores between ethnic groups although differences between scales (interpersonal scale) | 8 |
| Cohen et al (2009)48 | USA | SPQ | 1395 | College students | White, African American, Asian American, Hispanic, other | Significant difference in total score for Asians. Differences between scales for african Americans (disorganised) and Asian (negative symptoms) | 16 |
| Goulding et al (2009)49 | USA | SPQ | 825 | College students | White caucasian, black African, Asian American | African American the lowest perceptual disorganisation, Caucasian showed lower social anhedonia | 15 |
| Cicero (2015)51 | USA (Hawaii) | SPQ | 1239 | College students | Asian, Pacific islander, white, multi-ethnic | Differences between scales, trend to lower scores among White and higher scores among Pacific Islander. | 11 |
PLE by ethnicity
Lifetime PLE
Six citations reported data by lifetime PLE and ethnicity.20,21,33–36 Study quality scores ranged from 14 to 19 (mean 17, s.d. 2.1).
In unadjusted analyses, any lifetime PLE or hallucinations were associated with Black ethnic groups across studies conducted in any area that included this ethnicity.20,21,34,35 In the USA, the Latino minority population also showed higher prevalence of lifetime PLE compared with the White population.20,21 These associations, including those among Black minorities, were no longer statistically significant when adjusted for psychological stress20 or clinical diagnosis, after adjustment for supplementary factors (other than sociodemographic).21 In Turkey, no differences (P = 0.6) between Turkish and non-Turkish ethnic groups were found after adjustments for age and gender across five levels of expression of psychosis (from absence of psychosis outcome to psychotic disorder).33 Finally, in Australia, Saha et al found an association between delusional symptoms and ethnic minority status (the study did not distinguish between first- and second-generation migrants), after adjustment for drug addiction, anxiety and depressive disorders (odds ratio 1.3, 95% CI 1.0–1.7).36
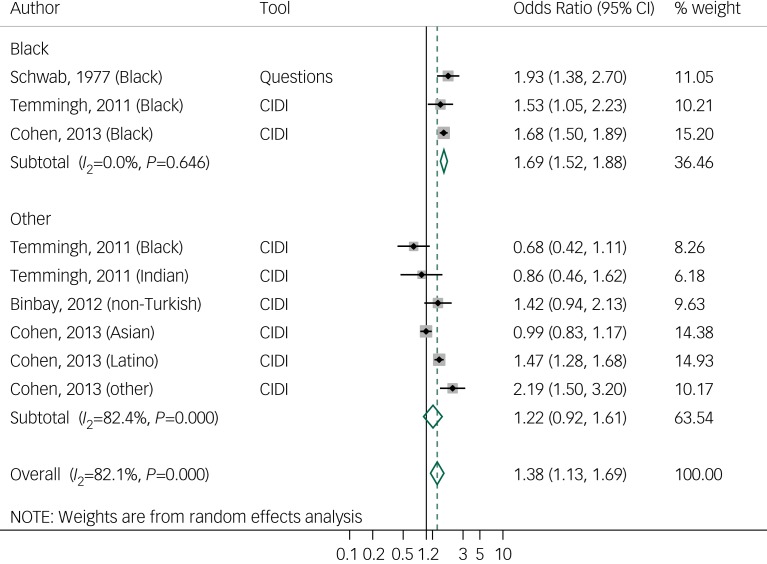
Random effects meta-analysis of four studies of lifetime PLE20,33–35 with nine effect sizes showed significant differences between ethnic minorities and the majority group (odds ratio 1.3, 95% CI, 1.1–1.6, I2 = 82.1%). No publication bias was found in Egger's test (P = 0.5; funnel plot in Supplementary material 2). When analysing PLE by ethnicity, we found a pooled odds ratio of 1.6 (95% CI 1.5–1.8, I2 = 0.0%) in the Black ethnicity group (three studies, three effect sizes) and an odds ratio of 1.2 (95% CI 0.9–1.6, I2 = 82.4%) in the ‘other’ ethnic group, compared with the reference group (Fig. 2). To examine the differences in results according to the use of validated questionnaires, we repeated the analysis but included only studies that used validated interviews (CIDI), therefore one study (quality score of 15)35 was excluded; however, a similar result was observed (odds ratio 1.3, 95% CI 1.0–1.6, I2 = 83.2%) (Supplementary material 4). When analysing only high-quality studies (quality score >17), we found a slightly increase in the odds ratio (odds ratio 1.4, 95% CI 1.1–1.8, I2 = 86.7%). Robust variation estimation method could not be used because of the amount of effect sizes under 10.
Fig. 2.
Forest plot of studies on lifetime psychotic-like experiences, by tool and ethnicity, using random effects meta- analysis, crude odds ratios, and 95% confidence intervals.
CIDI, Composite International Diagnostic Interview.
Current PLE
Eleven citations were found on current PLE by ethnicity, including seven in the UK,24,25,37–41 one in the USA,20 two in the Netherlands19,42 and one in Singapore.18 Study quality scores ranged from 16 to 20 (mean 18.5, s.d. 1.4).
Studies on any current PLE conducted in the UK found results similar to studies on lifetime prevalence, with higher non-adjusted prevalence in Black ethnic groups compared with White majority groups, which decreased but remained significant after adjustments for stress20 and urban dwelling.39 One study analysed PLE among Black Caribbean and Black African groups separately, and showed that among Black African groups, this association remained significant after adjustments (odds ratio 3.4, 95% CI 1.1–10.4).41 In the Netherlands, higher prevalence (odds ratio 2.7, 95% CI 2.1–3.6) was found among non-Dutch individuals compared with Dutch individuals.42 In the USA, minority groups (Latino, Black and Asian groups) tended to show significantly higher current PLE prevalence than White groups, even after adjustments for age, gender, stress and drug use.20 One study in Singapore among young male pre-enlistees for the National Service observed lower prevalence (after adjustments for age, marital status, education and psychiatric disorders) among the Indian population (odds ratio 0.75, 95% CI 0.5–0.9), but not among the Malay population (odds ratio 1.0, 95% CI 0.8–1.2), compared with the Chinese reference group.18
Hallucinations were reported separately in three studies. In the UK, higher prevalence was found among Black Caribbean women in two studies, in both unadjusted analysis (odds ratio 2.3, 95% CI 1.4–3.8, P = 0.006)37 and adjusted analysis (adjusted for age, IQ, alcohol misuse, victimisation and anxiety or depression; odds ratio 2.4, 95% CI 0.9–6.2).38 In the Netherlands,19 non-Dutch individuals (mostly Turkish and Moroccan, followed by Antillean/Surinamese, Indonesian and other) tended to show a significantly higher prevalence of hallucinations than Dutch individuals, although there was a reduction (from 28 to 52% across groups) after adjustment for social adversity. Delusions were analysed in two studies in the UK, with similar findings: increased prevalence among Black and Asian groups compared with White groups.24,38
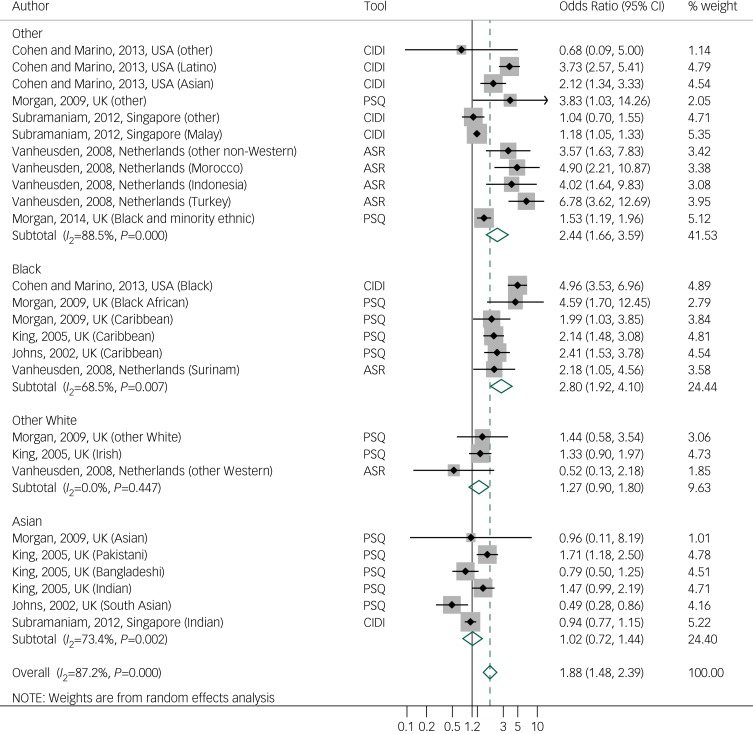
Random effects meta-analysis of 7 studies of current PLE18–20,37,39–41 with 26 effect sizes showed a pooled odds ratio of 1.8 (95% CI 1.4–2.3, I2 = 87.2%). There is some weak evidence of publication bias, related to the lack of smaller studies reporting a positive association (Egger's test 0.07; funnel plot in Supplementary material 3). When we used the robust variation estimation method, the odds ratio decreased to 1.4 (95% CI 1.0–1.8, τ2 = 0.19). We examined differences in results according to the use of a self-questionnaire or an interview, by repeating the analysis with only studies that used interviews (CIDI, PSQ). One study that used a self-questionnaire was excluded,19 resulting in a small decrease in the odds ratio to 1.6 (95% CI 1.2–2.0, I2 = 87.3%; Supplementary material 5). Similarly to lifetime PLE studies, analysis with higher-quality studies (quality score >17) showed an increased odds ratio of 2.4 (95% CI 1.7–2.9, I2 = 79.5%). When analysing by ethnicity, random effects meta-analysis showed a pooled odds ratio of 2.8 (95% CI 1.9–4.1, I2 = 68.5%) among Black ethnic groups (five studies, six effect sizes) and a pooled odds ratio of 1.0 in the Asian group (95% CI 0.7–1.4, I2 = 73.4%) (four studies in the UK, six effect sizes) compared with the reference population (Fig. 3). Meta-analyses of hallucinations and delusions outcomes were not performed because of to the small number of studies.
Fig. 3.
Forest plot of studies on current psychotic-like experiences, by tool and ethnicity, using random effects meta-analysis, crude odds ratios, and 95% confidence intervals.
ASR, Adult Self Report; CIDI, Composite International Diagnostic Interview; PSQ, Psychosis Screening Questionnaire.
PLE by migrant status
Five studies analysed PLE and migrant status,20–22,43,44 and study quality scores ranged from 17 to 20 (mean 18.8, s.d. 1.1).
A negative association of migrant status with any lifetime PLE (after adjustment for sociodemographic variables; odds ratio 0.8, 95% CI 0.6–1.0) and with hallucinations (odds ratio 0.7, 95% CI 0.5–0.9), but not with delusions (odds ratio 1.4, 95% CI 0.9–2.2), was reported in a cross-national study based on 31 261 responders in 18 middle- and high-income countries.43 In the USA, this negative trend of prevalence of lifetime20,21 and current22 PLE among migrants was replicated in first-generation migrants, but not among their descendants.22 In Australia, Scott et al44 found increased prevalence of current delusions among migrants of non-English-speaking background compared with migrants of English-speaking background (odds ratio 1.3, 95% CI 1.1–1.5). A meta-analysis was not performed because of the lack of available data on effect sizes and the different criteria used to define migrant status.
Schizotypal traits
Nine studies comparing different ethnic groups were found, but none analysed migrant status. Study quality scores ranged from 7 to 16 (mean 11.6, s.d. 3.1). Eight studies were carried out in the USA, among college students. In the USA, studies that used the Chapman scales45–47 observed similar findings: variation of scores across all scales by ethnic group, with an inclination toward lower scores in White groups and higher scores in the Black groups. Two studies that used the SPQ found discrepant results: one study found higher total scores among Asian Americans and higher disorganisation scores among Black Americans,48 whereas the second study showed lower disorganisation scores among Black Americans.49 Adjustment factors may account for these differences (age and gender in the first study, and marital status and history of treatment in the second study). One study that used 11 different scales in 321 participants found higher scores of schizotypal traits in Asian than in White or Black ethnic groups.30 In Hawaii, one study did not report any differences (SPQ-Brief) between ethnic groups,50 whereas another reported lower scores of schizotypal traits (SPQ) in the White group and higher scores among Pacific Islanders.51
One study in the UK analysed schizotypal traits in a small sample (N = 48) from the general population.31 They did not find significant differences in the O-LIFE scale between Black Caribbean and White ethnic groups, adjusting for socioeconomic level. Meta-analysis of these studies could not be performed because of the heterogeneity of scales and measures used, as well as the unavailability of scores by ethnic groups in many studies.
Discussion
Association between subclinical psychosis and ethnicity or migration
Data from 16 studies regarding PLE and ethnicity were analysed. We found evidence in the narrative review and the meta-analysis for an association between ethnicity and PLE, in line with a previous meta-analysis,4 although variations were found in contexts and ethnic groups across studies. We extended these outcomes by observing a variation of this risk among different ethnic groups, with a constant trend of higher prevalence of lifetime and current PLE among Black ethnic groups.
We did not find clear evidence of an association between PLE and migrant status. However, except for the cross-national study43 that included European countries, the number of studies included from outside Europe was limited. On the other hand, in line with findings for psychosis, a trend toward higher prevalence of PLE was observed among second-generation migrants.22,36
With respect to the association between schizotypal traits and ethnicity, the methods used across studies were too heterogeneous to allow for a summary of findings. Moreover, the fact that data were gathered from college students and not the general population provided less reliability and generalisability of results. However, we observed a trend toward lower total scores in White ethnic groups even when they belonged to the ethnic minority.34,51
Finally, adjustment for gender was made in most studies, with some reporting gender differences (higher prevalence among women) with respect to the prevalence of PLE18,19,38,39,52 and schizotypal traits.47
Does subclinical psychosis have the same risk factors as psychosis?
In studies that provided unadjusted and adjusted odds ratios, we found evidence of a decrease in the effect of ethnicity after adjustment for life and social adversity events (rather than sociodemographic factors),19–21,25,38,41 suggesting that social adversity might be a moderator/confounder for the ethnicity effect in subclinical psychosis, as it is in clinical psychosis.
When comparison was possible, we observed that ethnic groups known to be at risk of psychotic disorders displayed higher prevalence of PLE. This was the case in the UK for Black Caribbean and Black African individuals,53,54 and in the Netherlands for Moroccan and Turkish individuals.19,55
Strengths and limitations
To our knowledge, this is the first systematic review that focuses on the association between subclinical psychosis and ethnicity and migrant status, providing further evidence of the shared risk factors of the psychosis continuum.
Our study has some limitations leading to a less accurate summary and limited generalisability of findings. We could not perform meta-analysis for migrant status because of insufficient data. Similarly, regarding studies on schizotypal traits, lower-quality assessment scores than PLE studies (schizotypal traits: mean 11.6, s.d. 3.1 v. PLE: mean 18.1, s.d. 1.7) and insufficient availability of crude or homogeneous data did not allow meta-analysis of all studied outcomes, limiting our interpretation to the narrative review. Different assessment methods, outcomes definitions and representativeness of the sample across studies introduced different types of biases, leading to high heterogeneity (I2) in both current and lifetime PLE meta-analyses. In addition, meta-analyses were performed with unadjusted ratios, which do not reflect the real rates and variance because they can be influenced by other psychosocial risk factors for which no corrections were made, as was observed in studies that used those adjustments. There was a weak evidence of publication bias for current PLE studies related to the lack of smaller studies showing a positive association with ethnicity.
Robust variance estimation could be performed for current PLE studies and showed a decrease in the pooled odds ratios, suggesting an effect of dependent effect size estimates; therefore there is a need for more caution in the interpretation of findings in similar studies that do not correct for this dependency. The association between ethnicity and PLE was not found in any study when considered separately, but only when the studies were analysed together; when we analysed ethnic groups separately, we observed a decrease of inconsistency.
Sensitivity analysis for type of tool showed small differences in results, as observed in previous studies, which suggests that both self-administrated questionnaires and interview-based assessments may show similar reliability56 and are predictive of future psychotic disorders.57 On the other hand, when we ran meta-analysis with only studies of higher quality (quality score >17), we found higher odds ratios for lifetime PLE (odds ratio 1.4, 95% CI 1.1–1.8 instead of odds ratio 1.3, 95% CI 1.1–1.6) and current PLE (odds ratio 2.4, 95% CI 1.7–2.9 instead of odds ratio 1.8, 95% CI 1.4–2.3), with a decrease in I2 for current PLE only. Finally, responses could also have been biased by the influence of cultural factors on the expression of emotions and social behaviour, as well as on the cognitive appraisal of the psychiatric experience and explanatory models.58
Interpretation of findings
In concordance with the psychosis proneness-persistence-impairment model, emerging data show that increased exposure to social adversity is associated with risk of subclinical psychosis.2,57 On the other hand, growing evidence shows that subclinical psychosis might not only be related to psychosis, but also to other psychiatric conditions (depression, anxiety, post-traumatic stress disorder), making it difficult to differentiate specific putative mechanisms.21,42
Moreover, the variation of the prevalence of subclinical psychosis across different ethnic groups suggests that psychosocial risk and protective factors interplay and may affect these populations differently. For instance, the tendency toward higher prevalence of subclinical psychosis observed among Black ethnicity groups across countries and continents is consistent with findings related to associated risk factors for psychosis, such as experiences of discrimination and racism,59 as well as the vitamin D deficiency hypothesis.60 In the same vein, we observed that differences in acculturation factors such as language proficiency may play a role in the development of PLE.44 Finally, the ethnic density effect61 has been shown to be an important protective factor, although the potential mechanisms (stress-buffering effect) and factors underlying this effect (social support, social capital) are not completely understood.62
In our review, the weak association observed in the narrative review between PLE and migrant status (in USA and Australia) may seem to contradict the large evidence base for a positive association mostly established in European countries. Possible explanations to our findings may be related to, and the influence of, sociopolitical contexts on their living conditions across countries, such as immigration policies (national origin quotas, the choice of skilled migration, screening for diseases) and resettlement factors (access to regular status, housing, jobs and health).22 Likewise, the ‘healthy immigrant effect’ (better health status than natives) is shown to be heterogeneous across European countries.63 However, the lack of consistent association between migrant status and subclinical psychosis is not in favour of the selective migration hypothesis, which suggests that individuals more prone to developing psychosis have a greater tendency to migrate.64
The role of biological and inflammatory factors has been scarcely studied in these groups. Furthermore, despite the fact that the association between cannabis use and psychotic disorders and subclinical psychosis outcomes is well documented,65,66 the effect of this risk factor in migrant populations is less documented, although some studies suggest a positive relationship.67,68
To conclude, this study reveals evidence that ethnicity is associated with subclinical psychosis. However, when exploring environmental risk factors of the psychosis continuum, the development of more generalisable and standardised cohort studies of PLE and schizotypal traits in relation to migration and ethnicity are necessary to examine the effect of multiple exposures in different contexts, and to understand the underlying mechanisms across different migrant generations and ethnicities.
Acknowledgements
We thank Sarah Boster from INSERM (U-955), for English language editing.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2018.68.
click here to view supplementary material
References
- 1.Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med 2011; 41(5): 897–910. [DOI] [PubMed] [Google Scholar]
- 2.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 2009; 39(2): 179–95. [DOI] [PubMed] [Google Scholar]
- 3.Mason OJ. The assessment of schizotypy and its clinical relevance. Schizophr Bull 2015; 41(Suppl 2): S374–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med 2013; 43(6): 1133–49. [DOI] [PubMed] [Google Scholar]
- 5.Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res 2002; 54(1): 59–65. [DOI] [PubMed] [Google Scholar]
- 6.Murphy J, Shevlin M, Houston J, Adamson G. A population based analysis of subclinical psychosis and help-seeking behavior. Schizophr Bull 2010; 38(2): 360–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhavsar V, Maccabe JH, Hatch SL, Hotopf M, Boydell J, McGuire P. Subclinical psychotic experiences and subsequent contact with mental health services. BJPsych Open 2017; 3(2): 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Veling W. Ethnic minority position and risk for psychotic disorders. Curr Opin Psychiatry 2013; 26(2): 166–71. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meehl PE. Schizotaxia, schizotypy, schizophrenia. Am Psychol 1962; 17: 827–38. [Google Scholar]
- 11.Debbane M, Barrantes-Vidal N. Schizotypy from a developmental perspective. Schizophr Bull 2015; 41(Suppl 2): S386–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manage 2014; 3(3): 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Valentine JC, Pigott TD, Rothstein HR. How many studies do you need? A primer on statistical power for meta-analysis. J Edu Behav Statist 2010; 35(2): 215–47. [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327(7414): 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sterne JA, Becker BJ, Egger M. The funnel plot In: Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments (eds Rothstein HR, Sutton AJ, Borenstein M): 75–98. Wiley, 2005. [Google Scholar]
- 16.Hedges LV, Tipton E, Johnson MC. Robust variance estimation in meta-regression with dependent effect size estimates. Res Synth Methods 2010; 1(1): 39–65. [DOI] [PubMed] [Google Scholar]
- 17.Hedberg EC. ROBUMETA: Stata Module to Perform Robust Variance Estimation in Meta-Regression with Dependent Effect Size Estimates, Statistical Software Components S457219. Boston College Department of Economics, 2014. (https://ideas.repec.org/c/boc/bocode/s457219.html
- 18.Subramaniam M, Verma S, Cheok C, Lee IM, Wong J, Chong SA. Prevalence and correlates of psychotic symptoms among Asian males. Soc Psychiatry Psychiatr Epidemiol 2012; 47(1): 137–44. [DOI] [PubMed] [Google Scholar]
- 19.Vanheusden K, Mulder CL, van der Ende J, Selten JP, van Lenthe FJ, Verhulst FC, et al. Associations between ethnicity and self-reported hallucinations in a population sample of young adults in The Netherlands. Psychol Med 2008; 38(8): 1095–102. [DOI] [PubMed] [Google Scholar]
- 20.Cohen CI, Marino L. Racial and ethnic differences in the prevalence of psychotic symptoms in the general population. Psychiatr Serv 2013; 64(11): 1103–9. [DOI] [PubMed] [Google Scholar]
- 21.DeVylder JE, Burnette D, Yang LH. Co-occurrence of psychotic experiences and common mental health conditions across four racially and ethnically diverse population samples. Psychol Med 2014; 44(16): 3503–13. [DOI] [PubMed] [Google Scholar]
- 22.Oh H, Abe J, Negi N, DeVylder J. Immigration and psychotic experiences in the United States: another example of the epidemiological paradox? Psychiatry Res 2015; 229(3): 784–90. [DOI] [PubMed] [Google Scholar]
- 23.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). Int J Methods Psychiatr Res 2004; 13(4): 221–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population. Psychol Med 2011; 41(5): 923–36. [DOI] [PubMed] [Google Scholar]
- 25.Wickham S, Taylor P, Shevlin M, Bentall RP. The impact of social deprivation on paranoia, hallucinations, mania and depression: the role of discrimination social support, stress and trust. PLoS One 2014; 9(8): e105140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler RC, Üstün TB. The world mental health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004; 13(2): 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bebbington P, Nayani T. The Psychosis Screening Questionnaire. Int J Methods Psychiatr Res 1996; 5(1): 11–9. [Google Scholar]
- 28.Chapman LJ, Chapman JP, Miller EN. Reliabilities and intercorrelations of eight measures of proneness to psychosis. J Consult Clin Psychol 1982; 50(2): 187–95. [DOI] [PubMed] [Google Scholar]
- 29.Raine A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophr Bull 1991; 17(4): 555–64. [DOI] [PubMed] [Google Scholar]
- 30.Kelley MP, Coursey RD. Lateral preference and neuropsychological correlates of schizotypy. Psychiatry Res 1992; 41(2): 115–35. [DOI] [PubMed] [Google Scholar]
- 31.Sharpley MS, Peters ER. Ethnicity, class and schizotypy. Soc Psychiatry Psychiatr Epidemiol 1999; 34(10): 507–12. [DOI] [PubMed] [Google Scholar]
- 32.Mason O, Claridge G, Jackson M. New scales for the assessment of schizotypy. Pers Individ Dif 1995; 18(1): 7–13. [Google Scholar]
- 33.Binbay T, Drukker M, Elbi H, Tanik FA, Ozkinay F, Onay H, et al. Testing the psychosis continuum: differential impact of genetic and nongenetic risk factors and comorbid psychopathology across the entire spectrum of psychosis. Schizophr Bull 2012; 38(5): 992–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Temmingh H, Stein DJ, Seedat S, Williams DR. The prevalence and correlates of hallucinations in a general population sample: findings from the South African Stress and Health Study. Afr J Psychiatry (Johannesbg) 2011; 14(3): 211–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwab ME. A study of reported hallucinations in a southeastern county. Ment Health Soc 1977; 4(5–6): 344–54. [PubMed] [Google Scholar]
- 36.Saha S, Scott JG, Varghese D, McGrath JJ. Socio-economic disadvantage and delusional-like experiences: a nationwide population-based study. Eur Psychiatry 2013; 28(1): 59–63. [DOI] [PubMed] [Google Scholar]
- 37.Johns LC, Nazroo JY, Bebbington P, Kuipers E. Occurrence of hallucinatory experiences in a community sample and ethnic variations. Br J Psychiatry 2002; 180: 174–8. [DOI] [PubMed] [Google Scholar]
- 38.Johns LC, Cannon M, Singleton N, Murray RM, Farrell M, Brugha T, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry 2004; 185: 298–305. [DOI] [PubMed] [Google Scholar]
- 39.King M, Nazroo J, Weich S, McKenzie K, Bhui K, Karlsen S, et al. Psychotic symptoms in the general population of England--a comparison of ethnic groups (the EMPIRIC study). Soc Psychiatry Psychiatr Epidemiol 2005; 40(5): 375–81. [DOI] [PubMed] [Google Scholar]
- 40.Morgan C, Fisher H, Hutchinson G, Kirkbride J, Craig TK, Morgan K, et al. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta Psychiatr Scand 2009; 119(3): 226–35. [DOI] [PubMed] [Google Scholar]
- 41.Morgan C, Reininghaus U, Reichenberg A, Frissa S, Hotopf M, Hatch SL. Adversity, cannabis use and psychotic experiences: evidence of cumulative and synergistic effects. Br J Psychiatry 2014; 204: 346–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breetvelt EJ, Boks MPM, Numans ME, Selten J-P, Sommer IEC, Grobbee DE, et al. Schizophrenia risk factors constitute general risk factors for psychiatric symptoms in the population. Schizophr Res 2010; 120(1): 184–90. [DOI] [PubMed] [Google Scholar]
- 43.McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross-national analysis based on 31,261 respondents From 18 countries. JAMA Psychiatry 2015; 72(7): 697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scott J, Chant D, Andrews G, McGrath J. Psychotic-like experiences in the general community: the correlates of CIDI psychosis screen items in an Australian sample. Psychol Med 2006; 36(2): 231–8. [DOI] [PubMed] [Google Scholar]
- 45.Kwapil TR, Crump RA, Pickup DR. Assessment of psychosis proneness in African-American college students. J Clin Psychol 2002; 58(12): 1601–14. [DOI] [PubMed] [Google Scholar]
- 46.Chmielewski PM, Fernandes LO, Yee CM, Miller GA. Ethnicity and gender in scales of psychosis proneness and mood disorders. J Abnorm Psychol 1995; 104(3): 464–70. [DOI] [PubMed] [Google Scholar]
- 47.Poreh AM, Ross TP, Hanks R, Whitman DR. Ethnicity, socioeconomic background, and psychosis-proneness in a diverse sample of college students. Curr Psychol 1994; 13(4): 365–70. [Google Scholar]
- 48.Cohen AS, Davis TE III. Quality of life across the schizotypy spectrum: findings from a large nonclinical adult sample. Compr Psychiatry 2009; 50(5): 408–14. [DOI] [PubMed] [Google Scholar]
- 49.Goulding SM, McClure-Tone E, Compton MT. Associations between multiple dimensions of schizotypy and sociodemographic variables in a nonpsychiatric sample of young adults. J Nerv Ment Dis 2009; 197(10): 786–9. [DOI] [PubMed] [Google Scholar]
- 50.Schiffman J. Schizotypal traits in a non-clinical sample from Hawai'i. Pac Health Dialog 2004; 11(1): 84–6. [PubMed] [Google Scholar]
- 51.Cicero DC. Measurement invariance of the Schizotypal Personality Questionnaire in Asian, Pacific Islander, White, and multiethnic populations. Psychol Assess 2016; 28(4): 351–61. [DOI] [PubMed] [Google Scholar]
- 52.Binbay T, Ulas H, Alptekin K, Elbi H. Batı Avrupa Ülkelerinde Yaşayan Türkiye Kökenli Göçmenlerde Psikotik Bozukluklar: Sıklık, Yaygınlık ve Başvuru Oranları Üzerine Bir Derleme. [Psychotic disorders among immigrants from Turkey in Western Europe: an overview of incidences, prevalence estimates, and admission rates.] Turk Psikiyatri Derg 2012; 23(1): 53–62. [PubMed] [Google Scholar]
- 53.Qassem T, Bebbington P, Spiers N, McManus S, Jenkins R, Dein S. Prevalence of psychosis in black ethnic minorities in Britain: analysis based on three national surveys. Soc Psychiatry Psychiatr Epidemiol 2015; 50(7): 1057–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tortelli A, Errazuriz A, Croudace T, Morgan C, Murray RM, Jones PB, et al. Schizophrenia and other psychotic disorders in Caribbean-born migrants and their descendants in England: systematic review and meta-analysis of incidence rates, 1950-2013. Soc Psychiatry Psychiatr Epidemiol 2015; 50(7): 1039–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Selten JP, Veen N, Feller W, Blom JD, Schols D, Camoenie W, et al. Incidence of psychotic disorders in immigrant groups to the Netherlands. Br J Psychiatry 2001; 178: 367–72. [DOI] [PubMed] [Google Scholar]
- 56.Kelleher I, Harley M, Murtagh A, Cannon M. Are screening instruments valid for psychotic-like experiences? A validation study of screening questions for psychotic-like experiences using in-depth clinical interview. Schizophr Bull 2011; 37(2): 362–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N, Weiser M, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med 2012; 42(11): 2239–53. [DOI] [PubMed] [Google Scholar]
- 58.Devylder JE, Oh HY, Yang LH, Cabassa LJ, Chen FP, Lukens EP. Acculturative stress and psychotic-like experiences among Asian and Latino immigrants to the United States. Schizophr Res 2013; 150(1): 223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nazroo JY. Ethnic inequalities in severe mental disorders: where is the harm? Soc Psychiatry Psychiatr Epidemiol 2015; 50(7): 1065–7. [DOI] [PubMed] [Google Scholar]
- 60.McGrath JJ, Burne TH, Feron F, Mackay-Sim A, Eyles DW. Developmental vitamin D deficiency and risk of schizophrenia: a 10-year update. Schizophr Bull 2010; 36(6): 1073–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Das-Munshi J, Becares L, Boydell JE, Dewey ME, Morgan C, Stansfeld SA, et al. Ethnic density as a buffer for psychotic experiences: findings from a national survey (EMPIRIC). Br J Psychiatry 2012; 201(4): 282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health 2015; 69(10): 1021–8. [DOI] [PubMed] [Google Scholar]
- 63.Moullan Y, Jusot F. Why is the ‘healthy immigrant effect’ different between European countries? Eur J Public Health 2014; 24(Suppl 1): 80–6. [DOI] [PubMed] [Google Scholar]
- 64.Ødegaard O. Emigration and insanity. Acta Psychiatr Neurol 1932; (Suppl 4): 1–206. [Google Scholar]
- 65.Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry 2015; 2(3): 233–8. [DOI] [PubMed] [Google Scholar]
- 66.Szoke A, Galliot AM, Richard JR, Ferchiou A, Baudin G, Leboyer M, et al. Association between cannabis use and schizotypal dimensions--a meta-analysis of cross-sectional studies. Psychiatry Res 2014; 219(1): 58–66. [DOI] [PubMed] [Google Scholar]
- 67.Allegri F, Belvederi Murri M, Paparelli A, Marcacci T, Braca M, Menchetti M, et al. Current cannabis use and age of psychosis onset: a gender-mediated relationship? Results from an 8-year FEP incidence study in Bologna. Psychiatry Res 2013; 210(1): 368–70. [DOI] [PubMed] [Google Scholar]
- 68.Ballon N, Ursulet G, Merle S, Eynaud M, Charles-Nicolas A, Michalon M. Excess of psychoses among the French West Indian population. Can J Psychiatry 2004; 49(5): 335–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2018.68.
click here to view supplementary material