Abstract
Neuromyelitis optica (NMO) is an immune-mediated inflammatory disorder of the central nervous system. It is characterized by concurrent inflammation and demyelination of the optic nerve (optic neuritis [ON]) and the spinal cord (myelitis). Multiple studies show variations in prevalence, clinical, and demographic features of NMO among different populations. In addition, ethnicity and race are known as important factors on disease phenotype and clinical outcomes. There are little data on information about NMO patients in underserved groups, including Puerto Rico (PR). In this research, we will provide a comprehensive overview of all aspects of NMO, including epidemiology, environmental risk factors, genetic factors, molecular mechanism, symptoms, comorbidities and clinical differentiation, diagnosis, treatment, its management, and prognosis. We will also evaluate the demographic features and clinical phenotype of NMO patients in PR. This will provide a better understanding of NMO and establish a basis of knowledge that can be used to improve care. Furthermore, this type of population-based study can distinguish the clinical features variation among NMO patients and will provide insight into the potential mechanisms that cause these variations.
Keywords: AQP4 antibodies, multiple sclerosis, myelitis, neuromyelitis optica, optic neuritis
INTRODUCTION
In 1894, Eugène Devic and his student Fernand Gault created the term neuromyelitis optica (NMO) in a published review of early cases of patients that presented with bilateral optic neuritis (ON) and myelitis accompanied by debilitating disability after series of attacks.[109,110] For years, NMO was considered a special form of multiple sclerosis (MS).[47]
In 2015, the International Panel for NMO Diagnosis proposed the unifying term of neuromyelitis optica spectrum disorders (NMOSD) for patients presenting selective demyelination of the spinal cord and the optic nerve. Specific criteria were established to facilitate earlier and more accurate diagnoses in AQP4 antibodies seropositive or seronegative patients presenting with ON, transverse myelitis, or area postrema clinical syndrome associated with a medullary MRI lesion.[289] Historically, NMO and MS are seen as overlapping central nervous system (CNS) inflammatory diseases. NMO was considered a variant of MS and the diagnosis of patients with NMO was delayed for many years due to the absence of specific criteria to recognize and distinguish the disease from MS.[69,116] With the discovery of AQP4 antibodies, the incidence of the disease started to be studied in a more accurate way.[154,206]
In the following sections, we will provide a comprehensive review of NMO that covers its epidemiology, environmental risk factors, genetic factors, molecular mechanism, symptoms, comorbidities and clinical differentiation, diagnosis, treatment, its management, and prognosis.
In addition, we also provide information specific to NMO patients in Puerto Rico (PR).
A recent study on Latin Americans with NMO (including patients from Caribbean islands) found the prevalence of NMO in this population ranged from 0.37/100,000 to 4.2/100,000 with African, Brazilian young women having the highest frequency.[10] However, there is no prior study on NMO patients specifically from PR.
We will evaluate contributing factors and clinical phenotype of NMO patients in PR. This type of population-based study can help the treating physicians with understanding the prognosis of NMO among this specific population. Furthermore, it will enhance their knowledge on the variability of the disease that is based on environmental factors and ethnicity. We believe that this research can delineate the clinical features variation among NMO patients and will provide insight into the potential mechanisms behind these variations.
EPIDEMIOLOGY OF NEUROMYELITIS OPTICA
The evolution in the knowledge of NMO and the changes in the selection criteria have influenced the incidence and prevalence rates reported in many countries, with prevalence ranging from 0.05 to 4.4/100,000 worldwide.[71,204,264] The highest incidence and prevalence reported is from a study performed from 2008 to 2012 in Barcelona, Spain with incidence of 5.35/100,000 and prevalence of 7.87/100,000; both values are outliers in the data found in literature.[162] In the United States, there is an estimated 4000–8000 patients (1–2% of formerly diagnosed MS patients).[170]
In some countries, the studies for diagnosing NMO are scarce and only an average age of onset for the disease is reported, such as in Algeria with a mean of 29.4 years old (range 16–44 years) or Iran with a mean of 36.6 years old (mode of 30).[58,70] A study in Spain reported a mean onset of 36 years, one study in Brazil reported a mean onset of 32.8 years (range 14–55), and in a study of six patients from Germany, there was a range of onset from 5 to 14 years.[92,162,208] These data represent a lower average age of onset than the numbers reported in different countries 5–10 years ago (41.1–45 years old), possibly attributed to improvement in technology and diagnostic studies.[172] There is also reportedly an increase in NMO risk among patients older than 48 years.[70]
For many years, NMO has been associated with Indian, black, and Asian populations: the Japanese population, for example, has one of the highest documented prevalence of NMO in the world at 3.4/100,000.[214,182,204] On the other hand, in studies performed in South East Wales, NMO is as frequent in populations of Northern European as in populations that are non-Caucasian.[52] Furthermore, multiethnic studies performed in Cuba found that prevalence rates do not differ between ethnic groups; black patients were older and experienced more relapses of NMO and worse motor deficiencies during their life which could lead to a longer period presenting symptoms and higher probability of being diagnosed in comparison with whites.[37] Recent studies in Southern Denmark also proposed that NMO prevalence in Caucasian population is higher than previously reported; results showed that all patients with complete criteria for NMO were Caucasian except for one. The prevalence was found to be 4.4/100,000 in this population.[16]
Studies in Latin America show patterns of higher relative frequency of NMO in relation with MS in populations with a higher presence of non-white descendants. In Buenos Aires, Argentina, the lowest relative frequency is reported at 2.1% in a population of high European descent. Paraguay, composed of 30% of mestizos population, reports a frequency of 8.7%. Caracas, Venezuela, reports the highest relative frequency of NMO at 11.8% with the highest non-white presence 79.15%.[10]
Female preponderance is reported in NMO patients, in both pediatrics and adults.[63] In many regions of the world, there is a pattern of female predominance: east Brazil 5:1, Iran 5.9:1, 2.8:1 in Germany, 7:1 in Pediatric patients treated at Mayo Clinic, Spain 2.4:1, Southern Denmark 2.8:1, and in Japan 6.4:1.[214,63,70,107,162,182,208] The disease predilection for females in NMO is stronger than in MS, in which gender ratio varies from 1.1:1 to 3.4:1 in Europe and 3.1:1 in United States.[31,65,296] Due to the high prevalence in females, some investigators suggest the possibility of hormones influencing the development of NMO.[214] Pregnant females with NMO have an increased odds ratio of miscarriage which have been associated with an imbalance in Th1 and Th2 cytokines.[75,196]
ENVIRONMENTAL RISK FACTORS IN NEUROMYELITIS OPTICA
The association between environmental factors with the incidence of autoimmune diseases is well studied over many years.[40,87,120] In this section, we review the most important environmental factors that promote the development of NMO.
Gastrointestinal
Many studies look for the association between diet and gastrointestinal infections with prevalent diseases in the Asian population.[303] In Japan, where the incidence of NMO is 3.42/100,000, Helicobacter pylori neutrophil activating protein increases the neutrophil infiltration in acute lesions of NMO patients.[155,182] Furthermore, a significantly higher number of patients positive to anti-H. pylori and anti-Chlamydia pneumoniae IgG are found among anti-AQP4 Ab-positive NMO patients in comparison with control patients, suggesting the association of H. pylori infection in NMO pathogenesis.[136] A higher prevalence of MS as compared to NMO is found in the northern latitudes of Japan.[135] In this area, westernization, changes in diet, and improvements in sanitation are more common. These processes may have played a contributive factor in decreasing the rate of infection of H. pylori and reduced the risk for NMO in the North during the past century.[117,136]
Clostridium perfringens (C. perfringens) is also found to be one of the most active bacteria in NMO patients microbiota.[55] Investigators suggest that the Epsilon toxin produced by C. perfringes causes blood–brain barrier damage facilitating the entrance of AQP4-IgG.[305] This mechanism is described in MS patients who showed a 10 times higher immunoreactivity to Epsilon toxin of C. perfringes Type A compared with healthy controls.[233]
Studies regarding the change in climate and seasonal viral infections in Japan showed an association with relapses in MS patients but not in NMO patients.[189]
Vitamin D
Though the importance of active vitamin D, or 1,25-dihydroxycholecalciferol, in immune system function is well known, it's role in the pathogenesis of autoimmune-mediated demyelinating neuropathies is only now just starting to be understood. Vitamin D acts to increase regulatory T cell (Treg) function via increased interleukin 10, as well as suppression of interferon Υ, interleukin 2, and, at least in-vitro, interleukin 4.[9,41,254,287] This increase in Treg dampens T-helper activation and is generally accepted as a means to control the immune system and avoid pathological self-reactivity.[183,248,250] Vitamin D dysregulation is posited as part of the pathophysiology of NMO.[114]
Vitamin D synthesis is dependent on ultraviolet (UV) light and is needed for adequate immunologic responses.[40,84] Decreased sun exposure, a demonstrated risk for MS, is not proven as a risk for NMO.[177] However, an increase in sun exposure could be a potential risk factor for NMO. The number of cases of NMO reported in 2011 in southern Japan is significantly higher in comparison with the North, which could be related to higher UV indices and annual sunshine duration.[90,135,182] On the contrary, in Korean NMO patients, levels of vitamin D were found to be significantly lower than controls and deficiency of vitamin D was found in patients having an NMO attack.[179] Also, studies performed in Thai NMO patients showed no association of vitamin D insufficiency with disease process and disease disability.[113]
Additional studies show a correlation between both NMO and MS and vitamin D deficiency, though neither study found correlation between either prevalence nor degree of vitamin D deficiency and annualized relapse rates of NMO.[114,179] One study did find an inverse relation between levels of vitamin D and the severity of NMO symptoms, while yet another study identified higher prevalence of reduced vitamin D levels in acute relapse of NMO versus stable remission.[179,245]
Other investigators report independent roles for the amount of vitamin D in the body and history of sun exposure on demyelinating disorders and this is an area in need of further study.[159]
Smoking
One study reports that smoking is more frequent in MS than NMO for two case cohorts, Canadian (37.5% vs. 10.5%, P = 0.039) and Chinese (14.5% vs. 0%, P = 0.004).[150] History of smoking is also reportedly inversely correlated to NMO in another study in which 72% of whites, 19% African-American, and 8% of Asian with NMO answer no to smoking history compared to the control group.[249]
Other
Determinant and protective factors like breastfeeding and daycare exposure are also reported in different populations for NMO patients.[70,82]
GENETIC RISK FACTORS IN NEUROMYELITIS OPTICA
Genetic predisposition of NMO to different alleles of Class I and II human leukocyte antigen (HLA) has been studied since NMO was considered a variant of MS. Studies performed before 2001 on natives of Canada with demyelinated lesions in optic nerve and cervical spinal cord showed association of these lesions with HLA alleles DRB1 and DQB1.[181] The specific allele HLA-DRB1*03 presents a risk for NMO in the French population.[161] In Brazilian NMO-Ig-positive patients and Afro-Caribbean populations, HLA-DRB1 * 03 is found to be more common than in healthy controls.[64,34]
In France, no association is found between NMO patients and HLA-DR-DPB1*05:01; nevertheless, a different investigation found this allele in NMO patients of African-American and Latino population.[48,96] In the Han Chinese population, DRB1 * 1602 is found to be higher in NMO patients in comparison with MS patients; DRB1*0501 correlated with higher risk of NMO.[280]
Protective factors
In Asian populations, AQP4 Ig seropositive or seronegative HLA-DRB1*0901 is protective against NMO.[302] In Southern Han Chinese population, HLA-DRB1*0901 is less common than in healthy controls (Puncorr = 0.022, OR: 0.194, 95% CI: 0.043–0.876).[280] In this population, reduced risk of NMO is associated with the polymorphism in CD58 with the haplotype HATTACGG.[186] Another protective effect on the risk for NMO is found in people with single nucleotide polymorphism (SNP) in CYP7A1 in chromosomes 8q11-q12.[127]
Genes associated with AQP4
Studies in Chinese patients found the 3′ UTR region of AQP4 gene to be susceptible in several sites to SNP that may represent a risk for NMO.[288] Matiello et al. in a study of AQP4 SNP reported two missense allelic mutations at Arg 19 that result in array formation changes of the AQP4 protein and are specific for NMO.[167]
In AQP4-Ig-positive Japanese patients, the allele frequency of T rs2075575 is higher than in controls (50% vs. 25.7%; P = 0.0036) and represents higher risk for AQP4-Ig NMO.[199]
Other genes associated with neuromyelitis optica
Genes involved in regulation of the autoimmune system and regulation processes are found in NMO patients with lesions.[239] In NMO AQP-4 seropositive Chinese patients, a higher frequency of polymorphism in interleukin 17 (IL-17) gene compared to healthy controls is observed.[283] Upregulation of inflammatory cytokines like IL-17, IL-6, and IL-32 is seen in patients with increased levels of these cytokines in plasma which could describe the process of NMO immune-mediated chronic inflammatory disease.[281] Programmed death-1 (PD-1) receptor gene is associated with inflammatory and autoimmune diseases such as MS, rheumatoid arthritis, and allergic asthma.[66,224] The polymorphisms in allele PD-1 PD-1.3 G/A is found in a higher frequency in NMO patients (P < 0.026) compared to the healthy controls and is found in familial cases of NMO and MS.[17] Han Chinese population with polymorphisms of CD58 (haplotype TAGCCCAA) have a higher risk for NMO.[156]
MOLECULAR MECHANISM OF NEUROMYELITIS OPTICA
Antibody mediated damage
The major pathological mechanism of injury in seropositive NMO involves the autoantibodies aquaporin-4 (AQP4-IgG) binding to aquaporin-4 water channels in the astrocytes of brain, spinal cord, and optic nerve, followed by inflammation, disruption of blood–brain barrier, and complement-dependent cytotoxicity.[153,278] Pisani et al., found that AQP-4 antibodies bind to at least two different epitopes made of three extracellular loops which changes its conformation organizing it into a supramolecular structure known as the orthogonal array of particles.[218] CNS-derived human fetal astrocytes are found to react with the sera from NMO-IgG-positive patients resulting in natural killer cell degranulation, antibody-dependent cellular cytotoxicity destruction of astrocyte, complement-dependent attraction of granulocytes, and an increased permeability of the blood–brain barrier.[278] Sera from MS patients did not react with the fetal astrocytes.[278]
Role of complement
The MAC-inhibitory protein, CD59 is responsible for protection from membrane attack complex (MAC) formation in AQP4-expressing tissues in the periphery of seropositive NMO patients.[299] CD59 and CD55, complement-regulating proteins also known as decay accelerating factor, are produced in limited quantities in the brain, providing limited ability to regulate complement.[251] While peripheral injury is not usually seen due to sufficient production of CD59, activated complement, inflammation, and injury were seen in skeletal muscle and kidney of CD59−/− rats.[251] Intracerebral injection of AQP4-IgG caused astrocyte damage, inflammation, deposition of activated complement, and demyelination in CD59−/− rats.[300] CD59+/+ rats showed minimal complement deposition and loss of AQP4 under the same treatment.[300] NMO-IgG-dependent complement-dependent cytotoxicity is also seen in astrocyte cultures and ex vivo spinal cord slice cultures in both CD59−/− mice and in CD59+/+ mice after inhibition by a CD59 neutralizing antibody.[307] Human complement with NMO-IgG injected intrathecally between the L5 and L6-produced white matter lesions in the spinal cord.[307]
T-cell-mediated damage
T cells may also play an important role. T cells from mice lacking AQP4 channels recognize AQP4 epitopes, unlike the T cells of wild-type mice.[57] TH17 cells specific for myelin-oligodendrocyte glycoprotein damage retinal ganglion cells and axons within the spinal cords of wild type.[57] This not only demonstrates a role for T cells in the mechanism of NMO (though the exact mechanism is not fully elucidated) but also suggests thymic negative selection plays an important role in removing autoreactive T cells, further evidenced by a higher frequency of reactive T cells in NMO patients.[57]
Other mechanisms
Autoantibodies against myelin–oligodendrocyte glycoprotein, a membrane protein expressed on the oligodendrocyte cell surface and the outermost surface of myelin sheaths, are found in AQP4-IgG-seronegative patients who meet the diagnostic criteria for NMO.[139] In addition to complement-related pathology, passive transfer of AQP4-IgG also caused deposition on retinal Müller cells and decreased AQP4 expression, and increased glial fibrillary acidic protein (GFAP) and is associated with retinal abnormalities including thinning of the retinal nerve fiber layer.[72] The loss of AQP4 took place even in the presence of prior complement inactivation, as opposed to the complement-dependent injury typically seen in the brain, spinal cord, and optic nerve.[72]
SYMPTOMS OF NEUROMYELITIS OPTICA
The international criteria for the diagnosis of NMOSD include core clinical characteristics related to the optic nerve, spinal cord, area postrema, brainstem, diencephalic, or cerebral presentations.[270,289] Optic nerve involvement can be unilateral or bilateral[163] and is a painful condition worsened by movement with decreased visual acuity in the affected eye and is the most common initial symptom.[18,187] Half of patients lose functional vision within 5 years of onset.[51,161,290] Myelitis involvement classically involves more than three spinal cord segments.[163] Urinary dysfunction is common in patients with spinal cord lesions.[298] Sensory symptoms such as numbness, dysesthesia, pain, and tonic spasms are well documented and neuropathic pruitis and sudden sensineurial hearing loss are also reported.[230,262,290,308] Headache of several etiologies is reported and is another possible first-presenting symptom.[163] NMOSD patients are also at an increased risk of seizures.[193] Involvement of the area postrema of the medulla, along with related nucleus solitaries, ventrolateral respiratory center, and nucleus ambiguous symptoms, can cause symptoms that include intractable nausea, vomiting, and hiccups.[1,12,112] Intractable vomiting is the initial presenting symptom in up to 12% of AQP-4-positive patients.[95] Atypical manifestations can include atypical transient asymptomatic elevation of creatine kinase levels. In other brainstem, diencephalic or cerebral presentations, hypersomnia and narcolepsy can be an initial symptom, presenting in both the hypothalamus and the temporal lobe.[21,145] Hypothalamic involvement can also include hyperthermia and galactorrhea.[91,285] Psychology changes may be associated with NMOSD.[186] Cognitive changes have been seen in NMOSD patients including impairment, depression, and suicidal ideation.[30,86,277] It was found that this criteria also apply well to the pediatric population.[46]
CLINICAL DIFFERENTIATION AND COMORBIDITIES OF NEUROMYELITIS OPTICA
Neurological pathologies present from several etiologies and the clinician must be able to identify subtle differences between the presentations by taking a detailed medical history.[269] The diagnosis of NMOSD from an alternative or concomitant autoimmune or neurologic disorder is identified through disease indicators such as AQP4 but the clinical presentation is significant in the differential.[104,105,108]
The predominant symptom in NMOSD is ON. As NMO and NMOSD are recent classifications apart from MS, the presentations between NMOSD and MS are similar. ON as a visual defect other than cecocentral scotoma and severe vision loss in the chronic stage occurs more frequently in NMOSD than in MS, as do the brainstem symptoms such as hiccup and nausea, myelitis with neuropathic pain, complete paraplegia, and tonic spasms.[14,121,261,269,295,122,128,129,173,191,223,225,260] Although the prevalence and profile of cognitive impairment and depression is equal in NMOSD and MS, NMOSD has significantly higher rates of recurrent depression and suicidal ideation.[186] Acute disseminated encephalomyelitis (ADEM) is another demyelinating disorder of the CNS that presents with ON. Clinically, NMOSD presents with a higher female predominance, focused neurologic symptoms at onset, higher recurrence rate and is less common to pediatric populations and lacks the characteristic onset encephalopathy of ADEM.[94,129,142,143] Idiopathic causes of both acute transverse myelitis (ATM) and ON must also be considered. Idiopathic ATM presents as an inflammatory spinal cord disorder without evidence of other etiologies, such as the characteristic paroxysmal spasms, female predominance, or recurrent course seen in NMOSD.[128,131] Ethnicity must also be considered as most patients with ATM convert to MS within European populations, but not in Asian populations.[79,132,268]
Idiopathic ON can be considered if the clinical presentation of relapsing disease course, bilateral simultaneous nerve involvement, and poor visual outcomes of NMOSD are absent.[166,289] Other diseases, like inflammatory disease due to antibody myelin oligodendrocyte glycoprotein (MOG), present with isolated neuritis and fewer relapsing courses.[133]
NMOSD is commonly associated with autoimmune disorders.[76] Sjogren's syndrome is the most common accompanying autoimmune disorder. Sjogren's myelitis has longitudinal spinal cord involvement that can be diagnosed as NMO or is AQP4+; therefore, most CNS involvement is due to coexisting NMOSD rather than direct CNS involvement.[130,178,310] In multiple studies, these types of comorbidities amongst NMO patients are discussed as an indication that NMO could be a complication of multisystem rheumatologic disease. Furthermore, the coexistence of these autoimmune comorbidities also suggested that NMO is an indication of a genetic propensity toward humoral autoimmunity.
In the limited research into the concurrent cases of myasthenia gravis (MG) and NMOSD, AQP4-NMOSD is recognized to be associated with other autoimmune manifestations in 25–50% of cases, suggesting that patients with NMOSD and MG have a predisposition to autoimmune disorders.[48,152,169,192,219,265] Systemic lupus erythematosus can present with several neurological symptoms including headache, seizure, and hemiparesis but only a few have ON or myelitis pointing to susceptibility to multiple autoimmune disorders.[219,294] A high prevalence of thyroid abnormalities is observed in NMOSD patients, which may be due to the AQP4 shown to be present in the thyroid tissue.[157]
Neuro Behçet's disease is a subset of Behçet's disease involving the CNS and can resemble longitudinally extensive transverse myelitis (LETM) of NMOSD.[7,20,39,89,118,149] The diagnosis of Behçet's normally includes ulcers, but the neuropathic symptoms can appear before the systemic symptoms and are not included in the recent diagnostic criteria.[56,118,6] Behçet's is similar to NMOSD with headache, a progressive disease course and requires treatment.[5,56,123,126,301] Gluten enteropathy, or celiac disease, is also studied but causation has not been shown in NMOSD.[61] Pregnancy induces changes in the immune system and may also have an effect on NMOSD. NMOSD may increase the risk of miscarriage, but larger databases are needed to study this population outcomes and treatment.[75,196]
Invasive etiologies may also be considered; NMOSD can be misdiagnosed for primary CNS lymphoma; diagnostic studies are important to differentiate the two. CNS lymphoma should be considered in patients with LETM if they continue to worsen despite treatment.[22,74,89,115,144,241] AQP4-NMOSD can also present as a paraneoplastic syndrome, in which NMOSD symptoms present after the diagnosis of a tumor, especially in those over the age of 50, with the most frequent being carcinoma.[38]
Similarly, sarcoidosis is a systemic granulomatous disease that can also involve the spinal cord and optic nerve resembling phenotypes of NMOSD.[234,256] Neurosarcoidosis can present with systemic involvements of sarcoid, but without the systemic symptoms, the clinical presentation can appear to be very similar to NMOSD.[73,304]
Another process that can be considered in the differential is a spinal dural arteriovenous fistula. A spinal dural arteriovenous fistula is a vascular malformation in spinal cord that can present as subacute and progressive myelopathy; symptoms appear after exercise or prolonged rest.[274,93,111] Radiology or catheter angiography is required for diagnosis.
An additional cause of neurological disorders is infection. Syphilis is a sexually transmitted infection that can cause ON that can mimic NMOSD.[24,197,210,252] Other infections that can mimic NMOSD include Epstein Barr virus,[11] herpes simplex virus,[190] cytomegalovirus,[267] human t-lymphocytic virus,[279] dengue fever,[147] lyme disease,[174] tuberculosis,[100] Mycoplasma pneumoniae,[80] and Streptococcus pneumoniae.[238]
Finally, Leber hereditary optic neuropathy is the most common hereditary ON affecting males in the second or third decade of life due to mutations in the mitochondria and can be considered in the differential.[129]
DIAGNOSIS OF NEUROMYELITIS OPTICA
With improved sensitivity and specificity of immunoassay techniques, as well as a deeper understanding of the pathogenesis of the disease, NMOSD diagnosis criteria have appreciably evolved over the past two decades.[68] In 1999, the Wingerchuk group proposed its original diagnostic criteria, which was limited to CNS involvement of brain, optic nerves, and spinal cord [Table 1].[290] Since the original criteria had challenges in diagnosing patients presenting with symptoms involving other areas, the NMOSD diagnostic criteria were again revised by the same group in 2006.[68] The newly revised criteria included the addition of specific NMOSD-IgG serology and an emphasis on longitudinally extensive spinal cord lesions [Table 2].[292] In 2015, the International Panel recently proposed the latest up-to-date NMOSD diagnostic criteria for NMOSD diagnosis (IPND).[289] IPND has further subdivided NMOSD diagnosis based on a patient's respective laboratory IgG seropositive or seronegative status [Table 3].[289] Yet in clinical setting, both comprehensive medical history and specific patient symptom evaluations are still the crucial first steps in diagnosing NMOSD.[269] Consequently, detailed physical and neurological examination is essential to distinguish NMO from NMOSD-mimics, including but not limited to MS, ADEM, idiopathic ATM, sarcoidosis, and other disorders.[131] Since NMOSD is characterized by worse prognosis in comparison with MS, accurate and early diagnosis can be critical for preventing flares and relapse of monophasic NMOSD.
Table 1.
Neuromyelitis Optica Spectrum Disorders Diagnostic Criteria, Wingerchuk et al.[290]
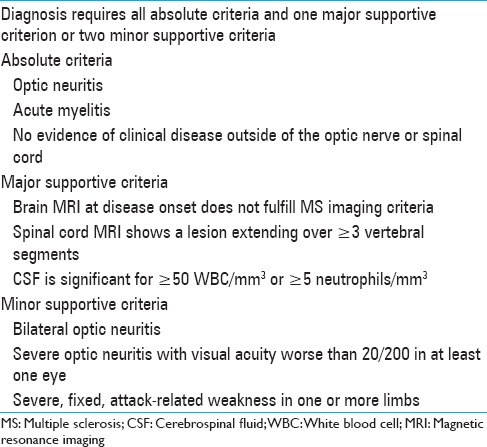
Table 2.
Neuromyelitis Optica Spectrum Disorders Revised Diagnostic Criteria, Wingerchuk et al.[292]

Table 3.
International Panel for Neuromyelitis Optica Diagnosis Neuromyelitis Optica Spectrum Disorders Diagnostic Criteria for adult patients, Wingerchuk et al.[289]

Neuromyelitis optica spectrum disorder brain and optic nerve MRI
Paraclinical imaging of brain-associated MRI lesions is widely employed for NMOSD supportive diagnosis but most importantly as a tool for differentiating NMOSD from MS.[146] Early asymptomatic NMOSD onset usually does not display any MRI scan lesions and almost always will be performed before the specific NMO-IgG biomarker serology.[67] However, if the lesions were present, imaging scan will reveal subcortical lesions without central veins.[137] The most common sites for abnormal brain lesions are brainstem and cerebellum, followed by area postrema, thalamus, hypothalamus, corpus collosum, periependymal-third ventricle, corticospinal tract, and finally, the hemispheric white matter.[43] In addition, vomiting in NMOSD patients demonstrates association with corresponding lesions in brainstem medulla.[289] While not visible on weighted-T1 MRI, NMOSD lesion abnormalities will display cerebral T2-/FLAIR hyperintensities in 60% of the patients.[168,220]
In patients presenting with ON, T1-weighted gadolinium coronal images or an increase in T2-weighted MRI signal of optic nerve and optic chiasm are seen unilaterally or bilaterally, after 2 weeks of onset, and may be associated with severe vision loss.[236] Also, distinguishable diagnostic NMOSD imaging sequences include bilateral optic nerve lesions with consequent extension into optic chiasm.[108] In addition, in patients presenting with acute ON, there is a presence of enhanced and diffused T2-weighted orbital MRI signal.[289]
Neuromyelitis optica spectrum disorder optical coherence tomography
ON is one of the primary clinical manifestations detected in 55% of NMOSD patients and leads to progressive changes in vision, reduction in high or low contrast visual acuity, and potential complete vision loss within several weeks from disease onset.[228] Affected structures include optic nerve and optic chiasm, with the retina being one of the most affected regions due to thinning of peripapillary retinal nerve fiber layer (pRNFL) and retinal ganglion cell-inner plexiform layer (GCIPL).[165] For several years, a great effort has been dedicated to understanding the role of optic coherence tomography (OCT) as a minimally invasive imaging technique to diagnose NMOSD. In addition, OCT is employed to assess neurodegenerative damage to pRNFL and GCIPL via retinal examination in NMOSD patients.[198] OCT employs low-coherent light to produce backscattered and reflected cross-sectional high-resolution 3D images of retinal structures that reveal NMOSD-specific intraretinal pathologies, but most importantly, OCT can provide differential diagnosis between MS and NMOSD.[165,198] In NMOSD patients, acute single ON attack causes more damage to pRNFL and GCIPL layers that can be detected via OCT.[146] Currently, OCT is widely used to measure NMOSD disease progression course, as well as outcome response to NMOSD neuroprotective therapies.[269]
Neuromyelitis optica spectrum disorder spinal cord lesion MRI
The hallmark of NMOSD is acute myelitis, which is associated with acute continuous LETM lesion patterns that are detected via T2-weighted sagittal spinal MRI.[289] NMOSD lesions are usually centrally located and cover three or more vertebral segments.[49] Previous research has demonstrated that those lesions often involve swelling of a gray matter of the spinal cord with cervical lesion extension to the brainstem.[146] Chronic and older NMOSD spinal cord lesions are characterized by patchy appearance with longitudinally extensive spinal cord atrophy.[146] In comparison, MS attacks tend to be less severe with MS patients displaying patchy lesions of spinal cord MRI that are rarely extend over one vertebral segment and are often located peripherally.[13,146]
Neuromyelitis optica spectrum disorder cerebrospinal fluid analysis
Examination of cerebrospinal fluid (CSF) can be performed in patients with acute NMOSD attacks since many NMOSD CSF distinctive cell types and biomarkers disappear once patients go into remission.[106] Suggestive NMOSD CSF diagnosis findings include moderate or severe pleocytosis (up to 1000/mm3), high neutrophil granulocyte count, and presence of eosinophils.[129] Presence of those cell types in NMOSD CSF is supportive in distinguishing NMOSD from MS.[269] As many as 30% of the patients may also present with CSF oligoclonal bands.[289] Presence of higher levels of GFAP indicative of astrocytic damage is also usually detected in CSF of NMOSD patients.[258] GFAP, cytoskeleton intermediate filament, indicative of astrocyte damage currently serves as a novel biomarker useful in differentiating NMOSD from MS, especially during NMOSD ON acute episodes.[258] Recent publications also indicate higher levels of electrolytes, such as chloride, in CSF of NMOSD patients, present during acute phase of ON; however, the chloride levels have reported to be much lower during the phase of acute myelitis.[4] Several publications have appeared in recent years documenting presence of higher levels of interleukin-6 (IL-6) and interleukin-6 receptor (IL-6R) in NMOSD patients when comparing them with MS patients.[271] Both IL-6 and IL-6R can also serve as additional biomarkers facilitating differentiation of NMOSD from other demyelinating diseases such as ADEM, idiopathic ATM, idiopathic ON, neuro-Behçet disease, and Leber heriditary optic neuropathy among others.[129,282]
Neuromyelitis optica spectrum disorder serum AQP4-AB IGG
Beyond certain characteristic clinical manifestations and specific neuroimaging findings, the presence of antibodies against water channel aquaporin-4 (AQP4), which is expressed in the astrocyte cell plasma membrane, is central for NMOSD diagnosis.[32] Eighty percent of the NMOSD patients test positive for AQP4-IgG.[124] AQP4 is also associated with peripheral tissues; however, in CNS, it is responsible for maintenance of cerebral water balance, blood–brain barrier development, and integrity.[207] AQP4-IgG positive antibody is produced by plasmablasts in peripheral circulation and is more frequently present in NMOSD patients presenting with MRI findings of ON and transverse myelitis.[276] In cases where patients may test negative for AQP4-IgG, a physician can also order a MOG-IgG serum antibody titer that binds to specific CNS tissues.[160] Patients who test positive for MOG-IgG are also at high risk of developing NMOSD.[160] In comparison with AQP4-IgG, a MOG-IgG serum antibody targets retinal nerve fibers of the patients.[257] MOG-IgG-positive patients also present with longitudinally extensive ON lesions. Both antibodies are measured quantitatively by ELISA testing; however, NMOSD disease course and progression is independent of the titer size.[124] NMOSD patients with low titers have the same disease course and progression as patients with a high titer.[124] Recent studies have also shown that patients who test positive for both AQP4-IgG and MOG-IgG biomarkers may suffer from visual, motor, and cognitive impairment due to inability of their neurons to function and relay information in a synchronized manner.[284] Although AQP4-Ab IgG antibody is also expressed in peripheral tissues, such as kidney stomach and skeletal muscle, in NMOSD patients, those other organs are not affected by AQP4-Ab IgG antibody.[77] A recent study shows that this occurs because the AQP4-Ab IgG receptor epitopes hold different supramolecular assemblies that account for low affinity of AQP4-IgG for its’ receptors in those tissues.[232] This novel finding might explain specific targeting of CNS tissues, resulting in predominantly CNS abnormalities.[232] Several recent publications document a potential role of soluble complement proteins in early oligodendrocyte injury in NMOSD patients.[266] The complement cascade is activated following AQP4-IgG binding to astrocyte's AQP4 epitope receptor, resulting in subsequent deposition of the complement MAC on the same or neighboring oligodendrocytes.[266]
TREATMENT OF NEUROMYELITIS OPTICA
Identifying an effective therapy for NMO is founded upon a basic understanding of the biological mechanisms that lead to the disease. Recent studies postulate that relapse in NMO disease has an association with chronic stress and hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis.[253] Consequently, during chronic stress or HPA axis overactivity, there is an overproduction of corticosteroids which causes the desensitization of glucocorticoid receptors in granular and lymphoid cells.[81,158,253] Elevated levels of catecholamines increase the release of cytokines MMP-9, IFN-gamma, TNF-alpha, and IL-6, which are in turn responsible for blood–brain barrier damage and AQP4 antibody production.[59,216] As a result, the entry of AQP4 antibodies into the brain becomes facilitated and disease is exacerbated.[59,216] The main therapies for NMO target specific steps in this disease process; it entails maintaining the disease in remission and preventing sudden outbreaks of symptoms. Classic corticosteroid and immunosuppressant clinical studies have contributed to the understanding of NMO and lead to the development of novel therapy options.[286] Treatment specifically focuses on diminishing inflammatory and/or autoimmune mechanisms that are characteristic of the disease. Monotherapy yields variable results and multiple compound therapy potentiates the effectiveness of the treatment.[29,171,184] Current research focuses on targeting auto anti-AQP4 antibodies and their lymphoid mediated production.[134]
The use of intravenous corticosteroids and/or plasmapheresis is two preventative measures to control sudden outbreaks for NMO patients. According to present literature, low-dose corticosteroid use is effective and reduces relapse rates in patients within a 1-year period.[286] These steroid hormone derivatives also carry reduced inflammatory properties, induce leukocyte apoptosis, hinder granulocyte migration, minimize capillary permeability, and reduce relapse rates.[29,134,171] For patients with acute crisis, plasmapheresis can be considered an alternative therapy. Combination therapy with immunosuppressors and plasmapheresis exhibits decreased anti-AQP4 antibody serum levels.[171,242,289]
There are various options for treatment during remission on the market; however, selecting an appropriate treatment plan can be complicated. For this reason, choosing a first-line therapy is the focus of recent studies. Chemo-pharmaceuticals such as mycophenolate, cyclophosphamide, and methotrexate show certain therapeutic effects for plasma cell dyscrasia and immunosuppression.[27] However, these medications should not be used as a monotherapy due to unreliable and variable effects.[184] Dual and combination therapy with chemopharmaceuticals does show improvement in patient outcome.[171,184] Examples include methotrexate in combination with oral corticosteroids resulting in disease stabilization,[171] and prednisone and azathioprine in reduction of relapse rate.[29,53,138] The latter is also used as a first-line therapy for remission prevention. Only cyclosporine A, combined with oral corticosteroids, has induced remission in NMO patients.[138]
An alternative therapy is rituximab, a selective monoclonal antibody that reduces serum CD20+ B lymphocytes, with effects lasting weeks due to its long half-life which include observed benefits such as reduced relapse rates and maintained or improved patients’ neurological health.[54,212] Despite these claims, not all patients respond favorably to this medication, as several cases report relapse episodes after therapy initiation.[171,212] This can happen due to a sudden increment of the anti-AQP4 antibodies expressed by the patients after a 2-week period.[171]
Therapy against key cytokines involved in NMO pathogenesis has drawn considerable interest. IL-6 is a key factor in B-cell differentiation and antibody production.[263] Tocilizumab is a humanized anti-interleukin 6 receptor antibody that has shown to reduce neuropathic pain and fatigue within NMO patients.[15] TNF-alpha plays a critical role in neuro-inflammation linked to neurodegeneration and is regulated by the NF-kB pathway.[185] Simultaneous stimulation of beta-adrenergic and TNF-alpha receptors has led to variable expression of certain NF-kB genes and stimulation of genes associated with IL-6.[255] The NF-κB pathway has been shown to modulate chemokine, cytokine and adhesion-molecule expression, CNS inflammatory cell migration, and along with TNF-alpha, could prove to be a future target for site-directed therapies.[275] Further research is needed into NF-kB function as a signaling mediator and as a possible facilitator of crosstalk between multiple signaling cascades in order to ensure effective therapy.[275,185,255]
Presently, interferon beta and natalizumab are no longer used as treatment options due to exacerbating NMO relapses or symptoms.[221,209] In recent years, new therapies are surfacing for NMO patients and a few have promising results, while others must be investigated further. Aquaporumab, a monoclonal NMO-derived antibody of high affinity to AQP4, is a prospective first-line treatment for relapses or acute and severe attacks.[134] Eculizumab, a humanized monoclonal antibody, neutralizes the C5 in the complement cascade and appears to reduce attack frequency and stabilize the neurological health in patients.[221] Finally, surgical intervention is the most novel and drastic approach for treating NMO. Recent studies have indicated that vascular hypoxia could play a role in NMO exacerbation.[227] Omental transplantation could decrease stress, and future relapses, by revascularizing the hippocampus, temporal lobes, and the surrounding structures. This would normalize the activity of the HPA axis and reduce its effects on the immune system of the NMO patient.[226]
DIETARY SUPPLEMENTATION IN NEUROMYELITIS OPTICA
Diet and nutrition, as either a management paradigm or as possible factor in NMO pathogenesis, has been minimally investigated. Current, cutting edge research, though, is starting to break the surface in three important areas: Vitamin D and its’ regulatory role in the immune system; cholesterol and cholesterol metabolites as inflammatory regulators; and finally, aberrations to the gut microbiome as inducers of pro-inflammatory T-helper cells.
Vitamin D
To date, there are no studies as to any palliative or curative efficacy of a vitamin D treatment in patients with NMO. MS research, though, has touched on the question and recent investigations into the effect of high-dose vitamin D therapies in reducing relapse rates are divided, some showing a promising reduction in relapse rates, while others are inconclusive.[8,102,114,148,176] As of 2016, there are six active large-scale studies into high-dose vitamin D treatment in reducing MS symptom severity and rate of relapse, with results pending.[8] A single prospective case control study to date into a putative neuroprotective role for vitamin D against demyelination diseases showed the risk for MS significantly decreased with increasing levels of 25-hydroxyvitamin D in blood.[188]
Cholesterol
For its role as a precursor in myelination of neurons by both CNS oligodendrocytes[235] and peripheral nervous system Schwann cells,[78] cholesterol synthesis and homeostasis in glial cells are considered a valid area of interest in demyelinating pathophysiology.[23,28,42] Recent studies hone in on specific hydroxycholesterol metabolites, such as 25 and 27 hydroxycholesterol, known control points in microglia inflammatory regulation.[44,103] Studies do show that there is a correlation between distinct genetic variants in 25 hydroxycholesterol metabolism and NMO, as well as increased levels of both 25 and 27 hydroxycholesterols, both in NMO patients, and as markers of severity of acute relapse[44] Though such research does not imply that dietary cholesterol nor even systemic cholesterol homeostasis may have either protective or causative role in NMO pathology, it must be noted that dietary cholesterol has now begun to be a topic of research in MS.[28,235]
Gut microflora
One of the most interesting recent discoveries as to the actual pathogenesis of NMO may lie in the ubiquitous commensal flora of the human gut. Recent gut microbiome analyses of NMO patients show a marked overabundance C. perfringens.[55] The AQP-4 epitope that CD4+ T cells target in NMO is defined as a 10 residue sequence that shares 90% homology to a specific ATP Binding Cassette Transporter of C. perfringens.[305] Pro-inflammatory T-helper 17 (Th17) cells from NMO patients do proliferate in response to this 10 residue peptide sequence.[273] Induced upregulation of Th17 with ileal colonization of segmented filamentous bacteria increases susceptibility to autoimmune encephalomyelitis (EAE), an experimental model of MS.[97,98,151] A logical sequitur to these findings is dietary modification or fecal transplantation to reduce pro-inflammatory effects of C. perfringens or as a treatment to avoid acute relapse. Dietary modifications could be avoidance of salt and long-chain fatty acids, both shown to be inducers of pro-inflammatory Th17.[98,297] Fecal transplantation, a treatment that is rapidly gaining acceptance worldwide, is already highly effective in treating recurrent Clostridium difficile infections in irritable bowel syndrome.[83,202]
SYMPTOM MANAGEMENT OF NEUROMYELITIS OPTICA
NMO is a challenging neurodegenerative disease whose long-term management strategy is confounded by the high prevalence of pain, urinary incontinence, loss of mobility, fatigue, and depression.[60,45,69,225,247] Long-term management strategies in NMO are aimed at rehabilitation and recovery of any loss of mobility for the patient, as well as improvement in the patient's quality of life via symptomatic treatment.[125] The current physical rehabilitation strategies, as well as pharmacological therapies, employed for NMO patients are similar to those used for MS, as both diseases show varying rates and degrees of impairment to bladder and bowel function, limb weakness and impairment to movement, pain, and depression.[195]
Mobility and ambulation
Physical therapy, in conjunction with pharmacological symptomatic management, is effective in improving measures of quality of life, functionality, and independence.[69,247] Cases studies highlighting functional blindness and advanced loss of ambulation do show increased functional independence measures (FIM) scores, but case studies show that such patients remain paraplegic and with no restoration of sigh t.[195,240] A basic challenge in rehabilitation therapy in both NMO and MS is fatigue, a common result of the pharmacological treatments, pain, sleep dysfunction, as well as the underlying nerve conduction disturbance.[34] Aerobic exercise, with a gradually increasing duration, reduces fatigue and allows effective rehabilitation.[215] Minimal impact aerobic exercise programs, aimed to reduce muscle wasting, slow muscle weakness, fatigue and depression, and even raise functional ambulation and FIM scores.[35,215,240]
Urinary function
A recent study focusing on urinary dysfunction in NMO patients found detrusor-sphincter dyssynergia and detrusor overactivity, either alone or together, in more than half of the patients assessed.[59] The dysfunction of urinary voiding shows a significant correlation to the generalized neurodegenerative progression of the disease.[60] Similar to MS, NMO patients often suffer incontinence with or without urinary retention, dependent upon the location of the lesion. Cervical lesions damage both sympathetic and parasympathetic outflow tracts, while a parasympathetic loss predominates with lumbar damage.[45,50,175] A review of antimuscarinics in the treatment of urinary urgency and incontinence determined solifenacin, oxybutynin, and propiverine to be most effective.[35] Detrusor overactivity, causing increased urinary frequency, is managed with pelvic muscle contraction exercises and localized electric muscle stimulation.[50,205,213,273] Intra-detrusor Botox® (onabotulinumtoxin A) injection is a very effective tri-annual intervention strategy to minimize incontinence, frequency, and urgency.[50,125,172,213] Treatment of urinary retention is treated with cholinergic agonists, such as bethanechol, a pure muscarinic agonist.[19,125] Newer, less lipophilic agents, such as tolterodine and trospium, are effective with less central side effects.[119] Otherwise, urinary retention is alleviated with clean intermittent self-catheterization.[119,125]
Pain
With a prevalence of up to 86%, more than twice as common in occurrence compared to MS, and up to three times more severe, pain is a great challenge for management of NMO patients.[33,225,309] The pain manifests from both tonic muscle spasms as well as prolonged dysthesia and paresthesia of neuropathic pain.[33,309] Current pain treatment commonly targets GABAergic agents, such as carbamazepine, baclofen and gabapentin, α2 agonists such as tizanidine, SNRIs, tricyclics, and traditional μ opioid agonists.[125] Current research, however, is now targeting the underlying mechanisms of the neuropathic pain.[33,225,309] For example, the cannabinoids are an interesting new drug target, given the role of local astrocyte-produced 2-arachidonoylglycerol (2-AG), a cannabinoid, in decreasing glutamatergic signaling and augmenting GABAergic signaling.[211,231] Co-expressed molecules in Aquaporin 4 (AQP4) membrane micro-domains include excitatory amino acid transporter 2, which limits synaptic glutamatergic signaling by removing synaptic glutamate.[33,88] This intrinsic control of glutamatergic signal is lost with antibody-mediated destruction of AQ4.[88] Glutamatergic antagonists must also be mentioned, as low-dose ketamine and memantine are effective in multiple etiologies of neuropathic pain.[2,33,237]
Depression
A recent study showed a direct positive correlation between the severity of depression in NMO and the degree of neuropathic pain reported by patients.[45,85,186,203] Though the rates of cognitive impairment in MS and NMO are similar, the rate of recurrent depression and suicidal ideations are higher in NMO.[45,85,186] Recent studies show that NMO patients suffer high rates of depression, similar to MS, the two greatest causal factors being pain and fatigue.[45] Current NMO depression management is similar to that of MS: SNRIs, such as duloxetine and venlafaxine; SSRIs, such as citalopram and sertraline; atypical antidepressants, including mirtazapine and the triclyclic amitriptyline, are all used for pain management.[45,203] Stimulants such as modafinil, effective in some autoimmune neurodegenerative cases, is effective to combat fatigue.[125,246]
SURVIVAL AND PROGNOSIS OF NEUROMYELITIS OPTICA
The prognosis of NMO can be challenging. The disease has either a monophasic or relapsing nature. NMO relapse can serve as the main indicator for survival and prognosis.[290,292] Other risk factors such as age of onset, genetics, gender, and ethnicity affect long-term outcomes. Additionally, other preexisting autoimmune diseases can also exacerbate the effects of NMO.[48,171,243,296] The factors that lead to a worse clinical outcome can be multifaceted.
The age of onset of NMO can severely affect the patient's prognosis. The average age of onset for NMO is 39 years, but the disease can manifest in children and adults as well.[25,244] Age correlates to the degree of NMO patients’ disability in cohort studies with AQP4 sero-positive patients.[292] In a recent study, patients had a hazard ratio of 1.7 for disability when compared to a subject 10 years younger.[244] Another study found that the onset of NMO in patients below the age of 30 serves as a protective factor while the onset in patients above the age of 50 has higher chances of developing clinically significant symptoms.[99] On the other hand, monophasic NMO does present earlier, with average age of 27 years. Monophasic presents with constant relapses, a torpid progression, and aggressive behavior, with neurological disability and a poor prognosis.[293]
The most important factor for survival and prognosis in NMO is relapse.[99,164,222,292,294] Approximately 80% of patients with NMO have a relapse,[291] 60% relapse within the first year, and 90% relapse 3 years later.[290] Patients who experience worsening clinical prognosis tend to exhibit more than two relapses within the first 2 years of onset and a severe initial episode.[291] The prognosis of patients with relapses is not favorable, most attacks are moderate or severe, remissions are not constant, and neurological incapacities accumulate with time.[99]
Over 60% of patients will develop severe vision loss within the first two years of onset and a severe ambulatory disability within the first 5 years of the disease.[222] The coexistence of an autoimmune disorder with NMO influences the long-term prognosis and is a portent for future relapse.[164] Early identification reduces relapse rates and it is correlated with a better prognosis.[164] Mortality rates are approximately 32% within the first 5 years; most of the cases are cervico-bulbar and exhibit a compromised respiratory capacity.[222]
Gender can affect the severity of NMO prognosis. Males have a higher age of onset (48.7 vs. 41 years, P = 0.037), and though they show a higher incidence rate of isolated myelitis, males present with a milder degree of ON upon onset and are more likely to not suffer ON attacks.[164] Although females are nine times more at risk for NMO compared to males,[62] the severity of disease among women is comparably less. Females have a lower age of onset for NMO, giving a better prognosis overall and survival.[99,244,62,293] Other factors, such as increased number of acute attacks within the first two years, show no significant results within various cohort studies.[244,292]
CHARACTERISTICS OF PATIENTS IN PUERTO RICO WITH NEUROMYELITIS OPTICA
Introduction
Despite recent advancements in understanding and diagnosing NMO, there has never been an epidemiological study of NMO patients from PR specifically.
For this study, we obtained the records of all NMO patients who visited Caribbean Neurological Center in PR. Table 4 provides a summary of the characteristic of these patents. There are nine NMO patients at the Neurological Center, all females aged from 26 to 63 years with average age of 41. The average age of disease onset was 35 years. For diagnosis, 90%, or eight out of nine patients, developed antibodies to aquaporin-4 (NMO-IgG or AQP4-Ab) which is a highly sensitive and specific NMO serum marker. Of the nine patients with NMO, 90% of patients reported that they are not able to work due to their medical limitations and 11% claimed to be totally disabled. Sixty-six percent of patents were using walking aid since they were no longer able to keep their balance when walking.
Table 4.
Characteristics of patients in Puerto Rico with neuromyelitis optica

Environmental factors
Gastritis is one of the unique comorbidities found in Puerto Rican NMO patients. Multiple studies have found higher incidence and prevalence of stomach cancer in PR compared to non-Hispanic Whites populations in the United States.[300,217] Contributing factors include higher H. pylori infection and high dietary intake of salty foods and/or N-nitroso compounds.[101] One study done specifically in the Puerto Rican population found a statistically significant dose response for the index of salt intake and gastric cancer.[194] Increased dietary salt intake is linked to higher prevalence of autoimmune diseases. Increased dietary salt can induce T-cell reception to IL-23 signaling, a cytokine historically linked to multiple autoimmune diseases including NMO.[140,26]
Whether NMO patients in PR have active C. perfringens bacteria or not is not captured in our data. However, in a study done by Pait et al., chemical and biological contaminants in the marine sediments of southwest of PR were recorded and analyzed. According to their result, the southwest region of PR, specifically Guanica Bay, has over 1700 colony forming units of C. perfringes per gram of sediment sample.[201] C. perfringes usually exists in fecal pollution sources and its presence in water implies contamination of water by sewage or similar wastes, which could in turn be a risk factor for the development of NMO.
Despite conflicting evidence between populations, vitamin D deficiency could also be a risk factor for NMO illness. The population of PR is vitamin D deficient, with only 31.5% of the studied population having sufficient vitamin D levels.[259] There are studies that analyzed the prevalence of vitamin D deficiency with influencing factors such as obesity among Puerto Ricans and concluded that individuals with a higher adiposity had a lower vitamin D status.[229]
Smoking has been found as a most consistent nongenetic factor in different neurodegenerative diseases.[306] Among our NMO patients in PR, only one patient out of nine had a smoking history. Her average number of relapse in 1 year was higher compared to other patients. In addition, at age 31, she had right eye blindness, severe chronic fibromyalgia, and neuropathic pain. Whether smoking contributed to the state of her NMO progression remains uncertain but we can conclude she presented with the most exacerbations in the study.
Genetic factors
HLA-DRB1*03 was also the most prevalent allele found in MS patients from PR.[180]
Symptoms
Sensory symptoms, loss of motor strength in extremities, migraine headache, decreased vision acuity, seizure, vomiting, and psychiatric problems are among the most common initial symptoms in NMO patients from PR. Two of the nine patients were previously diagnosed with progressive-relapsing multiple sclerosis before being diagnosed with NMO due to similarities of symptoms between the two disorders.
Comorbidities
Thyroid abnormalities were the most frequent comorbidities among NMO patients in PR. Two of the common autoimmune disorders among Puerto Rican NMO patients were immune thrombocytopenic purpura and rheumatoid arthritis.
In a study conducted by Ajmera et al., they found comorbidities among NMO patients in United States that were reported in ≥2% of patients.[3] In comparison to their study, Puerto Rican NMO patients presented with some unique comorbidities that were not listed in the aforementioned study. These include allergy, asthma, seizure, gastritis, anemia, hyperlipidemia, arthritis, osteopenia, bronchitis, and scoliosis. The differences among comorbidities can be related to multiple factors such as ethnicity, environmental factors, and diet habits due to cultural differences.
Future studies measuring these factors in a broader range of NMO participants will be required to validate and to expand upon these results.
Survival and prognosis
The average onset age for Puerto Rican NMO patients was 35 ranging from 15 to 59 years old. The patient with older age of onset had more sever comorbidities compared to the younger ones. These included fibrocystic disease of breast, esophageal hiatus hernia, osteopenia, and osteoporosis. Whether these differences are as the result of late age of NMO onset or normal aging comorbidities needs to be further investigated.
More than half of Puerto Rican NMO patients had at least one relapse in 1-year period, which again is the most important factor for survival and prognosis. Long-term studies can chart these outcomes and capture prognostic data for future generations.
DISCUSSION
Even though according to the information we obtained that all the NMO patients from Caribbean Neurological Center were female, such a small prevalence of NMO and the lack of male patients suggest that a systemic collection and publication of NMO patients data and epidemiology could benefit the process of investigation, treatment innovation, and improvement of NMO within this population and worldwide.
CONCLUSION
Improving knowledge of NMO pathogenesis is critical in developing diagnostic methods for earlier detection and planning new effective treatments. Thus, an extensive understanding in a range of information regarding NMO epidemiology, environmental and genetic factors, molecular mechanism, symptoms, clinical differentiation, treatment, dietary supplementation, management, and survival and prognosis is essential. As of now, there is no treatment that completely cures the NMO and patients can face debilitating disabilities throughout the course of their disease. Multiple compound therapy including corticosteroid, immunosuppressant, monoclonal antibody, and plasmapheresis reduces the relapse rates and also decreases anti-AQP4 antibody serum levels in some cases.[286]
Although the underlying mechanism of NMO has already been elucidated, implicating predominantly the existence of (AQP4-IgG) antibodies in NMO patients, changes in ethnicity and environmental factors also show their pivotal role in variations of NMO clinical features and prognosis.
One of the main limitations of this study was our small sample size of NMO patients. This prevented us from performing any statistical analysis or hypothesis testing to establish comprehensive results. After reviewing all these patients’ information, our findings suggest a unique set of comorbidities among NMO patients in PR that were different compared to the NMO patients in United States. They also had higher female-to-male ratio with a wide range of age of onset from 15 to 59 years.
These differences could be associated with environmental and/or genetic factors that we discussed earlier in our study. They include higher incidents of gastritis, presence of HLA-DRB1 * 03 allele, higher exposure to C. perfringens, vitamin D deficiency, and higher daily intake of salt in diet. Some of these factors may be eliminated by reducing the exposures to the infectious agents and improvements in access to preventive and treatment care. Further research studies are certainly warranted to confirm the prevalence and epidemiology of NMO in PR and to understand the observed differences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Sara Zarei, Email: sara.zarei@channing.harvard.edu.
James Eggert, Email: jeggert@sanjuanbautista.edu.
Laura Franqui-Dominguez, Email: lfranqui@sanjuanbautista.edu.
Yonatan Carl, Email: yonatanc@sanjuanbautista.edu.
Fernando Boria, Email: fernandobg@sanjuanbautista.edu.
Marina Stukova, Email: marinas@sanjuanbautista.edu.
Alessandro Avila, Email: alessandroa@sanjuanbautista.edu.
Cristina Rubi, Email: cristi_rubi2010@hotmail.com.
Angel Chinea, Email: achinea@me.com.
REFERENCES
- 1.Abkur TM, Foran E, Kearney H, Harkin G, Byrnes V, Lynch J, et al. Neuromyelitis optica presenting as intractable vomiting and hyperCKaemia. J Neurol. 2016;263:171–3. doi: 10.1007/s00415-015-7980-4. [DOI] [PubMed] [Google Scholar]
- 2.Aiyer R, Mehta N, Gungor S, Gulati A. A systematic review of NMDA receptor antagonists for treatment of neuropathic pain in clinical practice. Clin J Pain. 2018;34:450–67. doi: 10.1097/AJP.0000000000000547. [DOI] [PubMed] [Google Scholar]
- 3.Ajmera MR, Boscoe A, Mauskopf J, Candrilli SD, Levy M. Evaluation of comorbidities and health care resource use among patients with highly active neuromyelitis optica. J Neurol Sci. 2018;384:96–103. doi: 10.1016/j.jns.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 4.Akaishi T, Takahashi T, Nakashima I. Chloride imbalance between serum and CSF in the acute phase of neuromyelitis optica. J Neuroimmunol. 2018;315:45–9. doi: 10.1016/j.jneuroim.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Akman-Demir G, Serdaroglu P, Tasçi B. Clinical patterns of neurological involvement in Behçet's disease: Evaluation of 200 patients. The neuro-Behçet study group. Brain. 1999;122(Pt 11):2171–82. doi: 10.1093/brain/122.11.2171. [DOI] [PubMed] [Google Scholar]
- 6.Al Sawaf A, Berger JR. Longitudinally extensive transverse myelitis suspected for isolated neuro-Behçet: A diagnostic conundrum. Mult Scler Relat Disord. 2015;4:395–9. doi: 10.1016/j.msard.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Al-Araji A, Kidd DP. Neuro-Behçet's disease: Epidemiology, clinical characteristics, and management. Lancet Neurol. 2009;8:192–204. doi: 10.1016/S1474-4422(09)70015-8. [DOI] [PubMed] [Google Scholar]
- 8.Alharbi FM. Update in Vitamin D and multiple sclerosis. Neurosciences (Riyadh) 2015;20:329–35. doi: 10.17712/nsj.2015.4.20150357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen AC, Kelly S, Basdeo SA, Kinsella K, Mulready KJ, Mills KH, et al. Apilot study of the immunological effects of high-dose Vitamin D in healthy volunteers. Mult Scler. 2012;18:1797–800. doi: 10.1177/1352458512442992. [DOI] [PubMed] [Google Scholar]
- 10.Alvarenga MP, Schimidt S, Alvarenga RP. Epidemiology of neuromyelitis optica in Latin America. Mult Scler J Exp Transl Clin. 2017;3:2055217317730098. doi: 10.1177/2055217317730098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amaral DM, Parreira T, Sampaio M. Longitudinally extensive transverse myelitis and meningitis due to a rare infectious cause. 2015;(BMJ Case Rep 2015):pii: Bcr2015211761. doi: 10.1136/bcr-2015-211761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amirjamshidi A, Abbassioun K, Parsa K. Hiccup and neurosurgeons: A report of 4 rare dorsal medullary compressive pathologies and review of the literature. Surg Neurol. 2007;67:395–402. doi: 10.1016/j.surneu.2006.10.070. [DOI] [PubMed] [Google Scholar]
- 13.Anadure R, Narayanan CS, Varadraj G. Recurrent longitudinally extensive myelitis and aquaporin-4 seronegativity – The expanding spectrum of neuromyelitis optica. J Clin Diagn Res. 2017;11:OD05–7. doi: 10.7860/JCDR/2017/24186.9564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Apiwattanakul M, Popescu BF, Matiello M, Weinshenker BG, Lucchinetti CF, Lennon VA, et al. Intractable vomiting as the initial presentation of neuromyelitis optica. Ann Neurol. 2010;68:757–61. doi: 10.1002/ana.22121. [DOI] [PubMed] [Google Scholar]
- 15.Araki M, Matsuoka T, Miyamoto K, Kusunoki S, Okamoto T, Murata M, et al. Efficacy of the anti-IL-6 receptor antibody tocilizumab in neuromyelitis optica: A pilot study. Neurology. 2014;82:1302–6. doi: 10.1212/WNL.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asgari N, Lillevang ST, Skejoe HP, Falah M, Stenager E, Kyvik KO, et al. Apopulation-based study of neuromyelitis optica in Caucasians. Neurology. 2011;76:1589–95. doi: 10.1212/WNL.0b013e3182190f74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asgari N, Nielsen C, Stenager E, Kyvik KO, Lillevang ST. HLA, PTPN22 and PD-1 associations as markers of autoimmunity in neuromyelitis optica. Mult Scler. 2012;18:23–30. doi: 10.1177/1352458511417480. [DOI] [PubMed] [Google Scholar]
- 18.Ashtari F, Safaei A, Shaygannejad V, Najafi MA, Vesal S. Neuromyelitis optica spectrum disease characteristics in Isfahan, Iran: A cross-sectional study. J Res Med Sci. 2017;22:41. doi: 10.4103/1735-1995.202142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Awad SA, Wilson JW, Fenemore J, Kiruluta HG. Dysfunction of the detrusor and urethra in multiple sclerosis: The role of drug therapy. Can J Surg. 1982;25:259–62. [PubMed] [Google Scholar]
- 20.Azizlerli G, Köse AA, Sarica R, Gül A, Tutkun IT, Kulaç M, et al. Prevalence of Behçet's disease in Istanbul, Turkey. Int J Dermatol. 2003;42:803–6. doi: 10.1046/j.1365-4362.2003.01893.x. [DOI] [PubMed] [Google Scholar]
- 21.Baba T, Nakashima I, Kanbayashi T, Konno M, Takahashi T, Fujihara K, et al. Narcolepsy as an initial manifestation of neuromyelitis optica with anti-aquaporin-4 antibody. J Neurol. 2009;256:287–8. doi: 10.1007/s00415-009-0139-4. [DOI] [PubMed] [Google Scholar]
- 22.Baehring JM, Hochberg FH, Betensky RA, Longtine J, Sklar J. Immunoglobulin gene rearrangement analysis in cerebrospinal fluid of patients with lymphoproliferative processes. J Neurol Sci. 2006;247:208–16. doi: 10.1016/j.jns.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 23.Baker RW, Thompson RH, Zilkha KJ. Serum fatty acids in multiple sclerosis subject age (yr.) diagnosis. J Neurol Neurosurg Psychiat. 1964;27:5. doi: 10.1136/jnnp.27.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bandettini di Poggio M, Primavera A, Capello E, Bandini F, Mazzarello G, Viscoli C, et al. Acase of secondary syphilis presenting as optic neuritis. Neurol Sci. 2010;31:365–7. doi: 10.1007/s10072-010-0222-8. [DOI] [PubMed] [Google Scholar]
- 25.Barbieri F, Buscaino GA. Neuromyelitis optica in the elderly. Acta Neurol (Napoli) 1989;11:247–51. [PubMed] [Google Scholar]
- 26.Barros PO, Cassano T, Hygino J, Ferreira TB, Centurião N, Kasahara TM, et al. Prediction of disease severity in neuromyelitis optica by the levels of interleukin (IL)-6 produced during remission phase. Clin Exp Immunol. 2016;183:480–9. doi: 10.1111/cei.12733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ben-Ari ET. Dual purpose: Some cancer therapies used to treat autoimmune diseases. J Natl Cancer Inst. 2004;96:577–9. doi: 10.1093/jnci/96.8.577. [DOI] [PubMed] [Google Scholar]
- 28.Berghoff SA, Gerndt N, Winchenbach J, Stumpf SK, Hosang L, Odoardi F, et al. Dietary cholesterol promotes repair of demyelinated lesions in the adult brain. Nat Commun. 2017;8:14241. doi: 10.1038/ncomms14241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bichuetti DB, Lobato de Oliveira EM, Oliveira DM, Amorin de Souza N, Gabbai AA. Neuromyelitis optica treatment: Analysis of 36 patients. Arch Neurol. 2010;67:1131–6. doi: 10.1001/archneurol.2010.203. [DOI] [PubMed] [Google Scholar]
- 30.Blanc F, Noblet V, Jung B, Rousseau F, Renard F, Bourre B, et al. White matter atrophy and cognitive dysfunctions in neuromyelitis optica. PLoS One. 2012;7:e33878. doi: 10.1371/journal.pone.0033878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boström I, Stawiarz L, Landtblom AM. Sex ratio of multiple sclerosis in the national swedish MS register (SMSreg) Mult Scler. 2013;19:46–52. doi: 10.1177/1352458512446169. [DOI] [PubMed] [Google Scholar]
- 32.Bouzar M, Daoudi S, Hattab S, Bouzar AA, Deiva K, Wildemann B, et al. Neuromyelitis optica spectrum disorders with antibodies to myelin oligodendrocyte glycoprotein or aquaporin-4: Clinical and paraclinical characteristics in Algerian patients. J Neurol Sci. 2017;381:240–4. doi: 10.1016/j.jns.2017.08.3254. [DOI] [PubMed] [Google Scholar]
- 33.Bradl M, Kanamori Y, Nakashima I, Misu T, Fujihara K, Lassmann H, et al. Pain in neuromyelitis optica – Prevalence, pathogenesis and therapy. Nat Rev Neurol. 2014;10:529–36. doi: 10.1038/nrneurol.2014.129. [DOI] [PubMed] [Google Scholar]
- 34.Brum DG, Barreira AA, dos Santos AC, Kaimen-Maciel DR, Matiello M, Costa RM, et al. HLA-DRB association in neuromyelitis optica is different from that observed in multiple sclerosis. Mult Scler. 2010;16:21–9. doi: 10.1177/1352458509350741. [DOI] [PubMed] [Google Scholar]
- 35.Burks JS, Bigley GK, Hill HH. Rehabilitation challenges in multiple sclerosis. Ann Indian Acad Neurol. 2009;12:296–306. doi: 10.4103/0972-2327.58273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buser N, Ivic S, Kessler TM, Kessels AG, Bachmann LM. Efficacy and adverse events of antimuscarinics for treating overactive bladder: Network meta-analyses. Eur Urol. 2012;62:1040–60. doi: 10.1016/j.eururo.2012.08.060. [DOI] [PubMed] [Google Scholar]
- 37.Cabrera-Gómez JA, Kurtzke JF, González-Quevedo A, Lara-Rodríguez R. An epidemiological study of neuromyelitis optica in Cuba. J Neurol. 2009;256:35–44. doi: 10.1007/s00415-009-0009-0. [DOI] [PubMed] [Google Scholar]
- 38.Cai G, He D, Chu L, Dai Q, Xu Z, Zhang Y, et al. Paraneoplastic neuromyelitis optica spectrum disorders: Three new cases and a review of the literature. Int J Neurosci. 2016;126:660–8. doi: 10.3109/00207454.2015.1054481. [DOI] [PubMed] [Google Scholar]
- 39.Calamia KT, Wilson FC, Icen M, Crowson CS, Gabriel SE, Kremers HM, et al. Epidemiology and clinical characteristics of Behçet's disease in the US: A population-based study. Arthritis Rheum. 2009;61:600–4. doi: 10.1002/art.24423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cantorna MT, Mahon BD. Mounting evidence for vitamin D as an environmental factor affecting autoimmune disease prevalence. Exp Biol Med (Maywood) 2004;229:1136–42. doi: 10.1177/153537020422901108. [DOI] [PubMed] [Google Scholar]
- 41.Cantorna MT, Snyder L, Lin YD, Yang L. Vitamin D and 1,25(OH)2D regulation of T cells. Nutrients. 2015;7:3011–21. doi: 10.3390/nu7043011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cantuti-Castelvetri L, Fitzner D, Bosch-Queralt M, Weil MT, Su M, Sen P, et al. Defective cholesterol clearance limits remyelination in the aged central nervous system. Science. 2018;359:684–8. doi: 10.1126/science.aan4183. [DOI] [PubMed] [Google Scholar]
- 43.Carnero Contentti E, Daccach Marques V, Soto de Castillo I, Tkachuk V, Antunes Barreira A, Armas E, et al. Frequency of brain MRI abnormalities in neuromyelitis optica spectrum disorder at presentation: A cohort of Latin American patients. Mult Scler Relat Disord. 2018;19:73–8. doi: 10.1016/j.msard.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 44.Cha E, Lee KM, Park KD, Park KS, Lee KW, Kim SM, et al. Hydroxycholesterol levels in the serum and cerebrospinal fluid of patients with neuromyelitis optica revealed by LC-ag+CIS/MS/MS and LC-ESI/MS/MS with picolinic derivatization: Increased levels and association with disability during acute attack. PLoS One. 2016;11:e0167819. doi: 10.1371/journal.pone.0167819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chavarro VS, Mealy MA, Simpson A, Lacheta A, Pache F, Ruprecht K, et al. Insufficient treatment of severe depression in neuromyelitis optica spectrum disorder. Neurol Neuroimmunol Neuroinflamm. 2016;3:e286. doi: 10.1212/NXI.0000000000000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chitnis T, Ness J, Krupp L, Waubant E, Hunt T, Olsen CS, et al. Clinical features of neuromyelitis optica in children: US network of pediatric MS centers report. Neurology. 2016;86:245–52. doi: 10.1212/WNL.0000000000002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collongues N, de Seze J. Current and future treatment approaches for neuromyelitis optica. Ther Adv Neurol Disord. 2011;4:111–21. doi: 10.1177/1756285611398939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collongues N, Marignier R, Zéphir H, Papeix C, Blanc F, Ritleng C, et al. Neuromyelitis optica in France: A multicenter study of 125 patients. Neurology. 2010;74:736–42. doi: 10.1212/WNL.0b013e3181d31e35. [DOI] [PubMed] [Google Scholar]
- 49.Combes AJE, Matthews L, Lee JS, Li DKB, Carruthers R, Traboulsee AL, et al. Cervical cord myelin water imaging shows degenerative changes over one year in multiple sclerosis but not neuromyelitis optica spectrum disorder. Neuroimage Clin. 2017;16:17–22. doi: 10.1016/j.nicl.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corcos J. A urological challenge: Voiding dysfunction in multiple sclerosis. Can Urol Assoc J. 2013;7:S181–2. doi: 10.5489/cuaj.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cornelio DB, Braga RP, Rosa MW, Ayub AC. Devic's neuromyelitis optica and pregnancy: Distinction from multiple sclerosis is essential. Arch Gynecol Obstet. 2009;280:475–7. doi: 10.1007/s00404-008-0918-7. [DOI] [PubMed] [Google Scholar]
- 52.Cossburn M, Tackley G, Baker K, Ingram G, Burtonwood M, Malik G, et al. The prevalence of neuromyelitis optica in South East wales. Eur J Neurol. 2012;19:655–9. doi: 10.1111/j.1468-1331.2011.03529.x. [DOI] [PubMed] [Google Scholar]
- 53.Costanzi C, Matiello M, Lucchinetti CF, Weinshenker BG, Pittock SJ, Mandrekar J, et al. Azathioprine: Tolerability, efficacy, and predictors of benefit in neuromyelitis optica. Neurology. 2011;77:659–66. doi: 10.1212/WNL.0b013e31822a2780. [DOI] [PubMed] [Google Scholar]
- 54.Cree BA, Lamb S, Morgan K, Chen A, Waubant E, Genain C, et al. An open label study of the effects of rituximab in neuromyelitis optica. Neurology. 2005;64:1270–2. doi: 10.1212/01.WNL.0000159399.81861.D5. [DOI] [PubMed] [Google Scholar]
- 55.Cree BA, Spencer CM, Varrin-Doyer M, Baranzini SE, Zamvil SS. Gut microbiome analysis in neuromyelitis optica reveals overabundance of Clostridium perfringens. Ann Neurol. 2016;80:443–7. doi: 10.1002/ana.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Criteria for diagnosis of Behçet's disease. International study group for Behçet's disease. Lancet. 1990;335:1078–80. [PubMed] [Google Scholar]
- 57.Cruz-Herranz A, Sagan SA, Sobel RA, Green AJ, Zamvil SS. T cells targeting neuromyelitis optica autoantigen aquaporin-4 cause paralysis and visual system injury. J Nat Sci. 2017;3:pii: e358. [PMC free article] [PubMed] [Google Scholar]
- 58.Daoudi S, Bouzar M. Neuromyelitis optica spectrum disorders in Algeria: A preliminary study in the region of Tizi Ouzou. Mult Scler Relat Disord. 2016;6:37–40. doi: 10.1016/j.msard.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 59.de Bie J, Lim CK, Guillemin GJ. Progesterone alters kynurenine pathway activation in IFN-γ-activated macrophages – Relevance for neuroinflammatory diseases. Int J Tryptophan Res. 2016;9:89–93. doi: 10.4137/IJTR.S40332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Carvalho FL, Gomes CM, Apostolos-Pereira SL, Bessa J, Jr, Pinheiro M, Marchiori PE, et al. Voiding dysfunction in patients with neuromyelitis optica spectrum disorders. Neurourol Urodyn. 2016;35:39–43. doi: 10.1002/nau.22667. [DOI] [PubMed] [Google Scholar]
- 61.de Oliveira P, de Carvalho DR, Brandi IV, Pratesi R. Serological prevalence of celiac disease in Brazilian population of multiple sclerosis, neuromyelitis optica and myelitis. Mult Scler Relat Disord. 2016;9:125–8. doi: 10.1016/j.msard.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 62.de Seze J, Lebrun C, Stojkovic T, Ferriby D, Chatel M, Vermersch P, et al. Is Devic's neuromyelitis optica a separate disease. A comparative study with multiple sclerosis? Mult Scler. 2003;9:521–5. doi: 10.1191/1352458503ms947oa. [DOI] [PubMed] [Google Scholar]
- 63.Derle E, Güneş HN, Konuşkan B, Tuncer-Kurne A. Neuromyelitis optica in children: A review of the literature. Turk J Pediatr. 2014;56:573–80. [PubMed] [Google Scholar]
- 64.Deschamps R, Paturel L, Jeannin S, Chausson N, Olindo S, Béra O, et al. Different HLA class II (DRB1 and DQB1) alleles determine either susceptibility or resistance to NMO and multiple sclerosis among the French Afro-Caribbean population. Mult Scler. 2011;17:24–31. doi: 10.1177/1352458510382810. [DOI] [PubMed] [Google Scholar]
- 65.Dilokthornsakul P, Valuck RJ, Nair KV, Corboy JR, Allen RR, Campbell JD, et al. Multiple sclerosis prevalence in the united states commercially insured population. Neurology. 2016;86:1014–21. doi: 10.1212/WNL.0000000000002469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dmitrieva-Zdorova EV, Gabaeva MV, Seregin YA, Bodoev NV, Voronko OE. PDCD1 PD-1.3 polymorphism and allergic bronchial asthma in Russian and buryat patients. J Asthma. 2017;54:46–52. doi: 10.1080/02770903.2016.1196366. [DOI] [PubMed] [Google Scholar]
- 67.Downer JJ, Leite MI, Carter R, Palace J, Küker W, Quaghebeur G, et al. Diagnosis of neuromyelitis optica (NMO) spectrum disorders: Is MRI obsolete? Neuroradiology. 2012;54:279–85. doi: 10.1007/s00234-011-0875-x. [DOI] [PubMed] [Google Scholar]
- 68.Drori T, Chapman J. Diagnosis and classification of neuromyelitis optica (Devic's syndrome) Autoimmun Rev. 2014;13:531–3. doi: 10.1016/j.autrev.2014.01.034. [DOI] [PubMed] [Google Scholar]
- 69.Eaneff S, Wang V, Hanger M, Levy M, Mealy MA, Brandt AU, et al. Patient perspectives on neuromyelitis optica spectrum disorders: Data from the patientsLikeMe online community. Mult Scler Relat Disord. 2017;17:116–22. doi: 10.1016/j.msard.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 70.Eskandarieh S, Nedjat S, Abdollahpour I, Moghadasi AN, Azimi AR, Sahraian MA, et al. Comparing epidemiology and baseline characteristic of multiple sclerosis and neuromyelitis optica: A case-control study. Mult Scler Relat Disord. 2017;12:39–43. doi: 10.1016/j.msard.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 71.Etemadifar M, Nasr Z, Khalili B, Taherioun M, Vosoughi R. Epidemiology of neuromyelitis optica in the world: A systematic review and meta-analysis. Mult Scler Int 2015. 2015:174720. doi: 10.1155/2015/174720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Felix CM, Levin MH, Verkman AS. Complement-independent retinal pathology produced by intravitreal injection of neuromyelitis optica immunoglobulin G. J Neuroinflammation. 2016;13:275. doi: 10.1186/s12974-016-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Flanagan EP, Kaufmann TJ, Krecke KN, Aksamit AJ, Pittock SJ, Keegan BM, et al. Discriminating long myelitis of neuromyelitis optica from sarcoidosis. Ann Neurol. 2016;79:437–47. doi: 10.1002/ana.24582. [DOI] [PubMed] [Google Scholar]
- 74.Flanagan EP, O’Neill BP, Porter AB, Lanzino G, Haberman TM, Keegan BM, et al. Primary intramedullary spinal cord lymphoma. Neurology. 2011;77:784–91. doi: 10.1212/WNL.0b013e31822b00b9. [DOI] [PubMed] [Google Scholar]
- 75.Fragoso YD, Adoni T, Bichuetti DB, Brooks JB, Ferreira ML, Oliveira EM, et al. Neuromyelitis optica and pregnancy. J Neurol. 2013;260:2614–9. doi: 10.1007/s00415-013-7031-y. [DOI] [PubMed] [Google Scholar]
- 76.Freitas E, Guimarães J. Neuromyelitis optica spectrum disorders associated with other autoimmune diseases. Rheumatol Int. 2015;35:243–53. doi: 10.1007/s00296-014-3066-3. [DOI] [PubMed] [Google Scholar]
- 77.Frigeri A, Gropper MA, Umenishi F, Kawashima M, Brown D, Verkman AS, et al. Localization of MIWC and GLIP water channel homologs in neuromuscular, epithelial and glandular tissues. J Cell Sci. 1995;108(Pt 9):2993–3002. doi: 10.1242/jcs.108.9.2993. [DOI] [PubMed] [Google Scholar]
- 78.Fu Q, Goodrum JF, Hayes C, Hostettler JD, Toews AD, Morell P, et al. Control of cholesterol biosynthesis in Schwann cells. J Neurochem. 1998;71:549–55. doi: 10.1046/j.1471-4159.1998.71020549.x. [DOI] [PubMed] [Google Scholar]
- 79.Gajofatto A, Monaco S, Fiorini M, Zanusso G, Vedovello M, Rossi F, et al. Assessment of outcome predictors in first-episode acute myelitis: A retrospective study of 53 cases. Arch Neurol. 2010;67:724–30. doi: 10.1001/archneurol.2010.107. [DOI] [PubMed] [Google Scholar]
- 80.Gebhardt A, Buehler R, Wiest R, Tewald F, Sellner J, Humpert S, et al. Mycoplasma pneumonia as a cause of neuromyelitis optica? J Neurol. 2008;255:1268–9. doi: 10.1007/s00415-008-0870-2. [DOI] [PubMed] [Google Scholar]
- 81.Gouin JP, Hantsoo L, Kiecolt-Glaser JK. Immune dysregulation and chronic stress among older adults: A review. Neuroimmunomodulation. 2008;15:251–9. doi: 10.1159/000156468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Graves J, Grandhe S, Weinfurtner K, Krupp L, Belman A, Chitnis T, et al. Protective environmental factors for neuromyelitis optica. Neurology. 2014;83:1923–9. doi: 10.1212/WNL.0000000000001001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Halkjær SI, Boolsen AW, Günther S, Christensen AH, Petersen AM. Can fecal microbiota transplantation cure irritable bowel syndrome? World J Gastroenterol. 2017;23:4112–20. doi: 10.3748/wjg.v23.i22.4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hall LM, Kimlin MG, Aronov PA, Hammock BD, Slusser JR, Woodhouse LR, et al. Vitamin D intake needed to maintain target serum 25-hydroxyvitamin D concentrations in participants with low sun exposure and dark skin pigmentation is substantially higher than current recommendations. J Nutr. 2010;140:542–50. doi: 10.3945/jn.109.115253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.He D, Chen X, Zhao D, Zhou H. Cognitive function, depression, fatigue, and activities of daily living in patients with neuromyelitis optica after acute relapse. Int J Neurosci. 2011;121:677–83. doi: 10.3109/00207454.2011.608456. [DOI] [PubMed] [Google Scholar]
- 86.He D, Wu Q, Chen X, Zhao D, Gong Q, Zhou H, et al. Cognitive impairment and whole brain diffusion in patients with neuromyelitis optica after acute relapse. Brain Cogn. 2011;77:80–8. doi: 10.1016/j.bandc.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 87.Hemminki K, Li X, Sundquist J, Sundquist K. The epidemiology of graves’ disease: Evidence of a genetic and an environmental contribution. J Autoimmun. 2010;34:J307–13. doi: 10.1016/j.jaut.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 88.Hinson SR, Roemer SF, Lucchinetti CF, Fryer JP, Kryzer TJ, Chamberlain JL, et al. Aquaporin-4-binding autoantibodies in patients with neuromyelitis optica impair glutamate transport by down-regulating EAAT2. J Exp Med. 2008;205:2473–81. doi: 10.1084/jem.20081241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hoang-Xuan K, Bessell E, Bromberg J, Hottinger AF, Preusser M, Rudà R, et al. Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: Guidelines from the European association for neuro-oncology. Lancet Oncol. 2015;16:e322–32. doi: 10.1016/S1470-2045(15)00076-5. [DOI] [PubMed] [Google Scholar]
- 90.Houzen H, Niino M, Hirotani M, Fukazawa T, Kikuchi S, Tanaka K, et al. Increased prevalence, incidence, and female predominance of multiple sclerosis in Northern Japan. J Neurol Sci. 2012;323:117–22. doi: 10.1016/j.jns.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 91.Hsu CL, Yeh JH, Lau CI. Persistent hyperthermia in a patient with aquaporin-4-antibody-positive neuromyelitis optica spectrum disorder. J Clin Neurol. 2016;12:515–6. doi: 10.3988/jcn.2016.12.4.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Huppke P, Blüthner M, Bauer O, Stark W, Reinhardt K, Huppke B, et al. Neuromyelitis optica and NMO-IgG in European pediatric patients. Neurology. 2010;75:1740–4. doi: 10.1212/WNL.0b013e3181fc2823. [DOI] [PubMed] [Google Scholar]
- 93.Hurst RW, Kenyon LC, Lavi E, Raps EC, Marcotte P. Spinal dural arteriovenous fistula: The pathology of venous hypertensive myelopathy. Neurology. 1995;45:1309–13. doi: 10.1212/wnl.45.7.1309. [DOI] [PubMed] [Google Scholar]
- 94.Hyun JW, Jeong IH, Joung A, Kim SH, Kim HJ. Evaluation of the 2015 diagnostic criteria for neuromyelitis optica spectrum disorder. Neurology. 2016;86:1772–9. doi: 10.1212/WNL.0000000000002655. [DOI] [PubMed] [Google Scholar]
- 95.Iorio R, Lucchinetti CF, Lennon VA, Farrugia G, Pasricha PJ, Weinshenker BG, et al. Intractable nausea and vomiting from autoantibodies against a brain water channel. Clin Gastroenterol Hepatol. 2013;11:240–5. doi: 10.1016/j.cgh.2012.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Isobe N, Oksenberg JR. Genetic studies of multiple sclerosis and neuromyelitis optica: Current status in European, African American and Asian populations. Clin Exp Neuroimmunol. 2014;5:61–8. [Google Scholar]
- 97.Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–98. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ivanov II, McKenzie BS, Zhou L, Tadokoro CE, Lepelley A, Lafaille JJ, et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+T helper cells. Cell. 2006;126:1121–33. doi: 10.1016/j.cell.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 99.Jacob A, Matiello M, Wingerchuk DM, Lucchinetti CF, Pittock SJ, Weinshenker BG, et al. Neuromyelitis optica: Changing concepts. J Neuroimmunol. 2007;187:126–38. doi: 10.1016/j.jneuroim.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 100.Jain RS, Kumar S, Tejwani S. A rare association of tuberculous longitudinally extensive transverse myelitis (LETM) with brain tuberculoma. Springerplus. 2015;4:476. doi: 10.1186/s40064-015-1232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jakszyn P, Gonzalez CA. Nitrosamine and related food intake and gastric and oesophageal cancer risk: A systematic review of the epidemiological evidence. World J Gastroenterol. 2006;12:4296–303. doi: 10.3748/wjg.v12.i27.4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.James E, Dobson R, Kuhle J, Baker D, Giovannoni G, Ramagopalan SV, et al. The effect of Vitamin D-related interventions on multiple sclerosis relapses: A meta-analysis. Mult Scler. 2013;19:1571–9. doi: 10.1177/1352458513489756. [DOI] [PubMed] [Google Scholar]
- 103.Janowski BA, Willy PJ, Devi TR, Falck JR, Mangelsdorf DJ. An oxysterol signalling pathway mediated by the nuclear receptor LXR alpha. Nature. 1996;383:728–31. doi: 10.1038/383728a0. [DOI] [PubMed] [Google Scholar]
- 104.Jarius S, Jacobi C, de Seze J, Zephir H, Paul F, Franciotta D, et al. Frequency and syndrome specificity of antibodies to aquaporin-4 in neurological patients with rheumatic disorders. Mult Scler. 2011;17:1067–73. doi: 10.1177/1352458511403958. [DOI] [PubMed] [Google Scholar]
- 105.Jarius S, Paul F, Franciotta D, de Seze J, Münch C, Salvetti M, et al. Neuromyelitis optica spectrum disorders in patients with myasthenia gravis: Ten new aquaporin-4 antibody positive cases and a review of the literature. Mult Scler. 2012;18:1135–43. doi: 10.1177/1352458511431728. [DOI] [PubMed] [Google Scholar]
- 106.Jarius S, Paul F, Franciotta D, Ruprecht K, Ringelstein M, Bergamaschi R, et al. Cerebrospinal fluid findings in aquaporin-4 antibody positive neuromyelitis optica: Results from 211 lumbar punctures. J Neurol Sci. 2011;306:82–90. doi: 10.1016/j.jns.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 107.Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-igG in NMO and related disorders: A multicenter study of 50 patients. Part 2: Epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J Neuroinflammation. 2016;13:280. doi: 10.1186/s12974-016-0718-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jarius S, Ruprecht K, Wildemann B, Kuempfel T, Ringelstein M, Geis C, et al. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: A multicentre study of 175 patients. J Neuroinflammation. 2012;9:14. doi: 10.1186/1742-2094-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jarius S, Wildemann B, Paul F. Neuromyelitis optica: Clinical features, immunopathogenesis and treatment. Clin Exp Immunol. 2014;176:149–64. doi: 10.1111/cei.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jarius S, Wildemann B. The history of neuromyelitis optica. J Neuroinflammation. 2013;10:8. doi: 10.1186/1742-2094-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jellema K, Canta LR, Tijssen CC, van Rooij WJ, Koudstaal PJ, van Gijn J, et al. Spinal dural arteriovenous fistulas: Clinical features in 80 patients. J Neurol Neurosurg Psychiatry. 2003;74:1438–40. doi: 10.1136/jnnp.74.10.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jin X, Pei S, Liu Y, Li X. Clinical analysis of neuromyelitis optica presenting as intractable nausea, vomiting and hiccups. Int J Neurosci. 2017;127:854–8. doi: 10.1080/00207454.2016.1269090. [DOI] [PubMed] [Google Scholar]
- 113.Jitprapaikulsan J, Siritho S, Prayoonwiwat N. Vitamin D level status in thai neuromyelitis optica patients. J Neuroimmunol. 2016;295-296:75–8. doi: 10.1016/j.jneuroim.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 114.Jitprapaikulsan SS. Vitamin D and neuromyelitis optica spectrum disorders. Austin J Mult Scler Neuroimmunol. 2016;3:1–3. [Google Scholar]
- 115.Johnson BA, Fram EK, Johnson PC, Jacobowitz R. The variable MR appearance of primary lymphoma of the central nervous system: Comparison with histopathologic features. AJNR Am J Neuroradiol. 1997;18:563–72. [PMC free article] [PubMed] [Google Scholar]
- 116.Juryńczyk M, Craner M, Palace J. Overlapping CNS inflammatory diseases: Differentiating features of NMO and MS. J Neurol Neurosurg Psychiatry. 2015;86:20–5. doi: 10.1136/jnnp-2014-308984. [DOI] [PubMed] [Google Scholar]
- 117.Kagawa Y. Impact of westernization on the nutrition of Japanese: Changes in physique, cancer, longevity and centenarians. Prev Med. 1978;7:205–17. doi: 10.1016/0091-7435(78)90246-3. [DOI] [PubMed] [Google Scholar]
- 118.Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS, et al. Diagnosis and management of neuro-Behçet's disease: International consensus recommendations. J Neurol. 2014;261:1662–76. doi: 10.1007/s00415-013-7209-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kalsi V, Fowler CJ. Therapy insight: Bladder dysfunction associated with multiple sclerosis. Nat Clin Pract Urol. 2005;2:492–501. doi: 10.1038/ncpuro0323. [DOI] [PubMed] [Google Scholar]
- 120.Kampman MT, Steffensen LH. The role of Vitamin D in multiple sclerosis. J Photochem Photobiol B. 2010;101:137–41. doi: 10.1016/j.jphotobiol.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 121.Kanamori Y, Nakashima I, Takai Y, Nishiyama S, Kuroda H, Takahashi T, et al. Pain in neuromyelitis optica and its effect on quality of life: A cross-sectional study. Neurology. 2011;77:652–8. doi: 10.1212/WNL.0b013e318229e694. [DOI] [PubMed] [Google Scholar]
- 122.Kanbayashi T, Shimohata T, Nakashima I, Yaguchi H, Yabe I, Nishizawa M, et al. Symptomatic narcolepsy in patients with neuromyelitis optica and multiple sclerosis: New neurochemical and immunological implications. Arch Neurol. 2009;66:1563–6. doi: 10.1001/archneurol.2009.264. [DOI] [PubMed] [Google Scholar]
- 123.Kanoto M, Hosoya T, Toyoguchi Y, Oda A. Brain stem and cerebellar atrophy in chronic progressive neuro-Behçet's disease. Eur J Radiol. 2013;82:146–50. doi: 10.1016/j.ejrad.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 124.Kessler RA, Mealy MA, Jimenez-Arango JA, Quan C, Paul F, López R, et al. Anti-aquaporin-4 titer is not predictive of disease course in neuromyelitis optica spectrum disorder: A multicenter cohort study. Mult Scler Relat Disord. 2017;17:198–201. doi: 10.1016/j.msard.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 125.Kessler RA, Mealy MA, Levy M. Treatment of neuromyelitis optica spectrum disorder: Acute, preventive, and symptomatic. Curr Treat Options Neurol. 2016;18:2. doi: 10.1007/s11940-015-0387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kikuchi H, Takayama M, Hirohata S. Quantitative analysis of brainstem atrophy on magnetic resonance imaging in chronic progressive neuro-Behçet's disease. J Neurol Sci. 2014;337:80–5. doi: 10.1016/j.jns.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 127.Kim HJ, Park HY, Kim E, Lee KS, Kim KK, Choi BO, et al. Common CYP7A1 promoter polymorphism associated with risk of neuromyelitis optica. Neurobiol Dis. 2010;37:349–55. doi: 10.1016/j.nbd.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 128.Kim SM, Go MJ, Sung JJ, Park KS, Lee KW. Painful tonic spasm in neuromyelitis optica: Incidence, diagnostic utility, and clinical characteristics. Arch Neurol. 2012;69:1026–31. doi: 10.1001/archneurol.2012.112. [DOI] [PubMed] [Google Scholar]
- 129.Kim SM, Kim SJ, Lee HJ, Kuroda H, Palace J, Fujihara K, et al. Differential diagnosis of neuromyelitis optica spectrum disorders. Ther Adv Neurol Disord. 2017;10:265–89. doi: 10.1177/1756285617709723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kim SM, Waters P, Vincent A, Kim SY, Kim HJ, Hong YH, et al. Sjogren's syndrome myelopathy: Spinal cord involvement in Sjogren's syndrome might be a manifestation of neuromyelitis optica. Mult Scler. 2009;15:1062–8. doi: 10.1177/1352458509106636. [DOI] [PubMed] [Google Scholar]
- 131.Kim SM, Waters P, Woodhall M, Kim JY, Kim JE, Yang JW, et al. Utility of aquaporin-4 antibody assay in patients with neuromyelitis optica spectrum disorders. Mult Scler. 2013;19:1060–7. doi: 10.1177/1352458512472748. [DOI] [PubMed] [Google Scholar]
- 132.Kim SM, Waters P, Woodhall M, Yang JW, Yang H, Kim JE, et al. Characterization of the spectrum of Korean inflammatory demyelinating diseases according to the diagnostic criteria and AQP4-ab status. BMC Neurol. 2014;14:93. doi: 10.1186/1471-2377-14-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kim SM, Woodhall MR, Kim JS, Kim SJ, Park KS, Vincent A, et al. Antibodies to MOG in adults with inflammatory demyelinating disease of the CNS. Neurol Neuroimmunol Neuroinflamm. 2015;2:e163. doi: 10.1212/NXI.0000000000000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kimbrough DJ, Fujihara K, Jacob A, Lana-Peixoto MA, Leite MI, Levy M, et al. Treatment of neuromyelitis optica: Review and recommendations. Mult Scler Relat Disord. 2012;1:180–7. doi: 10.1016/j.msard.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kinoshita M, Obata K, Tanaka M. Latitude has more significant impact on prevalence of multiple sclerosis than ultraviolet level or Sunshine duration in Japanese population. Neurol Sci. 2015;36:1147–51. doi: 10.1007/s10072-015-2150-0. [DOI] [PubMed] [Google Scholar]
- 136.Kira J. Genetic and environmental factors underlying the rapid changes in epidemiological and clinical features of multiple sclerosis and neuromyelitis optica in Japanese. Clin Exp Neuroimmunol. 2013;4:261–73. [Google Scholar]
- 137.Kister I, Herbert J, Zhou Y, Ge Y. Ultrahigh-field MR (7 T) imaging of brain lesions in neuromyelitis optica. Mult Scler Int 2013. 2013 doi: 10.1155/2013/398259. 398259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kitley J, Elsone L, George J, Waters P, Woodhall M, Vincent A, et al. Methotrexate is an alternative to azathioprine in neuromyelitis optica spectrum disorders with aquaporin-4 antibodies. J Neurol Neurosurg Psychiatry. 2013;84:918–21. doi: 10.1136/jnnp-2012-304774. [DOI] [PubMed] [Google Scholar]
- 139.Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, et al. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: A comparative study. JAMA Neurol. 2014;71:276–83. doi: 10.1001/jamaneurol.2013.5857. [DOI] [PubMed] [Google Scholar]
- 140.Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013;496:518–22. doi: 10.1038/nature11868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kleiter I, Hellwig K, Berthele A, Kümpfel T, Linker RA, Hartung HP, et al. Failure of natalizumab to prevent relapses in neuromyelitis optica. Arch Neurol. 2012;69:239–45. doi: 10.1001/archneurol.2011.216. [DOI] [PubMed] [Google Scholar]
- 142.Koelman DL, Chahin S, Mar SS, Venkatesan A, Hoganson GM, Yeshokumar AK, et al. Acute disseminated encephalomyelitis in 228 patients: A retrospective, multicenter US study. Neurology. 2016;86:2085–93. doi: 10.1212/WNL.0000000000002723. [DOI] [PubMed] [Google Scholar]
- 143.Krupp LB, Tardieu M, Amato MP, Banwell B, Chitnis T, Dale RC, et al. International pediatric multiple sclerosis study group criteria for pediatric multiple sclerosis and immune-mediated central nervous system demyelinating disorders: Revisions to the 2007 definitions. Mult Scler. 2013;19:1261–7. doi: 10.1177/1352458513484547. [DOI] [PubMed] [Google Scholar]
- 144.Kumar N, Keegan BM, Rodriguez FJ, Hammack JE, Kantarci OH. Intravascular lymphoma presenting as a longitudinally-extensive myelitis: Diagnostic challenges and etiologic clues. J Neurol Sci. 2011;303:146–9. doi: 10.1016/j.jns.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 145.Kume K, Deguchi K, Ikeda K, Takata T, Kokudo Y, Kamada M, et al. Neuromyelitis optica spectrum disorder presenting with repeated hypersomnia due to involvement of the hypothalamus and hypothalamus-amygdala linkage. Mult Scler. 2015;21:960–2. doi: 10.1177/1352458515569100. [DOI] [PubMed] [Google Scholar]
- 146.Lalan S, Khan M, Schlakman B, Penman A, Gatlin J, Herndon R, et al. Differentiation of neuromyelitis optica from multiple sclerosis on spinal magnetic resonance imaging. Int J MS Care. 2012;14:209–14. doi: 10.7224/1537-2073-14.4.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Larik A, Chiong Y, Lee LC, Ng YS. Longitudinally extensive transverse myelitis associated with dengue fever. BMJ Case Rep 2012. 2012:pii: bcr1220115378. doi: 10.1136/bcr.12.2011.5378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Laursen JH, Søndergaard HB, Sørensen PS, Sellebjerg F, Oturai AB. Vitamin D supplementation reduces relapse rate in relapsing-remitting multiple sclerosis patients treated with natalizumab. Mult Scler Relat Disord. 2016;10:169–73. doi: 10.1016/j.msard.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 149.Lee HS, Kim do Y, Shin HY, Choi YC, Kim SM. Spinal cord involvement in Behçet's disease. Mult Scler. 2016;22:960–3. doi: 10.1177/1352458515613642. [DOI] [PubMed] [Google Scholar]
- 150.Lee JD. Multiple Sclerosis in Asian Populations: The Genetic and Environmental Determinants of Variable Susceptibility and Clinical Profile. 2014. [Last accessed on 2018 Apr 09]. Available from: https://www.open.library.ubc.ca/cIRcle/collections/ubctheses/24/items/1.0165922 .
- 151.Lee YK, Menezes JS, Umesaki Y, Mazmanian SK. Proinflammatory T-cell responses to gut microbiota promote experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4615–22. doi: 10.1073/pnas.1000082107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Leite MI, Coutinho E, Lana-Peixoto M, Apostolos S, Waters P, Sato D, et al. Myasthenia gravis and neuromyelitis optica spectrum disorder: A multicenter study of 16 patients. Neurology. 2012;78:1601–7. doi: 10.1212/WNL.0b013e31825644ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–7. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: Distinction from multiple sclerosis. Lancet. 2004;364:2106–12. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 155.Li W, Minohara M, Piao H, Matsushita T, Masaki K, Matsuoka T, et al. Association of anti-Helicobacter pylori neutrophil-activating protein antibody response with anti-aquaporin-4 autoimmunity in Japanese patients with multiple sclerosis and neuromyelitis optica. Mult Scler. 2009;15:1411–21. doi: 10.1177/1352458509348961. [DOI] [PubMed] [Google Scholar]
- 156.Liu J, Shi Z, Lian Z, Chen H, Zhang Q, Feng H, et al. Association of CD58 gene polymorphisms with NMO spectrum disorders in a Han Chinese population. J Neuroimmunol. 2017;309:23–30. doi: 10.1016/j.jneuroim.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 157.Long Y, Zheng Y, Chen M, Zhang B, Gao C, Shan F, et al. Serum thyroid-stimulating hormone and anti-thyroglobulin antibody are independently associated with lesions in spinal cord in central nervous system demyelinating diseases. PLoS One. 2014;9:e100672. doi: 10.1371/journal.pone.0100672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lovera J, Reza T. Stress in multiple sclerosis: Review of new developments and future directions. Curr Neurol Neurosci Rep. 2013;13:398. doi: 10.1007/s11910-013-0398-4. [DOI] [PubMed] [Google Scholar]
- 159.Lucas RM, Ponsonby AL, Dear K, Valery PC, Pender MP, Taylor BV, et al. Sun exposure and Vitamin D are independent risk factors for CNS demyelination. Neurology. 2011;76:540–8. doi: 10.1212/WNL.0b013e31820af93d. [DOI] [PubMed] [Google Scholar]
- 160.Luppe S, Robertson NP. MOG-IgG in neuromyelitis optica. J Neurol. 2014;261:640–2. doi: 10.1007/s00415-014-7277-z. [DOI] [PubMed] [Google Scholar]
- 161.Marignier R, De Sèze J, Vukusic S, Durand-Dubief F, Zéphir H, Vermersch P, et al. NMO-igG and devic's neuromyelitis optica: A French experience. Mult Scler. 2008;14:440–5. doi: 10.1177/1352458507084595. [DOI] [PubMed] [Google Scholar]
- 162.Martínez-Lapiscina EH, Fraga-Pumar E, Pastor X, Gómez M, Conesa A, Lozano-Rubí R, et al. Is the incidence of optic neuritis rising? Evidence from an epidemiological study in barcelona (Spain), 2008-2012. J Neurol. 2014;261:759–67. doi: 10.1007/s00415-014-7266-2. [DOI] [PubMed] [Google Scholar]
- 163.Masters-Israilov A, Robbins MS. Headache in neuromyelitis optica. Curr Pain Headache Rep. 2017;21:20. doi: 10.1007/s11916-017-0620-1. [DOI] [PubMed] [Google Scholar]
- 164.Masuda H, Mori M, Uzawa A, Muto M, Uchida T, Kuwabara S, et al. Serum antinuclear antibody may be associated with less severe disease activity in neuromyelitis optica. Eur J Neurol. 2016;23:276–81. doi: 10.1111/ene.12714. [DOI] [PubMed] [Google Scholar]
- 165.Mateo J, Esteban O, Martínez M, Grzybowski A, Ascaso FJ. The contribution of optical coherence tomography in neuromyelitis optica spectrum disorders. Front Neurol. 2017;8:493. doi: 10.3389/fneur.2017.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Matiello M, Lennon VA, Jacob A, Pittock SJ, Lucchinetti CF, Wingerchuk DM, et al. NMO-IgG predicts the outcome of recurrent optic neuritis. Neurology. 2008;70:2197–200. doi: 10.1212/01.wnl.0000303817.82134.da. [DOI] [PubMed] [Google Scholar]
- 167.Matiello M, Schaefer-Klein JL, Hebrink DD, Kingsbury DJ, Atkinson EJ, Weinshenker BG, et al. Genetic analysis of aquaporin-4 in neuromyelitis optica. Neurology. 2011;77:1149–55. doi: 10.1212/WNL.0b013e31822f045b. [DOI] [PubMed] [Google Scholar]
- 168.Matthews L, Marasco R, Jenkinson M, Küker W, Luppe S, Leite MI, et al. Distinction of seropositive NMO spectrum disorder and MS brain lesion distribution. Neurology. 2013;80:1330–7. doi: 10.1212/WNL.0b013e3182887957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McKeon A, Lennon VA, Jacob A, Matiello M, Lucchinetti CF, Kale N, et al. Coexistence of myasthenia gravis and serological markers of neurological autoimmunity in neuromyelitis optica. Muscle Nerve. 2009;39:87–90. doi: 10.1002/mus.21197. [DOI] [PubMed] [Google Scholar]
- 170.Mealy MA, Wingerchuk DM, Greenberg BM, Levy M. Epidemiology of neuromyelitis optica in the United States: A multicenter analysis. Arch Neurol. 2012;69:1176–80. doi: 10.1001/archneurol.2012.314. [DOI] [PubMed] [Google Scholar]
- 171.Mealy MA, Wingerchuk DM, Palace J, Greenberg BM, Levy M. Comparison of relapse and treatment failure rates among patients with neuromyelitis optica: Multicenter study of treatment efficacy. JAMA Neurol. 2014;71:324–30. doi: 10.1001/jamaneurol.2013.5699. [DOI] [PubMed] [Google Scholar]
- 172.Mehnert U, Birzele J, Reuter K, Schurch B. The effect of botulinum toxin type a on overactive bladder symptoms in patients with multiple sclerosis: A pilot study. J Urol. 2010;184:1011–6. doi: 10.1016/j.juro.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 173.Merle H, Olindo S, Bonnan M, Donnio A, Richer R, Smadja D, et al. Natural history of the visual impairment of relapsing neuromyelitis optica. Ophthalmology. 2007;114:810–5. doi: 10.1016/j.ophtha.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 174.Meurs L, Labeye D, Declercq I, Piéret F, Gille M. Acute transverse myelitis as a main manifestation of early stage II neuroborreliosis in two patients. Eur Neurol. 2004;52:186–8. doi: 10.1159/000081864. [DOI] [PubMed] [Google Scholar]
- 175.Michel MC, Barendrecht MM. Physiological and pathological regulation of the autonomic control of urinary bladder contractility. Pharmacol Ther. 2008;117:297–312. doi: 10.1016/j.pharmthera.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 176.Miclea A, Miclea M, Pistor M, Hoepner A, Chan A, Hoepner R, et al. Vitamin D supplementation differentially affects seasonal multiple sclerosis disease activity. Brain Behav. 2017;7:e00761. doi: 10.1002/brb3.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Milo R, Kahana E. Multiple sclerosis: Geoepidemiology, genetics and the environment. Autoimmun Rev. 2010;9:A387–94. doi: 10.1016/j.autrev.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 178.Min JH, Kim HJ, Kim BJ, Lee KW, Sunwoo IN, Kim SM, et al. Brain abnormalities in Sjogren syndrome with recurrent CNS manifestations: Association with neuromyelitis optica. Mult Scler. 2009;15:1069–76. doi: 10.1177/1352458509106228. [DOI] [PubMed] [Google Scholar]
- 179.Min JH, Waters P, Vincent A, Cho HJ, Joo BE, Woo SY, et al. Low levels of Vitamin D in neuromyelitis optica spectrum disorder: Association with disease disability. PLoS One. 2014;9:e107274. doi: 10.1371/journal.pone.0107274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Miranda MT, Suárez E, Abbas M, Chinea A, Tosado R, Mejías IA, et al. HLA class I & II alleles in multiple sclerosis patients from Puerto Rico. Bol Asoc Med P R. 2013;105:18–23. [PMC free article] [PubMed] [Google Scholar]
- 181.Mirsattari SM, Johnston JB, McKenna R, Del Bigio MR, Orr P, Ross RT, et al. Aboriginals with multiple sclerosis: HLA types and predominance of neuromyelitis optica. Neurology. 2001;56:317–23. doi: 10.1212/wnl.56.3.317. [DOI] [PubMed] [Google Scholar]
- 182.Miyamoto K, Fujihara K, Kira JI, Kuriyama N, Matsui M, Tamakoshi A, et al. The prevalence and characteristics of neuromyelitis optica in Japan: A nationwide epidemiological study. J Neurol Sci. 2017;381:787. doi: 10.1136/jnnp-2017-317321. [DOI] [PubMed] [Google Scholar]
- 183.Miyara M, Gorochov G, Ehrenstein M, Musset L, Sakaguchi S, Amoura Z, et al. Human foxP3+ regulatory T cells in systemic autoimmune diseases. Autoimmun Rev. 2011;10:744–55. doi: 10.1016/j.autrev.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 184.Mok CC, To CH, Mak A, Poon WL. Immunoablative cyclophosphamide for refractory lupus-related neuromyelitis optica. J Rheumatol. 2008;35:172–4. [PubMed] [Google Scholar]
- 185.Montgomery SL, Bowers WJ. Tumor necrosis factor-alpha and the roles it plays in homeostatic and degenerative processes within the central nervous system. J Neuroimmune Pharmacol. 2012;7:42–59. doi: 10.1007/s11481-011-9287-2. [DOI] [PubMed] [Google Scholar]
- 186.Moore P, Methley A, Pollard C, Mutch K, Hamid S, Elsone L, et al. Cognitive and psychiatric comorbidities in neuromyelitis optica. J Neurol Sci. 2016;360:4–9. doi: 10.1016/j.jns.2015.11.031. [DOI] [PubMed] [Google Scholar]
- 187.Morrow MJ, Wingerchuk D. Neuromyelitis optica. J Neuroophthalmol. 2012;32:154–66. doi: 10.1097/WNO.0b013e31825662f1. [DOI] [PubMed] [Google Scholar]
- 188.Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296:2832–8. doi: 10.1001/jama.296.23.2832. [DOI] [PubMed] [Google Scholar]
- 189.Muto M, Mori M, Sato Y, Uzawa A, Masuda S, Kuwabara S, et al. Seasonality of multiple sclerosis and neuromyelitis optica exacerbations in Japan. Mult Scler. 2013;19:378–9. doi: 10.1177/1352458512452332. [DOI] [PubMed] [Google Scholar]
- 190.Nakajima H, Furutama D, Kimura F, Shinoda K, Ohsawa N, Nakagawa T, et al. Herpes simplex virus myelitis: Clinical manifestations and diagnosis by the polymerase chain reaction method. Eur Neurol. 1998;39:163–7. doi: 10.1159/000007927. [DOI] [PubMed] [Google Scholar]
- 191.Nakajima H, Hosokawa T, Sugino M, Kimura F, Sugasawa J, Hanafusa T, et al. Visual field defects of optic neuritis in neuromyelitis optica compared with multiple sclerosis. BMC Neurol. 2010;10:45. doi: 10.1186/1471-2377-10-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Nakamura H, Usa T, Motomura M, Ichikawa T, Nakao K, Kawasaki E, et al. Prevalence of interrelated autoantibodies in thyroid diseases and autoimmune disorders. J Endocrinol Invest. 2008;31:861–5. doi: 10.1007/BF03346432. [DOI] [PubMed] [Google Scholar]
- 193.Nakano H, Tanaka M, Kinoshita M, Tahara M, Matsui M, Tanaka K, et al. Epileptic seizures in Japanese patients with multiple sclerosis and neuromyelitis optica. Epilepsy Res. 2013;104:175–80. doi: 10.1016/j.eplepsyres.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 194.Nazario CM, Szklo M, Diamond E, Román-Franco A, Climent C, Suarez E, et al. Salt and gastric cancer: A case-control study in Puerto Rico. Int J Epidemiol. 1993;22:790–7. doi: 10.1093/ije/22.5.790. [DOI] [PubMed] [Google Scholar]
- 195.Nechemia Y, Moreh E, Weingarden H, Bloch A, Givon U, Vaknin-Dembinsky A, et al. Effectiveness of multi-disciplinary rehabilitation for patients with neuromyelitis optica. J Spinal Cord Med. 2016;39:311–6. doi: 10.1179/2045772315Y.0000000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Nour MM, Nakashima I, Coutinho E, Woodhall M, Sousa F, Revis J, et al. Pregnancy outcomes in aquaporin-4-positive neuromyelitis optica spectrum disorder. Neurology. 2016;86:79–87. doi: 10.1212/WNL.0000000000002208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.O’Connell K, Marnane M, McGuigan C. Bilateral ocular perineuritis as the presenting feature of acute syphilis infection. J Neurol. 2012;259:191–2. doi: 10.1007/s00415-011-6148-0. [DOI] [PubMed] [Google Scholar]
- 198.Oertel FC, Zimmermann H, Paul F, Brandt AU. Optical coherence tomography in neuromyelitis optica spectrum disorders: Potential advantages for individualized monitoring of progression and therapy. EPMA J. 2018;9:21–33. doi: 10.1007/s13167-017-0123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Ogasawara M, Meguro A, Sakai T, Mizuki N, Takahashi T, Fujihara K, et al. Genetic analysis of the aquaporin-4 gene for anti-AQP4 antibody-positive neuromyelitis optica in a Japanese population. Jpn J Ophthalmol. 2016;60:198–205. doi: 10.1007/s10384-016-0441-5. [DOI] [PubMed] [Google Scholar]
- 200.Ortiz AP, Soto-Salgado M, Calo WA, Tortolero-Luna G, Pérez CM, Romero CJ, et al. Incidence and mortality rates of selected infection-related cancers in Puerto Rico and in the United States. Infect Agent Cancer. 2010;5:10. doi: 10.1186/1750-9378-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Pait AS, Whitall DR, Jeffrey CF, Caldow C, Mason AL, Lauenstein GG, et al. Chemical contamination in Southwest Puerto Rico: An assessment of organic contaminants in nearshore sediments. Mar Pollut Bull. 2008;56:580–7. doi: 10.1016/j.marpolbul.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 202.Pamer EG. Fecal microbiota transplantation: Effectiveness, complexities, and lingering concerns. Mucosal Immunol. 2014;7:210–4. doi: 10.1038/mi.2013.117. [DOI] [PubMed] [Google Scholar]
- 203.Pan J, Zhao P, Cai H, Su L, Wood K, Shi FD, et al. Hypoxemia, sleep disturbances, and depression correlated with fatigue in neuromyelitis optica spectrum disorder. CNS Neurosci Ther. 2015;21:599–606. doi: 10.1111/cns.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Pandit L, Kundapur R. Prevalence and patterns of demyelinating central nervous system disorders in urban Mangalore, South India. Mult Scler. 2014;20:1651–3. doi: 10.1177/1352458514521503. [DOI] [PubMed] [Google Scholar]
- 205.Pandit L, Mustafa S, Kunder R, Shetty R, Misri Z, Pai S, et al. Optimizing the management of neuromyelitis optica and spectrum disorders in resource poor settings: Experience from the mangalore demyelinating disease registry. Ann Indian Acad Neurol. 2013;16:572–6. doi: 10.4103/0972-2327.120474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Papadopoulos MC, Verkman AS. Aquaporin 4 and neuromyelitis optica. Lancet Neurol. 2012;11:535–44. doi: 10.1016/S1474-4422(12)70133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Papadopoulos MC, Verkman AS. Aquaporin water channels in the nervous system. Nat Rev Neurosci. 2013;14:265–77. doi: 10.1038/nrn3468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Papais-Alvarenga RM, Miranda-Santos CM, Puccioni-Sohler M, de Almeida AM, Oliveira S, Basilio De Oliveira CA, et al. Optic neuromyelitis syndrome in Brazilian patients. J Neurol Neurosurg Psychiatry. 2002;73:429–35. doi: 10.1136/jnnp.73.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Papeix C, Vidal JS, de Seze J, Pierrot-Deseilligny C, Tourbah A, Stankoff B, et al. Immunosuppressive therapy is more effective than interferon in neuromyelitis optica. Mult Scler. 2007;13:256–9. doi: 10.1177/1352458506070732. [DOI] [PubMed] [Google Scholar]
- 210.Parker SE, Pula JH. Neurosyphilis presenting as asymptomatic optic perineuritis. Case Rep Ophthalmol Med 2012. 2012 doi: 10.1155/2012/621872. 621872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Pellkofer HL, Havla J, Hauer D, Schelling G, Azad SC, Kuempfel T, et al. The major brain endocannabinoid 2-AG controls neuropathic pain and mechanical hyperalgesia in patients with neuromyelitis optica. PLoS One. 2013;8:e71500. doi: 10.1371/journal.pone.0071500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Pellkofer HL, Krumbholz M, Berthele A, Hemmer B, Gerdes LA, Havla J, et al. Long-term follow-up of patients with neuromyelitis optica after repeated therapy with rituximab. Neurology. 2011;76:1310–5. doi: 10.1212/WNL.0b013e3182152881. [DOI] [PubMed] [Google Scholar]
- 213.Pereira CM, Castiglione M, Kasawara KT. Effects of physiotherapy treatment for urinary incontinence in patient with multiple sclerosis. J Phys Ther Sci. 2017;29:1259–63. doi: 10.1589/jpts.28.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Pereira WL, Reiche EM, Kallaur AP, Kaimen-Maciel DR. Epidemiological, clinical, and immunological characteristics of neuromyelitis optica: A review. J Neurol Sci. 2015;355:7–17. doi: 10.1016/j.jns.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 215.Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW, et al. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol. 1996;39:432–41. doi: 10.1002/ana.410390405. [DOI] [PubMed] [Google Scholar]
- 216.Petković F, Castellano B. The role of interleukin-6 in central nervous system demyelination. Neural Regen Res. 2016;11:1922–3. doi: 10.4103/1673-5374.195273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Pinheiro PS, Sherman RL, Trapido EJ, Fleming LE, Huang Y, Gomez-Marin O, et al. Cancer incidence in first generation U.S. Hispanics: Cubans, Mexicans, Puerto Ricans, and New Latinos. Cancer Epidemiol Biomarkers Prev. 2009;18:2162–9. doi: 10.1158/1055-9965.EPI-09-0329. [DOI] [PubMed] [Google Scholar]
- 218.Pisani F, Mastrototaro M, Rossi A, Nicchia GP, Tortorella C, Ruggieri M, et al. Identification of two major conformational aquaporin-4 epitopes for neuromyelitis optica autoantibody binding. J Biol Chem. 2011;286:9216–24. doi: 10.1074/jbc.M110.123000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Pittock SJ, Lennon VA, de Seze J, Vermersch P, Homburger HA, Wingerchuk DM, et al. Neuromyelitis optica and non organ-specific autoimmunity. Arch Neurol. 2008;65:78–83. doi: 10.1001/archneurol.2007.17. [DOI] [PubMed] [Google Scholar]
- 220.Pittock SJ, Lennon VA, Krecke K, Wingerchuk DM, Lucchinetti CF, Weinshenker BG, et al. Brain abnormalities in neuromyelitis optica. Arch Neurol. 2006;63:390–6. doi: 10.1001/archneur.63.3.390. [DOI] [PubMed] [Google Scholar]
- 221.Pittock SJ, Lennon VA, McKeon A, Mandrekar J, Weinshenker BG, Lucchinetti CF, et al. Eculizumab in AQP4-IgG-positive relapsing neuromyelitis optica spectrum disorders: An open-label pilot study. Lancet Neurol. 2013;12:554–62. doi: 10.1016/S1474-4422(13)70076-0. [DOI] [PubMed] [Google Scholar]
- 222.Pittock SJ, Weinshenker BG, Lucchinetti CF, Wingerchuk DM, Corboy JR, Lennon VA, et al. Neuromyelitis optica brain lesions localized at sites of high aquaporin 4 expression. Arch Neurol. 2006;63:964–8. doi: 10.1001/archneur.63.7.964. [DOI] [PubMed] [Google Scholar]
- 223.Popescu BF, Lennon VA, Parisi JE, Howe CL, Weigand SD, Cabrera-Gómez JA, et al. Neuromyelitis optica unique area postrema lesions: Nausea, vomiting, and pathogenic implications. Neurology. 2011;76:1229–37. doi: 10.1212/WNL.0b013e318214332c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Prokunina L, Padyukov L, Bennet A, de Faire U, Wiman B, Prince J, et al. Association of the PD-1.3A allele of the PDCD1 gene in patients with rheumatoid arthritis negative for rheumatoid factor and the shared epitope. Arthritis Rheum. 2004;50:1770–3. doi: 10.1002/art.20280. [DOI] [PubMed] [Google Scholar]
- 225.Qian P, Lancia S, Alvarez E, Klawiter EC, Cross AH, Naismith RT, et al. Association of neuromyelitis optica with severe and intractable pain. Arch Neurol. 2012;69:1482–7. doi: 10.1001/archneurol.2012.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Rafael H. Omental transplantation against nmo and MS: A method to Decrease or Prevent Relapses. Neurol Clin Therapeut J. 2018;2:102. [Google Scholar]
- 227.Rafael H. Omental transplantation for neuromyelitis optica. J Neurol Stroke. 2017;6:00194. [Google Scholar]
- 228.Ramanathan S, Prelog K, Barnes EH, Tantsis EM, Reddel SW, Henderson AP, et al. Radiological differentiation of optic neuritis with myelin oligodendrocyte glycoprotein antibodies, aquaporin-4 antibodies, and multiple sclerosis. Mult Scler. 2016;22:470–82. doi: 10.1177/1352458515593406. [DOI] [PubMed] [Google Scholar]
- 229.Ramírez-Vick M, Hernández-Dávila L, Rodríguez-Rivera N, López-Valentín M, Haddock L, Rodríguez-Martínez R, et al. Prevalence of Vitamin D insufficiency and deficiency among young physicians at university district hospital in San Juan, Puerto Rico. P R Health Sci J. 2015;34:83–8. [PMC free article] [PubMed] [Google Scholar]
- 230.Rodríguez-Quiroga SA, Abaroa L, Arakaki T, Garretto NS, Villa AM. Commentary on neuromyelitis optica associated with painful paroxysmal dystonia: Case report and literature review. Acta Neurol Belg. 2015;115:523–4. doi: 10.1007/s13760-014-0389-5. [DOI] [PubMed] [Google Scholar]
- 231.Rog DJ, Nurmikko TJ, Friede T, Young CA. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology. 2005;65:812–9. doi: 10.1212/01.wnl.0000176753.45410.8b. [DOI] [PubMed] [Google Scholar]
- 232.Rosito S, Nicchia GP, Palazzo C, Lia A, Buccoliero C, Pisani F, et al. Supramolecular aggregation of aquaporin.4 is different in muscle and brain: Correlation with tissue susceptibility in neuromyelitis optica. J Cell Mol Med. 2018;22:1236–46. doi: 10.1111/jcmm.13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Rumah KR, Linden J, Fischetti VA, Vartanian T. Isolation of clostridium perfringens type B in an individual at first clinical presentation of multiple sclerosis provides clues for environmental triggers of the disease. PLoS One. 2013;8:e76359. doi: 10.1371/journal.pone.0076359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Rybicki BA, Major M, Popovich J, Jr, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: A 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145:234–41. doi: 10.1093/oxfordjournals.aje.a009096. [DOI] [PubMed] [Google Scholar]
- 235.Saher G, Brügger B, Lappe-Siefke C, Möbius W, Tozawa R, Wehr MC, et al. High cholesterol level is essential for myelin membrane growth. Nat Neurosci. 2005;8:468–75. doi: 10.1038/nn1426. [DOI] [PubMed] [Google Scholar]
- 236.Sahraian MA, Moghadasi AN, Azimi AR, Asgari N, H Akhoundi F, Abolfazli R, et al. Diagnosis and management of neuromyelitis optica spectrum disorder (NMOSD) in Iran: A consensus guideline and recommendations. Mult Scler Relat Disord. 2017;18:144–51. doi: 10.1016/j.msard.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 237.Sang CN. NMDA-receptor antagonists in neuropathic pain: Experimental methods to clinical trials. J Pain Symptom Manage. 2000;19:S21–5. doi: 10.1016/s0885-3924(99)00125-6. [DOI] [PubMed] [Google Scholar]
- 238.Sato DK, Callegaro D, Lana-Peixoto MA, Nakashima I, Fujihara K. Seronegative neuromyelitis optica spectrum – The challenges on disease definition and pathogenesis. Arq Neuropsiquiatr. 2014;72:445–50. doi: 10.1590/0004-282x20140032. [DOI] [PubMed] [Google Scholar]
- 239.Satoh J, Obayashi S, Misawa T, Tabunoki H, Yamamura T, Arima K, et al. Neuromyelitis optica/Devic's disease: Gene expression profiling of brain lesions. Neuropathology. 2008;28:561–76. doi: 10.1111/j.1440-1789.2008.00915.x. [DOI] [PubMed] [Google Scholar]
- 240.Schreiber AL, Fried GW, Formal CS, DeSouza BX. Rehabilitation of neuromyelitis optica (Devic syndrome): Three case reports. Am J Phys Med Rehabil. 2008;87:144–8. doi: 10.1097/PHM.0b013e31815b5e1a. [DOI] [PubMed] [Google Scholar]
- 241.Scott BJ, Douglas VC, Tihan T, Rubenstein JL, Josephson SA. A systematic approach to the diagnosis of suspected central nervous system lymphoma. JAMA Neurol. 2013;70:311–9. doi: 10.1001/jamaneurol.2013.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sellner J, Boggild M, Clanet M, Hintzen RQ, Illes Z, Montalban X, et al. EFNS guidelines on diagnosis and management of neuromyelitis optica. Eur J Neurol. 2010;17:1019–32. doi: 10.1111/j.1468-1331.2010.03066.x. [DOI] [PubMed] [Google Scholar]
- 243.Seok JM, Cho HJ, Ahn SW, Cho EB, Park MS, Joo IS, et al. Clinical characteristics of late-onset neuromyelitis optica spectrum disorder: A multicenter retrospective study in Korea. Mult Scler. 2017;23:1748–56. doi: 10.1177/1352458516685416. [DOI] [PubMed] [Google Scholar]
- 244.Sepúlveda M, Armangué T, Sola-Valls N, Arrambide G, Meca-Lallana JE, Oreja-Guevara C, et al. Neuromyelitis optica spectrum disorders. Neurol Neuroimmunol Neuroinflammation. 2016;3:e225. doi: 10.1212/NXI.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Shan Y, Tan S, Zhang L, Huang J, Sun X, Wang Y, et al. Serum 25-hydroxyvitamin D3 is associated with disease status in patients with neuromyelitis optica spectrum disorders in South China. J Neuroimmunol. 2016;299:118–23. doi: 10.1016/j.jneuroim.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 246.Sheng P, Hou L, Wang X, Wang X, Huang C, Yu M, et al. Efficacy of modafinil on fatigue and excessive daytime sleepiness associated with neurological disorders: A systematic review and meta-analysis. PLoS One. 2013;8:e81802. doi: 10.1371/journal.pone.0081802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sherman E, Han MH. Acute and chronic management of neuromyelitis optica spectrum disorder. Curr Treat Options Neurol. 2015;17:48. doi: 10.1007/s11940-015-0378-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Shevach EM. Regulatory T cells in autoimmmunity*. Annu Rev Immunol. 2000;18:423–49. doi: 10.1146/annurev.immunol.18.1.423. [DOI] [PubMed] [Google Scholar]
- 249.Simon KC, Schmidt H, Loud S, Ascherio A. Risk factors for multiple sclerosis, neuromyelitis optica and transverse myelitis. Mult Scler. 2015;21:703–9. doi: 10.1177/1352458514551780. [DOI] [PubMed] [Google Scholar]
- 250.Singh B, Schwartz JA, Sandrock C, Bellemore SM, Nikoopour E. Modulation of autoimmune diseases by interleukin (IL)-17 producing regulatory T helper (Th17) cells. Indian J Med Res. 2013;138:591–4. [PMC free article] [PubMed] [Google Scholar]
- 251.Singhrao SK, Neal JW, Rushmere NK, Morgan BP, Gasque P. Spontaneous classical pathway activation and deficiency of membrane regulators render human neurons susceptible to complement lysis. Am J Pathol. 2000;157:905–18. doi: 10.1016/S0002-9440(10)64604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Smith GT, Goldmeier D, Migdal C. Neurosyphilis with optic neuritis: An update. Postgrad Med J. 2006;82:36–9. doi: 10.1136/pgmj.2004.020875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Smith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci. 2006;8:383–95. doi: 10.31887/DCNS.2006.8.4/ssmith. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Spach KM, Nashold FE, Dittel BN, Hayes CE. IL-10 signaling is essential for 1,25-dihydroxyvitamin D3-mediated inhibition of experimental autoimmune encephalomyelitis. J Immunol. 2006;177:6030–7. doi: 10.4049/jimmunol.177.9.6030. [DOI] [PubMed] [Google Scholar]
- 255.Spooren A, Kooijman R, Lintermans B, Van Craenenbroeck K, Vermeulen L, Haegeman G, et al. Cooperation of NFkappaB and CREB to induce synergistic IL-6 expression in astrocytes. Cell Signal. 2010;22:871–81. doi: 10.1016/j.cellsig.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 256.Stern BJ, Krumholz A, Johns C, Scott P, Nissim J. Sarcoidosis and its neurological manifestations. Arch Neurol. 1985;42:909–17. doi: 10.1001/archneur.1985.04060080095022. [DOI] [PubMed] [Google Scholar]
- 257.Stiebel-Kalish H, Lotan I, Brody J, Chodick G, Bialer O, Marignier R, et al. Retinal nerve fiber layer may be better preserved in MOG-IgG versus AQP4-IgG optic neuritis: A Cohort study. PLoS One. 2017;12:e0170847. doi: 10.1371/journal.pone.0170847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Storoni M, Petzold A, Plant GT. The use of serum glial fibrillary acidic protein measurements in the diagnosis of neuromyelitis optica spectrum optic neuritis. PLoS One. 2011;6:e23489. doi: 10.1371/journal.pone.0023489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Suárez-Martínez EB, Pérez CM, Cruz SK, Khorsandi S, Chardón C, Ferder L, et al. Importance of Vitamin D and Vitamin D levels status in Puerto Ricans. J Health Care Poor Underserved. 2013;24:38–47. doi: 10.1353/hpu.2014.0000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Suzuki K, Nakamura T, Hashimoto K, Miyamoto M, Komagamine T, Nagashima T, et al. Hypothermia, hypotension, hypersomnia, and obesity associated with hypothalamic lesions in a patient positive for the anti-aquaporin 4 antibody: A case report and literature review. Arch Neurol. 2012;69:1355–9. doi: 10.1001/archneurol.2012.300. [DOI] [PubMed] [Google Scholar]
- 261.Takahashi T, Miyazawa I, Misu T, Takano R, Nakashima I, Fujihara K, et al. Intractable hiccup and nausea in neuromyelitis optica with anti-aquaporin-4 antibody: A herald of acute exacerbations. J Neurol Neurosurg Psychiatry. 2008;79:1075–8. doi: 10.1136/jnnp.2008.145391. [DOI] [PubMed] [Google Scholar]
- 262.Tanaka M, Tanaka K. Sudden hearing loss as the initial symptom in Japanese patients with multiple sclerosis and seropositive neuromyelitis optica spectrum disorders. J Neuroimmunol. 2016;298:16–8. doi: 10.1016/j.jneuroim.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 263.Tanaka T, Kishimoto T. Targeting interleukin-6: All the way to treat autoimmune and inflammatory diseases. Int J Biol Sci. 2012;8:1227–36. doi: 10.7150/ijbs.4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Tenembaum S, Chitnis T, Nakashima I, Collongues N, McKeon A, Levy M, et al. Neuromyelitis optica spectrum disorders in children and adolescents. Neurology. 2016;87:S59–66. doi: 10.1212/WNL.0000000000002824. [DOI] [PubMed] [Google Scholar]
- 265.Thorlacius S, Aarli JA, Riise T, Matre R, Johnsen HJ. Associated disorders in myasthenia gravis: Autoimmune diseases and their relation to thymectomy. Acta Neurol Scand. 1989;80:290–5. doi: 10.1111/j.1600-0404.1989.tb03881.x. [DOI] [PubMed] [Google Scholar]
- 266.Tradtrantip L, Yao X, Su T, Smith AJ, Verkman AS. Bystander mechanism for complement-initiated early oligodendrocyte injury in neuromyelitis optica. Acta Neuropathol. 2017;134:35–44. doi: 10.1007/s00401-017-1734-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Tran C, Du Pasquier RA, Cavassini M, Guex-Crosier Y, Meuli R, Ciuffreda D, et al. Neuromyelitis optica following CMV primo-infection. J Intern Med. 2007;261:500–3. doi: 10.1111/j.1365-2796.2007.01794.x. [DOI] [PubMed] [Google Scholar]
- 268.Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002;59:499–505. doi: 10.1212/wnl.59.4.499. [DOI] [PubMed] [Google Scholar]
- 269.Trebst C, Jarius S, Berthele A, Paul F, Schippling S, Wildemann B, et al. Update on the diagnosis and treatment of neuromyelitis optica: Recommendations of the neuromyelitis optica study group (NEMOS) J Neurol. 2014;261:1–6. doi: 10.1007/s00415-013-7169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Uribe-San Martin R, Ciampi E, Galilea A, Sandoval P, Miranda H, Mellado P, et al. Neuromyelitis optica spectrum disorders: Profile of a cohort according to the 2015 diagnostic criteria. Rev Neurol. 2017;65:193–202. [PubMed] [Google Scholar]
- 271.Uzawa A, Mori M, Arai K, Sato Y, Hayakawa S, Masuda S, et al. Cytokine and chemokine profiles in neuromyelitis optica: Significance of interleukin-6. Mult Scler. 2010;16:1443–52. doi: 10.1177/1352458510379247. [DOI] [PubMed] [Google Scholar]
- 272.Vahtera T, Haaranen M, Viramo-Koskela AL, Ruutiainen J. Pelvic floor rehabilitation is effective in patients with multiple sclerosis. Clin Rehabil. 1997;11:211–9. doi: 10.1177/026921559701100304. [DOI] [PubMed] [Google Scholar]
- 273.Vaknin-Dembinsky A, Brill L, Kassis I, Petrou P, Ovadia H, Ben-Hur T, et al. T-cell responses to distinct AQP4 peptides in patients with neuromyelitis optica (NMO) Mult Scler Relat Disord. 2016;6:28–36. doi: 10.1016/j.msard.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 274.Van Dijk JM, TerBrugge KG, Willinsky RA, Farb RI, Wallace MC. Multidisciplinary management of spinal dural arteriovenous fistulas: Clinical presentation and long-term follow-up in 49 patients. Stroke. 2002;33:1578–83. doi: 10.1161/01.str.0000018009.83713.06. [DOI] [PubMed] [Google Scholar]
- 275.van Loo G, De Lorenzi R, Schmidt H, Huth M, Mildner A, Schmidt-Supprian M, et al. Inhibition of transcription factor NF-kappaB in the central nervous system ameliorates autoimmune encephalomyelitis in mice. Nat Immunol. 2006;7:954–61. doi: 10.1038/ni1372. [DOI] [PubMed] [Google Scholar]
- 276.van Pelt ED, Wong YY, Ketelslegers IA, Hamann D, Hintzen RQ. Neuromyelitis optica spectrum disorders: Comparison of clinical and magnetic resonance imaging characteristics of AQP4-IgG versus MOG-IgG seropositive cases in the Netherlands. Eur J Neurol. 2016;23:580–7. doi: 10.1111/ene.12898. [DOI] [PubMed] [Google Scholar]
- 277.Vanotti S, Cores EV, Eizaguirre B, Melamud L, Rey R, Villa A, et al. Cognitive performance of neuromyelitis optica patients: Comparison with multiple sclerosis. Arq Neuropsiquiatr. 2013;71:357–61. doi: 10.1590/0004-282X20130038. [DOI] [PubMed] [Google Scholar]
- 278.Vincent T, Saikali P, Cayrol R, Roth AD, Bar-Or A, Prat A, et al. Functional consequences of neuromyelitis optica-IgG astrocyte interactions on blood-brain barrier permeability and granulocyte recruitment. J Immunol. 2008;181:5730–7. doi: 10.4049/jimmunol.181.8.5730. [DOI] [PubMed] [Google Scholar]
- 279.von Glehn F, Jarius S, Penalva de Oliveira AC, Brandão CO, Farias AS, Damasceno A, et al. Aquaporin-4 antibodies are not related to HTLV-1 associated myelopathy. PLoS One. 2012;7:e39372. doi: 10.1371/journal.pone.0039372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Wang H, Dai Y, Qiu W, Zhong X, Wu A, Wang Y, et al. HLA-DPB1 0501 is associated with susceptibility to anti-aquaporin-4 antibodies positive neuromyelitis optica in Southern Han Chinese. J Neuroimmunol. 2011;233:181–4. doi: 10.1016/j.jneuroim.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 281.Wang H, Wang K, Wang C, Xu F, Qiu W, Hu X, et al. Increased plasma interleukin-32 expression in patients with neuromyelitis optica. J Clin Immunol. 2013;33:666–70. doi: 10.1007/s10875-012-9837-2. [DOI] [PubMed] [Google Scholar]
- 282.Wang H, Wang K, Zhong X, Dai Y, Qiu W, Wu A, et al. Notable increased cerebrospinal fluid levels of soluble interleukin-6 receptors in neuromyelitis optica. Neuroimmunomodulation. 2012;19:304–8. doi: 10.1159/000339302. [DOI] [PubMed] [Google Scholar]
- 283.Wang H, Zhong X, Wang K, Qiu W, Li J, Dai Y, et al. Interleukin 17 gene polymorphism is associated with anti-aquaporin 4 antibody-positive neuromyelitis optica in the Southern Han Chinese – A case control study. J Neurol Sci. 2012;314:26–8. doi: 10.1016/j.jns.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 284.Wang J, Tian Y, Shao Y, Feng H, Qin L, Xu W, et al. Comparison of spontaneous brain activity revealed by regional homogeneity in AQP4-IgG neuromyelitis optica-optic neuritis versus MOG-IgG optic neuritis patients: A resting-state functional MRI study. Neuropsychiatr Dis Treat. 2017;13:2669–79. doi: 10.2147/NDT.S145183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Watanabe M, Furusho K, Takahashi T, Tamaoka A. Galactorrhea in a patient with aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder: A case report and review of the literature. Neurologist. 2015;20:101–3. doi: 10.1097/NRL.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 286.Watanabe S, Misu T, Miyazawa I, Nakashima I, Shiga Y, Fujihara K, et al. Low-dose corticosteroids reduce relapses in neuromyelitis optica: A retrospective analysis. Mult Scler. 2007;13:968–74. doi: 10.1177/1352458507077189. [DOI] [PubMed] [Google Scholar]
- 287.Weaver CT, Elson CO, Fouser LA, Kolls JK. The Th17 pathway and inflammatory diseases of the intestines, lungs, and skin. Annu Rev Pathol. 2013;8:477–512. doi: 10.1146/annurev-pathol-011110-130318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Wei Q, Yanyu C, Rui L, Caixia L, Youming L, Jianhua H, et al. Human aquaporin 4 gene polymorphisms in Chinese patients with neuromyelitis optica. J Neuroimmunol. 2014;274:192–6. doi: 10.1016/j.jneuroim.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 289.Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85:177–89. doi: 10.1212/WNL.0000000000001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic's syndrome) Neurology. 1999;53:1107–14. doi: 10.1212/wnl.53.5.1107. [DOI] [PubMed] [Google Scholar]
- 291.Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG. The spectrum of neuromyelitis optica. Lancet Neurol. 2007;6:805–15. doi: 10.1016/S1474-4422(07)70216-8. [DOI] [PubMed] [Google Scholar]
- 292.Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66:1485–9. doi: 10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 293.Wingerchuk DM, Weinshenker BG. Neuromyelitis optica: Clinical predictors of a relapsing course and survival. Neurology. 2003;60:848–53. doi: 10.1212/01.wnl.0000049912.02954.2c. [DOI] [PubMed] [Google Scholar]
- 294.Wingerchuk DM, Weinshenker BG. The emerging relationship between neuromyelitis optica and systemic rheumatologic autoimmune disease. Mult Scler. 2012;18:5–10. doi: 10.1177/1352458511431077. [DOI] [PubMed] [Google Scholar]
- 295.Wingerchuk DM. Neuromyelitis optica: Current concepts. Front Biosci. 2004;9:834–40. doi: 10.2741/1267. [DOI] [PubMed] [Google Scholar]
- 296.Wingerchuk DM. Neuromyelitis optica: Effect of gender. J Neurol Sci. 2009;286:18–23. doi: 10.1016/j.jns.2009.08.045. [DOI] [PubMed] [Google Scholar]
- 297.Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013;496:513–7. doi: 10.1038/nature11984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Yamamoto T, Mori M, Uzawa A, Uchiyama T, Sakakibara R, Yanagisawa M, et al. Urinary symptoms and neurological disabilities are differentially correlated between multiple sclerosis and neuromyelitis optica. Clin Exp Neuroimmunol. 2016;7:52–8. [Google Scholar]
- 299.Yao X, Verkman AS. Complement regulator CD59 prevents peripheral organ injury in rats made seropositive for neuromyelitis optica immunoglobulin G. Acta Neuropathol Commun. 2017;5:57. doi: 10.1186/s40478-017-0462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Yao X, Verkman AS. Marked central nervous system pathology in CD59 knockout rats following passive transfer of neuromyelitis optica immunoglobulin G. Acta Neuropathol Commun. 2017;5:15. doi: 10.1186/s40478-017-0417-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Yesilot N, Mutlu M, Gungor O, Baykal B, Serdaroglu P, Akman-Demir G, et al. Clinical characteristics and course of spinal cord involvement in Behçet's disease. Eur J Neurol. 2007;14:729–37. doi: 10.1111/j.1468-1331.2007.01754.x. [DOI] [PubMed] [Google Scholar]
- 302.Yoshimura S, Isobe N, Matsushita T, Yonekawa T, Masaki K, Sato S, et al. Distinct genetic and infectious profiles in Japanese neuromyelitis optica patients according to anti-aquaporin 4 antibody status. J Neurol Neurosurg Psychiatry. 2013;84:29–34. doi: 10.1136/jnnp-2012-302925. [DOI] [PubMed] [Google Scholar]
- 303.Zaidi SF. Helicobacter pylori associated asian enigma: Does diet deserve distinction? World J Gastrointest Oncol. 2016;8:341–50. doi: 10.4251/wjgo.v8.i4.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, et al. Central nervous system sarcoidosis – Diagnosis and management. QJM. 1999;92:103–17. doi: 10.1093/qjmed/92.2.103. [DOI] [PubMed] [Google Scholar]
- 305.Zamvil SS, Spencer CM, Baranzini SE, Cree BA. The gut microbiome in neuromyelitis optica. Neurotherapeutics. 2018;15:92–101. doi: 10.1007/s13311-017-0594-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Zarei S, Carr K, Reiley L, Diaz K, Guerra O, Altamirano PF, et al. A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int. 2015;6:171. doi: 10.4103/2152-7806.169561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Zhang H, Verkman AS. Longitudinally extensive NMO spinal cord pathology produced by passive transfer of NMO-IgG in mice lacking complement inhibitor CD59. J Autoimmun. 2014;53:67–77. doi: 10.1016/j.jaut.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Zhao S, Mutch K, Elsone L, Miller J, Jacob A. An unusual case of ‘itchy paralysis’: Neuromyelitis optica presenting with severe neuropathic itch. Pract Neurol. 2015;15:149–51. doi: 10.1136/practneurol-2014-000936. [DOI] [PubMed] [Google Scholar]
- 309.Zhao S, Mutch K, Elsone L, Nurmikko T, Jacob A. Neuropathic pain in neuromyelitis optica affects activities of daily living and quality of life. Mult Scler. 2014;20:1658–61. doi: 10.1177/1352458514522103. [DOI] [PubMed] [Google Scholar]
- 310.Zhong YH, Zhong ZG, Zhou Z, Ma ZY, Qiu MY, Peng FH, et al. Comparisons of presentations and outcomes of neuromyelitis optica patients with and without Sjögren's syndrome. Neurol Sci. 2017;38:271–7. doi: 10.1007/s10072-016-2751-2. [DOI] [PubMed] [Google Scholar]


