Abstract
A female patient, 20 years old, with a history of a progressive increase in abdominal volume on the left side, starting 3 years ago, with no associated symptoms and no history of trauma. Ultrasonography and a computed tomography scan of the abdomen were performed, which revealed a large splenomegaly, and a partial minilaparoscopic splenectomy was indicated. We opted for unroofing of the cyst, and the procedure was uneventful, with a total surgical time of 47 min. The patient progressed clinically well, without abdominal pain, being discharged on the 2nd post-operative day.
Keywords: Abdominal surgery, minimally invasive surgery, needlescopic surgery, partial splenectomy, splenic cyst, video surgery
INTRODUCTION
Splenic cysts are an uncommon disease in all age groups but predominate in the second and third decades of life, with no difference in prevalence between the sexes.[1] They are classified into true cysts (parasitic or nonparasitic), which are encapsulated; and pseudocysts (or secondary), which are not. Currently, minimally invasive surgery has been considered the gold standard approach due to its effectiveness.[2,3]
CASE REPORT
A 20-year-old female patient, previously healthy, presented with a history of progressive abdominal volume increase on the left side starting 3 years ago, with no associated symptoms and no history of trauma. General physical examination showed no specific signs; on examination of the abdomen, a large, painless, solid mass was palpated in the left hypochondrium. Ultrasonography (USG) of the abdomen showed splenomegaly, without specifying characteristics or size.
She was hospitalised for a diagnostic investigation of giant splenomegaly, and we performed a Doppler USG, which found a hypoechogenic splenic cyst, with thick contents and no vascularisation. A computed tomography (CT) scan of the abdomen was performed, showing a large cystic expansive cystic enlargement in the spleen, measuring 21.0 cm × 14.0 cm × 18.0 cm [Figure 1].
Figure 1.

Ultrasonography of the abdomen (a) showing significant splenomegaly, later confirmed by computed tomography (b and c), which showed a large, simple cystic expansion of the spleen, measuring 21.0 cm × 14.0 cm × 18.0 cm
The diagnosis was a giant splenic cyst, and surgical treatment of partial splenectomy by minilaparoscopy was indicated.
Surgical description
The surgery was performed with the patient in the right lateral decubitus position. The pneumoperitoneum was made by the open technique, introducing a 10 mm trocar into an umbilical incision. Then, a 5 mm trocar was placed in the mesogastrium, a 3 mm one in the left flank and another 3 mm one in the epigastrium. A large cyst was observed in close communication with the spleen with small adherence to the left hepatic lobe. The procedure was initiated by the perforation of the cyst, at its apex, with the aspirator by the 5 mm trocar for complete emptying of its contents, which totalled 1800 mL [Figure 2]. Following the precepts of splenic preservation, we chose to perform unroofing of the cyst, trying to save as much splenic tissue as possible. Resection and sanding of a large part of the cyst wall were performed with advanced bipolar energy tweezers, and a small fragment of splenic tissue was also removed [Figure 2].
Figure 2.
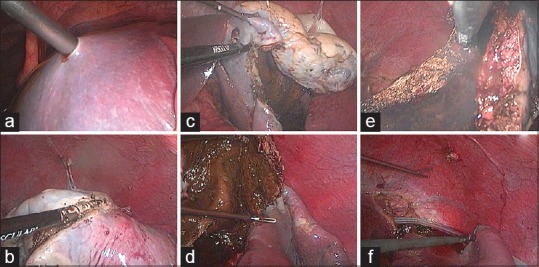
(a) Cyst perforation, at its apex, with the aspirator for complete emptying of its contents, which totalled 1800 mL. (b) Beginning of resection of the cyst with the advanced caliper of Caiman. (c) Follow-up of unroofing. (d) Very friable area inside the cyst, which is subject to bleeding in cases of unsatisfactory haemostasis. (e) Cauterisation of the edges of the cyst, to avoid relapses. (f) Counter critical drain placement through the 3 mm portal on the left flank
The cyst capsule was retrograded through the 10 mm portal of the umbilical region. The histopathological study proved the lesion was a non-parasitic splenic cyst. The procedure was uncomplicated, with a total surgical time of 47 min. The patient progressed clinically well, without abdominal pain, haemodynamically stable and was discharged on the 2nd post-operative day.
DISCUSSION
Most primary cysts are clinically silent and are diagnosed incidentally on USG or CT.[1] Large spleen cysts are susceptible to various complications, such as bleeding and rupture after abdominal trauma or infection.[2]
Most cases require only expectant follow-up, with USG performed every 6 months. The surgical approach is indicated for symptomatic cysts or those with a diameter >5 cm because of the increased risk of bleeding, rupture and infection.[3] Total laparotomy splenectomy used to be the surgical treatment of choice for splenic cysts. However, the minimally invasive approach has been shown to be effective in these cases and is currently considered the gold standard.[4]
Among the new minimally invasive techniques, minilaparoscopy has advantages when compared with traditional laparoscopy because it causes less trauma to the abdominal wall, leading to less pain and a shorter time of hospitalisation. Firme et al.[4] have shown that for coarser approaches conventional 5 mm instruments are better, but for more precise and complex procedures the low friction offered by 3 mm instruments are better. These conclusions lead to the possibility of greater preservation of splenic tissue. Minilaparoscopy has also been shown to be safe and effective for other approaches, such as cholecystectomy and herniorrhaphy. Other more complex procedures have also been described.[5] This is the second report in the literature of a giant splenic cyst resected by minilaparoscopy.
This case report describes minilaparoscopy being successfully used to treat a nonparasitic giant splenic cyst. Although there is no consensus on the ideal approach in this case, minilaparoscopic decapsulation of the cyst proved to be a safe and effective method, and its advantages were useful for the procedure performed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ingle SB, Hinge Ingle CR, Patrike S. Epithelial cysts of the spleen: A minireview. World J Gastroenterol. 2014;20:13899–903. doi: 10.3748/wjg.v20.i38.13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farhangi B, Farhangi A, Firouzjahi A, Jahed B. Huge epithelial nonparasitic splenic cyst: A case report and a review of treatment methods. Caspian J Intern Med. 2016;7:146–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Carvalho GL, Lima DL, Silva FW, Góes GH. Giant nonparasitic splenic cyst managed by minilaparoscopy. CRSLS MIS Case Rep SLS. 2017;21:1–5. [Google Scholar]
- 4.Firme WA, Carvalho GL, Lima DL, Lopes VG, Montandon ID, Santos Filho F, et al. Low-friction minilaparoscopy outperforms regular 5-mm and 3-mm instruments for precise tasks. JSLS. 2015;19:pii: e201500067. doi: 10.4293/JSLS.2015.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carvalho GL, Abreu GF, Lima DL, Góes GH. Type IV mirizzi syndrome treated by hepaticoduodenostomy by minilaparoscopy. CRSLS. e2016;3:e201600057. Doi: 10.4293/CRSLS.2016.00057. [Google Scholar]


