Abstract
Aim:
The aim of this study was to analyse our data of laparoscopic hysterectomy for large uteri (>16 weeks size) regarding their perioperative outcomes and possible factors for conversions to open surgery over 5 years. It also describes our techniques for the feasibility of performing such hysterectomies by the minimally invasive way.
Materials and Methods:
A five-year retrospective chart review was performed at the Minimal Access and Robotic Surgery Unit of the Department of Gynecology at Apollo Hospital, Hyderabad. Demographic and pre-operative and post-operative data were recorded. Clinical assessment including bimanual examination and surgery was made by a single senior surgeon. Intra-operative conversions, complications and post-operative complications were recorded.
Results:
A total of 128 women were included in this study, 5 patients underwent robotic-assisted hysterectomy. The average age was 44.4, body mass index - was 27.6 and size of the uterus was 17.5 weeks. The most common diagnosis was leiomyoma. The median Operating room (OR) time was 107 min. There was a need for myomectomy in 39.8%, extensive adhesiolysis in 33.6% and dense bladder adhesion in 26.6%. The average drop in haemoglobin was 1.72 g%, and hospital stay was 2 days. The specimen was removed by vaginal morcellation (2 cases via an umbilical port). Conversion to open surgery was required in 10.9% of cases. The conversion was significantly correlated with excessive haemorrhage and bladder injury but not with difficult hysterectomy, difficult bladder dissection or adhesions. There were 3 cases of bladder injury detected and managed intraoperatively.
Conclusion:
Laparoscopic hysterectomy is technically feasible and safe procedure for large uteri. The learning curve is about 50 cases and can be performed by experienced surgeons regardless of the size, number or location of the myomas without much morbidity.
Keywords: Conversion, feasibility, fibroid, hysterectomy, laparoscopic, outcomes, robotic, techniques
INTRODUCTION
Hysterectomy is one of the most common gynaecological surgeries performed on women and 70% indications are benign disease. In a survey done at Manipal Hospital, India, in 2014, around 60% of major gynaecological surgeries were hysterectomy. The most common surgical approach was abdominal (74.7%), followed by vaginal (17.8%) and laparoscopic hysterectomy in (6.6%). The most common indication for hysterectomy was symptomatic fibroid uterus (39.9%), and this data include all hysterectomies and not only for the large uteri.[1] A decade long data from the UK shows the same trend of abdominal hysterectomies being 5–6-fold more common than vaginal or laparoscopic approach.[2] Various scientific papers have shown clear benefits to a minimally invasive approach for hysterectomy, however, we have limited evidence regarding outcomes large uterus and laparoscopy.[3,4,5,6] Hysterectomy for large uteri is challenging, especially so when attempted with the laparoscopic approach as large fibroids fill the pelvis obstructing the view and ability to reach the pedicles. These uteri are also difficult to mobilise and manipulate, thus obscuring surrounding anatomic structures. One cannot deny the advantages of laparoscopic surgeries such as less blood loss, less post-operative pain due to less insult to the abdominal wall, quick mobilisation and recovery. In fact, the laparoscopic approach is advantageous to the surgeon as well as surgery is performed in better and magnified vision of deep pelvic structures and gives the ability to perform detailed surgery. Despite the advantages of laparoscopic surgery, laparotomy remains the most widely used access route for performing hysterectomy worldwide, especially for the large uterus. There are no clear guidelines about surgical approach to large uteri, but each surgeon should approach with the method they are most competent with. Literature recommends that cases with uterus >15 weeks size or weight >500 g should not be attempted as minimally invasive surgery.[7] Uccella et al. published a series of 258 patients who underwent hysterectomy for uteri ≥1 kg. They attempted 55 (21.3%) women by open surgery and 203 (78.7%) by laparoscopy.[8] In tertiary referral centres with extensive experience and high volume as ours, one may attempt larger uteri for laparoscopic hysterectomy. The volume of the uterus is more critical than the weight as this is the limiting factor both during the steps in performing the surgery as well as retrieving the specimen by morcellation in the end. Both of these steps determine the operative time and the feasibility.
The aim of this study was to analyse our data of laparoscopic hysterectomy for large uteri (>16 weeks size) regarding their perioperative outcomes and possible factors for conversions to open surgery over 5 years. It also describes our techniques for the feasibility of performing such hysterectomies by the minimally invasive way.
MATERIALS AND METHODS
This is a retrospective analytical study review at Apollo Health City, Hyderabad, India of patients who underwent minimally invasive hysterectomy, during the past 5 years. Data were collected for all patients with clinical size >16 weeks of the uterus. The estimated clinical weight has a significant correlation with the actual weight of specimen according to PRESS scores;[9] hence, we used this pre-operative criteria in deciding the route of hysterectomy [Figure 1a and b]. All women underwent a routine pre-operative assessment including a bimanual exam, Papanicolaou smear, and a pelvic ultrasound scan. Women presenting with abnormal bleeding had either diagnostic hysteroscopy with an endometrial biopsy or pipelle biopsy in the office to rule out endometrial pathology. Every patient was thoroughly counselled regarding the non-surgical options and then surgical procedure recommended. A written informed consent was taken. All cases included in this study, underwent pre-operative clinical assessment of uterine size by a single senior surgeon. The same surgeon performed all surgeries (laparoscopic and robotic). Pre-operatively clinical characteristics were collected including age, body mass index (BMI), parity and history of prior abdominal surgeries. The data regarding surgery were the surgical approach, operative time from incision to closure estimated blood loss and conversion to laparotomy. A decrease in haemoglobin (haemoglobin drop) was calculated as the pre-operative haemoglobin value minus the haemoglobin value on the 1st post-operative day. Intra-operative data collected were number and location of ports, number and location of fibroids, need for intra-uterine manipulator and the use of myoma screw for manipulation. Any need for adhesiolysis, intra-operative myomectomy and difficulty in bladder dissection due to previous adhesions of caesarean section were recorded from the operative notes. Intra-operative suprapubic incision (used as a marker for conversion to open surgery from laparoscopy) was noted. Visceral injury (bladder, bowel or ureters) was also recorded. All specimens were removed by cold knife morcellation either through vagina or umbilical port. Details of post-operative analgesia requirement, length of hospital stay, blood transfusion requirement and pathologic diagnosis from pathology reports were noted. The hospital stay was counted from the day of the surgery. Post-operative complications were classified according to the Clavin–Dindo classification.[10]
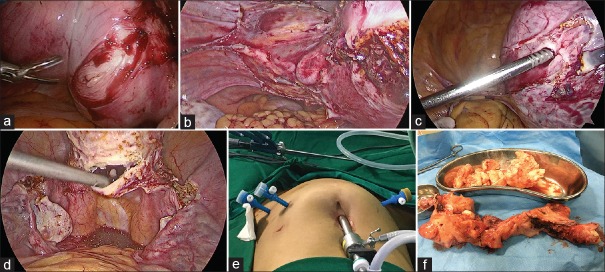
Figure 1.
(a) Clinical picture showing the size of uterus of 22 weeks included in study. (b) Laparoscopic view of the same case (22 weeks) before starting the laparoscopic hysterectomy
RESULTS
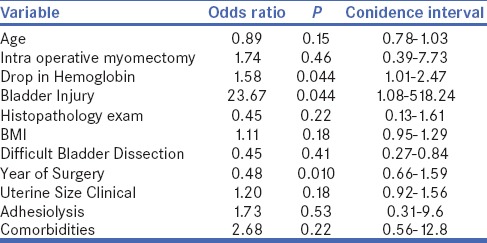
A total of 128 patients were selected for this study from 2011 to 2016. All cases included in this study were >16 weeks size with average clinical size being 17.5 weeks, the upper limit being 28 weeks. One hundred and twenty-three underwent laparoscopic hysterectomy while 5 patients in this series underwent robotic-assisted hysterectomy. A uterine manipulator was used 66% of cases, and the rest were manipulated intraoperatively by myoma screw. Patient characteristics are shown in Table 1. All women in this series were Asian Indian with median (range) age was 44.4 (31–62) years, and BMI was 27.7 (24–44). Forty-seven (36.7%) had prior caesarean sections and 11 (8.5%) patients had an abdominal laparotomy (excluding lower segment caesarean section). The majority of cases had single myoma (64%). Multiple myomas were in 26.5% of cases while 9.5% of cases had adenomyosis. The median operative time was 107 min, and the median stay of patients in hospital was 2 days. Table 2 includes the surgical characteristics of the various intra-operative modifications and strategies used by our unit to complete minimally invasive hysterectomies. Fourteen cases were converted to laparotomy via a suprapubic incision (10.9%). Six conversions were secondary to haemorrhage, 5 cases due to the difficulty to reaching all pedicles, 1 case secondary to extensive adhesions and two cases due to bladder injury. Ten cases were classified to have intra operative complications. Six patients had haemorrhage was >1000 ml and were managed by converting to laparotomy and blood transfusion. In addition to this 30 additional cases needed transfusion. Seventeen cases were transfused to build up haemoglobin levels as this was below 8 g/dl at the time of admission. In 13 cases, transfusion was done in post-operative period for unstable vital signs in the setting of a low starting haemoglobin; although, the estimated blood loss in these cases was not >300 ml. Three cases of bladder injury were detected, 2 underwent repair by open surgery, and one was managed by laparoscopic suturing. The average drop in haemoglobin was 1.72 g/dl. We further analysed our results for factors that contributed to intra-operative conversion. A multiple regression analysis of various parameters with suprapubic incision was done [Table 3]. Suprapubic incision or conversion significantly correlated with a drop in haemoglobin (excessive haemorrhage) and bladder injury. The factors such as inability to complete hysterectomy due to location and size of myoma, difficult bladder dissection (previous caesarean sections) or adhesions did not correlate significantly with conversion. Neither obesity nor the presence of comorbidities in patients correlated to conversions.
Table 1.
Patient characteristics
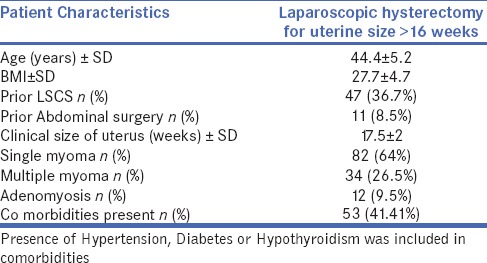
Table 2.
Surgical characteristics
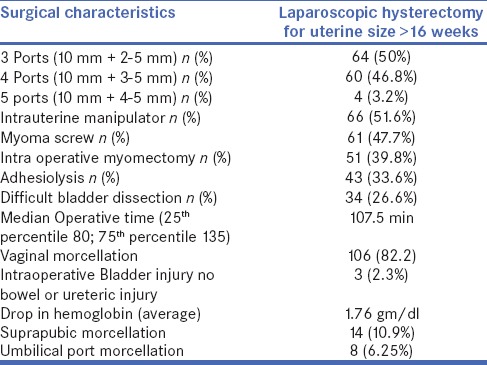
Table 3.
Multiple Logistic Regression analysis for Suprapubic Incision (conversion) during operation with various parameters
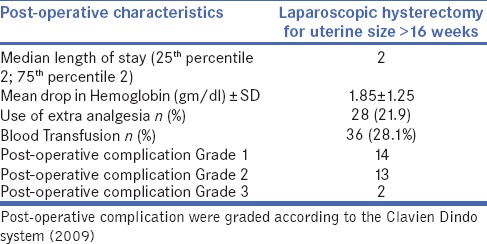
When we evaluated our data year wise, the need for conversion to laparotomy gradually decreased over the years. In fact, there are no conversions after the first 3 years (completion of 53 cases). According to this analysis, we propose that about 50 cases are needed as a learning curve to be able to complete hysterectomy in a minimally invasive way for large uterus. There was also decline in the number of intra-operative haemorrhage cases needing to resort to open surgery for salvage. In fact, there were no such cases after the first 2 years. The transfusions have remained roughly constant as this is not directly proportional to intra-operative bleeding and factors as mentioned above are also responsible [Figure 2]. Organ damage was considered as an intra-operative complication. There was only three cases of bladder injury and were managed intraoperatively. Post-operative complications were graded according to the Clavien–Dindo score [Table 4]. Fourteen cases were classified as Grade 1 complications of which 3 patients reported redness and sore umbilical wound, managed by dressing and local antibiotic ointments. In Grade 1 group, 5 patients developed paralytic ileus, managed conservatively. In Grade 1 group, six patients reported with pyrexia in the post-operative period who were then managed with antipyretics. These cases did not show any localised or generalised signs of infection; hence, no additional antibiotics were given. Three patients went home on catheter all of them were the ones with intra-operative bladder repair. Thirteen patients were classified as Grade 2 as they needed blood transfusion in the post-operative period. One case classified as Grade 3a as she needed embolisation due to haemorrhage in the post-operative period and an aberrant bleeding vessel at the vaginal vault was embolised in catheterization laboratory. Another patient underwent exploratory laparotomy under general anaesthesia, 6 h after surgery on suspicion of haemorrhage due to unstable vital signs. However, no active bleeding was encountered, and the case closed with peritoneal toilet, and she subsequently recovered well with conservative management. No unexpected malignant disease was discovered during the final histologic examination.
Figure 2.
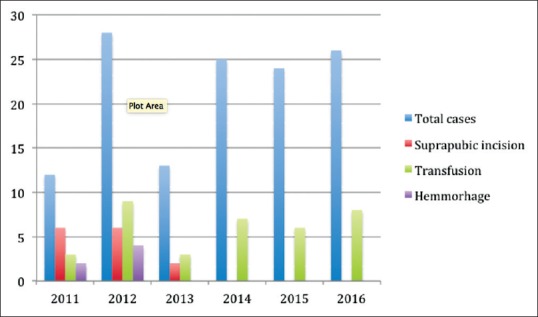
Depicts the number of cases, need for supra pubic incisions, haemorrhage and blood transfusions over 5 years
Table 4.
Post-operative characteristics
DISCUSSION
This is a case series of 128 cases undergoing minimally invasive hysterectomy for large volume uterus (>16 weeks clinical size) with a 10.9% conversion rate compared to 4.4% conversion reported by Uccella et al. in 2017.[8] Similar papers have been published earlier that discuss that laparoscopic hysterectomy in large uterine pathology is a safe and feasible option. Outcomes when compared to open method are better.[6,11,12] Since our unit also has access to Da Vinci Robotic platform, we included 5 cases that were done with robotic assistance, as outcomes are clinically comparable to laparoscopic hysterectomy.[13] In our series, the main indication is fibroid uterus. Large uteri are the challenging cases in benign gynaecology for the minimally invasive approach. Most centres resort to traditional open hysterectomy.[14] The two main technical challenges are the inability to complete the hysterectomy and to retrieve the specimen. While achieving the above two, the concern remains for haemorrhage and injury to organs around. While discussing our perioperative outcome, we also discuss our techniques to overcome these challenges. We observed that with each year our indications gradually expanded in attempting cases with large uteri. This tendency has also been documented in previous publications by Uccella et al.[3,12]
In our series, fourteen cases were converted to open surgery by making a suprapubic incision. There were roughly equal numbers for difficulty in completing the surgery and for uncontrolled haemorrhage. Six cases were converted due to intra-operative haemorrhage and 5 cases due to difficulty to reach all pedicles. All conversions were in the first 2 years of this study, which also indicates that with increased surgical experience improves the ability to complete hysterectomy in the minimally invasive way. The learning curve according to our study is about 50 cases. Altgassen et al., demonstrated the minimum number of operations before surgical complications of laparoscopic-assisted vaginal hysterectomy decreased to be 30 cases, however, they included all sizes of the uterus and not only enlarged ones.[15] Ou et al., in their multicentre study, demonstrated lack of correlation between surgeon experience and operative time.[16] This could be because the more experienced the surgeon becomes, the more complicated cases s/he attempts to perform therefore, the operative time did not change markedly. The other reasons for conversion in our series were extensive adhesions (1 case) and bladder injury (2 cases). A population-based data in Germany estimated 10% of laparoscopic hysterectomies and 1% of vaginal hysterectomies necessitated a conversion to an abdominal hysterectomy.[17] Laparoscopic surgery has some limitations when approaching bulky masses, especially if it is in the lower segment or extending into broad ligament. They tend to fill the pelvis causing difficulty in visualising the anatomic structures like ureters. It may cause difficulty in gaining access to anatomic planes risking haemorrhage or organ injury. Over the years, we developed some techniques to help us achieve this.
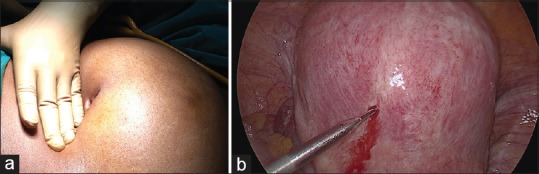
The first technique we evolved during the study period was to do intra-operative myomectomy [Figure 3a] and then proceed with hysterectomy. This was preceded by injecting diluted vasopressin (20 units in 100 ml saline) into the uterus before staring the hysterectomy. This was the key to reducing haemorrhage. Myomectomy was done if there was a large myoma anteriorly or in lower segment obscuring the vesicouterine reflection making the bladder dissection difficult or in cases with large broad ligament fibroid in attempt to make the anatomy normal before hysterectomy. The second technique was to use a 30° 10 mm telescope skilfully by the assistant [Figure 3b]. Hence by rotating the endoscopic light cable to required side by the assistant brings the area of surgical intervention in close up view. This helps the surgeon to execute the surgical steps with ease and confidence. The third technique was to effectively manipulate the uterus with the help of a uterine manipulator by an assistant sitting in between the legs. Uterus that are very large and heavy, we used myoma screw through one of the 5 mm ancillary ports to apply upward traction mimicking what is done during open hysterectomy [Figure 3c]. Van den Haak et al. also found uterine manipulator extremely useful because it aids very efficiently in mobilisation and exposure. When cranial traction is given to the uterus and the distance between the cervix and the ureters increases, allowing (at least in theory) a safer dissection and a potentially lower risk of ureteric injuries.[18] The fourth technique is to not use a colpotomiser. We open the posterior fornix in most cases. If the fornix in not clear an assistant highlights it by a swab held with artery forceps. The vault is opened using harmonic scalpel [Figure 3d], and once the vaginal canal identified, the cervix is cut from the vaginal vault, again mimicking the open hysterectomy method. The fifth technique was to keep the port placements simple and use minimal instruments [Figure 3e]. Most cases had primary port was at umbilicus as the uterine enlargement is in cranial direction and umbilicus port gives adequate exposure to all pedicles. We typically use only six hand instruments-plain and tooth grapers, myoma screw, harmonic scalpel, bipolar fenestrated forceps and suction and irrigation cannula. We use a combination of bipolar and harmonic for desiccation and transection of all pedicles. This helps the assisting team to remain in control as well as the scrub nurse to pass instruments effectively. Some authors suggest the use of supraumbilical ports or additional trocars in cases of giant uteri.[19] The sixth technique was effective specimen retrieval. The specimen was morcellated with scalpel using number 11 blade after bringing the uterus into the vagina. In cases of the very narrow vagina, the specimen was brought out through the umbilical port incision and morcellated with scalpel. A cold-scalpel and paper roll method were used for tissue extraction.[20] The concept was to convert a globular specimen into a longitudinal one by making repeated lateral incisions [Figure 3f]. In some cases where there was some doubt about the pathology, the uterus was placed inside an endobag and then morcellated inside the bag in the vagina.
Figure 3.
(a) Intra-operative myomectomy being performed before hysterectomy in a case with large right lower uterine myoma extending into broad ligament. (b) 30° degree, 10 mm telescope camera skilfully rotated to visualize the left uterine artery from the left lateral aspect. (c) Myoma screw being used for manipulation and cranial traction during laparoscopic hysterectomy. (d) Vaginal vault opened posteriorly without any colpotomiser. This is then extended both sides to severe cervix from vault. (e) Port placement; 10 mm primary port at upper border of umbilicus, two 5 mm ports on the left side and one 5 mm port on the right side of abdomen. (f) Morcellated specimen depicting the technique to convert a globular specimen to longitudinal one
The limitation of the study is in its retrospective nature. The main strength of the present study is to show that limitations of laparoscopic hysterectomy in cases of extremely large uteri can be overcome with learning curve experience.
CONCLUSION
Developing a team and discussing the steps and planning the surgery beforehand helps in smooth intra-operative execution of surgical steps. Along with this dedication, patience and persistence helps to endoscopically manage this kind of situation. Our team has developed these techniques and are now able to complete hysterectomy for large uteri safely and effectively. This study is testimony of this fact. Learning curve in our series is about 50 cases for hysterectomy for enlarged uterus (>16 weeks). In referral centres with high volume endoscopic experience, laparoscopic hysterectomy is a safe and feasible alternative to open surgery, even in case of large uteri. This technique is beneficial in terms of lower complications, shorter hospital stay with an acceptable conversion rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pandey D, Sehgal K, Saxena A, Hebbar S, Nambiar J, Bhat RG, et al. An audit of indications, complications, and justification of hysterectomies at a teaching hospital in India. Int J Reprod Med 2014. 2014 doi: 10.1155/2014/279273. 279273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mukhopadhaya N, Manyonda IT. The hysterectomy story in the United Kingdom. J Midlife Health. 2013;4:40–1. doi: 10.4103/0976-7800.109635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uccella S, Cromi A, Bogani G, Casarin J, Formenti G, Ghezzi F, et al. Systematic implementation of laparoscopic hysterectomy independent of uterus size: Clinical effect. J Minim Invasive Gynecol. 2013;20:505–16. doi: 10.1016/j.jmig.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Walid MS, Heaton RL. Total laparoscopic hysterectomy for uteri over one kilogram. JSLS. 2010;14:178–82. doi: 10.4293/108680810X12785289143837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rolla M, Gagliardi ML, Giacomantonio L, Cecaroni M, Bruni F, Minelli L, et al. Total laparoscopic hysterectomy of an uterus of 1840 grams: A case report. Acta Biomed. 2009;80:282–5. [PubMed] [Google Scholar]
- 6.Kondo W, Bourdel N, Marengo F, Botchorishvili R, Pouly JL, Jardon K, et al. Is laparoscopic hysterectomy feasible for uteri larger than 1000 g? Eur J Obstet Gynecol Reprod Biol. 2011;158:76–81. doi: 10.1016/j.ejogrb.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 7.Kluivers KB, Hendriks JC, Mol BW, Bongers MY, Bremer GL, de Vet HC, et al. Quality of life and surgical outcome after total laparoscopic hysterectomy versus total abdominal hysterectomy for benign disease: A randomized, controlled trial. J Minim Invasive Gynecol. 2007;14:145–52. doi: 10.1016/j.jmig.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Uccella S, Morosi C, Marconi N, Arrigo A, Gisone B, Casarin J, et al. Laparoscopic versus open hysterectomy for benign disease in uteri weighing >1kg: A retrospective analysis on 258 patients. J Minim Invasive Gynecol. 2018;25:62–9. doi: 10.1016/j.jmig.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Harb TS, Adam RA. Predicting uterine weight before hysterectomy: Ultrasound measurements versus clinical assessment. Am J Obstet Gynecol. 2005;193:2122–5. doi: 10.1016/j.ajog.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 11.Uccella S, Cromi A, Serati M, Casarin J, Sturla D, Ghezzi F, et al. Laparoscopic hysterectomy in case of uteri weighing ≥1 kilogram: A series of 71 cases and review of the literature. J Minim Invasive Gynecol. 2014;21:460–5. doi: 10.1016/j.jmig.2013.08.706. [DOI] [PubMed] [Google Scholar]
- 12.Uccella S, Casarin J, Marconi N, Cromi A, Morosi C, Gisone B, et al. Laparoscopic versus open hysterectomy for benign disease in women with giant uteri (≥1500 g): Feasibility and outcomes. J Minim Invasive Gynecol. 2016;23:922–7. doi: 10.1016/j.jmig.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, et al. Robotically assisted vs.laparoscopic hysterectomy among women with benign gynecologic disease. JAMA. 2013;309:689–98. doi: 10.1001/jama.2013.186. [DOI] [PubMed] [Google Scholar]
- 14.Loring M, Morris SN, Isaacson KB. Minimally invasive specialists and rates of laparoscopic hysterectomy. JSLS. 2015;19:e2014.00221. doi: 10.4293/JSLS.2014.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004;104:308–13. doi: 10.1097/01.AOG.0000132806.46344.05. [DOI] [PubMed] [Google Scholar]
- 16.Ou CS, Beadle E, Presthus J, Smith M. A multicenter review of 839 laparoscopic-assisted vaginal hysterectomies. J Am Assoc Gynecol Laparosc. 1994;1:417–22. doi: 10.1016/s1074-3804(05)80811-4. [DOI] [PubMed] [Google Scholar]
- 17.Stang A, Merrill RM, Kuss O. Nationwide rates of conversion from laparoscopic or vaginal hysterectomy to open abdominal hysterectomy in Germany. Eur J Epidemiol. 2011;26:125–33. doi: 10.1007/s10654-010-9543-4. [DOI] [PubMed] [Google Scholar]
- 18.van den Haak L, Alleblas C, Nieboer TE, Rhemrev JP, Jansen FW. Efficacy and safety of uterine manipulators in laparoscopic surgery: A review. Arch Gynecol Obstet. 2015;292:1003–11. doi: 10.1007/s00404-015-3727-9. [DOI] [PubMed] [Google Scholar]
- 19.Ceccaroni M, Roviglione G, Pesci A, Quintana S, Bruni F, Clarizia R, et al. Total laparoscopic hysterectomy of very enlarged uterus (3030 g): Case report and review of the literature. Wideochir Inne Tech Maloinwazyjne. 2014;9:302–7. doi: 10.5114/wiitm.2014.43026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong WS, Lee TC, Lim CE. Novel vaginal “paper roll” uterine morcellation technique for removal of large (>500 g) uterus. J Minim Invasive Gynecol. 2010;17:374–8. doi: 10.1016/j.jmig.2010.02.005. [DOI] [PubMed] [Google Scholar]