Abstract
Introduction:
In India, significant number of individuals suffers from ischemic heart disease (IHD). Majority of chest pain victim initially report to his family physician. At times, sudden death is the first and last manifestation of IHD. Doctors are aware of various risk factors for IHD. The diagonal ear lobe crease (DELC) has been characterized in medical literature as a surrogate marker which can be easily identified as high-risk case for impending IHD. We report here the incidence of IHD accompanied with DELC in rural population.
Patients and Methods:
Eight hindered and eighty eight patients attended to general physician Mahad during January 2012 to December 2015 with complaints of chest pain were investigated for presence of DELC. Presence of DELC was correlated to varies risk factors including hypertension, hyperlipidemia, diabetes mellitus (DM), body mass index (BMI), occipital baldness, and tobacco consumption.
Results:
Out of patients studied, 645 (72.6%) had hypertension, 508 (57.2%) had DELC, of these 486 (95%) suffered from IHD, 246 (48%) had DM, 246 (48%) had occipital baldness, and 325 (64%) had hyperlipidemia. Significant association between BMI > 25+ in male >50 years old with odd ratio 2.08 (95% CI: 1.27–3.39; P = 0.003).
Interpretation:
Presence of DELC with or without risk factors is a simple clinical observation easily noted during examination by family physician to investigate and to rule out IHD.
Keywords: Ear crease, hyperlipidemia, ischemic heart disease
Introduction
Still in rural setting, family physicians exist. Majority of villagers irrespective of severity illness first visits to their family physician. Because of improvement in literacy, villagers are health conscious. Acute infectious diseases like diarrhea, bacillary dysentery, cholera, chicken pox, measles scabies, and worm infestations are on the way of vanishing. These diseases are replaced by noncommunicable diseases (NCDS) like hypertension, ischemic heart diseases (IHDs), diabetes, and mental illness. General physicians are now aware of NCDS. The prevalence of coronary heart disease has progressively increasing from 10.4% to 13.1% during last decade in developing country like India.[1,2] Pre-hospital sudden death preceded by chest pain has led to a search of risk factors responsible for coronary heart disease (IHD). More than 200 risk markers of IHD have been identified. Major factors are hypertension, diabetes mellitus (DM), hyperlipidemia, hyper-homocysteinemia, tobacco consumption in the form of smoking or tobacco chewing, obesity, sedentary stressful life, male sex, and familial history of premature IHD or sudden death. Frank in 1973 first time observed that the diagonal ear crease (DELC) associated with premature IHD.[3] Lichtenstein et al. in 1974[3] reported that 47% had diagonal ear crease associated with myocardial infarction. Prevalence of ear crease often reported in the sixth to ninth decades of life.[4] Presence of bilateral ear lobe crease often accompanied by vascular dysfunction[5] Postmortem study confirmed the significant positive correlation between the presence of ear lobe crease and coronary heart diseases. Similarly, risk of cardiovascular death were 1.55–1.74 times greater than those without crease.[6] Male pattern baldness, diagonal ear lobe crease, and xanthoma alone or combination accompanied with increased risk of IHD and acute myocardial infarction.[7] DELC is independent or accompanied with ischemic stroke in addition to IHD.[8] DELC can be easily seen while examining ear, nose, throat to rule out malignancy, IHD and carotid artery disease.[9] Patients with classical IHD accompanied with risk factors had DELC at a higher frequency.[10] In a busy outpatient department, clinical detection of earlobe crease may facilitate early diagnosis in patients at high risk for IHD[11] We report that ear lobe crease is a premonitory sign of impending IHD, accompanied with hypertension, DM, hyperelipidemia, smoking, raised body mass index (BMI), and occipital baldness at peripheral hospital.
Patients and Methods
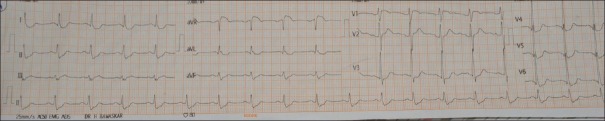
Patients with the complain of chest pain at outpatient department from January 2012 to December 2015 were studied in detail and investigated to rule out angina pectoris, acute myocardial infarction, hypertension, DM, raised lipid levels, smokers, tobacco chewers, and occipital baldness. All the patients examined for presence of diagonal ear lobe crease (DELC) and investigated for BMI, height, electrocardiography changes, and coronary angiography. DELC is characterized by a deep, obliquely diagonal earlobe creases run from lower pole of the external meatus, diagonally backward to the edge of the lobe at approximately 45° [Figure 1 and Table 1],[3] premature arcus senilis and cataract [Figure 2].
Figure 1.
Diagonal ear lobe crease seen in 53 years old male suffered of unstable angina pectoris
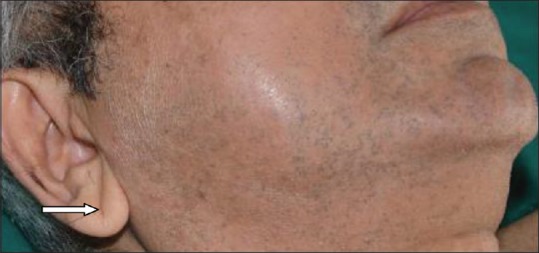
Table 1.
Shows basic socio-demographic characteristics of study subjects
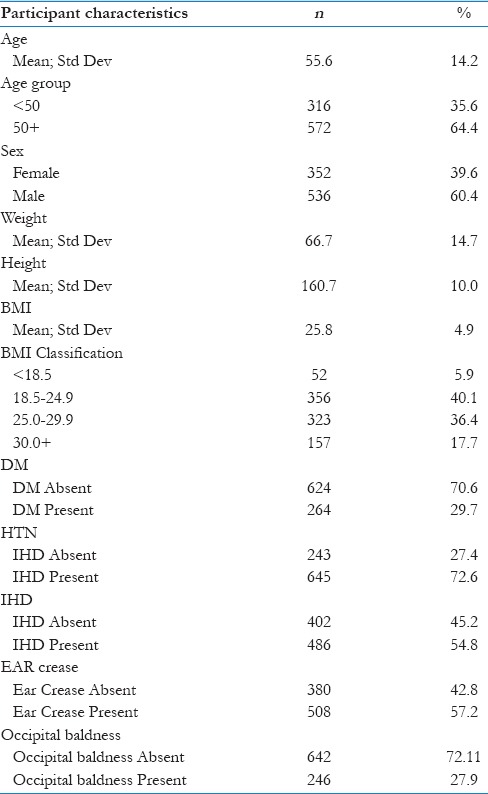
Figure 2.

Bilateral premature arcus senilis seen in patient described in fig 1
Hypertension
Blood pressure Measured by mercury sphygmomanometer >140/90 mm hg included in hypertension group.[12]
Ischemic heart diseases
Classic manifestation of IHD is angina which is characterized by heaviness in the chest, squeezing or a burning feeling, or suffocation or difficult in breathing. Chest pain or discomfort radiated to left shoulder, neck, jaw, epigastrium, or inner side of left arm or at times both arms. Chest pain intensity is built up over period of minutes (less than 2–10 minutes). Pain may start with exercise or psychological stress and strain or cold weather. Unstable angina is characterized by severe intolerable chest pain at rest. Acute myocardial infarction is characterized by sudden onset of retro-sternal severe agonizing chest pain lasting for >30 minutes or longer, pain referred to both shoulder and arms, associated with shortness of breath, profuse sweating, weakness, nausea, and vomiting or shock.[13] Electrocardiograms (ECG).-Angina-resting ECG may be normal. During chest pain, ST-T changes suggestive IHD or positive stress test further evaluated by coronary angiography.
Acute myocardial infarction
Patients presenting with ischemic symptoms and typical ST – segment elevation measured at the “J” point. ST segment elevation should be found in two contiguous leads and ≤0.25 mV in men below the age of 40 years and ≥0.2 mV in men over the age of 40 years or ≥0.15 mV in women in leads V2-V3 or ≥0.01 mV in other leads without left ventricular hypertrophy or LBBB and new LBBB and appearance of new pathological “Q” waves. Acute inferior wall infarction accompanied with ST elevation in right precordial chest leads suggestive of right ventricular Infarction and reciprocal changes in lead V1-V3. The terminal T-wave is positive (ST elevation equivalent) and may be confirmed by concomitant ST elevation in lead V7-V9. ST elevation in AVR [Figure 3] and inferior lateral ST depression indicates left main coronary obstruction.[14]
Figure 3.
ST segment 3 MM elevated in AVR, 3MM ST segment depression in lead I, AVL, V4toV6, left anterior hemiblock with right bundle branch block, patient of unstable angina pectoris
DM – Fasting blood sugar: 126 mg/dL or ≥7.0 mmol/L (normal 100 mg/dL or <5.6 mmol/L, HbA1c <5.6%); 2 hours of postglucose (1 g/kg glucose): 200 mg/dL or 11.1 mmol (normal 140 mg/dL or <7.8 mmol, Hba1c > 6.5%).
Lipids-Optimal total cholesterol level <200 mg/dl (5.2 mmol/L) and LDL-C <115 mg/dl (3mmol/L); above this is hyperlipidemia.[15]
Smoker – One pack of cigarettes or bidis (tobacco packed in a rolled leaves) per day for period between 1 month and 20 years.
Crown top baldness or occipital with or without fronto-parietal male pattern baldness. BMI is calculated by weight in kg/m2.
About 177 patients undergone coronary angiography; of these, 22 had normal coronaries with no DELC.
About 155 (87.57%) cases with DELC showed lesion in one vessel, 24 (15.49%); two vessels, 79 (50.96%); and three vessels, 52 (33.54%). About 10 (6.45%) patients had acute myocardial infarction, 7 (4.51%) had old myocardial infarction, 5 (3.22%) undergone CABG, and 23 (14.83%) undergone angioplasty. Remaining could not afford the invasive treatment and were put on medical line of treatment.
Results
Out of 888 patients studied, 645 (72.6%) had hypertension, 508 (57.2%) had DELC, of these, 486 (95%) suffered from IHD, 264 (52%) had DM, 508 had raised blood pressure, occipital baldness were present in 246 (48%), and hyperlipidemia in 325 (64%). In males, aged ≥50 years, DELC is significant with odds ratio 7.49 (95%CI: 3.97–14.1, P < 0.001). Significant association between DELC and BMI ≥25 in male >50-year old with odds ratio 2.08 (95% CI: 1.27–3.39, P = 0.003).
Interpretations – Presence of DELC with or without hypertension, hyperlipidemia, smoking, overweight, occipital baldness, and DM is a diagnostic sign of impending IHD.
Statistical analysis
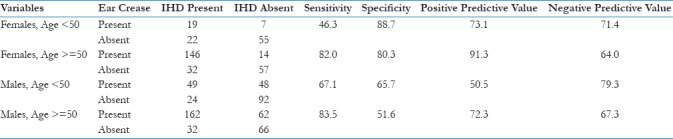
All statistical analysis was done by using Epi-Info 7 software [Tables 2 and 3]. Descriptive analysis was done by using counts and percentages. Numerical variables were summarized using mean and standard deviation and were also converted into appropriate categories and then summarized as counts and percentages. Association of ear crease with all variables was tested by using Chi-square test and odds ratios with 95% confidence intervals. Similarly association of IHD with all variables was tested using Chi-square test and odds ratios with 95% confidence intervals. Age (>50 years) and gender (males) are known independent risk factors; therefore, we have performed all analyses in four subgroups, that is, age <50 years: males, females and age >50 years: males, females. Logistic regression analysis was used, wherein IHD was entered as outcome, and presence of ear crease, smoking, hyperlipidemia, BMI >25, hypertension, DM, occipital baldness, and height >160 cm were entered as independent factors depending on their P value in univariate analysis. For all analyses, P < 0.05 was considered as statistically significant.
Table 2.
Shows univariate analysis for association of ear crease with other variables
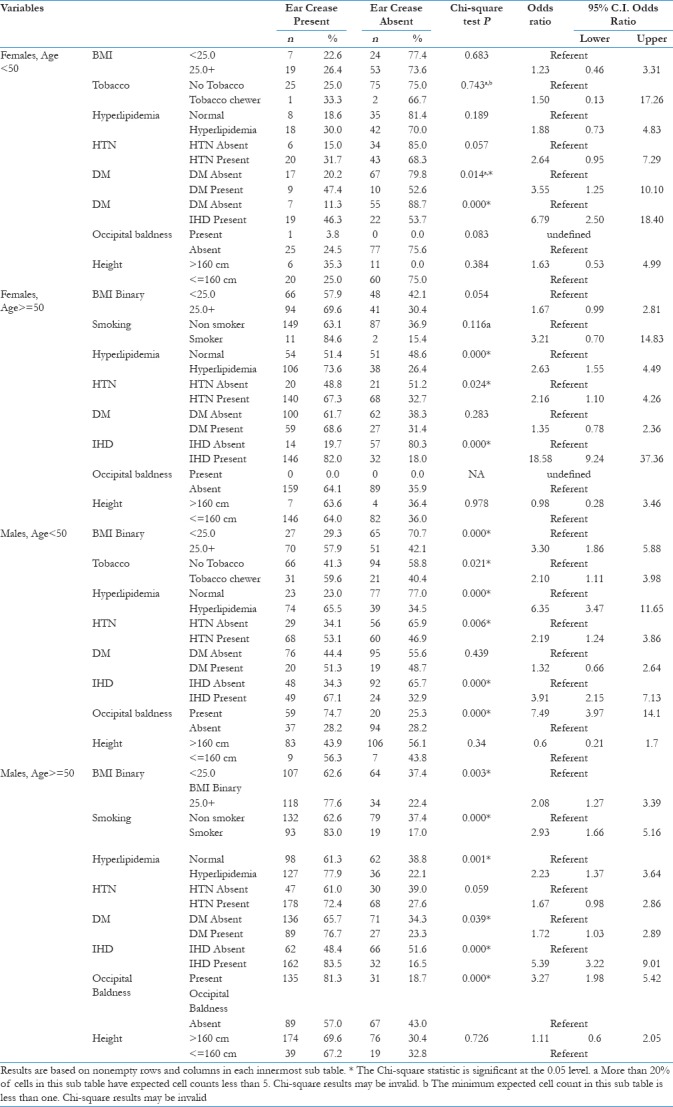
Table 3.
Shows diagnostic test parameters for presence of ear crease as test for IHD
Presence of DELC along with risk factors such as hypertension, hyperlipidemia, smoking, occipital baldness, and DM is a diagnostic and significant clinical sign of IHD.
Discussion
This is the first prospective study of DELC in 888 patients studied at peripheral hospital at Mahad. DELC a premonitory skin marker of IHD accompanied with risk factors such as hypertension, smoking, tobacco consumption, hyperlipidemia, DM, BMI and crown top or occipital baldness in Indian population. Our findings confirmed that the presence of DELC is indicative of undermined or impending IHD.[8,11,16,17]
DELC characterized by crease run from lower pole of the external meatus, diagonally backward to the edge of the lobe at approximately 45° [Figure 1]. DELC and coronary artery sclerosis arose simultaneously because the ear lobe and heart are supplied by “end arteries” without possibility of collateral circulation. DELC may reflect skin aging that parallels the aging changes in coronary arteries.[18] Study of Japanese male patients having DELC and multiple metabolic risk factors for coronary artery disease demonstrated shortened telomeres.[19,20] Early atherosclerosis results in smooth muscles’ hypertrophy and proliferation with contraction band ear crease.[21] The hair follicles are target for androgens and androgen receptors are significantly higher in dermal papilla cells from balding scalp compared with nonbalding scalp follicles.[7] This and other observations showed that free testosterone acts on both the hair and the vessel wall, resulting in both male pattern baldness and proliferation of smooth muscle cells and atherosclerosis. Loci on chromosome 7 and 20 associated with male pattern baldness and cardiovascular disease in males. Possible explanation for increased risk of IHD associated with presence of ear lobe crease due to altered characteristics of the connective tissue in men and postmenopausal women reflected both in the dermis and arterial intima [Table 2].[7]
In this study, out of 277 patients undergone coronary angiography; of these, 155 (87%) had significant coronary artery stenosis and are more significance in Indian population as compared with 64.30% reported from Finland.[22] In rural Indian population, significant correlation of DELC with DM, IHD, and tobacco chewing seen in females. In males, hyperlipidemia, IHD, and crown top baldness are accompanied with DELC [Tables 2 and 3].
Presence of DELC is most sensitive and significant external marker for IHD. We noted that there is significant association between DELC and IHDs in females ≥50- year old with odds ratio 18.54, and in males >50 IHD with odds ratio 5.39, whereas <50 DELC accompanied with IHD, odd ratio 3.79, hyperlipidemia 6.35, and occipital baldness 7.49.[18] Significant association between DELC and BMI ≥25 in males >50-year old with odds ratio 2.08 (95% CI: 1.27–3.39, P = 0.003). In this study, we reported 57% patients had DELC as compared with 47% patients studied at New York urban population.[8] Main finding of this study is that there was significant association between DELC and IHD, hypertension, DM, hyperlipidemia, tobacco consumption (smoking and tobacco chewer), and occipital baldness [Figures 1-5], similar to Chinese patients.[23] In terms of gender, our result showed that DELC is more common in female associated with IHD hyperlipidemia, DM, than males except occipital baldness. Genetic association between C-3-F Gene, DELC and essential hypertension with atherosclerosis reported from Demark study.[24] Hou et al. from China in a small study reported that DELC is an independent risk factor or early sign of atherosclerosis.[25] In this study, 10 patient had acute myocardial infarction, and 7 with old myocardial infarction, which confirmed that patients with DELC more likely to have cardiac events than those without. About 87% of cases with DELC undergone coronary angiography and had lesion in coronaries as compared with 12.42% with without DELC having normal coronaries. Similarly, almost 11,000 Danish participants were closely studied and were followed to 35 years. The study found that DELC was significantly associated with an increased risk of developing clinically significant heart diseases including acute myocardial infarction.[7] The association remained, even when accounting for the effects of the risk factors suggesting that DELC was independently associated with heart disease.
Figure 5.
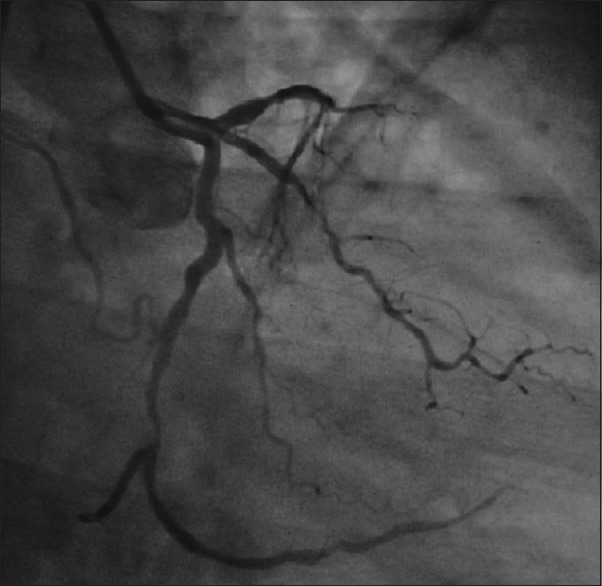
Extensive diffuse atherosclerotic lesion in left circumflex and anterior descending coronary patient of unstable angina pectoris
Figure 4.

Extensive diffuse atherosclerotic lesion in right coronary of patient of unstable angina pectoris
In this study, the sensitivity of DELC and IHD varied from 46 to 83.5 and specificity from 51 to 81.7 in relation to different age and sex [Table 3]; our findings are comparable with the report of Rodríguez-López et al.[8] Roman emperor Hardian died of heart disease due to hypertension and coronary atherosclerosis supported by the identification of bilateral ear lobe creases on sculptures.[8] Similar observation of correlation of DELC with diabetic retinopathy was noted in Indian urban population. Presence of DELC with vertex baldness or occipital or crown top baldness associated with increased risk of IHD. Males aged 50 years are significant with odds ratio 7.49 (95% CI: 3.97–14.1, P < 0.001), whereas males aged ≥50 are significant with odds ratio 3.27 (95% CI: 1.1.98–5.42, P < 0.001). In this study, we noted significant comparable association between DELC and IHD [Tables 2 and 3]. There is a strong genetic predisposition to occipital baldness-related high circulating androgen. Size of coronaries depends upon height of individual. Nelson et al. from UK reported that person with height >180 cm is less likely suffered of premature coronary heart disease.[26] Indian population with low height accompanied with small size coronaries is more prone for obstruction with a size of plaque seen in UK population with height 180 ± 8 cm.[23] In this study, we noted that male with mean height 166.4 and female with mean height 151.1 are more prone for coronary artery disease with DELC.
In developing country like in India, 70%–80% population stays at rural setting with no laboratory investigations and no specialists are available. In such situation, health workers and peripheral doctors can be trained. Regarding presence of the DELC, a clinical marker can be easily noted by nonclinician or health workers may be used to identify person with high risk of IHD accompanied with risk factors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are grateful to DR Abhijit P Pakhare department of community and family medicine, AIIMS Bhopal, Madhya Pradesh For statistical analysis.
References
- 1.Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–10. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ke C, Gupta R, Xavier D, Prabhakaran D, Mathur P, Kalkonde YV, et al. Divergent trends in ischaemic heart disease and stroke mortality in India from 2000 to 2015: A nationally representative mortality study. Lancet Glob Health. 2018;6:e914–23. doi: 10.1016/S2214-109X(18)30242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank ST. Aural sign of coronary-artery disease. N Engl J Med. 1973;289:327–8. doi: 10.1056/nejm197308092890622. [DOI] [PubMed] [Google Scholar]
- 4.Lichstein E, Chadda KD, Naik D, Gupta PK. Diagonal ear-lobe crease: Prevalence and implications as a coronary risk factor. N Engl J Med. 1974;290:615–6. doi: 10.1056/NEJM197403142901109. [DOI] [PubMed] [Google Scholar]
- 5.Oda N, Maruhashi T, Kishimoto S, Kajikawa M, Iwamoto Y, Iwamoto A, et al. Relation of the bilateral earlobe crease to endothelial dysfunction. Am J Cardiol. 2017;119:1983–8. doi: 10.1016/j.amjcard.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 6.Cumberland GD, Riddick L, Vinson R. Earlobe creases and coronary atherosclerosis. The view from forensic pathology. Am J Forensic Med Pathol. 1987;8:9–11. doi: 10.1097/00000433-198703000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Christoffersen M, Frikke-Schmidt R, Schnohr P, Jensen GB, Nordestgaard BG, Tybjærg-Hansen A, et al. Visible age-related signs and risk of ischemic heart disease in the general population: A prospective cohort study. Circulation. 2014;129:990–8. doi: 10.1161/CIRCULATIONAHA.113.001696. [DOI] [PubMed] [Google Scholar]
- 8.Rodríguez-López C, Garlito-Díaz H, Madroñero-Mariscal R, Sánchez-Cervilla PJ, Graciani A, López-Sendón JL, et al. Earlobe crease shapes and cardiovascular events. Am J Cardiol. 2015;116:286–93. doi: 10.1016/j.amjcard.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 9.Friedlander AH, López-López J, Velasco-Ortega E. Diagonal ear lobe crease and atherosclerosis: A review of the medical literature and dental implications. Med Oral Patol Oral Cir Bucal. 2012;17:e153–9. doi: 10.4317/medoral.17390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazzal S, Hijazi B, Khalila L, Blum A. Diagonal earlobe crease (Frank's sign): A Predictor of cerebral vascular events. Am J Med. 2017;130:1324.e1–5. doi: 10.1016/j.amjmed.2017.03.059. [DOI] [PubMed] [Google Scholar]
- 11.Qamar A, Ioannides KL, Khetarpal SA, Kiss D. Bilateral earlobe creases and coronary artery disease. Circulation. 2014;130:92–3. doi: 10.1161/CIRCULATIONAHA.114.009738. [DOI] [PubMed] [Google Scholar]
- 12.Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;386:801–12. doi: 10.1016/S0140-6736(14)61468-9. [DOI] [PubMed] [Google Scholar]
- 13.Cannon CP, Lee TH. Approach to the patient with chest pain. In: Libby P, Bonow RO, Mann DL, Zipes DP, editors. Braunwald's Heart Disease: A Text Book of Cardiovascular Medicine. 8th ed. Ch. 49. Philadelphia: Saunders; 2008. pp. 1195–205. [Google Scholar]
- 14.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389:197–210. doi: 10.1016/S0140-6736(16)30677-8. [DOI] [PubMed] [Google Scholar]
- 15.Cholesterol Treatment Trialists’ (CTT) Collaboration. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aligisakis M, Marques-Vidal P, Guessous I, Vollenweider P. Did Dumbo suffer a heart attack. Independent association between earlobe crease and cardiovascular disease? BMC Cardiovasc Disord. 2016;16:17. doi: 10.1186/s12872-016-0193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christiansen JS, Mathiesen B, Andersen AR, Calberg H. Letter: Diagonal ear-lobe crease in coronary heart disease. N Engl J Med. 1975;293:308–9. doi: 10.1056/NEJM197508072930626. [DOI] [PubMed] [Google Scholar]
- 18.Bouissou H, Pieraggi MT, Julian M, Pendaries I, Seguier J, Salvador M, et al. Value of skin biopsy in coronary insufficiency. Arch Mal Coeur Vaiss. 1973;66:655–60. [PubMed] [Google Scholar]
- 19.Standring S, editor. Grays Anatomy. 39th ed. Ch. 38. Philadelphia: Elsevier Churchill Livingstone; 2006. External and middle ear; p. 649. [Google Scholar]
- 20.Higuchi Y, Maeda T, Guan JZ, Oyama J, Sugano M, Makino N, et al. Diagonal earlobe crease are associated with shorter telomere in male Japanese patients with metabolic syndrome. Circ J. 2009;73:274–9. doi: 10.1253/circj.cj-08-0267. [DOI] [PubMed] [Google Scholar]
- 21.Kaukola S, Manninen V, Valle M, Halonen PI. Ear-lobe crease and coronary atherosclerosis. Lancet. 1979;2:1377. doi: 10.1016/s0140-6736(79)92868-x. [DOI] [PubMed] [Google Scholar]
- 22.Rhoads GG, Klein K, Yano K, Preston H. The earlobe crease – Sign of obesity in middle-aged Japanese men. Hawaii Med J. 1977;36:74–7. [PubMed] [Google Scholar]
- 23.Wu XL, Yang DY, Zhao YS, Chai WH, Jin ML. Diagonal earlobe crease and coronary artery disease in a Chinese population. BMC Cardiovasc Disord. 2014;14:43. doi: 10.1186/1471-2261-14-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyboe J, Jensen G, Appleyard M, Schnohr P. Risk factors for acute myocardial infarction in copenhagen. I: Hereditary, educational and socioeconomic factors. Copenhagen city heart study. Eur Heart J. 1989;10:910–6. doi: 10.1093/oxfordjournals.eurheartj.a059401. [DOI] [PubMed] [Google Scholar]
- 25.Hou X, Jiang Y, Wang N, Shen Y, Wang X, Zhong Y, et al. The combined effect of ear lobe crease and conventional risk factor in the diagnosis of angiographically diagnosed coronary artery disease and the short-term prognosis in patients who underwent coronary stents. Medicine (Baltimore) 2015;94:e815. doi: 10.1097/MD.0000000000000815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nelson CP, Hamby SE, Saleheen D, Hopewell JC, Zeng L, Assimes TL, et al. Genetically determined height and coronary artery disease. N Engl J Med. 2015;372:1608–18. doi: 10.1056/NEJMoa1404881. [DOI] [PMC free article] [PubMed] [Google Scholar]