Abstract
Introduction:
In India, intestinal parasitic infection and anemia remain the most important cause of morbidity especially among the adolescent school children due to lack of awareness of personal hygiene practices, leading to intestinal parasite infections which could in turn lead to anemia.
Aim:
This study was conducted with the aim to find out the prevalence of intestinal parasitic infection and anemia among adolescent female school children in an urban area of Tamil Nadu.
Materials and Method:
This descriptive cross-sectional study was done among adolescent female school children in Anakaputhur area of Kancheepuram district. Three schools were selected randomly from a total of eight schools in the study area. Universal sampling was applied in each school, and a total of 250 willing children participated in the study. Early morning stool specimen was collected for microscopic examination and hemoglobin estimation was done. A pretested structured questionnaire was used to collect relevant data which were analyzed using SPSS version 22.
Results:
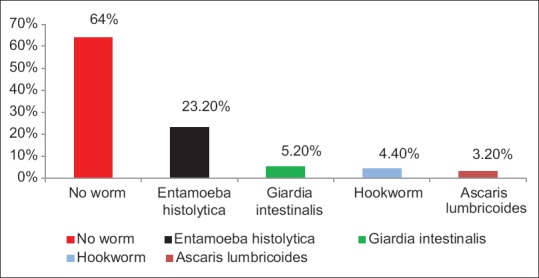
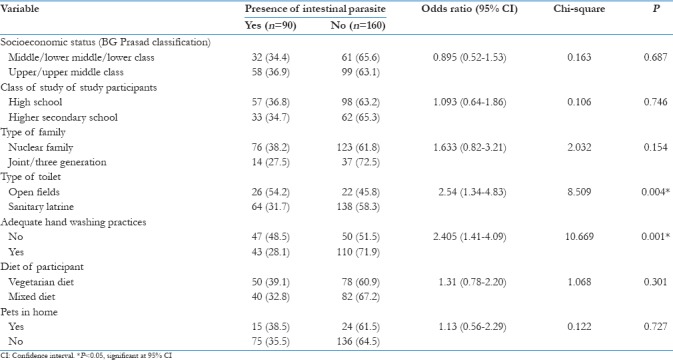
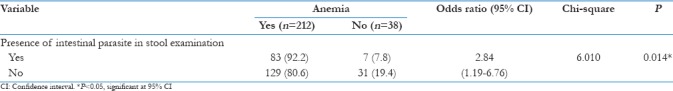
The prevalence of intestinal parasitic infection was found to be 36% with Entamoeba histolytica being the commonly isolated organism (23.2%) followed by Giardia intestinalis (5.2%), Hookworm (4.4%), and Ascaris lumbricoides (3.2%). The prevalence of anemia among them was found to be 84.8% with mild, moderate, and severe anemia being 12.8%, 46.8%, and 25.2%, respectively. Statistically significant association was found between intestinal parasitic infection and open field defecation, inadequate hand washing practices, and anemia.
Conclusion:
The study reveals high prevalence of anemia and intestinal parasitic infection among female school children. Preventive measures such as periodic deworming and health education about nutritional balanced diet, iron supplements, and personal hygiene practices have to be given to both the parents and their children to prevent and reduce disease burden.
Keywords: Adolescents, helminths, hemoglobin, hygiene, protozoa
Introduction
India, being one of the developing tropical countries with increasing population, continuous urbanization, ethnic food habits, and poor socioeconomic conditions, has paved way for the emergence of previously unrecognized diseases and food-borne parasitic infections.[1] This has, in turn, led to nutritional problems such as anemia in those affected, increasing their morbidity.
Parasitic diseases have been with mankind since time immemorial. Even today, these diseases remain among the major causes of human misery and death in the world and are important obstacles to the development of economically less developed countries.[2] Helminthiasis and other parasitic infections in India contribute to nearly 40% of the global burden of tropical diseases.[3] These parasites live in the intestine of affected persons and lay thousands of eggs, which get passed through the faces. In areas of inadequate sanitation and with open-air defecation practices, it could contaminate the soil and could get transmitted to children when they play in that area and when they do not follow adequate personal hygiene practices.[4]
In developing countries, the most common parasitic infections are those caused by helminths and protozoan parasites, which are listed in Table 1.
Table 1.
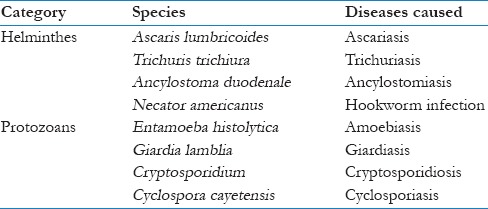
The diseases caused by helminthic parasites are collectively called helminthiasis, and it impairs the nutritional status of those affected by causing intestinal bleeding, loss of appetite, diarrhea, and reducing the absorption of micronutrients. These infections are highly prevalent in the tropical and subtropical regions where there is lack of adequate water supply and proper sanitation facilities.[4,5] The diseases caused by the intestinal protozoan parasites are associated with diarrhea and dysentery.[6] Globally, it is estimated that nearly 1.5 billion are affected by chronic infestation with soil-transmitted helminths and this high prevalence is associated with poverty and poor environmental hygiene. These problems are more pronounced in the developing countries.[4]
Anemia is defined as a condition in which the oxygen-carrying capacity of the red blood cells is reduced and is insufficient to meet the various physiologic needs, which varies by age, sex, and pregnancy status. There are various causes of anemia among which iron deficiency is the most common cause followed by folate, vitamin B12, vitamin A deficiencies, and parasitic infections. Severe form of anemia is associated with weakness, fatigue, and drowsiness. Children, adolescent girls, and pregnant women are particularly vulnerable.[7]
Adolescents constitute to nearly 21% of the total population in India.[8] One of the most easily identifiable adolescent target groups are the school children and the schools can be considered as one of the major source to obtain the epidemiological information regarding the local causes of anemia and to plan the interventions accordingly. The overall iron requirement in the body increases during adolescence period and combined with repeated menstrual blood loss in girls, it leads to iron deficiency anemia.[9] Some parasitic infections, especially soil-transmitted helminths and protozoan parasites, have a higher prevalence among school children and it feeds on the blood of the host tissue leading to the loss of iron and protein resulting in anemia.[4] Because of these reasons, adolescent school girls were chosen as study subjects, as they are a vulnerable group for both anemia and intestinal parasitic infections.
Based on the above factors, this study was planned and conducted among female school children with the following objectives:
To find out the prevalence of intestinal parasitic infections and its association with sociodemographic factors among female school children in the study area.
To find out the prevalence of anemia among female school children in the study area.
To find out whether there is an association between presence of intestinal parasitic infestations and anemia among the study participants.
Materials and Methods
Study area and population
This descriptive cross-sectional study was carried out among female school children studying in and around Anakaputhur, which is an urban area of Kancheepuram district, Tamil Nadu. The study was carried out between January 2017 and March 2017.
Sample size and sampling method
Data collection was carried out from among the schools located in the urban field practice area of our medical college situated in Anakaputhur. There were a total of eight schools in Anakaputhur. From among them, three schools were selected randomly and universal sampling method was followed for data collection.
The details and the purpose of the study were explained to the school authorities and permission was obtained from them before conducting the study. The lists of adolescent girls between the age group of 13 and 18 years were obtained from each of the school. There were a total of 360 students distributed in three schools. Among them, 110 did not give consent to participate in the study. Therefore, a total of 250 willing participants were selected for the study.
Ethical approval and informed consent
Ethical approval was obtained from Institutional ethical Committee. Informed consent was obtained from each of the selected participants and their parents.
Data collection method
Data for this study were collected using a pretested structured questionnaire consisting of sociodemographic details of the participants, their dietary habits, type of toilet used by them, their hand washing practices, and the regularity of their menstrual cycles.
For stool sample collection, the students were given sterile screw capped bottles and both the students and their parents were instructed on the procedure of collection of early morning stool specimen in a sterile manner. The stool specimen was transported to the laboratory and examined under microscope for the presence of parasites, ova, and cysts using standard techniques.[10]
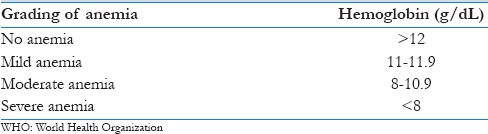
For the estimation of hemoglobin, portable digital hemoglobin meter (manufactured by Goodhealth, Inc.) was used. Standard procedures were followed to collect the blood sample by finger prick method. They were classified into normal, mild, moderate, and severe anemia as per the guidelines laid down by the World Health Organization (WHO) [Table 2].[11]
Table 2.
Classification of anemia as per the WHO[11]
Statistical analysis
Data analysis was carried out using SPSS software version 22 (SPSS Inc., Chicago, USA). The prevalence of intestinal parasitic infection and anemia and sociodemographic characteristics of the study participants were analyzed using descriptive statistics. The strength of association [odds ratio (OR), 95% confidence interval (CI)] and statistical significance (Chi-square and P value) were tested to look for association between anemia and intestinal parasitic infection.
Results
Sociodemographic characteristics of study participants
Table 3 shows the sociodemographic characteristics of the study participants. The study participants were distributed between 8th and 12th standards ranging between 11.2% and 26.8% of the study sample in each class, respectively. According to BG Prasad classification of socioeconomic status, most of the study participants belonged to upper class (33.6%) and upper middle class (29.2%). Regarding the type of family, nearly 79.6% of them belonged to a nuclear family. Around 16.4% of respondent's home had at least one type of pet (dogs, cattle, cats, and birds). Around 19.2% of the study participants used open field for toilet purposes, whereas 80.8% had sanitary toilet facilities in their homes. Nearly 38.8% of them reported that they would either wash their hands before eating or after using the toilet. Around 66.8% of the study participants had regular menstrual cycles with normal flow and pattern and 15.2% of them had irregular menstrual cycle with increased flow lasting for more than 5 days and 18% of them had not attained menarche.
Table 3.
Sociodemographic characteristics and related variables of the study participants

Clinical characteristics of the study participants
Table 4 shows the clinical characteristics of the study participants. It was found that about 84.8% of the study participants were anemic. On microscopic examination of stool samples, it was found that 36% of the participants had at least one of the intestinal parasitic organisms. Among those who were diagnosed with anemia, 12.8%, 46.8%, and 25.2% were found to be having mild, moderate, and severe anemia as per the guidelines recommended by the WHO [Figure 1]. Entamoeba histolytica was the most common intestinal parasite present in the stool samples (23.2%), followed by Giardia intestinalis (5.2%) and hookworms (4.4%) [Figure 2].
Table 4.
Clinical characteristics of the study participants
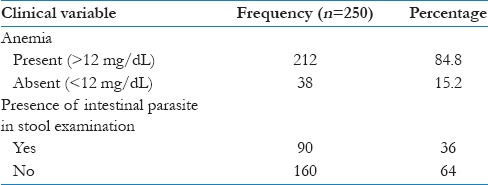
Figure 1.
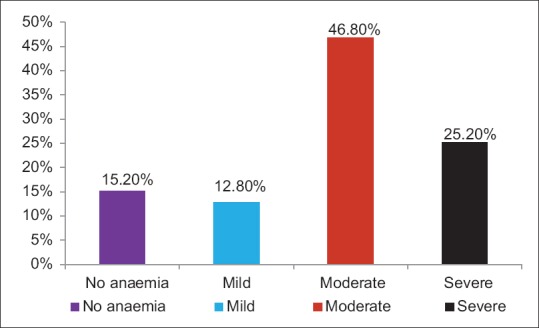
Grading of anemia among the study participants
Figure 2.
Type of intestinal parasite in stool examination
Among those diagnosed as having an intestinal parasitic infection, it was found that using open air defecation increased the odds of being affected by intestinal parasitic infestation by 2.5 times (OR: 2.54, 95% CI: 1.34–4.83]. The association was also found to be statistically significant (P = 0.004). It was found that those who did not follow adequate hand washing practices had 2.4 times increased odds of being affected by intestinal parasitic infection which is also statistically significant (P = 0.001) [Table 5].
Table 5.
Association between Intestinal parasite infection and related variables
Among the study participants, it was found that having intestinal parasitic infection increased the odds of having anemia by 2.84 times (OR: 2.84, 95% CI: 1.19–6.76). The association between intestinal parasitic infection and anemia was found to be statistically significant (P = 0.014) [Table 6].
Table 6.
Association between intestinal parasitic infection and anemia
Discussion
Intestinal parasitic infection is more prevalent in developing countries like India, and when it is present in adolescent school girls, it increases the risk of developing iron deficiency anemia increasing their morbidity leading to malnutrition and lowered academic performance. This study, conducted among adolescent school girls, to find out the prevalence of anemia and intestinal parasitic infection, showed varied and interesting results.
In this study, it was found that 36% of study participants had intestinal parasitic infection. These findings were found to be almost similar to studies conducted by Tsuyuoka et al. in Brazil and Okyay et al. in Turkey, where the prevalence among school children was found to be 42% and 31.8%, respectively.[12,13] In India, there was a wide variation in the prevalence of intestinal parasitic infection. The prevalence was found to be as low as 11.4% in a study conducted by Kotian et al. in Uttarakhand, 23.4% in a study conducted by Mareeswaran et al. in Tamil Nadu, 30.11% in a study conducted by Rai et al. in Nepal, and as high as 63.9% in a study conducted by Ashok et al. among school children in Andhra Pradesh.[1,14,15,16] These variations may have been due to the heterogeneity in the sociodemographic characteristics of the study participants and between the various study locations.
On microscopic stool examination, it was found that Entamoeba histolytica was the most common parasite (23.2%), followed by Giardia intestinalis (5.2%) and hookworms (4.4%) among the study group. Similar results were obtained in a study done by Dhanabal et al.[17] Since presence of protozoan species was common, it shows that feco-oral contamination of food and water is high in the study area.
From this study, it was found that 19.2% of the study participants were using open fields for toilet purposes. In a study done by Ashok et al., it was found that nearly 74.5% were using open fields for toilet purposes.[16] This difference may have been due to the fact that this study was conducted among urban school children as opposed to the study done by Ashok et al. which was done among rural schools in Andhra Pradesh. In both these studies, it was found that using open fields for toilet purposes increases the risk of developing intestinal parasitic infection.
In this study, the prevalence rate of intestinal parasitic infection was higher (48.5%) in those who did not follow adequate hand washing practices before taking food and/or after going to toilets. Similar results were obtained in a study done by Ashok et al.[15] This necessitates the need to create awareness of adequate hand washing practices and its importance among all the school-going children, to reduce the incidence of parasitic infection in them.
From this study, it was found that the prevalence of anemia among the school children was 84.8%. Similar results were obtained in studies conducted by Mandot and Bamnawat, Poyyamozhi et al., Melwani et al., Soman et al., where the prevalence rates were found to be 41.1%, 62%, 67.77%, and 83.6% respectively.[9,18,19,20] Any developing nation, which has a prevalence of anemia more than 40%, is categorized as of severe public health significance.[21] This shows that the burden of anemia is very high among adolescent girls and it poses a major public health problem and interventions have to be carried out to improve their overall health and well-being.
This study has shown that diet did not play any significant role in the prevalence of anemia as it was found to be nearly equally distributed between those who follow vegetarian diet (83.6%) and mixed diet (86.1%). These findings are contradictory to the study done by Rati and Jawadagi where anemia was found to be more prevalent among those who followed a vegetarian diet.[22]
In this study, there was a comparatively higher prevalence of moderate anemia (46.5%). These results were similar to the study findings by Rati and Jawadagiand Mandot et al. where the prevalence of moderate anemia was comparatively higher.[9,22] This study shows that there was a statistically significant association between menstrual irregularities, intestinal worm infection and the presence of anemia. This implies that periodic deworming, increased awareness about iron and folic acid supplementation, and health education about menstrual problems could play a major role in bringing down the burden of anemia and intestinal parasitic infections.
It has been established beyond dispute that parasitic infestation plays a major role in the etiology of anaemia by causing chronic blood loss. Hence, deworming should be done routinely as part of primary healthcare services along with measures to eradicate the reservoir of infection in the community by preventing open air defecation, encouraging the use of footwear and sanitary latrine. Health education regarding personal and environmental hygiene will help reduce the worm load and decrease the burden of anaemia. Thereby, anemia control through primary healthcare should be seen as an integral part of total health care and socioeconomic development.[23]
Conclusion
The findings of this study will help the family physicians and primary healthcare professionals to get adequately sensitized about the significance of high burden of anemia and intestinal parasitic infection and its close association among adolescent school children in our country. Intestinal parasitic infection is a major public health problem as it is directly associated with high prevalence of anemia and poor hygienic conditions and practices.
Interventional measures such as health education to school children about the various personal and environmental hygienic practices such as proper hand washing, waste disposal, and eating a balanced nutritional diet could be provided. Health education should also be targeted toward the parents of school children about periodic deworming and its importance, common menstrual problems and how to tackle it, and the importance of building proper sanitary toilet facilities in their individual homes.
Schools can play a major role in bringing together the stakeholders to improve the knowledge, attitude, and practice of healthy living among adolescents. These measures will help in bringing down the prevalence of both intestinal parasitic infection and anemia, which could directly improve the overall health and well-being of both the individual and the community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors greatly appreciate the support and cooperation given by the medical officer, interns, lab technician, and the field staff attached to the Urban Health Training Centre for carrying out this study in the urban field practice area.
References
- 1.Kotian S, Sharma M, Juyal D, Sharma N. Intestinal parasitic infection-intensity, prevalence and associated risk factors, a study in the general population from the Uttarakhand hills. Int J Med Public Health. 2014;4:422–5. [Google Scholar]
- 2.Savioli L, Albonico M. Soil-transmitted helminthiasis. Nat Rev Microbiol. 2004;2:618–9. doi: 10.1038/nrmicro962. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Schistosomiasis and soil.transmitted helminthic infections – Preliminary estimates of the number of children treated with albendazole or mebendazole. Weekly Epidemiological Record. [Last Cited on 2018 Jan 12]. Available from: http://www.who.int/neglected_diseases/resources/who_wer8116/en/
- 4.WHO. Soil-transmitted helminth infection. [Last Cited on 2018 Jan 12]. Available from: http://www.who.int/mediacentre/factsheets/fs366/en/
- 5.Cappello M. Global health impacts of soil-transmitted nematodes. Pediatr Infect Dis J. 2004;23:663–4. doi: 10.1097/01.inf.0000132228.00778.e4. [DOI] [PubMed] [Google Scholar]
- 6.Davis AN, Haque R, Petri WA. Update on protozoan parasites of the intestine. Curr Opin Gastroentrol. 2002;18:10–4. doi: 10.1097/00001574-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Anemia. World Health Organization. [Last cited 2018 Jan 14]. Available from: http://www.who.int/topics/anemia/en/
- 8.Sivagurunathan C, Umadevi R, Rama R, Gopalakrishnan S. Adolescent health: Present status and its related programmes in India? Are we in the right direction. J Clin Diagn Res. 2015;9:LE01–6. doi: 10.7860/JCDR/2015/11199.5649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mandot S, Bamnawat S. Prevalence of Anemia among rural school children of Rajasthan. Int J Cur Res Rev. 2015;7:40–3. [Google Scholar]
- 10.CDC. DPDx – Laboratory identification of parasitic diseases of public health concern. Stool specimen. [Last Cited on 2018 Jan 16]. Available from: https://www.cdc.gov/dpdx/diagnosticprocedures/stool/index.html .
- 11.Haemoglobin concentrations for the diagnosis of anemia and assessment of severity. World Health Organization. [Last Cited on 2018 Jan 12]. p. 3. Available from: http://www.who.int/iris/bitstream/10665/85839/http://apps.who.int//iris/bitstream/10665/85839/3/WHO_NMH_NHD_MNM_11.1_eng.pdf?ua=1 .
- 12.Tsuyuoka R, Bailey JW, Guimarães AM, Gurgel RQ, Cuevas LE. Anemia and intestinal parasitic infections in primary school students in Aracaju, Sergipe, Brazil. Cad Saude Publica. 1999;15:413–21. doi: 10.1590/s0102-311x1999000200026. [DOI] [PubMed] [Google Scholar]
- 13.Okyay P, Ertug S, Gultekin B, Onen O, Beser E. Intestinal parasites prevalence and related factors in school children, a western city sample-Turkey. BMC Public Health. 2004;4:64. doi: 10.1186/1471-2458-4-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mareeswaran N, Savitha AK, Gopalakrishnan S. Prevalence of intestinal parasites among urban and rural population in Kancheepuram district of Tamil Nadu. Int J Community Med Public Health. 2018;5:2585–9. [Google Scholar]
- 15.Rai L, Saud B, Paudel G, Dhungana G. Prevalence of intestinal parasitic infection among rural area school children of Lokhim VDC, Nepal. J Microbiol Exp. 2017;4:00102. [Google Scholar]
- 16.Ashok R, Suguneswari G, Satish K, Kesavaram V. Prevalence of intestinal parasitic infection in school going children in Amalapuram, Andhra Pradesh, India. Shiraz E-Med J. 2013;14:e16652. [Google Scholar]
- 17.Dhanabal J, Selvadoss PP, Muthuswamy K. Comparative study of the prevalence of intestinal parasites in low socioeconomic areas from South Chennai, India. J Parasitol Res. 2014;2014:1–7. doi: 10.1155/2014/630968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poyyamozhi JS, Rushender R, Reddy GM. Prevalence and factors influencing anaemia among urban adolescent females, a cross sectional study. Int J Community Med Public Health. 2018;5:976–81. [Google Scholar]
- 19.Melwani V, Dubey M, Khan A, Toppo M, Choudhary Y, Priya A. A study to assess the prevalence of anaemia amongst adolescent girls residing in selected slum of Bhopal city. Int J Community Med Public Health. 2018;5:1096–9. [Google Scholar]
- 20.Soman SK, Areekal B, Murali AJ, Varghese RG. Adolescent anaemia its prevalence and determinants: A cross-sectional study from south Kerala, India. Int J Community Med Public Health. 2017;4:2750–6. [Google Scholar]
- 21.Benoist B de, McLean E, Egli I, Cogswell M. Worldwide prevalence of anemia 1993–2005. WHO Global Database on Anemia. 2008. [Last Cited on 2018 Jan 12]. pp. 21–31. Available from: http://whqlibdoc.who.int/publications/2008/9789241596657_eng.pdf .
- 22.Rati S, Jawadagi S. Prevalence of anemia among adolescent girls studying in selected schools. IJSR. 2014;3:1237–42. [Google Scholar]
- 23.DeMaeyer EM. Preventing and controlling iron deficiency anaemia through primary health care. A Guide for Health Administrators and Programme Managers. WHO; 1990. [Last Cited on 2018 Jun 25]. pp. 40–53. Available from: http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/9241542497.pdf?ua=1 . [Google Scholar]


