Abstract
Context:
Early thrombolytic therapy in acute ischemic stroke has proven to reduce the associated morbidity. Many factors are in play, delaying the arrival of patients.
Aim:
To ascertain the factors causing delay in patients with acute ischemic stroke presenting beyond the window period of thrombolysis in and around Chennai, Tamil Nadu, India.
Subjects and Methods:
An observational cross-sectional study involving 200 patients with acute ischemic stroke at Sri Ramachandra Medical College, Chennai, India between June 2015 and July 2016 was conducted. The data was collected by direct interview using a questionnaire designed to study factors such as age, family structure, residence, distance from the hospital, education status, wake-up stroke, transport, symptoms, knowledge about symptoms, seriousness of symptoms, waiting on symptoms, insurance and point of admission. Data was analyzed for means, frequencies, percentages and multiple linear regression analysis was performed to identify factors independently influencing delayed arrival.
Results:
Mean age of the cohort was 58.08 years: 142 men and 58 women. Mean time of delayed arrival was 13.6 hours. Multiple linear regression analysis revealed that seriousness of symptoms (P = 0.001), residence (P = 0.001), point of admission (P = 0.033) and wake-up stroke (P = 0.005) were statistically significant predictors of delayed arrival.
Conclusion:
Patients not perceiving their symptoms to be serious, residing in a rural area, not arriving to the emergency, and having a stroke while awake were all the significant predictors of pre-hospital delay in our study. Awareness among the masses about symptom recognition and early arrival to a tertiary care center will reduce the delay and associated morbidity. Primary care physicians notably play a significant role in educating patients at risk, identifying the symptoms of stroke and referring them for thrombolysis.
Keywords: Acute ischemic stroke, pre-hospital delay, thrombolysis
Introduction
India is in the midst of an epidemiological transition. Hypertension and diabetes are markers of such a transition. This directly leads to the increase in prevalence of stroke. Stroke is defined by the World Health Organization (WHO) as ‘a clinical syndrome consisting of rapidly developing clinical signs of focal (or global in case of coma) disturbance of cerebral function lasting more than 24 hours or leading to death with no apparent cause other than a vascular origin’. According to the India Stroke Factsheet, the prevalence rate of stroke ranges between 84/100,000 and 262/100,000 in rural and between 334/100,000 and 424/100,000 in urban areas.[1] There is solid evidence that early thrombolysis in acute ischemic stroke is beneficial. Recombinant tissue plasminogen activator (r tPA) is currently the only Food and Drug Administration approved therapy for thrombolysis in acute ischemic stroke.[2,3,4] The recommended therapeutic window, ranges from 3 to 4.5 hours.[5,6,7,8] Since the window period is narrow, quick access to thrombolytic therapy is essential. Early hospitalization of suspected stroke patients for immediate diagnostic intervention as well as adequate treatment is an effective pre-hospital management.[9] This is challenging even in developed countries with a well developed health care system where living alone, nocturnal onset, past history of stroke were notable causes of delayed arrival.[10,11,12,13,14,15,16,17,18] In developing countries like India, the problem is compounded by a larger population living is rural areas, low health education, preference of native treatment over evidence based medicine. India is also diverse in terms of quality of health care, socio-economic status, transportation and education, with a significant rural–urban divide. These factors, indigenous to India, may affect the timely arrival of patients with acute ischemic stroke. Two previous studies from North India and one study from South India (Kerala) recognized certain factors like knowledge about stroke, transportation, education status and living distance from hospital to be responsible for delayed arrival.[19,20,21,22]. There is no data specific to Tamil Nadu (South India) with a population of 79 million. Hence, we intended to study the factors causing delayed arrival of patients with acute ischemic stroke, in and around Chennai (Tamil Nadu).
Subjects and Methods
An observational cross-sectional study was conducted at Sri Ramachandra Medical College and Research Institute, Chennai, Tamil Nadu. All patients admitted in Stroke ICU and Stroke ward from June 1, 2016 to July 31, 2017 (13 months) were screened. Patients who fulfilled our criteria of age more than 18 years, symptoms persisting for more than 24 hours, arriving after 4.5 hours of symptom onset and diagnosed as acute ischemic stroke by computerized tomography CT/Magnetic Resonance Imaging MRI were included. Patients with age less than 18 years, who presented within 4.5 hours, cases of cerebral haemorrhage, subarachnoid haemorrhage, subdural haematoma, transient ischemic attack, cerebral venous thrombosis and intra-cerebral malignancy were excluded from the study. The study was stopped when the study population reached 200. According to WHO, Stroke was defined as ‘a clinical syndrome consisting of rapidly developing clinical signs of focal (or global in case of coma) disturbance of cerebral function lasting more than 24 hours or leading to death with no apparent cause other than a vascular origin.’[23]
The time of onset of stroke was defined as the time when the patient noted the first neurological symptom suggestive of stroke. The time of arrival to the hospital was defined as the time the patient was examined by a physician at our hospital. The difference between onset and arrival was taken as the time delay. After obtaining consent, the patient or a relative was directly interviewed using a questionnaire containing the patient's age, sex, family structure, residence, distance from hospital, education status, wake up stroke, transport, symptoms, knowledge about symptoms, seriousness of symptoms, waiting on symptoms, insurance and point of admission.[10,11,19]. Age was categorized arbitrarily into four groups. Family structure was categorized into Joint family, defined as two or more generations living together; Nuclear family, defined as a couple with their dependent children and Living alone. Education was categorized into primary (below 5th standard), secondary (6th–12th standard), and college education. Residence was categorized into Urban, Semi Urban and Rural based on the patient's locality. Distance to the hospital was divided arbitrarily into 5 km radiuses of <5 km, 5–10 km, 10–15 km and >15 km. Mode of transportation, point of admission in the hospital and presence of any health insurance were also noted. To analyze the patient's view of his ailment, we noted three specific factors. ‘Knowledge of symptoms’ meant if the patient knew that he was experiencing a stroke. ‘Seriousness of symptoms’ meant if the patient thought his symptoms were a manifestation of a serious disease, i.e. Stroke. ‘Waiting on symptoms’ meant if the patient thought his symptoms did not need immediate medical intervention.
SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) was used for all analyses. Descriptive statistics, mean and standard deviation were calculated for continuous variables like age and time delay. For other categorical or ordinal variables including sex, family structure, residence, distance to hospital, wakeup stroke, transport, insurance, point of admission, symptoms, knowledge about symptoms, seriousness of symptoms, and waiting on symptoms, frequency distribution and percentage were calculated. t-test was applied to continuous variables, and Chi-square test was applied to categorical or nominal variables. The independent variables with a P value of <0.05 were selected for univariate analysis. Multiple linear regression analysis (step-wise) was done to identify significant predictors delayed arrival.
Results
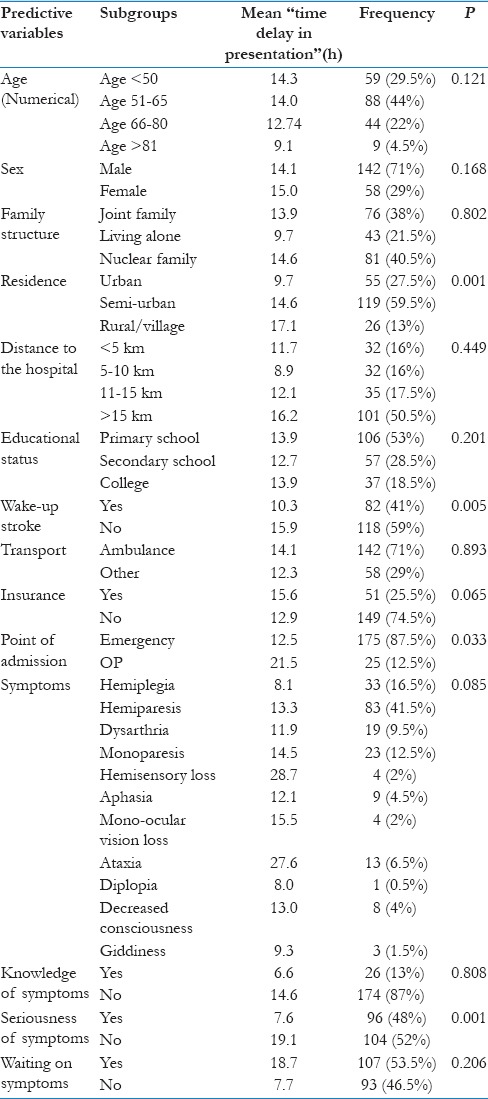
In the 13 month period of study, 200 patients who fulfilled the criteria for the study were included. The cohort contained 142 men and 58 women with a mean age of 58.08 (range 22–90) years. The descriptive statistics is given in [Table 1]. With regards to family structure, 76 (38%) patients were from a joint family system, 43 (21.5%) living alone and 81 (40.5%) from a nuclear family system. Based on residence, 55 (27.5%) patients were from an urban area, 119 (59.5%) from semi urban area and 26 (13%) from rural area. With regards to distance from the hospital, 32 (16%) patients travelled <5 km, 32 (16%) travelled 5–10 km and 35 (17.5%) travelled 10–15 km and 101 (50.5%) travelled >15 km to reach our hospital. With regards to education, 106 (53%) were primary, 57 (28.5%) secondary and 37 (18.5%) college. 82 (41%) patients woke up with a stroke while 118 (59%) had a stroke when they were awake. 142 (71%) patients travelled to the hospital using an ambulance, while 58 (29%) used other modes of transportation. 51 (25.5%) patients were covered with some type of health insurance while 149 (74.5%) weren’t. 175 (87.5%) patients reported to the Emergency Department (ED) while 25 (12.5%) to Neurology out patient. 11 different presentations of stroke were studied where hemiparesis (41.5%) was the most common symptom followed by hemiplegia (16.5%), mono paresis (12.5%) and dysarthria (9.5%). 26 (13%) patients knew that they were having a stroke while 174 (87%) did not. 96 (48%) patients considered their symptoms to be serious enough to require medical attention while 104 (52%) thought that it did not need medical attention. 107 (53.5%) patients decided to wait on their symptoms while 93 (46.5%) thought that their symptoms needed medical intervention.
Table 1.
Descriptive statistics
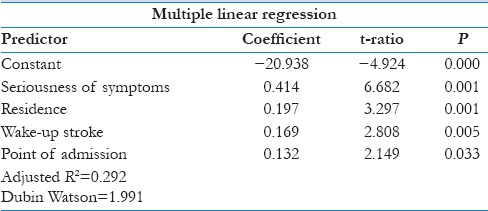
Multiple regression analysis (Step-wise) [Table 2] showed that not considering the symptoms to be serious enough to require medical attention, having a stroke while awake, living in a semi-urban or rural area and presenting to the outpatient and not ED were significant factors contributing to the delayed arrival of patients with acute ischemic stroke.
Table 2.
Multiple linear regression
Discussion
Previous studies from developed countries, on pre-hospital delays recognized factors such as living alone, nocturnal onset, ischemic stroke, lack of recognition of symptoms, lack of knowledge of stroke, perceived seriousness of symptoms, not acting immediately, initial contact with non-emergency services, inability of healthcare personnel to recognize stroke to be important factors delaying arrival.[24,25,26,27] A study from Pakistan revealed lack of knowledge of stroke, symptoms, contact with a local doctor before arrival and lack of ambulance services to be associated with delayed arrival.[22] A few studies from India showed that distance from the hospital, low perception threshold, lack of transport services and contact with local doctor before arrival were associated with delayed arrival.[19,20,21]
In our study, the median time of delayed arrival was 13.6 hours. There was no significant difference in arrival time among age groups or sexes. Contrary to the study done is Leicester, people living alone came earlier than those living in joint or nuclear families.[10] Patients who came to the outpatient department arrived much later than those who came to the ED. Urban dwellers arrived relatively early with a mean time of 9.7 hours, whereas semi urban and rural patients arrived with a mean time of 14.5–17.2 hours respectively. With regards to distance, patients travelling more than 15 km presented with a mean delay time of 16.2 hours. Interestingly, education level did not affect the delay times significantly. Also contrary to the study done by Song D et al., people waking up with stroke arrived relatively earlier than those with a stroke while awake.[28] Predictably, patients with knowledge of stroke arrived earlier.[24,25,26,27,29] Williams LS et al. noted that patients with prior stroke were more likely to correctly interpret their symptoms but were not more likely to present early.[27] With respect to symptoms, patients with hemiplegia, monocular vision loss and giddiness were presented relatively earlier. Hence the type of stroke did not significantly affect delay times. Also predictably, patients who waited on their symptoms arrived later than those who didn’t.
With multiple regression analysis, patients not considering the symptoms to be serious enough to require medical attention, having a stroke while awake, living in a semi-urban or rural areas and presenting to the outpatient and not ED were found to independently delay arrival. Further studies involving many centers in the state may give more information, since our study is based in a single center which can be considered a limitation.
The importance of a primary care physician (PCP) in reducing the pre-hospital delay cannot be understated. There were quite a few patients who reported to a PCP before arriving to our center. After some extensive literature review, we noted that around 50% of patients first present to a PCP after the onset of stroke.[9,30,31] In western countries, many people believe the most appropriate action is to telephone the PCP.[26] Although PCPs recognized stroke and TIA, only two-thirds of PCPs would immediately refer stroke suspected patients with clear symptoms to a tertiary care hospital as medical emergency.[9] Incorrect interpretation of symptoms by PCPs could lead to a preventable pre-hospital delay.[30,32,33] Primary prevention is the best way to tackle the problem of stroke in the community.[18] Patients at risk should be counseled by PCPs periodically, imparting knowledge about the disease and the importance of thrombolysis in the acute setting.[23] Studies specific to India with regards to the referral pattern of PCPs may shed light on awareness and action taken by PCPs.
Finally, patients must be empowered to act in the event of an acute stroke through education and stroke preparedness.[34,35,36] Numerous studies pointing towards the lack of knowledge being an important cause of pre-hospital delay must be addressed.[24,25,26,27,29] Educating them through simple understandable ways should be explored like advertisements in all health centers and mass media. Public information campaigns will most definitely reduce the pre-hospital delay.
Conclusion
Patients not perceiving their symptoms to be serious, residing in a rural area, not arriving to the emergency, and having a stroke while awake were all the significant predictors of pre-hospital delay in our study. Awareness among the masses about symptom recognition and early arrival to a tertiary care center will reduce the delay and associated morbidity. PCPs notably play a significant role in educating patients at risk, identifying the symptoms of stroke and referring them for thrombolysis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013;15:128–34. doi: 10.5853/jos.2013.15.3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke. Stroke. 2016;47:581–641. doi: 10.1161/STR.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 3.National Collaborating Centre for Chronic Conditions. Stroke: National Clinical Guideline for Diagnosis and initial Management of Acute Stroke and Transient Ischaemic Attack. London: Royal College of Physicians; 2008. [Last accessed on 2016 May 12]. www.nice.org.uk/nicemedia/pdf/CG68FullGuideline.pdf . [PubMed] [Google Scholar]
- 4.Meretoja A, Kaste M. Pre- and in-hospital intersection of stroke care. Ann N Y Acad Sci. 2012;1268:145–51. doi: 10.1111/j.1749-6632.2012.06664.x. [DOI] [PubMed] [Google Scholar]
- 5.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 6.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 7.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: An updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 8.Gumbinger C, Reuter B, Stock C, Sauer T, Wietholter H, Bruder I, et al. Time to treatment with recombinant tissue plasminogen activator and outcome of stroke in clinical practice: Retrospective analysis of hospital quality assurance data with comparison with results from randomised clinical trials. BMJ. 2014;348:g3429. doi: 10.1136/bmj.g3429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roebers S, Wagner M, Ritter MA, Dornbach F, Wahle K, Heuschmann PU. Attitudes and Current Practice of Primary Care Physicians in Acute Stroke Management. Stroke. 2007;38:1298–303. doi: 10.1161/01.STR.0000259889.72520.07. [DOI] [PubMed] [Google Scholar]
- 10.Harper GD, Haigh RA, Potter JF, Castleden CM. Factors delaying hospital admission after stroke in Leicestershire. Stroke. 1992;23:835–8. doi: 10.1161/01.str.23.6.835. [DOI] [PubMed] [Google Scholar]
- 11.Feldman E, Gordon N, Brooks JM, Brass LM, Fayad PB, Sawaya KL, et al. Factors associated with early presentation of acute stroke. Stroke. 1993;24:1805–10. doi: 10.1161/01.str.24.12.1805. [DOI] [PubMed] [Google Scholar]
- 12.Barsan WG, Brott TG, Broderick JP, Haley EC, Levy DE, Marler JR. Time of hospital presentation in patients with acute stroke. Arch Intern Med. 1993;153:2558–61. [PubMed] [Google Scholar]
- 13.Fogelhom R, Murros K, Rissananen A, Brass LM, Fayad PB, Sawaya KL, et al. Factors associated with early presentation of acute stroke. Stroke. 1996;27:398–400. [Google Scholar]
- 14.Jorgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Factors delaying hospital admission in acute stroke: The Copenhagen stroke study. Neurology. 1996;47:383387. doi: 10.1212/wnl.47.2.383. [DOI] [PubMed] [Google Scholar]
- 15.Alberts MJ, Bertels C, Dawson DV. An analysis of time of presentation after stroke. JAMA. 1990;263:65–69. [PubMed] [Google Scholar]
- 16.Andeson NE, Broad J, Bonita R. Delays in hospital admission and investigation in acute stroke. BMJ. 1995;31:162. doi: 10.1136/bmj.311.6998.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davalos A, Castillo J, Mavtinaz E. Delay in neurological attention and stroke outcome. Stroke. 1995;26:2233–37. doi: 10.1161/01.str.26.12.2233. [DOI] [PubMed] [Google Scholar]
- 18.Kay R, Woo J, Poon S. Hospital arrival times after onset of stroke. J Neurol Neurosurg Psychiatry. 1992;55:973–74. doi: 10.1136/jnnp.55.10.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashraf VV, Maneesh M, Praveenkumar R, Saifudheen K, Girija AS. Factors delaying hospital arrival of patients with acute stroke. Ann Indian Acad Neurol. 2015;18:162–6. doi: 10.4103/0972-2327.150627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pandian JD, Kalra G, Jaison A, Deepak SS, Shamsher S, Padala S, et al. Factors delaying admission to a hospital-based stroke unit in India. J Stroke Cerebrovasc Dis. 2006;15:81–7. doi: 10.1016/j.jstrokecerebrovasdis.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Srivastava AK, Prasad K. A study of factors delaying hospital arrival of patients with acute stroke. Neurol India. 2001;49:272–6. [PubMed] [Google Scholar]
- 22.Siddhiqui M, Siddiqui SR, Zafar A, Khan SF. Factors delaying hospital arrival of patients with acute stroke. J Pak Med Assoc. 2008;58:178–82. [PubMed] [Google Scholar]
- 23.Hatano S. Experience from a multicentre stroke register: A preliminary report. Bull World Health Organ. 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
- 24.Mellor RM, Bailey S, Sheppard J, Carr P, Quinn T, Boyal A, et al. Decisions and delays within stroke patients’ route to the hospital: A qualitative study. Ann Emerg Med. 2015;65:279–87. doi: 10.1016/j.annemergmed.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 25.Bouckaert M, Lemmens R, Thijs V. Reducing prehospital delay in acute stroke. Nat Rev Neurol. 2009;5:477–83. doi: 10.1038/nrneurol.2009.116. [DOI] [PubMed] [Google Scholar]
- 26.Mackintosh JE, Murtagh MJ, Rodgers H, Thomson RG, Ford GA, White M. Why people do, or do not, immediately contact emergency medical services following the onset of acute stroke: Qualitative interview study. PLoS One. 2012;7:e46124. doi: 10.1371/journal.pone.0046124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams LS, Bruno A, Rouch D, Marriott DJ, Mas DJ. Stroke patients’ knowledge of stroke: Influence on time to presentation. Stroke. 1997;28:912–5. doi: 10.1161/01.str.28.5.912. [DOI] [PubMed] [Google Scholar]
- 28.Song D, Tanaka E, Lee K, Sato S, Koga M, Kim YD, et al. Factors associated with early hospital arrival in patients with acute ischemic stroke. J Stroke. 2015;17:159–67. doi: 10.5853/jos.2015.17.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saengsuwan J, Suangpho P, Tiamkao S. Knowledge of stroke risk factors and warning signs in patients with recurrent stroke or recurrent transient ischaemic attack in Thailand. Neurol Res Int 2017. 2017 doi: 10.1155/2017/8215726. 8215726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson AD, Coleby D, Taub NA, Weston C, Robinson TG. Delay between symptom onset and clinic attendance following TIA and minor stroke: The BEATS study. Age Ageing. 2014;43:253–6. doi: 10.1093/ageing/aft144. [DOI] [PubMed] [Google Scholar]
- 31.Sprigg N, Machili C, Otter ME, Wilson A, Robinson TG. A systematic review of delays in seeking medical attention after transient ischaemic attack. J Neurol Neurosurg Psychiatry. 2009;80:871–5. doi: 10.1136/jnnp.2008.167924. [DOI] [PubMed] [Google Scholar]
- 32.Clarey J, Lasserson D, Levi C, Parsons M, Dewey H, Barber PA, et al. Absolute cardiovascular risk and GP decision making in TIA and minor stroke. Fam Pract. 2014;31:664–9. doi: 10.1093/fampra/cmu054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson A, Coleby D, Regen E, Phelps K, Windridge K, Willars J, et al. Service factors causing delay in specialist assessment for TIA and minor stroke: A qualitative study of GP and patient perspectives. BMJ Open. 2016;6:e011654. doi: 10.1136/bmjopen-2016-011654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dombrowski SU, Ford GA, Morgenstern LB, White M, Sniehotta FF, Mackintosh JE, et al. Differences between US and UK adults in stroke preparedness-evidence from parallel population-based community surveys. Stroke. 2015;46:3220–5. doi: 10.1161/STROKEAHA.115.009997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skolarus LE, Zimmerman MA, Bailey S, Dome M, Murphy JB, Kobrossi C, et al. Stroke ready intervention: Community engagement to decrease prehospital delay. J Am Heart Assoc. 2016;5:e003331. doi: 10.1161/JAHA.116.003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caminiti C, Schulz P, Marcomini B, Iezzi E, Riva S, Scoditti U, et al. Development of an education campaign to reduce delays in pre-hospital response to stroke. BMC Emerg Med. 2017;17:20. doi: 10.1186/s12873-017-0130-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


