Abstract
Background:
Calcium is the most abundant mineral in our body with varied functions, and its dietary deficiency leads to osteoporosis. Various studies have shown that adequate dietary calcium intake (DCI) and moderately increased physical activity if maintained for long term prevent osteoporosis. The data regarding DCI of people living in Karnataka, south India, are limited. Thus, we aimed to assess DCI, physical activity, and their predictors among people living in Karnataka.
Methodology:
A cross-sectional study was done among 250 inpatients and normal relatives of orthopedics department of a tertiary care teaching hospital. Multistage random sampling was performed. DCI and physical activity were measured using validated questionnaires.
Results:
The mean (standard deviation) DCI was 499.94 (251.5). The prevalence [95 confidence interval (CI)] of poor intakers of DCI [DCI < Recommended Dietary Allowance (RDA)] was 76.6% (70.9, 81.7). However, only 43.52% of all participants with poor DCI were on supplements. Male gender [2.189 (1.125, 4.257)], elderly [1.988 (1.067, 3.705)], and low knowledge score [1.240 (1.093, 1.407)] were significant predictors of low DCI. The proportion (95 CI) of patients who were categorized as having low physical activity (LPA) was 44.0% (37.8, 50.4). The predictors for LPA [adjusted odds ratio (95 CI)] were marital status, being single [1.853 (1.047, 3.282)], and low socioeconomic status class [1.209 (1.002, 1.458)].
Conclusion:
DCI was below the RDA for three-fourths of our patients with nearly half of them being physically inactive, indicating the need for better education regarding DCI and improving physical activity, all of which can prevent osteoporosis.
Keywords: Dietary calcium intake, exercise, osteoporosis, physical activity
Introduction
Calcium is the most abundant mineral in our body accounting to nearly 1–1.25 kg. Nearly 99% of this is stored in our bones and teeth and is responsible for maintaining the structure and integrity.[1] The most common disorder affecting the bone is osteoporosis which is characterized by low bone mineral density (BMD) and micro-architectural deterioration of bone tissue resulting in enhanced bone fragility and increased susceptibility to fractures.[2] The prevalence of low BMD has almost doubled from 1990 (0.12%) to 2010 (0.21%) with regards to the total global burden.[3] Almost a one-third of fall-related deaths were attributable to low BMD according to the global burden of diseases study 2010.[3] The prevalence of osteoporosis from 58 countries around the world representing four-fifths of the total world population age 50 years and above was estimated to be around 3% and 10% in men and women 50–59 years of age, respectively. This percentage increased to 6% and 19% in age group 60–69 years, 9% and 35% in 70–79 years, and, 19% and 51%, respectively, in people 80 years of age and above.[4] A systematic review and meta-analysis reported that the median cost for treatment of osteoporosis-related hip fracture is $2943 which represents 18.95% of the Asian countries’ 2014 gross domestic product per capita.[5] Various studies have shown that adequate dietary calcium intake (DCI) and moderately increased physical activity if maintained for long term improve considerably the mechanical competence of the skeletal system.[6,7] Studies have also shown a significant positive correlation between the physical activity levels and various types of fractures such as hip fracture, vertebral fracture, and Colle's fracture.[8,9] The American Diabetes Association advises adults to carry out a minimum of 150 min/week moderate intensity aerobic exercise which would increase the heart rate by 50%–70% from baseline and the exercise should be carried out over a minimum of 3 days a week with no more than 2 consecutive days of no physical activity.[10] In a recent ICMR-INDIAB study which was done among 14,227 individuals from four regions of India, namely, Tamil Nadu, Chandigarh, Maharashtra, and Jharkhand, 54.4% of them were inactive.[11] Similarly, various studies from the neighboring states of Tamil Nadu[2,12,13] and Andhra Pradesh[14] have reported poor DCI. To the best of our knowledge, the data regarding DCI among adults in Karnataka, India, are limited and the data in men are scarce. There are no current guidelines in India regarding calcium supplementation in adults and we hypothesize that DCI would be less than the Recommended Dietary Allowance (RDA), that is, 800 mg/day of DCI in postmenopausal women and 600 mg/day for other adult women and all men.[15] Since calcium has a large number of homeostatic functions and also has close association with osteoporosis, we felt it is important to estimate the average DCI along with daily physical activity levels among both genders in our cultural setting.
Methodology
This was a cross-sectional study that was conducted in a tertiary care teaching hospital in Bengaluru, a south Indian metropolitan city, between November 2016 and October 2017. The primary objective of the study was to determine the DCI, physical activity levels, and their determinants among adults (age ≥18 years) inpatients and normal relatives from the department of orthopedics. All consenting adults whose domicile was Bangalore, Karnataka, for the past 5 years at least were included to maintain homogeneity in the participant's cultural activities including dietary habits. Subjects who were seriously ill, diagnosed with psychiatric illnesses with loss of insight or major neurocognitive disorder, and those with pre-existing clinician diagnosed conditions such as metastatic cancer, chronic kidney disease, hypothyroidism due to any cause, liver cirrhosis, surgical menopause, chronic diarrhoea, and other diseases with impaired entero-hepatic circulation, where we anticipate that the participant would already have undergone formal nutrition advise to enhance DCI, were excluded.
Based on a study done among 106 postmenopausal women by Raj et al.[12] in an urban city in Tamil Nadu, the standard error of mean in our population was estimated to be around 30 mg/day. The sample size calculated with an alpha error of 5%, power 80%, and an estimated error (d) of 4 mg/day using the formula n = [1.962 × (SEM/√n)2] was 217. Accounting for 10% non-responders and rounding off, the final sample size was increased to 250. A maximum of five participants were randomly chosen (using random number table) from the inpatient register maintained in the orthopedics ward on 2 randomly chosen days (lottery method) in a week till the calculated sample size was reached. If the chosen patient was found ineligible, one of their normal relative who fulfils the eligibility criteria was chosen.
After obtaining written informed consent, a pretested semi-structured questionnaire was administered which contained the following sections, namely, basic and demographic details, calcium food frequency questionnaire, questions pertaining to physical activity levels, and knowledge regarding DCI. The food frequency questionnaire used to assess DCI was validated for use among south Indian people in comparison with the dietary record dairy of 5 days and laboratory values of serum calcium.[13] Using this questionnaire, the average daily intake of each food item was assessed in grams and DCI was calculated per 100 grams of the specified food item. We also assessed participants for using calcium supplements but were not included under DCI, rather reported separately. The short version of the International Physical Activity Questionnaire (IPAQ) was used to measure the physical activity levels. IPAQ short version has four questions on duration (in minutes per week) of having performed a high-intensity activity, moderate-intensity activity, walking, and sitting.[16] IPAQ was supplemented with the show cards designed by the World Health Organization describing the intensity of physical activity. Metabolic equivalent of tasks were calculated and participants were classified into low, moderate, and high physical activities based on the criteria prescribed in IPAQ.[17] The knowledge questionnaire comprised 10 multiple-choice questions pertaining to food items rich in calcium, the RDA, and clinical significance of poor DCI. After formal assessment, all patients were taught on how to enhance DCI in their regular diet and on the importance of good physical activity for optimum health. Those found with poor DCI along with risk factors for osteoporosis were referred back to the treating surgeon with a request to evaluate for possible osteoporosis. The study was approved by the Institutional Ethics Committee (reference No. 178/2016).
Data entry was done in Epi Info™ software version 7 (CDC, USA; 2011). Statistical analyses were performed with IBM's Statistical Package for Social Sciences (SPSS) version 20 (IBM Corp., USA; 2011). Sociodemographic characteristics, DCI levels, and levels of physical activity were summarized using descriptive statistics. The predictors of poor DCI (DCI < RDA) were subjected to a univariate analysis. Those predictors whose significance levels (P-value) were less than 0.2 were subjected to a multivariate analysis using appropriate regression models. In the same manner, multivariate analysis for predictors of low physical activity (LPA) and poor knowledge were computed. Statistical significance was set at P-value less than 0.05.
Results
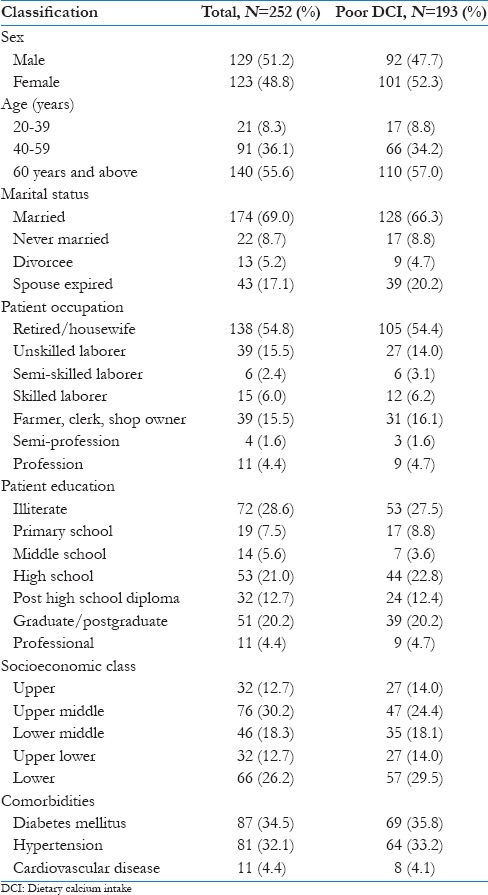
A total of 318 patients were screened and 252 patients were enrolled. The mean [standard deviation (SD)] age of the study participants was 59.05 (12.61) years. More than half of the participants were elderly, above the age of 60 years. Diabetes mellitus (34.5%) and hypertension (32.1%) were the two most common comorbidities. The other sociodemographic features of the study population are enumerated in Table 1. The mean (SD) DCI was 499.94 (251.52). The prevalence [95 confidence interval (CI)] of poor intakers of DCI (DCI < RDA) was 76.6% (70.9, 81.7). About 43.25% of all study participants (33.33% of all men and 53.66% of all women) were taking calcium supplements. However, only 43.52% of all participants with poor DCI (32.61% of all men with poor DCI and 53.47% of all women with poor DCI) were on supplements.
Table 1.
Demographic characteristics
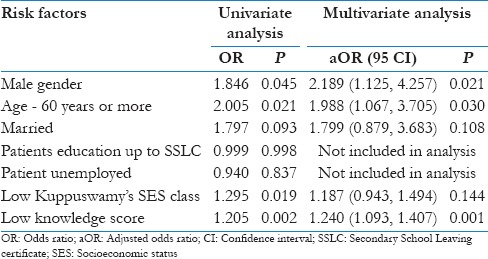
The results of univariate and multivariate analyses of the barriers for an adequate DCI are tabulated in Table 2. Male gender, age 60 years and above, being married, poor education, unemployment, lower Kuppuswamy's socioeconomic status (SES), and poor knowledge score were considered for univariate analysis. Apart from education and unemployment, all the other factors were subjected to binary logistic regression. The barriers [adjusted odds ratio (aOR) (95% CI)] identified were male gender [2.189 (1.125, 4.257)], 60 years of age and above [1.988 (1.067, 3.705)], and low knowledge score [1.240 (1.093, 1.407)].
Table 2.
Predictors of poor dietary calcium intake
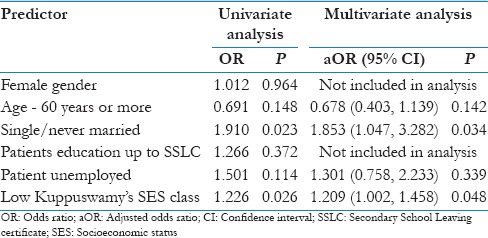
The mean (SD) knowledge score computed was 3.73 (2.66). The proportion (95 CI) of participants having poor knowledge, that is, less than 50% of the maximum score, was 55.2% (48.8, 61.4). The univariate and multivariate analyses of predictors of poor knowledge are depicted in Table 3. The significant predictors [aOR (95 CI)] were female gender [2.630 (1.519, 4.554)] and poor education [2.701 (1.405, 5.194)]. With regard to physical activity levels, the proportion (95 CI) of patients who were categorized as having LPA was 44.0% (37.8. 50.4), whereas 30.2% (24.6, 36.2) and 25.8% (20.5, 31.7) were categorized as having moderate and high physical activity, respectively. The predictors for LPA [aOR (95 CI)] that were identified were marital status, being single [1.853 (1.047, 3.282)], and low SES class [1.209 (1.002, 1.458)] which are s enumerated in Table 4.
Table 3.
Predictors of poor knowledge
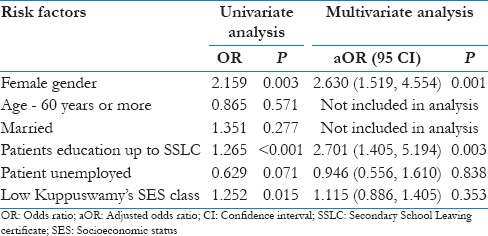
Table 4.
Predictors of low physical activity
Discussion
The mean DCI intake of around 500 mg/day is below the RDA for all adults. About three-fourths of the study population were assessed to be taking DCI below the RDA. These findings are similar to those reported from other studies in the neighboring south Indian states of Tamil Nadu and Andhra Pradesh. Raj et al. in the year 2015 using the same validated questionnaire reported that the mean (SD) DCI intake among 106 urban postmenopausal women from Tamil Nadu was 632.72 (28.23) mg/day and the prevalence of people with low DCI was 74.5%.[12] Malathy et al. using similar methodology reported that the mean (SD) of DCI among residents of Chennai city, Tamil Nadu, was 707.14 (107.96) mg/day.[13] The third study from Tamil Nadu which was done among semi-urban post-menopausal women using 24-h dietary recall method reported a mean (SD) DCI of 398.76 (190.13) mg/day.[2] The study by Harinarayan et al. from Tirupathi, Andhra Pradesh, using a 5- to 7-day dietary recall method reported that the mean (standard error) of DCI among urban and rural men was 328 (8) and 271 (3) mg/day, whereas in women it was 306 (2) and 262 (3) mg/day, respectively.[14] Another study conducted among three different groups of construction workers in Delhi, north India, reported a mean average DCI between 400 and 500 mg/day.[18] Our findings also corroborate with the report from a recent systematic review of 78 studies covering 74 countries and the best estimate of DCI ranged from 175 mg/day (Nepal) to 1233 mg/day (Iceland) among general population. Notably, there was a definitive pattern globally with many countries in the south, east, and southeast Asia having low DCI (<400 mg/day) while those from Africa and south America having moderately low DCI (400–700 mg/day). On the other hand, all countries which had a DCI >1000 mg/day were from northern Europe.[19] With regard to calcium supplementation, we see that only around 43% of those with poor DCI are on supplements and also men were using supplements less comparatively than women.
We report that men and elderly have approximately two times the increased odds of having poor DCI. For long time now, the focus was on perimenopausal women as they were at higher risk of developing osteoporosis due to the decreasing oestrogen levels,[20] and it is rather interesting to find that women have a lesser chance than men in being poor consumers of calcium-rich diet according to our findings. Reports also suggest that men were about 75% less likely to receive treatment of osteoporosis when compared with women. Only 1% of the male population have their BMD assessed.[21] Another report from Australia has pointed out that only 24.1% of men who experienced two consecutive fractures within a time frame of less than 1 year received treatment.[22] Men are also at higher risk of experiencing worse outcomes than women after a fracture.[21] For example, men are twice likely to die than women after a hip fracture.[23] Furthermore, 42% of all fall-related injuries lead to fractures of the femur, pelvis, arm and forearm which are the most common causes of geriatric mortality.[24] It is well known that fall among elderly is common and the prevalence of fall in elderly in India is estimated anywhere between 14% and 53%.[25] We therefore would like to reiterate the fact that men also should be equally screened for osteoporosis and its risk factors such as poor DCI or LPA, more so in the geriatric age group, and appropriate treatment comprising diet and lifestyle-related education, calcium supplementation, or anti-resorptive medications be initiated on a timely basis.
Poor knowledge on calcium-rich diet and its importance was the third risk factor of poor DCI which was identified in our study. For every unit fall in the knowledge score, there was a 20% increased chance of poor DCI intake. This finding again is consistent with the findings by Raj et al. wherein poor knowledge had an increased chance of nearly five times for poor DCI.[12] A regression analysis to identify the risk factors of poor knowledge revealed that female gender and lower educational status were the two main factors that increased the odds by approximately 2.6 and 2.7 times, respectively. Education and knowledge go hand in hand. According to the 2011 census of Karnataka state, the literacy rate of women in the state was 68.08% when compared to men at 82.47%.[26] As mentioned, women in the perimenopausal age group have increased chances of osteoporosis, and our findings with regard to knowledge serves as a reminder to all physicians to continue educating women with poor educational background on the importance of adequate DCI and physical activity.
Besides DCI, the second most important modifiable risk factor of osteoporosis is LPA. The majority (44%) were classified as LPA. This is, however, less than that reported from other studies in India. The prevalence of LPA in the ICMR-INDIAB study was 54%.[11] A study by Tripathy et al. among 5127 participants from Punjab reported that 29.2% and 32.6% of respondents reported light levels of physical activity in urban and rural areas, respectively.[27] Similarly, another study from Kerala has reported that LPA was seen in 65.8% of the 240 study participants.[28] The risk factors for LPA identified in our study were marital status being single (unmarried/spouse expired), and SES class. Marital status being single had an increased odd of approximately two times, while low SES demonstrated an increased odd by 23% to have LPA.
The strengths of our study are that it is the first of its kind to assess DCI among participants who have their domicile in Karnataka, India. Our study also throws light on the status of DCI among men. Third, we have used a food frequency questionnaire to assess DCI that has been validated specifically among the people of south India. However, it is not considered the gold standard since it does not objectively measure DCI and the estimation is purely based on the last weeks’ dietary intake. Therefore, the estimate obtained may not necessarily be representative of the participants’ long-term dietary habits which would be a more important determinant of bone health. The other limitation is that LPA was assessed using a validated questionnaire which could have been assessed using advanced devices such as calorimetry[29] that could estimate physical activity objectively and prospectively. Finally, this study was hospital-based.
Conclusion
The mean DCI (~500 mg/day) of our population was below the RDA, and approximately three-fourths of them were poor dietary intakers of calcium. Elderly, especially men form the high-risk group for poor DCI. Prompt dietary assessment with equal importance to men should be done at the primary care level, and wherever appropriate, calcium supplementation, lifestyle modification education, or anti-osteoporosis therapy be initiated. Women with poor literacy are vulnerable due to their lack of knowledge on importance of adequate DCI, and hence this group should naturally become the target for intense dietary education. The majority (44%) are still classified as having LPA and the high-risk groups being marital status – single and those in lower SES class. We believe a good understanding and knowledge of the various risk factors for poor DCI and LPA by the primary care physicians among the local population these physicians cater to will go a long way in prevention of osteoporosis and related bone fractures. We further recommend much larger studies making prospective measurements of DCI and LPA involving people of varied cultural diversities of India to be conducted which would enable us to make policy-level decisions especially with regard to calcium supplementation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vasudevan DM, Sreekumari S. Textbook of Biochemistry. 5th ed. Chapter 28. 2007. pp. 314–315. [Google Scholar]
- 2.Paul TV, Thomas N, Sheshadri MS, Oommen R, Jose A, Mahendri NV. Prevalence of osteoporosis in ambulatory postmenopausal women from a semi-urban region in southern India: Relationship to calcium nutrition and vitamin D status. Endocr Pract. 2008;14:665–71. doi: 10.4158/EP.14.6.665. [DOI] [PubMed] [Google Scholar]
- 3.Sànchez-Riera L, Carnahan E, Vos T, Veerman L, Norman R, Lim SS, et al. The global burden attributable to low bone mineral density. Ann Rheum Dis. 2014;73:1635–45. doi: 10.1136/annrheumdis-2013-204320. [DOI] [PubMed] [Google Scholar]
- 4.Oden A, McCloskey EV, Johansson H, Kanis JA. Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int. 2013;92:42–9. doi: 10.1007/s00223-012-9666-6. [DOI] [PubMed] [Google Scholar]
- 5.Mohd-Tahir NA, Li SC. Economic burden of osteoporosis-related hip fracture in Asia: A systematic review. Osteoporos Int. 2017;28:2035–44. doi: 10.1007/s00198-017-3985-4. [DOI] [PubMed] [Google Scholar]
- 6.Uusi-Rasi K, Sievänen H, Vuori I, Pasanen M, Heinonen A, Oja P. Associations of physical activity and calcium intake with bone mass and size in healthy women at different ages. J Bone Miner Res. 1998;13:133–42. doi: 10.1359/jbmr.1998.13.1.133. [DOI] [PubMed] [Google Scholar]
- 7.Wallace LS, Ballard JE. Lifetime physical activity and calcium intake related to bone density in young women. J Womens Health Gend Based Med. 2002;11:389–98. doi: 10.1089/152460902317586029. [DOI] [PubMed] [Google Scholar]
- 8.Wickham CA, Walsh K, Cooper C, Barker DJ, Margetts BM, Morris J, et al. Dietary calcium, physical activity, and risk of hip fracture: A prospective study. BMJ. 1989;299:889–92. doi: 10.1136/bmj.299.6704.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan HL, Lau EMC, Woo J, Lin F, Sham A, Leung PC. Dietary calcium intake, physical activity and the risk of vertebral fracture in Chinese. Osteoporos Int. 1996;6:228–32. doi: 10.1007/BF01622739. [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association. Foundations of care: education, nutrition, physical activity, smoking cessation, psychosocial care, and immunization. Sec. 4. In Standards of Medical Care in Diabetes—2015. Diabetes Care. 2015;38(Suppl. 1):S20–30. doi: 10.2337/dc15-S007. [DOI] [PubMed] [Google Scholar]
- 11.Anjana RM, Pradeepa R, Das AK, Deepa M, Bhansali A, Joshi SR, et al. Physical activity and inactivity patterns in India – Results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5] Int J Behav Nutr Phys Act. 2014;11:26. doi: 10.1186/1479-5868-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raj JP, Oommen AM, Paul TV. Dietary calcium intake and physical activity levels among urban South Indian postmenopausal women. J Family Med Prim Care. 2015;4:461–4. doi: 10.4103/2249-4863.161355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malathy S, Gayathri G, Hemamalini AJ. Developing and validating food frequency questionnaire to assess dietary calcium intake in adults. Int J Food Nutr Sci. 2013;2:113–5. [Google Scholar]
- 14.Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D, Srinivasarao PV, Sarma KV, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am J Clin Nutr. 2007;85:1062–7. doi: 10.1093/ajcn/85.4.1062. [DOI] [PubMed] [Google Scholar]
- 15.Nutrient requirements and recommended dietary allowances for Indians. A Report of the Expert Group of the Indian Council of Medical Research. 2009. [Last accessed on 2015 Apr 05]. Available from: http://www.icmr.nic.in/final/RDA-2010.pdf .
- 16.International Physical Activity Questionnaire (IPAQ) [Last accessed on 2015 Apr 05]. Available from: https://www.sites.google.com/site/theipaq/questionnaire_links .
- 17.Global Physical Activity Questionnaires (GPAQ) generic show cards. [Last accessed on 2015 Feb 25]. Available from: http://www.who.int/entity/chp/steps/GPAQ_GenericShowCards.pdf .
- 18.Goswami R, Saha S, Sreenivas V, Singh N, Lakshmy R. Vitamin D-binding protein, vitamin D status and serum bioavailable 25(OH) D of young Asian Indian males working in outdoor and indoor environments. J Bone Miner Metab. 2017;35:177–84. doi: 10.1007/s00774-016-0739-x. [DOI] [PubMed] [Google Scholar]
- 19.Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR, et al. Global dietary calcium intake among adults: a systematic review. Osteoporos Int. 2017;28:3315–24. doi: 10.1007/s00198-017-4230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.America's Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington, DC: National Osteoporosis Foundation; 2002. [Google Scholar]
- 21.Cawthon PM. Gender differences in osteoporosis and fractures. Clin Orthop Relat Res. 2011;469:1900–5. doi: 10.1007/s11999-011-1780-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Otmar R, Henry MJ, Kotowicz MA, Nicholson GC, Korn S, Pasco JA. Patterns of treatment in Australian men following fracture. Osteoporos Int. 2011;22:249–54. doi: 10.1007/s00198-010-1204-7. [DOI] [PubMed] [Google Scholar]
- 23.Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–90. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens JA, Curse PS, Finkelstein EA, Miller TR. The costs of fatal and nonfatal falls among older adults. Inj Prev. 2006;12:290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dsouza SA, Rajashekar B, Dsouza HS, Kumar KB. Falls in Indian older adults: A barrier to active ageing. Asian J Gerontol Geriatr. 2014;9:1–8. [Google Scholar]
- 26.Census2011.co.in. Karnataka population sex ratio in Karnataka literacy rate data. [online] 2017. [Last accessed on 2017 Dec 31]. Available from: http://www.census2011.co.in/census/state/karnataka.html .
- 27.Aslesh OP, Mayamol P, Suma RK, Usha K, Sheeba G, Jayasree AK. Level of physical activity in population aged 16 to 65 years in rural Kerala, India. Asia Pac J Public Health. 2016;28(1 Suppl):53S–61S. doi: 10.1177/1010539515598835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: Are we witnessing the great Indian equalisation? Results from a cross-sectional STEPS survey. BMC Public Health. 2016;16:816. doi: 10.1186/s12889-016-3489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Westerterp KR. Control of energy expenditure in humans. [Updated 2016 Nov 11] In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, et al., editors. Endotext [Internet] South Dartmouth (MA): MDText. com, Inc; 2000. [Last accessed on 2017 Sep 17]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278963 . [Google Scholar]


