Abstract
Background:
India has a vast public health infrastructure with 23,391 primary health centers (PHCs) and 145,894 subcenters providing health services to 72.2% of the country's population living in rural areas. Although the numbers look impressive, their functional status needs to be studied in terms of physical infrastructure, manpower, equipment, drugs, and other logistical supplies that are greatly needed for ensuring quality services. This work aims to study the infrastructure facilities and manpower in a sample of PHCs in the district of Nellore in the state of Andhra Pradesh in India.
Methods:
Randomly selected samples of 15 PHCs have been studied using structured and pretested performance standard questionnaire. Data have been analyzed with reference to the Indian Public Health Standards (IPHS) of the Government of India.
Results:
Many deficiencies were identified in infrastructure and manpower in the PHCs studied. Some of the important findings were that the deficiency of AYUSH medical officers was 86.6% and the deficiency of health workers (female) was 13.33%. Some of the important drugs such as antihypertensives, anticonvulsants, emergency drugs, drops, ointments, and solutions were available in less than 50% of the PHCs. Only 47% of the PHCs had Typhidot tests and H2S test strips, and in the labor rooms only 20% of the PHCs have a Standard Surgical Set for episiotomies in accordance with IPHS.
Conclusion:
PHCs lack the manpower and vital infrastructure that are necessary for the effective day-to-day functioning and provision of primary healthcare to the population.
Keywords: Indian Public Health Standards, National Rural Health Mission, primary health center
Introduction
Primary health centers (PHCs) are the cornerstone of rural healthcare in India, as they are the first point of contact with a qualified doctor. PHCs are a part of the three-tier healthcare system in India; they act as referral centers for the community health centers, 30-bed hospitals, and higher order public hospitals at the taluka and district levels.[1] The PHCs are established and maintained by the state governments under the Minimum Needs Program and the Basic Minimum Services Program.[2] PHCs form the first level of contact and serve as a link between individuals and the national health system by bringing healthcare delivery as close as possible to where people live and work. Each PHC is targeted to cover a population of approximately 20,000 in hilly, tribal, or difficult-to-access areas, and a population of 30,000 in plain areas, with four to six indoor/observation beds, and is entrusted with providing promotive, preventive, curative, and rehabilitative care.[3] This implies offering a wide range of services such as health education, promotion of nutrition, provision of mother and child family welfare services, immunization, disease control, appropriate treatment for illness and injury, basic sanitation, and safe drinking water supply.[3]
Historically, the concept of primary healthcare came into existence following an international conference at Alma-Ata, USSR, in 1978.[1] After this conference, healthcare became regarded as synonymous with “basic health services, first contact care and easily accessible care.”[4] The four principles of primary healthcare include equitable distribution, community participation, intersectoral coordination, and appropriate technology. Even though the Bhore Committee[5] in India proposed this concept way back in 1946, the establishment of PHCs in India did not start to grow at a rapid pace until after 1978.[1]
In 2005, the Government of India launched the National Rural Health Mission (NRHM), with the goal of improving the availability and access to quality healthcare, particularly for people in rural areas.[6] The NRHM envisages a synergistic primary healthcare approach for decentralized health planning and implementation at the village and district level.[7] The NRHM was made operational in April 2005 throughout the country, with special focus on 18 states that have weak demographic indicators and infrastructure.[7] It reaffirms the political will of the Government to increase public health fund allocation to 2%–3% of the gross domestic product (GDP) from the existing allocation of 0.9% of the GDP.[7] The NRHM increases public accountability to the community through Indian Public Health Standards (IPHS). One of the important aims of the NRHM is to develop effective human resource management that can generate more manpower and equip health personnel with multiple adequate skills.[7]
Rural healthcare in India faces a crisis unmatched by any other sector. Only 20% of the population seeking outpatient services and 45% of those seeking inpatient treatment make use of public services due to run-down infrastructure and a poor supply of drugs and equipment.[8] Standards are the main drive for continuous improvements in quality. The performance of PHCs can be assessed against the set standards to provide the optimal level of quality healthcare. The Department of Health and Family Welfare of the Government of India has prepared the IPHS for PHCs with three objectives: first, to provide comprehensive primary healthcare to the community through primary healthcare; second, to achieve and maintain acceptable standards of quality healthcare; and third, to make the services more responsive and sensitive to the needs of the community.[3]
Keeping in view the resources available in India with respect to the functional requirement for PHCs with minimum standards such as building, manpower, instruments, equipment, drugs, and other facilities, these standards would help monitor and improve the functioning of the PHCs. The overall objective of the IPHS for PHCs is to provide healthcare that is quality-oriented and sensitive to the needs of the community. The objectives of the study are to examine the availability of infrastructure facilities at PHCs, investigate the availability of adequate manpower in PHCs, and assess them by comparing them to the IPHS.
Methods
The cross-sectional, community-based study was conducted in Nellore district, Andhra Pradesh, in the study setting of PHCs. There are 60 PHCs in Nellore district that are distributed in three divisions (Gudur, Nellore, and Kavali). About 25% of the PHCs have been selected randomly – that is, 5 PHCs have been taken from each division randomly, for a total of 15 randomly selected PHCs. The five PHCs selected randomly from the Nellore division are A. S Peta, Mohammadapuram, Varigonda, Podalakur, and Mahimalur. The five PHCs selected from the Gudur division are Ozili, Ramapuram, Kota, Griddalur, and Pernadu, and the remaining PHCs selected from the Kavali division are Ramatheerdham, Marripadu, Yellayapalem, Jaladanki, and SR Puram. The duration of the study was for 2 years between August 2010 and July 2012. Permission was obtained from the District Medical and Health Officer (DMHO) for studying the infrastructure and manpower of PHCs. The list of medical officers (MOs) along with their phone numbers was obtained from the DMHO office. MOs were informed about the visit the day before it took place. After confirming their convenience and availability, the PHCs were visited and primary data were collected through the questionnaires that were developed using the IPHS for PHCs. Data have been analyzed using SPSS software.
Results
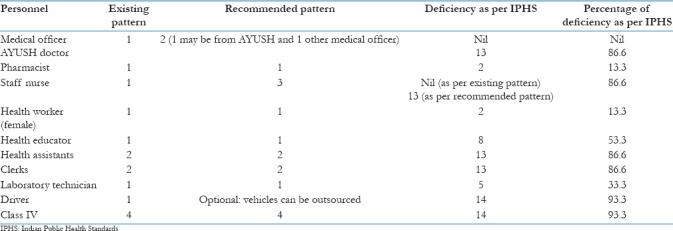
The deficiency of health manpower according to the IPHS varied significantly across the different types of health personnel in the PHCs, as shown in Table 1. All the PHCs have only one MO. The deficiency of AYUSH medical officers (AMOs) was 86.6%. The deficiency of pharmacists as per IPHS was 13.3%. A staff nurse was available at all the PHCs, which satisfied the IPHS requirement for one nurse per PHC, but considering the recommended norm of three staff nurses per PHC, the deficiency was 86.6%. In terms of the requirement that each PHC has one female health worker (HW), the deficiency was 13.3%. Finally, 93.33% of the PHCs lacked Class IV employees who were directly employed by the government. However, all the PHCs had contingent workers who were employed as needed for purposes such as cleaning.
Table 1.
Availability of manpower in primary health centers
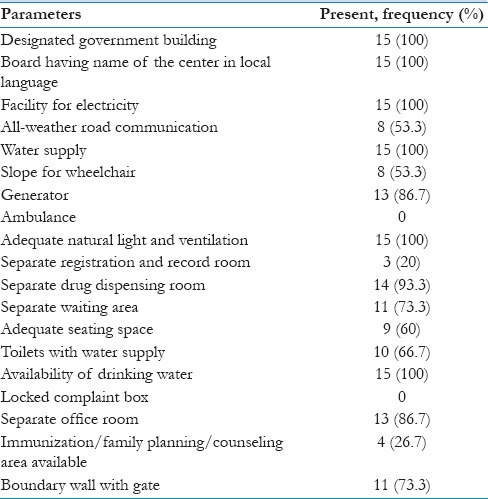
The availability of general infrastructure in the PHCs is shown in Table 2. All PHCs are located in a designated government building that displays the name of the building in the local language, and they all have the facility for electricity. All-weather road communication and a slope for wheelchairs were available in 53.3%. No ambulances or complaint boxes were found in any of the PHCs. A boundary wall with a gate was present in only 73.3% of the PHCs.
Table 2.
Availability of general infrastructure in primary health centers
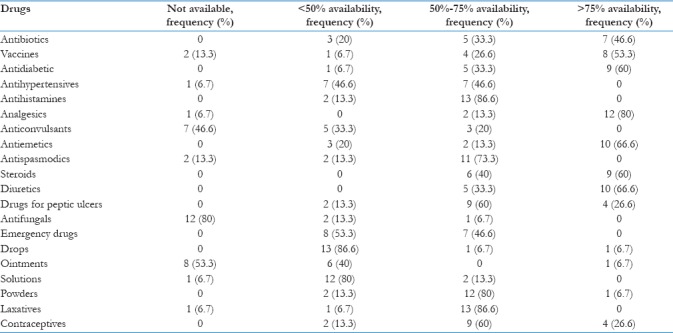
The availability of the different categories of drugs in the PHCs as recommended by the IPHS is shown in Table 3. The drugs that were in less than 50% of the PHCs were antihypertensives, anticonvulsants, emergency drugs, drops, ointments, and solutions. The drugs that were available in more than 50% of the PHCs were antibiotics, vaccines, antidiabetic drugs, antihistamines, analgesics, antiemetics, antispasmodics, steroids, diuretics, powders, laxatives, contraceptives, and drugs for peptic ulcers.
Table 3.
Availability of drugs in primary health centers
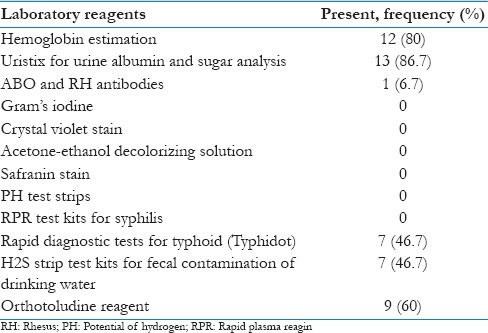
The presence of laboratory reagents in the PHCs is shown in Table 4. About 80% of the PHCs had laboratory reagents for hemoglobin (Hb) estimation. Around 87% of the PHCs had Uristix for urine albumin and sugar analysis. Only 6.7% of the PHCs were doing ABO and RH antibody testing. None of the PHCs had Gram's iodine, crystal violet stain, acetone-ethanol decolorizing solution, safranin stain, PH test strips, or RPR test kits for syphilis, as per IPHS. About 60% of the PHCs had orthotoludine reagent. Around 47% of the PHCs had Typhidot tests and H2S test strips, as per IPHS.
Table 4.
Availability of laboratory reagents in primary health centers
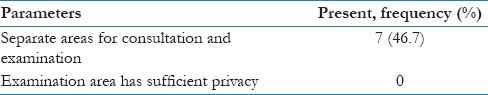
The infrastructure of outpatient departments in the PHCs is shown in Table 5. Around 47% of the PHCs had separate areas for consultation and examination. None of the PHCs had an examination area with sufficient privacy.
Table 5.
Infrastructure of outpatient department in primary health centers
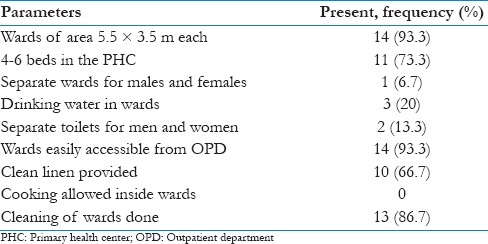
The availability of an inpatient ward with minimal facilities is mandated under the IPHS, as shown in Table 6. Around 74% of the PHCs had four to six beds, as per IPHS. Around 94% of the PHCs did not have separate wards for males and females, and 80% of the PHCs did not have drinking water in the wards. Around 87% of the PHCs did not have separate toilets for men and women. Cooking inside the wards is not allowed in any of the PHCs. Around 87% of the PHCs had been cleaned.
Table 6.
Infrastructure of inpatient department in primary health centers
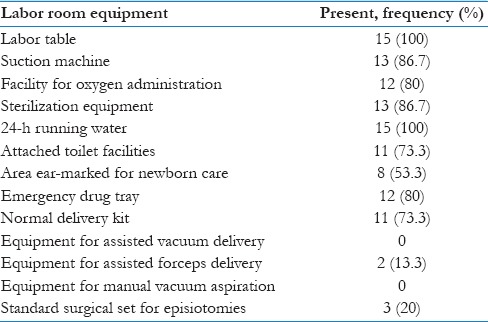
IPHS mandates the presence of a completely functional labor room. Table 7 shows the availability of equipment in the labor room. All the PHCs had a labor table. In addition, 86.7% of the PHCs had a suction machine, 80% had a facility for oxygen administration, 86.7% had sterilization equipment, 80% had an emergency drug tray fully equipped with emergency drugs as per IPHS, and only 20% of the PHCs had a Standard Surgical Set for episiotomies as prescribed by IPHS.
Table 7.
Availability of equipment in primary health center labor rooms
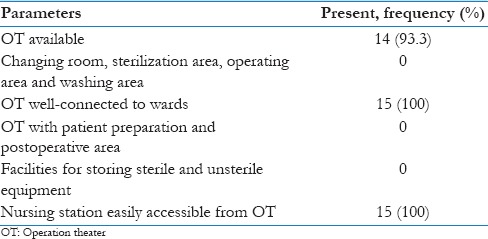
IPHS recommends the presence of a completely functional operation theater (OT) in the PHCs, as shown in Table 8. Around 94% of the PHCs had an OT, and 100% of those PHCs had an OT that was well-connected to wards and easily accessible to the nursing station. None of the PHCs had an OT with a separate changing room, sterilization area, operating area, or washing area. In addition, none of the PHCs had an OT with separate patient preparation and postoperation areas, or separate facilities for storing sterile and unsterile equipment.
Table 8.
Infrastructure of operation theaters in primary health centers
Discussion
Manpower
The PHCs in Nellore district have been assessed for their infrastructure and manpower. This is compared with the results from studies assessing the PHCs in different parts of India. As per the IPHS, each PHC should consist of one MO and one AYUSH medical officer (AMO). In our study, 100% of the PHCs had one MO. A study showed that 80% of the PHCs in the state of Assam had an MO, while in Karnataka it was 90%.[9] The findings of our study are much better than that of the situation in the northeastern state of Assam and the neighboring state of Karnataka. Another study showed that the percentage of PHCs that had at least one MO was 65% in Uttar Pradesh, 100% in Madhya Pradesh, Assam, Jammu and Kashmir, and Rajasthan, 75% in Chattisgarh, and 50% in Himachal Pradesh. Our findings in Nellore district are in the same line as that of Madhya Pradesh, Assam, Jammu and Kashmir, and Rajasthan.[10]
The deficiency of pharmacists in Nellore district was 13.3%. In Assam, the presence of pharmacists according to the IPHS was 100%, while in Karnataka it was only 60%.[9] The findings of our study show that the situation in Nellore district was better than Karnataka but not Assam. The reason may be that as a state in the Empowered Action Group (EAG), Assam gets more funds and undergoes stricter facility inspections.[9] Another study in the tribal districts of Karnataka reported a high vacancy rate for pharmacists (52%).[11] Our study has much better findings than the tribal districts of Karnataka. A possible reason may be that many medical personnel were not willing to work in the tribal areas. Another study in Gujarat showed that the post of compounder was filled in only 70% of the PHCs.[12]
The availability of staff nurses was 100%, as per the existing norm of one for each PHC, yet when considering the recommended norm of three staff nurses per PHC, the deficiency was 86.6%. In Assam, it was found that 80% of the PHCs met the manpower requirements for Nurse-Midwife according to the IPHS, while in Karnataka it was found to be 50%.[9] Sekhar et al. reported that the nurse:midwife ratio was 1:1.5 in the PHCs in Andhra Pradesh.[13] The findings of our study are better than the findings of the other reported studies.
Among the PHCs in Nellore district, the deficiency of HWs was 13.33%. A national study reported that there is a 1.9% deficit in the number of HWs in PHCs.[14] The deficiency of health educators was 53.3%. Contrary to this finding, another study in Andhra Pradesh reported that health educators are available in 94% of the centers.[13] The situation is found to be poor in Nellore district when compared to the results of the study from the whole of Andhra Pradesh. The deficiency of health assistants in Nellore district was 86.6%. In the EAG state of Assam, the deficiency of health assistants was 60%; in the non-EAG state of Karnataka, it was found to be 30%.[9] Other states in India such as Madhya Pradesh, Uttar Pradesh, Rajasthan, and Tamil Nadu were found have 56%, 14%, 25%, and 40% deficiencies, respectively.[15] The findings of our study show that the deficiency was much higher in all other states in India.
In Nellore district, 66.66% of the PHCs have at least one clerk, and 86.66% are deficient according to the two-clerk guideline set forth by the IPHS. In Assam, it was found that 40% of the PHCs had two clerks, while only 30% in Karnataka satisfied that standard.[9] The PHCs in our district showed a high percentage of deficiency. In Nellore district, 33.33% of the PHCs did not have lab technicians (LTs). In Assam, it was found that the presence of LTs was 100%; however, in Karnataka it was found to be only 80%.[9] Another study showed that the proportion of LTs present in PHCs in Madhya Pradesh, Uttar Pradesh, Rajasthan, Andhra Pradesh, Karnataka, and Tamil Nadu was 11%, 86%, 75%, 67%, 67%, and 80%, respectively.[15] UP, Rajasthan, and Tamil Nadu had higher numbers of LTs in their PHCs than the PHCs in our study.
In our study, we determined that 93.33% of the PHCs in Nellore district did not have drivers. The reason may be that the Government of Andhra Pradesh has provided 108 ambulance services, which play a vital role in the case of referrals. Therefore, the need for individual ambulances in the PHCs is practically nonexistent, so there are no drivers in the PHCs except in cases where there is a separate vehicle for the MO. The findings of our study in Nellore district showed that 93.33% of the PHCs did not have Class IV employees who were directly employed by the government. But all PHCs had contingent workers who were employed as needed for purposes such as cleaning.
Infrastructure
According to IPHS, it is expected that all PHCs function in their own buildings. The status of ownership of a designated PHC building in Nellore district is slightly lower when compared with Assam and Karnataka, where the Designated Government Building ownership was 100%.[9] A study in the tribal districts of Karnataka showed that only 32% of the PHCs had their own building.[11] This is significantly lower than the findings of our study. The reason may be that Nellore is not a tribal area and is one of the developed areas of Andhra Pradesh, where 83% of the PHCs function from their own buildings.[13] All the PHCs in Madhya Pradesh, Uttar Pradesh, Rajasthan, Andhra Pradesh, Karnataka, and Tamil Nadu have their own Designated Government Building.[15] Our study in Nellore district shows that the number of PHCs with their own building is above the state average of Andhra Pradesh, but lower than some of the other states.
In this study, 53.3% of the PHCs had all-weather road communication. This means that half of the PHCs cannot be reached throughout the year, which causes severe access barriers. A study of the entire Andhra Pradesh reported that more than 90% of the PHCs had all-weather roads.[13] Our study findings are much lower than the state average, which shows that the PHCs in Nellore district are less accessible than other PHCs in the state. In Madhya Pradesh, Uttar Pradesh, Rajasthan, and Tamil Nadu, all-weather roads were present in 78%, 93%, 88%, and 90% of the PHCs, respectively.[15] The findings of our study were lower than the results reported for the lesser developed North Indian states of MP, UP, and Rajasthan, as well as the better developed neighboring South Indian state of Tamil Nadu. A boundary wall is essential for maintaining cleanliness and for prevention of encroachment of government land, which is quite common in many parts of India. In our study, 73.3% of the PHCs had a boundary wall with a gate. The findings of our study are slightly lower than that of the state average for Andhra Pradesh as reported by Sekhar et al.[13] In addition, in our study only 53.3% of the PHCs had a slope for wheelchairs. Therefore, only about half of the PHCs had a slope for wheelchairs, which shows that there was a failure either in the planning stage or the implementation stage. Creating a slope for wheelchairs is not an activity that would require considerable resources. Not having a slope indicates that those PHC facilities are insensitive to the needs of people with disabilities.
India has many regional languages that are understandable by the majority of the local population, but many of the official communications are written in English, which is understandable mostly by the educated population. Having the name of the PHC displayed in the local language is vital for the poor and uneducated people to access the services. In our study in Nellore district, 100% of the PHCs had the name of the center in the local language. All the PHCs in Assam had display boards in the local language, and 70% in Karnataka.[9] The state average of PHCs in Andhra Pradesh with a local language display board was only 91%.[13] All the PHCs had the facility for electricity. Electricity was present in 78% of the PHCs in Madhya Pradesh, 79% in Uttar Pradesh, and 100% in Rajasthan, Andhra Pradesh, Karnataka, and Tamil Nadu.[15] It was found that electricity was present in almost all the PHCs in South Indian states, even in the tribal areas of Karnataka, whereas in the North Indian states the number of PHCs with electricity was less than 80%. None of the PHCs in our study had a complaint box. This is a very bad situation, since the feedback from the public about problems with the services or facilities cannot be obtained by the authorities, leaving no opportunity for improvement. In this study, 100% of the PHCs had a water supply that was either piped or from a bore well. This is significantly better than the PHCs in Punjab, which reported that a water supply was available in only 26.3% of the PHCs.[16] Toilets with an adequate water supply were available in 66.7% of the PHCs in our study, which is almost similar to that of the tribal districts of Karnataka (73%).[11] This level is high when compared with the Andhra Pradesh state average of toilets in only 45% of the PHCs.[13]
In Nellore district, 73.3% of the PHCs had an inpatient ward with four to six beds. A study in the tribal districts of Karnataka reported that 62% of the PHCs had four to six beds.[11] However, a study in Ahmedabad, Gujarat, reported that only 30% of the PHCs had indoor bed facilities.[12] In this study, the laboratory tests that were found in the various PHCs were as follows: blood examination (Hb, total count, differential count) estimation 80%, urine albumin and sugar analysis 86.7%, blood grouping and typing 6.7%, RPR test for typhoid 46.7%, H2S test strip for fecal contamination of drinking water 46.7%, and orthotoludine test 60%. Basic laboratory facilities for routine blood, urine, and stool examination were available in 80% of the PHCs studied in Karnataka, while they were present in only 20% of the PHCs studied in Assam.[9] The presence of drugs in our study according to IPHS was 69.6%. A study done in Bihar reported that essential drugs required for various health centers were in short supply or unavailable in medical stores.[17] In Punjab, the reported deficiency of drugs as per IPHS in the PHCs is 90.2%.[16] Our study's findings were better than the situations in some of the other states.
All the PHCs in our district had a labor room for deliveries, but many of the facilities in the labor rooms were inadequate. In the tribal districts of Karnataka, the availability of labor rooms was reported as 62%.[11] In Punjab, the reported labor room availability was 10.5%. The findings of our study were much better than that of Punjab.[16] Zakir Husain (2011) reported that the availability of a labor room in the PHCs in these states was as follows: 40% in Uttar Pradesh, 91.7% in Madhya Pradesh, 87.5% in Assam, 75% in Jammu and Kashmir, 50% in Chattisgarh, 75% in Himachal Pradesh, and 100% in Rajasthan.[10] The findings of our study were the same as that of the state of Rajasthan, which also had labor rooms in all its PHCs, and our findings were better than the states of UP, MP, Assam, Jammu and Kashmir, Chattisgarh, and Himachal Pradesh. Although the availability of labor rooms was adequate, the facilities inside the labor rooms need to be improved.
In Nellore district, 93.3% of the PHCs had OTs. However, in the tribal districts of Karnataka, the reported presence of OTs was 59%.[11] Furthermore, in Assam the OT availability was 0%, and in Karnataka it was 70%.[9] The availability of an OT in the PHCs in Madhya Pradesh, Uttar Pradesh, and Tamil Nadu was 22%, 14%, and 40%, respectively. The findings of our study were much better than those of the states of Karnataka, MP, UP, and Tamil Nadu.[15] Thus, our study demonstrated that the PHCs in Nellore district were much better equipped with OTs than the other states in India.
Conclusion
The manpower and infrastructure in the PHCs in Nellore district are severely lacking. Although the presence of MOs in the PHCs is adequate, the presence of para-medical staff and supporting staff is insufficient. Steps should be taken by the state governments and district administration to fill the vacancies of para-medical and supporting staff in the PHCs. AYUSH treatment, which is prioritized under the current government, should be implemented by appointing AYUSH doctors and pharmacists and by providing AYUSH drugs.
Many aspects of the infrastructure of the PHCs need improvement. All-weather road facilities to reach the PHCs should be improved to reduce access barriers. Proper slopes should be provided for the movement of wheelchairs, making the PHCs sensitive to the needs of disabled people. Health education leaflets in Telugu should be made available in the patient waiting area. Labor rooms with separate areas for septic and aseptic deliveries for effective infection control should be provided. India already has high rates of maternal and infant mortality; to help avoid increasing these rates, PHCs should be well equipped to conduct normal deliveries, as well as manage emergencies. Equipment for assisted forceps delivery and episiotomies should be provided to provide safe delivery services. Residential accommodation for MO and other staff needs to be provided in all the PHCs. The supply of some categories of drugs, such as antifungal, anticonvulsants, and ointments, needs to be improved. The condition of the wards also needs to be improved by providing mattresses on beds and maintaining cleanliness. Thus, there is a need to improve both the manpower and infrastructure in the PHCs to deliver effective primary care services to the nearly 70% of the Indian population living in rural areas. Although commitment from both the state and central governments is necessary to improve the health infrastructure and manpower in the PHCs, it is the primary duty of the state governments to address this issue, since public health is a state subject, while the central government provides directive and technical guidance.
Limitations
In the absence of readily available official records, MOs, staff nurses, and pharmacists in the PHCs furnished some of the information from their knowledge and memory. Thus, there is a possibility that some of the information may be inaccurate due to recall bias. Although appointments were made in advance with MOs, some of them were not available during the time of our visit due to some unforeseen reason, so the para-medical staff provided information in these centers. In the absence of many studies in the area since the framing of the IPHS, our discussion of the results was limited by the minimal data which we could compare our findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Park K. Park's Textbook of Preventive and Social Medicine. 24th ed. Jabalpur: M/s Banarasidas Bhanot Publishers; 2017. [Google Scholar]
- 2.State wise functioning Primary Health Centers (PHCs) in Government Buildings of. Open Government Data Platform India. Ministry of Health and Family Welfare. Government of India. 31st March. 2014. [Last accessed on 2018 Jun 20]. Available from: https://www.community.data.gov.in/state-wise-functioning-primary-health-centres-phcs-in-government-buildings-of-india-as-on-31st-march-2014/
- 3.Indian Public Health Standards. Guidelines for Primary Health Centers. Directorate General of Health Services. Ministry of Health and Family Welfare. Government of India; Revised. 2012. [Last accessed on 2018 Jul 29]. Available from: http://www.nhm.gov.in/images/pdf/guidelines/iphs/iphs-revised-guidlines-2012/primay-health-centres.pdf .
- 4.World Health Organization. Primary Health Care: Now More than Ever. The World Health Report. 2008. [Last accessed on 2018 Jul 01]. Available from: http://www.who.int/whr/2008/whr08_en.pdf .
- 5.Bhalwar R. Textbook of Public Health and Community Medicine. 2nd ed. Department of Community Medicine AFMC Pune; 2013. [Google Scholar]
- 6.Srivastava Committee Report. Health Series and Medical Education: A Programme for Immediate Action. Report of the Group on Medical Education and Support Manpower. [Last accessed on 2018 Jul 04]. Available from: https://www.nhp.gov.in/sites/default/files/pdf/Srivastava_Committee_Report.pdf .
- 7.Chokshi M, Patil B, Khanna R, Neogi SB, Sharma J, Paul VK, et al. Health systems in India. J Perinatol. 2016;36:S9–12. doi: 10.1038/jp.2016.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Health Policy 2017. Ministry of Health and Family Welfare. Government of India. 2017. [Last accessed on 2018 Jul 08]. Available from: https://www.mohfw.gov.in/sites/default/files/9147562941489753121.pdf .
- 9.Zaman FA, Laskar NB. An application of Indian public health standard for evaluation of primary health centers of an EAG and a non-EAG state. Indian J Public Health. 2010;54:36–9. doi: 10.4103/0019-557X.70551. [DOI] [PubMed] [Google Scholar]
- 10.Hussain Z. Health of the national rural health mission. Econ Polit Wkly. 2011;46:53–60. [Google Scholar]
- 11.Nanjunda DC. Functioning of primary health centres in the selected tribal districts of Karnataka-India: Some preliminary observations. Online J Health Allied Sci. 2011;10:3. [Google Scholar]
- 12.Rakesh S, Bhavsar BS, Sunil N, Mihir G. Availability of services and facilities at primary health centres in Ahmedabad district, Gujarat. Natl J Community Med. 2010;1:24–6. [Google Scholar]
- 13.Sekhar PS, Rajeswari NV, Rao VS, Punetha AC. Indian Institute of Health and Family Welfare. Facility Survey of Public Health Institutions in Andhra Pradesh. 2008:77–131. [Google Scholar]
- 14.Garg S, Singh R, Grover M. India's health workforce: Current status and the way forward. Natl Med J India. 2012;25:111–3. [PubMed] [Google Scholar]
- 15.Iyengar S, Dholakia RH. Access of the rural poor to primary healthcare in India. Rev Market Integr. 2012;4:71–109. [Google Scholar]
- 16.Ghuman BS, Mehta A. Health care services in India: Problems and prospects. International Conference on the Asian Social Protection in Comparative Perspective. National University of Singapore. 2009 [Google Scholar]
- 17.Roy C, Das JK, Jha HK, Bhattacharya V, Shivdasani JP, Nandan D, et al. Logistics and supply management system of drugs at different levels in Darbhanga district of Bihar. Indian J Public Health. 2009;53:147–50. [PubMed] [Google Scholar]


