Abstract
Objectives
This article models the chain of risk that links life course socioeconomic status (SES), daily stressor exposure and severity, and daily well-being.
Method
Data from the main survey and the daily diary project of the Midlife in the United States (MIDUS) Refresher study were combined, resulting in 782 participants (55.6% female; age 25–74, Mage = 47.9) who reported on 5,849 days of information on daily stressors and daily well-being. Data were measured at both person and day levels. Between-person predictor variables include childhood SES, education, and adult SES. Within-person daily variables assessed exposure to daily stressors, severity of daily stressors, positive affect, negative affect, and daily physical symptoms. We contrasted hypothesized models, the chain of risk trigger effect model versus the additive model within a multilevel structural equation modeling framework.
Results
The influences of life course SES and daily stressor exposure and severity on daily well-being were better described by the chain of risk additive model than the chain of risk trigger effect model. Childhood SES was directly and indirectly (through education, adult SES, and daily stressor exposure and severity) associated with daily well-being (in between-person level), especially daily physical symptoms and daily negative affect.
Discussion
Childhood may be a sensitive period that has salient implications for day-to-day well-being later in life.
Keywords: Cumulative advantage/disadvantage, Daily stressors, Health disparities, Life course analysis, Structural equation models
Studies have shown that childhood is a sensitive period, during which low socioeconomic status (SES) has long-term effects on health (Miller, Chen, & Parker, 2011). Daily stress processes are one pathway through which childhood SES may lead to disparities in health due to persistent lower levels of daily well-being that is caused by daily stressor exposure and severity (Leger, Charles, Ayanian, & Almeida, 2015; Miller et al., 2011). However, the precise mechanisms through which childhood SES and daily stressor exposure and severity affect daily well-being have rarely been clearly articulated, nor have they been explicitly tested. This article presents a multilevel structural equation modeling (MSEM) approach to simultaneously investigate within-person links among childhood SES, daily stressor exposure and severity, and daily well-being, as well as between-person differences in such links. We define daily well-being as a combination of physical and psychological well-being, including daily negative affect, daily positive affect, and daily physical symptoms (Leger et al., 2015; Reis, Sheldon, Gable, Roscoe, & Ryan, 2000).
Childhood SES and Adult Health: Chain of Risk of Life Course SES
According to the life course epidemiology framework, early-life disadvantages increase one’s exposure to later hardships, forming what is known as the “chain of risk” of health in adulthood (Ben-Shlomo, Mishra, & Kuh, 2014). In terms of SES, previous studies have shown that there are lower levels of intergenerational mobility in the United States (Torche, 2015), which suggests that social status remain relatively stable between different generations within the same family (Chetty, Hendren, Kline, Saez, & Turner, 2014). The majority of people in the United States accumulate either socioeconomic opportunities (high SES) or risks (low SES) across their life course (Luo & Waite, 2005). These chains of socioeconomic opportunities or risks generally depend on individual’s early-life SES, which is determined by their parental SES.
Life course epidemiology holds two competing models of pathways that link chain of risk of SES to health: the trigger effect model and the additive model (Ben-Shlomo et al., 2014), also known as the social trajectory model and the cumulative exposure model (Berkman, 2009). The trigger effect model contends that the most recent risk in the life course solely affects health. In contrast, the additive model is used to propose that the presence of independent effects from earlier risks affect later-life health. Current literature provides mixed results with respect to the pathways through which childhood SES is associated with health and well-being in later life. Luo and Waite (2005), for example, found that childhood SES is associated with physical, mental, and cognitive well-being in later life, independent of adult SES. However, Marmot, Shipley, Brunner, and Hemingway (2001) found that childhood SES had little impact on health in later life and that adult SES was a more important factor that contributes to health problems, such as coronary disease.
Chain of Risk of Life Course SES, Daily Stressor Exposure and Severity, and Daily Well-Being
Daily stressors (or daily hassles) are minor yet frequent day-to-day disruptions, such as family arguments and work deadlines (Almeida, 2005). One possible mechanism that links daily stressors to health outcomes is frequency of stressor exposure, which is the probability that a person will experience a daily stressor (Almeida, Piazza, Stawski, & Klein, 2011). Furthermore, daily stressor exposure is partially related to structural factors, such as SES, that increase an individual’s chance of experiencing day-to-day stressors (Almeida, 2005; Almeida et al., 2011). However, previous studies have shown that individuals with less education report lower exposure to daily stressors. At the same time, when these same individuals do experience daily stressors, the stressors are often perceived as more severe (Almeida, Neupert, Banks, & Serido, 2005; Grzywacz, Almeida, Neupert, & Ettner, 2004).
Higher daily stressor severity has been shown to be associated with lower levels of daily positive affect, daily negative affect, and daily physical symptoms (Almeida, 2005; Almeida et al., 2005; Grzywacz et al., 2004). Furthermore, persistent lower levels of daily well-being that is caused by higher daily stressor severity may be the mechanism by which SES is linked to chronic diseases. A previous study found that higher levels of daily negative affect associated with daily stressors significantly predicted chronic physical and psychological distress (Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013; Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013) and mortality risk (Chiang, Turiano, Mroczek, & Miller, 2018). In addition, Leger and colleagues (2015) found that higher daily physical symptoms associated with daily stressors predicted chronic conditions and functional impairment 10 years later. Finally, lower levels of daily positive affect associated with daily stressors significantly predicted elevated levels of inflammation (Sin, Graham-Engeland, Ong, & Almeida, 2015) and mortality (Mroczek et al., 2015).
Studies on the influence of childhood SES on daily biological functioning in later life have shown the importance of daily stress processes and daily well-being as possible mechanisms of disparities in health. For example, early-life SES has been linked to alterations in autoimmune and endocrine regulation in later life that may presage chronic diseases (Carroll, Cohen, & Marsland, 2011; Desantis, Kuzawa, & Adam, 2015; Miller et al., 2011). These alterations of biological processes may be associated with persistent lower levels of daily well-being that is associated with daily stress processes. A previous study found that reactivity to daily stressors is associated with increased cortisol output (Stawski, Cichy, Piazza, & Almeida, 2013). Elevated cortisol output has been linked to chronic diseases and mortality (Schoorlemmer, Peeters, van Schoor, & Lips, 2009).
Hypotheses
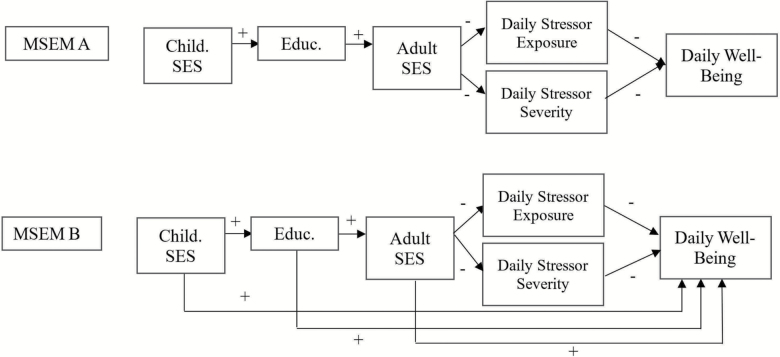
Given that daily stressor exposure and severity and levels of daily well-being are important predictors of long-term health, it is essential to analyze their associations with childhood SES to better understand the influence of early-life experiences on later disparities in health conditions. This article evaluates whether the influence of the chain of risk of life course SES, daily stressor exposure and severity, and daily well-being follow better the trigger effect model or the additive model (Figure 1).
Figure 1.
Hypothesized models: MSEM A, chain of risk trigger model; MSEM B, chain of risk additive model.
Method
Participants
Data are from the Midlife in the United States (MIDUS) Refresher study. The MIDUS Refresher study was performed to investigate the health impacts (broadly defined) of the great recession in the late 2000s among adults in the United States. The MIDUS Refresher was also intended to refresh and expand the MIDUS study by recruiting a new set of participants (Kirsch & Ryff, 2016). The present analysis included 782 participants (55.6% female; ages 25–75, Mage = 47.91) who participated in the MIDUS Refresher daily diary study. All participants had previously joined the MIDUS Refresher main survey, a nationally representative telephone–mail survey conducted between 2011 and 2014 involving 3,577 people, aged 23–76 years old.
Participants in the daily diary study (conducted between 2012 and 2016) were randomly selected from the main survey participants. They completed telephone interviews for eight consecutive evenings regarding their daily experiences. On average, participants completed 7.5 of the eight interview days, which resulted in a total of 5,849 daily diary days. Participants signed an informed consent to participate in both the main survey and the daily diary study. Sociodemographic characteristics of the participants in the daily diary study were similar to those of participants in the main survey (Table 1), which was also the case in the previous waves of MIDUS (Almeida, Wethington, & Kessler, 2002; Cichy, Stawski, & Almeida, 2012).
Table 1.
Demographic Comparison of the MIDUS Refresher Main Survey and the Daily Diary Study
| Demographic variable | MIDUS Refresher baseline surveya | MIDUS Refresher daily diary studyb |
|---|---|---|
| Age | ||
| Young adults (23–39) | 27.3 | 27.7 |
| Midlife adults (40–59) | 39.9 | 51.2 |
| Older adults (60–76) | 32.8 | 21.1 |
| Gender (%) | ||
| Males | 48.1 | 44.4 |
| Females | 51.9 | 55.6 |
| Education (%) | ||
| No bachelor degree | 50.1 | 53.9 |
| Bachelor degree and above | 49.9 | 46.1 |
| Average household income in USD (SD) | 85,285.55 (64,367.35) | 84,458.33 (67,206.75) |
| Marital status (%) | ||
| Married | 64.0 | 65.3 |
| All others | 36.0 | 34.7 |
| Children in householdc (%) | ||
| Yes | 45.1 | 45.8 |
| No | 54.9 | 54.2 |
| Race (%) | ||
| Caucasian | 82.3 | 82.6 |
| African American | 7.7 | 7.4 |
| All other races | 10.0 | 10.0 |
Note: MIDUS Refresher = Midlife in the United States Refresher Study.
aRespondents in the MIDUS Refresher baseline survey (N = 3,577). bRespondents in the MIDUS Refresher daily diary study, all of whom had previously participated in the MIDUS Refresher main survey (N = 782). cWhether respondent had at least one child aged 18 or younger living in the house.
Measures
The variables in this study were divided into day-level and person-level data. Day-level data were measured during eight consecutive days of the daily diary study, whereas person-level data were obtained through the baseline survey of the MIDUS Refresher. As days are nested within individuals (Almeida, Stawski, & Cichy, 2011), MSEM permits the examination of within-person links among childhood SES, daily stressor exposure and severity, and daily well-being, as well as between-person differences in such links (see Analysis for a more detailed explanation of MSEM; see Supplementary Table 1 for correlations among the variables used in model fitting).
Day-Level Variables
Daily Positive and Negative Affect
During the daily telephone interviews, participants were asked to indicate the frequency at which they experienced a certain positive and negative emotion during that day on a 0–4 scale (0 = none of the time, 1 = a little of the time, 2 = some of the time, 3 = most of the time, and 4 = all the time). Daily positive affect was computed using 14 items (Cronbach’s alpha = .95 across all persons and days) associated with positive feelings or emotions (adapted from Mroczek & Kolarz, 1998). This measure has been shown to be associated with health outcomes such as inflammation among people from different age groups across adulthood (Sin et al., 2015). Daily negative affect was measured using 14 items (Cronbach’s alpha = .87 across all persons and days) from the adapted version of the Non-Specific Psychological Distress Scale (Kessler et al., 2002). This measure has been shown to be associated with health outcomes such as chronic physical health conditions among people from different age groups across adulthood (Piazza et al., 2013). Daily positive affect and daily negative affect were calculated by taking the mean responses from each scale in each day of the daily diary study. Across all persons and days, the mean of daily positive affect was 2.52 (SD = 2.62, minimum–maximum = 0–4) and the mean of daily negative affect was 0.22 (SD = 0.07, minimum–maximum = 0–3.43).
Daily Physical Symptoms
Participants were asked to indicate whether they experienced each of the 22-physical symptoms in a physical symptoms checklist (Leger et al., 2015) during the day. The instrument measures five groups of symptoms: aches/pain, gastrointestinal symptoms, chest pain or dizziness, flu symptoms, and an open-ended response for other type of physical symptoms. This measure has been shown to be associated with health outcomes including chronic conditions and functional impairment among different age groups across adulthood (Leger et al., 2015). Daily physical symptoms were calculated by summing the number of symptoms experienced by each participant across the 8 days of the telephone interview (Cronbach’s alpha = .74 across all persons and days). Across all persons and days, the mean of daily physical symptoms was 1.87 (SD = 2.33, minimum–maximum = 0–22).
Daily Stressor Exposure
Participants were asked whether they experienced any stressor event covered in the Daily Inventory of Stressor Events (DISE; Almeida et al., 2002). The DISE includes seven different types of stressors: arguments, avoided arguments, discrimination, work/education stressors, home stressors, network stressors (events that occur to close friends and family), and other stressors. Participants who experienced at least one type of stressor in each day of the daily diary interview were coded as 1 (yes) for daily stressor exposure; otherwise, they were coded as 0 (no). Participants in the MIDUS Refresher reported at least one daily stressor on 40% of the study days, which coincides with the percentage of stressor days found in previous waves of the MIDUS daily diary study (Almeida et al., 2002; Cichy et al., 2012).
Daily Stressor Severity
Participants also reported the severity (“How stressful was this stressor for you?”) of each reported stressor in each study day using a 4-point Likert scale (0 = not at all, 1 = not very, 2 = somewhat, 3 = very stressful). The daily stressor severity variable was the mean of each day’s reported stressor severity. Participants who reported zero stressors in any of the study days were assigned a zero for their daily stressor severity. Across all persons and days, the mean of daily stressor severity was 0.75 (SD = 1.02, minimum–maximum = 0–3).
Person-Level Variables
Childhood SES
Data regarding participant’s SES are from the MIDUS Refresher main survey. Participants’ childhood SES was measured using four indicators: (a) parent’s highest level of education (0 = < high school, 1 = high school/GED, 2 = some college and above), (b) parent’s employment status during childhood (0 = not working at all/a little of time, 1 = some of the time/most of the time, 2 = all the time), (c) whether the family of origin received welfare (0 = all the time/most of the time, 1 = some of the time/a little of the time, 2 = never in welfare), and (d) financial situation growing up (0 = a lot/somewhat/a little worse off than average family, 1 = same as average family, 2 = a lot/somewhat, a little better off than average family). The mean childhood SES score was 5.95 (SD = 1.60, median = 6, minimum–maximum = 0–8). This set of childhood SES measures has been shown to be a significant predictor of health outcomes in adulthood, such as allostatic load (Friedman, Karlamangla, Gruenewald, Koretz, & Seeman, 2015; Gruenewald et al., 2012), reported chronic diseases (Ferraro, Schafer, & Wilkinson, 2016), and diabetes (Tsenkova, Pudrovska, & Karlamangla, 2014).
Education
Level of education was measured by asking participants to report their highest level of education on a 12-level scale (1 = no school/some grade school, 5 = graduated from high school, 9 = graduated with bachelor’s degree, 12 = PhD, EdD, MD, JD). Participants’ responses were transformed into no bachelor’s degree (coded as 0) and bachelor’s degree and above (coded as 1). Almost half of the participants (49.9%) reported that they had at least a bachelor’s degree.
Adult SES
Adult SES was measured using four indicators: (a) household-size adjusted income to poverty ratio (0 = less than 300%, 1 = more than or equal to 300% but less than 600%, 2 = more than equal to 600%), (b) current financial situation (0 = worse, 1 = average, 2 = best), (c) availability of money to meet basic needs (0 = not enough money, 1 = just enough money, 2 = more money than need), and (d) difficulty level paying bills (0 = very/somewhat difficult, 1 = not very difficult, 2 = not at all difficult). The mean adult SES score was 3.80 (SD = 2.31, median = 4, minimum–maximum = 0–8). This set of adulthood SES measures has been a significant predictor of health outcomes in adulthood, such as allostatic load (Gruenewald et al., 2012) and diabetes (Tsenkova et al., 2014).
Other Demographic Variables
Age (in years), gender (0 = female, 1 = male), and race (1 = White, 0 = others) were used as additional covariates to predict individual differences in each outcome variable given previous reports of their effects on the accumulation of risks or opportunities across the life course (Ferraro, Shippee, & Schafer, 2009).
Analysis
This article models the linkages of life course SES with daily stressor exposure, daily stressor severity, and daily well-being. Our analyses also include testing multiple pathways to test the two competing hypothetical models. MSEM is an appropriate and innovative method to test these hypotheses. Combining the strengths of multilevel modeling and structural equation modeling, MSEM partitions nested data into within- and between-person components, incorporates multivariate information by modeling means and variance–covariance structures of the data, and simultaneously test measurement models of latent variables and relations among the latent variables (Heck & Thomas, 2015; Mehta & Neale, 2005).
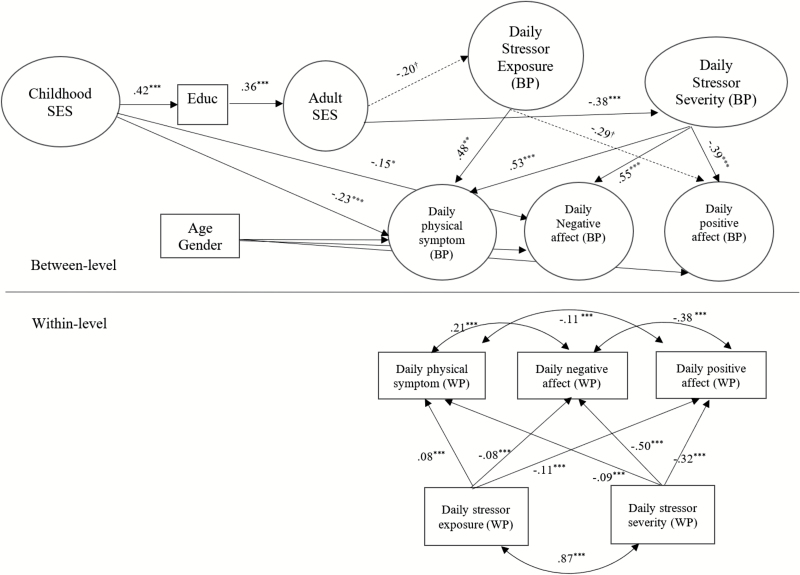
We tested our hypothetical models (Figure 1) using a series of two-level MSEMs, one variation is shown in Figure 2 (the final model). Level 1 of the models explains within-person associations among daily-level variables, including daily stressor exposure, daily stressor severity, daily physical symptoms, daily negative affect, and daily positive affect. Parameter estimates from Level 1 help answer questions such as on the days on which individuals reported high (relative to their latent, person-specific means) daily stressor exposure and daily stressor severity, did they tend to report high (relative to their latent, person-specific means) daily physical symptoms, daily negative affect, and low daily positive affect?
Figure 2.
Final model, chain of risk additive model of life course SES, daily stressors, and daily well-being. BP = between person, WP = within person. Rectangular shapes indicate observed variables; oval shapes indicate latent variables. *p < .05; **p < .01; ***p < .001; †p < .10.
Level 2 of the MSEMs serves to delineate the links among between-person predictor variables and individuals’ latent person-specific means of physical symptoms, negative affect, and positive affect across the 8 days of the study (Lüdtke, Marsh, Robitzsch, & Trautwein, 2011; Lüdtke et al., 2008; Marsh et al., 2009). These latent person-specific means may be regarded as individuals’ overall stress exposure and severity and overall levels on those three well-being variables (we refer to them as between-person daily stressor exposure, between-person daily stressor severity, between-person daily physical symptoms, between-person daily positive affect, and between-person daily negative affect), and have been shown in the past to produce a more accurate representation (i.e., lower biases) as estimates of individuals’ true underlying means that observed aggregates of daily variable scores over time (Lüdtke et al., 2008, 2011; Marsh et al., 2009). Between-person variables used to predict individual differences in Level-2 well-being include childhood SES, education, adult SES, and other demographic variables (age, gender, and race).
Level 2 provides a proxy for testing targeted aspects of the two chain of risk models. MSEM motivated directly by the chain of risk trigger effect model and the additive model are denoted herein as MSEM A and MSEM B (see Figure 1). Thus, under MSEM A, for instance, participants with low adult SES would tend to report heightened levels of between-person daily stressor exposure and severity compared with other participants in the sample. Furthermore, under MSEM A, there were no direct paths from distal risk factors (life course SES) to any of the three latent well-being variables at Level 2. In contrast, MSEM B, as a proxy for testing the chain of risk additive model, differed from MSEM A only in the inclusion of direct paths from all distal risk factors (life course SES) to those three latent well-being variables at Level 2. Thus, MSEM B postulates, for instance, that among individuals with the same levels of between-person daily stressor exposure and severity, individuals with low childhood SES would tend to report higher between-person negative affect, higher between-person physical symptoms, and lower between-person positive affect than those with high childhood SES (Figure 1).
Required pre-analysis steps were performed, including extensive data assessment and cleaning, missing data analysis, and assessment of the measurement model (Leedahl, Chapin, & Little, 2015). All latent constructs in this analysis (childhood SES and adult SES) were between level, and thus, we conducted a one-level confirmatory factor analysis (CFA) to assess the measurement model. Due to missing data and some concerns of normality (especially for the outcome variables), we utilized robust maximum likelihood estimation, which is the default setting in MPlus (Heck & Thomas, 2015; Muthén & Muthén, 2012). The accuracy and fit of the models were assessed using multiple criteria, including (a) multiple fit indices to evaluate overall goodness of fit; (b) assessing whether there were localized areas of strain in the solution, and (c) magnitude, statistical significance, and the interpretability of the model’s parameter estimates (Heck & Thomas, 2015; Leedahl et al., 2015). All analyses were conducted using MPlus version 7.3 (Muthén & Muthén, 2012).
We first examined the goodness of fit of a CFA model in which four observed indicators were used, respectively, to identify two latent factors: childhood SES and adult SES. The final CFA model fulfilled overall goodness-of-fit criteria (χ2 = 470.88, df = 19, χ2/df = 24.78, p < .001; RMSEA = 0.06; CFI = 0.95; TLI = 0.93; SRMR = 0.04). The standardized factor loadings across all latent constructs ranged from .37 to .81, exceeding the cutoff of 0.30 (Floyd & Widaman, 1995). MSEMs A and B, based on the same measurement model, were then estimated. Indirect effects in each model and their associated statistical significance (e.g., the indirect effect from childhood SES to overall physical symptoms) were tested using the MODEL INDIRECT command (Muthén & Muthén, 2012). The estimates reported are based on the standardized results.
Results
The average cluster size for MSEM A was 7.45, with intraclass correlations ranging from .16 to .76. Thus, the design effect for the outcomes ranged from 2.0 to 5.9, confirming the need to account for the within-person associations in the data. The model showed overall acceptable goodness-of-fit criteria (see Table 2). Assessment of parameter estimates indicated that all the hypothesized paths of chain of risk were significant, except that adult SES was only marginally associated with daily stressor exposure (p < .10). MSEM B yielded similar design effect values and goodness-of-fit values (see Table 2). Likelihood ratio test was used to compare the change in fit from MSEM B to MSEM A. When additional direct paths from MSEM B were omitted to yield MSEM A, significant decrement in fit was observed (χ2diff = 31.77, dfdiff = 9, p < .001).
Table 2.
Model Fit Indices for Comparison of MSEMs
| Model | χ2 | df | p | RMSEA | CFI | TLI | SRMR-W | SRMR-B | AIC | BIC | Adj-BIC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement model | 470.88 | 19 | <.001 | 0.06 | 0.95 | 0.93 | 0.04a | 83,873.14 | 84,039.99 | 83,960.55 | |
| Hypothesized trigger effect model (MSEM A in Figure 1) | 863.79 | 103 | <.001 | 0.04 | 0.93 | 0.90 | 0.02 | 0.11 | 57,288.25 | 57,775.05 | 57,543.08 |
| Hypothesized additive model (MSEM B in Figure 1) | 832.02 | 94 | <.001 | 0.04 | 0.93 | 0.90 | 0.02 | 0.11 | 57,254.84 | 57,801.66 | 57,541.09 |
| Final model (Figure 2) | 812.88 | 90 | <.001 | 0.04 | 0.93 | 0.90 | 0.02 | 0.11 | 57,683.77 | 58,164.30 | 57,935.51 |
Note: χ2 = chi-square test of model fit; adj-BIC = sample-size adjusted Bayesian information criterion; AIC = Akaike’s information criterion; BIC = Bayesian information criterion; CFI = comparative fit index; df = degree of freedom for the chi-square test of model fit; MSEM = multilevel structural equation modelling; p = p-value for the chi-square test of model fit; RMSEA = root mean square error of approximation; SRMR-B = standardized root mean square residual for between level; SRMR-W = standardized root mean square residual for within level; TLI = Tucker–Lewis index.
aMeasurement model only has one value of standardized root mean square residual.
A final modified version of the hypothesized additive model in which only the significant paths were retained is included (Figure 2). The within-level part of the final MSEM model indicated that at the day level, the days on which individuals experience higher stressors compared with their person-specific means were associated with higher daily positive affect, lower level of daily negative affect, and higher number of daily physical symptoms. In addition, higher daily stressor severity was associated with lower daily positive affect, higher daily negative affect, and higher daily physical symptoms.
Assessment of parameter estimates at Level 2 indicated that all the hypothesized direct paths of additive risk were significant with the following exceptions (see Figure 2): (a) adult SES was only marginally associated with between-person daily stressor exposure; (b) childhood SES was only directly associated with between-person daily physical symptoms and daily negative affect, but not between-person daily positive affect; and (c) education and adult SES were not directly associated with any of the three Level-2 well-being variables (see Figure 2).
Sensitivity Analysis
We conducted sensitivity analysis for both the measurement and structural models. We removed one random observed variable for both childhood SES and adult SES factors to test the robustness of our measurement model. We removed overall positive affect from the structural model to test the robustness of the final model. In general, substantive conclusions remained largely the same. Childhood SES directly predicted daily negative affect and daily physical symptoms. In addition, daily stressor severity was a better predictor of daily well-being than exposure. The results of our sensitivity analysis indicated that the proposed model yielded results that were robust to minor changes to the measurement and structural models.
Discussion
This article is among the first to investigate the chain of risk of life course SES, daily stressor exposure and severity, and daily well-being. In addition, this article is intended to investigate the direct and indirect influence of childhood SES on daily positive affect, daily negative affect, and daily physical symptoms. We found that childhood SES links to education and that education, in turn, links to adult SES. The results also support previous findings that adult SES is associated with severity of daily stressors, but not daily stressor exposure (Almeida et al., 2005; Grzywacz et al., 2004). We also found that daily stressor severity is a better predictor of daily well-being compared with daily stressor exposure. Furthermore, we found that childhood SES was directly associated with between-person levels of daily physical and psychological well-being, especially daily physical symptoms and daily negative affect. Childhood SES was also indirectly associated with overall well-being through the chain of risk of life course SES and daily stressor exposure and severity.
Findings from this article extend the literature of socioeconomic disparities in health and stress in several ways. First, this article complemented other findings regarding the “long arm” of early-life conditions on adult health. This article is among the first to show that childhood SES has a direct influence on day-to-day well-being. Childhood may be a sensitive period that has salient implications for daily well-being in adulthood. On the other hand, another study has shown a less powerful influence of childhood SES relative to adult SES on influencing health in later life (Marmot et al., 2001). These mixed results may be due to differences in the health outcomes being analyzed or due to structural differences between the United Kingdom (where the study by Marmot et al. was conducted) and the United States (this study), especially with respect to the availability of universal health care and social welfare programs for low-income families in the United Kingdom.
This study adds to the knowledge that early-life SES indirectly links to daily between-person psychosocial demands and well-being through the chain of risk of life course SES. The indirect link between childhood SES and day-to-day well-being is especially associated with stressor severity. Although proximal SES (adult SES) was not associated with between-person daily stressor exposure, individuals from lower levels of adult SES reported higher levels of between-person daily stressor severity (Almeida et al., 2005; Grzywacz et al., 2004). These results suggest that daily stressor severity matters more than exposure to daily stressors in explaining socioeconomic disparities in daily well-being (Almeida et al., 2005; Grzywacz et al., 2004). Grzywacz and colleagues (2004) have speculated that daily stressor exposure is not significantly linked to SES differentials in daily well-being for the following reasons: (a) the chronic stressors that are experienced by lower SES individuals may desensitize their experience to minor day-to-day stressors (although in this study we controlled for life course SES that may reflect chronic socioeconomic hardships); (b) the possibility of gender and race on masking the systematic variation in exposure to daily stressors; and (c) the possibility that lower SES individuals are less reflective and articulate on reporting daily stressors. It is also possible that lower SES individuals encounter similar types of daily stressors, indicating a low number of daily stressors encountered and lower levels of daily stressor diversity. A previous study found that lower levels of daily stressor diversity are associated with lower levels of daily well-being (Koffer, Ram, Conroy, Pincus, & Almeida, 2016). Future studies should consider including stressor diversity when studying the influence of daily stress exposure on socioeconomic disparities in daily well-being.
Third, we demonstrate that, in between-person level, childhood SES directly associates with daily physical symptoms and daily negative affect, but not with daily positive affect. These results may have important public health implications, given that previous studies have shown that higher daily physical symptoms and negative affect due to daily stressors are associated with long-term health outcomes such as chronic physical and psychological distress (Charles et al., 2013; Piazza et al., 2013), functional impairment (Leger et al., 2015), and mortality risk (Chiang et al., 2018). In addition, studies on the influence of childhood SES on daily biological functioning in later life (e.g., alterations in autoimmune and endocrine regulation) have shown the importance of daily stress processes and daily well-being as possible mechanisms of disparities in chronic diseases (Carroll et al., 2011; Desantis et al., 2015; Miller et al., 2011). Future studies should prioritize examination of the linkages among childhood SES, daily stressors, daily well-being, daily biological functioning, and long-term health outcomes simultaneously.
Finally, this study utilized multiple indicators of SES across the life course, incorporating both subjective and objective measures as recommended by several scholars (Adler & Tan, 2017; Braveman et al., 2005; Shavers, 2007). These measures of SES have been shown as predictors of several health outcomes, including allostatic load, diabetes, and other chronic diseases (Ferraro et al., 2016; Friedman et al., 2015; Gruenewald et al., 2012; Tsenkova et al., 2014). However, results from this study are unable to explain specific roles of objective and subjective SES measures on health outcomes. Previous studies have found that subjective SES is a better predictor of general health compared with objective measures of SES (Adler, Epel, Castellazzo, & Ickovics, 2000; Singh-Manoux, Marmot, & Adler, 2005). Future studies should investigate the unique contribution of subjective and objective measures of SES across the life course on day-to-day health and well-being.
Strengths and Limitations
This article presents a multilevel structural equation modeling (MSEM) approach to simultaneously investigate within-person links among childhood SES, daily stressor exposure and severity, and daily well-being, as well as between-person differences in such links. The MSEM method partitions variance of nested data into within- and between-person and also has the ability to incorporate measurement models and pathway analyses simultaneously. As stated previously, this article also incorporated multiple indicators to measure childhood and adult SES, combining both subjective and objective indicators. Finally, this study incorporated three measures of daily well-being and analyzed them simultaneously, minimalizing the symptom perception bias (Leger et al., 2015).
In light of these strengths, this article also has several limitations. First, life course data for the analyses were collected using a retrospective cross-sectional research design. Other research on life course epidemiology using prospective data, for example, Marmot and colleagues (2001), shows the limited role of childhood SES and supports the chain of risk trigger effect model. Thus, future replication is needed using longitudinal data to test whether the links between life course socioeconomic hardships and daily well-being still follow the chain of risk additive model. Second, participants in this sample did not reflect the national distribution of the U.S. population, especially in terms of racial and socioeconomic composition. Future replication is required to explore the chain of risk models among a more nationally representative population in terms of race and SES. Third, our analyses excluded other types of early-life hardship such as early traumatic experiences (e.g., child abuse), which have been shown to be important predictors of health in later life (Springer, 2009). Fourth, our analyses did not incorporate the timing and duration of hardships, which are also important predictors of health in adulthood (Friedman, Montez, Sheehan, Guenewald, & Seeman, 2015). Fifth, our model is unable to explain the interindividual variability regarding mobility of SES across the life course and the influence of education, personality, and resiliency on buffering life course hardships. Luo and Waite (2005) found that one fifth of participants in their sample experienced SES mobility (upward or downward).
Finally, there are several potential constraints of the SES measures used in this study. The measure about parental employment status does not distinguish part-time or full-time employment status, number of jobs held, or spells of unemployment. The item regarding family welfare receipt may be biased toward single mother households. Thus, instead of a reflection of childhood SES, this variable may reflect participants’ experience of growing up in a single-parent household. In addition, participants’ answers to questions about their financial situation may depend on social comparison, which may depend on neighborhood-level SES. These limitations may lead to biased estimation of the influence of childhood SES on daily well-being. Replications are needed to test the consistency of these results using different data sets. In addition, more studies are needed to investigate the validity of these childhood SES measures.
Conclusion
In summary, the current study adds to the knowledge of the “long arm” of early-life influence on later-life daily well-being. We demonstrated that life course SES and daily stressor exposure and severity predict daily well-being and fit the chain of risk additive model. We found that childhood may be a sensitive period that has salient implications for day-to-day well-being later in life directly and indirectly through daily stressor severity.
Funding
This work was supported by the National Institute on Aging (grant numbers P01-AG020166 and U19-AG051426) and previously by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development.
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
A. Surachman performed all statistical analyses and wrote the article. B. Wardecker contributed to write and revise the article. S.-M. Chow supervised the data analysis and contributed to revise the article. D. M. Almeida planned the study, supervised the data analysis, and contributed to revise the article.
References
- Adler N. E., Epel E. S., Castellazzo G., & Ickovics J. R (2000). Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, white women. Health Psychology, 19, 586. doi:10.1037/ 0278-6133.19.6.586 [DOI] [PubMed] [Google Scholar]
- Adler N. E., & Tan J. J (2017). Tackling the health gap: The role of psychosocial processes. International Journal of Epidemiology, 46, 1329–1331. doi:10.1093/ije/dyx167 [DOI] [PubMed] [Google Scholar]
- Almeida D. M. (2005). Resilience and vulnerability to daily stressors assessed via diary methods. Current Directions in Psychological Science, 14, 64–68. doi:10.1111/j.0963-7214.2005.00336.x [Google Scholar]
- Almeida D. M., Neupert S. D., Banks S. R., & Serido J (2005). Do daily stress processes account for socioeconomic health disparities?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, S34–S39. doi:10.1093/geronb/60.Special_Issue_2.S34 [DOI] [PubMed] [Google Scholar]
- Almeida D. M., Piazza J. R., Stawski R. S., & Klein L. C (2011). The speedometer of life: Stress, health, and aging. In K. W. Schaie & R. Levey (Eds.), Handbook of aging (pp. 191–206). New York, NY: Elsevier. [Google Scholar]
- Almeida D. M., Stawski R. S., & Cichy K. E (2011). Combining checklist and interview approaches for assessing daily stressors: The Daily Inventory of Stressful Events. In R. J., Contrada A., Baum (Eds.), The handbook of stress science: Biology, psychology, and health (pp. 583–595). New York: Springer. [Google Scholar]
- Almeida D. M., Wethington E., & Kessler R. C (2002). The daily inventory of stressful events: An interview-based approach for measuring daily stressors. Assessment, 9, 41–55. doi:10.1177/1073191102009001006 [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y., Mishra G., & Kuh D (2014). Life course epidemiology. In W. Ahrens & I. Pigeot (Eds.), Handbook of epidemiology (2nd ed., pp. 1521–1549). New York, NY: Springer. [Google Scholar]
- Berkman L. F. (2009). Social epidemiology: Social determinants of health in the United States: Are we losing ground?Annual Review of Public Health, 30, 27–41. doi:10.1146/annurev.publhealth.031308.100310 [DOI] [PubMed] [Google Scholar]
- Braveman P. A., Cubbin C., Egerter S., Chideya S., Marchi K. S., Metzler M., & Posner S (2005). Socioeconomic status in health research: One size does not fit all. JAMA, 294, 2879–2888. doi:10.1001/jama.294.22.2879 [DOI] [PubMed] [Google Scholar]
- Carroll J. E., Cohen S., & Marsland A. L (2011). Early childhood socioeconomic status is associated with circulating interleukin-6 among mid-life adults. Brain, Behavior, and Immunity, 25, 1468–1474. doi:10.1016/j.bbi.2011.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles S. T., Piazza J. R., Mogle J., Sliwinski M. J., & Almeida D. M (2013). The wear and tear of daily stressors on mental health. Psychological Science, 24, 733–741. doi:10.1177/ 0956797612462222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R., Hendren N., Kline P., Saez E., & Turner N (2014). Is the United States still a land of opportunity? Recent trends in intergenerational mobility. The American Economic Review, 104, 141–147. doi:10.1257/aer.104.5.141 [Google Scholar]
- Chiang J. J., Turiano N. A., Mroczek D. K., & Miller G. E (2018). Affective reactivity to daily stress and 20-year mortality risk in adults with chronic illness: Findings from the national study of daily experiences. Health Psychology, 37, 170–178. doi:10.1037/hea0000567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cichy K. E., Stawski R. S., & Almeida D. M (2012). Racial differences in exposure and reactivity to daily family stressors. Journal of Marriage and Family, 74, 572–586. doi:10.1111/ j.1741-3737.2012.00971.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desantis A. S., Kuzawa C. W., & Adam E. K (2015). Developmental origins of flatter cortisol rhythms: Socioeconomic status and adult cortisol activity. American Journal of Human Biology, 27, 458–467. doi:10.1002/ajhb.22668 [DOI] [PubMed] [Google Scholar]
- Ferraro K. F., Schafer M. H., & Wilkinson L. R (2016). Childhood disadvantage and health problems in middle and later life: Early imprints on physical health?American Sociological Review, 81, 107–133. doi:10.1177/0003122415619617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro K. F., Shippee T. P., & Schafer M. H (2009). Cumulative inequality theory for research on aging and the life course. In V. L. Bengtson M. Silverstein N. M. Putney, & D. Gans (Eds.), Handbook of theories of aging (pp. 413–433). New York, NY: Springer. [Google Scholar]
- Floyd F. J., & Widaman K. F (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment, 7, 286. doi:10.1037/ 1040-3590.7.3.286 [Google Scholar]
- Friedman E. M., Karlamangla A. S., Gruenewald T., Koretz B., & Seeman T. E (2015). Early life adversity and adult biological risk profiles. Psychosomatic Medicine, 77, 176–185. doi:10.1097/PSY.0000000000000147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman E. M., Montez J. K., Sheehan C. M., Guenewald T. L., & Seeman T. E (2015). Childhood adversities and adult cardiometabolic health: Does the quantity, timing, and type of adversity matter?Journal of Aging and Health, 27, 1311–1338. doi:10.1177/0898264315580122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald T. L., Karlamangla A. S., Hu P., Stein-Merkin S., Crandall C., Koretz B., & Seeman T. E (2012). History of socioeconomic disadvantage and allostatic load in later life. Social Science & Medicine, 74, 75–83. doi:10.1016/j.socscimed.2011.09.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzywacz J. G., Almeida D. M., Neupert S. D., & Ettner S. L (2004). Socioeconomic status and health: A micro-level analysis of exposure and vulnerability to daily stressors. Journal of Health and Social Behavior, 45, 1–16. doi:10.1177/002214650404500101 [DOI] [PubMed] [Google Scholar]
- Heck R. H., & Thomas S. L (2015). An introduction to multilevel modeling techniques: MLM and SEM approaches using Mplus (3rd ed.). New York, NY: Routledge. [Google Scholar]
- Kessler R. C., Andrews G., Colpe L. J., Hiripi E., Mroczek D. K., Normand S. L.,…Zaslavsky A. M (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32, 959–976. doi:10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- Kirsch J. A., & Ryff C. D (2016). Hardships of the great recession and health: Understanding varieties of vulnerability. Health Psychology Open, 3, 2055102916652390. doi:10.1177/2055102916652390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffer R. E., Ram N., Conroy D. E., Pincus A. L., & Almeida D. M (2016). Stressor diversity: Introduction and empirical integration into the daily stress model. Psychology and Aging, 31, 301. doi:10.1037/pag0000095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leedahl S. N., Chapin R. K., & Little T. D (2015). Multilevel examination of facility characteristics, social integration, and health for older adults living in nursing homes. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 111–122. doi:10.1093/geronb/gbu112 [DOI] [PubMed] [Google Scholar]
- Leger K. A., Charles S. T., Ayanian J. Z., & Almeida D. M (2015). The association of daily physical symptoms with future health. Social Science & Medicine, 143, 241–248. doi:10.1016/ j.socscimed.2015.08.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüdtke O., Marsh H. W., Robitzsch A., & Trautwein U (2011). A 2 × 2 taxonomy of multilevel latent contextual models: Accuracy–bias trade-offs in full and partial error correction models. Psychological Methods, 16, 444. doi:10.1037/a0024376 [DOI] [PubMed] [Google Scholar]
- Lüdtke O., Marsh H. W., Robitzsch A., Trautwein U., Asparouhov T., & Muthén B (2008). The multilevel latent covariate model: A new, more reliable approach to group-level effects in contextual studies. Psychological Methods, 13, 203. doi:10.1037/a0012869 [DOI] [PubMed] [Google Scholar]
- Luo Y., & Waite L. J (2005). The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60, S93–S101. doi:10.1093/geronb/60.2.S93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M., Shipley M., Brunner E., & Hemingway H (2001). Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. Journal of Epidemiology & Community Health, 55, 301–307. doi:10.1136/jech.55.5.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh H. W., Lüdtke O., Robitzsch A., Trautwein U., Asparouhov T., Muthén B., & Nagengast B (2009). Doubly-latent models of school contextual effects: Integrating multilevel and structural equation approaches to control measurement and sampling error. Multivariate Behavioral Research, 44, 764–802. doi:10.1080/00273170903333665 [DOI] [PubMed] [Google Scholar]
- Mehta P. D., & Neale M. C (2005). People are variables too: Multilevel structural equations modeling. Psychological Methods, 10, 259. doi:10.1037/1082-989X.10.3.259 [DOI] [PubMed] [Google Scholar]
- Miller G. E., Chen E., & Parker K. J (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137, 959. doi:10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek D. K., & Kolarz C. M (1998). The effect of age on positive and negative affect: A developmental perspective on happiness. Journal of Personality and Social Psychology, 75, 1333. doi:10.1037/0022-3514.75.5.1333 [DOI] [PubMed] [Google Scholar]
- Mroczek D. K., Stawski R. S., Turiano N. A., Chan W., Almeida D. M., Neupert S. D., & Spiro A. III (2015). Emotional reactivity and mortality: Longitudinal findings from the VA normative aging study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 398–406. doi:10.1093/geronb/gbt107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O (2012). Mplus version 7 user’s guide. Los Angeles, CA: Author. [Google Scholar]
- Piazza J. R., Charles S. T., Sliwinski M. J., Mogle J., & Almeida D. M (2013). Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine, 45, 110–120. doi:10.1007/s12160-012-9423-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis H. T., Sheldon K. M., Gable S. L., Roscoe J., & Ryan R. M (2000). Daily well-being: The role of autonomy, competence, and relatedness. Personality and Social Psychology Bulletin, 26, 419–435. doi:10.1177/0146167200266002 [Google Scholar]
- Schoorlemmer R. M., Peeters G. M., van Schoor N. M., & Lips P (2009). Relationships between cortisol level, mortality and chronic diseases in older persons. Clinical Endocrinology, 71, 779–786. doi:10.1111/j.1365-2265.2009.03552.x [DOI] [PubMed] [Google Scholar]
- Shavers V. L. (2007). Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association, 99, 1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Sin N. L., Graham-Engeland J. E., Ong A. D., & Almeida D. M (2015). Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychology, 34, 1154–1165. doi:10.1037/hea0000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A., Marmot M. G., & Adler N. E (2005). Does subjective social status predict health and change in health status better than objective status?Psychosomatic Medicine, 67, 855–861. doi:10.1097/01.psy.0000188434.52941.a0 [DOI] [PubMed] [Google Scholar]
- Springer K. W. (2009). Childhood physical abuse and midlife physical health: Testing a multi-pathway life course model. Social Science & Medicine, 69, 138–146. doi:10.1016/ j.socscimed.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stawski R. S., Cichy K. E., Piazza J. R., & Almeida D. M (2013). Associations among daily stressors and salivary cortisol: Findings from the national study of daily experiences. Psychoneuroendocrinology, 38, 2654–2665. doi:10.1016/ j.psyneuen.2013.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torche F. (2015). Analyses of intergenerational mobility: An interdisciplinary review. The Annals of the American Academy of Political and Social Science, 657, 37–62. doi:10.1177/0002716214547476 [Google Scholar]
- Tsenkova V., Pudrovska T., & Karlamangla A (2014). Childhood socioeconomic disadvantage and prediabetes and diabetes in later life: A study of biopsychosocial pathways. Psychosomatic Medicine, 76, 622–628. doi:10.1097/PSY.0000000000000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.