Abstract
G4C14-A4T14 polymorphism of TP73 gene has been reported with a potential association in cancer risks through affected cell homeostasis; however the results were not consistent. We performed a comprehensive meta-analysis to explore the associations between G4C14-A4T14 polymorphism and cancer susceptibility. Extensive retrieve was performed in PubMed, EMBASE, Google Scholar, Web of Science, Wanfang database and CNKI database up to May 20, 2018. Odds ratios (ORs) and 95% confidence intervals (CIs) were conducted to evaluate the overall strength of the associations in five genetic models, as well as in subgroup analyses. Q-test, false-positive report probability analysis and trial sequential analysis, Egger’s test and Begg’s funnel plot were applied to evaluate the robustness of the results. In silico analysis was managed to demonstrate the relationship of TP73 expression correlated with cancer tissues. Finally, 36 case–control studies with a total of 9493 cancer cases and 13,157 healthy controls were enrolled into the meta-analysis. The pooled results present a significantly higher risk of G4C14-A4T14 polymorphism in all the five genetic models, as well as in the subgroups of Caucasian, cervical cancer, colorectal cancer, H-B subgroup and comfort to Hardy–Weinberg equilibrium subgroup. In silico analysis revealed that the expression of TP73 in cervical cancer tissue is higher than it in corresponding normal tissue, as well as in cervical cancer. All in all, TP73 G4C14-A4T14 polymorphism causes an upgrade cancer risk, especially in Caucasian population. G4C14-A4T14 polymorphism might be a potential biomarker for judging the tumorigenesis of cervical cancer and colorectal cancer.
Keywords: cancer, genetic variation, G4C14-A4T14, meta-analysis, polymorphism, tumor protein P73
Introduction
Cancer is a pivotal public health and leads to the second cause of death problem around the world. In 2018, there are almost 4700 new cancer diagnoses per day, as well as about 1700 cancer-related deaths in United States [1]. Breast cancer, lung cancer and colorectal cancer are the most three frequently cancer of female in United States, while prostate cancer occupied the first diagnosis cancer in male [1]. Attributed to the increasing population growth and aging, cancer has also been the leading cause of death around China. In 2015, there are about 12,000 newly diagnosed invasive cancer cases on average per day, while over 7500 cancer death [2]. In the past decades, biological scientists have reported that environmental factors, genetic mutations and the multiple interactions between them mainly affect the process of tumorigenesis, and the new research results are also on the road, such as epigenetic control [3–5].
Tumor protein P73 (TP73), also known as P53-like transcription factor, is a pivotal member of TP53 family, which affects cell proliferation, apoptosis and cell-cycle regulation [6–8]. Compared with frequently mutant TP53 gene, TP73 is rarely mutated [9]. p73 protein, the encoded product of TP73, is homologous with p53, 63% of p73 has the same amino acid sequence with p53, so it plays a critical role in normal cell homeostasis, while it can partially compensate the loss of p53 protein function [10,11].
G4A (rs2273953) and C14T (rs1801173), the two single-nucleotide polymorphisms (SNPs) of TP73 at positions 4 (G>A) and 14 (C>T), are incomplete linkage disequilibrium with each other, so we called it as G4C14-A4T14. G4C14-A4T14 is located at the upstream of TP73 promoter in exon 2, it could influence the expression of TP73 through a stem–loop structure [12,13]. In recent years, G4C14-A4T14 polymorphism of TP73 was identified implicated in the tumorigenesis of a variety of cancer types, including breast cancer, colorectal cancer, lung cancer, cervical cancer, esophageal cancer and so on [14–17]. Nevertheless, data arising from these published case–control studies were not consistent. One single study may have no sufficient power to identify slight influences of these polymorphisms on cancer susceptibility. Therefore, we conducted a comprehensive meta-analysis to explore the association between G4C14-A4T14 polymorphism and cancer susceptibility.
Materials and methods
Literature search and study selection criteria
We conducted a comprehensive literature search from PubMed, EMBASE, Google Scholar, Web of Science, Wanfang database and CNKI database (up to May 20, 2018). The keywords applied to literature retrieve are as follows: “TP73 OR (Tumor Protein P73) OR (P53-Like Transcription Factor)” AND “cancer OR carcinoma OR tumor OR tumor OR neoplasm.” AND “SNP OR mutation OR variant OR polymorphism”. Furthermore, the references from eligible studies were manually checked for additional relevant literature. The titles and abstracts of identifying studies were examined to exclude obvious irrelevant records. The full-text of the remaining articles was further carefully inspected to determine whether to report the correlation of between G4C14-A4T14 polymorphism and cancer susceptibility.
All the eligible studies should fulfill the following inclusion criteria: (1) case–control studies focus on the correlation between G4C14-A4T14 polymorphism and cancer susceptibility; (2) genotype frequency of the cases and controls could be obtained directly or indirectly through calculation; and (3) articles in English or Chinese. On the contrary, studies would be removed if they were: (1) case–report, meta-analysis, systematic review or repetitive publication; (2) lack of genotype frequency data; and (3) publications conducted on animals or cell lines.
Data extraction
Two independent investigators separately extracted the relative data with any disagreement resolved by rechecking and discussion. For every eligible study, the following data were extracted: the name of the first author, the data of publication, ethnicity, sample size, genotyping methods, and genotype frequency of the cases and controls. In the subgroup analysis by race, the Caucasian population typically lived in Europe or America, and the Asian population typically lived in Asia.
Statistical methods
All the statistical calculation was conducted with STATA 12.0 software (Stata, College Station, Texas) in the present study. ORs with corresponding 95% CIs were performed to measure the strength of the relationship between G4C14-A4T14 polymorphism and cancer susceptibility. Five common genetic models applied for assessing gene–disease associations are allele contrast model (GC vs. AT), homozygote comparison model (GC/GC vs. AT/AT), heterozygote comparison model (GC/AT vs. AT/AT), dominant comparison model (GC/GC+GC/AT vs. AT/AT) and recessive comparison model (GC/GC vs. GC/AT+AT/AT) (AT/AT, homozygotes for the common allele; GC/AT, heterozygotes; GC/GC, homozygotes for the rare allele). Stratified analyses were also calculated by ethnicity, cancer type and the source of control. In addition, we applied the chi-squared (χ2)-based Q-test to calculate between-study heterogeneity [18]. P<0.1 was indicated as a substantial level of heterogeneity, and a random-effects model (the DerSimonian and Laird method) was selected to pool the data [19]; or else, the fixed-effects model (the Mantel–Haenszel method) was adopted. Moreover, we also conducted the Begg’s funnel plots and Egger’s test to evaluate the publication bias [20,21]. Hardy–Weinberg equilibrium (HWE) of controls was calculated by the χ2 test to compare the expected and actual genotype frequencies among the controls in each study. All the statistical tests in this meta-analysis were two-tailed, and P-values ≤ 0.05 were considered statistically significant.
False-positive report probability analysis and trial sequential analysis
We also use the false-positive report probability (FPRP) method to evaluate the results. 0.2 was set as an FPRP threshold and assigned a prior probability of 0.1 to detect the odds ratio (OR) of 0.67/1.50 (protective/risk effects). The significant result with the FPRP values less than 0.2 was considered as a worthy finding [22,23]. Trial sequential analysis (TSA) was conducted with the guideline of a former publication. We set a significance of 5% for type I error, as well as a 30% significance of type II error, to calculate the required sample size, and built the TSA monitoring boundaries.
In silico analysis of TP73 expression
In order to further explore the relationship between TP73 expression and cancer, we used a newly developed interactive web server, GEPIA (http://gepia.cancer-pku.cn/), to see the difference between tumor tissue and normal tissue. GEPIA provided the mRNA sequencing expression data of tumors and normal samples from the TCGA and the GTEx projects [24].
Results
Study characteristics
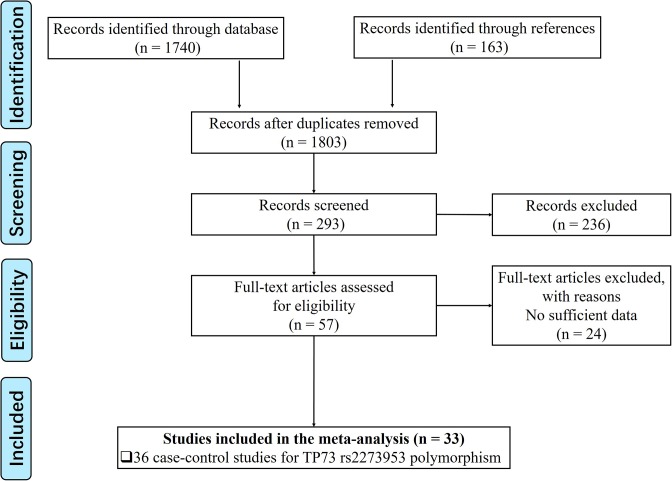
As shown in Figure 1, we found 1740 potentially relevant studies from PubMed, EMBASE, Google Scholar, Web of Science, Wanfang database and CNKI database. After reviewing titles and abstracts, we excluded 1537 publications not investigating the association between TP73 G4C14-A4T14 polymorphism and cancer risk. And then, full texts of remaining articles were evaluated. In the end, 36 case–control studies with a total of 9493 cancer cases and 13,157 healthy controls were enrolled into the meta-analysis [14–17,25–53]. The characteristics of these studies were showed in Table 1. Among these publications, there are 6 concerned about cervical cancer [17,34,40,50–52], 5 about lung cancer [16,29,33,35,38], 4 about colorectal cancer [28,37,46,47], 4 about esophageal cancer [14,27,28,39], 4 about gastric cancer [28,39,43,48], 3 about breast cancer [15,26,30], 3 about squamous cell carcinoma of the head and neck [32,41,45], as well as other 7 publications focus on Endometrial cancer [36], lymphoma [31], melanoma [42], nasopharyngeal carcinoma [53], neuroblastoma [25], ovarian cancer [44] and prostate cancer [49], respectively. As to the ethnicity, 14 studies were performed in Caucasians, while the other 22 studies were managed in Asian population. The characteristics of each case–control study, genotype frequencies and HWE examination results were presented in Table 1. Four case–control studies were not comforted to HWE [16,32,37,45], and we further conducted a sensitive analysis to validate the influence of the three studies on the integrated data. In order to evaluate the quality of each enrolled studies, we applied Newcastle–Ottawa Scale (NOS) [45] and fill the result in Table S1, the result of PRISMA2009 checklist was also listed to present our meta-analysis work (Table S2).
Figure 1. Flowchart presenting the study selection procedure.
Table 1. Characteristics of the enrolled studies on TP73 G4C14-A4T14 polymorphism and cancer.
| First author | Year | Ethnicity | Genotyping method | Source of control | Cancer type | HWE | Case | Control | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PAA | PAB | PBB | HAA | HAB | HBB | |||||||
| Romain et al. | 1999 | Caucasian | PCR | P-B | Neuroblastoma | Y | 31 | 39 | 3 | 94 | 49 | 7 |
| Ahomadegbe et al. | 2000 | Caucasian | PCR | H-B | Breast cancer | Y | 36 | 22 | 1 | 27 | 7 | 0 |
| Ryan et al. | 2001 | Caucasian | PCR | P-B | Esophageal cancer | Y | 42 | 41 | 1 | 72 | 65 | 15 |
| Hamajima et al. | 2002 | Asian | PCR–CTPP | H-B | Esophageal cancer | Y | 67 | 29 | 6 | 133 | 98 | 10 |
| Hamajima et al. | 2002 | Asian | PCR–CTPP | H-B | Gastric cancer | Y | 84 | 51 | 9 | 133 | 98 | 10 |
| Hamajima et al. | 2002 | Asian | PCR–CTPP | H-B | Colorectal cancer | Y | 87 | 50 | 10 | 133 | 98 | 10 |
| Hiraki et al. | 2003 | Asian | PCR–CTPP | H-B | Lung cancer | Y | 109 | 68 | 12 | 130 | 95 | 10 |
| Huang et al. | 2003 | Asian | PCR–CTPP | P-B | Breast cancer | Y | 118 | 64 | 18 | 153 | 112 | 17 |
| Hishida et al. | 2004 | Asian | PCR–CTPP | H-B | Lymphoma | Y | 49 | 43 | 11 | 261 | 152 | 27 |
| Li(a) et al. | 2004 | Caucasian | PCR–CTPP | H-B | SCCHN | N | 399 | 271 | 38 | 773 | 387 | 69 |
| Li(b) et al. | 2004 | Caucasian | PCR | P-B | Lung cancer | Y | 593 | 394 | 67 | 721 | 365 | 53 |
| Niwa(a) et al. | 2004 | Asian | PCR–CTPP | H-B | Cervical cancer | Y | 57 | 52 | 3 | 270 | 150 | 22 |
| Hu et al. | 2005 | Asian | PCR-SSCP | P-B | Lung cancer | Y | 255 | 149 | 21 | 295 | 248 | 45 |
| Niwa(b) et al. | 2005 | Asian | PCR | H-B | Endometrial cancer | Y | 61 | 39 | 14 | 270 | 150 | 22 |
| Pfeifer et al. | 2005 | Caucasian | PCR–RFLP | P-B | Colorectal cancer | N | 113 | 54 | 12 | 159 | 96 | 5 |
| Choi et al. | 2006 | Asian | PCR | P-B | Lung cancer | Y | 320 | 221 | 41 | 338 | 212 | 32 |
| Ge et al. | 2006 | Asian | PCR–RFLP | H-B | Gastric cancer | Y | 146 | 99 | 14 | 391 | 210 | 29 |
| Ge et al. | 2006 | Asian | PCR–RFLP | H-B | Esophageal cancer | Y | 214 | 113 | 21 | 391 | 210 | 29 |
| Zheng et al. | 2006 | Asian | PCR–RFLP | P-B | Cervical cancer | Y | 58 | 22 | 2 | 77 | 19 | 4 |
| Chen et al. | 2008 | Caucasian | PCR–RFLP | P-B | SCCHN | Y | 195 | 111 | 20 | 214 | 115 | 20 |
| Li(c) et al. | 2008 | Caucasian | PCR | H-B | Melanoma | Y | 468 | 287 | 150 | 497 | 302 | 39 |
| Zheng et al. | 2008 | Asian | PCR–CTPP | P-B | Cervical cancer | Y | 71 | 28 | 2 | 77 | 19 | 4 |
| Deo Feo et al. | 2009 | Caucasian | PCR | H-B | Gastric cancer | Y | 84 | 22 | 8 | 214 | 71 | 10 |
| Kang et al. | 2009 | Asian | PCR | P-B | Ovarian cancer | Y | 164 | 74 | 19 | 151 | 92 | 14 |
| Misra et al. | 2009 | Caucasian | PCR | H-B | SCCHN | N | 112 | 176 | 15 | 186 | 124 | 9 |
| Lee et al. | 2010 | Asian | PCR–CTPP | P-B | Colorectal cancer | Y | 183 | 171 | 29 | 271 | 173 | 25 |
| Shirai et al. | 2010 | Asian | PCR–CTPP | H-B | Gastric cancer | Y | 220 | 142 | 26 | 239 | 156 | 24 |
| Arfaoui et al. | 2010 | Caucasian | PCR | P-B | Colorectal cancer | Y | 77 | 47 | 26 | 109 | 73 | 22 |
| Mittal et al. | 2011 | Caucasian | PCR–RFLP | P-B | Prostate cancer | Y | 121 | 56 | 0 | 192 | 66 | 7 |
| Craveiro et al. | 2012 | Caucasian | PCR | P-B | Cervical cancer | Y | 95 | 38 | 8 | 119 | 48 | 9 |
| Sun et al. | 2012 | Asian | PCR–CTPP | P-B | Cervical cancer | Y | 107 | 100 | 11 | 128 | 80 | 12 |
| Umar et al. | 2012 | Caucasian | PCR | P-B | Esophageal cancer | Y | 174 | 70 | 11 | 200 | 51 | 4 |
| Zhou et al. | 2012 | Asian | MALDI-TOF | P-B | Breast cancer | Y | 106 | 59 | 5 | 100 | 67 | 11 |
| Zhang et al. | 2014 | Asian | PCR | P-B | Nasopharyngeal carcinoma | Y | 163 | 116 | 14 | 247 | 120 | 13 |
| Wang et al. | 2014 | Asian | PCR–CTPP | P-B | Lung cancer | N | 101 | 59 | 8 | 102 | 68 | 25 |
| Feng et al. | 2017 | Asian | PCR | H-B | Cervical cancer | Y | 103 | 67 | 10 | 114 | 55 | 11 |
Abbreviations: H-B, hospital based; HWE, Hardy–Weinberg equilibrium; N, polymorphisms did not conform to HWE in the control group; P-B, population based; SCCHN, squamous cell carcinoma of the head and neck; Y, polymorphisms conformed to HWE in the control group.
Quantitative synthesis
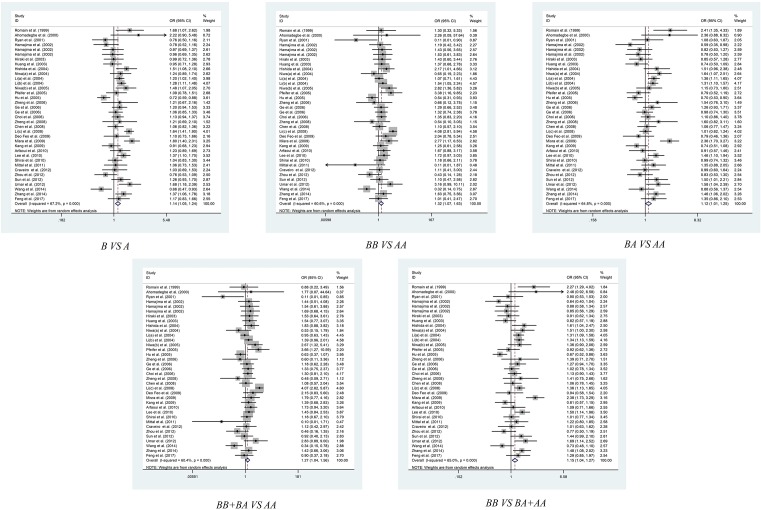
Table 2 listed the main results of current meta-analysis work of polymorphisms in G4C14-A4T14 and risk of cancer. The pooled results of the 36 included studies had shown that G4C14-A4T14 polymorphism conferred a significantly higher overall risk to cancer susceptibility in all the five genetic models, allelic contrast model (GC vs. AT: OR = 1.139, 95% CI = 1.048–1.238, P=0.002), homozygote comparison model (GC/GC vs. AT/AT: OR = 1.320, 95% CI = 1.071–1.627, P=0.009), heterozygote comparison model (GC/AT vs. AT/AT: OR = 1.123, 95% CI = 1.012–1.245, P=0.028), dominant comparison model (GC/GC+GC/AT vs. AT/AT: OR = 1.152, 95% CI = 1.044–1.272, P=0.005) and recessive comparison model (GC/GC vs. GC/AT+AT/AT: OR = 1.273, 95% CI = 1.038–1.563, P=0.021) (Table 2 and Figure 2).
Table 2. Results of pooled analysis for TP73 G4C14-A4T14 polymorphism and cancer susceptibility.
| Comparison | Subgroup | N | PH | PZ | Random | Fixed |
|---|---|---|---|---|---|---|
| B vs. A | Overall | 36 | <0.001 | 0.002* | 1.139 (1.048–1.238) | 1.170 (1.119–1.223) |
| Caucasian | 14 | 0.001 | <0.001* | 1.279 (1.131–1.446) | 1.317 (1.232–1.407) | |
| Asian | 22 | <0.001 | 0.228 | 1.062 (0.963–1.172) | 1.060 (0.998–1.126) | |
| Breast cancer | 3 | 0.091 | 0.940 | 0.985 (0.666–1.457) | 0.929 (0.747–1.156) | |
| Colorectal cancer | 4 | 0.339 | 0.011* | 1.197 (1.027–1.395) | 1.204 (1.044–1.389) | |
| SCCHN | 3 | 0.007 | 0.062 | 1.308 (0.987–1.733) | 1.274 (1.134–1.432) | |
| Cervical cancer | 6 | 0.982 | 0.031* | 1.190 (1.016–1.393) | 1.189 (1.016–1.392) | |
| Esophageal cancer | 4 | 0.010 | 0.873 | 1.027 (0.738–-1.430) | 1.057 (0.903–1.236) | |
| Gastric cancer | 4 | 0.739 | 0.261 | 1.084 (0.943–1.247) | 1.084 (0.942–1.247) | |
| Lung cancer | 5 | <0.001 | 0.657 | 0.943 (0.726–1.224) | 1.034 (0.945–1.132) | |
| P-B | 20 | <0.001 | 0.176 | 1.082 (0.965–1.213) | 1.098 (1.033–1.168) | |
| H-B | 16 | <0.001 | 0.001* | 1.213 (1.079–1.365) | 1.256 (1.177–1.340) | |
| HWE(Y) | 32 | <0.001 | 0.003* | 1.138 (1.044–1.239) | 1.165 (1.109–1.222) | |
| HWE(N) | 4 | <0.001 | 0.484 | 1.132 (0.799–1.604) | 1.200 (1.071–1.345) | |
| BB vs. AA | Overall | 36 | <0.001 | 0.009* | 1.320 (1.071–1.627) | 1.420 (1.265–1.593) |
| Caucasian | 14 | <0.001 | 0.011* | 1.649 (1.119–2.431) | 1.806 (1.523–2.142) | |
| Asian | 22 | 0.033 | 0.151 | 1.170 (0.944–1.450) | 1.152 (0.984–1.350) | |
| Breast cancer | 3 | 0.189 | 0.952 | 0.918 (0.370–2.279) | 0.983 (0.558–1.732) | |
| Colorectal cancer | 4 | 0.676 | 0.001* | 1.807 (1.258–2.595) | 1.820 (1.270–2.608) | |
| SCCHN | 3 | 0.136 | 0.196 | 1.336 (0.807–2.211) | 1.235 (0.897–1.699) | |
| Cervical cancer | 6 | 0.949 | 0.697 | 0.925 (0.590–1.451) | 0.916 (0.587–1.428) | |
| Esophageal cancer | 4 | 0.048 | 0.734 | 1.165 (0.484–2.804) | 1.168 (0.762–1.79) | |
| Gastric cancer | 4 | 0.815 | 0.114 | 1.351 (0.935–1.951) | 1.345 (0.931–1.944) | |
| Lung cancer | 5 | 0.001 | 0.748 | 0.912 (0.522–1.595) | 1.039 (0.823–1.311) | |
| P-B | 20 | 0.002 | 0.470 | 1.107 (0.841–1.457) | 1.136 (0.968–1.335) | |
| H-B | 16 | 0.001 | 0.001* | 1.625 (1.210–2.183) | 1.809 (1.532–2.136) | |
| HWE(Y) | 32 | <0.001 | 0.007* | 1.342 (1.085–1.659) | 1.476 (1.303–1.671) | |
| HWE(N) | 4 | 0.001 | 0.579 | 1.288 (0.526–3.152) | 1.117 (0.819–1.524) | |
| BA vs. AA | Overall | 36 | <0.001 | 0.028* | 1.123 (1.012–1.245) | 1.133 (1.070–1.200) |
| Caucasian | 14 | <0.001 | 0.008* | 1.252 (1.061–1.477) | 1.251 (1.149–1.362) | |
| Asian | 22 | <0.001 | 0.458 | 1.049 (0.924–1.191) | 1.044 (0.966–1.129) | |
| Breast cancer | 3 | 0.100 | 0.284 | 0.941 (0.587–1.510) | 0.859 (0.651–1.134) | |
| Colorectal cancer | 4 | 0.026 | 0.901 | 0.978 (0.693–1.381) | 1.059 (0.879–1.276) | |
| SCCHN | 3 | 0.002 | 0.051 | 1.494 (0.998–2.236) | 1.446 (1.246–1.678) | |
| Cervical cancer | 6 | 0.748 | 0.001* | 1.414 (1.159–1.725) | 1.413 (1.159–1.722) | |
| Esophageal cancer | 4 | 0.031 | 0.953 | 1.011 (0.702–1.457) | 1.023 (0.841–1.244) | |
| Gastric cancer | 4 | 0.295 | 0.867 | 1.007 (0.821–1.234) | 1.015 (0.849–1.214) | |
| Lung cancer | 5 | 0.002 | 0.781 | 0.964 (0.742–1.251) | 1.044 (0.929–1.172) | |
| P-B | 20 | <0.001 | 0.129 | 1.113 (0.969–1.279) | 1.118 (1.033–1.209) | |
| H-B | 16 | <0.001 | 0.129 | 1.134 (0.964–1.334) | 1.152 (1.059–1.253) | |
| HWE(Y) | 32 | <0.001 | 0.065 | 1.101 (0.994–1.219) | 1.098 (1.032–1.169) | |
| HWE(N) | 4 | <0.001 | 0.325 | 1.245 (0.805–1.927) | 1.348 (1.165–1.560) | |
| BB+BA vs. AA | Overall | 36 | <0.001 | 0.005* | 1.152 (1.044–1.272) | 1.174 (1.111–1.240) |
| Caucasian | 14 | 0.004 | <0.001* | 1.312 (1.140–1.511) | 1.327 (1.224–1.440) | |
| Asian | 22 | <0.001 | 0.332 | 1.063 (0.940–1.203) | 1.059 (0.984–1.141) | |
| Breast cancer | 3 | 0.096 | 0.860 | 0.959 (0.605–1.520) | 0.880 (0.675–1.148) | |
| Colorectal cancer | 4 | 0.073 | 0.538 | 1.092 (0.824–1.447) | 1.151 (0.964–1.375) | |
| SCCHN | 3 | 0.001 | 0.061 | 1.482 (0.982–2.237) | 1.415 (1.226–1.633) | |
| Cervical cancer | 6 | 0.861 | 0.003* | 1.339 (1.107–1.619) | 1.338 (1.106–1.618) | |
| Esophageal cancer | 4 | 0.020 | 0.910 | 1.022 (0.706–1.477) | 1.050 (0.870–1.267) | |
| Gastric cancer | 4 | 0.477 | 0.522 | 1.058 (0.892–1.255) | 1.057 (0.892–1.254) | |
| Lung cancer | 5 | <0.001 | 0.694 | 0.943 (0.704–1.263) | 1.045 (0.935–1.167) | |
| P-B | 20 | <0.001 | 0.130 | 1.112 (0.969–1.275) | 1.124 (1.043–1.211) | |
| H-B | 16 | <0.001 | 0.012* | 1.204 (1.042–1.392) | 1.234 (1.139–1.337) | |
| HWE(Y) | 32 | <0.001 | 0.010* | 1.138 (1.032–1.255) | 1.150 (1.084–1.221) | |
| HWE(N) | 4 | <0.001 | 0.376 | 1.223 (0.783–1.911) | 1.315 (1.143–1.512) | |
| BB vs. BA+AA | Overall | 36 | <0.001 | 0.021* | 1.273 (1.038–1.563) | 1.374 (1.227–1.538) |
| Caucasian | 14 | <0.001 | 0.046* | 1.509 (1.008–2.261) | 1.697 (1.437–2.005) | |
| Asian | 22 | 0.074 | 0.097 | 1.160 (0.951–1.415) | 1.141 (0.976–1.332) | |
| Breast cancer | 3 | 0.172 | 0.798 | 0.984 (0.388–2.493) | 1.075 (0.617–1.875) | |
| Colorectal cancer | 4 | 0.512 | 0.002* | 1.746 (1.228–2.484) | 1.760 (1.241–2.496) | |
| SCCHN | 3 | 0.416 | 0.642 | 1.075 (0.782–1.477) | 1.078 (0.786–1.477) | |
| Cervical cancer | 6 | 0.913 | 0.349 | 0.825 (0.530–1.286) | 0.811 (0.524–1.256) | |
| Esophageal cancer | 4 | 0.052 | 0.688 | 1.193 (0.504–2.824) | 1.165 (0.764–1.777) | |
| Gastric cancer | 4 | 0.717 | 0.118 | 1.342 (0.934–1.927) | 1.334 (0.929–1.915) | |
| Lung cancer | 5 | 0.006 | 0.794 | 0.938 (0.578–1.521) | 1.029 (0.818–1.294) | |
| P-B | 20 | 0.006 | 0.532 | 1.086 (0.839–1.404) | 1.106 (0.945–1.296) | |
| H-B | 16 | <0.001 | 0.005* | 1.545 (1.139–2.094) | 1.734 (1.474–2.039) | |
| HWE(Y) | 32 | <0.001 | 0.011* | 1.309 (1.063–1.613) | 1.446 (1.280–1.633) | |
| HWE(N) | 4 | 0.003 | 0.743 | 1.145 (0.509–2.579) | 1.000 (0.736–1.358) |
PH: P value of Q-test for heterogeneity test; PZ: means statistically significant (P<0.05); HWE, Hardy–Weinberg equilibrium; N, polymorphisms did not conform to HWE in the control group; P-B, population based; SCCHN, squamous cell carcinoma of the head and neck; Y, polymorphisms conformed to HWE in the control group; *P value less than 0.05 was considered as statistically significant.
Figure 2. Meta-analysis of the association between TP73 G4C14-A4T14 polymorphism and overall cancer risk.
Stratification analysis by cancer type
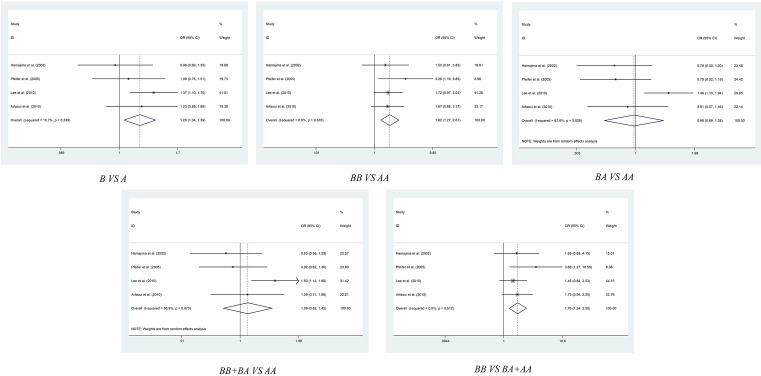
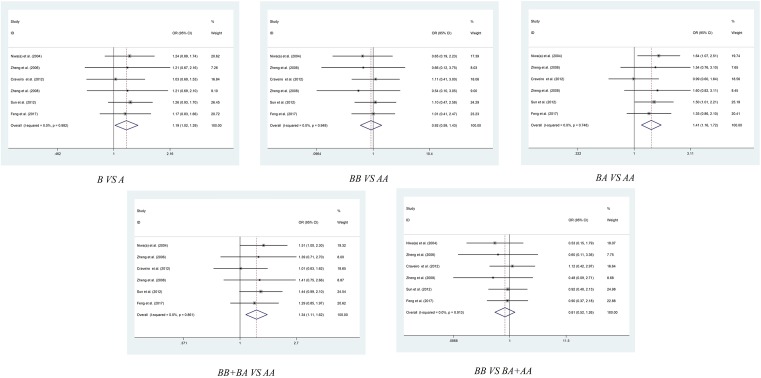
After overall pooled analysis, we also conducted stratification analysis by cancer type, in order to obtain more precise result about the G4C14-A4T14 polymorphism and cancer susceptibility. As shown in Table 2 and Figure 3, the subgroup analysis of six enrolled colorectal cancer related studies have shown that G4C14-A4T14 polymorphism was related to an increased cancer risk in allelic contrast model (GC vs. AT: OR = 1.204, 95% CI = 1.044–1.389, P=0.011), homozygote comparison model (GC/GC vs. AT/AT: OR = 1.820, 95% CI = 1.270–2.608, P=0.001) and recessive comparison model (GC/GC vs. GC/AT+AT/AT: OR = 1.760, 95% CI = 1.241–2.496, P=0.002). As to cervical cancer, there are also some interesting results. The meta-analysis revealed an increasing risk of cancer caused by G4C14-A4T14 polymorphism in allelic contrast model (GC vs. AT: OR = 1.189, 95% CI = 1.016–1.392, P=0.031), heterozygote comparison model (GC/AT vs. AT/AT: OR = 1.413, 95% CI = 1.159–1.722, P=0.001) and dominant comparison model (GC/GC+GC/AT vs. AT/AT: OR = 1.338, 95% CI = 1.106–1.618, P=0.003) (Table 2, Figure 4). We also performed subgroup analysis of breast cancer, esophageal cancer, gastric cancer, lung cancer and squamous cell carcinoma of the head and neck, no significant association was found between G4C14-A4T14 polymorphism and these carcinomas in all five genetic models (Table 2 and Figures S1–S4).
Figure 3. Meta-analysis of the association between TP73 G4C14-A4T14 polymorphism and colorectal cancer risk.
Figure 4. Meta-analysis of the association between TP73 G4C14-A4T14 polymorphism and cervical cancer risk.
Stratification analysis by ethnicity
There was some significant result shown in subgroup analysis of ethnicity. The 14 Caucasian based case–control studies shown a significantly increasing risk between G4C14-A4T14 polymorphism and cancer in allelic contrast model (GC vs. AT: OR = 1.279, 95% CI = 1.131–1.446, P<0.001), homozygote comparison model (GC/GC vs. AT/AT: OR = 1.649, 95% CI = 1.119–2.431, P<0.001), heterozygote comparison model (GC/AT vs. AT/AT: OR = 1.252, 95% CI = 1.061–1.477, P<0.001), dominant comparison model (GC/GC+GC/AT vs. AT/AT: OR = 1.312, 95% CI = 1.140–1.511, P=0.004) and recessive comparison model (GC/GC vs. GC/AT+AT/AT: OR = 1.509, 95% CI = 1.008–2.261, P<0.001) (Table 2 and Figure S5).
Stratification analysis by source of control
Due to there are 20 case–control studies based on population controls, whereas another 16 studies enrolled hospital-based controls, we performed the stratified analysis by HWE status to obtain more precise results. The remarkable result shown a noticeable upgrade cancer risk of G4C14-A4T14 polymorphism of the hospital-based control subgroup in allelic contrast model (GC vs. AT: OR = 1.213, 95%CI = 1.079–1.365, P=0.001), homozygote comparison model (GC/GC vs. AT/AT: OR = 1.625, 95% CI = 1.210–2.183 P=0.001), dominant comparison model (GC/GC+GC/AT vs. AT/AT: OR = 1.204, 95% CI = 1.042–1.392, P=0.012) and recessive comparison model (GC/GC vs. GC/AT+AT/AT: OR = 1.545, 95% CI = 1.139–2.094, P=0.005), while there was no significant result of the heterozygote comparison model (GC/AT vs. AT/AT: OR = 1.134, 95% CI = 0.964–1.334, P=0.129). Nevertheless, there are no significant result revealed in population-based control subgroup in overall cancer (Table 2 and Figure S6).
Stratification analysis by HWE status
In order to exclude the influence of allele frequency changing, we calculated whether the control group conform to HWE, and conducted the stratification meta-analysis in subgroups of HWE status. As shown in Table 2 and Figure S7, the subgroup that conforms to HWE was uncovered responsible to the remarkable increasing cancer risk of G4C14-A4T14 polymorphism in allelic contrast model (GC vs. AT: OR = 1.138, 95%CI = 1.044–1.239, P=0.003), homozygote comparison model (GC/GC vs. AT/AT: OR = 1.342, 95% CI = 1.085–1.659, P=0.007), dominant comparison model (GC/GC+GC/AT vs. AT/AT: OR = 1.138, 95% CI = 1.032–1.255, P=0.010) and recessive comparison model (GC/GC vs. GC/AT+AT/AT: OR = 1.309, 95% CI = 1.063–1.613, P=0.011), whereas the other four case–control studies that do not conform to HWE did not influence the result in overall cancer (Table 2 and Figure S7).
Sensitivity analysis and publication bias
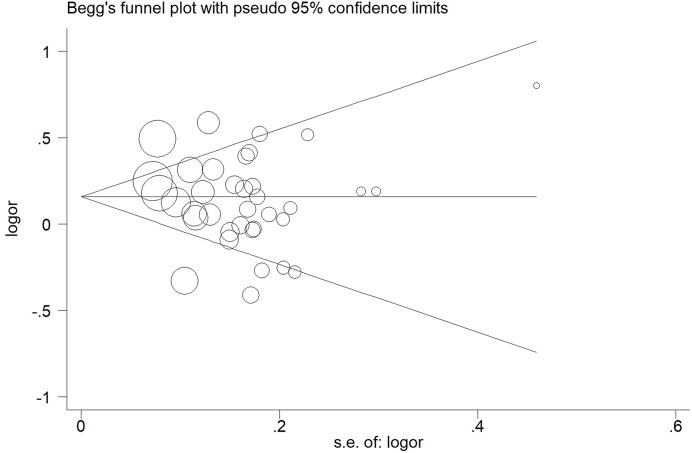
Sensitivity analysis was performed to assess the influence of each individual study on the pooled OR by sequential removal of individual studies, the results showed that the study material alteration did not influence the corresponding pooled ORs for the overall meta-analysis (Figure 5 and Table S3). In addition, Begg’s funnel plot and Egger’s test were presented to assess the potential publication bias, no evidence of publication bias was revealed by evaluating the shape of Begg’s funnel plot and by Egger’s regression test (Figures S8, S9 and Table S4).
Figure 5. Begg’s funnel plot for publication bias test for TP73 G4C14-A4T14 polymorphism (GC vs. AT).
The x-axis is log (OR), and the y-axis is natural logarithm of OR. The horizontal line in the figure represents the overall estimated log (OR). The two diagonal lines indicate the pseudo 95% confidence limits of the effect estimate.
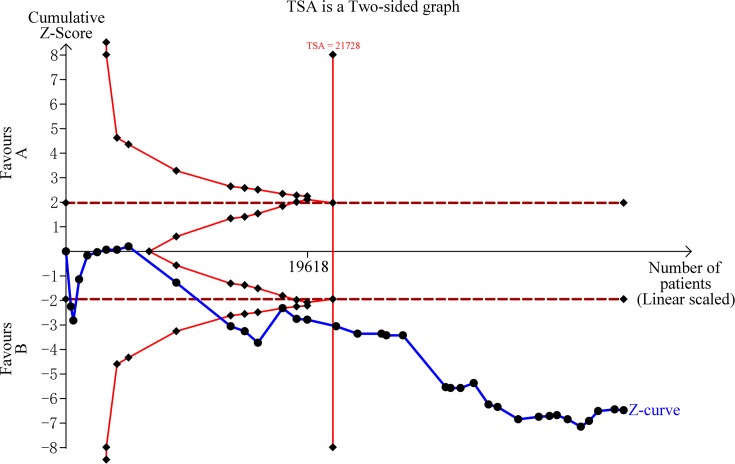
Result of FPRP and TSA
The FPRP values for significant findings at different prior probability levels are shown in Table 3. In the result of overall group in five genetic models, all the statistical power is about 1, and the FPRP values are all less than 0.2, under the prior probability of 0.1. On the subgroup of cervical cancer and colorectal cancer, the FPRP values are also less than 0.2. The result of TSA is shown in Figure 6, the required sample size is 21,728 samples, and the cumulative z-curve crossed the trial sequential monitoring boundary before reaching the required sample size, which means that our conclusions are robust with these sufficient evidence.
Table 3. False-positive report probability values for associations between the risk of cancer and the frequency of genotypes of TP73 Gene.
| Comparison | Subgroup | Pz | OR (95% CI) | Statistical power* | Prior probability | ||||
|---|---|---|---|---|---|---|---|---|---|
| 0.250 | 0.1 | 0.01 | 0.001 | 0.0001 | |||||
| B vs. A | Overall | 0.002 | 1.139 (1.048–1.238) | 1.000 | <0.001 | <0.001 | 0.001 | 0.006 | 0.053 |
| Caucasian | <0.001 | 1.279 (1.131–1.446) | 0.809 | <0.001 | <0.001 | 0.001 | 0.006 | 0.054 | |
| Colorectal cancer | 0.011 | 1.204 (1.044–1.389) | 0.754 | <0.001 | <0.001 | 0.001 | 0.007 | 0.062 | |
| Cervical cancer | 0.031 | 1.189 (1.016–1.392) | 0.446 | <0.001 | <0.001 | 0.001 | 0.008 | 0.075 | |
| H-B | 0.001 | 1.213 (1.079–1.365) | 1.000 | <0.001 | <0.001 | 0.001 | 0.006 | 0.054 | |
| HWE(Y) | 0.003 | 1.138 (1.044–1.239) | 1.000 | <0.001 | <0.001 | 0.001 | 0.006 | 0.053 | |
| BB vs. AA | Overall | 0.009 | 1.320 (1.071–1.627) | 1.000 | <0.001 | <0.001 | 0.002 | 0.024 | 0.196 |
| Caucasian | 0.011 | 1.649 (1.119–2.431) | 0.467 | 0.003 | 0.008 | 0.081 | 0.469 | 0.898 | |
| Colorectal cancer | 0.001 | 1.820 (1.270–2.608) | 0.901 | 0.002 | 0.005 | 0.053 | 0.362 | 0.850 | |
| H-B | 0.001 | 1.625 (1.210–2.183) | 1.000 | 0.001 | 0.002 | 0.017 | 0.148 | 0.635 | |
| HWE(Y) | 0.007 | 1.342 (1.085–1.659) | 1.000 | <0.001 | <0.001 | 0.003 | 0.025 | 0.208 | |
| BA vs. AA | Overall | 0.028 | 1.123 (1.012–1.245) | 0.992 | <0.001 | <0.001 | 0.001 | 0.006 | 0.053 |
| Caucasian | 0.008 | 1.252 (1.061–1.477) | 0.557 | <0.001 | <0.001 | 0.001 | 0.009 | 0.085 | |
| Cervical cancer | 0.001 | 1.413 (1.159–1.722) | 0.822 | <0.001 | <0.001 | 0.002 | 0.018 | 0.157 | |
| BB+BA vs. AA | Overall | 0.005 | 1.152 (1.044–1.272) | 1.000 | <0.001 | <0.001 | 0.001 | 0.006 | 0.053 |
| Caucasian | <0.001 | 1.312 (1.140–1.511) | 0.703 | <0.001 | <0.001 | 0.001 | 0.006 | 0.061 | |
| Cervical cancer | 0.003 | 1.338 (1.106–1.618) | 0.714 | <0.001 | <0.001 | 0.002 | 0.015 | 0.135 | |
| H-B | 0.012 | 1.204 (1.042–1.392) | 1.000 | <0.001 | <0.001 | 0.001 | 0.007 | 0.064 | |
| HWE(Y) | 0.010 | 1.138 (1.032–1.255) | 0.996 | <0.001 | <0.001 | 0.001 | 0.006 | 0.053 | |
| BB vs. BA+AA | Overall | 0.021 | 1.273 (1.038–1.563) | 1.000 | <0.001 | <0.001 | 0.002 | 0.022 | 0.182 |
| Caucasian | 0.046 | 1.509 (1.008–2.261) | 0.341 | 0.003 | 0.010 | 0.100 | 0.528 | 0.918 | |
| Colorectal cancer | 0.002 | 1.760 (1.241–2.496) | 0.888 | 0.001 | 0.004 | 0.045 | 0.323 | 0.827 | |
| H-B | 0.005 | 1.545 (1.139–2.094) | 1.000 | 0.001 | 0.002 | 0.020 | 0.172 | 0.675 | |
| HWE(Y) | 0.011 | 1.309 (1.063–1.613) | 1.000 | <0.001 | <0.001 | 0.002 | 0.024 | 0.195 | |
CI, confidence interval; H-B, hospital based; HWE(Y), Polymorphisms conformed to Hardy–Weinberg equilibrium in the control group; OR, odds ratio.
Statistical power was calculated using the number of observations in the subgroup and the OR and P values in this table.
Figure 6. Trial sequential analysis for TP73 G4C14-A4T14 polymorphism under the allele contrast model.
In silico analysis of TP73 expression
In silico analysis, we draw out the correlation between TP73 expression and breast invasive carcinoma, cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC), colon adenocarcinoma (COAD), esophageal carcinoma, head and neck squamous cell carcinoma, lung adenocarcinoma, lung squamous cell carcinoma (LUSC), ovarian serous, prostate adenocarcinoma, rectum adenocarcinoma, skin cutaneous melanoma, Ssomach adenocarcinoma, with the help of GEPIA web server. The result indicated that the expression of TP73 in tumor tissue is higher than it in corresponding normal tissue of CESC (TPM = 9.60 vs. 0.58 respectively, P<0.01), COAD (TPM = 1.93 vs. 0.56 respectively, P<0.01), LUSC (TPM = 7.64 vs. 1.07 respectively, P<0.01), whereas lower than it in normal tissue of SKCM (TPM = 0.67 vs. 7.62 respectively, P<0.01) ( Figure S10).
Discussion
TP73 gene is located at chromosome 1p36 and comprises 15 exons [54]. TP73 could be transcribed from two individual promoters, one is in the upstream of exon 1, it could produce p53-like proteins containing transactivation domain (TAp73) and another TA lacking protein (ΔTAp73). The second promoter is situated in intron 3, it could turn out the N-terminal truncated isoform (ΔNp73) [55]. What’s more, both TAp73 and ΔNp73 undergo the alternative splicing and initiation of translation, and lead to several splicing isoforms [56,57]. While sharing the similar sequence with p53, TAp73 could activate the expression of downstream genes through specifically binding domain of p53 response element, regulating cell apoptosis or cell-cycle arrest [58,59]. On the meanwhile, ΔNp73 could present a potent anti-oncogenic function through inhibiting the key role of TAp63, TAp73 or p53 [60]. Several publications had reported that the TP73 expression plays critical role in tumorigenesis, combined with different isoforms or several mutations [61–64].
In the past decades, almost 146 unique variations had been reported (shown in the Biomuta database [65]), while numerous studies had probed into the relationship of G4C14-A4T14 polymorphism and cancer genomics. G4A (rs2273953) and C14T (rs1801173) polymorphisms are located at position 4 (G to A) and 14 (C to T) of exon 2 5’-untranslated region, which might influence the initiating AUG codon through constructing a stem–loop [54]. Zheng et al. [40] and Niwa et al. [34] reported that G4C14-A4T14 polymorphism was not associated with the cancer susceptibility of cervical cancer in Uighur and Japanese, respectively. However, Craveiro et al. [51] revealed that G4C14-A4T14 polymorphism leads to an increasing risk of cervical cancer, as well as the newest study conducted by Feng et al. [17].As colorectal cancer, Hamajima et al. [28] presented that no significant differences in the genotype frequencies were observed among the enrolled cases and controls in his study. On the contrast, Lee et al. [47] reported that GC/AT and AT/AT genotypes were significantly associated with colorectal cancer risk in Korean population. Arfaoui et al. [66] also uncovered that no remarkable differences of genotype frequencies in cancers and controls, but they found that AT/AT genotype might cause the poor prognosis of colorectal cancer. Several researches also managed in lung cancer. Hu et al. [35] indicated that both AT/AT and GC/AT variants were associated with a remarkable decreased risk for lung cancer, distinguishingly, Li et al. [64] suggested that the AT/AT and GC/AT genotypes were related with a statistically significantly increased risk for lung cancer. Choi et al. [38] did not agree with each of them, they revealed that TP73 G4C14-A4T14 polymorphism does not affect the susceptibility to lung cancer in Korean population.
Among these publications concerned about G4C14-A4T14 polymorphism and cancer risk, the result is not consistent. Liang et al. [67] conducted a meta-analysis about G4C14-A4T14 polymorphism and cervical cancer, they only enrolled 5 studies, as well as Liu et al. [68], they only enrolled 5 studies about lung cancer. Yu et al. [69] had performed a meta-analysis with only 23 eligible studies; however, they draw a decreased risk of G4C14-A4T14 polymorphism, this mistake may cause by the fewer samples. Therefore, our team carried out the present comprehensive meta-analysis aiming at shedding light on the multiple lines of evidence. Finally, 36 case–control studies comprise 9493 cases and 13,157 controls were enrolled and analyzed. All in all, our recent updated meta-analysis draws a comprehensive, precise and convincible result, which is that G4C14-A4T14 polymorphism of TP73 is strongly associated with the increasing cancer risk, especially for Caucasian, cervical cancer and colorectal cancer. Therefore, in the future, G4C14-A4T14 polymorphism might be a useful diagnostic marker for cervical cancer and colorectal cancer, especially in Caucasian population. On the other hand, for researchers, other polymorphisms of TP73 should be focused on to assess whether they change cancer risks.
The current result about G4C14-A4T14 polymorphism and cancer risk should be cautiously interpreted, because there are some limitations. First, an insufficient capacity that slight effects on cancer susceptibility occurred when a stratified analysis was conducted by the cancer type, ethnicity and source of control. Second, several potential confounding factors were ignored, such as age, gender, smoking, drinking and etc., so we are unable to perform a further assessment of potential gene–environment interactions. Third, we only enrolled publications written in English or Chinese, missing publications from other languages may cause potential bias. On the meanwhile, the advantages of this research should not be buried. First, a comprehensive search was conducted to identify more qualified studies, so this analysis is persuasive and substantive. Second, the quality of each registered research was evaluated by NOS scale, low-quality studies were eliminated to raise the credibility of results. Third, stratification analysis was performed by ethnicity, source of controls, tumor type or ethnicity, in order to decrease the impact of heterogeneity and obtain the real conclusion.
In conclusion, our meta-analysis had successfully elaborated that TP73 G4C14-A4T14 polymorphism causes an upgrade cancer risk, especially in Caucasian population. G4C14-A4T14 polymorphism might be a potential biomarker for judging the tumorigenesis of cervical cancer and colorectal cancer.
Supporting information
Fig. S1.
Fig. S2.
Fig. S3.
Fig. S4.
Fig. S5.
Fig. S6.
Fig. S7.
Fig. S8.
Fig. S9.
Fig. S10.
Supplementary Table 1. Methodological quality of the included studies according to the Newcastle-Ottawa Scale.
Supplementary Table 2. PRISMA 2009 Checklist.
Supplementary Table 3. Details of the sensitivity analyses for TP73 G4C14-A4T14 polymorphism and cancer risk.
Supplementary Table 4. P values of the Egger's test for TP73 G4C14-A4T14 polymorphism.
Abbreviations
- CESC
cervical squamous cell carcinoma and endocervical adenocarcinoma
- COAD
colon adenocarcinoma
- HWE
Hardy–Weinberg equilibrium
- LUSC
lung squamous cell carcinoma
- NOS
Newcastle–Ottawa Scale
- SNP
single-nucleotide polymorphism
- TSA
trial sequential analysis
- TP73
tumor protein P73
Author Contribution
M.J.L. and W.S. accessed information from literature for this article. M.J.L., Z.M. and F.S. designed and performed the meta-analysis. M.J.L., Z.L. and L.C.Z. contributed toward writing, discussing and editing the manuscript. All authors discussed the results and contributed to the final manuscript.
Funding
This manuscript was supported by National Natural Science Foundation of China [81630019 (to L.C.Z)].
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
References
- 1.Siegel R.L., Miller K.D. and Jemal A. (2018) Cancer statistics, 2018. CA Cancer J. Clin. 68, 7–30 10.3322/caac.21442 [DOI] [PubMed] [Google Scholar]
- 2.Chen W., Zheng R., Baade P.D., Zhang S., Zeng H. and Bray F. (2016) Cancer statistics in China, 2015. CA Cancer J. Clin. 66, 115–132 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 3.Vineis P. and Fecht D. (2018) Environment, cancer and inequalities – the urgent need for prevention. Eur. J. Cancer 10.1016/j.ejca.2018.04.018 [DOI] [PubMed] [Google Scholar]
- 4.Tanaka T., Watanabe M. and Yamashita K. (2018) Potential therapeutic targets of TP53 gene in the context of its classically canonical functions and its latest non-canonical functions in human cancer. Oncotarget 9, 16234–16247 10.18632/oncotarget.24611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tidwell T.R., Soreide K. and Hagland H.R. (2017) Aging, metabolism, and cancer development: from Peto’s Paradox to the Warburg Effect. Aging Dis. 8, 662–676 10.14336/AD.2017.0713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tozluoglu M., Karaca E., Haliloglu T. and Nussinov R. (2008) Cataloging and organizing p73 interactions in cell cycle arrest and apoptosis. Nucleic Acids Res. 36, 5033–5049 10.1093/nar/gkn481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jost C.A., Marin M.C. and Kaelin W.G. Jr. (1997) p73 is a simian [correction of human] p53-related protein that can induce apoptosis. Nature 389, 191–194 10.1038/38298 [DOI] [PubMed] [Google Scholar]
- 8.Candi E., Agostini M., Melino G. and Bernassola F. (2014) How the TP53 family proteins TP63 and TP73 contribute to tumorigenesis: regulators and effectors. Hum. Mutat. 35, 702–714 10.1002/humu.22523 [DOI] [PubMed] [Google Scholar]
- 9.Monti P., Ghiorzo P., Menichini P., Foggetti G., Queirolo P. and Izzotti A. (2017) TP63 mutations are frequent in cutaneous melanoma, support UV etiology, but their role in melanomagenesis is unclear. Oncol. Rep. 38, 1985–1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vilgelm A.E., Washington M.K., Wei J., Chen H., Prassolov V.S. and Zaika A.I. (2010) Interactions of the p53 protein family in cellular stress response in gastrointestinal tumors. Mol. Cancer Ther. 9, 693–705 10.1158/1535-7163.MCT-09-0912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levrero M., De Laurenzi V., Costanzo A., Gong J., Wang J.Y. and Melino G. (2000) The p53/p63/p73 family of transcription factors: overlapping and distinct functions. J. Cell Sci. 113, 1661–1670 [DOI] [PubMed] [Google Scholar]
- 12.Kaghad M., Bonnet H., Yang A., Creancier L., Biscan J.C. and Valent A. (1997) Monoallelically expressed gene related to p53 at 1p36, a region frequently deleted in neuroblastoma and other human cancers. Cell 90, 809–819 10.1016/S0092-8674(00)80540-1 [DOI] [PubMed] [Google Scholar]
- 13.Peters M.A., Janer M., Kolb S., Jarvik G.P., Ostrander E.A. and Stanford J.L. (2001) Germline mutations in the p73 gene do not predispose to familial prostate-brain cancer. Prostate 48, 292–296 10.1002/pros.1109 [DOI] [PubMed] [Google Scholar]
- 14.Umar M., Upadhyay R., Khurana R., Kumar S., Ghoshal U.C. and Mittal B. (2012) Role of p53 and p73 genes polymorphisms in susceptibility to esophageal cancer: a case control study in a northern Indian population. Mol. Biol. Rep. 39, 1153–1162 10.1007/s11033-011-0844-9 [DOI] [PubMed] [Google Scholar]
- 15.Zhou X. and Wu C. (2012) Association of p73 G4C14-A4T14 polymorphisms with genetic susceptibilities to breast cancer: a case-control study. Chin. J. Clin. Oncol. 29, 3216–3221 [DOI] [PubMed] [Google Scholar]
- 16.Wang S.S., Guo H.Y., Dong L.L., Zhu X.Q., Ma L. and Li W. (2014) Association between a p73 gene polymorphism and genetic susceptibility to non-small cell lung cancer in the South of China. Asian. Pac. J. Cancer Prev. 15, 10387–10391 10.7314/APJCP.2014.15.23.10387 [DOI] [PubMed] [Google Scholar]
- 17.Feng H., Sui L., Du M. and Wang Q. (2017) Meta-analysis of TP73 polymorphism and cervical cancer. Genet. Mol. Res. 16, 10.4238/gmr16016571 [DOI] [PubMed] [Google Scholar]
- 18.Lau J., Ioannidis J.P. and Schmid C.H. (1997) Quantitative synthesis in systematic reviews. Ann. Internal Med. 127, 820–826 10.7326/0003-4819-127-9-199711010-00008 [DOI] [PubMed] [Google Scholar]
- 19.R D. and N L. (1986) Meta-analysis in clinical trials. Control. Clin. Trials 7, 177 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 20.Begg C.B. and Mazumdar M. (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- 21.Higgins J.P. and Thompson S.G. (2002) Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 22.Wacholder S., Chanock S., Garcia-Closas M., El Ghormli L. and Rothman N. (2004) Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J. Natl. Cancer Inst. 96, 434–442 10.1093/jnci/djh075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He J., Wang M.Y., Qiu L.X., Zhu M.L., Shi T.Y. and Zhou X.Y. (2013) Genetic variations of mTORC1 genes and risk of gastric cancer in an Eastern Chinese population. Mol. Carcinog. 52, E70–E79 [DOI] [PubMed] [Google Scholar]
- 24.Tang Z., Li C., Kang B., Gao G., Li C. and Zhang Z. (2017) GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 45, W98–W102 10.1093/nar/gkx247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Romani M., Scaruffi P., Casciano I., Mazzocco K., Lo Cunsolo C. and Cavazzana A. (1999) Stage-independent expression and genetic analysis of tp73 in neuroblastoma. Int. J. Cancer 84, 365–369 10.1002/(SICI)1097-0215(19990820)84:4%3c365::AID-IJC6%3e3.0.CO;2-X [DOI] [PubMed] [Google Scholar]
- 26.Ahomadegbe J.C., Tourpin S., Kaghad M., Zelek L., Vayssade M. and Mathieu M.C. (2000) Loss of heterozygosity, allele silencing and decreased expression of p73 gene in breast cancers: prevalence of alterations in inflammatory breast cancers. Oncogene 19, 5413–5418 [DOI] [PubMed] [Google Scholar]
- 27.Ryan B.M., Mcmanus R., Daly J.S., Carton E., Keeling P.W. and Reynolds J.V. (2001) A common p73 polymorphism is associated with a reduced incidence of oesophageal carcinoma. Br. J. Cancer 85, 1499–1503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamajima N., Matsuo K., Suzuki T., Nakamura T., Matsuura A. and Hatooka S. (2002) No associations of p73 G4C14-to-A4T14 at exon 2 and p53 Arg72Pro polymorphisms with the risk of digestive tract cancers in Japanese. Cancer Lett. 181, 81–85 10.1016/S0304-3835(02)00041-1 [DOI] [PubMed] [Google Scholar]
- 29.Hiraki A., Matsuo K., Hamajima N., Ito H., Hatooka S. and Suyama M. (2003) Different risk relations with smoking for non-small-cell lung cancer: comparison of TP53 and TP73 genotypes. Asian Pac. J. Cancer Prev. 4, 107. [PubMed] [Google Scholar]
- 30.Huang X.E., Hamajima N., Katsuda N., Matsuo K., Hirose K. and Mizutani M. (2003) Association of p53 codon arg72pro and p73 G4C14-to-A4T14 at exon 2 genetic polymorphisms with the risk of japanese breast cancer. Breast Cancer 10, 307–311 [DOI] [PubMed] [Google Scholar]
- 31.Hishida A., Matsuo K., Tajima K., Ogura M., Kagami Y. and Taji H. (2004) Polymorphisms of p53 Arg72Pro, p73 G4C14-to-A4T14 at Exon 2 and p21 Ser31Arg and the risk of non-Hodgkin’’s Lymphoma in Japanese. Leukemia Lymphoma 45, 957–964 10.1080/10428190310001638878 [DOI] [PubMed] [Google Scholar]
- 32.Li G., Sturgis E.M., Wang L.E., Chamberlain R.M., Amos C.I. and Spitz M.R. (2004) Association of a p73 exon 2 G4C14-to-A4T14 polymorphism with risk of squamous cell carcinoma of the head and neck. Carcinogenesis 25, 1911 10.1093/carcin/bgh197 [DOI] [PubMed] [Google Scholar]
- 33.Li G., Wang L.E., Chamberlain R.M., Amos C.I., Spitz M.R. and Wei Q. (2004) p73 G4C14-to-A4T14 polymorphism and risk of lung cancer. Cancer Res. 64, 6863 10.1158/0008-5472.CAN-04-1804 [DOI] [PubMed] [Google Scholar]
- 34.Niwa Y., Hamajima N., Atsuta Y., Yamamoto K., Tamakoshi A. and Saito T. (2004) Genetic polymorphisms of p73 G4C14-to-A4T14 at exon 2 and p53 Arg72Pro and the risk of cervical cancer in Japanese. Cancer Lett. 205, 55–60 10.1016/j.canlet.2003.11.014 [DOI] [PubMed] [Google Scholar]
- 35.Hu Z., Miao X., Ma H., Tan W., Wang X. and Lu D. (2005) Dinucleotide polymorphism of p73 gene is associated with a reduced risk of lung cancer in a Chinese population. Int. J. Cancer 114, 455–460 10.1002/ijc.20746 [DOI] [PubMed] [Google Scholar]
- 36.Niwa Y., Hirose K., Matsuo K., Tajima K., Ikoma Y. and Nakanishi T. (2005) Association of p73 G4C14-to-A4T14 polymorphism at exon 2 and p53 Arg72Pro polymorphism with the risk of endometrial cancer in Japanese subjects. Cancer Lett. 219, 183–190 10.1016/j.canlet.2004.10.018 [DOI] [PubMed] [Google Scholar]
- 37.Pfeifer D., Arbman G. and Sun X.F. (2005) Polymorphism of the p73 gene in relation to colorectal cancer risk and survival. Carcinogenesis 26, 103–107 10.1093/carcin/bgh305 [DOI] [PubMed] [Google Scholar]
- 38.Choi J.E., Kang H.G., Chae M.H., Kim E.J., Lee W.K. and Cha S.I. (2006) No association between p73 G4C14-to-A4T14 polymorphism and the risk of lung cancer in a Korean population. Biochem. Genet. 44, 543 10.1007/s10528-006-9056-8 [DOI] [PubMed] [Google Scholar]
- 39.Ge H., Wang Y., Cao Y., Zhang X. and Yan L. (2006) Correlation of p73 polymorphisms to genetic susceptibilities to esophageal carcinoma and gastric cardiac carcinoma. Chinese J. Cancer 25, 1351–1355 [PubMed] [Google Scholar]
- 40.Zheng L. (2006) Association of p53 Arg72Pro Polymorphism, p73G4A Polymorphism with Cervical Cancer in Xinjiang Uygur Population, Shihezi University [Google Scholar]
- 41.Chen X., Sturgis E.M., Elnaggar A.K., Wei Q. and Li G. (2008) Combined effects of the p53 codon 72 and p73 G4C14-to-A4T14 polymorphisms on the risk of HPV16-associated oral cancer in never-smokers. Carcinogenesis 29, 2120 10.1093/carcin/bgn191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li C., Chen K., Liu Z., Wang L., Gershenwald J.E. and Lee J.E. (2008) Polymorphisms of TP53 Arg72Pro, but not p73 G4C14>A4TA4 and p21 Ser31Arg, contribute to risk of cutaneous melanoma. J. Invest. Dermatol. 128, 1585–1588 10.1038/sj.jid.5701186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feo E.D., Persiani R., Greca A.L., Amore R., Arzani D. and Rausei S. (2009) A case-control study on the effect of p53 and p73 gene polymorphisms on gastric cancer risk and progression. Mut. Res. 675, 60–65 10.1016/j.mrgentox.2009.02.009 [DOI] [PubMed] [Google Scholar]
- 44.Kang S., Wang D.J., Li W.S., Wang N., Zhou R.M. and Sun D.L. (2009) Association of p73 and MDM2 polymorphisms with the risk of epithelial ovarian cancer in Chinese women. Int. J. Gynecol. Cancer 19, 572–577 10.1111/IGC.0b013e3181a130ab [DOI] [PubMed] [Google Scholar]
- 45.Misra C., Majumder M., Bajaj S., Ghosh S., Roy B. and Roychoudhury S. (2009) Polymorphisms at p53, p73, and MDM2 loci modulate the risk of tobacco associated leukoplakia and oral cancer. Mol. Carcinog. 48, 790–800 10.1002/mc.20523 [DOI] [PubMed] [Google Scholar]
- 46.Arfaoui A.T., Kriaa L.B., El HOA, Ben Hmida M.A., Khiari M. and Khalfallah T. (2010) Association of a p73 exon 2 GC/AT polymorphism with colorectal cancer risk and survival in Tunisian patients. Virchows Archiv. 457, 359–368 10.1007/s00428-010-0942-4 [DOI] [PubMed] [Google Scholar]
- 47.Lee K.E., Hong Y.S., Kim B.G., Kim N.Y., Lee K.M. and Kwak J.Y. (2010) p73 G4C14 to A4T14 polymorphism is associated with colorectal cancer risk and survival. World J. Gastroenterol. 16, 4448 10.3748/wjg.v16.i35.4448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shirai O., Ohmiya N., Taguchi A., Nakamura M., Kawashima H. and Miyahara R. (2010) P53, p21, and p73 gene polymorphisms in gastric carcinoma. Hepatogastroenterology 57, 1595. [PubMed] [Google Scholar]
- 49.Mittal R.D., George G.P., Mishra J., Mittal T. and Kapoor R. (2011) Role of functional polymorphisms of P53 and P73 genes with the risk of prostate cancer in a case-control study from Northern India. Arch. Med. Res. 42, 122–127 10.1016/j.arcmed.2011.03.001 [DOI] [PubMed] [Google Scholar]
- 50.Li-li Z., Xiao-lin P., An-qiang Y., Xing-zheng Z., Xiao-ling W. and Qiu-yuan Z. (2008) Study of p73G4A polymorphism in HPV-associated cervicalcarcinoma in Uigur woman in Xinjiang. China J. Modern Med. 18, 2302–2306 [Google Scholar]
- 51.Craveiro R., Bravo I., Catarino R., Teixeira A.L., Sousa H. and Pereira D. (2012) The role of p73 G4C14-to-A4T14 polymorphism in the susceptibility to cervical cancer. DNA Cell Biol. 31, 224 10.1089/dna.2011.1294 [DOI] [PubMed] [Google Scholar]
- 52.Sun L., Zhu Z., Ni G. and Zhu X. (2012) Correlation of P73 polymorphisms to genetic susceptibilities to cervical carcinoma and Meta-analysis. Basic Clin. Med. 32, 1421–1425 [Google Scholar]
- 53.Zhang X., Cao P., Zhai Y., Zhang H., Cui Y. and Wu Z. (2014) Association between the p73 G4C14-to-A4T14 polymorphism and risk of nasopharyngeal carcinoma: a case control and family-based study. Carcinogenesis. 35, 1977–1982 [DOI] [PubMed] [Google Scholar]
- 54.Kaghad M., Bonnet H., Yang A., Creancier L., Biscan J.C. and Valent A. (1997) Monoallelically expressed gene related to p53 at 1p36, a region frequently deleted in neuroblastoma and other human cancers. Cell 90, 809–819 10.1016/S0092-8674(00)80540-1 [DOI] [PubMed] [Google Scholar]
- 55.Conforti F., Yang A.L., Agostini M., Rufini A., Tucci P. and Nicklisonchirou M.V. (2012) Relative expression of TAp73 and ΔNp73 isoforms. Aging 4, 202–205 10.18632/aging.100441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Murrayzmijewski F., Lane D.P. and Bourdon J.C. (2006) p53|[sol]|p63|[sol]|p73 isoforms: an orchestra of isoforms to harmonise cell differentiation and response to stress. Cell Death Differ. 13, 962 10.1038/sj.cdd.4401914 [DOI] [PubMed] [Google Scholar]
- 57.De V.L., Costanzo A., Barcaroli D., Terrinoni A., Falco M. and Annicchiaricopetruzzelli M. (1998) Two new p73 splice variants, gamma and delta, with different transcriptional activity. J. Exp. Med. 188, 1763–1768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang J., Liu Y.X., Hande M.P., Wong A.C., Jin Y.J. and Yin Y. (2007) TAp73 is a downstream target of p53 in controlling the cellular defense against stress. J. Biol. Chem. 282, 29152–29162 10.1074/jbc.M703408200 [DOI] [PubMed] [Google Scholar]
- 59.Müller M., Schleithoff E.S., Stremmel W., Melino G., Krammer P.H. and Schilling T. (2006) One, two, three—p53, p63, p73 and chemosensitivity. Drug Resist. Update. 9, 288–306 10.1016/j.drup.2007.01.001 [DOI] [PubMed] [Google Scholar]
- 60.Moll U.M. (2004) Slade N. p63 and p73: roles in development and tumor formation11National Cancer Institute. Mol. Cancer Res. 2, 371 [PubMed] [Google Scholar]
- 61.Rodríguez N., Peláez A., Barderas R. and Domínguez G. (2017) Clinical implications of the deregulated TP73 isoforms expression in cancer. Clin. Transl. Oncol. 20, 1–10 [DOI] [PubMed] [Google Scholar]
- 62.Chen J., Li D., Killary A.M., Sen S., Amos C.I. and Evans D.B. (2009) Polymorphisms of p16, p27, p73, and MDM2 modulate response and survival of pancreatic cancer patients treated with preoperative chemoradiation. Ann. Surg. Oncol. 16, 431 10.1245/s10434-008-0220-8 [DOI] [PubMed] [Google Scholar]
- 63.Coates P.J. (2006) Regulating p73 isoforms in human tumours. J. Pathol. 210, 385 10.1002/path.2080 [DOI] [PubMed] [Google Scholar]
- 64.Li G., Sturgis E.M., Wang L., Chamberlain R.M., Amos C.I. and Spitz M.R. (2004) Association of a p73 exon 2 G4C14-to-A4T14 polymorphism with risk of squamous cell carcinoma of the head and neck. Carcinogenesis 25, 1911 10.1093/carcin/bgh197 [DOI] [PubMed] [Google Scholar]
- 65.Dingerdissen H.M., Torcivia-Rodriguez J., Hu Y., Chang T.C., Mazumder R. and Kahsay R. (2018) BioMuta and BioXpress: mutation and expression knowledgebases for cancer biomarker discovery. Nucleic Acids Res. 46, D1128–D1136 10.1093/nar/gkx907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Arfaoui A.T., Ben Mahmoud L.K., Ben H.A., Khiari M., Mohamed A.L. and Chaar I. (2010) Relationship between p73 polymorphism and the immunohistochemical profile of the full-length (TAp73) and NH2-truncated (ΔNp73) isoforms in Tunisian patients. Appl. Immunohistochem. Mol. Morphol. 18, 546–554 10.1097/PAI.0b013e3181e9fe58 [DOI] [PubMed] [Google Scholar]
- 67.Liang X., Chen B. and Zhong J. (2017) Association of P73 polymorphisms with susceptibilities of cervical carcinoma: a meta-analysis. Oncotarget 8, 57409–57413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu H., Liang Y., Liao H., Li L. and Wang H. (2014) Association of p73 G4C14-to-A4T14 polymorphism with lung cancer risk. Tumour Biol. 35, 9311–9316 10.1007/s13277-014-2061-3 [DOI] [PubMed] [Google Scholar]
- 69.Yu X.J., Fang F. and Xie J. (2011) Relationship between TP73 polymorphism (G4C14-A4T14) and cancer risk: a meta-analysis based on literatures. Gene 484, 42–46 10.1016/j.gene.2011.05.022 [DOI] [PubMed] [Google Scholar]