Abstract
Background:
Bariatric surgery is underutilized.
Objectives:
To identify factors associated with eligible patient dropout from bariatric surgery.
Setting:
University hospital, United States.
Methods:
Eligible candidates were identified after multidisciplinary review committee (MRC) from all patients (n=484) who attended a bariatric surgery informational session (BIS) at a single-center academic institution in 2015. We compared patients who underwent surgery within 2 years of BIS to those who did not (i.e. dropped out) by evaluating patient, insurance, and program-specific variables. Univariate analyses and multivariable regressions were performed to identify factors associated with patient dropout among eligible candidates.
Results:
We identified 307 (63%) patients who underwent MRC. Thirty-three (11%) patients were deemed poor candidates and surgery was not recommended. Among eligible candidates, 82 (30%) dropped out from the program. Factors independently associated with eligible patient dropout included: coronary artery disease (OR 0.13[0.02–0.66];p=0.014), hypertension (OR 0.46[0.24–0.87];p=0.017), time from BIS to MRC (OR 0.99[0.99–0.99];p=0.002), 3 months of medically supervised weight loss documentation (OR 0.09[0.02–0.51];p=0.007), endocrinology clearance (OR 0.26[0.09–0.76];p=0.014), hematology clearance (OR 0.37[0.14–0.95];p=0.039), urine drug screen testing (OR 0.31[0.13–0.72];p=0.006), additional psychological evaluation (OR 0.43[0.20–0.93];p=0.031), and required extra sessions with the dietitian (OR 0.39[0.17– 0.92];p=0.032). Thirty-three (6.8%) patients underwent surgery at another institution and 42% of these patients lived more than 50 miles from attended BIS site.
Conclusions:
Twenty-seven percent of patients did not undergo bariatric surgery at their initial site of evaluation despite being considered eligible candidates after MRC. Dropout was independently associated with patient, insurance, and program-specific variables which may represent barriers to care amenable to improvement.
Keywords: Bariatric surgery, patient characteristics, insurance requirements, bariatric program requirements, patient dropout, failure to progress to bariatric surgery
Graphical Abstract

Eligible Candidate Dropout from Bariatric Surgery is Independently Associated with Patient, Insurance, and Bariatric Program-specific Factors. MRC, multidisciplinary review committee; CAD, coronary artery disease; HTN, hypertension; BIS, bariatric informational session; MSWLD, medically supervised weight loss documentation.
Introduction
Bariatric surgery remains the most effective therapy for severe obesity and related comorbidities. [1–5] Despite these well-stablished benefits, less than one percent of adult patients undergo bariatric surgery in the United States (US) annually. [6–8] Meanwhile, the prevalence of obesity continues to grow both globally and in the US, where over 36% of adults and 17% of youth are affected. [9,10] According to the National Institutes of Health (NIH), patients who are eligible for bariatric surgery must have a body mass index (BMI) over 40 kg/m2 or over 35 kg/m2 plus obesity-related comorbidities. Patients are also required to be well-informed of the risks and benefits of surgery, have failed non-surgical attempts at weight loss, and be committed to lifelong healthy eating. [11]
In order to address these requirements and allow for insurance coverage, bariatric surgery programs typically offer a group session to inform potential patients about surgical options for obesity. Next, interested patients undergo a medical, dietary, and psychological evaluation in order to ascertain suitability in a multidisciplinary fashion. In addition, some patients may be required by their insurance carrier to undergo 3, 6 or 12 months of documented medically supervised weight loss. Moreover, some patients may require further testing or consultation with subspecialists as their initial bariatric surgery evaluation may uncover additional health problems. Given the complexity and duration of the current pathway to bariatric surgery, it is unclear how many patients continue to pursue surgery even after being considered a suitable candidate by a bariatric surgery program.
Herein we explored the rate of bariatric surgery utilization within a group of patients who attended a bariatric informational session (BIS) and were considered eligible candidates after a multidisciplinary review committee (MRC). We compared patients who underwent surgery to those who did not to identify patient, insurance, and program-specific variables that were associated with patients who dropped out.
Methods
Data Source, Study Population, and Data Collection
This study is based on the analysis of patient data collected from a single academic center bariatric program. This research was approved by the Institutional Review Board and was in compliance with the Health Information Portability and Accountability Act. All adults who attended a BIS in 2015 were identified (n=484). Patients who completed all of their evaluations (medical, dietary and psychological) underwent MRC and eligible patients were offered laparoscopic sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB). Patients who had uncompensated cardiac, pulmonary, renal or hepatic disease, were not able to tolerate anesthesia, or attempted suicide within 1 year were not considered surgical candidates. Patients who failed to undergo surgery within 2 years of their initial BIS were considered to have dropped out. Dates of BIS, MRC, and surgery were collected and the length of time, in days, from BIS to MRC and to surgery calculated. Data were abstracted for all patients who underwent all clinic evaluations within the bariatric surgery program using the electronic medical record (EMR). Data included age, gender, body mass index (BMI), and diagnosed comorbidities including coronary artery disease (CAD), asthma, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), diabetes, gastroesophageal reflux disease (GERD), hyperlipidemia (HL), hypertension (HTN), psychological diagnoses, arrhythmias, and active smoking. Patient Zone Improvement Plan (ZIP) codes were also obtained from the EMR and were used to calculate the distance between their residence and BIS/clinic site. Insurance and program specific requirements were obtained from a letter that was mailed to the patient after undergoing MRC. Insurance-specific variables included: type of insurance (Blue Cross Blue Shield/Blue Complete Network—BCBS/BCN, other private insurance, or Medicare), duration of medically supervised weight loss documentation (MSWLD) and requirements including a primary care physician letter, psychological, cardiology, and pulmonology evaluations, alcohol/drug screening, esophagogastroduodenoscopy (EGD), nicotine testing, thyroid function testing, and 1-year free from substance abuse. Bariatric surgery program-specific variables included: laboratory testing (cotinine level, urine drug/alcohol screen, Helicobacter pylori breath test), imaging and additional testing (electrocardiogram, echocardiogram, cardiac stress test, abdominal ultrasound, abdominal computer tomography, EGD, esopahgram, upper gastrointestinal study, colonoscopy), consultation with specialists (sleep clinic, psychological, cardiology, endocrinology, neurology, pulmonology, nephrology, hematology, and gastroenterology) and social/financial/lifestyle/educational tasks (preparation of a financial/childcare/caregiver plan, attendance of a support person to clinic visits or nutrition education class, attendance of the bariatric program run support group meeting, required extra sessions with a dietitian, required 4 weeks of a preoperative low calorie liquid diet, required ambulation to all clinic visits, and required that the patient pursue sleeve gastrectomy only).
Patients who dropped out after undergoing a BIS or MRC and underwent surgery at another institution were identified by querying a statewide, bariatric-specific clinical registry described elsewhere. [12] Data obtained from these patients included procedure type and distance from initial BIS/MRC evaluation and patient residence.
Study Design and Statistical Analysis
The primary outcome of this study was patient dropout after being considered an eligible candidate for bariatric surgery following MRC. Secondary outcomes included overall dropout defined as the proportion of patients initially presenting to BIS but failing to progress to surgery after excluding unsuitable surgical candidates and patient, insurance, and program- specific factors. We identified all patients that underwent MRC (n=307) and compared patient, insurance, and program-specific variables between those who underwent surgery (n=192) and those who dropped out from our program (n=82). Univariate analyses and multivariable regression were performed to identify factors predictive of eligible patient dropout from surgery after MRC.
Sample characteristics are presented as means ± standard deviations (SD) or medians with interquartile ranges as appropriate for continuous variables and frequencies and percentages for categorical variables. Individual univariate comparisons for continuous variables were compared surgery (1=yes, 0=no) via independent samples t-test or Mann- Whitney tests and categorical variables were compared by using Pearson chi-squared tests or Fisher’s exact test as appropriate. Variables found to be significant at p<0.05 were further examined in a multivariable logistic regression to determine independent predictor variables while accounting for others. P values <0.05 were identified as statistically significant and all analyses were performed in STATA13 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
Results
A total of 484 patients underwent BIS and 307 (63%) patients underwent MRC. Thirty- three (11%) patients were not considered candidates for surgery. Among eligible candidates, 82 (30%) patients dropped out and 192 (70%) patients underwent surgery (176, SG and 16, RYGB). Average time from BIS to MRC was 122 (±121) days and from MRC to surgery was 175 (±93) days (Figure 1).
Figure 1.
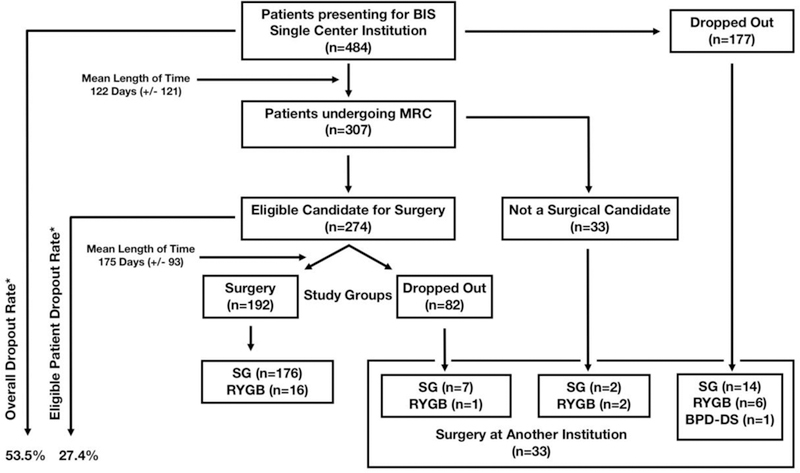
Design, Overall, and Eligible Patient Dropout Rates. BIS indicates bariatric informational session; MRC, multidisciplinary review committee; SG, sleeve gastrectomy; RYGB, Roux-en-Y gastric bypass; BPD-DS, biliopancreatic diversion with duodenal switch; *, rates account for patients undergoing surgery at another institution.
Characteristics of patients who underwent surgery at our institution and those who dropped out are compared in Table 1. The groups were similar in terms of age, sex, and BMI. Eligible patients who dropped out had a higher rate of CAD (11.0% vs. 1.0%; p<0.0001), HTN (63.4% vs. 42.7%; p=0.002), active smoking (18.3% vs. 7.2%; p=0.007), and a longer waiting period between BIS and MRC (164 days vs. 103 days; p=0.004) when compared to patients who underwent surgery.
Table 1.
Patient Characteristics by Group
| Characteristic | Surgery (n=192) | Dropped Out (n=82) | p-value |
|---|---|---|---|
| Age (years); mean (± SD) | 44.9 (±11.8) | 46.1 (±12.3) | 0.472 |
| Female; % | 82.8 | 73.1 | 0.068 |
| BMI (kg/m2); mean (± SD) | 46.9 (±7.3) | 47.5 (±8.0) | 0.604 |
| Comorbidity | |||
| CAD; % | 1.0 | 10.9 | <0.0001 |
| Asthma; % | 29.1 | 29.2 | 0.986 |
| CHF; % | 0.5 | 2.4 | 0.214 |
| COPD; % | 2.0 | 6.1 | 0.133 |
| Diabetes; % | 30.2 | 29.2 | 0.876 |
| GERD; % | 61.4 | 63.4 | 0.760 |
| HLD; % | 44.7 | 46.3 | 0.813 |
| HTN; % | 42.7 | 63.4 | 0.002 |
| Psychological; % | 74.4 | 63.4 | 0.064 |
| Arrhythmia; % | 5.2 | 7.3 | 0.495 |
| OSA; % | 60.4 | 48.7 | 0.075 |
| Smoking; % | 7.2 | 18.2 | 0.007 |
| Distance from clinic (miles); mean (± SD) | 19.7 (±19.3) | 18.4 (±17.2) | 0.614 |
| Days from BIS to MRC; mean (± SD) | 103.7 (±94.2) | 164.2 (±160.2) | 0.004 |
| On-line informational meeting; % | 2.0 | 3.6 | 0.431 |
SD indicates standard deviation; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; GERD, gastroesophageal reflux disease; HLD, hyperlipidemia; HTN, hypertension; OSA, obstructive sleep apnea; BIS, bariatric informational session; MRC, multidisciplinary review committee
Insurance-specific requirements for each group are contrasted in Table 2. Patients dropping out were less likely to have private insurance (81.2% vs. 91.1%; p=0.022) including BCBS/BCN (63.7% vs. 82.2%; p<0.001) and more likely to have private insurance other than BCBS/BCN (17.5% vs. 8.9%; p=0.042) or Medicare (8.9% vs. 18.7%; p=0.022). Though insurances for patients dropping out were less likely to offer a waiver for MSWLD than payers for patients undergoing surgery (59.7% vs. 75.5%; p=0.009), the proportion of patients meeting this criterium and having this requirement waived did not differ between groups. Duration of MSWLD varied between groups with patients dropping out more likely to have 3 months (7.3% vs. 1.0%; p=0.01) and less likely to have 6 months of MSWLD (69.5% vs. 88.0%; p<0.001).
Table 2.
Insurance Requirements by Group
| Characteristic | Surgery (n=192) | Dropped Out (n=82) | p-value |
|---|---|---|---|
| Insurance | |||
| Private; % | 91.1 | 81.2 | 0.022 |
| BCBS/BCN; % | 82.2 | 63.7 | <0.001 |
| Other private; % | 8.9 | 17.5 | 0.042 |
| Medicare; % | 8.9 | 18.7 | 0.022 |
| Requirement | |||
| MSWLD required; % | 91.1 | 84.1 | 0.089 |
| MSWLD waiver offered for BMI > 50 kg/m2; % | 75.5 | 59.7 | 0.009 |
| MSWLD waived for BMI > 50 kg/m2; % | 2.0 | 6.1 | 0.088 |
| Duration of MSWLD | 0.001 | ||
| No MSWLD; % | 8.8 | 15.8 | 0.089 |
| 3 months MSWLD; % | 1.0 | 7.3 | 0.01 |
| 6 months MSWLD; % | 88.0 | 69.5 | <0.001 |
| 12 months MSWLD; % | 2.0 | 7.3 | 0.07 |
| PCP letter; % | 100.0 | 100.0 | 1.000 |
| Psychological evaluation; % | 1.0 | 1.2 | 0.214 |
| Cardiology evaluation; % | 9.3 | 9.7 | 0.921 |
| Pulmonology evaluation; % | 9.3 | 9.7 | 0.921 |
| Alcohol/drug screen; % | 9.3 | 10.9 | 0.684 |
| EGD; % | 9.3 | 9.7 | 0.921 |
| Nicotine testing; % | 0.5 | 1.2 | 0.506 |
| 1-year substance abuse free; % | 0.5 | 0.0 | 0.515 |
| TSH; % | 9.3 | 9.7 | 0.921 |
BCBS/BCN indicates Blue Cross & Blue Shield/Blue Cross Network; MSWLD, medically supervised weight loss documentation; BMI, body mass index; PCP, primary care physician; EGD, esophagogastroduodenoscopy; TSH, thyroid stimulating hormone
Program-specific requirements are compared between patients who dropped out and those undergoing surgery in Table 3. Laboratory tests including cotinine level (23.1% vs. 10.4%; p=0.006) and urine drug screen (UDS) (25.6% vs. 7.8%; p<0.001) were more frequently requested from patients who dropped out compared with those who had surgery. Patients dropping out were also more likely to be referred for specialist assessment including endocrinology (14.6% vs. 4.1%; p=0.002), nephrology (9.7% vs. 1.5%; p=0.004), hematology (14.6% vs. 6.7%; p=0.038), and additional psychological evaluation (25.6% vs. 13.0%; p=0.011) than patients undergoing surgery. Other program requirements including having patients provide a financial plan (35.3% vs. 22.4%; p=0.026), being accompanied by a support person during clinic visits (8.5% vs. 2.6%; p=0.047) and nutrition education class (48.7% vs. 32.2%; p=0.01), attending extra sessions with the Registered Dietitian (RD) (21.9% vs. 9.9%; p=0.007), and being able to walk to appointments (7.3% vs. 1.5%; p=0.023) were more frequently requested of patients dropping out than from those proceeding with surgery. Altogether, patients who dropped out were faced with more overall program requirements (7.2±2.9 vs. 5.3±2.4; p<0.0001) including laboratory requirements (0.6±0.9 vs. 0.2±0.6; p=0.0007), specialists’ consultations (1.8±1.4 vs. 1.1±1.1; p<0.0001), and other program requirements (4.0%±1.6 vs. 3.2±1.1; p<0.0001) compared to those undergoing surgery.
Table 3.
Program Requirements by Group
| Requirement | Surgery (n=192) | Dropped Out (n=82) | p-value | |
|---|---|---|---|---|
| Laboratory | ||||
| Cotinine level; % | 10.4 | 23.1 | 0.006 | |
| UDS level; % | 7.8 | 25.6 | <0.001 | |
| ETOH level; % | 4.6 | 7.3 | 0.381 | |
| Urea breath test; % | 3.1 | 3.6 | 1 | |
| Imaging and special tests | ||||
| EKG; % | 0.5 | 2.4 | 0.214 | |
| Echo; % | 5.2 | 4.8 | 1 | |
| Stress test; % | 4.1 | 9.7 | 0.071 | |
| Abdominal US; % | 6.7 | 8.5 | 0.607 | |
| Abdominal CT; % | 2.6 | 4.8 | 0.459 | |
| EGD; % | 25.5 | 25.6 | 0.988 | |
| Esophagram; % | 5.2 | 4.8 | 1 | |
| UGI; % | 3.1 | 3.6 | 1 | |
| Colonoscopy; % | 7.2 | 6.1 | 0.802 | |
| Specialists | ||||
| Sleep clinic/CPAP compliance; % | 33.3 | 43.9 | 0.096 | |
| Additional psychological evaluation; % | 13.0 | 25.6 | 0.011 | |
| Cardiology clearance; % | 21.8 | 32.9 | 0.054 | |
| Endocrinology clearance; % | 4.1 | 14.6 | 0.002 | |
| Neurology clearance; % | 3.6 | 6.1 | 0.352 | |
| Pulmonology clearance; % | 11.4 | 15.8 | 0.318 | |
| Nephrology clearance; % | 1.5 | 9.7 | 0.004 | |
| Hematology clearance; % | 6.7 | 14.6 | 0.038 | |
| Gastroenterology clearance; % | 10.4 | 12.2 | 0.666 | |
| Other | ||||
| Social and financial support | ||||
| Financial plan; % | 22.4 | 35.3 | 0.026 | |
| Childcare plan; % | 10.9 | 13.4 | 0.559 | |
| Caregiver plan; % | 25.5 | 32.9 | 0.21 | |
| Support person during clinic visits; % | 2.6 | 8.5 | 0.047 | |
| SO/family required at NE class; % | 32.2 | 48.7 | 0.01 | |
| SGM 1; % | 99.4 | 100.0 | 0.513 | |
| SGM 2; % | 100.0 | 100.0 | 1 | |
| Education, lifestyle, and surgical | ||||
| Extra sessions with RD; % | 9.9 | 21.9 | 0.007 | |
| 4 weeks of liquid diet; % | 20.3 | 28.0 | 0.161 | |
| Must walk; % | 1.5 | 7.3 | 0.023 | |
| SG only option; % | 3.1 | 6.1 | 0.314 | |
| All program requirements; mean (± SD) | 5.3(2.4) | 7.2(2.9) | <0.0001 | |
| Laboratory program requirements; mean (± SD) | 0.2(0.6) | 0.6(0.9) | 0.0007 | |
| Imaging program requirements; mean (± SD) | 0.6(0.8) | 0.7(0.8) | 0.4139 | |
| Specialists program requirements; mean (± SD) | 1.1(1.1) | 1.8(1.4) | <0.0001 | |
| Other program requirements; mean (± SD) | 3.2(1.1) | 4.0(1.6) | <0.0001 | |
UDS indicates urine drug screen; ETOH, ethanol; EKG, electrocardiogram; US, ultrasound; CT, computerized tomography; EGD, esophagogastroduodenoscopy, UGI, upper gastrointestinal series; CPAP, continuous positive airway pressure therapy; SO, significant other; NE, nutrition education; SGM, support group meeting; RD, registered dietitian; SG, sleeve gastrectomy
Odds ratios derived from multivariable regression of patient, insurance, and program- specific factors are summarized in Table 4. After controlling for age, sex, BMI, and distance from clinic, characteristics associated with decreased odds (95%CI; p value) of undergoing surgery included CAD 0.13 (0.02–0.66; p=0.014), HTN 0.46 (0.24–0.87; p=0.017), time from BIS to MRC 0.99 (0.99–0.99; p=0.002), 3 months of MSWLD 0.09 (0.02–0.51; p=0.007), endocrinology clearance 0.26 (0.09–0.76; p=0.014), hematology clearance 0.37 (0.14–0.95; p=0.039), UDS 0.31 (0.13–0.72; p=0.006), additional psychological evaluation 0.43 (0.20–0.93; p=0.031), and extra sessions with RD 0.39 (0.17–0.92] p=0.032).
Table 4.
Multivariable Regression of Patient, Insurance, and Program Factors
| Characteristic* | Odds of undergoing surgery (95% CI) | p-value |
|---|---|---|
| Patient factors | ||
| CAD | 0.13 (0.02–0.66) | 0.014 |
| HTN | 0.46 (0.24–0.87) | 0.017 |
| Days from BIS to MRC | 0.99 (0.99–0.99) | 0.002 |
| Insurance requirements | ||
| 3 months MSWLD | 0.09 (0.02–0.51) | 0.007 |
| Program requirements | ||
| Endocrinology clearance | 0.26 (0.09–0.76) | 0.014 |
| Hematology clearance | 0.37 (0.14–0.95) | 0.039 |
| UDS level | 0.31 (0.13–0.72) | 0.006 |
| Additional psychological evaluation | 0.43 (0.20–0.93) | 0.031 |
| Extra sessions with RD | 0.39 (0.17–0.92) | 0.032 |
CI indicates confidence interval; CAD, coronary artery disease; HTN, hypertension; BIS, bariatric informational session; MRC, multidisciplinary review committee; MSWLD, medically supervised weight loss documentation; UDS, urine drug screen; RD, registered dietitian
Variables with p value <0.05 after stepwise regression shown. All variables with univariate p value <0.05 were included
Out of 484 patients attending BIS at our bariatric program, 33 (7%) underwent surgery at another institution. Among these patients, 21 (64%) had dropped out after BIS but before undergoing MRC, while 8 (24%) dropped out after being considered eligible surgical candidates. Interestingly, 4 (12%) patients considered poor surgical candidates after MRC by our program underwent surgery elsewhere in the state (Figure 1). Forty-two percent of patients who underwent surgery at another institution lived 50 or more miles away from our center.
Discussion
In this study, we explore the impact of patient, insurance, and program-specific factors on dropout rates for bariatric surgery among patients already considered suitable candidates by a bariatric surgery program. Our data show that approximately one quarter of patients failed to pursue surgery after MCR and that these patients tended to have more comorbidities, Medicare or private insurance other than BCBS/BCN, longer wait times from BIS to MRC, insurance-mandated MSWLD, and more laboratory and subspecialty evaluations as required by the bariatric surgery program. Identifying the reasons behind patient dropout is an important step to improving bariatric surgery utilization among patients who need it most.
Reported dropout rates for bariatric surgery among eligible candidates in the US range from 27.2 to 30.8%, which is similar to the findings in our study. [13,14] In addition, we report an overall dropout rate after initial BIS of 53.5%. Likewise, similar rates anywhere from 43.9 to 51.1% have been reported by others. [15–17] Interestingly, equivalent rates ranging from 47.7 to 48.6% have also been reported in Canada despite differences in healthcare payment models. [18,19] Given these similarities, it is possible that patients’ attitudes, motivations, and perceptions regarding surgery may play a more significant role in early dropout (i.e. prior to initial evaluations and MRC) than healthcare policy. Further studies addressing these are needed and may help explain why overall utilization of bariatric surgery is so low.
We found that dropout was higher among smokers, which is not surprising as our program requires patients to quit smoking preoperatively with a negative urine cotinine and some patients may be unwilling or unable to do so. Smoking cessation is a common requirement given the link between tobacco use and worse outcomes. [20,21] Not surprisingly, others have also noted an association between smoking and patient dropout. [16,22] We also found that CAD and HTN were independently associated with dropping out. Earlier reports have not shown an association between HTN and patient dropout and to date CAD is a variable that has not been captured. [16,22] We hypothesize that HTN and CAD are associated with greater need for cardiology evaluation, which may prolong the time to bariatric surgery and result in patient dropout. Thus, streamlining access to subspecialty services as well as access to tobacco cessation programs may decrease dropout rates among eligible patients.
In addition, the type of insurance and length of required MSWLD was associated with patient dropout. Patients with Medicare and private insurance other than BCBS/BCN were more likely to drop out as did patients who required 3 months of MSWLD. Likewise, Love et al., [16] demonstrated that patients with private insurance were more likely to proceed with surgery. Also, their study suggested that longer duration of MSWLD was associated with patient dropout. It is important to note that BCBS/BCN is the major payer at our center, insuring 76.6% of patients included in this sample and that this payer requires 6 months of MSWLD. Thus, it is likely that the familiarity of our program with the policies and procedures of this major insurance carrier resulted in lower patient dropout despite requiring a longer period of MSWLD. Nevertheless, there are no data supporting insurance-mandated MSWLD prior to bariatric surgery, a requirement which is inconsistently and arbitrarily applied to eligible patients seeking a lifesaving treatment. [23] Our study advocates for collaboration between bariatric surgery programs and payers to improve patient access to surgery.
Finally, our report offers a detailed analysis of program-specific requirements that influenced eligible patient dropout. Our data indicate that patients who faced additional laboratory testing, specialist evaluation, and other requirements targeting social and financial support, education, and lifestyle modifications were more likely to drop out, even though it was considered necessary for postoperative success. Several studies have shown an association between psychological comorbidities, particularly substance abuse, and patient dropout. [13,15,18,24] Ongoing psychological therapy has also been associated with outstanding program requirements and may result in patient dropout. [25] Given that preoperative optimization of both medical and psychological diagnoses can improve outcomes for elective surgery, our study highlights how a multidisciplinary bariatric surgery program can impose its own requirements based on their clinical evaluation. As such, we feel that it is unnecessary for insurance to mandate specific requirements that are not based on clinical necessity. However, we do recognize that additional requirements, even when clinically necessary, can increase wait times for surgery and thus contribute to higher patient dropout rates. Patients’ perceived barriers to care may also influence their decision to switch programs, as eight eligible candidates (9.8%) did so in our study. Overall, our findings highlight the need for improved access to specialty care services including registered dietitians and mental health professionals.
When interpreting these data some limitations should be considered. This a single- center study with a major insurance payer which may limit generalizability. Although we were able to obtain granular data on program-specific requirements applied to patients eligible for bariatric surgery, further studies that include a wide range of practice types (i.e. academic and private) are necessary. Also, our data does not capture the exact time patients started and finished MSWLD relative to their bariatric surgery evaluations, which could have biased our analysis of this insurance requirement. Lastly, we did not explore wait times for specialists’ evaluations or patient perceptions of bariatric surgery, which may have affected dropout rates. Nevertheless, this study explores numerous program-specific factors which have not been examined in prior studies and are not captured by current data registries.
Conclusions
Approximately one quarter of patients failed to pursue bariatric surgery after being considered eligible candidates by a multidisciplinary bariatric surgery program. Dropout rates were independently associated with cardiovascular disease, insurance-mandated MSWLD, and additional program-specific requirements such as substance use cessation and subspecialty evaluations. Efficient coordination of care along with elimination of arbitrary requirements may help improve dropout among eligible candidates for bariatric surgery.
Highlights.
Twenty-seven percent of eligible candidates drop out from bariatric surgery.
Heart disease and time to multidisciplinary review were associated with dropout.
Insurance-mandated medical weight loss documentation was associated with dropout.
Specialist evaluation and substance use cessation were associated with dropout
Acknowledgements and sources of support:
Supported by a Ruth L. Kirschstein National Research Service Award (T32) grant awarded to Dr. Justin B. Dimick through the National Institutes of Health (1T32DK108740-01).
One of the authors receives salary support from Blue Cross Blue Shield for leadership and participation in statewide quality improvement initiatives. The remaining authors have no commercial associations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
References
- [1].Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–37. doi:10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- [2].Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–76. doi:10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 2012;366:1577–85. doi:10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- [4].Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet Lond Engl 2015;386:964–73. doi:10.1016/S0140-6736(15)00075-6. [DOI] [PubMed] [Google Scholar]
- [5].Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes. N Engl J Med 2017;376:641–51. doi:10.1056/NEJMoa1600869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Funk LM, Jolles S, Fischer LE, Voils CI. Patient and Referring Practitioner Characteristics Associated With the Likelihood of Undergoing Bariatric Surgery: A Systematic Review. JAMA Surg 2015;150:999–1005. doi:10.1001/jamasurg.2015.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes 2005 2013;37:889–91. doi:10.1038/ijo.2012.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Nguyen NT, Masoomi H, Magno CP, Nguyen X-MT, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg 2011;213:261–6. doi:10.1016/j.jamcollsurg.2011.04.030. [DOI] [PubMed] [Google Scholar]
- [9].Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief 2015:1–8. [PubMed]
- [10].WHO | Obesity and overweight n.d http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed August 15, 2015).
- [11].Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr 1992;55:615S–619S. [DOI] [PubMed] [Google Scholar]
- [12].Finks JF, English WJ, Carlin AM, Krause KR, Share DA, Banerjee M, et al. Predicting Risk for Venous Thromboembolism With Bariatric Surgery: Results From the Michigan Bariatric Surgery Collaborative. Ann Surg 2012;255:1100–4. doi:10.1097/SLA.0b013e31825659d4. [DOI] [PubMed] [Google Scholar]
- [13].Marek RJ, Tarescavage AM, Ben-Porath YS, Ashton K, Heinberg LJ, Rish JM. Associations between psychological test results and failure to proceed with bariatric surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2017;13:507–13. doi:10.1016/j.soard.2016.09.007. [DOI] [PubMed] [Google Scholar]
- [14].Mahony D Bariatric surgery attrition secondary to psychological barriers. Clin Obes 2013;3:32–8. doi:10.1111/cob.12013. [DOI] [PubMed] [Google Scholar]
- [15].Sala M, Haller DL, Laferrère B, Homel P, McGinty JJ. Predictors of Attrition Before and After Bariatric Surgery. Obes Surg 2017;27:548–51. doi:10.1007/s11695-016-2510-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Love KM, Mehaffey JH, Safavian D, Schirmer B, Malin SK, Hallowell PT, et al. Bariatric surgery insurance requirements independently predict surgery dropout. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2017;13:871–6. doi:10.1016/j.soard.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sadhasivam S, Larson CJ, Lambert PJ, Mathiason MA, Kothari SN. Refusals, denials, and patient choice: reasons prospective patients do not undergo bariatric surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2007;3:531–5; discussion 535–536. doi:10.1016/j.soard.2007.07.004. [DOI] [PubMed] [Google Scholar]
- [18].Diamant A, Milner J, Cleghorn M, Sockalingam S, Okrainec A, Jackson TD, et al. Analysis of patient attrition in a publicly funded bariatric surgery program. J Am Coll Surg 2014;219:1047–55. doi:10.1016/j.jamcollsurg.2014.08.003. [DOI] [PubMed] [Google Scholar]
- [19].Pitzul KB, Jackson T, Crawford S, Kwong JCH, Sockalingam S, Hawa R, et al. Understanding disposition after referral for bariatric surgery: when and why patients referred do not undergo surgery. Obes Surg 2014;24:134–40. doi:10.1007/s11695-013-1083-z. [DOI] [PubMed] [Google Scholar]
- [20].Haskins IN, Nowacki AS, Khorgami Z, Schulz K, Heinberg LJ, Schauer PR, et al. Should recent smoking be a contraindication for sleeve gastrectomy? Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2017;13:1130–5. doi:10.1016/j.soard.2017.02.028. [DOI] [PubMed] [Google Scholar]
- [21].Inadomi M, Iyengar R, Fischer I, Chen X, Flagler E, Ghaferi AA. Effect of patient-reported smoking status on short-term bariatric surgery outcomes. Surg Endosc 2017. doi:10.1007/s00464-017-5728-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Taylor T, Wang Y, Rogerson W, Bavin L, Sharon C, Beban G, et al. Attrition after Acceptance onto a Publicly Funded Bariatric Surgery Program. Obes Surg 2018. doi:10.1007/s11695-018-3195-y. [DOI] [PubMed] [Google Scholar]
- [23].Kim JJ, Rogers AM, Ballem N, Schirmer B, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS updated position statement on insurance mandated preoperative weight loss requirements. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2016;12:955–9. doi:10.1016/j.soard.2016.04.019. [DOI] [PubMed] [Google Scholar]
- [24].Sockalingam S, Cassin S, Crawford SA, Pitzul K, Khan A, Hawa R, et al. Psychiatric predictors of surgery non-completion following suitability assessment for bariatric surgery. Obes Surg 2013;23:205–11. doi:10.1007/s11695-012-0762-5. [DOI] [PubMed] [Google Scholar]
- [25].Merrell J, Ashton K, Windover A, Heinberg L. Psychological risk may influence drop-out prior to bariatric surgery. Surg Obes Relat Dis Off J Am Soc Bariatr Surg 2012;8:463–9. doi:10.1016/j.soard.2012.01.018. [DOI] [PubMed] [Google Scholar]


