Abstract
Background:
The goal of this work was to examine associations among childhood trauma, combat trauma and substance use (alcohol problems, frequent heavy drinking (FHD), current cigarette smoking, and current/lifetime drug use) and the interaction effects of childhood trauma and combat exposure on those associations among National Guard/Reserve soldiers.
Methods
Participants (n=248) completed an electronic survey asking questions about their military experiences, physical and mental health, and substance use. Childhood trauma and combat exposure were examined jointly in regression models, controlling for age, marital satisfaction, and number of deployments.
Results:
Childhood trauma was associated with current drug use (trend level, OR = 1.44, 95% CI: 0.97, 2.14; p = .072) in the main effect model; however, there was not a significant interaction with combat. Combat exposure had a significant interaction with childhood trauma on alcohol problems (b = −0.56, 95% CI: −1.12, −0.01; p = .048), FHD (b = −0.27, 95% CI: −0.47, −0.08; p = .007), and lifetime drug use (OR = 1.78, 95% CI: 1.04, 3.04; p = .035). There were no associations with either of the trauma measures and current cigarette smoking.
Conclusions:
Our results demonstrate that childhood and combat trauma have differential effects on alcohol use, such that combat trauma may not add to the effect on alcohol use in those with greater child maltreatment, but may contribute to greater alcohol use among those with low child maltreatment. As expected, childhood and combat trauma had synergistic effects on lifetime drug use. Screening for multiple types of trauma prior to enlistment and/or deployment may help to identify at-risk individuals and allow time for early intervention to prevent future adverse outcomes.
Keywords: Childhood trauma, combat trauma, military, substance use
The connection among deployment, combat trauma, and substance use has been well-established in military populations.1–8 For example, deployment to Iraq and/or Afghanistan was found to greatly increase the incidence of substance use disorders, particularly among service members in combat positions.9 However, combat exposure and deployment are not the only factors that need to be considered to understand substance use among soldiers. Research in both animals and humans has repeatedly shown that chronic or repeated stress over the life course is crucially important to consider in examining substance use and addiction.10–12 Evidence from civilian populations has demonstrated that adult substance use is strongly related to childhood trauma, often exacerbated by more recent adult trauma.13–15 Childhood trauma, coupled with repeated stress after childhood, has been linked to substance use vulnerability, including initiation of use, escalation of use, problematic use, less motivation to quit and more frequent relapse.11 Early trauma, experienced during childhood, has been related to disordered brain function that may persist into adulthood.16 Early trauma appears to sensitize neural response pathways, which may lead to elevated risk for substance use initiation and risky behaviors by impacting impulsivity, decision making, and stress and reward systems; which may be exacerbated by additional traumatic exposures later in life.11Furthermore, effects of cumulative stress appear to be dose-dependent, such that the cumulative number of events experienced predicts risk of alcohol and drug dependence.12
Early trauma exposures, prior to military experiences, are therefore important to consider when examining outcomes among military service members. Evidence regarding mental health outcomes, particularly posttraumatic stress disorder (PTSD), suggests that service members who experienced childhood and other non-military-related trauma in addition to military trauma, are at greater risk for adverse outcomes.17–20 Several studies have found that childhood trauma is associated with greater risk for PTSD and/or greater PTSD symptom severity among deployed soldiers.17–21 Specifically, in large pre- and post-deployment samples of soldiers, having experienced two or more adverse childhood events was associated with increased risk of depression and PTSD.17 Childhood physical assault greatly increased the risk of PTSD and PTSD combined with other comorbid disorders, such as major depressive disorder.21 Similar associations between childhood abuse and/or adverse experiences and higher rates of PTSD and/or more severe PTSD symptoms have been found in US Army active duty22 and Canadian military active duty members.19 Veterans who experienced relapse after PTSD treatment had significantly higher rates of childhood abuse, both physical and sexual, as well as higher rates of substance use.23 Childhood maltreatment has also been shown to be related to alcohol misuse24 among active duty soldiers after returning from deployment. Furthermore, childhood adversity was linked to a variety of negative outcomes, including heavy drinking among British active duty soldiers.25 Griffith demonstrated that National Guard and reserve soldiers were 3 to 8 times more likely to report suicidal behavior if they had experienced childhood abuse.26
In spite of these studies, to our knowledge there has been limited examination of the synergistic or interactional effects of childhood trauma and combat trauma on substance use among soldiers, and even less among reserve or National Guard soldiers specifically. However, this subset of the military population is important to examine separately, as reserve soldiers may be particularly vulnerable to experiencing the adverse effects of combat and deployment.7, 27 Unlike active duty military members, reserve soldiers have active civilian lives and careers and live in civilian communities, often far from centralized military support services.28 When they are not deployed, their military participation consists of monthly drill weekends and annual training. Deployment for reserve soldiers then represents a significant disruption of their civilian lives, with potentially less support than that offered to full-time military members. As such, the stress and challenges of deployment are different for reserve soldiers; namely being unaccustomed to prolonged absences from family,28, 29 experiencing difficulties with finances, healthcare, and employment during transitions between military service and civilian life,29, 30 and often being removed from centrally-located support services.28, 31 Given the previously described importance of considering chronic stress in examining substance use outcomes and the greater stress related to deployment that may be experienced by reserve soldiers, attention to the individual and cumulative effects of exposure to childhood and combat trauma are important to consider.
The goal of this paper, therefore, was to examine the associations among childhood trauma, combat trauma and substance use (alcohol problems, frequent heavy drinking (FHD), current cigarette smoking, current and lifetime drug use) among National Guard and Reserve soldiers. We first examined the independent effects of childhood trauma and combat on substance use outcomes. We then tested for the interactive effect of childhood trauma and combat on substance use outcomes to determine if soldiers who experienced both were at greater risk for substance use. This work is based on baseline data from an ongoing longitudinal study, Operations: SAFETY (Solders and Families Excelling Through the Years), which is broadly focused on the health of National Guard and Reserve soldiers and their spouses.
Method
The study protocol was approved by the University at Buffalo’s Institutional Review Board. The Army Human Research Protections Office, Office of the Chief, Army Reserve as well as the Adjutant General of the National Guard also vetted the study protocol.
Data collection
Recruitment.
From summer 2014-fall 2015, the Operation: SAFETY study recruited US Army Reserve and Army National Guard soldiers and their partners.32–34 Participants were recruited from a purposeful sample across the Western New York region, that accounted for geographic variation, as well as inclusion of unit types (e.g. combat vs. support). Research staff presented the project at drill weekends. Soldiers were given an overview of the project and were told that participation for the soldier and their spouse would involve the completion of three online surveys (baseline with two yearly follow-ups), covering a variety of general health topics such as nutrition, physical and mental health, caffeine intake, sleep, substance use, romantic relationship, social network information, and deployment information and events. For their time, soldiers and their partners received $60 for baseline and $70 for each of the follow-ups ($200 per person/$400 couple over the study period).
Interested participants were invited to complete a screening form and were provided with an information packet to share with their partner. Potential participants were screened on six inclusion criteria: (1) the couple is married or living as if married; (2) one member of the dyad is a current Army Reserve Soldier or National Guard Soldier; (3) the soldier is between the ages of 18 and 45; (4) both partners are able to speak and understand English; (5) both partners are willing and able to participate; and (6) both partners have had at least one alcoholic beverage in the past year. Following this in-person screening, all soldiers were contacted within one week regarding their eligibility status.
In total, research staff met with 47 units across New York State resulting in identification of 731 eligible soldiers and partners. Of those, 572 (78%) agreed to participate and 472 (83%) completed some part of the survey. Given that the nature of the main study was to examine spousal influence, only surveys where both partners completed the entire survey were included for follow-up (N = 418). The only difference between couples who enrolled and those who did not was that couples where a civilian partner screened for the study (n = 11) were less likely to enroll (p<.001). No differences existed between soldiers’ screening health variables between those who enrolled and completed vs those who enrolled and did not complete.
Participants.
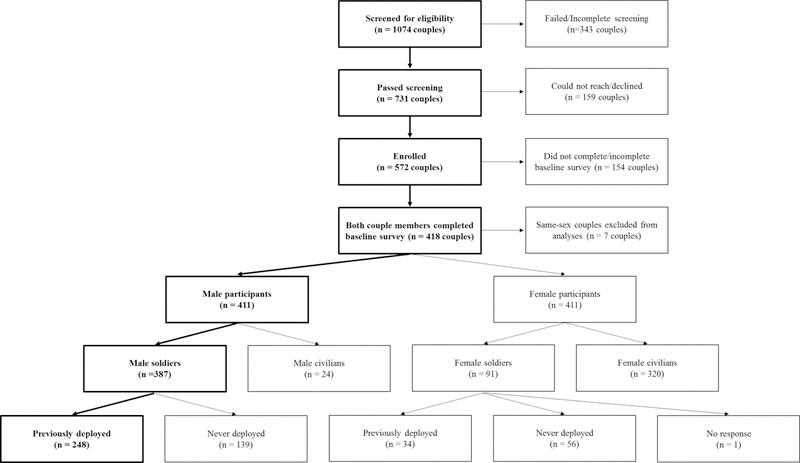
The sample for the present analysis consisted of baseline data from a sub-set of the total sample; male soldiers who were deployed (n = 248). Female soldiers who were deployed were excluded from the analysis due to the small sample size (n = 34). See Figure 1 for a flow chart from recruitment to the analytic sample. The final study sample was predominantly Non-Hispanic White, with at least some college education, and had a median family income of $60,000–$79,000 (Table 1).
Figure 1.
Operation: SAFETY recruitment from initial screening to analytic sample.
Table 1.
Demographic characteristics.
| Participants (N = 248) | M or % | SD or N |
|---|---|---|
| Age | 33.4 | (6.2) |
| Race/Ethnicity | ||
| Non-Hispanic White | 81.1% | (201) |
| Non-Hispanic Black | 4.4% | (11) |
| Hispanic | 9.7% | (24) |
| Other | 3.2% | (8) |
| Education | ||
| <HS – HS Grad | 14.1% | (35) |
| Some College | 60.1% | (149) |
| College + | 25.8% | (64) |
| Median Household Income | $60,000 to $79,000 | |
| Marital Status | ||
| Married | 75.4% | (187) |
| Cohabitating | 24.6% | (61) |
| Military Service | ||
| Total Years Served | 11.9 | (6.09) |
| Number of Deployments | 1.6 | (0.9) |
Survey administration.
The surveys were administered through a secure HIPAA-compliant online survey programming software, StudyTrax™, which allowed for data encryption. Soldiers and partners who lived in the area were invited to the university to complete their online surveys. Partners could come in together or separately, and were each given a private room with a touchscreen computer on which to complete their survey. Informed consent was conducted in person with a research staff member. Because it is common for NG/Reserve soldiers to live great distances from their unit location and it is possible for soldiers to be deployed during the study, participants could also complete the surveys remotely. In these cases, separate login information was sent to each partners’ email.
Measures
Childhood trauma.
The Comprehensive Child Maltreatment Scale (CCMS)35 was used to assess three domains of childhood trauma: physical abuse, psychological abuse, and neglect. Each subscale is composed of three questions on each of the different forms of abuse (e.g., “Physically punished for wrongdoing”) and broken down by three separate perpetrators (“Mother,” “Father,” and “Other adult/older adolescent (5 or more years older)”), for a total of nine questions in each domain. In addition, there are two questions on whether the individual witnessed such behaviors being directed towards others in the household. Participants reported the frequency of events for each item on a five point scale (0= never or almost never to 4= very frequently) for a total score of 0–116. Greater scores indicate greater maltreatment during childhood. The CCMS has shown good internal consistency (e.g., total CCMS alpha = 0.93) and high test-retest reliability (r = 0.92).35 In our sample, total CCMS alpha = 0.91.
Combat exposure.
Combat exposure was assessed with the Combat Experiences Scale from the Deployment Risk and Resilience Inventory-2 (DRRI-2).36 Participants reported on the frequency with which they encountered 17 objective events and circumstances occurring in their most recent warzone experience, ranging from 1 (never) to 6 (daily or almost daily). Items include things such as, “I personally witnessed enemy combatants being seriously wounded or killed,” “I was exposed to hostile incoming fire,” and “I fired my weapon at enemy combatants.” Scores range from 17–102 with higher scores indicating greater combat exposure (alpha = 0.94).
Alcohol problems.
Alcohol problems were assessed with the AUDIT (Alcohol Use Disorders Identification Test).37 The AUDIT consists of 10 items rated on a 4-point scale from 0 (never) to 4 (daily or almost daily), with scores ranging from 0–40 (alpha = 0.76). Items include things such as: “Have you or someone else been injured because of your drinking?”, and “How often during the last year have you had a feeling of guilt or remorse after drinking?”
Frequent heavy drinking.
Consistent with other work38 frequent heavy drinking was assessed using the maximum report of two items: 1) the reported frequency of getting drunk in the past year, ranging on a 9-point scale from never to every day in the past year, and 2) the frequency of five or more (for males) or four or more (for females) drinks in a single setting, ranging on a 9-point scale from never to every day in the past year.
Current and lifetime drug use.
The NIDA Modified ASSIST 2.0 was used to assess current use (i.e., past 3 months) and lifetime use of drugs. Reported use within each time frame of any of the following substances was considered a positive screen for current and/or lifetime drug use: cannabis, cocaine, methamphetamine, inhalants, hallucinogens, street opioids, non-medical use of prescription drugs, or any other specified illicit drug. The ASSIST was vigorously tested with three phases to examine and ensure reliability and validity across settings and cultures.39
Current cigarette smoking.
Current cigarette smoking was assessed with two questions: “In your entire life have you ever smoked 100 cigarettes?” and “Do you currently smoke cigarettes?” Endorsement of both of the aforementioned questions was considered a positive screen for current cigarette smoking. This approach allowed for the exclusion of individuals who have only recently tried cigarettes. This item was dichotomized to yes/no.
Marital satisfaction.
Relationship functioning was assessed with the Marital Adjustment Test (MAT).40 This 15-item instrument has been well validated in measuring overall marital satisfaction and adjustment of husbands and wives to each other. Scores range from 2 to 158, with higher scores indicating greater relationship adjustment (alpha = 0.76).
Age.
Participants provided their full date of birth. Age was calculated based on the date of the survey and the participant’s date of birth.
Number of deployments.
Participants reported their total number of deployments. This item was dichotomized as one/more than one.
Data analysis
Descriptive statistics were used to characterize the study sample by reporting means and standard deviations for continuous variables and distributions for categorical variables. Childhood trauma and combat exposure were each considered in unadjusted univariate regression models for each substance use outcome. In our main effects models, we examined the independent effects of soldiers’ childhood trauma and combat exposure on alcohol problems, FHD, current cigarette smoking, and current and lifetime drug use. Given the different ranges of the childhood trauma and combat exposure measures, the scales were standardized to allow for comparison.
Both increasing age and increasing number of military deployments may provide greater opportunities for lifetime traumatic exposures. Additionally, we know from previous work that marital satisfaction is associated with increased resiliency for mental health outcomes among soldiers33 and that reservists with stronger relationships were more likely to report that they coped well with deployment.31 Therefore adjusted models controlled for age, marital satisfaction, and number of deployments (1 vs. more than 1). Finally, the possible synergistic effects of combat exposure and childhood trauma on substance use were examined using interaction models while controlling for age, marital satisfaction, and number of deployments. Predictive margins were calculated to further examine these interactions at the 10th and 90th percentiles of DRRI and CCMS scores. We used linear regression models for continuous outcomes (alcohol problems and FHD) and logistic models for binary outcomes (current cigarette smoking, current and lifetime drug use). Missing data were minimal. All analyses were performed using Stata version 14.2 software (Stata Corporation, College Station, TX).
Results
Descriptive results
Among male soldiers who were deployed, the mean (M) and standard deviation (SD) CCMS and DRRI scores were M = 10.8, SD = 12.0 and M = 32.2, SD = 16.5, respectively. The prevalence of substance use was: current cigarette smoking 20.2% (n = 50), current drug use 6.5% (n = 16), and lifetime drug use 56.5% (n = 140). The AUDIT score was M = 5.1, SD = 4.0 and 19.0% (n = 47) of the sample had an AUDIT score ≥ 8, the recommended cutoff indicating hazardous drinking.37 The frequent heavy drinking (FHD) score was M = 2.6, SD = 1.4 and 33.9% (n = 86) of the sample reported drinking heavily on at least a monthly basis over the past year. In the sample, 42.3% (n = 105) of the soldiers reported multiple deployments.
Main effects
Alcohol problems
Combat exposure was associated with alcohol problems in our first univariate model (regression coefficient = 0.77, 95% Confidence Interval [CI]: 0.28, 1.26; p = .002). In our second univariate model, childhood trauma was not associated with alcohol problems. In our full model (see Table 2), including combat exposure and childhood trauma, the association between combat exposure and alcohol problems persisted, even after controlling for age, marital satisfaction, and number of deployments (regression coefficient = 0.81, 95% CI: 0.33, 1.29; p = .001) (Table 2). Childhood trauma was not associated with alcohol problems in the full model.
Table 2.
Effects of male soldiers’ combat exposure, childhood maltreatment, age, marital satisfaction, and number of deployments on his substance use.
| Alcohol Problems | Frequent Heavy Drinking |
Current Cigarette Smoking |
Current Drug Use |
Lifetime Drug Use | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| DRRI Score | .81** | 0.33, 1.29 | .29** | 0.12, 0.46 | 1.13 | 0.84, 1.54 | 0.96 | 0.54, 1.72 | 1.10 | 0.85, 1.43 |
| CCMS Score | .21 | −0.28, 0.70 | −.11 | −0.29, 0.06 | 1.25 | 0.94, 1.66 | 1.44 | 0.97, 2.14 | 1.61** | 1.14, 2.27 |
| Age | −.10* | −0.19, −0.02 | −.04** | −0.07, −0.01 | 0.97 | 0.91, 1.02 | 0.92 | 0.82, 1.02 | 0.98 | 0.94, 1.03 |
|
Marital
Satisfaction |
−.03** | −0.05, −0.01 | −.01 | −0.01, 0.00 | 1.00 | 0.99, 1.01 | 1.00 | 0.98, 1.01 | 0.99** | 0.98, .99 |
|
Number of
Deployments |
.58 | −0.47, 1.62 | .35 | −0.03, 0.73 | 1.03 | 0.52, 2.04 | 0.62 | 0.18, 2.16 | .92 | 0.52, 1.63 |
p < 0.05
p < 0.01
p < 0.001
Frequent heavy drinking
Greater combat exposure was also associated with FHD in our first univariate model (regression coefficient = 0.28, 95% CI: 0.10, 0.46; p = .002). In our second univariate model, childhood trauma did not have a significant effect on FHD. In our full model, including combat exposure and childhood trauma, the association between combat exposure and FHD persisted after adjusting for age, marital satisfaction, and number of deployments (regression coefficient = 0.29, 95% CI: 0.12, 0.46; p = .001; Table 2). Childhood trauma was not associated with frequent heavy drinking in the full model.
Current cigarette smoking
In univariate models, neither combat exposure nor childhood trauma were associated with current cigarette smoking. The full model also failed to show any associations.
Current drug use
In our first univariate model, combat exposure was not associated with current drug use. However, childhood trauma had a trend-level association with current drug use in our second univariate model (OR = 1.40, 95% CI: 0.96, 2.02; p = .077). This trend-level association persisted in our full model, even after controlling for age, marital satisfaction, and number of deployments (OR = 1.44, 95% CI: 0.97, 2.14; p = .072; Table 2). Combat exposure remained non-significant.
Lifetime drug use
There was no association between combat exposure and lifetime drug use in our first univariate model. Conversely, childhood trauma was significantly associated with lifetime drug use in our second univariate model (OR = 1.73, 95% CI: 1.23, 2.44; p = .002). This association persisted in our full model, even after controlling for age, marital satisfaction, and number of deployments (OR = 1.61, 95% CI: 1.14, 2.27; p = .006; Table 2). Combat exposure remained non-significant.
Interaction effects
Alcohol problems
Combat exposure had a significant interaction with childhood trauma on alcohol problems (regression coefficient = −0.56, 95% CI: −1.12, −0.01; p = .048), as shown in Table 3. Childhood and combat trauma had a differential effect on alcohol problems. In the presence of high childhood trauma, increasing combat exposure was not associated with a greater likelihood of alcohol problems; however, in the presence of low levels of childhood trauma, greater combat exposure was associated with a greater likelihood of alcohol problems (Figure 2).
Table 3.
Interaction effects of male soldiers’ combat exposure and childhood trauma on substance use, controlling for age, marital satisfaction, and number of deployments.
| Alcohol Problems | Frequent Heavy Drinking | Lifetime Drug Use | ||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | OR | 95% CI | |
| DRRI Score X CCMS Score | −0.56* | −1.12, −0.01 | −0.27** | −0.47, −0.08 | 1.78* | 1.04, 3.04 |
| DRRI Score | 0.71** | 0.22, 1.20 | 0.24** | 0.06, 0.41 | 1.31 | 0.95, 1.83 |
| CCMS Score | 0.25 | −0.24, 0.74 | −0.10 | −0.27, 0.08 | 1.84** | 1.24, 2.73 |
| Age | −0.10* | −0.19, −0.02 | −0.04** | −0.07, −0.01 | 0.98 | 0.94, 1.03 |
| Marital Satisfaction | −0.03** | −0.04, −0.01 | −0.01 | −0.01, 0.00 | 0.99** | 0.98, 0.99 |
| Number of Deployments | 0.59 | −0.45, 1.62 | 0.35 | −0.02, 0.73 | 0.95 | 0.54, 1.69 |
p < 0.05
p < 0.01
p < 0.001
Figure 2.
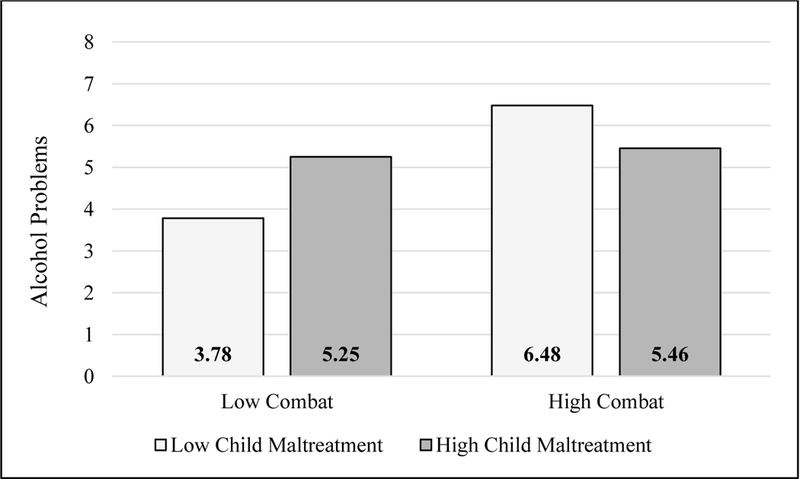
Predictive margins of alcohol problems by combat exposure and child maltreatment.
Frequent heavy drinking
Combat exposure had a significant interaction with childhood trauma on frequent heavy drinking (regression coefficient = −0.27, 95% CI: −0.47, −0.08; p = .007; Table 3). Similar to alcohol problems, in the presence of low levels of childhood trauma, increasing combat exposure was associated with a greater likelihood of frequent heavy drinking (Figure 3).
Figure 3.
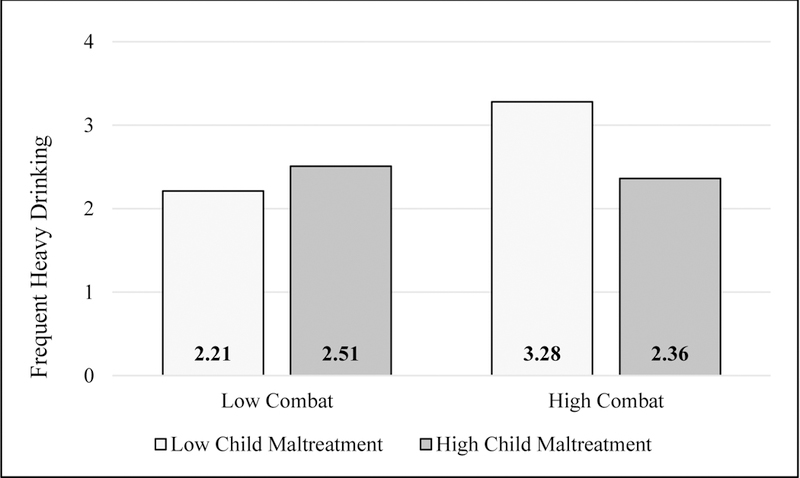
Predictive margins of frequent heavy drinking by combat exposure and child maltreatment.
Lifetime drug use
Combat exposure had a significant interaction with childhood trauma on lifetime drug use (OR = 1.78, 95% CI: 1.04, 3.04; p = .035; Table 3). Childhood and combat trauma had a synergistic effect on lifetime drug use; the presence of both high levels of childhood trauma and high combat exposure was associated with the greatest likelihood of lifetime drug use (Figure 4).
Figure 4.
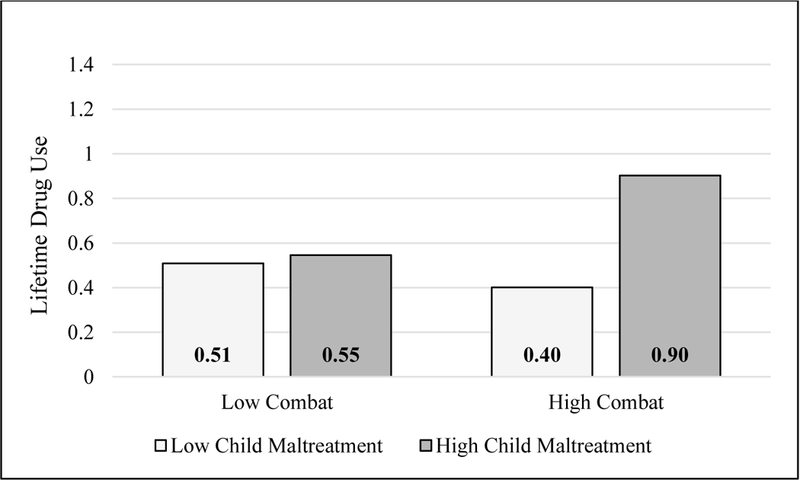
Predictive margins of lifetime drug use by combat exposure and child maltreatment.
There were no significant interactions for smoking or current drug use.
Discussion
Our results indicate that childhood trauma and combat trauma have differential effects on alcohol problems and frequent heavy drinking, but have a synergistic effect on lifetime drug use among male National Guard and Reserve soldiers who have experienced combat. In the interaction models, soldiers with high levels of childhood trauma were at increased risk of alcohol problems and frequent heavy drinking; combat exposure did not significantly increase this risk. However, among soldiers with low levels of childhood trauma and high levels of combat exposure, combat exposure significantly interacted with childhood trauma, resulting in greater likelihood of both frequent heavy drinking and alcohol problems. To our knowledge, this is the first work to demonstrate this type of interaction.
Our findings that demonstrate differential effects of childhood and combat trauma on alcohol problems and frequent heavy drinking are counterintuitive. The stress sensitization hypothesis would suggest that adverse childhood experiences may lead to greater sensitivity to future trauma (e.g. combat) and therefore a greater likelihood of adverse outcomes.41, 42 Previous work has similarly demonstrated conflicting results in this area, finding a dose-dependent response for childhood traumas on depression, PTSD, and health-related quality of life among active duty Marines,43 but no relationship between childhood trauma and alcohol abuse. Research with a sample of Navy recruits, however, documented a significant relationship among childhood physical and sexual trauma and problematic drinking.44 However, both of these studies were conducted with a sample of never-deployed individuals, and therefore did not account for additional adult trauma exposures, including combat. It is possible that among those with high child maltreatment, there is a ceiling effect of trauma with respect to its effect on the likelihood of alcohol problems and frequent heavy drinking. Therefore, the additional effect of combat trauma is only seen among those with low child maltreatment. Furthermore, our study was conducted with a community sample of Reserve/NG soldiers, rather than a clinical sample, and therefore may be capturing less severe alcohol problems. Kim and colleagues41 likewise demonstrated that among individuals with only moderate alcohol intake, stressful life events had a greater effect on alcohol craving among individuals with no history of childhood maltreatment compared to those with childhood maltreatment. This underscores the fact that combat trauma, when combined with even low levels of childhood trauma, may result in a greater risk for problematic alcohol use.
Our results also demonstrate that soldiers with both high levels of childhood trauma and combat exposure had the greatest likelihood of lifetime drug use. The relationship between childhood trauma and illicit drug use is well documented.13–15 More severe trauma in childhood has a strong, linear relationship with the odds of having initiated illicit drug use in adolescence.45 Additionally, research has shown an additive effect of multiple trauma experiences on use of multiple substances.46 Evidence on the developmental implications of trauma in childhood compared to later trauma suggest that severe trauma in childhood may disrupt developmental processes, leading to complex impairment across emotion regulation and interpersonal skills.47–49 The additional trauma of combat exposure later in life is associated with greater risk of drug use in our sample. However, given the cross-sectional nature of the current analyses, it is not possible to determine if participants’ drug use pre-dated their combat exposure. Future waves of longitudinal data from this study will help to further illuminate this relationship.
We found no association in our sample among either childhood or combat trauma and current cigarette smoking. This is surprising, given the well-documented association between trauma, PTSD, and cigarette smoking.50, 51 Research has shown that military-related stress52 and deployment53 increase rates of smoking among soldiers, as a possible maladaptive coping mechanism. Although our rates of smoking are in line with other similar studies, it is possible that heaviness of smoking, rather than a simple dichotomous measure of smoking, is what is driving the association between trauma and smoking shown in other studies. For instance, we have a prevalence of smoking of 20%, however, based on the Heaviness of Smoking Index,54the majority of smokers in our study are light smokers.
Further research is needed to better understand soldiers’ likelihood of engaging in substance use. Future longitudinal analysis generated by ongoing data collected in this study may help to answer some of these questions by looking at trends in drug use over time.
Limitations
This work is subject to limitations. First, the data represent baseline data from an ongoing longitudinal study. Longitudinal data will help to strengthen these findings by allowing us to tease out some of the temporal relationships between trauma and substance use. Second, all data are self-report and therefore subject to bias. However, this is common in epidemiological surveys and self-report data have been shown to be reliable estimates of behavior. Third, the study sample consisted of a non-randomized group of individuals who volunteered to participate in the study, which may limit generalizability; however, efforts were made to purposefully sample from National Guard and Reserve units across the entire region, with specific attention to including a diversity of unit types and geographic areas. Finally, the small sample size of combat deployed females precluded us from examining outcomes for this population. Future work in this area is important, especially with the increasing combat exposure experienced by female soldiers.
Conclusions
Overall, our results demonstrate childhood and combat trauma significantly interact and are associated with increased risk of alcohol problems, frequent heavy drinking, and lifetime drug use among Reserve and National Guard soldiers. Given that interaction effects were found, even among individuals with lower levels of childhood trauma, and given high prevalence of childhood trauma among military service members,55 screening for trauma prior to enlistment and/or deployment may help identify at-risk individuals and allow time for early intervention to prevent future adverse outcomes. Knowing that cumulative trauma may be associated with worse outcomes,16, 41, 42, 56 it is important to evaluate all sources of trauma in military populations, not just combat exposure. Our results also demonstrate that even low levels of childhood trauma, when combined with later combat exposure, may increase the risk for use of certain substances. A better understanding of the full extent of trauma in military personnel will help improve prevention and identification of substance use problems in this population both during and after separation from service.
Acknowledgments
Funding
This work was supported by the National Institute on Drug Abuse of the National Institutes of Health [R01DA034072] to GGH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Bray RM and Hourani LL. Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction 2007;102(7):1092–1101. [DOI] [PubMed] [Google Scholar]
- 2.Green KT, Beckham JC, Youssef N and Elbogen EB. Alcohol misuse and psychological resilience among U.S. Iraq and Afghanistan era veterans. Addict Behav 2014;39(2):406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoge CW, Auchterlonie JL and Milliken CS. Mental Health Problems, Use of Mental Health Services, and Attrition From Military Service After Returning From Deployment to Iraq or Afghanistan. JAMA 2006;295(9):1023–1032. [DOI] [PubMed] [Google Scholar]
- 4.Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S and Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend 2011;116(1–3):93–101. [DOI] [PubMed] [Google Scholar]
- 5.Homish GG, Homish DL, Cummings KJ and Heavey SC. Military Deployments, Combat Exposure and Partner Drinking. Conference Presentation. Research Society on Alcoholism San Antonio, Texas, 2015. [Google Scholar]
- 6.Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA 2008;300(6):663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milliken CS, Auchterlonie JL and Hoge CW. Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning From the Iraq War. JAMA 2007;298(18):2141–2148. [DOI] [PubMed] [Google Scholar]
- 8.Wright KM, Foran HM, Wood MD, Eckford RD and McGurk D. Alcohol problems, aggression, and other externalizing behaviors after return from deployment: understanding the role of combat exposure, internalizing symptoms, and social environment. J Clin Psychol 2012;68(7):782–800. [DOI] [PubMed] [Google Scholar]
- 9.Shen YC, Arkes J and Williams TV. Effects of Iraq/Afghanistan deployments on major depression and substance use disorder: analysis of active duty personnel in the US military. Am J Public Health 2012;102 Suppl 1:S80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady KT and Sinha R. Co-Occurring Mental and Substance use Disorders: The Neurobiological Effects of Chronic Stress. Am J Psychiatry 2005;162(8):1483–1493. [DOI] [PubMed] [Google Scholar]
- 11.Lifjffijt M, Hu K and Swann AC. Stress modulates illness-course of substance use disorders: a translational review. Front psychiatry 2014;5:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinha R Chronic Stress, Drug Use, and Vulnerability to Addiction. Ann N Y Acad Sci 2008;1141:105–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kendall-Tackett K The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl 2002;26(6–7):715–729. [DOI] [PubMed] [Google Scholar]
- 14.Sachs-Ericsson N, Cromer K, Hernandez A and Kendall-Tackett K. A review of childhood abuse, health, and pain-related problems: the role of psychiatric disorders and current life stress. J Trauma Dissociation 2009;10(2):170–188. [DOI] [PubMed] [Google Scholar]
- 15.Simpson TL and Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clin Psychol Rev 2002;22(1):27–77. [DOI] [PubMed] [Google Scholar]
- 16.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006;256(3):174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cabrera OA, Hoge CW, Bliese PD, Castro CA and Messer SC. Childhood Adversity and Combat as Predictors of Depression and Post-Traumatic Stress in Deployed Troops. Am J Prev Med 2007;33(2):77–82. [DOI] [PubMed] [Google Scholar]
- 18.Clancy CP, Graybeal A, Tompson WP, et al. Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: association with current symptomatology. J Clin Psychiatry 2006;67(9):1346–1353. [DOI] [PubMed] [Google Scholar]
- 19.Sareen J, Henriksen CA, Bolton SL, Afifi TO, Stein MB and Asmundson GJ. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychol Med 2013;43(1):73–84. [DOI] [PubMed] [Google Scholar]
- 20.Van Voorhees EE, Dedert EA, Calhoun PS, Brancu M, Runnals J and Beckham JC. Childhood trauma exposure in Iraq and Afghanistan war era veterans: Implications for posttraumatic stress disorder symptoms and adult functional social support. Child Abuse Negl 2012;36(5):423–432. [DOI] [PubMed] [Google Scholar]
- 21.Dedert EA, Green KT, Calhoun PS, et al. Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. J Psychiatr Res 2009;43(9):830–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seifert AE, Polusny MA and Murdoch M. The association between childhood physical and sexual abuse and functioning and psychiatric symptoms in a sample of U.S. Army soldiers. Mil Med 2011;176(2):176–181. [DOI] [PubMed] [Google Scholar]
- 23.Whelan J Exploring the Relationships Between Untreated Adverse Childhood Events and Substance Abuse, and Their Impact on PTSD Relapse Rates Among Canadian Military Veterans. In: Aiken AB and Belanger SAH eds. Beyond the Line: Military and Veteran Health Research Montreal, Quebec: MQUP; 2013:180–195. [Google Scholar]
- 24.Clarke-Walper K, Riviere LA and Wilk JE. Alcohol misuse, alcohol-related risky behaviors, and childhood adversity among soldiers who returned from Iraq or Afghanistan. Addict Behav 2014;39(2):414–419. [DOI] [PubMed] [Google Scholar]
- 25.Iversen AC, Fear NT, Simonoff E, et al. Influence of childhood adversity on health among male UK military personnel. Br J Psychiatry 2007;191:506–511. [DOI] [PubMed] [Google Scholar]
- 26.Griffith J Prevalence of Childhood Abuse among Army Naitonal Guard Soldiers and Its Relationship to Suicidal Behavior. Mil Behav Health 2014;2(2):114–122. [Google Scholar]
- 27.Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA and Hoge CW. Prevalence of Mental Health Problems and Functional Impairment Among Active Component and National Guard Soldiers 3 and 12 Months Following Combat in Iraq. Arch Gen Psychiatry 2010;67(6):614–623. [DOI] [PubMed] [Google Scholar]
- 28.Lapp CA, Taft LB, Tollefson T, Hoepner A, Moore K and Divyak K. Stress and coping on the home front: guard and reserve spouses searching for a new normal. J Fam Nurs 2010;16(1):45–67. [DOI] [PubMed] [Google Scholar]
- 29.Griffith J Decades of transition for the US reserves: Changing demands on reserve identity and mental well-being. Int Rev Psychiatry 2011;23(2):181–191. [DOI] [PubMed] [Google Scholar]
- 30.Griffith J Citizens Coping as Soldiers: A Review of Deployment Stress Symptoms Among Reservists. Mil Psychol 2010;22(2):176–206. [Google Scholar]
- 31.Castaneda LW, Harrell MC, Varda DM, Curry Hall K, Beckett MK and Stern S. Deployment Experiences of Guard and Reserve Families: Implications for Support and Retention Santa Monica, CA: RAND Corporation;2008. [Google Scholar]
- 32.[BLINDED]. Stress Health 2017.
- 33.[BLINDED]. Mil Behav Health 2017.
- 34.[BLINDED]. Addict Behav 2017.
- 35.Higgins DJ and McCabe MP. The development of the comprehensive child maltreatment scale. J Fam Stud 2001;7(1):7–28. [Google Scholar]
- 36.Vogt D, Smith BN, King DW and King LA. Manual for the Deployment Risk and Resilience Inventory-2 (DRRI-2): A Collection ofMeasures for Studying Deployment-Related Experiences of Military Veterans Boston, MA: National Center for PTSD;2012. [Google Scholar]
- 37.Babor TF and Del Boca FK. Just the facts: Enhancing Measurement of Alcohol Consumption Using Self-Report Methods. In: Litten RZ and Allen JP eds. Measuring alcohol consumption: psychosocial and biochemical methods Totowa, NJ: Humana Press; 1992:3–20. [Google Scholar]
- 38.Homish GG and Leonard KE. The drinking partnership and marital satisfaction: The longitudinal influence of discrepant drinking. J Consult Clin Psychol 2007;75(1):43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.WHO Assist Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction 2002;97(9):1183–1194. [DOI] [PubMed] [Google Scholar]
- 40.Locke HJ and Wallace KM. Short marital-adjustment prediction tests: Their reliability and validity. Marriage Fam Living 1959;21:251–255. [Google Scholar]
- 41.Kim JH, Martins SS, Shmulewitz D, et al. Childhood maltreatment, stressful life events, and alcohol craving in adult drinkers. Alcohol Clin Exp Res 2014;38(7):2048–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McLaughlin KA, Conron KJ, Koenen KC and Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med 2010;40(10):1647–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agorastos A, Pittman JO, Angkaw AC, et al. The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. J Psychiatr Res 2014;58:46–54. [DOI] [PubMed] [Google Scholar]
- 44.Trent L, Stander V, Thomsen C and Merrill L. Alcohol abuse among U.S. Navy recruits who were maltreated in childhood. Alcohol Alcohol 2007;42(4):370–375. [DOI] [PubMed] [Google Scholar]
- 45.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH and Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics 2003; 111:564+. [DOI] [PubMed] [Google Scholar]
- 46.Khoury L, Tang YL, Bradley B, Cubells JF and Ressler KJ. Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population. Depress Anxiety 2010;27(12):1077–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cloitre M, Stolbach BC, Herman JL, et al. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress 2009;22(5):399–408. [DOI] [PubMed] [Google Scholar]
- 48.Evans SE, Steel AL and DiLillo D. Child maltreatment severity and adult trauma symptoms: does perceived social support play a buffering role? Child Abuse Negl 2013;37(11):934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dembo R, Dertke M, La Voie L, Borders S, Washburn M and Schmeidler J. Physical abuse, sexual victimization and illicit drug use: a structural analysis among high risk adolescents. J Adolesc 1987;10(1):13–34. [DOI] [PubMed] [Google Scholar]
- 50.Feldner MT, Babson KA and Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clin Psychol Rev 2007;27(1):14–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fu SS, McFall M, Saxon AJ, et al. Post-Traumatic Stress Disorder and Smoking: A Systematic Review. Nicotine Tob Res 2007;9(11):1071–1084. [DOI] [PubMed] [Google Scholar]
- 52.Bray RM, Fairbank JA and Marsden ME. Stress and Substance Use Among Military Women and Men. Am J Drug Alcohol Abuse 1999;25(2):239–256. [DOI] [PubMed] [Google Scholar]
- 53.Smith B, Ryan MAK, Wingard DL, Patterson TL, Slymen DJ and Macera CA. Cigarette Smoking and Military Deployment: A Prospective Evaluation. Am J Prev Med 2008;35(6):539–546. [DOI] [PubMed] [Google Scholar]
- 54.Heatherton TF, Kozlowski LT, Frecker RC and Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 55.Blosnich JR and Bossarte RM. Childhood Abuse and Military Experience-Important Information to Better Serve Those Who Have Served. JAMA Psychiatry 2016;73(3):195–196. [DOI] [PubMed] [Google Scholar]
- 56.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]