Abstract
Introduction
Cirrhotic patients have been considered for decades to have a pro-haemorrhagic pattern and were treated as such based on the results from standard coagulation tests. The aim of our study was to determine the effects of platelet count and fibrinogen levels on rotational thromboelastometry (ROTEM) parameters.
Methods
We prospectively included 176 patients with End-Stage Liver Disease (ESLD) admitted to our Intensive Care Unit prior to liver transplantation. Collected data consisted of severity scores, liver, renal and standard coagulation tests, fibrinogen levels, platelet counts and ROTEM parameters. Four ROTEM assays were performed (ExTEM, InTEM, ApTEM and FibTEM) and the following parameters included: CT – clotting time, CFT – clot formation time, MCF – maximum clot firmness, ML – maximum lysis, alpha angle, TPI – thrombin potential index, MaxV - maximum velocity of clot formation (MaxV), MaxVt - time to MaxV, MCE - maximum clot elasticity and AUC - area under the curve.
Results
Statistical analysis demonstrated a linear correlation between platelet counts and ExTEM TPI (R2 linear =0.494), ExTEM MaxV (R2 linear =0.253), ExTEM MCE (R2 linear = 0.351) and ExTEM MCF (R2 cubic = 0.498). Fibrinogen levels correlated linearly with ExTEM MCF (R2 linear = 0.426), ExTEM TPI (R2 linear = 0.544), ExTEM MaxV (R2 linear = 0.332), ExTEM MCE (R2 linear = 0.395) and non-linearly with ExTEM CFT (R2 cubic = 0.475).
Conclusion
Fibrinogen levels and platelet counts had an important effect on both standard and derived ROTEM parameters. Further analysis is required in order to determine clinically oriented cut-off values below which severe coagulopathy would develop.
Keywords: cirrhotic coagulopathy, rotational thromboelastometry, platelet count, fibrinogen levels
Introduction
For decades patients with End-Stage Liver Disease (ESLD) have been considered be naturally anti-coagulated and they were consecutively treated in order to normalize standard coagulation tests. Recent studies [1] have demonstrated a rebalanced haemostasis in which pro-haemostatic and anti-haemostatic systems complemented each other [2]. Moreover, many cirrhotic patients who suffered from thrombotic complications such as portal vein thrombosis could be attributed to local endothelial factors and liver inflammation [3]. Because of these findings, the exact threshold for blood products transfusion and administration of both pro- and anti- coagulant therapies became a challenge [4].
Rotational thromboelastometry (ROTEM) is currently consider the method of choice in guiding haemostatic management in acute care settings in cirrhotic patients [5]. Different algorithms have been developed for the management of severe bleeding in liver transplantation [6] and variceal bleeding [7]. Despite this, fine tuning of haemostasis in non-urgent situations remains debatable.
The aim of the present study was to assess the impact of fibrinogen levels and platelet count on ROTEM parameters and to determine the cut-off value below which severe coagulopathy develops.
Materials and Methods
The ethical approval for the present study was provided by the Ethical Committee of Fundeni Clinical Institute, Bucharest, Romania.
Patient inclusion
We prospectively included 260 patients with ESLD admitted to the Intensive Care Unit (ICU) prior to liver transplantation between March 2013 and March 2016. Exclusion criteria consisted of: age under 18 years, diagnosis of hepatocellular carcinoma, portal vein thrombosis, use of anticoagulant or anti-thrombotic therapy within the last 7 days, use of pro-haemostatic therapy within the last 7 days, systemic infection or sepsis and splenectomy performed prior to inclusion.
Collected data
Patient demographic data, aetiology of liver disease, severity scores (Model for End-Stage Liver Disease – MELD and MELD-Sodium), liver function tests (total bilirubin, conjugated bilirubin, serum transaminases), renal function test (serum creatinine and urea), standard coagulation tests (Fibrinogen level, aPTT – activated partial thromboplastin time, PT- prothrombin time, International Normalized Ratio - INR), ROTEM parameters, platelet count and spleen size were recorded. All tests were performed from venous blood collected by a single puncture needle system. Biochemical tests (liver and renal functional tests), standard coagulation tests and platelet count were performed in the central laboratory in accordance with our institutional protocol. Fibrinogen levels were determined using the Claus method. Spleen size was determined echographically by a senior radiologist as the longest diameter between the spleen poles.
ROTEM (ROTEM®, Tem Innovations GmbH, Germany) assay was performed using whole blood (collected on standard citrated tubes) as a point-of-care test in the ICU. The following ROTEM tests were used: ExTEM, InTEM, ApTEM, FibTEM and the following parameters were recorded: CT – clotting time, CFT – clot formation time, MCF – maximum clot firmness, ML – maximum lysis. Derived parameters were recorded from the ROTEM ExTEM assay: alpha angle, TPI – thrombin potential index, MaxV - maximum velocity of clot formation (MaxV), MaxVt - time to MaxV, MCE- maximum clot elasticity and AUC - area under the curve. Results were recorded after 10 minutes running time and at the end of the assay (one hour and 30 minutes). A graphic representation of the results was printed, and a senior anaesthesiologist reviewed the results. If the results were considered inappropriate due to external factors (e.g. machine malfunction), the test was repeated.
Statistical analysis
Statistical analyses were performed using SPSS 19.0 (SPSS Inc®, Chicago, IL, USA). Data are presented as mean ± standard deviation of the mean, median (minimum, maximum), otherwise percentage. Data distribution was assessed in order to insure the proper statistical examination. Categorical variables were analysed with Chi-square test and quantitative data were analysed with independent samples t-test. Mann-Whitney test was used when the analysed data did not follow a normal distribution. All P values are two-tailed and a P value of less than 0.05 was considered statistically significant.
Results
After applying exclusion criteria, 176 patients were included in the final analysis. Demographic data, ESLD severity scores, spleen size and standard coagulation tests are presented in table 1.
Table 1.
Demographic data, severity scores and standard coagulation tests of patients included
| Parameter | |
|---|---|
| Age (years) | 50.5 ± 12.5 |
| Aetiology of liver disease | |
| HBV liver cirrhosis | 36.9 % (n=65) |
| HCV liver cirrhosis | 34.2 % (n=60) |
| Alcoholic liver cirrhosis | 28.9 % (n=51) |
| MELD score | 19.3 ± 6.1 |
| MELD-sodium score | 23.2 ± 6.3 |
| Spleen size (mm) | 159 ± 33 |
| INR | 1.6 ± 0.4 |
| aPTT (sec) | 39.2 ± 10.5 |
| PT (sec) | 17.8 ± 5.2 |
| Fibrinogen (mg/dL) | 184 ± 97 |
| Platelet count (/mm3) | 91347 [12000 - 434000] |
Thrombocytopenia was associated with higher MELD scores (correlation coefficient: -0.422, p=0.004) and spleen size (correlation coefficient: -443, p=0.003). There was no statistically significant correlation between aetiology of liver disease and platelet count.
From the univariate analysis, platelet count correlated with ExTEM MCF (p<0.01), ExTEM TPI (p<0.01), ExTEM MaxV (p<0.01), ExTEM AUC (p=0.037) and ExTEM MCE (p<0.01). Fibrinogen levels correlated significantly with ExTEM CFT (p=0.036), ExTEM MCF (p<0.01), ExTEM TPI (p<0.01), ExTEM MaxV (p<0.01) and ExTEM MCE (p<0.01). Except for a significant linear correlation between fibrinogen levels and FibTEM MCF (p=0.01), no other significant correlations were found between either platelet count or fibrinogen levels and InTEM or ApTEM parameters.
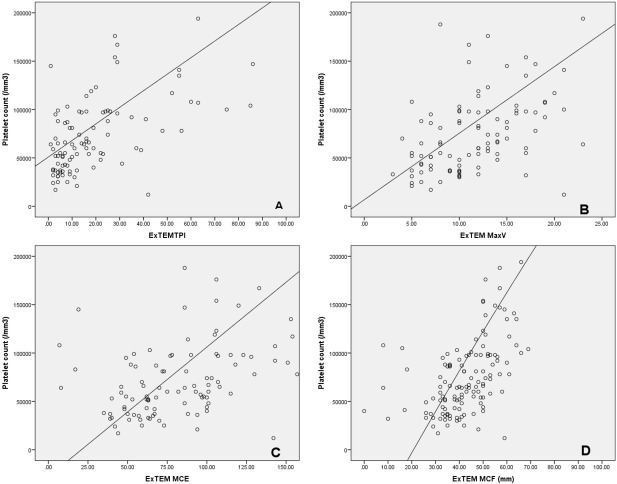
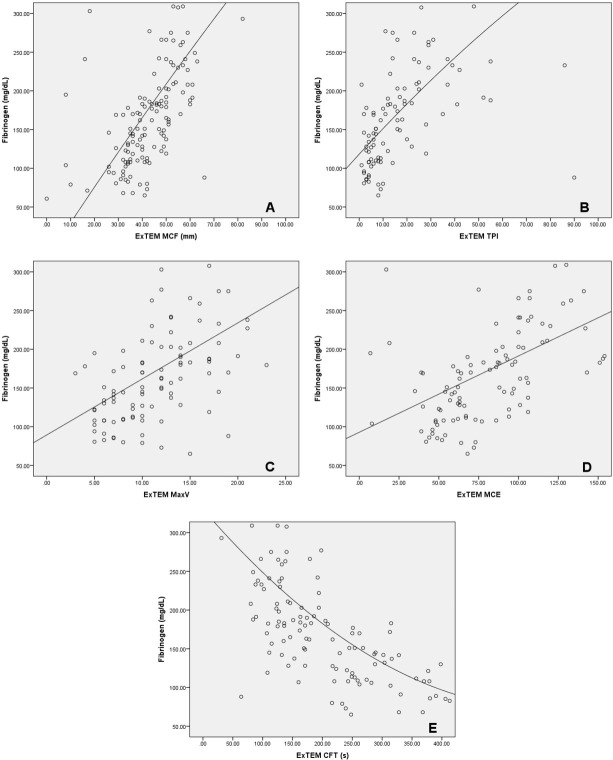
Further analysis revealed a linear correlation between platelet count and ExTEM TPI (R2 linear =0.494), ExTEM MaxV (R2 linear =0.253), ExTEM MCE (R2 linear = 0.351) and ExTEM MCF (R2 linear = 0.498) – Figure 1. Fibrinogen levels correlated linearly with ExTEM MCF (R2 linear = 0.426), ExTEM TPI (R2 linear = 0.544), ExTEM MaxV (R2 linear = 0.332), ExTEM MCE (R2 linear = 0.395) and non-linearly with ExTEM CFT (R2 cubic = 0.475) – Figure 2.
Fig. 1.
Correlation between platelet count and ROTEM parameters: ExTEM TPI (A), ExTEM MaxV (B), ExTEM MCE (C) and ExTEM MCF (D).
Fig. 2.
Correlation between fibrinogen levels and ROTEM parmeters: ExTEM MCF (A), ExTEM TPI (B), ExTEM MaxV (C), ExTEM MCE (D) and ExTEM CFT (E).
For non-linear correlations, we determined a cut-off value for fibrinogen of 200 mg /dL that corresponds to an ExTEM CFT of 160 s and a maximum inflection point for ExTEM CFT of 320 s that corresponds to a fibrinogen level of 115 mg/dL. For platelet count we
determined a cut-off value of 23000/mm3 that corresponds to an ExTEM MCF of 72 mm and a maximum inflection point for ExTEM MCF of 38 mm that corresponds to a platelet count of 57000/mm3.
Discussions
The main results of our study show that both platelet counts and fibrinogen levels significantly impacted whole blood haemostasis as assessed by ROTEM. We found a linear correlation between platelet counts, fibrinogen levels, extrinsically activated thrombin potential index, maximum clot velocity and maximum clot elasticity. Moreover, we determined a cut-off value of 200 mg/dL for fibrinogen and 57000/mm3 for platelet counts below which coagulopathy developed and another cut-off value of 115 mg/dL for fibrinogen and 23000/mm3 below which severe coagulopathy developed.
The main disadvantage of our study is represented by its observational nature. Although from a rational point of view, the thresholds determined corresponded to the development of coagulopathy we did not evaluate their impact on blood loss or transfusion in acute bleeding situations. Therefore, the exact clinical value of our data must be further assessed in randomized clinical trials.
In a study performed by Jeong et al. [8], the authors demonstrated that maximum clot firmness could be used for the prediction of intra-operative blood loss in liver transplantation and recently Dotsch et al [9] showed that FibTEM MCF correlated significantly with postoperative bleeding in liver transplantation. Further studies demonstrated that fibrinogen levels but not platelet counts correlated with excessive transfusion [10]. On the other hand, Seo et al. [11] demonstrated that FibTEM assay did not correlate with fibrinogen levels in severe hypo-fibrinogenemia during liver transplantation. Furthermore, Lentschener et al. [12] stipulated that the use of viscoelastic testing in guiding pro-haemostatic interventions could lead to unnecessary transfusion.
Our results show that both fibrinogen levels and platelet counts had a significant impact on whole blood coagulation. We found that as platelet counts fell in a linear model below 57000/mm3, so did clot firmness, elasticity and clot kinetics. At a platelet count below 23000/mm3 , blood viscosity was detrimentally affected to a point that could not sustain clot formation.
To our knowledge, few studies have shown the utility of derived ROTEM parameters in assessing coagulation kinetics. These parameters are beginning to be used in septic patients with multiple system organ failure with promising results [13]. Solomon et al. [14] demonstrated that clot elasticity and clot firmness did not follow a linear correlation and that the use of clot elasticity could prove to offer a more significant insight into clot strength. Also, platelet counts are more importantly reflected by clot elasticity compared to clot firmness and so a more precise decision can be made in regard to platelet transfusion in cases of massive bleeding.
Viscoelastic tests have become the method of choice in assessing coagulopathy and guiding transfusion in patients with ESLD with a decrease in blood product administration, costs and an overall improved outcome [15]. We consider that the next logical step will be to use derived ROTEM parameters that are able to provide new insights into coagulation kinetics. Thrombin potential index and maximum clot velocity represent the most significant parameters associated with coagulation kinetics and the magnitude of platelet counts and fibrinogen levels on these parameters are able to assess the haemostatic reserve in cirrhotic patients. Furthermore, clot elasticity, as measured by ExTEM MCE, is a marker of clot stability. The combination of these parameters may be able to offer a better picture and form the basis for fine tuning in the management of cirrhotic coagulopathy.
In conclusion, both platelet counts and fibrinogen levels have significant effects on clot kinetics and clot strength in patients with ESLD. The cut-off values of both fibrinogen and platelet count we determined need further investigation in clinical studies and should be adjusted so that fine tuning of haemostasis can be performed without the risk of either over- or under- correction of coagulopathy.
Footnotes
Conflict of interest No conflict of interests to declare.
This article did not benefit from any support in the form of grants, equipment or drugs.
References
- 1.Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365:147–56. doi: 10.1056/NEJMra1011170. [DOI] [PubMed] [Google Scholar]
- 2.Tripodi A, Primignani M, Mannucci PM, Caldwell SH. Changing Concepts of Cirrhotic Coagulopathy. Am J Gastroenterol. 2017;112:274–81. doi: 10.1038/ajg.2016.498. [DOI] [PubMed] [Google Scholar]
- 3.Tripodi A, Primignani M, Lemma L, Chantarangkul V, Mannucci PM. Evidence that low protein C contributes to the procoagulant imbalance in cirrhosis. J Hepatol. 2013;59:26570. doi: 10.1016/j.jhep.2013.03.036. [DOI] [PubMed] [Google Scholar]
- 4.Mannucci PM, Tripodi A.. Liver disease, coagulopathies and transfusion therapy. Blood Transfus. 2013;11:32–6. doi: 10.2450/2012.0151-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saner FH, Abeysundara L, Hartmann M, Mallett SV. Rational approach to transfusion in liver transplantation. Minerva Anestesiol. 2017 doi: 10.23736/S0375-9393.17.12231-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Roullet S, Freyburger G, Cruc M. Management of bleeding and transfusion during liver transplantation before and after the introduction of a rotational thromboelastometry–based algorithm. Liver Transpl. 2015;21:169–79. doi: 10.1002/lt.24030. [DOI] [PubMed] [Google Scholar]
- 7.Hernández-Gea V, Berbel C, Baiges A, García-Pagán JC. Acute variceal bleeding: risk stratification and management (including TIPS) Hepatol Int. 2017. [Epub ahead of print] [DOI] [PubMed]
- 8.Jeong SM, Song JG, Seo H, Choi JH, Jang DM, Hwang GS. Quantification of Both Platelet Count and Fibrinogen Concentration Using Maximal Clot Firmness of Thromboelastometry During Liver Transplantation. Transplant Proc. 2015;47:1890–5. doi: 10.1016/j.transproceed.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Dötsch TM, Dirkmann D, Bezinover D. Assessment of standard laboratory tests and rotational thromboelastometry for the prediction of postoperative bleeding in liver transplantation. Br J Anaesth. 2017;119:402–10. doi: 10.1093/bja/aex122. [DOI] [PubMed] [Google Scholar]
- 10.Thakrar S, Mallet S. Thrombocytopenia in cirrhosis: Impact of fibrinogen on bleeding risk. World J Hepatol. 2017;9:318–25. doi: 10.4254/wjh.v9.i6.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seo H, Choi JH, Moon YJ, Jeong SM. FIBTEM of Thromboelastometry does not Accurately Represent Fibrinogen Concentration in Patients with Severe Hypofibrinogenemia During Liver Transplantation. Ann Transplant. 2015;20:342–50. doi: 10.12659/AOT.893741. [DOI] [PubMed] [Google Scholar]
- 12.Lentschener C, Flaujac C, Ibrahim F. Assessment of haemostasis in patients with cirrhosis: Relevance of the ROTEM tests?A prospective, cross-sectional study. Eur J Anaesthesiol. 2016;33:126–33. doi: 10.1097/EJA.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 13.Scărlătescu E, Lancé MD, White NJ, Aramă SS, Tomescu DR.. Effects of malignancy on blood coagulation in septic intensive care patients. Blood Coagul Fibrinolysis. 2018;29:92–6. doi: 10.1097/MBC.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 14.Solomon C, Rannuci M, Hochleitner G, Schochl H, Schlimp C. Assessing the Methodology for Calculating Platelet Contribution to Clot Strength (Platelet Component) in Thromboelastometry and Thrombelastography. Anesth Analg. 2015;121:868–78. doi: 10.1213/ANE.0000000000000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smart L, Mumtaz K, Scharpf D. Rotational Thromboelastometry or Conventional Coagulation Tests in Liver Transplantation: Comparing Blood Loss, Transfusions, and Cost. Ann Hepatol. 2017;16:916–23. doi: 10.5604/01.3001.0010.5283. [DOI] [PubMed] [Google Scholar]