Abstract
Though palliative care is appropriate for patients with serious illness at any stage of the illness and treatment process, the vast majority of palliative care is currently delivered in inpatient medical settings in the past month of life during an acute hospitalization. Palliative care can have maximal benefit to patients when it is integrated earlier in the illness trajectory. One possible way to increase earlier palliative care use is to screen for unmet palliative care needs in community settings. The goal of this study was to assess the rates of unmet palliative care needs in older adults who attend New York City–based senior centers. The results of this study revealed that 28.8% of participants screened positive for unmet palliative care needs. Lower education and living alone were predictors of positive palliative care screens, but age, gender, marital status, and race were not. This study determined that the rate of unmet palliative care needs in community-based older adults who attend senior center events was high and that living arrangement and education level are both correlates of unmet palliative care needs. Screening for unmet palliative care needs in community settings is a promising approach for moving palliative care upstream to patients who could benefit from the additional supportive services prior to an acute hospitalization.
Keywords: palliative care, community, screening, palliative care screening, senior centers, community-based palliative care
Introduction
Palliative care focuses on improving quality of life in patients with advanced illness and their family members. Patients who receive palliative care experience improved quality of life,1–5 fewer depressive symptoms,1,3,5 decreased emergency room visits and hospital admissions,6–8 as well as higher levels of satisfaction with care.4 Despite these documented positive associations with palliative care, many individuals who could benefit from palliative care never see a palliative care provider.9 Currently, the vast majority of palliative care is delivered in the inpatient medical setting during an acute hospitalization,10 but palliative care is appropriate at any stage of serious illness and can be most beneficial when integrated early in a patient’s illness trajectory.1,11–13 The number of older adults living with serious illness is expected to increase rapidly as the population ages,14 and palliative care teams will need to find additional ways to reach patients with high multidomain symptom burden who could benefit from palliative care.
One way to increase the reach of palliative care is to screen for palliative care needs in nonclinical settings, such as senior centers, case management agencies, and congregate housing facilities. In 2012, approximately 13 million older adults (ages 60 years and above) received services from community-based supports and organizations.15 Screens implemented in community-based organizations could reach large numbers of older adults from diverse backgrounds and theoretically increase access to palliative care services providing that screen-positive adults are referred to outpatient-based palliative care programs.
In order to identify individuals with unmet palliative care needs in the community, appropriate screening measures would have to be utilized. We developed a new screening tool using a community-based participatory research approach that is intended to be used in nonclinical settings.16 Prior screening tools for unmet palliative care needs have primarily focused on inpatient populations, patients with cancer, and patients who are nearing the end of life17,18 and thus are not appropriate for community-based populations who are likely earlier in the illness trajectory. The new tool is composed of 3 specific domains: symptom burden, emotional concerns, and goals of care (Table 1). A preliminary study recently demonstrated that the newly developed tool can be feasibly implemented in senior centers to screen for unmet palliative care needs in community-dwelling older adults.16
Table 1.
Items in the Community-Based Palliative Care Screening Tool.16
| Physical symptoms |
| Feeling tired or fatigued |
| Low energy |
| Difficulty sleeping (sleeping too much or can’t sleep) |
| Pain or physical discomfort |
| Difficulty standing or walking |
| Shortness of breath |
| Emotional concerns |
| Feeling nervous, anxious, or on edge |
| Not being able to stop or control worrying |
| Having little interest or pleasure in usual activities |
| Feeling down, depressed, or hopeless |
| Feeling overwhelmed about any medical treatment |
| Feeling a loss of meaning or purpose in your life at the moment |
| Worried about being dependent, or a burden on friends of family |
| Feeling like there is no one in your life whom you can talk to |
| Having conflicts with friends or family |
| Goals of care |
| Feeling confused about your medical care |
| Feeling uncomfortable asking questions about your care |
| Feeling like you want more support with your medical care |
| Feeling like you need access to more medical providers |
| Feeling like you need more information about available providers |
| Have you given thought to how you want to be cared for when your illness(es) advance? |
| Have you talked with anyone about how you want to be cared for? |
| Do you have a document that indicates what your wishes are and who will make decisions for you? |
| Do you have a Health Care Proxy? Have you completed a Living Will? |
The goal of this study was to assess the rates of unmet palliative care needs in older adults attending several New York City–based senior centers. We hypothesized that administering the palliative care screening tool in New York City–based senior centers would successfully identify individuals with unmet palliative care needs. We further hypothesized that positive screens would be more prevalent among participants with demographic factors associated with higher unmet palliative care needs and more barriers to receiving a palliative care referral. For example, older adults,19–25 ethnic minorities,15,25,26 men,21,22 unmarried or widowed adults,19 and adults without home caregivers21 are all less likely to receive palliative care services despite, in many cases, having high needs.
Methods
Sample
The current study was conducted as part of the TRIO for Successful Aging (TRIO) Program, a partnership between the Institute of Geriatric Psychiatry in the Department of Psychiatry and the Division of Geriatrics and Palliative Medicine, both located at Weill Cornell Medicine, and the New York City Department for the Aging.27 TRIO integrates the importance of medical and social aspects of chronic illnesses into mental health service delivery in New York City–based senior center settings. Designed using an innovative service delivery model, that is, a combination of innovative outreach and case identification, TRIO brings mental health services to community-based settings.28 TRIO staff host a variety of engagement activities (eg, lectures, discussion groups) to promote mental health awareness and healthy aging in participating senior centers. As part of the service delivery model, multifaceted needs assessments are conducted with consenting older adults who attend the engagement activities.
Participants in the current study consisted of adults aged 60 years and above receiving services at 1 of 5 senior centers located in Brooklyn and Staten Island, New York. TRIO staff asked older adults attending the center-based events whether they would be willing to participate in a needs assessment. The palliative care screening tool was administered as part of a broader needs assessment that included questions about elder abuse, functional impairment, and mental health care, among other domains and took approximately 40 minutes to administer. Assessments were conducted in English, Cantonese, or Spanish when appropriate and when multilingual staff were available. The needs assessment underwent back-translation procedures to ensure content was identical in English, Cantonese, and Spanish. Any older adult who screened positive on the palliative care screening tool was offered a palliative care referral to a local outpatient palliative care clinic. Participation was voluntary, and participants received a tote bag as a token of appreciation.
The local institutional review board approved the project and all participants provided oral consent.
Measures
Demographic data (ie, age, gender, marital status, education level, senior center location, and living status) were collected at the time of the assessment. Medical comorbidity data were also collected using a 22-item medical condition checklist.29 A comorbidity sum score was calculated, with 1 point attributed to each item on the checklist; possible sum scores ranged from 0 to 22, with higher scores reflecting a greater number of medical conditions.
The recently developed 22-item palliative care screening tool was also adminstered.16 For each item, the participant was asked whether he or she experienced a given concern “never,” “sometimes,” or “all the time.” The 22 items are divided into 3 domains: physical symptoms, emotional concerns, and goals of care (Table 1). Participants screened positive if they reported experiencing 2 or more items within a domain “all the time” in at least 2 domains. For example, if a patient experienced 2 or more physical symptoms and 2 or more emotional concerns all of the time, they were considered to have screened positive for unmet palliative care needs.
Analysis
Means (M) and standard deviations (SD) were computed to characterize the sample. χ2 tests were conducted to assess for differences in screening outcome (positive vs negative) for categorical variables (gender, education level, living situation, marital status, and race), and t tests were used for to determine whether age or number of medical comorbidities varied between those who screened positive versus negative. SPSS version 24 was used to perform all statistical analyses.
Results
Over the 18-month recruitment period (July 2016 to December 2017), 240 individuals provided oral consent to complete a needs assessment, and 219 (91.3%) completed the palliative care screener. Demographic characteristics of the sample are shown in Table 2.
Table 2.
Demographics and Associations With Screening Positive on Palliative Care Screen.
| n (%)/M (SD) | Percentage of Category With Positive Screen | P Value | |
|---|---|---|---|
| Age (n = 237) | 75.01 (9.14) | NA | NS |
| Gender (n = 237) | |||
| Male | 69 (29.1) | 22.6 | NS |
| Female | 168 (70.9) | 31.2 | |
| Race (n = 230) | |||
| White | 124 (51.7) | 30.9 | NS |
| Nonwhite | 106 (46.1) | 25.7 | |
| Education (n = 200) | |||
| <High school | 27 (11.3) | 52.1 | .03 |
| High school | 74 (30.8) | 24.6 | |
| College + | 99 (41.3) | 28.3 | |
| Marital status (n = 218) | |||
| Married | 63 (28.4) | 26.3 | |
| Divorced | 74 (30.8) | 35.9 | |
| Single | 42 (17.5) | 28.1 | |
| Widowed | 34 (14.2) | 25.4 | |
| Other | 6 (2.5) | 5.3 | NS |
| Living arrangement (n = 217) | |||
| Alone | 101 (46.5) | 36.7 | |
| Not alone | 116 (53.5) | 23.6 | .046 |
| Medical comorbidities | 4.2 (2.7) | NA | .04 |
| (n = 215) | |||
Abbreviations: M, mean; NA, not applicable; NS, nonsignificant; SD, standard deviation.
Screening Tool Results
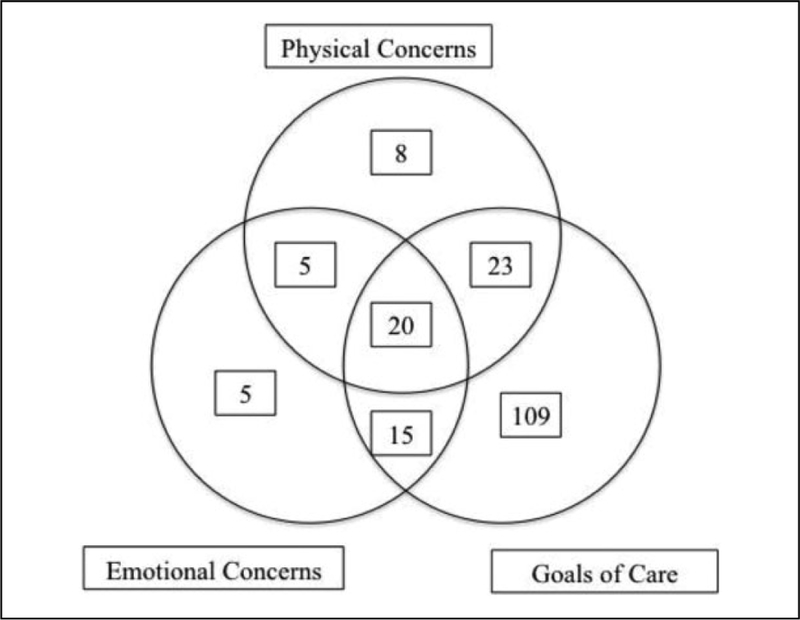
Of the 219 participants, 63 (28.8%) screened positive on the palliative care screening tool (ie, endorsed experiencing at least 2 symptoms “all of the time” in at least 2 domains). Across the 3 palliative care domains on the screening tool, participants screened positive most frequently for unmet needs in goals of care (n = 166, 75.1%) followed by physical concerns (n = 59, 25.7%) and emotional concerns (n = 50, 21.8%). Figure 1 shows the breakdown of total positive screens by domain. For example, 5 participants endorsed having emotional concerns but did not screen positive on either goals of care or physical concerns while 15 partipants screened positive for both emotional concerns and goals of care concerns.
Figure 1.
Breakdown of positive screens by domain.
Predictors of Positive Screen
The following variables were examined as possible predictors of a positive palliative care screen: age, race/ethnicity, gender, marital status, education level, living situation, and the number of medical comorbidities (Table 2). Age, gender, marital status, and race were not associated with screen positives; however, education, the number of medical comorbidities, and living arrangement were significantly associated with a screen-positive result. Those with lower education were significantly more likely to screen positive for unmet palliative care needs, χ2 (2, n = 182) = 6.8 (P < .05). The percentage of positive palliative care screens in individuals with less than a high school education was 52% compared with 25% and 28% for those with a high school education or college and graduate school education, respectively. Regarding living arrangements, the percentage of positive screens among individuals living alone was 37% compared to 24% for those who did not live alone, χ2 (2, n = 196) 4.0 (P < .05).
Finally, there was a significant difference in the number of medical comorbidities in those who screened positive for palliative care needs compared to those who screened negative (M = 4.89 [SD = 2.64] and M = 3.96 [SD = 2.64], respectively; t[178] = 2.05, P < .04).
Discussion
This study sought to examine the rates and predictors of unmet palliative care needs in an urban community-based sample using a newly developed palliative care needs screening tool.16 Our results demonstrated that over one-quarter of seniors who attend community-based senior centers in New York City screen positive for unmet palliative care needs and would therefore likely benefit from receiving palliative services. Given the high rates of individuals in the community who may benefit from palliative care, more outpatient palliative care services are warranted, and community-based agencies, such as senior centers, represent feasible locations to screen for unmet palliative care needs in the community.
This study identified several predictors of positive palliative care screens in community settings. Having less education, higher rates of medical comorbidities and living alone were associated with screening positive for unmet palliative care needs. Lower education is associated with lower socioeconomic status and reduced access to health care, as well as lower health literacy and limited knowledge of end-of-life care.30 Given the many additional barriers to quality health care that adults with limited education face, it is unsurprising that lower education was associated with more unmet palliative care needs. Appropriate informational resources about palliative care, such as educational pamphlets and videos, must be developed to reach individuals with high palliative care needs and low education. Furthermore, prior research has highlighted that people are generally unaware of or misinformed about palliative care,31,32 which may serve as a key barrier to accessing the service. Fortunately, preliminary studies suggest that brief videos and informational pamphlets are successful methods for improving peoples’ knowledge of palliative care services,33 but more research is needed to elucidate the role knowledge of palliative services has in increasing access to palliative care.
Living alone was also associated with higher rates of unmet palliative care needs. Older adults who live alone may experience more psychological distress than those who live with a partner or spouse, which could contribute to or exacerbate mental health problems and other difficulties related to end of-life planning.34–36 Given the results of this study, older adults who live alone may be good targets for more rigorous screening and assessment for unmet palliative care needs.
Similarly, individuals who screened positive for unmet palliative care needs had more medical comorbidities, on average, than individuals who screened negative. This aligned with our hypothesis, as medical illnesses are associated with increased physical symptom burden. Given that physical symptomatology is a domain on the palliative care screening tool, we expected individuals with positive screens to have more medical illnesses.
Though age, gender, race, and marital status were hypothesized to be predictors of positive palliative care screens, our study failed to confirm these anticipated relationships. As adults age, they tend to have more medical comorbidities,37 which could contribute to screening positive on palliative care needs assessments. However, all adults in this study were older individuals who were able to attend activities at a senior center, which implies a reasonable level of health and functional status. Age by itself was therefore not a predictor; however, the number of medical conditions was significantly predictive of positive palliative care screens. In populations that are more heterogeneous in regard to age, it may make sense to include age as a possible predictor of unmet palliative care needs, but results from our study suggest that age is not predictive of unmet palliative care needs in a population of adults older than 60 years who are attending senior centers.
Our results did not confirm the previous literature that suggested that men, racial minorities, and unmarried individuals are more likely to have palliative care needs. Perhaps, receiving services at senior centers mitigates the isolation and lack of emotional support associated with these variables, as senior center programs have been shown to improve both physical and emotional health.38
Our study has several limitations. Our sample was likely subject to selection bias as participants were individuals who attended activities promoting health and wellness. These participants were likely more open to talking about health or may have more health concerns than the average older adult. Additionally, our study was limited to 5 senior centers in 2 boroughs of New York City, so our findings may not be generalizable to the broader older adult population nor nonurban-dwelling older adults. Another limitation is that we did not collect data on whether participants who screened positive and received a palliative care referral followed through with the referral. Further studies looking at the follow-through rate of palliative care referrals following a positive screen are warranted to determine the effectiveness of screening for unmet palliative care needs and referring for appropriate services. Lastly, we had incomplete or missing data for 40 participants. We handled missing data by not analyzing cases that were missing variables of interest in each analysis. Sample sizes for each analysis are reported in Table 2.
Conclusions
Identifying individuals with unmet palliative care needs in a nonclinical setting is feasible; however, challenges related to how best to address unmet needs in the community remain. For example, there are limited resources available for out-patient palliative care despite the growing palliative care needs of community-based older. Given the success of identifying palliative care needs through collaboration with preexisting programs in the aging services network, there may be value in exploring the possibility of partnerships between aging services and clinical palliative care providers to deliver palliative services to community-based adults. Screening for and delivering palliative care to community-based older adults in settings that they already frequent, such as senior centers, have the potential to remove many of the obstacles older adults face in accessing health care, including issues of mobility and disability.39,40
Acknowledgments
The authors would like to acknowledge the older adults and aging services staff who support our work.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Elissa Kozlov, PhD, is supported by a fellowship from NIH/NIA (T32 AG049666–01A1 PI: Reid, M.C/Prigerson, HG). Jo Anne Sirey, PhD, is supported by grants from NIH/NIMH (P50 MH113838) and the NYC Department for the Aging. M. Carrington Reid is supported by grants from NIH/NIA (2P30AG022845–14 and K24AGO53462).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi:10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 2.Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I. Effectiveness of specialized palliative care: a systematic review. JAMA. 2008;299(14):1698–1709. doi:10.1001/jama.299.14.1698. [DOI] [PubMed] [Google Scholar]
- 3.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer. JAMA. 2009;302(7):741–749. doi:10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greer JA, Traeger L, Bemis H, et al. A pilot randomized controlled trial of brief cognitive-behavioral therapy for anxiety in patients with terminal cancer. Oncologist. 2012;17(10): 1337–1345. doi:10.1634/theoncologist.2012-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pirl WF, Greer JA, Traeger L, et al. Depression and survival in metastatic non-small-cell lung cancer: effects of early palliative care. J Clin Oncol. 2012;30(12):1310–1315. doi:10.1200/JCO.2011.38.3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seow H, Brazil K, Sussman J, et al. Impact of community based, specialist palliative care teams on hospitalisations and emergency department visits late in life and hospital deaths: a pooled analysis. BMJ. 2014;348: g3496. doi:10.1136/bmj.g3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55(7):993–1000. doi:10.1111/j.1532-5415.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 8.Fernandes R, Braun KL, Ozawa J, Compton M, Guzman C, Somogyi-Zalud E. Home-based palliative care services for under-served populations. J Palliat Med. 2010;13(4):413–419. doi:10.1089/jpm.2009.0216. [DOI] [PubMed] [Google Scholar]
- 9.Center for the Advancement of Palliative Care. Palliative Care Service Penetration by Hospital Size, 2015. New York, NY; 2015. https://registry.capc.org/wp-content/uploads/2016/10/PalliativeCarePenetration2015.pdf. Accessed May 7, 2018.
- 10.Morrison RS. Models of palliative care delivery in the United States. Curr Opin Support Palliat Care. 2013;7(2):201–206. doi:10.1097/SPC.0b013e32836103e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devi PS. A timely referral to palliative care team improves quality of life. Indian J Palliat Care. 2011;17(suppl):S14–S16. doi:10.4103/0973-1075.76233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: outcomes from the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33(13): 1446–1452. doi:10.1200/JCO.2014.58.7824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parikh RB, Kirch RA, Smith TJ, Temel JS. Early specialty palliative care — translating data in oncology into practice. N Engl J Med. 2013;369(24):2347–2351. doi:10.1056/NEJMsb1305469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Center to Advance Palliative Care. Palliative care facts and stats. 2014. https://media.capc.org/filer_public/68/bc/68bc93c7-14ad-4741-9830-8691729618d0/capc_press-kit.pdf. Accessed May 7, 2018.
- 15.Siegler EL, Lama SD, Knight MG, Laureano E, Reid MC. Community based supports and services for older adults: a primer for clinicians. J Geriatr. 2013;18(9):1199–1216. doi:10.1016/j.micinf.2011.07.011.Innate. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghesquiere A, Gardner DS, McAfee C, et al. Development of a community-based palliative care screening tool for underserved older adults with chronic illnesses. Am J Hosp Palliat Care. 2018: doi:http://10.1177/1049909117749467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Isenberg S, Aslakson R, Dy SM, et al. Assessment tools for palliative care. 2017;(30). doi:10.23970/AHRQEPCTB30. [PubMed] [Google Scholar]
- 18.Emanuel LL, Alpert HR, Emanuel EE. Concise screening questions for clinical assessments of terminal care: the needs near the end-of-life care screening tool. J Palliat Med 2001;4(4):465–474. doi:10.1089/109662101753381601. [DOI] [PubMed] [Google Scholar]
- 19.Kozlov E, McDarby M, Reid MC, Carpenter BD. Knowledge of palliative care among community-dwelling adults. Am J Hosp Palliat Med 2017:104990911772572. doi:10.1177/1049909117725725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burge FI, Lawson BJ, Johnston GM, Grunfeld E. A population-based study of age inequalities in access to palliative care among cancer patients. Med Care. 2008;46(12):1203–1211. doi:10.1097/MLR.0b013e31817d931d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burge F, Johnston G, Lawson B, Dewar R, Cummings I. Population-based trends in referral of the elderly to a comprehensive palliative care programme. Palliat Med. 2002;16(3): 255–256. doi:10.1191/0269216302pm550xx. [DOI] [PubMed] [Google Scholar]
- 22.Rosenwax LK, McNamara BA. Who receives specialist palliative care in Western Australia – and who misses out. Palliat Med 2006;20(4):439–445. doi:10.1191/0269216306pm1146oa. [DOI] [PubMed] [Google Scholar]
- 23.Burt J, Raine R. The effect of age on referral to and use of specialist palliative care services in adult cancer patients: a systematic review. Age Ageing. 2006;35(5):469–476. doi:10.1093/ageing/afl001. [DOI] [PubMed] [Google Scholar]
- 24.Walshe C, Todd C, Caress A, Chew-Graham C. Patterns of access to community palliative care services: a literature review. J Pain Symptom Manage. 2009;37(5):884–912. doi:10.1016/j.jpainsymman.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Adsersen M, Thygesen LC, Jensen AB, Neergaard MA, Sjøgren P, Groenvold M. Is admittance to specialised palliative care among cancer patients related to sex, age and cancer diagnosis? A nation-wide study from the Danish Palliative Care Database (DPD). BMC Palliat Care 2017;16(1). doi:10.1186/s12904-017-0194-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson KS. Racial and ethnic disparities in palliative care. J Palliat Med 2013;16(11):1329–1334. doi:10.1089/jpm.2013.9468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sirey J Reducing Depression and Suicide Risk by Integrating Brief Therapy into Senior Centers in NYC. Lecture Presented at the International College of Geriatric Psychoneuropharmcology Annual Meeting; October 2017; Chicago Illinois. [Google Scholar]
- 28.Sirey JA, Berman J, Halkett A, et al. Storm impact and depression among older adults living in hurricane sandy-affected areas. Disaster Med Public Health Prep. 2017;11(1):97–109. doi:10.1017/dmp.2016.189. [DOI] [PubMed] [Google Scholar]
- 29.Lawton MP, Moss M, Fulcomer M, Kleban MH. A research and service oriented multilevel assessment instrument. J Gerontol. 1982;37(1):91–99. doi:10.1093/geronj/37.1.91. [DOI] [PubMed] [Google Scholar]
- 30.Silveira MJ, Dipiero A, Gerrity MS, Page P, Feudtner C. Patients’ knowledge of options at the end of life: ignorance in the face of death. JAMA. 2000;284(19):2483–2488. doi:[pii] [DOI] [PubMed] [Google Scholar]
- 31.Kozlov E, McDarby M, Reid MC, Carpenter BD. Knowledge of palliative care among community-dwelling adults. Am J Hosp Palliat Med. 2018;35(4):647–651. doi:10.1177/1049909117725725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shalev A, Phongtankuel V, Kozlov E, et al. Awareness and mis-perceptions of hospice and palliative care: a population-based survey study. Am J Hosp Palliat Med. 2018;35(3):431–439. doi:10.1177/1049909117715215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozlov E, Reid MC, Carpenter BD. Improving patient knowledge of palliative care: a randomized controlled intervention study. Patient Educ Couns. 2017;100(5):1007–1011. doi:10.1016/j.pec.2016.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henning-Smith C Quality of life and psychological distress among older adults: the role of living arrangements. J Appl Gerontol 2016;35(1):39–61. doi:10.1177/0733464814530805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kharicha K, Iliffe S, Harari D, Swift C, Gillmann G, Stuck AE. Health risk appraisal in older people 1: are older people living alone an ‘at-risk’ group? Br J Gen Pract. 2007;57(537):271–276. http://www.ncbi.nlm.nih.gov/pubmed/17394729. Accessed February 26, 2018. [PMC free article] [PubMed] [Google Scholar]
- 36.Hellströ Y, Persson G, Hallberg IR. Quality of life and symptoms among older people living at home. J Adv Nurs. 2004;48(6): 584–593. http://www.diva-portal.org/smash/get/diva2:838043/FULLTEXT01.pdf. Accessed February 26, 2018. [DOI] [PubMed] [Google Scholar]
- 37.Gerteis J, Izrael D, Deitz D, et al. Multiple chronic conditions chartbook 2014. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf. Accessed May 7, 2018.
- 38.Hamar B, Coberley CR, Pope JE, Rula EY. Impact of a senior fitness program on measures of physical and emotional health and functioning. Popul Health Manag 2013;16(6):364–372. doi:10.1089/pop.2012.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blazer DG, Landerman LR, Fillenbaum G, Homer R. Health services access and use among older adults in North Carolina: urban vs rural residents; 1995. https://ajph.aphapublications.org/doi/pdfplus/10.2105/AJPH.85.10.1384. Accessed May 7, 2018. [DOI] [PMC free article] [PubMed]
- 40.Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to health care access among the elderly and who perceives them. Am J Public Health. 2004;94(10):1788–1794. http://www.ncbi.nlm.nih.gov/pubmed/15451751. Accessed April 24, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]