Abstract
Background and aims:
South Asian (SA) individuals are thought to represent a group that is at high-risk for atherosclerotic cardiovascular disease (ASCVD). However, the performance of the Pooled Cohort Equations (PCE) remains uncertain in SAs living in the US. We aimed to study the interplay between predicted 10-year ASCVD risk and coronary artery calcium (CAC) in SAs compared to other racial/ethnic groups.
Methods:
We studied 536 SAs from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study, and 2,073 Non-Hispanic Whites (NHWs), 1,514 African Americans (AAs), 1,254 Hispanics, and 671 Chinese Americans (CAs) from the Multi-Ethnic Study of Atherosclerosis (MESA) who were not currently on statins. We used logistic regression models to assess the association between race/ethnicity and CAC within each ASCVD risk stratum.
Results:
SAs at low and at intermediate estimated ASCVD risk were more likely to have CAC =0 compared to NHWs, while SAs at high risk had a similar CAC burden to NHWs. For example, intermediate-risk SAs had a 73% higher odds of CAC =0 compared to NHWs (95% 1.00–2.99), while high-risk SAs were equally likely to have CAC =0 (OR 0.95, 95% CI 0.65–1.38) and CAC >100 (OR 0.86, 95% CI 0.61–1.22).
Conclusions:
Our results suggest that the extent of ASCVD risk overestimation using the PCEs may be even greater among SAs considered at low and intermediate risk than among NHWs. Studies with incident ASCVD events are required to validate and/or recalibrate current ASCVD risk prediction tools in this group.
Keywords: Atherosclerosis, Cardiovascular Disease, Coronary Artery Calcium, Race/Ethnicity, Risk, South Asian
Introduction
South Asian (SA) individuals currently represent the second fastest growing ethnic group in the US, with nearly 5 million residents.1 Several studies have reported a high prevalence of cardiovascular risk factors and atherosclerotic cardiovascular disease (ASCVD) in this group, the latter being higher among SAs than any other racial/ethnic group living in North America or Europe.2–6
SAs therefore represent a group in whom ASCVD prevention efforts should be intensified.7,8 However, in the US there is no specific guidance for ASCVD risk assessment in these individuals. The 2013 American College of Cardiology / American Heart Association (ACC/AHA) ASCVD risk assessment guidelines included the pooled cohort equations (PCE), which allow estimating 10-year ASCVD risk by race/ethnicity [non-Hispanic Whites (NHWs) and African Americans (AAs)] and sex. For other racial/ethnic groups living in the US, including individuals of SA ancestry, the ACC/AHA recommends using the equations for NHWs.9 However, the performance of the equations and their potential for over- or underestimation of ASCVD risk in this group remains unknown.10
To date, there is no study on SAs living in the US with sufficient follow-up length to allow a formal 10-year validation of the 2013 ACC/AHA PCE. The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study11 enrolled individuals of SA ancestry in the US and assessed coronary artery calcium (CAC) burden.11,12 CAC is a robust predictor of ASCVD events13–16 and, in the absence of prospective ASCVD outcomes, provides an opportunity to conduct a preliminary evaluation of the performance of the risk estimator in SA individuals.17
The aim of our study was therefore to evaluate, in a representative population of SAs in the US, the interrelationship between 10-year ASCVD risk estimates (using the 2013 ACC/AHA PCE for NHWs) and CAC burden. Specifically, we assessed the prevalence of clinically relevant CAC categories such as a CAC score of 0 (which is known to be associated with very low event rates)18 and a CAC score >100 (which is associated with high ASCVD event rates approaching secondary prevention populations)16. For comparison, we performed the same analysis among the 4 racial/ethnic groups included in the similarly-designed Multi-Ethnic Study of Atherosclerosis (MESA).19
Materials and methods
Study design
Full details of the design and methods of the MASALA and MESA studies have been reported elsewhere.11,20 Briefly, MASALA is a community-based prospective cohort study of 906 asymptomatic US adults of SA ancestry free from clinical ASCVD, who were enrolled from two clinical sites (San Francisco Bay Area at the University of California, San Francisco (UCSF) and the greater Chicago area at Northwestern University (NWU). MASALA investigators recruited participants of SA ancestry, defined as having at least 3 grandparents born in India, Pakistan, Bangladesh, Nepal, or Sri Lanka. The first study examination began in October 2010, and final participant enrollment was concluded in March 2013. The study protocol was designed to be similar to MESA, and was approved by the institutional review boards of University of California, San Francisco and Northwestern University. All participants provided written informed consent.11
MESA is a multi-ethnic, community-based, prospective cohort study of 6,814 men and women aged 45 to 84 years who were free from clinical ASCVD at the time of recruitment. Study participants were enrolled between July 2000 and September 2002 at six field centers in the US and identified themselves as NHW, AA, Hispanic (Latino) or Chinese American (CA). The study was approved by the institutional review boards at each center and all MESA participants provided written informed consent.20
Study population
All participants from MASALA and MESA with information on baseline CAC burden were included. Participants from both studies were free of clinical ASCVD at the time of study entry. To assess the performance of the PCE specifically in the population they are intended to be used,9 we excluded participants older than 80 years and those already taking statins. To allow direct comparisons between the two studies, MASALA participants aged <45 years were also excluded from the analysis as the minimum age of MESA participants at enrollment was 45 years. Finally, individuals with missing information on any of the variables used by the 2013 ACC/AHA PCE were excluded.
10-year ASCVD risk estimation
In each study participant, 10-year ASCVD risk was estimated using the ACC/AHA 2013 PCE.9 Risk estimates for NHWs, Latinos, CAs and SAs were calculated using the equations for NHWs men and women, and the corresponding PCE for AA men and women were used for ASCVD risk estimates in AAs.9
Assessment of coronary artery calcium
Details on the CAC quantification methods implemented in each of the two studies have been reported elsewhere. In MESA, CAC was measured was measured using either an electronbeam CT (at the Chicago, Los Angeles, and New York centers) or a multidetector CT (at the Baltimore, Forsyth County, and St. Paul centers). All images were interpreted at the Los Angeles Biomedical Research Center, Torrance, CA. In MASALA, CAC was assessed using a cardiacgated electron-beam computed tomography scanner.21 All images were analyzed at the Los Angeles Biomedical Research Center according to MESA study methods.11 In both studies CAC scans were interpreted blinded to race/ethnicity and quantified using the Agatston scoring system.12 In MESA, both intraobserver and interobserver agreement for CAC were excellent (kappa statistics, 0.93 and 0.90, respectively). These estimates are expected to be similar for MASALA give that identical scanning protocols were used and images were interpreted at the same reading center.
Assessment of traditional cardiovascular risk factors
Information on sociodemographic characteristics, tobacco use, family history of coronary heart disease, medication use, and physical activity was collected using validated questionnaires that were similar for both studies. The body mass index was calculated as weight in kilograms divided by height in meters squared. Systolic and diastolic blood pressures were measured three times using an automated sphygmomanometer and the mean of the last two measurements was used. Lipid profile and plasma glucose levels were measured in blood samples collected at baseline and after a 12-hour overnight fast.
Statistical analyses
Baseline demographics, cardiovascular risk factors and 10-year ASCVD risk estimates of the study participants were described for each race/ethnicity, both overall and further stratified by ASCVD risk score categories. Categorical variables were presented as number (%), and continuous variables as mean (SD) or median (IQR) depending on the distribution of the data. Differences between racial/ethnic groups were assessed using chi-square tests, t-tests, and nonparametric tests as appropriate.
The frequency of ASCVD risk categories (low: <5%, intermediate: 5 to < 7.5%, and high: ≥7.5%) and the proportion of key, clinically relevant CAC score categories (0 and ≥100) were described for each racial/ethnic group adjusted for age. To study the interplay between 10year ASCVD risk estimates and CAC burden, we also described the distribution of clinically relevant age-adjusted CAC categories (0, 1–100, and ≥100) across ASCVD risk categories (<5%, ≥5 to 7.5%, and ≥7.5%), for each racial/ethnic group. Chi-square tests were used to compare these proportions across each racial/ethnic groups.
To compare CAC group distribution within similar risk groups across race/ethnicity, logistic regression was used to evaluate the associations between racial/ethnic groups (NHWs as the reference category) and CAC burden categories within each ASCVD risk group. For these analyses, dependent variables were CAC = 0 (vs. CAC > 0), and CAC > 100 (vs. CAC ≤ 100). Analyses were conducted both unadjusted and adjusting for age and sex.
Two sensitivity analyses were conducted. First, we repeated the analyses using alternative cutpoints for ASCVD risk categories: low (<5%), intermediate (5–15%), and high (>15%).22 Second, we excluded individuals considered to benefit from statin therapy by the ACC/AHA 2013 guidelines (LDL cholesterol ≥190 mg/dL, and individuals with diabetes and LDL cholesterol ≥70 mg/dL) despite the fact that they were not being treated with statins at baseline.9,23 Third we further adjusted for family history of CHD and education.
A p value <0.05 was considered statistically significant. All analyses were performed using Stata version 13 (StataCorp. 2011, College Station, TX).
Results
Study population
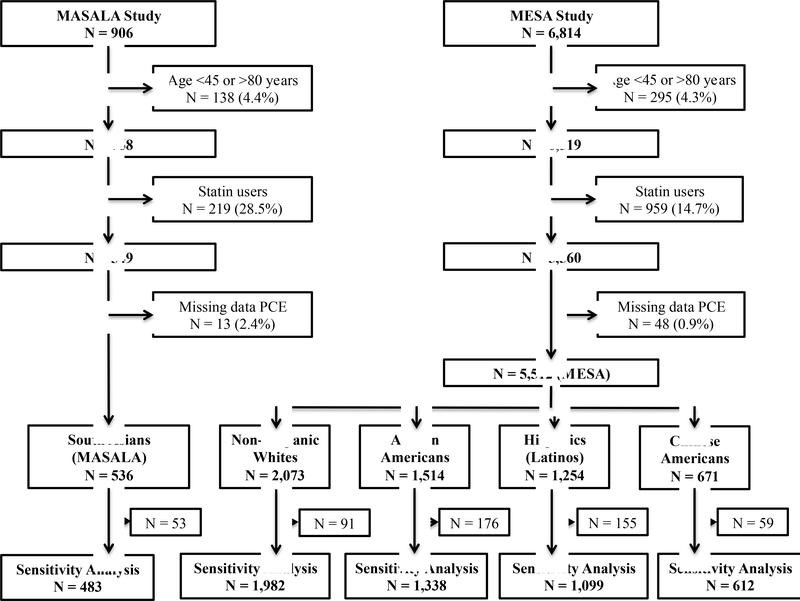
We included 536 SAs participants from MASALA, and 5,512 participants from MESA (2,073 NHW [37.6%], 1,514 AA [27.5%], 1,254 Hispanics [22.8%], and 671 CA [12.2%]), all of whom were not taking statins at baseline and had ages ranging 45–80 years (Figure 1).
Figure 1.
Flowchart diagram demonstrating inclusion/exclusion criteria in each cohort to derive the final study population We excluded participants older than 80 years and those already taking statins.
To allow direct comparisons between the two studies, MASALA participants aged <45 years were also excluded from the analysis as the minimum age of MESA participants at enrollment was 45 years. Finally, individuals with missing information on any of the variables used by the 2013 ACC/AHA PCE were excluded.
Table 1 presents the characteristics of the study participants by racial/ethnic group. MASALA participants were on average younger, had a higher educational level, lower estimated ASCVD risk, were less likely to smoke, and were less active compared to the racial/ethnic groups in MESA (all p <0.05). No clear differences were observed in the prevalence of other cardiovascular risk factors between SAs and the other racial/ethnic groups.
Table 1.
Baseline demographics, cardiovascular risk factors, and 10-year ASCVD estimated risk using the 2013 ACC/AHA risk estimator, by racial/ethnic group.
| South Asians (n = 536) | Non-Hispanic Whites (n = 2073) | African Americans (n = 1514 ) | Hispanics (Latinos) (n = 1254) | Chinese Americans (n = 671) | p value | |
|---|---|---|---|---|---|---|
| Age, y | 55 (50–62) | 61 (53–69) | 60 (52–68) | 59 (51–67) | 60 (53–69) | <0.001 |
| Men | 264(49) | 980 (47) | 689 (46) | 612 (49) | 332 (49) | 0.29 |
| Education > Bachelors | 467 (87) | 1069 (52) | 521 (34) | 133 (11) | 262 (39) | <0.001 |
| Family history of heart disease | 238 (45) | 963 (49) | 582 (41) | 464 (39) | 119 (19) | <0.001 |
| Current smoker | 19 (4) | 260 (13) | 290 (19) | 186 (15) | 42 (6) | <0.001 |
| SBP, mmHg | 125 (16) | 122 (20) | 131 (21) | 125 (21) | 123 (21) | <0.001 |
| BMI, kg/m2 | 25.4 (23.2–28.0) | 26.9 (24.0–30.3) | 29.4 (26.3–33.6) | 28.7 (25.9–31.9) | 23.7 (21.7–25.8) | <0.001 |
| LDL-C, mg/dL | 118 (98–136) | 119 (100–140) | 119 (97–137) | 120 (100–141) | 116 (99–134) | 0.01 |
| Medications for hypertension | 126 (24) | 452 (22) | 655 (43) | 321 (26) | 155 (23) | <0.001 |
| Diabetes | 43 (8) | 69 (3) | 154 (10) | 150 (12) | 52 (8) | <0.001 |
| Total cholesterol, mg/dL | 197(34) | 199 (35) | 191 (36) | 200 (38) | 195 (31) | <0.001 |
| HDL cholesterol, mg/dL | 49(41–59) | 50 (41–61) | 50 (41–61) | 45 (39–54) | 47 (40–56) | <0.001 |
| Triglycerides, mg/dL | 120 (89–159) | 112(76–161) | 90 (66–123) | 135(94–189) | 123 (86–169) | <0.001 |
| Physical activity, MET- min/week | 945 (330–1905) | 4328 (2340–7410) | 4725 (2295–8888) | 4440 (1815–8430) | 2730 (1403–5123) | <0.001 |
| 10-year ASCVD risk, % | 4.1 (1.7–9.2) | 6.9 (2.7–15.4) | 10.0 (5.0–17.5) | 7.0 (2.9–16.1) | 6.8 (2.5–15.7) | <0.001 |
| CAC, AU | 0 (0–32) | 2(0–110) | 0 (0–32) | 0 (0–36) | 0 (0–55) | <0.001 |
Data presented as n (%), mean (SD) or median (25th percentile – 75th percentile)
ASCVD = atherosclerotic cardiovascular disease; AU = Agatston units; CAC = coronary artery calcium; HDL = high density lipoprotein; SBP = systolic blood pressure; BMI = Body Mass Index; LDL-C = Low-Density Lipoprotein Cholesterol
Supplementary Tables 1–5 display the characteristics of the study participants further stratified by baseline 10-year ASCVD estimated risk. Among those at low (<5%) 10-year risk similar patterns were noted in the distribution of risk factors as in the overall group presented in Table 1. Among higher risk strata the following differences were noted: SAs at intermediate risk (5 to <7.5%) were more likely to be male, diabetic, and have higher triglyceride levels, while those at high risk (≥7.5%) were also more likely to be male compared to MESA participants (all p<0.05).
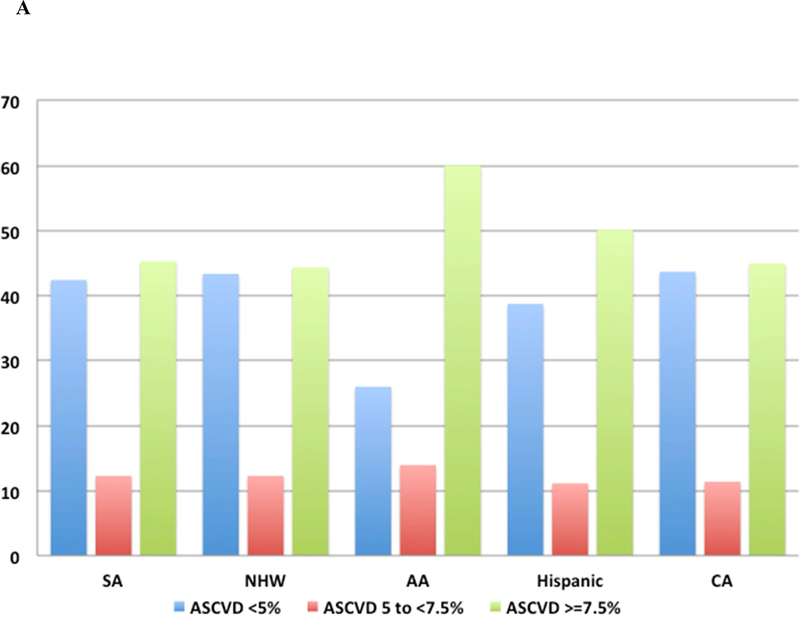
Distribution of estimated 10-year ASCVD risk
Figure 2A displays the age-adjusted distribution of 10-year ASCVD risk categories across racial/ethnic groups. The prevalence of low, intermediate, and high ASCVD risk was almost identical comparing SAs and NHWs.
Figure 2.
Distribution of categories.
(A) Distribution of low (<5%), intermediate (5 to 7.5%) and high (≥7.5%) 10-year estimated ASCVD risk categories by racial/ethnic group. (B) Distribution of clinically relevant coronary artery calcium categories (0, 1 – 100, >100), by racial/ethnic group. (C) Distribution of clinically relevant coronary artery calcium categories (0, 1 – 100, >100), by racial/ethnic group and ASCVD risk categories. Data are presented as percentages. AA = African American; CA = Chinese American; NHW = Non-Hispanic White; SA = South Asian; ASCVD = atherosclerotic cardiovascular risk disease; CAC = coronary artery calcium.
Burden of CAC in the study population
Figure 2B displays the age-adjusted distribution of key clinically relevant CAC burden categories across racial/ethnic groups. The prevalence of CAC was very similar comparing SAs to NHWs, with nearly 50% CAC =0 and 25% for CAC 1–100 and >100.
Interplay between 10-year ASCVD risk estimates and CAC burden
Table 2 and Figure 2C present age-adjusted proportions of CAC burden categories by ASCVD risk strata and racial/ethnic groups. Among SAs the prevalence of CAC=0 was inversely proportional to ASCVD risk (prevalence of CAC =0: 86%, 62%, and 34% for low, intermediate and high ASCVD risk groups respectively; p<0.001). Similar trends were noted among other race/ethnicities. In contrast, the prevalence of CAC >100 among SAs was correlated with estimated ASCVD risk (prevalence of CAC >100: 3%, 6%, and 31% for low, intermediate, and high ASCVD risk groups respectively; p < 0.001). The same was true for other race/ethnicities. Supplementary Table 6 presents these results using alternative ASCVD risk cutpoints (<5%, 5 to 15%, and >15%).
Table 2.
The prevalence of CAC* by 10-year ASCVD risk categories and racial/ethnic group.
| 10-Year ASCVD risk estimates (2013 ACC/AHA) | South Asians | Non-Hispanic Whites | African Americans | Hispanics (Latinos) | Chinese Americans |
|---|---|---|---|---|---|
| < 5% ASCVD risk | |||||
| CAC =0 | 237 (86) | 628 (70) | 326 (90) | 422 (82) | 212 (70) |
| CAC 1–100 | 48 (11) | 166 (23) | 47 (9) | 68 (16) | 55 (19) |
| CAC >100 | 10 (3) | 48 (7) | 7 (1) | 15 (2) | 16 (11) |
| 5 to 7.5%ASCVD risk | |||||
| CAC =0 | 43 (62) | 120 (48) | 141 (65) | 87 (63) | 36 (46) |
| CAC 1–100 | 22 (33) | 93 (37) | 45 (21) | 41 (28) | 30 (42) |
| CAC >100 | 6 (6) | 40 (14) | 21 (14) | 13 (9) | 10 (11) |
| ≥ 7.5% ASCVD risk | |||||
| CAC =0 | 48 (34) | 260 (31) | 445 (55) | 229 (44) | 106 (42) |
| CAC 1–100 | 56 (35) | 265 (30) | 266 (27) | 202 (31) | 112 (36) |
| CAC >100 | 66 (31) | 453 (38) | 216 (18) | 177 (25) | 93 (22) |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Results are age-standardized.
Data presented as n (%).
Percentages may not add 100% due to rounding.
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CAC = coronary artery calcium.
Associations between race/ethnicity and CAC burden within estimated ASCVD risk strata
Table 3 presents the associations between race/ethnicity and CAC categories across estimated 10-year ASCVD risk strata. In the low and intermediate ASCVD risk strata, SAs had a higher odds of CAC =0 compared to NHWs (ORs 1.26, 95% 0.91–1.76 and 1.73, 95% CI 1.00–2.99, respectively). In the high ASCVD risk group, SAs had similar odds of CAC=0 and CAC >100 compared to NHWs (OR 0.95, 95% CI 0.65–1.38 and 0.86, 95% CI 0.61–1.22 respectively).
Table 3.
Age- and sex-adjusted associations between race/ethnicity and CAC categories across 10-year ASCVD risk categories.
| 10-Year ASCVD risk estimates (2013 ACC/AHA) | South Asians | Non-Hispanic Whites | African Americans | Hispanics (Latinos) | Chinese Americans |
|---|---|---|---|---|---|
| Age- and sex-adjusted | |||||
| < 5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 1.26 (0.91, 1.76) | 1.00 (Ref) | 1.76 (1.26, 2.45) | 1.67 (1.25, 2.22) | 1.02 (0.74, 1.40) |
| CAC >100 (vs. CAC ≤100) | 0.67 (0.33, 1.35) | 1.00 (Ref) | 0.39 (0.17, 0.88) | 0.55 (0.30, 0.99) | 1.00 (0.56, 1.81) |
| 5 to < 7.5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 1.73 (1.00, 2.99) | 1.00 (Ref) | 2.23 (1.51, 3.30) | 1.74 (1.14, 2.66) | 1.03 (0.61, 1.72) |
| CAC >100 (vs. CAC ≤100) | 0.53 (0.21, 1.32) | 1.00 (Ref) | 0.68 (0.38, 1.21) | 0.58 (0.30, 1.14) | 0.79 (0.37, 1.67) |
| ≥ 7.5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 0.95 (0.65, 1.38) | 1.00 (Ref) | 1.97 (1.61, 2.40) | 1.47 (1.18, 1.85) | 1.47 (1.11, 1.95) |
| CAC >100 (vs. CAC ≤100) | 0.86 (0.61, 1.22) | 1.00 (Ref) | 0.44 (0.35, 0.54) | 0.52 (0.42, 0.65) | 0.47 (0.36, 0.62) |
Results presented as odds ratios (95% confidence intervals) of each of the CAC endpoints comparing individuals from each of the racial/ethnic groups to Non-Hispanic Whites (reference category).
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CAC = coronary artery calcium.
Among other racial/ethnic groups, AAs and Hispanics considered at low ASCVD risk had lower odds than NHWs of having CAC>100. Among individuals considered at intermediate ASCVD risk, AA and Hispanic ancestries were associated with higher odds of having CAC=0 compared to NHWs (ORs 2.23, 95% CI 1.51–3.30 and 1.74, 95% CI 1.14–2.66, respectively). In the high-risk stratum, AAs, Hispanics and CAs had higher odds of having CAC=0 than NHWs.
Supplementary Table 7 presents the results using alternative ASCVD risk cutpoints (<5%, 5–15%, and >15%). Similar results were observed in analyses further excluding individuals with LDL cholesterol >190 mg/dL and diabetic patients with LDL cholesterol > 70 mg/dL (Table 4, Supplementary Table 8). We also obtained similar results after additonally adjusting for family history of coronary heart disease and education (Supplementary Table 9).
Table 4.
Age- and sex-adjusted associations between race/ethnicity and CAC categories across 10-year ASCVD risk categories after further excluding individuals with LDL cholesterol > 190 mg/dL, and diabetic patients with LDL > 70 mg/dL.
| 10-Year ASCVD risk estimates (2013 ACC/AHA) | South Asians | Non-Hispanic Whites | African Americans | Hispanics (Latinos) | Chinese Americans |
|---|---|---|---|---|---|
| Age- and sex-adjusted | |||||
| < 5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 1.29 (0.92, 1.81) | 1.00 (Ref) | 1.73 (1.23, 2.43) | 1.71 (1.27, 2.29) | 1.03 (0.74, 1.42) |
| CAC >100 (vs. CAC ≤100) | 0.62 (0.30, 1.30) | 1.00 (Ref) | 0.41 (0.18, 0.93) | 0.54 (0.29, 1.00) | 1.04 (0.58, 1.88) |
| 5 to < 7.5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 1.79 (1.00, 3.20) | 1.00 (Ref) | 2.30 (1.54, 3.43) | 1.65 (1.07, 2.55) | 0.99 (0.58, 1.67) |
| CAC >100 (vs. CAC ≤100) | 0.59 (0.23, 1.48) | 1.00 (Ref) | 0.62 (0.34, 1.13) | 0.61 (0.31, 1.20) | 0.72 (0.33, 1.58) |
| ≥ 7.5% ASCVD risk | |||||
| CAC =0 (vs. CAC >0) | 0.96 (0.64, 1.45) | 1.00 (Ref) | 2.01 (1.63, 2.49) | 1.57 (1.23, 2.00) | 1.42 (1.05, 1.92) |
| CAC >100 (vs. CAC ≤100) | 0.83 (0.57, 1.22) | 1.00 (Ref) | 0.42 (0.34, 0.52) | 0.49 (0.38, 0.62) | 0.44 (0.32, 0.60) |
Results presented as odds ratios (95% confidence intervals) of each of the CAC endpoints comparing individuals from each of the racial/ethnic groups to Non-Hispanic Whites (reference category).
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CAC = coronary artery calcium.
Discussion
In two community-based study populations of adults living in the US comprising 5 racial/ethnic groups, a SA ancestry was associated with higher odds of having CAC=0 compared to NHWs in the low and in the intermediate risk groups, while SAs in the high risk group had a similar distribution of CAC compared to NHWs. These findings have implications for the interpretation of ASCVD risk estimates and for the utility of CAC scoring in SAs, a large group living in the US in whom optimal ASCVD risk estimation strategy is currently uncertain.
Our study has important clinical implications. In the absence of 10-year longitudinal data and therefore of specific ASCVD risk equations for SAs in the US, the ACC/AHA currently recommends using the 2013 PCE for NHWs to assess 10-year ASCVD risk in this group.9 Nevertheless, two considerations lead to great uncertainty when following this strategy. First, release in 2013 of the ACC/AHA PCE was followed by concerns regarding their potential for global ASCVD risk overestimation.24–26 Second, a number of studies have shown SAs having higher event rates than NHWs in almost every country where this has been evaluated.5,6,27–29 In this context, the performance of the 2013 PCE specifically in SAs is unclear. Based on our preliminary results, we posit that the PCEs may overestimate risk in low and intermediate risk SAs even to a greater extent than they do in NHWs.24,25
Previous reports comparing MASALA and MESA cohorts have shown SAs from MASALA and NHWs from MESA having a similar profile in terms of age-standardized CAC burden at baseline.21,30 Similar results have been reported in European studies as well.31 This appears to be true particularly among high risk SAs based on results of our study. This may seem in contradiction with prior studies conducted in Europe and Canada, which consistently showed higher ASCVD event rates in SAs compared to NHWs.5,6,27–29 Nevertheless, while SAs migrants included in those studies tended to have low income, low education, and a high burden of cardiovascular risk factors, SAs from MASALA represent a highly educated and high income group consistent with the immigration patterns of SAs in the US compared to Europe and Canada.11
It is therefore possible that MASALA comprised a lower-risk SA subgroup compared to the aforementioned studies. MASALA also excluded SAs with a history of clinical ASCVD and we further excluded those on statins at baseline enriching our study population with healthy SAs. Furthermore, MASALA was initiated 10 years later than MESA, when key prevention programs such as anti-tobacco laws had already been instituted,32 and statin therapies were more commonly prescribed for primary prevention.33,34 The latter is consistent with our finding of a larger proportion of individuals excluded due to baseline statin use in MASALA (30%) than in MESA (12–17%). The combination of these factors may explain the greater similarity between SAs and NHWs when comparing MESA and MASALA than that observed in prior multi-ethnic evaluations.
Study Limitations
Our study has some limitations that are worth discussing. First, the key limitation of our analysis is the lack of longitudinal data for SAs, which precluded performing a formal validation study of the PCE. Nevertheless, CAC is considered a robust predictor of CVD events, and the CAC burden categories used in our analyses (CAC=0 and CAC>100) have shown strong associations with very low and very high ASCVD event rates, respectively.16,18 Therefore, until 10-year follow-up data is available for SAs, our analysis provides valuable preliminary insights on the potential performance that the PCE may have in this important group.
Second, the sample size of the SA population was relatively small, particularly after excluding individuals using statins, which likely limited statistical power. This may be particularly true to low risk SAs who tend to have CAC =0. Nevertheless, we were able to identify statistically significant differences in the intermediate risk stratum, which is indeed the most likely to benefit from further testing using tools such as CAC. Important differences between MESA and MASLA must be acknowledged with direct comparisons between the two cohorts. Despite rigorous adjustment for potential confounders, there remains the possibility for residual confounding. While the high SES among SAs in the MASALA study is consistent with national survey data, it is possible that non-responders or those who declined to participate in the study had lower SES thus potentially limiting generalizability of the study to SAs of lower SES in the US or SA globally.11 Finally, as discussed above, the exclusion of individuals with a history of ASCVD and those taking statins, as well as the 10-year lag between MASALA and MESA initiation may have resulted in a healthy SA population and thus results may not be generalizable to all SAs. However our study population is a true primary prevention cohort in whom ASCVD risk estimation is used to guide the decision to initiate lipid-lowering therapy. 9,23 Therefore, our results may be used to guide clinicians when interpreting risk estimations and prescribing lipid-lowering therapies in this group.
Conclusion
Until prospective information on cardiovascular outcomes becomes available for SA individuals living in the US, understanding the relationship between 10-year cardiovascular risk estimates and CAC burden provides preliminary insights on the potential performance of the PCE in this important racial/ethnic group. Our findings suggest that risk overestimation among low and intermediate-risk SAs may be even greater than among their NHW counterparts. In this context, CAC may be a very valuable tool to help further refine risk estimations in SAs considered at intermediate risk. Validation studies are needed to confirm these preliminary 2 findings.
Supplementary Material
The performance of the pooled cohort equations (PCE) among South Asians (SAs) is uncertain.
In the absence of 10-year follow-up data for ASCVD events, coronary artery calcium (CAC) may be used as a surrogate outcome.
We studied the prevalence of CAC across strata of ASCVD risk in SAs as well as in other 4 races/ethnicities.
There was a higher odds of CAC=0 among low and intermediate risk SAs as compared to NHWs.
The PCE may overestimate risk in low and intermediate risk in SAs living in the US even to a greater extent than in NHWs.
ACKNOWLEDGEMENTS
The authors thank the other investigators, the staff, and the participants of the MASALA and MESA study for their valuable contributions. A full list of participating MASALA investigators and institutions can be found at https://www.masalastudy.org. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org
MESA: This research was supported by contracts HHSN268201500003I, N01-HC95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from NCATS.
FINANCIAL SUPPORT
MASALA: This research was supported by the National Institutes of Health (NIH) grant no.1 R01 HL093009. Data collection at UCSF was also supported by NIH/NCRR UCSF-CTSI Grant Number UL1 RR024131. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
ABBREVIATIONS
- AA
African American
- ACC
American College of Cardiology
- AHA
American Heart Association
- ASCVD
Atherosclerotic Cardiovascular Disease
- CA
Chinese American
- CAC
coronary artery calcium
- CT
computed tomography
- MASALA
Mediators of Atherosclerosis in South Asians Living in America
- MESA
Multi-Ethnic Study of Atherosclerosis
- NHW
non-Hispanic White
- PCE
Pooled Cohort Equations
- SA
South Asian
Footnotes
CONFLICT OF INTEREST
The authors declared they do not have anything to disclose regarding conflict of interest with respect to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hoeffel Elizabeth M.; Rastogi Sonya ; Kim Myoung Ouk; Shahid H The Asian Population: 2010. 2012.
- 2.Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet (London, England) 2000; 356: 279–84. [DOI] [PubMed] [Google Scholar]
- 3.Chambers JC, Eda S, Bassett P, et al. C-reactive protein, insulin resistance, central obesity, and coronary heart disease risk in Indian Asians from the United Kingdom compared with European whites. Circulation 2001; 104: 145–50. [DOI] [PubMed] [Google Scholar]
- 4.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol 2004; 14: 499–506. [DOI] [PubMed] [Google Scholar]
- 5.Khan NA, Grubisic M, Hemmelgarn B, Humphries K, King KM, Quan H. Outcomes After Acute Myocardial Infarction in South Asian, Chinese, and White Patients. Circulation 2010; 122: 1570–7. [DOI] [PubMed] [Google Scholar]
- 6.Toor IS, Jaumdally R, Lip GYH, et al. Differences between South Asians and White Europeans in five year outcome following percutaneous coronary intervention. Int J Clin Pract 2011; 65: 1259–66. [DOI] [PubMed] [Google Scholar]
- 7.Sharma M, Ganguly NK. Premature coronary artery disease in Indians and its associated risk factors. Vasc Health Risk Manag 2005; 1: 217–25. [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res 2006; 124: 235–44. [PubMed] [Google Scholar]
- 9.Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 63: 2935–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Huffman MD, Karmali KN, et al. Estimating Longitudinal Risks and Benefits From Cardiovascular Preventive Therapies Among Medicare Patients: The Million Hearts Longitudinal ASCVD Risk Assessment Tool. Circulation 2016; published online Nov 4. http://circ.ahajournals.org/content/early/2016/11/03/CIR.0000000000000467.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanaya AM, Kandula N, Herrington D, et al. Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study: Objectives, Methods, and Cohort Description. Clin Cardiol 2013; 36: 713–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827–32. [DOI] [PubMed] [Google Scholar]
- 13.Detrano R, Guerci AD, Carr JJ, et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. N Engl J Med 2008; 358: 1336–45. [DOI] [PubMed] [Google Scholar]
- 14.Kavousi M, Elias-Smale S, Rutten JHW, et al. Evaluation of Newer Risk Markers for Coronary Heart Disease Risk Classification. Ann Intern Med 2012; 156: 438. [DOI] [PubMed] [Google Scholar]
- 15.Yeboah J, Young R, McClelland RL, et al. Utility of Nontraditional Risk Markers in Atherosclerotic Cardiovascular Disease Risk Assessment. J Am Coll Cardiol 2016; 67: 139–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin SS, Blaha MJ, Blankstein R, et al. Dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation 2014; 129: 77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kandula NR, Kanaya AM, Liu K, et al. Association of 10-Year and Lifetime Predicted Cardiovascular Disease Risk With Subclinical Atherosclerosis in South Asians: Findings From the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J Am Heart Assoc 2014; 3: e001117–e001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blaha MJ, Blumenthal RS, Budoff MJ, Nasir K. Understanding the utility of zero coronary calcium as a prognostic test: a Bayesian approach. Circ Cardiovasc Qual Outcomes 2011; 4: 253–6. [DOI] [PubMed] [Google Scholar]
- 19.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol 2002; 156: 871–81. [DOI] [PubMed] [Google Scholar]
- 20.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002; 156: 871–81. [DOI] [PubMed] [Google Scholar]
- 21.Kanaya AM, Kandula NR, Ewing SK, et al. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: The MASALA and MESA studies. Atherosclerosis 2014; 234: 102–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McEvoy JW, Martin SS, Dardari ZA, et al. Coronary Artery Calcium to Guide a Personalized Risk-Based Approach to Initiation and Intensification of Antihypertensive Therapy. Circulation 2017; 135: 153–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stone NJ, Robinson J, Lichtenstein AH, et al. 2013. ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; published online Nov 7. DOI:10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Cook NR, Ridker PM. Further Insight Into the Cardiovascular Risk Calculator. JAMA Intern Med 2014; 174: 1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeFilippis AP, Young R, Carrubba CJ, et al. An Analysis of Calibration and Discrimination Among Multiple Cardiovascular Risk Scores in a Modern Multiethnic Cohort. Ann Intern Med 2015; 162: 266–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet 2013; 382: 1762–5. [DOI] [PubMed] [Google Scholar]
- 27.Hajra A, Li Y, Siu S, et al. Risk of Coronary Disease in the South Asian American Population. J Am Coll Cardiol 2013; 62: 644–5. [DOI] [PubMed] [Google Scholar]
- 28.Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia 2006; 49: 2580–8. [DOI] [PubMed] [Google Scholar]
- 29.Lee J, Heng D, Chia KS, Chew SK, Tan BY, Hughes K. Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore Cardiovascular Cohort Study. Int J Epidemiol 2001; 30: 983–8. [DOI] [PubMed] [Google Scholar]
- 30.Patel J, Al Rifai M, Cainzos-Achirica M, et al. Family History of CHD Is Associated With Severe CAC in South Asians. JACC Cardiovasc Imaging 2017; 10: 958–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain P, Kooner JS, Raval U, Lahiri A. Prevalence of coronary artery calcium scores and silent myocardial ischaemia was similar in Indian Asians and European whites in a crosssectional study of asymptomatic subjects from a UK population (LOLIPOP-IPC). J Nucl Cardiol 2011; 18: 435–42. [DOI] [PubMed] [Google Scholar]
- 32.U.S Food and Drug Administration. Rules, Regulations & Guidance - Family Smoking Prevention and Tobacco Control Act - An Overview. https://www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm246129.htm (accessed April 1, 2018).
- 33.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–97. [DOI] [PubMed] [Google Scholar]
- 34.Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010; 122: 2748–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.