Abstract
Objectives:
To evaluate kidney stone patients’ interest in lifestyle behavior modification and a variety of mobile health (mHealth) technologies to improve adherence to fluid consumption recommendations for the prevention of nephrolithiasis. Of particular interest was the acceptability of various intervention components for the design of a stone-specific mHealth technology.
Materials and Methods:
Using a cross-sectional design, adult patients with a diagnosis of kidney stones (N = 94) were recruited from outpatient clinics to complete a three-part questionnaire.
Results:
Patients reported being willing to make lifestyle changes to prevent kidney stones (97%). The majority of the patients recalled the recommendation to increase fluid intake (93%) but few monitored their daily fluid intake (30%). Most patients had never installed an app (95%) or owned a device (100%) to help with increasing fluid consumption, but believed an app or device could improve their adherence (72%) and would be interested in using an app or device (86%). The mHealth intervention components most widely perceived as useful included automated lapse detection with notifications, educational materials, self-monitoring tools, scheduler with prompts/reminders/notifications, connected water bottles and text message reminders to drink.
Conclusions:
Patients are interested in lifestyle behavior change to prevent stones but technology has not been widely adopted to improve adherence to fluid intake recommendations for stone prevention. This study identified a number of viable mHealth intervention components that should be considered when designing a stone-specific mHealth technology to support adherence to increased fluid consumption recommendations.
Keywords: Kidney stones, Fluid Consumption, Technology, Mobile Health
Introduction:
Nephrolithiasis affects an estimated 8.8% of American adults with annual medical care costs in the United States exceeding $2 billion.1,2 Recurrence rates are as high as 80% within 10 years.3 Prevention requires long-term lifestyle changes and commitment, often in the absence of immediate rewards or reinforcements to indicate that one is succeeding.4 The American Urological Association recommends increasing fluid consumption to produce at least 2.5L of urine daily and this strategy is well established as effective for the prevention of all kidney stone compositions.5–11 Unfortunately, adherence with this simple and inexpensive recommendation is commonly below 50%.12, 13
Adherence to lifestyle behavior change in daily life can be challenging for patients. The use of mobile health (mHealth) technology offers a new opportunity to support adherence to preventive strategies within the context of daily life.14 Such technology, combined with behavioral science principles, has been used to support a variety of lifestyle behavior changes, such as smoking cessation, physical activity, and diet modification.15, 16 Technology can also be used to support patients with nephrolithiasis, but any mHealth interventions must be acceptable to patients for long-term feasibility and maintenance.17, 18 With the current gap in efficacious stone-specific mHealth technology for increasing fluid consumption, an opportunity exists to co-design a multicomponent intervention with patients. The acceptability of intervention components to patients is a prerequisite for their engagement with a behavioral intervention so co-design should increase intervention feasibility for subsequent efficacy trials and clinical use.19
The purpose of this study was to begin that design process by evaluating kidney stone patients’ interest in lifestyle behavior modification and a variety of mHealth technologies for increasing fluid consumption to prevent the recurrence of nephrolithiasis. Of particular interest was the acceptability of various mHealth intervention components to support adherence to fluid consumption recommendations and whether perceived usefulness varies as a function of age or sex.
Materials and Methods:
After obtaining approval from our institutional review board, adult patients with a history of nephrolithiasis were recruited during outpatient clinic visits from October 2016 to February 2017. Patients were excluded if they were under the age of 18 or cognitively impaired. A total of 110 patients consented to participate and 94 completed the questionnaire (85%) in a cross-sectional design.
Patients completed a three-part questionnaire, either on paper in clinic or electronically with the web-based questionnaire service Qualtrics. In section 1 (patient characteristics), patients reported their demographic characteristics (age, sex, race, ethnicity, height, weight, employment status, education) and stone history, including the time since their first stone (years), time since their most recent stone (years), number of lifetime stone episodes, number of surgical interventions for a stone, current stone status, and pain intensity during the most recent episode.
In section 2 (prevention motivation), patients rated their willingness to make lifestyle changes to prevent kidney stones on a scale ranging from 1 (not at all willing) to 5 (very willing). Participants were asked which of the following recommendations they received to prevent a stone recurrence: increase fluid intake, change diet, lose weight, take medication, and parathyroid surgery (response options: yes, no, unsure). Participants reported whether they kept track of their daily fluid consumption (response options: yes, no, unsure) and the number of days/week that they typically adhered to fluid consumption recommendations. They also reported how frequently they complied with four prevention guidelines (increase fluid intake, change diet, lose weight, take medication) using response options that included 1 (never), 2 (sometimes), 3 (about half the time), 4 (most of the time), and 5 (always). Next, patients ranked a set of factors in the order that they interfered with their ability to meet fluid consumption recommendations. Reasons included not being thirsty, not having water with them, forgetting to drink, losing track of time, not being motivated to drink, and other (with an option to describe any other reason). Participants also had the option of answering that none of the remaining factors affected their ability to meet fluid consumption recommendations.
In section 3 (mHealth technology), patients were asked if they owned a smartphone or tablet computer (response options: yes, no, unsure). Patients who owned smartphones or tablet computers were asked (a) if they had ever installed an app to prevent recurrence of kidney stones,(b) if they had ever installed an app to help increase their fluid consumption, and (c) if they ever owned a connected water bottle that tracked or provided reminders about fluid consumption (response options: yes, no, unsure). All patients were asked to indicate their interest in using a new smartphone application or device to aid in complying with fluid consumption recommendations to prevent kidney stones on a scale ranging from 1 (not at all interested) to 5 (very interested). They also indicated how likely they thought they were to use a smartphone application or device on a regular basis to help them comply with behavioral recommendations to prevent kidney stones. The response scale included 1 (not at all), 2 (a little likely), 3 (somewhat likely), 4 (mostly likely), and 5 (very likely). Finally, patients rated the perceived utility of possible components of an intervention for increasing fluid consumption (listed in Table 2). Each intervention component was described in case patients were not familiar with it. For example, automated lapse detection was described as “automated notification triggered by technology that detected a lapse in preventive behavior (e.g., not drinking enough)”. Online intervention was described as an online community or forum for patients to share stories, advice, etc. Lapse-contingent calls from clinic were described as a call from clinic triggered by technology that detected a lapse in preventive behavior. Social media intervention was described as use of social media connections for support (e.g. Twitter, Facebook groups).
Table 2.
Perceived usefulness of intervention components to increase fluid consumption: Sex, age, and BMI-related differences
| Classificatio n |
Odds Ratios (95% CI) |
|||||
|---|---|---|---|---|---|---|
| Usefu l (%) |
Nagelkerk e R2 |
Accuracy (%) |
Sex | Age | BMI | |
| Automated lapse detection and notification |
79.5 | .07 | 79.5 | 0.80 (0.26− 2.46) |
0.97 (0.93 − 1.01) |
0.97 (0.91 − 1.04) |
| Educational materials | 75.3 | .14 | 76.5 | 0.25* (0.08− 0.73) |
1.02 (0.98 − 1.06) |
0.98 (0.92 − 1.05) |
| Self-monitoring tools | 75.3 | .08 | 75.3 | 0.33 (0.12− 0.94) |
1.00 (0.97 − 1.04) |
0.98 (0.92 − 1.04) |
| Scheduler with prompts/reminders/notificatio ns |
69.5 | .22 | 73.2 | 0.22* (0.08− 0.63) |
0.96 (0.92 − 1.00) |
0.98 (0.92 − 1.04) |
| Connected water bottle | 66.7 | .27 | 71.4 | 0.31 (0.11− 0.89) |
0.94* (0.91 − 0.98) |
0.94 (0.88 − 1.00) |
| Text message reminders | 64.7 | .08 | 65.9 | 0.45 (0.18− 1.12) |
0.98 (0.94 − 1.01) |
1.01 (0.95 − 1.06) |
| Online patient community/forum |
43.5 | .17 | 68.2 | 0.28* (0.11− 0.70) |
0.98 (0.95 − 1.01) |
1.04 (0.98 − 1.10) |
| Lapse-contingent calls from clinic |
41.5 | .10 | 59.8 | 0.33 (0.13− 0.84) |
1.00 (0.97 − 1.03) |
0.98 (0.92 − 1.03) |
| Social media | 32.1 | .33 | 74.1 | 0.10** (0.03− 0.34) |
0.97 (0.94 − 1.01) |
1.05 (0.98 − 1.12) |
| Telephone coaching | 22.8 | .06 | 77.2 | 0.47 (0.16− 1.43) |
1.00 (0.96 − 1.04) |
0.96 (0.89 − 1.03) |
p < .01
p < .05 (all values adjusted for multiple tests)
Descriptive statistics were calculated using IBM SPSS 24.0. Categorical variables were described by their frequencies, and continuous variables were described by their mean, standard deviation, median and range. Pearson correlation coefficients were calculated to estimate bivariate associations between variables. Multiple logistic and linear regression models were estimated to evaluate factors that influenced perceptions of intervention utility and the likelihood of using each mHealth technology. For the logistic regression models, the Nagelkerke R2 was reported to describe the extent to which the predictor variables improved model fit, and classification accuracy was reported to describe the proportion of the sample that would be accurately classified by the regression model (= [true positives + true negatives] / [ true positives + true negatives + false positives + false negatives]). A p value (adjusted for the number of predictors in each regression model to limit bias) less than .05 was considered to be statistically significant.
Results:
There were a total of 94 patients (53% female) with an average age of 51.8±13.9 years (range 19–77). They were almost exclusively white (96%) and not Hispanic or Latino (99%). As shown in Table 1, most of the sample population was overweight, full-time employed, and at least high school educated. Many patients (63%) believed they currently had kidney stones at the time of the questionnaire with 88% reporting a symptomatic stone episode within the past year. Most participants had undergone at least one surgery to treat a stone (77%), with 48% having had multiple surgeries.
Table 1.
Patient Demographics and Stone-Specific Characteristics
| n (%) | |
|---|---|
| Sex | |
| Female | 50 (53%) |
| Male | 44 (47%) |
| Weight | |
| Obese | 46 (49%) |
| Overweight | 29 (31%) |
| Normal weight | 17 (18%) |
| Underweight | 1 (1%) |
| Employment Status | |
| Full-time | 52 (55%) |
| Retired | 23 (25%) |
| Part-time | 11 (12%) |
| Unemployed | 7 (7%) |
| Prefer not to answer | 1 (1%) |
| Education | |
| Less than HS diploma | 3 (3%) |
| HS diploma | 23 (25%) |
| Some college | 20 (21%) |
| Associate’s degree | 10 (11%) |
| Bachelor’s degree | 18 (19%) |
| Master’s degree | 13 (14%) |
| Doctoral or professional degree | 7 (8%) |
| Stone Characteristics |
|
| Time since first stone episode (years) | 8.1±5.9 (Mdn = 8) |
| Time since recent stone episode (years) |
1.0±1.7 (Mdn = 0.5) |
| Number stone episodes | 10.8±18.6 (Mdn = 4) |
| Number surgical interventions | 3.24±8.57 (Mdn = 1) |
| Currently have stones, n (%) | 59 (63%) |
Patients were receptive to kidney stone prevention, with almost all participants mostly (15%) or very interested (77%) in preventing another kidney stone. The majority were mostly (40%) or very willing (44%) to make lifestyle changes to prevent another stone episode. Patients were able to recall the following stone prevention recommendations, including: increase their fluid intake (93%) modify their diet (65%), taking a medication (33%), losing weight (26%), or having parathyroid surgery (12%). Age, sex, number of stone episodes, pain severity, number of surgical interventions and presence of a current stone did not correlate with patient’s interest in lifestyle modification to prevent another stone (p > .05).
The majority of patients recalled the recommendation to increase fluid intake for stone prevention (93%). Only 30% currently monitored their daily fluid intake, yet participants believed they adhered to daily fluid consumption recommendations on 4.3 days/week (SD = 2.4, Mdn = 5). Approximately 85% believed that they adhered to increased fluid intake recommendations at least half of the time. In contrast, only 56% believed they adhered to diet recommendations, 48% believed they adhered to weight loss recommendations, and 58% believed they adhered to medication recommendations. Figure 1 presents patients’ rankings of reasons for not drinking enough fluids. Not feeling thirsty, forgetting to drink, and losing track of time were consistently ranked as top reasons for not drinking.
Figure 1.
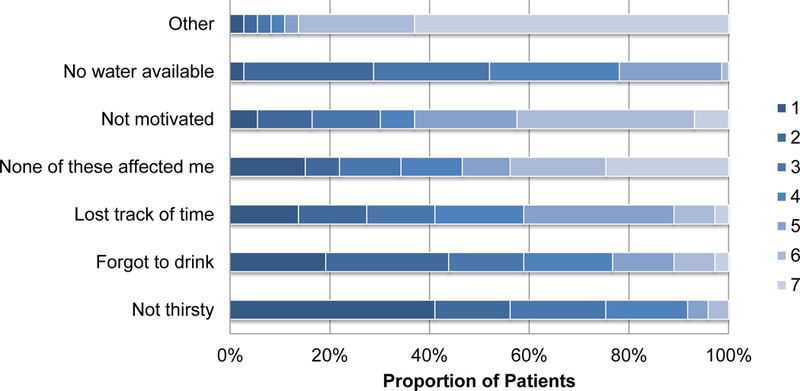
Rankings of barriers for not complying with fluid recommendations.
The majority of participants owned smartphones or tablet devices (85%). Among those participants, very few had ever installed an app to help prevent kidney stones (3%) or to increase fluid consumption (5%). None of the participants owned a connected water bottle or other digital devices to support fluid consumption. Despite this limited experience, the majority of participants (88%) were at least a little interested in using mHealth technology to increase their fluid consumption. Patients generally (72%) believed that an app or connected water bottle would be at least slightly likely to increase their fluid consumption. Most patients (76%) believed they were at least somewhat likely to use an app or device to aid with adherence to guidelines for preventing kidney stones. The expected likelihood of using mHealth technology to prevent the recurrence of kidney stones was regressed on age, sex, and BMI, F(3,87) = 2.79, p < .05, R2 = .09. After adjusting for multiple tests, none of these predictors were significantly associated with the expected likelihood of using an app or device.
Table 2 summarizes the proportion of participants who rated possible intervention components as useful for increasing fluid consumption. The components most widely perceived as useful included automated lapse detection with notifications, educational materials, self-monitoring tools, scheduler with prompts/reminders/notifications, connected water bottles, and text message reminders to drink.
A series of logistic regression models were estimated to evaluate whether perceived usefulness varied as a function of sex, age, or BMI. As seen in Table 2, women were more likely than men to rate educational materials, schedulers with prompts/reminders/notifications, online patient communities/ forums, and social media as being useful. Younger patients were more likely to rate the connected water bottle as useful. BMI was not associated with the perceived utility of any mHealth intervention features.
Discussion:
Patients who have experienced a kidney stone almost uniformly report a desire to prevent a recurrence and a willingness to modify their lifestyle to prevent another stone from forming. Increasing fluid intake was the lifestyle behavior change that almost all patients were able to recall and willing to perform. This result corroborates findings from McCauley et al. who found that patients were more willing to increase fluid intake over dietary or medication therapy.20 Increasing fluid intake is also the least expensive intervention, and has been shown to be a cost-effective prevention strategy.21
Although most patients know that increasing fluid intake reduces the recurrence of stone disease and are motivated to make lifestyle behavior changes, adherence with these recommendations remains poor. Khambati et al. reported only 50% adherence to fluid intake recommendations.13 In our study, patients self-reported adherence on average 4.3 days per week, however only one-third monitored their fluid intake on a daily basis. Common barriers to meeting fluid intake guidelines included: not feeling thirsty, forgetting to drink, and losing track of time. These barriers aligned with the three stages of barriers previously identified by McCauley and colleagues: (1) not knowing the benefits of fluid or not remembering to drink, (2) disliking the taste of water, lack of thirst, and lack of availability, and (3) need to void frequently and related issues at work or school.20
These findings highlighted the need for new tools to address disease-specific barriers and improve adherence to fluid intake recommendations. Technology has created new opportunities to promote behavior change in the natural context of patients’ daily lives. For example, behavior change techniques can be implemented in smartphone apps to support self-monitoring, goal setting, and prompt drinking behavior.17 These apps can also be paired with connected devices, such as water bottles, to track and provide regular feedback on fluid intake.22 In the general population, 58% of smartphone users (estimated at 77% of American adults) had downloaded an mHealth app to support healthy behaviors.23, 24 Yet few patients in our cohort reported ever installing an app to help prevent kidney stones or to increase fluid consumption and none reported owning a connected water bottle or other digital device to support prevention goals. Despite this limited experience, the majority of participants expressed interest in using mHealth technology to achieve their fluid intake goals and generally believed that mHealth technology would improve their fluid consumption. These findings reinforced proposals to develop mHealth interventions to prevent the recurrence of stones.18 They also highlighted the need to raise patients’ awareness of existing digital tools they can use to support adherence to fluid consumption guidelines.
This study also identified a number of acceptable intervention components to support adherence to fluid consumption recommendations. These components included automated lapse detection with notifications, educational materials, self-monitoring tools, scheduler with prompts/reminders/notifications, connected water bottles, and text message reminders to drink. Although little is known about the efficacy of any of these individual components on increasing fluid consumption, the difficulty of changing lifestyle behaviors suggests that a multicomponent intervention strategy may be needed. For instance, prior research on dietary intervention for weight loss has been found to be more effective when they include techniques based on control theory (e.g., goal setting, self-monitoring of behavior, behavioral feedback on discrepancy between behavior and goals). 25 Technology can be used to facilitate the delivery and implementation of evidence-based behavior change techniques but it is important that the techniques themselves be evidence-based. Behavioral science theories of adherence should also be considered to ensure that the techniques are implemented in a sustainable way for long-term behavior change. Fluid consumption interventions must yield sustained effects to produce their intended clinical impact on stone prevention. Of course, every component adds expense for payers and burden for patients without any guarantee that the component increases the effect for the treatment.26 Thus, it would be helpful to screen individual components to estimate their effects (both with and without other components) on engagement, hydration, and recurrence before implementing a potentially expensive and burdensome multi-component treatment.27 Participant engagement is especially important to consider in this decision-making process because the disengagement undermines the cost effectiveness of any intervention.21
Some sub-populations accepted mHealth intervention components more readily than others. Female patients and, to a much lesser degree, younger patients appear to be especially open to mHealth interventions and could be targeted in a future trial.28 Patient BMI did not impact perceptions of acceptability which was surprising given popular beliefs that increasing fluid consumption can promote satiety and facilitate successful weight management.29, 30 Incorporating components that address patient-identified barriers to adherence and are acceptable to patients will increase the feasibility of future clinical trials using mHealth tools for promoting fluid consumption.19
This study was based on a relatively homogeneous sample of patients from central Pennsylvania. Conclusions may not generalize to populations with greater racial, ethnic, socioeconomic, educational or geographic diversity. All patients in this study were receiving care at a tertiary center so findings may not generalize to those receiving care in other healthcare settings. The sample in this study had a higher education level than the general population with only 3% having less than a high school diploma so findings may not generalize to those with less education. All data were obtained from patient’s self-reports and responses about acceptability may not predict actual adoption and engagement. Data were cross-sectional and do not indicate how perceptions about intervention acceptability might change over time.
Conclusions:
Patients are interested in making lifestyle behavior changes to prevent kidney stones. Increasing fluid consumption is a well-known and accepted prevention strategy but few patients currently make consistent efforts to monitor their fluid intake. Patients with nephrolithiasis have largely adopted smartphones or tablet computers but few have enlisted this technology in disease management. In light of evidence that thirst and memory are insufficient for increasing fluid consumption, mobile technology provides new opportunities to support patients’ adherence to prevention guidelines. This study identified a number of viable intervention components that should be considered when designing a disease-specific mHealth intervention to support adherence to increased fluid consumption recommendations. Designing interventions with components that patients accept will increase the feasibility of implementing and evaluating the effects of that intervention on patient health outcomes.
Acknowledgements:
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR000127 and TR002014. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Scales CD, Smith AC, Hanley JM, et al. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol 2012; 62:160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America Project: urolithiasis. J Urol 2005; 173: 848–857. [DOI] [PubMed] [Google Scholar]
- 3.Sutherland JW, Parks JH, Coe FL. Recurrence after a single renal stone in a community practice. Miner Electrolyte Metab 1985; 11: 267. [PubMed] [Google Scholar]
- 4.Fineberg HV. The paradox of disease prevention: celebrated in principle, resisted in practice. JAMA 2013; 310: 85–90. [DOI] [PubMed] [Google Scholar]
- 5.Pearle MS, Goldfarb DS, Assimos DG, et al. Medical management of kidney stones: AUA guideline. J Urol 2014; 192: 316–324. [DOI] [PubMed] [Google Scholar]
- 6.Cheungpasitporn W, Rossetti S, Friend K, et al. Treatment effect, adherence, and safety of high fluid intake for the prevention of incident and recurrent kidney stones: a systematic review and meta-analysis. J Nephrol 2016; 29: 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siener R, Hesse A. Fluid intake and epidemiology of urolithiasis. Eur J Clin Nutr 2003; 57: S47–S51. [DOI] [PubMed] [Google Scholar]
- 8.Borghi L, Meschi T, Amato F, et al. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol 1996; 155: 839–843. [PubMed] [Google Scholar]
- 9.Fink HA, Akornor JW, Garimella PS, et al. Diet, fluid or supplements for secondary prevention of nephrolithiasis: a systematic review and meta-analysis of randomized trials. European Urology 2009. July; 56: 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor EN, Curhan GC. Diet and fluid prescription in stone disease. Kidney Int 2006; 70:835–9. [DOI] [PubMed] [Google Scholar]
- 11.Pak CYC, Sakhaee K, Crowther C, et al. Evidence justifying a high fluid intake in treatment of nephrolithiasis. Ann Intern Med 1980; 93: 36–39. [DOI] [PubMed] [Google Scholar]
- 12.Van Drongelen J, Kiemeney LA, Debruyne FM, et al. Impact of urometabolic evaluation on prevention of urolithiasis: A retrospective study. Urology 1998; 52: 384–391. [DOI] [PubMed] [Google Scholar]
- 13.Khambati A, Matulewicz RS, Perry KT, et al. Factors associated with compliance to increased fluid intake and urine volume following dietary counseling in first-time kidney stone patients. J Endourol 2017; 31: 605–610. [DOI] [PubMed] [Google Scholar]
- 14.Spring B, Gotsis M, Paiva A, et al. Healthy apps: mobile devices for continuous monitoring and intervention. IEEE Pulse 2013; 4: 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pagoto S, Bennett GG. How behavioral science can advance digital health. Transl Behav Med 2013; 3: 271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar S, Nilsen WJ, Abernethy A, et al. Mobile health technology evaluation: the mHealth evidence workshop. Am J Prev Med 2013; 45: 228–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conroy DE, Dubansky A, Remillard J, et al. Evaluation of behavior change techniques in commercially-available mobile applications to promote fluid consumption in patients with urolithiasis. Urology 2017; 99: 33–37. [DOI] [PubMed] [Google Scholar]
- 18.Kok DJ. The preventive treatment of recurrent stone-formation: How can we improve compliance in the treatment of patients with recurrent stone disease? Urolithiasis 2016; 44: 83–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med 2009; 36: 452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCauley LR, Dyer AJ, Stern K, et al. Factors influencing fluid intake behavior among kidney stone formers. J Urol 2012; 187: 1282–1286. [DOI] [PubMed] [Google Scholar]
- 21.Lotan Y, Jimenez IB, Lenoir-Wijnkoop I, et al. Increased water intake as a prevention strategy for recurrent urolithiasis: major impact of compliance on cost-effectiveness. J Urol 2013; 189: 935–939. [DOI] [PubMed] [Google Scholar]
- 22.Borofsky MS, Dauw CA, York N, et al. Accuracy of daily fluid intake measurements using a “smart” water bottle. Urolithiasis 2017: https://doi.org/10.1007/s00240-017-1006-x. [DOI] [PubMed]
- 23.Krebs P, Duncan DT. Health App Use Among US Mobile Phone Owners: A National Survey. JMIR Mhealth Uhealth 2015; 3 (4): e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pew Research Center. Mobile Fact Sheet; 2018.
- 25.Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009; 28(6):690–701. [DOI] [PubMed] [Google Scholar]
- 26.Collins LM, Kugler KC, Gwadz MV. Optimization of multicomponent behavioral and biobehavioral interventions for the prevention and treatment of HIV/AIDS. AIDS Behav 2016; 20: S197–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Collins LM, Murphy SA, Nair VN, et al. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med 2005; 30: 65–73. [DOI] [PubMed] [Google Scholar]
- 28.Kreuter MW, Skinner CS. Tailoring: what’s in a name? Health Education Research 2000; 15: 1–4. [DOI] [PubMed] [Google Scholar]
- 29.An R, McCaffrey J. Plain water consumption in relation to energy intake and diet quality among US adults, 2005–2012. J Hum Nutr Diet 2016; 29: 624–32. [DOI] [PubMed] [Google Scholar]
- 30.Dennis EA, Flack KD, Davy BM. Beverage consumption and adult weight management: A review. Eat Behav 2009; 10: 237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]


