Abstract
There is a need to investigate which health information sources are used and trusted by people with limited health literacy to help identify strategies for addressing knowledge gaps that can contribute to preventable illness. We examined whether health literacy was associated with people’s use of and trust in a range of potential health information sources. Six hundred participants from a GfK Internet survey panel completed an online survey. We assessed health literacy using the Newest Vital Sign, the sources participants used to get health information, and the extent to which participants trusted health information from these sources. We performed multivariable regressions, controlling for demographic characteristics. Lower health literacy was associated with lower odds of using medical websites for health information and with higher odds of using television, social media, and blogs or celebrity webpages. People with lower health literacy were less likely to trust health information from specialist doctors and dentists, but more likely to trust television, social media, blogs/celebrity webpages, friends, and pharmaceutical companies. People with limited health literacy had higher rates of using and trusting sources such as social media and blogs, which might contain lower quality health information compared to information from healthcare professionals. Thus, it might be necessary to enhance the public’s ability to evaluate the quality of health information sources. The results of this study could be used to improve the reach of high quality health information among people with limited health literacy and thereby increase the effectiveness of health communication programs and campaigns.
Keywords: health literacy, health information source, use, trust
Introduction
Seeking, understanding, and using health information is critical to health decision making. Information about health problems, self-care, and illness prevention can increase understanding of personal risk factors and preventive strategies, and thereby help individuals improve their health outcomes (Brashers, Goldsmith, & Hsieh, 2002; Benigeri & Pluye, 2003). Health information also helps patients understand their diagnosis, decide on treatments, predict their prognosis (Brashers et al., 2002), and cope with illness (Lambert & Loiselle, 2007). With this in mind, health professionals develop interventions and campaigns to modify attitudes, increase service use, and promote health behaviors (Poínhos et al., 2017; Geana, Greiner, Cully, Talawyma, & Daley, 2012). However, people with limited health literacy benefit less from the available health information (Kandula et al., 2009).
The Institute of Medicine (2004) defines health literacy as the ability to “obtain, process, and understand basic health information and services needed to make appropriate health decisions” (p. 32). Approximately 36% of U.S. adults (77 million people) have basic or below basic health literacy (U.S. Department of Health and Human Services, 2008). Having adequate health literacy means, in part, being able to apply health literacy skills to health-related materials such as prescriptions, appointment cards, and medicine labels (Parker, Baker, Williams, & Nurss, 1995). Compared to individuals with adequate health literacy, people with limited health literacy have more difficulty understanding and applying health information (Geana et al., 2012), with negative consequences for their health (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). For example, those with limited health literacy have worse self-perceived health status (Toci et al., 2014) and higher rates of hospitalization and death (Wu et al., 2013). Limited health literacy is also a barrier to the success of health education programs and health communication campaigns (Livaudais-Toman, Burke, Napoles, & Kaplan, 2014).
Most theoretical frameworks for understanding health literacy identify the process of using information as a key component of health literacy and posit that compared to people with adequate health literacy, people with limited health literacy have more barriers in using accurate health information (Institute of Medicine, 2004; Baker, 2006; Manganello, 2008; Nutbeam, 2008; Sørensen et al., 2012; Squiers, Peinado, Berkman, Boudewyns, & McCormack, 2012). Sørensen and colleagues’ (2012) integrated model of health literacy illustrates the proximal and distal factors influencing health literacy and the pathways linking health literacy to health outcomes. One of the four core competencies that they theorize contribute to health literacy is the ability to access health information (seeking, finding, and obtaining health information); the other competencies are understanding, applying, and appraising health information. The Health Literacy Skills (HLS) conceptual framework also integrates theoretical and empirical work identifying determinants, mediators and outcomes of health literacy. It too identifies information seeking skills, including Internet-navigation skills and print literacy as crucial components of health literacy. The extent to which people lack these skills interacts with the health literacy demand of the source, or how difficult it is to use and understand the information source to predict message comprehension (Squiers et al., 2012). In sum, information seeking behavior, including the skills that enable people to find and select the most relevant and highest quality information sources are thought to be central to the processes by which health literacy affects health outcomes.
While limited primarily to convenience samples, empirical research supports the notion that health literacy is related to information source use. Having lower health literacy has been associated with less use of Internet for health information among specific sub-populations such as older adults, parents of children with health conditions, adolescents, pregnant women, and African Americans (Cutilli, Simko, Colbert, & Bennett, 2018; Sheng & Simpson, 2013; Fagnano et al., 2012; Knapp et al., 2010; Shieh et al., 2009; Ghaddar, Valerio, Garcia, & Hansen, 2012; McCleary-Jones et al., 2013). Previous studies have also explored sources other than the Internet to examine the relationship between health literacy and source use. Lower health literacy correlates with less use of doctors/healthcare providers, books, newspapers, magazines, family, and friends, but more use of television and radio for health information (Koo, Krass, & Aslani, 2006; Zoellner, Connell, Bounds, Crook, & Yadrick, 2009; Fagnano et al., 2012; Cutilli et al., 2018; Weiss, Reed, & Kligman, 1995; Kutner, Greenburg, Jin, & Paulsen, 2006). While the patterns of results have varied to some degree across samples, findings indicate that people with limited health literacy appear to be not using health information as widely as their higher literacy counterparts, perhaps preferring non-print sources. In order to develop health messages that reach people with lower health literacy, it would be helpful to better understand which sources these individuals are most likely to use and trust.
The goal of the present research is to better understand the patterns of information source use and trust among people with different levels of health literacy. This will provide insight into the real-world consequences of limited health literacy on information source access. It will also contribute to developing theory by helping generate hypotheses about which aspects of the media environment interact with limited health literacy to impact information seeking and health knowledge. It will help practitioners ‘meet people where they are at’ by delivering health messages through sources that are used most frequently by people with limited health literacy, as well as increasing the acceptance of high quality sources to reach this population. Finally, to improve information use from these sources, it would be useful to understand barriers people with lower health literacy face in using sources that are more commonly used by their counterparts with higher literacy. Lack of trust in a source may be such a barrier.
Both theory and empirical research have focused on trust as a barrier to message use, integration, or acceptance rather than source access. Trust is a mediator between health literacy and health outcomes in the HLS (Squiers et al., 2012). Empirical work demonstrates that people tend to shape their attitudes, beliefs, and behaviors based on health information from the sources they trust (Clayman, Manganello, Viswanath, Hesse, & Arora, 2010). Not many studies have explored the associations between health literacy and people’s levels of trust in health information sources; however, those that have indicate that trust in health information sources may vary by a person’s health literacy level (Fagnano, Halterman, Conn, & Shone, 2012; Lubetkin, Zabor, Isaac, Brennessel, Kemeny, & Hay, 2015; Paige, Krieger, & Stellefson, 2017). Previous studies show that trust in Internet sources is associated with greater use of those sources (Lemire, Paré, Sicotte, & Harvey, 2008; Lee, Yang, & Tsai, 2012; Sheng & Simpson, 2015). Trust may also be a mediator of the relationship between health literacy and choice of health information sources.
Study Purpose and Research Questions
Although prior research shows that health literacy is associated with use of health information sources, few studies have examined the relationship between health literacy and use of and trust in health information sources with a nationally representative sample, included a broad array of sources, or differentiated among the wide variety of Internet sources. This paper fills these gaps. Specifically, we tested the associations between people’s health literacy and their use of and trust in various sources and examined whether health literacy was indirectly associated with use of a given source through trust in that source. The results of this study could be used to improve the reach of health information among people with limited health literacy and thereby increase the effectiveness of health communication programs and campaigns. Based on the literature above, we proposed the following research questions:
Do people’s use of health information sources differ based on their health literacy levels?
Do people’s trust in health information sources differ based on their health literacy levels?
Is health literacy indirectly associated with use of a given source through trust in that source?
Methods
Participants
Data for the present analyses were from a larger study designed to examine differences in health information seeking behavior between rural and metropolitan residents. Because this paper does not focus on comparing rural and metropolitan populations, the design of the main study is described briefly. Recruitment and data collection were conducted by GfK (formerly Knowledge Networks) from February to April 2017. GfK maintains a standing representative panel of 55,000 individuals. These individuals were invited into the panel by post mail invitations. GfK provides Internet-enabled devices if needed. GfK sent email invitations to 1066 KnowledgePanel members; 618 (57.9%) completed the survey. Responses for 18 participants were dropped because they met two or more of the following criteria for inattentive responding: (1) completed the survey in less than 8 minutes (median time to completion was 32 minutes), (2) marked identical responses on more than 4 grids that contained one or more items that were worded in the direction opposite to the others, (3) failed on both of the survey validation items (asking participants to select “somewhat agree” for one item and “somewhat disagree” for the other item), and (4) gave different answers to a repeated factual question. Thus, we included a final sample of 600 participants in our data analyses. The study was approved by the University at Buffalo’s Institutional Review Board.
Measures
Health Literacy
We administered the Newest Vital Sign (NVS) to assess participants’ health literacy (Weiss et al., 2005). We selected NVS as our health literacy measure because it is an objective (i.e. a test with questions that have a single correct answer) rather than subjective (i.e., a self-reported survey) assessment (Weiss et al., 2005). The latter are not an accurate assessment of people’s true ability to understand and apply health information (Logan & Siegel, 2017). The NVS is shown to yield reliable and valid scores among global populations across age, race/ethnicity, and health conditions (Shealy & Threatt, 2016). In addition, compared to other commonly used health literacy instrument such as the Test of Functional Health Literacy in Adults (TOFHLA) and the Rapid Estimate of Adult Literacy in Medicine (REALM), the NVS has a higher feasibility to adapt in our online survey. The NVS can be administered much more quickly than TOFHLA (Weiss et al., 2005). The REALM is based on word pronunciation so it could not be adapted to an online survey format. Moreover, the NVS is a reliable and accurate measure of health literacy with high sensitivity (more sensitive than the TOFHLA) for detecting individuals with limited health literacy (Weiss et al., 2005). The NVS contains a mock-up of an ice-cream nutrition label and asks participants six open-ended questions based on the information on the label. Answers to each answer were scored as correct (coded as 1) or incorrect (including missing items; coded as 0), yielding a score from 0 to 6. Higher health literacy scores indicate higher health literacy levels.
Information Use and Trust
We examined participants’ self-reported use of 25 different health information sources (see Table 1 for a complete list) with the question, “Do you get health information from the following sources? [Yes/No].” We assessed the extent to which they trusted the health information from each source with the question, “How much do you trust health information from the following sources? [Not at all, Some, Quite a bit, A great deal].” We created the list of 25 health information sources and the measures of use of and trust in these sources; the list was adapted from the Health Information National Trends Survey (National Cancer Institute, 2017) and the Pew Research Center (2008, 2013). Some sources (e.g., newspapers, magazines) are accessible both online and in printed materials, but we did not separately assess these two forms (i.e. asking whether participants get health information from printed and digital newspapers).
Table 1.
Outcome variables, questions, information sources, and response modes
| Variables | Questions asked | Response | Information sources (25 items) |
|---|---|---|---|
| Use sources for health information | Do you get health information from the following sources? | 1=Yes 0=No |
▪ Primary care providers ▪ Nurses ▪ Specialist doctors ▪ Pharmacists ▪ Veterinarians ▪ Dentists ▪ Health fairs ▪ Newspaper ▪ Magazines ▪ Books ▪ Scientific literature ▪ Television ▪ Radio ▪ Search engines (e.g., Google, Yahoo, Bing, Ask, and AOL) ▪ Social media (e.g., Facebook, Twitter, YouTube, Google Plus+, and Instagram) ▪ Medical websites (e.g., WebMD, Mayo Clinic, Medscape, Medline Plus, and MedicineNet) ▪ Blogs or celebrity webpages (e.g., Dr. Oz) ▪ Local health department ▪ Federal government organizations (e.g., the Centers for Disease Control) ▪ Friends ▪ Family ▪ Religious organizations and leaders ▪ Scientists ▪ Pharmaceutical companies ▪ Other companies or corporations |
| Levels of trust in information sources | How much do you trust health information from the following sources? | 1=Not at all 2=Some 3=Quite a bit 4=A great deal |
Demographics
Demographics included residence status (metro, non-metro), sex, age, annual income (<$25k, $25k to <$50k, $50k to <$75k, $75k to <$100k, $100k to <$125k, $125k and up), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Other), and education (less than high school, high school, some college, and Bachelor’s degree and above). Residence status was based on whether or not participants’ location of primary residence was located in a Core Based Statistical Area (CBSA).
Data Analysis
We applied survey weights provided by GfK for all analyses. The samples were weighted using the geodemographic benchmarks from the Current Population Survey (CPS) information released in March 2017 (U.S. Census Bureau & U.S. Bureau of Labor Statistics, 2017) so that the analyses reported here are representative of the non-institutionalized, adult U.S. population. We used t-tests, ANOVAs and Pearson correlations to test for differences in health literacy as a function of demographic characteristics. We used multiple logistic regressions to test whether use of each health information source differed by health literacy. Similarly, we used multiple linear regressions to examine whether trust in each health information source differed by health literacy. We conducted separate regressions for each health information source, controlling for metro status, sex, age, income, race/ethnicity, and education using Stata 14. Finally, we tested whether there were indirect effects of health literacy on source use through trust for sources with bootstrap estimates (Bollen & Stine, 1990) using Mplus 7.
Results
Participants’ ages ranged from 18 to 89 (M=47.32, SD=16.47). The majority (64.98%) were non-Hispanic White. About one-third had a Bachelors’ degree or higher (30.95%). See Table 1 for weighted percentages of participants’ demographics. Participants’ mean health literacy score was 4.74 (SD=1.61) out of 6. Slightly less than half of the participants (48.1%) answered all questions on the NVS correctly. About a fifth of participants (20.2%) scored equal to or below 3, indicating “high likelihood” or “possibility of limited literacy” (Weiss et al., 2005). Health literacy differed by race/ethnicity [F(3,593)=9.96, p<.001]; health literacy was higher among the Non-Hispanic White participants (M=5.15, SD=1.45) than Hispanic (M=4.00, SD=1.35, p<.001) or Non-Hispanic Black participants (M=3.49, SD=1.41, p<.001), but not Non-Hispanic Other participants (M=4.68, SD=1.28, p=.875). The difference between Hispanic and non-Hispanic Black participants was not significant (p=.548). Health literacy was positively associated with income (r=.30, p<.001) and education (r=.28, p<.001), but not age (r=−.06, p=.180). Health literacy scores did not differ significantly between metro/non-metro residents (p=.889) or men and women (p=.783).
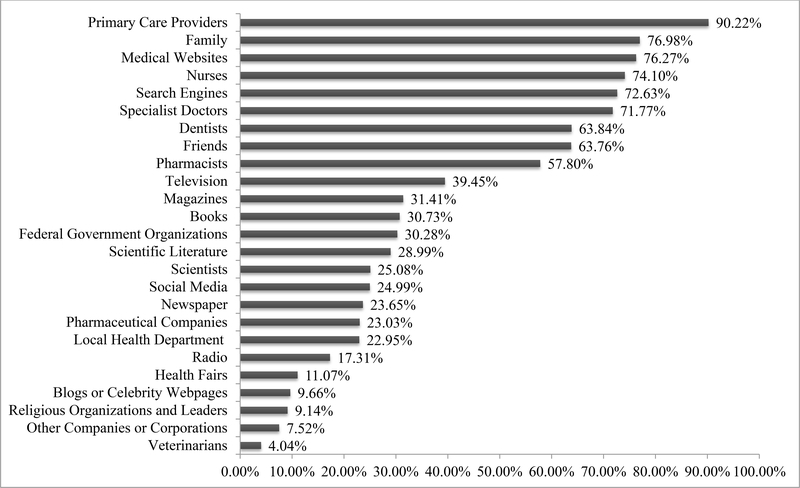
As shown in Figure 1, the majority of the sample reported using their primary care providers (90.22%), family (76.98%), medical websites (76.27%), nurses (74.10%), online search engines (72.63%), and specialist doctors (71.77%) as sources for health information. The least common sources were veterinarians (4.04%), other companies or corporations (7.52%), religious organizations and leaders (9.14%), blogs or celebrity webpages (9.66%), health fairs (11.07%), and radio (17.31%).
Fig. 1.
Use of each health information source
As shown in Table 3, participants reported trusting information from specialist doctors (M=3.38, SD=0.73), primary care providers (M=3.30, SD=0.75), and nurses (M=3.04, SD=0.76) the most. For the most trusted source, specialist doctors, more than half of the participants (51.81%) reported that they trusted health information from their specialist doctors “a great deal”. Participants trusted companies or corporations other than pharmaceutical companies (M=1.69, SD=0.71), blogs or celebrity webpages (M=1.71, SD=0.81), and social media (M=1.72, SD=0.76) the least. For the least trusted source, companies or corporations other than pharmaceutical companies, almost half of the participants (48.40%) reported that they trusted health information from companies or corporations other than pharmaceutical companies “not at all”.
Table 3.
Levels of trust in each source
| Health Information Sources | Mean (SD) | “not at all” % | “a great deal” % |
|---|---|---|---|
| Specialist doctors | 3.38 (0.73) | 0.74 | 51.81 |
| Primary care providers | 3.30 (0.75) | 0.65 | 46.72 |
| Nurses | 3.04 (0.76) | 1.47 | 29.96 |
| Pharmacists | 2.96 (0.81) | 2.87 | 28.07 |
| Federal government organizations | 2.94 (0.84) | 5.08 | 27.81 |
| Local health department | 2.85 (0.78) | 3.97 | 20.12 |
| Dentists | 2.84 (0.86) | 6.25 | 23.76 |
| Medical websites | 2.83 (0.85) | 6.54 | 22.19 |
| Scientific literature | 2.64 (0.95) | 12.21 | 21.43 |
| Family | 2.61 (0.83) | 7.01 | 15.11 |
| Scientists | 2.49 (0.91) | 15.55 | 13.54 |
| Books | 2.43 (0.86) | 13.49 | 10.81 |
| Friends | 2.36 (0.76) | 8.72 | 8.50 |
| Search engines | 2.31 (0.77) | 12.37 | 6.42 |
| Health fairs | 2.18 (0.87) | 21.69 | 8.74 |
| Magazines | 2.10 (0.74) | 18.78 | 3.75 |
| Newspaper | 2.06 (0.72) | 20.37 | 2.86 |
| Television | 2.02 (0.73) | 22.15 | 3.50 |
| Pharmaceutical companies | 1.96 (0.81) | 30.83 | 3.40 |
| Veterinarians | 1.96 (0.92) | 35.98 | 7.84 |
| Radio | 1.94 (0.73) | 26.93 | 2.87 |
| Religious organizations and leaders | 1.79 (0.84) | 42.82 | 5.59 |
| Social media | 1.72 (0.76) | 43.91 | 3.15 |
| Blogs or celebrity webpages | 1.71 (0.81) | 48.40 | 3.41 |
| Other companies or corporations | 1.69 (0.71) | 44.18 | 0.95 |
Note. Results were weighted using the overall U.S. population weights; trust ranges from 1–4.
Health Literacy and Information Use
Controlling for demographic variables, higher health literacy was associated with higher odds of using medical websites (OR=1.21, 95% CI [1.01, 1.45], p=.036) to get health information. Higher health literacy was associated with lower odds of using television (OR=0.83, 95% CI [0.70, 1.00], p=.044), social media (OR=0.80, 95% CI [0.65, 0.99], p=.041), and blogs or celebrity webpages (OR=0.74, 95% CI [0.58, 0.93], p=.010) to get health information (Table 4). Health literacy was not related to use of any other information source.
Table 4.
Health literacy and use of sources for health information
| Sources | OR | 95% CI for OR | p |
|---|---|---|---|
| Primary care providers | 1.18 | [0.90, 1.55] | .219 |
| Nurses | 1.13 | [0.94, 1.36] | .189 |
| Specialist doctors | 1.09 | [0.87, 1.37] | .449 |
| Pharmacists | 0.98 | [0.82, 1.17] | .793 |
| Veterinarians | 0.94 | [0.66, 1.34] | .719 |
| Dentists | 1.19 | [0.98, 1.44] | .072 |
| Health fairs | 1.01 | [0.75, 1.37] | .933 |
| Newspaper | 0.95 | [0.77, 1.18] | .672 |
| Magazines | 0.92 | [0.76, 1.11] | .391 |
| Books | 0.98 | [0.80, 1.18] | .824 |
| Scientific literature | 0.99 | [0.81, 1.21] | .925 |
| Television | 0.83 | [0.70, 1.00] | .044* |
| Radio | 0.90 | [0.73, 1.11] | .340 |
| Search engines | 1.09 | [0.92, 1.29] | .311 |
| Social media | 0.80 | [0.65, 0.99] | .041* |
| Medical websites | 1.21 | [1.01, 1.45] | .036* |
| Blogs or celebrity webpages | 0.74 | [0.58, 0.93] | .010* |
| Local health department | 1.04 | [0.84, 1.29] | .705 |
| Federal government organizations | 0.99 | [0.80, 1.23] | .927 |
| Friends | 1.05 | [0.88, 1.24] | .607 |
| Family | 1.04 | [0.86, 1.25] | .713 |
| Religious organizations and leaders | 0.96 | [0.76, 1.21] | .728 |
| Scientists | 1.15 | [0.91, 1.46] | .229 |
| Pharmaceutical companies | 0.89 | [0.73, 1.08] | .223 |
| Other companies or corporations | 0.98 | [0.70, 1.38] | .928 |
Note. Controlled for race/ethnicity, age, sex, education, income, and metro/non-metro status;
indicates p < .05; OR = odds ratio; CI = confidence interval.
Health Literacy and Information Trust
As shown in Table 5, controlling for demographic variables, lower health literacy was associated with less trust in health information from specialist doctors (b=0.06, SE=0.03, p=.034) and dentists (b=0.10, SE=0.04, p=.009); however, lower health literacy was associated with more trust in health information from television (b=−0.08, SE=0.03, p=.018), social media (b=−0.09, SE=0.03, p=.006), blogs or celebrity webpages (b=−0.09, SE=0.03, p=.007), friends (b=−0.08, SE=0.04, p=.019), and pharmaceutical companies (b=−0.09, SE=0.03, p=.004). Health literacy was not related to trust for any other information source.
Table 5.
Health literacy and trust in health information from sources
| Sources | b | SE | p |
|---|---|---|---|
| Primary care providers | 0.04 | 0.03 | .166 |
| Nurses | 0.04 | 0.04 | .260 |
| Specialist doctors | 0.06 | 0.03 | .034* |
| Pharmacists | 0.04 | 0.04 | .292 |
| Veterinarians | 0.03 | 0.04 | .554 |
| Dentists | 0.10 | 0.04 | .009** |
| Health fairs | 0.05 | 0.03 | .086 |
| Newspaper | −0.03 | 0.03 | .360 |
| Magazines | −0.03 | 0.03 | .235 |
| Books | −0.02 | 0.04 | .548 |
| Scientific literature | −0.002 | 0.04 | .970 |
| Television | −0.08 | 0.03 | .018* |
| Radio | −0.02 | 0.03 | .460 |
| Search engines | −0.02 | 0.03 | .527 |
| Social media | −0.09 | 0.03 | .006** |
| Medical websites | 0.01 | 0.03 | .670 |
| Blogs or celebrity webpages | −0.09 | 0.03 | .007** |
| Local health department | 0.02 | 0.03 | .581 |
| Federal government organizations | −0.01 | 0.04 | .882 |
| Friends | −0.08 | 0.04 | .019* |
| Family | −0.06 | 0.04 | .106 |
| Religious organizations and leaders | −0.05 | 0.04 | .159 |
| Scientists | 0.003 | 0.04 | .933 |
| Pharmaceutical companies | −0.09 | 0.03 | .004** |
| Other companies or corporations | −0.05 | 0.03 | .121 |
Note. Controlled for race/ethnicity, age, sex, education, income, and metro/non-metro status;
indicates p < .05;
indicates p < .01; b = regression coefficients; SE = standard errors.
Indirect Effects of Health Literacy on Source Use through Trust
There were significant indirect effects of health literacy on use through trust for seven sources: specialist doctors, dentists, television, social media, blogs or celebrity webpages, friends, and pharmaceutical companies. Higher health literacy was indirectly associated with a higher likelihood of using specialist doctors (ab=0.04, SE=0.02, p=.016) and dentists (ab=0.09, SE=0.03, p=.002) for health information through higher levels of trust. Higher health literacy was indirectly associated with lower likelihood of using television (ab=−0.10, SE=0.03, p=.006), social media (ab=−0.11, SE=0.04, p=.002), blogs or celebrity webpages (ab=−0.07, SE=0.03, p=.025), friends (ab=−0.08, SE=0.04, p=.027), and pharmaceutical companies (ab=−0.09, SE=0.04, p=.013) through lower levels of trust.
Discussion
We examined the relationship among health literacy, use of health information sources, and trust in health information sources. This study addressed gaps in the previous literature by examining the trend among adult U.S. population, by including a broad array of sources, and by differentiating among different types of online sources.
We identified the health information sources that were used and trusted by people with different health literacy levels and examined the associations between people’s health literacy. Participants were most likely to get health information from primary care providers, nurses, family, medical websites, online search engines, specialist doctors, and friends, in that order. Previous studies also reported that health professionals and the Internet were the most frequently used sources for health information and primary care providers were the most trusted source (Kelley, Su, & Britigan, 2016; Poínhos et al., 2017). Health care providers are commonly preferred sources for health information because of their professional training and credentials (Gaglio, Glasgow, & Bull, 2012; Learmonth et al., 2017). Online health information has become increasingly popular because of the rapid increase in Internet use and ease of access to Internet-based information (Jacobs, Amuta, & Jeon, 2017).
According to Nutbeam’s health literacy conceptual model (2000, 2008), critical health literacy represents the higher-level cognitive and social skills needed to critically analyze information. Health information appraisal is one factor of critical health literacy, indicating the extent to which individuals evaluate the reliability, validity, credibility, and applicability of health information (Chinn, 2011) when determining whether or not to use it. People with lower health literacy have greater difficulty evaluating and differentiating low quality health information from high quality health information (Ghaddar et al., 2012; Diviani et al., 2015), and have been found to give high quality ratings for low-quality health information (Benotsch, Kalichman, & Weinhardt, 2004). Our study contributes to a body of evidence demonstrating that, consistent with Nutbeam’s model, people with lower health literacy were more likely to use and trust health information from sources that might be lower quality (i.e., social media, blogs or celebrity webpages, and commercial/corporate sources). Low quality health information that is inaccurate or misleading could result in negative health consequences such as delaying health care seeking and engaging in unhealthy behaviors (Chen, Acosta, & Barry, 2016, 2017; Lau, Gabarron, Fernandez-Luque, & Armayones, 2012; Syed-Abdul et al., 2013).
We found that people with lower health literacy were more likely than those with higher health literacy to use television, social media, and blogs or celebrity webpages for health information. In contrast, previous studies reported that people with lower health literacy were less likely to use the Internet for health information (Shieh et al., 2009; Fagnano et al., 2012; Ghaddar et al., 2012; Sheng & Simpson, 2013; Cutilli et al., 2018). Our findings may seem inconsistent with those of prior research because we differentiated among on-line sources whereas previous work generalized across sources potentially obscuring variation by source. We found less use of medical websites but greater use and trust in social media, blogs and celebrity webpages among those with lower health literacy, which may be particularly accessible to this group (Hoedebecke et al., 2017). A second possible explanation is that Internet access and use which has increased over time, has in all likelihood improved among those with inadequate health literacy as well. Many of the previous studies were published between 2009 and 2012, when Americans had less widespread Internet access, in particular among those with low-income (Gaglio et al., 2012). The percentage of U.S. adults who use the Internet increased from 52% in 2000 to 76% in 2009 and 88% in 2016 (Pew Research Center, 2017). Finally, the majority of our participants (80%) had adequate health literacy (having NVS scores ≥ 4); therefore, people with the lowest levels of health literacy were not as represented in our sample.
It is possible that several of the health information sources preferred by people with lower health literacy (e.g., celebrity webpages, blogs, and social media) provide poorer quality health information than sources such as health care providers and government organizations (e.g., Centers for Disease Control and Prevention). Some health information from Internet-based sources and companies/corporations has been criticized for being of poor quality, lacking peer review or regulation (Cline & Haynes, 2001; Freudenberg, 2012), and for disseminating false and misleading health information (Freudenberg, 2014). Furthermore, commercial goals might override informational goals (Liu et al., 2015). Although some online health information sources (e.g., WebMD and Mayo Clinic) provide good quality information (Grohol, Slimowicz, & Granda, 2014; Guan, Maloney, Roter, & Pollin, 2017), much online information is sub-par. Indeed, a systematic literature review concluded that most previous studies (70%) reported quality was a problem for online health information (Eysenbach, Powell, Kuss, & Sa, 2002). In a more recent study, only 4 of 18 websites provided good quality health information (Tirlapur, Leiu, & Khan, 2013). Indeed, the main concern about health information on social media and blog sites is that these sources might have low quality information (Gibbons, Fleisher, Slamon, Bass, Kandadai & Beck, 2011; Moorhead, Hazlett, Harrison, Carroll, Irwin, & Hoving, 2013).
Our findings suggest that there may be a need to provide interventions targeting individuals with lower health literacy that would enhance their capabilities to evaluate health information quality, especially the health information from social media and blogs or celebrity websites. Having adequate critical health literacy is also important to evaluating the quality of online health information sources (Nutbeam, 2000, 2008; Chinn, 2011). Health consumers, especially individuals with lower health literacy may benefit from support in searching for credible and trustworthy health information (Atique et al., 2016). Health professionals could direct people to sources of high quality health information. For example, an intervention with instructional materials to increase older adults’ ability to access and use NIH online health information sources (i.e., the National Institutes of Health’s SeniorHealth.gov website) significantly improved participants’ eHealth literacy level (Xie, 2011). Providing a list of reliable health-related websites could benefit individuals with lower health literacy. It might also be possible to provide guidance to people with lower health literacy on how to differentiate poor quality health information sources from good quality ones. The Quality Guidelines provided by the U.S. Department of Health and Human Services (2016) include educational materials about how to navigate and select good quality online health information. They suggest people check the “last updated” date to ensure the currency of the health information and to be cautious about the “advertisement” labels to identify potential commercial bias due to conflicts of interest. Midlevel health care providers (e.g., nurse practitioner, physician assistants) and librarians could provide this guidance. It should also be integrated into high school health classes and informational pamphlets in healthcare clinics. Meanwhile, high quality health information sources should create messages that are more readable and understandable to increase the information accessibility among individuals with lower health literacy.
We also found that people with lower health literacy were less likely to trust health information from specialist doctors and dentists. A number of studies have demonstrated that people with limited health literacy are more likely to distrust their physicians (Paasche-Orlow & Wolf, 2007; Gupta et al., 2014). Source and message distrust likely go hand in hand. Compared to patients with adequate health literacy, those with lower health literacy are more likely to have negative perceptions of their healthcare experiences such as receiving little valuable health information and not receiving help with health problems (Wångdahl, Mårtensson, & Westerling, 2015) or not understanding physician instructions (Gupta et al 2014). This may undermine message trust. In addition, people with lower health literacy are also more likely to be seen by multiple rotating providers rather than have a personal provider. This is a barrier to developing a trusting provider-patient relationship (Egbert & Nanna, 2009), which also may undermine trust in providers’ health messages.
To encourage patients to engage in the decision-making process and improve their understanding and trust in the health information they received during the patient-clinician communication, health care providers might apply the teach-back method and use plain language when interacting with patients with lower health literacy (Kripalani & Weiss, 2006; Amuta, Chen, & Mkuu, 2017). Teach-back refers to asking health consumers to repeat in their own words what they have been told (Schillinger et al., 2003). When using the teach-back method, health care providers should use a caring tone of voice and attitude to create a “shame-free” environment for patients (Joint Commission, 2007). Plain language refers to providing health information (written or spoken) with common, everyday words so that people with lower health literacy can more easily understand (Agency for Healthcare Research and Quality, 2016).
Due to their relationships with health literacy and trust, television, social media, blogs or celebrity webpages, friends, and pharmaceutical companies might be platforms for reaching a broader audience with health messaging. Health professionals could use television, social media, or blogs sites to deliver high quality health education and campaign messages targeting individuals with lower health literacy. One of the benefits of television, social media, and blogs sites for health communication is allowing text information to be replaced by videos to target people with lower literacy (Moorhead et al., 2013; Adams, 2010). A number of researchers are exploring ways of influencing health communication transmitted through social networks (Napolitano, Hayes, Bennett, Ives, & Foster, 2013; Smit et al., 2017). In addition, further research is needed to investigate the factors driving greater use of, and trust in television, social media, and blogs for health information among individuals with lower health literacy. Lastly, we found that people with lower health literacy preferred sources such as social media and celebrity websites rather than medical websites and government. These sources are updated in real-time and contain brief health messages at lower reading grade levels (Boulos, Maramba, & Wheeler, 2006; Hoedebecke et al., 2017). Social media such as Facebook and Twitter provides opportunities for patients and caregivers to connect with, and support each other (Korda & Itani, 2013). Also, people with lower health literacy are relatively more likely to use celebrity endorsement when evaluating online health information quality (Diviani et al., 2015). Health professionals could apply strategies such as creating easy to understand brief messages and employing celebrity branding to increase use of and trust in credible medical websites and government sources among those with lower health literacy. For example, health-related organizations, including educational institutions, government agencies, and health-related corporations, use social media such as Twitter and Facebook to deliver credible health information to the public (Park, Rodgers, & Stemmle, 2013; Alas, Sajadi, Goldman, & Anger, 2013). Another example is that many tobacco control campaigns use famous celebrities to promote the behavior of not smoking; however, health professionals need to carefully select the celebrities to use as spokespeople because working with celebrities can have downsides such as if they suddenly become bad role models (CDC, 2003).
Limitations and Future Research
The cross-sectional design of the study restricts our ability to infer causal relationships between health literacy and health information source preferences, although testing the indirect effect of health literacy on source use through trust helps to identify plausible causal pathways that could be tested using an experimental paradigm. While some people with lower health literacy may be more likely to use and trust potentially lower quality sources, we did not directly evaluate the quality of the actual health information sources used by participants in our study. One possible future direction is to compare the quality of commonly used health information sources. Also, we did not distinguish between active and passive information seeking. Active information seeking refers to people who actively seek out information such as communicating with others, and passive information seeking refers to passive reception of information such as watching TV advertisements (Wilson, 2000). Future research could separate and compare passive and active information seeking behaviors between those with high and low literacy. Last, we used the NVS to measure health literacy; however, there are more than 50 instruments available for measuring individuals’ health literacy (Haun, Valerio, McCormack, Sørensen, & Paasche-Orlow, 2014). Other measures of health literacy could produce different results as measure may assess slightly different skills (Haun et al., 2014).
Conclusion
We investigated the association between people’s health literacy and their use of and levels of trust in 25 health information sources. Most participants used and trusted health information from healthcare professionals. People with lower health literacy were more likely to use and trust health information from social media and blogs or celebrity webpages where information accuracy and quality is less likely to be assured. Finally, people with lower health literacy scores were less likely to trust health information from specialist doctors and dentists. Our study raises concerns that people with lower health literacy may be less likely to evaluate the quality of health information sources and that public health efforts should be made to reach this audience with high quality information using channels they trust and use.
Table 2.
Weighted percentages of demographics and health literacy scores
| Demographic | % | HL Mean (SD) | p |
|---|---|---|---|
| Metro Status Category | |||
| Metro | 85.76 | 4.73 (1.24) | .889 |
| Non-Metro | 14.24 | 4.75 (2.99) | |
| Sex | |||
| Female | 51.45 | 4.76 (1.65) | .783 |
| Male | 48.56 | 4.71 (1.59) | |
| Race / Ethnicity | |||
| Non-Hispanic White | 64.98 | 5.15 (1.45) | < .001 |
| Non-Hispanic Black | 11.80 | 3.49 (1.41) | |
| Hispanic | 15.80 | 4.00 (1.35) | |
| Non-Hispanic Other | 7.41 | 4.68 (1.28) | |
| Age | |||
| 18 – 24 | 7.32 | 4.51 (1.38) | .180 |
| 25 – 34 | 20.08 | 5.22 (0.98) | |
| 35 – 44 | 18.47 | 4.67 (1.45) | |
| 45 – 54 | 17.52 | 4.70 (1.72) | |
| 55 – 64 | 18.34 | 4.66 (1.83) | |
| 65–74 | 14.16 | 4.40 (2.03) | |
| 75+ | 4.10 | 4.72 (1.87) | |
| Household Annual Income | |||
| <$25k | 16.13 | 3.49 (2.03) | < .001 |
| $25k to <$50k | 20.59 | 4.74 (1.52) | |
| $50k to <$75k | 17.41 | 4.81 (1.59) | |
| $75k to <$100k | 13.89 | 4.99 (1.41) | |
| $100k to <$125k | 10.00 | 5.36 (1.20) | |
| $125k and up | 21.98 | 5.13 (1.22) | |
| Education | |||
| Less than high school | 11.25 | 4.05 (1.82) | < .001 |
| High school | 29.04 | 4.18 (1.85) | |
| Some college | 28.76 | 4.89 (1.37) | |
| Bachelor and above | 30.95 | 5.37 (1.15) |
Note. Results were weighted using the overall U.S. population weights; HL = health literacy; health literacy scale: NVS ranges from 0 to 6.
Acknowledgement
Funding for the project leading to this manuscript was made possible by R01CA197351 from the National Cancer Institute.
References
- Adams SA (2010). Revisiting the online health information reliability debate in the wake of “web 2.0”: An inter-disciplinary literature and website review. International Journal of Medical Informatics, 79(6), 391–400. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality (2016). Plain Language at AHRQ. Retrieved from https://www.ahrq.gov/policy/electronic/plain-writing/index.html
- Alas A, Sajadi KP, Goldman HB, & Anger JT (2013). The rapidly increasing usefulness of social media in urogynecology. Female Pelvic Medicine & Reconstructive Surgery, 19(4), 210–213. [DOI] [PubMed] [Google Scholar]
- Amuta AO, Chen X, & Mkuu R (2017). The Effect of cancer information seeking on perceptions of cancer risks, fatalism, and worry among a US national sample. American Journal of Health Education, 1–8. [Google Scholar]
- Atique S, Hosueh M, Fernandez-Luque L, Gabarron E, Wan M, Singh O, ... & Shabbir SA (2016, August). Lessons learnt from a MOOC about social media for digital health literacy. In Engineering in Medicine and Biology Society (EMBC), 2016 IEEE 38th Annual International Conference of the (pp. 5636–5639). IEEE. [DOI] [PubMed] [Google Scholar]
- Baker DW (2006). The meaning and measure of health literacy. Journal of General Interna Medicine, 21, 878–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benigeri M, & Pluye P (2003). Shortcomings of health information on the Internet. Health Promotion International, 18(4), 381–386. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman S, & Weinhardt LS (2004). HIV-AIDS patients’ evaluation of health information on the Internet: The digital divide and vulnerability to fraudulent claims. Journal of Consulting and Clinical Psychology, 72(6), 1004. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, & Crotty K (2011). Low health literacy and health outcomes: an updated systematic review. Annals of Internal Medicine, 155(2), 97–107. [DOI] [PubMed] [Google Scholar]
- Bollen KA, & Stine R, (1990). Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology, 20, 115–40. [Google Scholar]
- Boulos MNK, Maramba I, & Wheeler S (2006). Wikis, blogs and podcasts: A new generation of Web-based tools for virtual collaborative clinical practice and education. BMC Medical Education, 6(1), 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brashers DE, Goldsmith DJ, & Hsieh E (2002). Information seeking and avoiding in health contexts. Human Communication Research, 28(2), 258–271. [Google Scholar]
- Centers for Disease Control and Prevention. (2003). Designing and implementing an effective tobacco counter-marketing campaign. Retrieved from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.692.2128&rep=rep1&type=pdf
- Chisolm DJ, Hardin DS, McCoy KS, Johnson LD, McAlearney AS, & Gardner W (2011). Health literacy and willingness to use online health information by teens with asthma and diabetes. Telemedicine and E-Health, 17(9), 676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Acosta S, & Barry AE (2016). Evaluating the accuracy of Google Translate for diabetes education material. Journal of Medical Internet Research (JMIR) Diabetes, 1(1), e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Acosta S, & Barry AE (2017). Machine or human? Evaluating a language translation mobile app for diabetes patients. Journal of Medical Internet Research (JMIR) Diabetes, 2(1), e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn D (2011). Critical health literacy: A review and critical analysis. Social science & medicine, 73(1), 60–67. [DOI] [PubMed] [Google Scholar]
- Clayman ML, Manganello JA, Viswanath K, Hesse BW, & Arora NK (2010). Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. Journal of Health Communication, 15(sup3), 252–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cline RJ, & Haynes KM (2001). Consumer health information seeking on the Internet: The state of the art. Health Education Research, 16(6), 671–692. [DOI] [PubMed] [Google Scholar]
- Cutilli CC, Simko LC, Colbert AM, & Bennett IM (2018). Health Literacy, Health Disparities, and Sources of Health Information in US Older Adults. Orthopaedic Nursing, 37(1), 54–65. [DOI] [PubMed] [Google Scholar]
- Diviani N, van den Putte B, Giani S, & van Weert JC (2015). Low health literacy and evaluation of online health information: a systematic review of the literature. Journal of Medical Internet Research, 17(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egbert N, & Nanna KM (2009). Health literacy: Challenges and strategies. The Online Journal of Issues in Nursing, 14(3). doi: 10.3912/OJIN.Vol14No03Man01 [Google Scholar]
- Eysenbach G, Powell J, Kuss O, & Sa ER (2002). Empirical studies assessing the quality of health information for consumers on the world wide web: A systematic review. JAMA, 287(20), 2691–2700. [DOI] [PubMed] [Google Scholar]
- Fagnano M, Halterman JS, Conn KM, & Shone LP (2012). Health literacy and sources of health information for caregivers of urban children with asthma. Clinical Pediatrics, 51(3), 267–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberg N (2012). The manufacture of lifestyle: The role of corporations in unhealthy living. Journal of Public Health Policy, 33(2), 244–256. [DOI] [PubMed] [Google Scholar]
- Freudenberg N (2014). Lethal but legal: Corporations, consumption, and protecting public health. Oxford University Press. [Google Scholar]
- Gaglio B, Glasgow RE, & Bull SS (2012). Do patient preferences for health information vary by health literacy or numeracy? A qualitative assessment. Journal of Health Communication, 17(sup3), 109–121. [DOI] [PubMed] [Google Scholar]
- Geana MV, Greiner KA, Cully A, Talawyma M, & Daley CM (2012). Improving health promotion to American Indians in the Midwest United States: Preferred sources of health information and its use for the medical encounter. Journal of Community Health, 37(6), 1253–1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaddar SF, Valerio MA, Garcia CM, & Hansen L (2012). Adolescent health literacy: the importance of credible sources for online health information. Journal of School Health, 82(1), 28–36. [DOI] [PubMed] [Google Scholar]
- Gibbons MC, Fleisher L, Slamon RE, Bass S, Kandadai V, & Beck JR (2011). Exploring the potential of Web 2.0 to address health disparities. Journal of Health Communication, 16(sup1), 77–89. [DOI] [PubMed] [Google Scholar]
- Grohol JM, Slimowicz J, & Granda R (2014). The quality of mental health information commonly searched for on the Internet. Cyberpsychology, Behavior, and Social Networking, 17(4), 216–221. [DOI] [PubMed] [Google Scholar]
- Guan Y, Maloney KA, Roter DL, & Pollin TI (2017). Evaluation of the informational content, readability and comprehensibility of online health information on monogenic diabetes. Journal of Genetic Counseling, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta C, Bell SP, Schildcrout JS, Fletcher S, Goggins KM, Kripalani S, & for the Vanderbilt Inpatient Cohort Study (VICS). (2014). Predictors of health care system and physician distrust in hospitalized cardiac patients. Journal of Health Communication, 19(sup2), 44–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF 2013. Introduction to mediation, moderation and conditional process analysis. New York, New York: Guilford Press. [Google Scholar]
- Haun JN, Valerio MA, McCormack LA, Sørensen K, & Paasche-Orlow MK (2014). Health literacy measurement: an inventory and descriptive summary of 51 instruments. Journal of Health Communication, 19(sup2), 302–333. [DOI] [PubMed] [Google Scholar]
- Hoedebecke K, Beaman L, Mugambi J, Shah S, Mohasseb M, Vetter C, ... & Couvillon E (2017). Health care and social media: What patients really understand. F1000Research, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2004). Health literacy: A prescription to end confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Jacobs W, Amuta AO, & Jeon KC (2017). Health information seeking in the digital age: An analysis of health information seeking behavior among US adults. Cogent Social Sciences, 3(1), 1302785. [Google Scholar]
- Joint Commission. (2007). “What Did the Doctor Say?:” Improving Health Literacy to Protect Patient Safety. Oakbrook Terrace, IL: The Joint Commission. [Google Scholar]
- Kandula NR, Nsiah-Kumi PA, Makoul G, Sager J, Zei CP, Glass S, ... & Baker DW (2009). The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Education and Counseling, 75(3), 321–327. [DOI] [PubMed] [Google Scholar]
- Kelley MS, Su D, & Britigan DH (2016). Disparities in health information access: results of a county-wide survey and implications for health communication. Health Communication, 31(5), 575–582. [DOI] [PubMed] [Google Scholar]
- Kim H, & Xie B (2017). Health literacy in the eHealth era: A systematic review of the literature. Patient Education and Counseling, 100(6), 1073–1082. [DOI] [PubMed] [Google Scholar]
- Knapp C, Madden V, Marcu M, Wang H, Curtis C, Sloyer P, & Shenkman E (2011). Information seeking behaviors of parents whose children have life‐threatening illnesses. Pediatric Blood & Cancer, 56(5), 805–811. [DOI] [PubMed] [Google Scholar]
- Koo M, Krass I, & Aslani P (2006). Enhancing patient education about medicines: Factors influencing reading and seeking of written medicine information. Health Expectations, 9, 174–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korda H, & Itani Z (2013). Harnessing social media for health promotion and behavior change. Health Promotion Practice, 14(1), 15–23. [DOI] [PubMed] [Google Scholar]
- Kripalani S, & Weiss BD (2006). Teaching about health literacy and clear communication. Journal of General Internal Medicine, 21(8), 888–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner M, Greenburg E, Jin Y, & Paulsen C (2006). The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006–483. National Center for Education Statistics. [Google Scholar]
- Lambert SD, & Loiselle CG (2007). Health information—seeking behavior. Qualitative Health Research, 17(8), 1006–1019. [DOI] [PubMed] [Google Scholar]
- Lau AY, Gabarron E, Fernandez-Luque L, & Armayones M (2012). Social media in health—What are the safety concerns for health consumers? Health Information Management Journal, 41(2), 30–35. [DOI] [PubMed] [Google Scholar]
- Learmonth YC, Adamson BC, Balto JM, Chiu C, Molina‐Guzman I, Finlayson M, Motl RW (2017). Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: A qualitative study. Health Expectations, 20(4), 574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HH, Yang TT, & Tsai CH (2012). To explore the social psychological factors influencing outcomes of health websites. Advanced Science Letters, 13(1), 774–779. [Google Scholar]
- Lemire M, Paré G, Sicotte C, & Harvey C (2008). Determinants of Internet use as a preferred source of information on personal health. International Journal of Medical Informatics, 77(11), 723–734. [DOI] [PubMed] [Google Scholar]
- Liu JM, Xu RX, Hu YS, Ren LK, Qiao H, Ding H, & Liu ZL (2015). Chinese Internet Searches Provide Inaccurate and Misleading Information to Epilepsy Patients. Chinese Medical Journal, 128(24), 3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livaudais-Toman J, Burke NJ, Napoles A, & Kaplan CP (2014). Health literate organizations: Are clinical trial sites equipped to recruit minority and limited health literacy patients? Journal of Health Disparities Research and Practice, 7(4), 1. [PMC free article] [PubMed] [Google Scholar]
- Logan RA, & Siegel ER (Eds.). (2017). Health Literacy: New Directions in Research, Theory and Practice (Vol. 240). IOS Press. [Google Scholar]
- Lubetkin EI, Zabor EC, Isaac K, Brennessel D, Kemeny MM, & Hay JL (2015). Health literacy, information seeking, and trust in information in Haitians. American Journal of Health Behavior, 39(3), 441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manganello JA (2007). Health literacy and adolescents: A framework and agenda for future research. Health Education Research, 23(5), 840–847. [DOI] [PubMed] [Google Scholar]
- McCleary-Jones V, Scheideman-Miller C, Dorn James A Jr, EdD., Johnson B R.N., Overall Mary M.S.N., B.S., & Dwyer Kathleen PhD., R.N. (2013). Health information technology use and health literacy among community-dwelling African Americans. ABNF Journal, 24(1), 10–6. [PubMed] [Google Scholar]
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, & Hoving C (2013). A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research, 15(4), e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napolitano MA, Hayes S, Bennett GG, Ives AK, & Foster GD (2013). Using Facebook and text messaging to deliver a weight loss program to college students. Obesity, 21(1), 25–31. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2017). Health Information National Trends Survey. Retrieved from https://hints.cancer.gov/data/survey-instruments.aspx
- National Institutes of Health. (2014). Health Information National Trends Survey. Retrieved from https://hints.cancer.gov/docs/Instruments/HINTS_4_Cycle_4_English_Annotated_Form.pdf
- Norman CD, & Skinner HA (2006). eHealth literacy: Essential skills for consumer health in a networked world. Journal of medical Internet research, 8(2): e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam D (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259–267. [Google Scholar]
- Nutbeam D (2008). The evolving concept of health literacy. Social science & medicine, 67(12), 2072–2078. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, & Wolf MS (2007). The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior, 31(1), S19–S26. [DOI] [PubMed] [Google Scholar]
- Paige SR, Krieger JL, & Stellefson ML (2017). The influence of eHealth literacy on perceived trust in online health communication channels and sources. Journal of Health Communication, 22(1), 53–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H, Rodgers S, & Stemmle J (2013). Analyzing health organizations’ use of Twitter for promoting health literacy. Journal of Health Communication, 18(4), 410–425. [DOI] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, & Nurss JR (1995). The test of functional health literacy in adults. Journal of General Internal Medicine, 10(10), 537–541. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2008). Sources of information on health and health care. Retrieved from http://www.pewhispanic.org/2008/08/13/iv-sources-of-information-on-health-and-health-care/
- Pew Research Center. (2013). Sources of health information. Retrieved from http://www.pewinternet.org/2013/11/26/part-two-sources-of-health-information/
- Pew Research Center. (2017). Internet/Broadband fact sheet. Retrieved from http://www.pewinternet.org/fact-sheet/internet-broadband/#
- Poínhos R, Oliveira BM, van der Lans IA, Fischer AR, Berezowska A, Rankin A, ... & de Almeida MD (2017). Providing personalized nutrition: Consumers’ trust and preferences regarding sources of information, service providers and regulators, and communication channels. Public Health Genomics. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, ... & Bindman AB (2003). Closing the loop: physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine, 163(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Shealy KM, & Threatt TB (2016). Utilization of the newest vital sign (NVS) in practice in the United States. Health Communication, 31(6), 679–687. [DOI] [PubMed] [Google Scholar]
- Sheng X, & Simpson PM (2013). Seniors, health information, and the Internet: motivation, ability, and Internet knowledge. Cyberpsychology, Behavior, and Social Networking, 16(10), 740–746. [DOI] [PubMed] [Google Scholar]
- Sheng X, & Simpson PM (2015). Health care information seeking and seniors: Determinants of Internet use. Health Marketing Quarterly, 32(1), 96–112. [DOI] [PubMed] [Google Scholar]
- Shieh C, Mays R, McDaniel A, & Yu J (2009). Health literacy and its association with the use of information sources and with barriers to information seeking in clinic-based pregnant women. Health Care for Women International, 30(11), 971–988. [DOI] [PubMed] [Google Scholar]
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, & Brand H (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(1), 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit AK, Keogh LA, Newson AJ, Butow PN, Dunlop K, Morton RL, ... & Cust (2017). Does personalised melanoma genomic risk information trigger conversations about skin cancer prevention and skin examination with family, friends and health professionals? British Journal of Dermatology, 177, 779–790. [DOI] [PubMed] [Google Scholar]
- Squiers L, Peinado S, Berkman N, Boudewyns V, & McCormack L (2012). The health literacy skills framework. Journal of Health Communication, 17(sup3), 30–54. [DOI] [PubMed] [Google Scholar]
- Syed-Abdul S, Fernandez-Luque L, Jian WS, Li YC, Crain S, Hsu MH, ... & Liou DM (2013). Misleading health-related information promoted through video-based social media: anorexia on YouTube. Journal of Medical Internet Research, 15(2), e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirlapur SA, Leiu C, & Khan KS (2013). Quality of information on the Internet related to bladder pain syndrome: A systematic review of the evidence. International Urogynecology Journal, 24(8), 1257–1262. [DOI] [PubMed] [Google Scholar]
- Toci E, Burazeri G, Jerliu N, Sørensen K, Ramadani N, Hysa B, & Brand H (2014). Health literacy, self-perceived health and self-reported chronic morbidity among older people in Kosovo. Health Promotion International, 30(3), 667–674. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau & U.S. Bureau of Labor Statistics. (2017). Current Population Survey (CPS). https://www.census.gov/programs-surveys/cps.html
- U.S. Department of Health and Human Services. (2008). America’s health literacy: Why we need accessible health information. An issue brief from the US Department of Health and Human Services. https://health.gov/communication/literacy/issuebrief/
- U.S. Department of Health and Human Services. Quality Guidelines. https://healthfinder.gov/aboutus/content_guidelines.aspx?_ga=1.201059694.1723099409.1489432918. Published July 18, 2016. Accessed November 1, 2017.
- Wångdahl J, Lytsy P, Mårtensson L, & Westerling R (2015). Health literacy and refugees’ experiences of the health examination for asylum seekers–a Swedish cross-sectional study. BMC Public Health, 15(1), 1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, ... & Hale FA (2005). Quick assessment of literacy in primary care: the newest vital sign. The Annals of Family Medicine, 3(6), 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BD, Reed RL, & Kligman EW (1995). Literacy skills and communication methods of low-income older persons. Patient Education and Counseling, 25(2), 109–119. [DOI] [PubMed] [Google Scholar]
- Wilson TD (2000). Human information behavior. Informing Science, 3(2), 49–56. [Google Scholar]
- Wu JR, Holmes GM, DeWalt DA, Macabasco-O’Connell A, Bibbins-Domingo K, Ruo B, ... & Erman B (2013). Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. Journal of General Internal Medicine, 28(9), 1174–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie B (2011). Effects of an eHealth literacy intervention for older adults. Journal of Medical Internet Research, 13(4): e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner J, Connell C, Bounds W, Crook L, & Yadrick K (2009). Peer reviewed: nutrition literacy status and preferred nutrition communication channels among adults in the lower Mississippi Delta. Preventing Chronic Disease, 6(4): A128. [PMC free article] [PubMed] [Google Scholar]