Abstract
There is growing evidence to suggest that multimorbidity is not only a consequence of aging but also other environmental risk factors such as socio-economic status and social marginalization. In this study, the prevalence of multimorbidity was examined (defined as the simultaneous occurrence of two or more chronic morbidities) by age, gender and the Ontario Marginalization index (material deprivation, residential instability, dependency and ethnic concentration). With a cross-sectional design, 2015 data on 18 morbidities from 12,516,587 residents of the province of Ontario, Canada, were analysed. About 82.1% of the population had one or no chronic conditions, 10.3% were multimorbid with two chronic conditions and 7.6% had three or more chronic conditions. The results showed that the prevalence of multimorbidity is noticeably higher in the most deprived areas compared to least deprived for all age groups. Our findings challenge the notion that multimorbidity is primarily driven by aging. Of the 18% of the total population which were multimorbid, 43% of them were under the age of 65. We noted a substantial excess of multimorbidity in younger and middle-aged adults who were most deprived. In some cases, those in the most deprived areas were showing increased cases of multimorbidity nearly 10 years sooner than those who were least deprived. This study shows that environmental factors such as material deprivation and residential instability are correlated with higher prevalence of multimorbidity.
Keywords: Multimorbidity, comorbidity, multiple-chronic conditions, long-term conditions, social determinants of health, population health, Ontario Marginalization index, cross-sectional study, material deprivation, poverty
Background
Multimorbidity is most commonly referred to as the simultaneous occurrence of two or more chronic health conditions and is traditionally associated with aging and seniors.1,2 There is growing evidence to suggest that multimorbidity is not only a consequence of aging and genetics but also other environmental risk factors such as socio-economic status (SES) and social marginalization.3,4 Multimorbidity is linked to higher mortality, reduced functional status and increased healthcare utilization.5,6 As the number of chronic conditions increases, patients tend to have more frequent and longer hospitalizations; increased risk of adverse drug effects; use of a greater range of specialist and other healthcare services and experience increased burden on themselves and caregivers.1,2,7 Healthcare utilization of patients that surpass three to five chronic conditions (variability depending on the nature of those conditions) is drastically increased and puts them at an increased risk for receiving inadequate or less than best practice care.7 Clinical best practices for managing multimorbidity are still lacking, as health systems are still largely configured for single-acute-based-illnesses, rather than multiple chronic diseases.3 Furthermore, the status quo of using many services to manage individual diseases has become duplicative, inefficient, burdensome and unsafe for patients’ due to poor coordination and integration of care.3
While it is well documented that multiple-chronic-conditions become progressively more common with aging, more recent publications seem to suggest that age is only one of many associated risk factors.3,4 These studies propose that multimorbidity is not just a by-product of time but other factors such as SES.3,4 According to Barnett et al.3 half of their observed multimorbid patients in Scotland were in fact under the age of 65. In addition, they found significant association between low SES and earlier onset of multimorbidity. Replication studies have surfaced to date, which have indicated similar associations in Canada.4,8,9
Long-term chronic health conditions are a fundamental challenge facing healthcare in Canada and other countries around the world. Healthcare spending in Ontario now accounts for nearly 40% of the entire provincial budget.10 In Ontario, 33% of healthcare service spending were incurred by the top 1% of users or 65% by the top 5%.11,12 Furthermore, studies on high-cost patients have shown that between 40% and 70% of high-cost patients did not improve in terms of transitioning to low-cost users and/or lower utilization patterns, especially in the later life course.12,13
As a result, prevention is currently the most viable solution for reducing the rise in multimorbid patients and associated costs. According to the World Health Organization,14 prevention and early interventions are still regarded as top solutions to combating the rise in chronic health conditions. Thus, as the proportion of Ontarians living with multimorbidity increases, we need to assess chronic diseases from a holistic perspective that captures not only the symbiotic relationship of chronic diseases downstream, but also the many risk factors upstream, that are drivers of chronic conditions and multimorbidity. However, current knowledge about the impacts of daily environments, social and material needs on multimorbidity are in their infancy. This study aims to contribute towards growing evidence that material deprivation, residential instability, ethnic concentration and dependency may potentially have significant impacts on multimorbidity. Moreover, no study to date has looked at the impact of marginalization on multimorbidity. The Ontario Marginalization (ON-Marg) and deprivation indices are considered to be more comprehensive measures for marginalization and poverty than SES alone.15–17
Objectives
The aim of this study is to provide an epidemiological descriptive overview of the relationship between the ON-Marg indices. The objectives for the study are to descriptively analyse the prevalence of multimorbidity across the province of Ontario by age, gender, material deprivation, residential instability, ethnic concentration and dependency, using health administrative databases.
Methods
Measuring multimorbidity
Multimorbidity has been conceptualized in many ways according to previous literature. A systematic review by Fortin et al.,18 compared studies reporting the prevalence of multimorbidity and found large variations with respect to both methodology and findings. They found disparities in terms of age cut-offs, number of conditions used, particularly, whether 2+ or 3+ chronic conditions constitute multimorbidity. Their study showed that this large variation in evaluation and methodology resulted in prevalence estimates ranging from 13% to 72%.18 They recommend using at least 12 or more commonly accepted chronic conditions, which drastically reduces this discrepancy.18 As per cut-offs in the number of conditions, they suggest using two or more chronic diseases as a general estimate and to use three or more to identify higher needs patients.18 Diederichs et al.1 conducted a systematic review that identified 39 different multimorbidity measures. Some measures were based on simple counts of chronic diseases, with considerable variation in the list of diseases used. Other articles for example, attempted to weigh diseases to account for burden of illness, number of body systems affected, patient preferences for care and so forth. There is still no ‘gold standard’ in measuring multimorbidity.1 Using counts of chronic conditions to define multimorbidity, based on prevalence and availability of health administrative data, continues to be a common choice by many researchers.3,4,9 Therefore, based on the objectives of this study, methodological design and available data, we will define multimorbidity: as the co-occurrence of 2+ chronic conditions from the province’s linked health administrative data, which can reliably provide a list of 18 chronic conditions (itemized subsequently). The co-occurrence of 3+ chronic conditions was also analysed to identify higher needs populations.
The ON-Marg index
The ON-Marg indices are the Ontario specific version of the Canadian marginalization index. The indices were developed using 42 census variables and are now available for 2001, 2006 and 2011. Previous theoretical frameworks on marginalization, deprivation and factor analysis were used to derive its four dimensions: material deprivation (composite measure of income, education, single-parent families and housing quality), residential instability (composite measure of dwelling/family characteristics, neighbourhood quality and cohesiveness), ethnic concentration (area-level measure of residents who are recent immigrants and visible minorities) and dependency (adults who are unemployed, unable to work and in unpaid professions).19 Each dimension is organized into quintiles, with quintile 1 representing those least deprived to quintile 5 (most deprived). We will be using material deprivation and residential instability measures from the ON-Marg tool as part of the primary analysis.19 The other two dimensions (ethnic concentration and dependency) will be used as part of the secondary analysis. The ON-Marg has been used in the field within this context previously.16,20
Study design and population
This study is a cross-sectional analysis of a series of linked health administrative databases in Ontario, Canada. The linked data consists of derived cohorts from the Institute for Clinical Evaluative Sciences (ICES), Canadian Institute for Health Information, Ontario Health Insurance Plan (OHIP) and the ON-Marg index databases. Our sample comprises all residents of the Province of Ontario alive in 2015.
Conditions and data sources
The study derived cohort demographic and health statistics, using linked health databases and the ON-Marg to geographically index neighbourhood ‘marginalization’ across Ontario. Our cohort and their conditions were drawn from a series of linked health administrative databases from ICES. In Ontario, the costs of all medically necessary care are covered by OHIP for all residents and immigrants (after a 3-month wait period). This includes all hospital, physician, in-home care and long-term care services.9 These data are kept secure and housed at ICES, in accordance with policies and guidelines set by the Office of the Information and Privacy Commissioners of Ontario.9 The Ontario healthcare system typically provides services by sector (e.g. physicians’ services, drugs, hospitalization, etc.) and tracks those services through distinct databases. Therefore, to compile a comprehensive portrait of underlying diagnoses and conditions of Ontarians, linked administrative databases were combined for analysis (using unique encrypted identifiers at the individual level).9 The international classification of disease (ICD) diagnostic codes used to identify the conditions are provided in Table 2A (see Appendix 2).
The following conditions were used to construct cases of multimorbidity: Alzheimer’s disease, arthritis (excluding osteoarthritis), asthma, cancer, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), Crohn’s and Colitis, depression, diabetes, epilepsy, human immunodeficiency virus (HIV), hypertension, multiple sclerosis, myasthenia gravis, myocardial infarction (MI), Parkinson’s disease, schizophrenia and stroke. We used Registered Persons Database to define the study cohort which is comprised of the residents of the province of Ontario, who were alive and eligible for OHIP coverage in 2015. The covariates sex, age, residential dissemination area (DA) and the ICES key numbers for merging individual health records across administrative databases were recorded. The following are ICES derived databases: the Ontario Asthma data set (ASTHMA), Ontario CHF data set, Ontario COPD data set, Ontario HIV data set, Ontario Hypertension data set (HYPER), Ontario Diabetes data set, Ontario MI data set, Ontario Rheumatoid Arthritis data set, Ontario Crohn’s and Colitis Cohort data set and Ontario Cancer Registry. The 10 years look back window for each patient was used. A specific algorithm was used to assign the conditions (i.e. one hospitalization or two OHIP visits for the same condition over a period of 2 years). Visits within a period of less than 30 days were counted as one visit.21 The ON-Marg index was used for assigning the marginalization indices to the cohort based on their residential DAs.
Statistical analysis
These data sets were linked using unique encoded identifiers and analysed at the ICES. The data were descriptively analysed, using summary statistics, frequency and percentages to describe the cohort and data sample. We used logistic regression to calculate age–sex adjusted proportion of multimorbidity in each deprivation quintile. SAS 7.1 Enterprise software was used for the statistical analysis and data manipulations.
Results
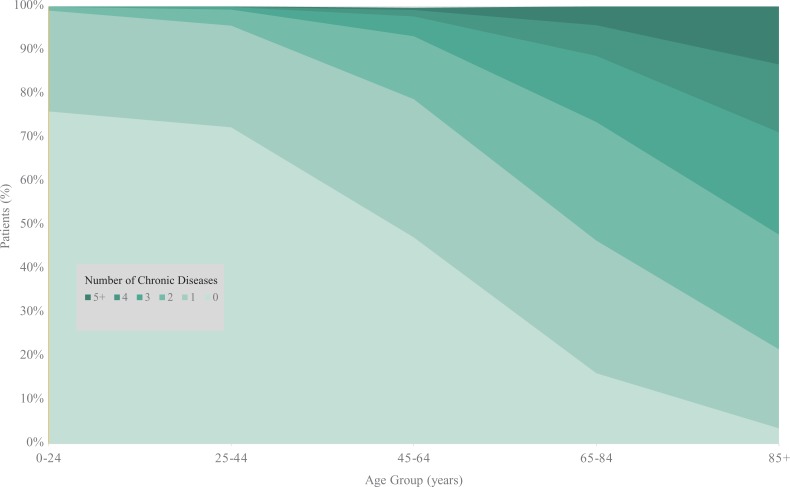
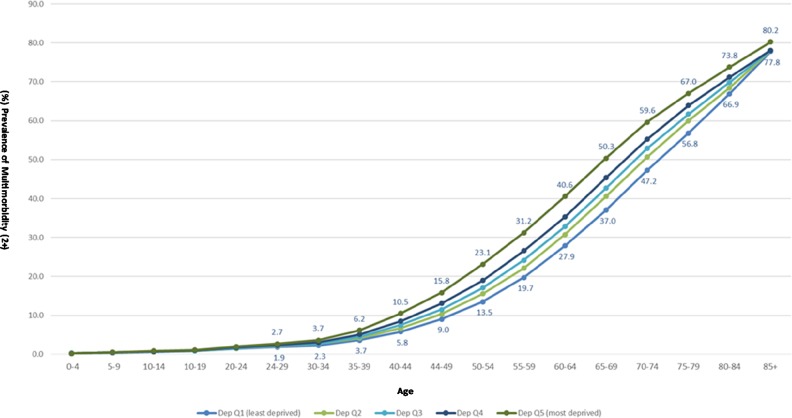
We analysed data from 12,516,587 residents of the province of Ontario derived from various health administrative data sources. Table 1 provides the demographic characteristics of the study population, the proportion of those with multimorbidity and severity by the number of chronic conditions. Both genders, men (48.7%) and women (51.3%), were equally represented, as well as all deprivation groups (Table 1). About 82.1% of the population had zero or one chronic condition, 10.3% had two chronic conditions and 7.6% had three or more chronic conditions (Table 1). Of the total population, the distribution of the number of chronic conditions was very similar in the male and female cohorts. As expected, the number of morbidities and the proportion of people with multimorbidity increased considerably with age (Figure 1). The results also showed that the prevalence of multimorbidity is noticeably higher in the most deprived areas compared to least deprived for all age groups (Figure 2). The difference of the prevalence of multimorbidity between the most and least deprived, increased steadily from less than 1% (age 0–29) to 12.7% (age 30–64) and 13.3% at the age of 65–69 (Figure 2). The difference then gradually decreased for residents 70 years of age and older (Figure 2). The largest gap between least and most deprived areas was observed at age 65–69 at 13.3% (Figure 2).
Table 1.
Demographics, material deprivation and multimorbidity prevalence.
| ON-Marg score | n (%) | Prevelance of multimorbidty, by (n) conditions | |||
|---|---|---|---|---|---|
| 0 and 1 | 2 | 3+ | |||
| All groups | Total | 12,516,587 (100) | 10,269,834 (82.1) | 1,291,642 (10.3) | 955,311 (7.6) |
| Male | 6,096,430 (48.7) | 5,007,988 (82.1) | 625,133 (10.3) | 463,509 (7.6) | |
| Female | 6,420,157 (51.3) | 5,261,846 (82) | 666,509 (10.4) | 491,802 (7.6) | |
| 1 and 2 Least deprived |
Sex | ||||
| Male | 2,733,312 (44.8) | 2,295,225 (84) | 261,655 (9.6) | 176,632 (6.4) | |
| Female | 2,872,143 (44.7) | 2,427,772 (84.5) | 266,931 (9.3) | 177,440 (6.2) | |
| Age, years | |||||
| 0–24 | 1,512,205 (46.3) | 1,499,667 (99.2) | 11,869 (0.8) | 669 (0.04) | |
| 25–44 | 1,450,118 (44.3) | 1,395,782 (96.3) | 46,728 (3.2) | 7,608 (0.5) | |
| 45–64 | 1,685,085 (45.2) | 1,382,333 (82.5) | 216,646 (12.9) | 76,106 (4.5) | |
| 65–84 | 825,288 (42.9) | 415,643 (50.4) | 218,227 (26.4) | 191,418 (23.2) | |
| 85+ | 132,759 (40.8) | 29,372 (22.1) | 35,116 (26.5) | 68,271 (51.4) | |
| 3 | Sex | ||||
| Male | 1,160,752 (19.0) | 946,584 (81.5) | 122,990 (10.6) | 91,178 (7.9) | |
| Female | 1,216,304 (19.0) | 991,581 (81.5) | 129,807 (10.7) | 94,916 (7.8) | |
| Age, years | |||||
| 0–24 | 600,456 (18.4) | 594,966 (99.1) | 5191 (0.9) | 300 (0.05) | |
| 25–44 | 608,604 (18.6) | 582,898 (95.8) | 21,633 (3.6) | 4073 (0.7) | |
| 45–64 | 720,129 (19.3) | 567,533 (78.8) | 104,636 (14.5) | 47,960 (6.7) | |
| 65–84 | 384,086 (20.0) | 178,711 (46.5) | 104,457 (27.2) | 100,918 (26.3) | |
| 85+ | 63,781 (19.6) | 14,057 (22.04) | 16,880 (26.5) | 32,844 (51.5) | |
| 4 and 5 Most deprived |
Sex | ||||
| Male | 2,202,366 (36.1) | 1,766,179 (80.2) | 240,488 (10.9) | 195,699 (8.9) | |
| Female | 2,331,710 (36.3) | 1,842,493 (79) | 269,771 (11.6) | 219,446 (9.4) | |
| Age, years | |||||
| 0–24 | 1,154,124 (35.3) | 1,142,326 (99) | 11,101 (1) | 697 (0.06) | |
| 25–44 | 1,212,980 (37.1) | 1,150,403 (94.9) | 51,163 (4.2) | 11,114 (0.9) | |
| 45–64 | 1,325,244 (35.5) | 989,976 (74.7) | 216,086 (16.3) | 119,182 (9) | |
| 65–84 | 712,851 (37.1) | 299,103 (41.9) | 198,501 (27.9) | 215,247 (30.2) | |
| 85+ | 128,877 (39.6) | 26,864 (20.8) | 33,408 (25.9) | 68,605 (53.2) | |
ON-Marg: Ontario Marginalization.
Figure 1.
Number of chronic disorders by age group.
Figure 2.
Prevalence of multimorbidity (2+) by age and material deprivation.
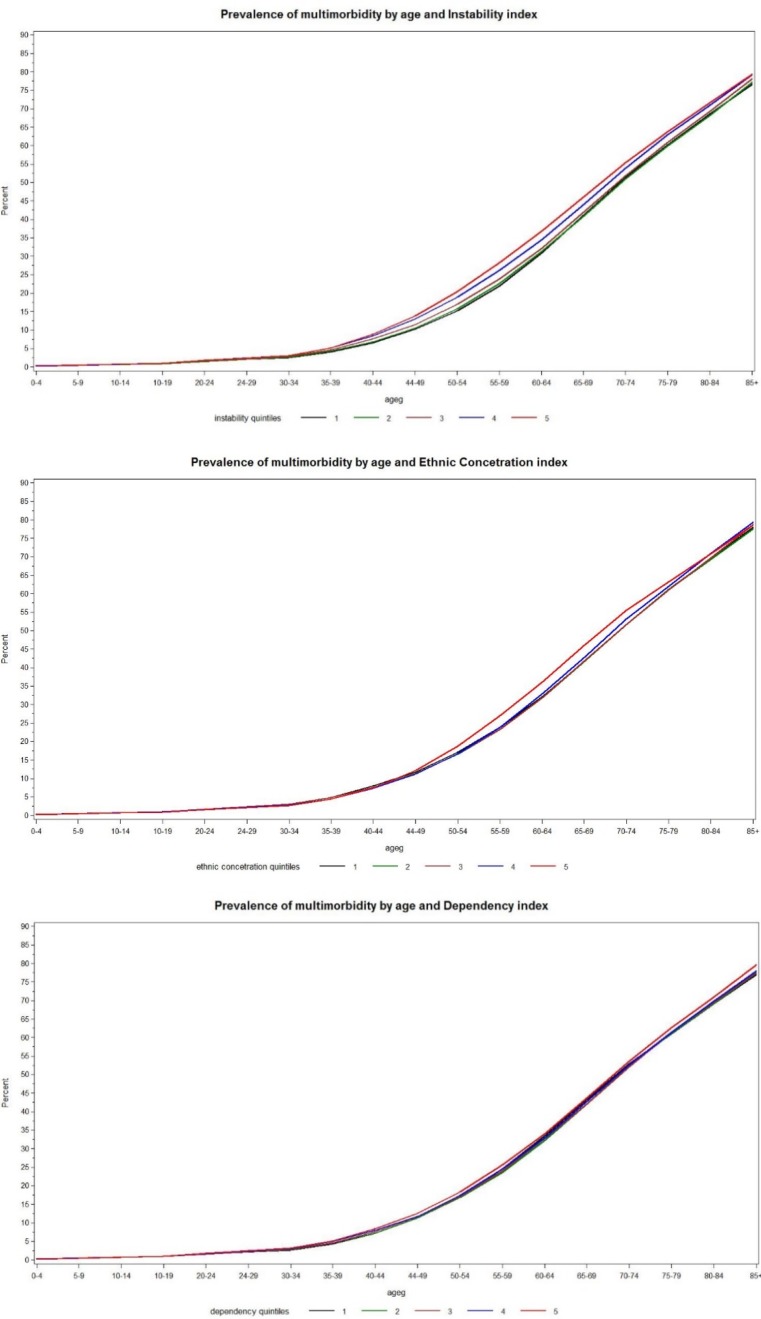
The pattern of the differences between the prevalence of multimorbidity by material deprivation was very similar for male and female across all age groups. The relationship between residential instability and prevalence of multimorbidity was similar to that of material deprivation. The gap between low and high residential instability showed similar pattern starting at an early age, then widening in middle-aged cohorts and narrowing for older residents. Also, the observed differences between those most and least deprived were consistent with the 2 counts definition, and when accounting for sicker populations with a multimorbidity measure of 3+ conditions. However, investigation of the relationship between ethnic concentration and dependency demonstrated little to no effect on the prevalence of multimorbidity (data not shown, plots provided in Figure 1A (see Appendix 1)).
Discussion
This study found that the prevalence of multimorbidity is noticeably higher in the most deprived areas compared to least deprived for all age groups. We also noted a substantial excess of multimorbidity in younger and middle-aged adults who were most deprived. In some cases, those in the most deprived areas were showing increased cases of multimorbidity nearly 10 years sooner than those who were least deprived. This study shows that environmental factors such as material deprivation and residential instability are correlated with higher prevalence of multimorbidity.
The results of this study corroborate previous studies suggesting that multimorbidity is common, especially with ageing.3,4 The strong association between age and multimorbidity is well-known but other associations are not as well recognized. First, although the prevalence of multimorbidity is much higher in older individuals, of the 18% of the total population which was multimorbid, 43% of them were under the age of 65. These findings support recent publications which have cautioned that multimorbidity is not just a problem of old age.3,4 Thus, nearly half of the individuals found to be multimorbid were under the age of 65. Second, although age had the strongest association with multimorbidity, we noted a substantial excess of morbidities in younger and middle-aged adults who were most deprived. In some cases, those in the most deprived areas were about 7–8 years younger than those in the most affluent areas. It is difficult to comment as to why such a difference is evident based on our study design. Perhaps, the difference is due to lifestyle choices (smoking, excessive drinking, etc.) or other factors such as nutrition, stress, security needs and the built environment. Future studies may be able to shed light and further inquire as to the observed difference in this study.
In terms of advancing the field, Pefoyo et al.9 did perform a similar study looking at the prevalence of multimorbidity within Ontario. However, our study is unique in that no one has looked at the prevalence of multimorbidity at the provincial level in relation to material deprivation and residential instability. According to Fitzpatrick et al.,16 the ON-Marg provides a broader range of determinants on health beyond conventional SES measures of income and education. Other studies similar to the one conducted by Roberts et al.4 calculated multimorbidity at the national level using self-reports and not actual health utilization data, which can be more accurate and less prone to response bias. This study advances the field: by examining the prevalence of multimorbidity within the largest Canadian province, using a more comprehensive measure of poverty/marginalization than conventional SES measures and multimorbidity estimates based on actual utilization of healthcare services and not self-reported diseases.
Our study used a very large sample which is well representative of the entire population in the province of Ontario. We must be mindful of potential data quality issues, when using administrative data. Also, the ICES algorithms are not perfect and there is potential for false positives and false negatives in identifying morbidities. However, the validated algorithms for most conditions are generally robust22–24 and with a sample size this large, any minor inaccuracies unless widespread should not be an issue. Also, we do not have an exhaustive list of morbidities, nor does a gold standard presently exist for better measuring multimorbidity with the use of health administrative databases. We included 18 chronic conditions which meet and exceed current research recommendations and practices in this field.4,9,18 We acknowledge that a simple count does not capture the heterogeneity and wide variation between individuals with multiple chronic conditions. Moreover, it is entirely possible that a younger patient could enjoy a better quality of life than someone older, although they share the same number of chronic conditions. We were also unable to account for several mental health conditions such as generalized anxiety disorder, dementia, post-traumatic stress disorder and so forth. As a result, our findings are likely underestimating the prevalence of multimorbidity by not accounting for certain mental health conditions.
In conclusion, we can not draw any definitive causal mechanisms on multimorbidity based on this study design. However, this study did show that age is not an absolute factor on the number of chronic illnesses and that other environmental factors such as material deprivation and housing instability were correlated with higher prevalence of multimorbidity. This has implications for health policy in that greater attention to prevention and increasing standards of living, earlier in the life course, especially in low SES neighbourhoods is warranted. The difference observed could be attributed to many causes; thus, more research is needed to better understand the specific or underlying mechanisms driving multimorbidity.
Supplemental Material
Supplemental Material, COB_Appendix_1 for Measuring the association between marginalization and multimorbidity in Ontario, Canada: A cross-sectional study by John Sina Moin, Rahim Moineddin, and Ross Edward Grant Upshur in Journal of Comorbidity
Appendix 1
Figure 1A.
Plots for residential instability, ethnic concentration and dependency.
Appendix 2
Table 2A.
List of diagnosis codes for defining the 18 selected conditions.a
| Condition | ICD 9/OHIP | ICD 10 |
|---|---|---|
| Alzheimer’s disease | 290, 294.1, 331 | F00–F03, F05.1, G30, G31.1 |
| Arthritis – rheumatoid arthritis (excluding osteoarthritis) | 714 | M05–M06 |
| Asthma | 493 | J45 |
| Cancer | 140–239 | C00–C26, C30–C44, C45–C97 |
| Chronic obstructive pulmonary disease | 491, 492, 496 | J41, J43, J44 |
| Congestive heart failure | 428 | I50, I50.1, I50.9 |
| Crohn’s and Colitis | 555, 556 | K50, K51 |
| Depression | 311, 300, 296 | F32, F33, F412, F480 |
| Diabetes | 250 | E08–E13 |
| Epilepsy | 345 | G40, G41 |
| Human immunodeficiency virus | 042, 043, 044 | B20–B24 |
| Hypertension | 401, 402, 403, 404, 405 | I10, I11, I12, I13, I15 |
| Multiple sclerosis | 340 | G35 |
| Myasthenia gravis | 358 | G700, G701, G702 |
| Myocardial infarction | 410 | I21, I22 |
| Parkinson’s disease | 332 | G20, G21, G22 |
| Schizophrenia | 295, 298 | F20, F21, F23.1, F25 |
| Stroke or transient ischemic attack | 430, 431, 432, 434, 436 | G45.0–G45.3, G45.8–G45.9, H34.1, I60, I61, I63, I634 |
Footnotes
Authors’ note: The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC).
References
- 1. Diederichs C, Berger K, Bartels D. The measurement of multiple chronic diseases: a systematic review on existing multimorbidity indices. J Gerontol A: Biol Sci Med Sci 2011; 66(3): 301–311. [DOI] [PubMed] [Google Scholar]
- 2. Tylor A, Price K, Gill T, et al. Multimorbidity – not just an older person’s issue. Results from an Australian biomedical study. BMC Public Health 2010; 10: 718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barnett K, Mercer S, Norbury M, et al. Epidemiology of multimorbidity and implications for healthcare, research, and medical education: a cross-sectional study. Lancet 2012; 380: 37–43. [DOI] [PubMed] [Google Scholar]
- 4. Roberts KC, Rao DP, Bennett TL, et al. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health Promot Chronic Dis Prev Can 2015; 35(6): 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tsoi CS, Chow JY, Choi KS, et al. Medical characteristics of the oldest old: retrospective chart review of patients aged 85+ in an academic primary care centre. BMC Res Notes 2014; 7: 340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Upshur RE, Wang L, Moineddin R, et al. The complexity score: towards a clinically-relevant, clinician-friendly measure of patient multi-morbidity. Int J of Pers Cent Med 2012; 2(4): 799–804. [Google Scholar]
- 7. Canadian Institute for Health Information. All-cause readmission to acute care and return to the Emergency Department. Ottawa: CIHI, 2012. [Google Scholar]
- 8. Nicholson K, Terry A, Fortin M, et al. Examining the prevalence and patterns of multimorbidity in Canadian primary healthcare: a methodologic protocol using a national electronic medical record database. J Comorb 2015; 5: 150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pefoyo AK, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health 2015; 15: 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The Government of Ontario. Jobs for today and tomorrow – 2016 Ontario Budget. Toronto: Queen’s Printer for Ontario, 2016. [Google Scholar]
- 11. Wodchis W. Deconstructing the 1–5%. Toronto: Health Systems Performance Research Network, 2014. [Google Scholar]
- 12. Wodchis W, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ 2016; 188(3): 182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moineddin R, Jason XN, Wang L, et al. Measuring change in health status of older adults at the population level: the transition probability model. BMC Health Serv Res 2010; 10: 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization. World report on ageing and health. Geneva: World Health Organization, 2015. [Google Scholar]
- 15. Berthoud R, Bryan M, Bardasi E. The dynamics of deprivation. Colchester: Institute for Social and Economic Research, 2004. [Google Scholar]
- 16. Fitzpatrick T, Rosella LC, Calzavara A, et al. Looking beyond income and education: socioeconomic status gradients among future high-cost users of health care. Am J Prev Med 2015; 49(2): 161–171. [DOI] [PubMed] [Google Scholar]
- 17. Notten G, Mendelson M. Using low income and material deprivation to monitor poverty reduction. Ottawa: Caledon Institute of Social Policy, 2016. [Google Scholar]
- 18. Fortin M, Stewart M, Poitras M, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012; 10(2): 142–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Matheson FI, Dunn JR, Smith K, et al. ON-Marg – User Guide Version 1.0. Toronto: Centre for Research on Inner City Health, 2012. [Google Scholar]
- 20. White LH, Matheson FI, Rahim M, et al. Neighbourhood deprivation and regional inequalities in self-reported health among Canadians: are we equally at risk? Health & Place 2011; 17: 361–369. [DOI] [PubMed] [Google Scholar]
- 21. Tonelli M, Wiebe N, Fortin M, et al. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 2015; 15: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Antoniou T, Zagorski B, Loutfy MR, et al. Validation of case-finding algorithms derived from administrative data for identifying adults living with human immunodeficiency virus infection. PLoS One 2011; 6: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hux JE, Flintoft V, Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 2002; 25(3): 512–516. [DOI] [PubMed] [Google Scholar]
- 24. Schultz SE, Rothwell DM, Chen Z, et al. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Inj Can 2013; 33(3): 160–166. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, COB_Appendix_1 for Measuring the association between marginalization and multimorbidity in Ontario, Canada: A cross-sectional study by John Sina Moin, Rahim Moineddin, and Ross Edward Grant Upshur in Journal of Comorbidity