Abstract
Case summary
Congenital or acquired hepatic cystic lesions in cats are a rare condition. Congenital hepatic cysts are often present as part of a systemic polycystic disease involving several organs. Most cats with hepatic cysts remain clinically normal for their lives, although some patients may show abdominal distension, vomiting, abdominal pain and jaundice. An 11-year-old female neutered Persian cat was presented to our institution 3 days after the onset of inappropriate defecation and urination. This patient had a history of polycystic kidney disease and a small hepatic cystic lesion. Physical examination showed pain on abdominal palpation. Abdominal ultrasonography revealed an increase in the size of the hepatic cyst and a partial obstruction of the biliary tract. Owing to the progression of the hepatic cyst, laparoscopic excision and omentalisation were performed. The cyst was completely resected using a 5 mm laparoscopic vessel sealer/divider device. It was removed from the abdomen through one of the portals and was submitted for histological study. After cyst excision, omentopexy was performed using 4-0 USP braided absorbable material. At follow-up examination 5 days later, the physical examination was normal and abdominal palpation was not painful. A biopsy report confirmed the diagnosis of a liver cyst. A follow-up abdominal ultrasonography performed 6 months after surgery revealed no recurrence of the liver cyst.
Relevance and novel information
To our knowledge, this is the first case report describing the laparoscopic technique of liver cystectomy and omentopexy in veterinary medicine. Minimally invasive surgery is gaining widespread acceptance within the veterinary community because of its benefits. However, further investigation with prospective studies are necessary.
Keywords: Hepatic cyst, laparoscopy, minimal invasive surgery, omentopexy, systemic polycystic disease
Introduction
Cystic lesions in the feline liver are epithelium-lined cavities filled with liquid of differing composition. The pathogenesis is not well defined, but they can be either congenital or acquired, but in either case they are a rare condition. Most congenital hepatic cysts are of bile duct origin, they are usually multiple and are often present as part of a systemic polycystic disease involving several organs.1 Acquired hepatic cysts may occur due to trauma, inflammation, neoplasia or liver hydatidosis.1,2
Polycystic disease is characterised by a number of cysts of various sizes affecting the renal cortex and medulla and occasionally the liver and pancreas.3 Persian cats and Persian crosses are over-represented because of a form of autosomal dominant polycystic kidney disease (ADPKD), affecting approximately 37% of Persian cats worldwide. Renal cysts are typically seen in ADPKD, although up to 9% of cats suffering from ADPKD may also develop hepatic cysts.3
Most cats with hepatic cysts remain clinically normal throughout their lives, and treatment is not recommended unless clinical signs occur. Mild signs may include abdominal distension, while more severe signs include vomiting, abdominal pain and jaundice. The decision of whether to treat liver cysts surgically depends on the cyst size, the progression of the illness and clinical signs, and the presence of further complications such as bile duct obstruction.1,2,4
Various treatment options have been described: ultrasound-assisted drainage, open surgical excision, fenestration or omentalisation. However, to our knowledge, laparoscopic excision and omentalisation has not been described for the treatment of a cystic liver lesion in cats. The undeniable advantages of minimally invasive surgery, including minimal surgical trauma, rapid postoperative recovery and reduced postoperative adhesions, prompted us to choose this technique.
Case description
An 11-year-old female neutered Persian cat was presented to our institution 3 days after the onset of inappropriate defecation and urination. The patient had a 4 year history of polycystic kidney disease (PKD) but was asymptomatic so far.
PKD was diagnosed in this patient 4 years previously, during a routine geriatric check out. Ultrasonography revealed multiple cysts at both kidneys, but no hepatic cyst was detected at that time. Two years later, the kidney cysts were stable in number and size, but two hepatic cysts were detected: one located near the diaphragm, which measured 8.3 mm, and a smaller one (5.2 mm) located in the left side of the liver.
Physical examination at the time of presentation to our institution revealed intense pain on cranial abdominal palpation. Routine haematology, coagulation tests and serum biochemistry were unremarkable, although urinalysis revealed lower-density urine (1020 mg/ml), mild haematuria and microscopic pyuria with intracellular bacilli. A urinary infection was confirmed and treated with amoxicillin–clavulanic acid 20 mg/kg PO q12h for 4 weeks. No urine culture was performed.
Abdominal ultrasonography revealed that the hepatic cyst located in the left side of the liver had increased in size, measured 4.5 cm × 3 cm, and was causing a partial obstruction of the bile duct, which measuring around 3 mm in diameter (Figure 1). The second hepatic cyst had not increased in size. No other causes of cranial abdominal pain were found from the blood results or ultrasound study. Owing to the enlargement of the hepatic cyst and developing clinical signs, surgical excision of the hepatic cyst was recommended through a laparoscopic approach.
Figure 1.
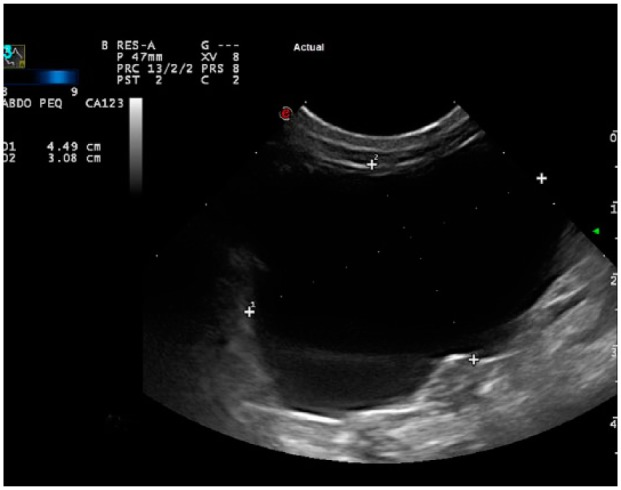
Ultrasonographic image of the hepatic cyst (4.5 cm × 3 cm)
The patient was placed under general anaesthesia and positioned in dorsal recumbency. A three-port technique was chosen introducing a Veress needle through the linea alba, 1 cm caudal to the umbilicus. A pneumo peritoneum was established using carbon dioxide via the Veress needle with a mechanical insufflator, until reaching an intra-abdominal pressure of 8 mmHg, which was maintained throughout the surgical procedure. Next, a 5 mm camera port was placed at the same position as the Veress needle. A 5 mm 30° laparoscope was inserted into the abdomen. The other two 5 mm portals for instrumentation were established under direct visualisation: one 5 cm lateral and 3 cm cranial to the umbilicus on the left side; and the other one 3 cm lateral and 3 cm cranial to the umbilicus on the right side, in a triangulating pattern.
Initially, a limited exploration of the abdomen was performed, with particular attention being paid to the liver. A large hepatic cyst was identified in the right cranial abdomen, which originated from the left medial hepatic lobe (Figure 2); a major part of the surface area of the cyst was projected beyond the hepatic parenchyma, while a minor part was causing a cavity in the liver. Two additional small cysts were seen during liver examination, but no other gross abnormalities were observed.
Figure 2.
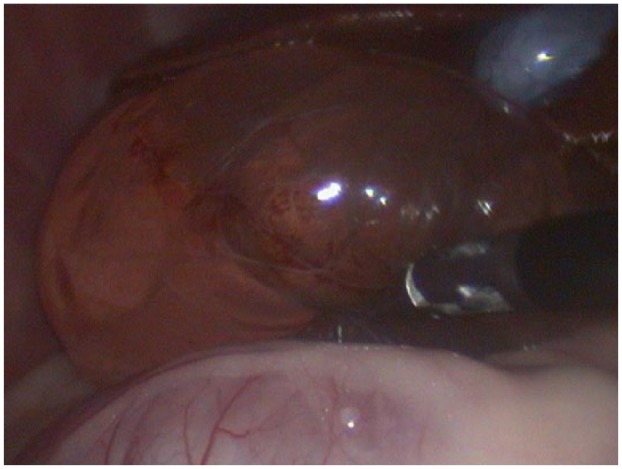
Laparoscopic visualisation of the hepatic cyst originated from the left medial hepatic lobe
An assistant was holding the camera and the surgeon used the other two ports for the laparoscopic instruments. Once adequate visualisation was obtained, a free area of the cystic wall was gently grasped using 5 mm laparoscopic grasping forceps. The Veress needle was used to puncture the cyst and aspirate its contents using an aspiration tube, to minimise intraperitoneal spillage. The cyst fluid was clear and translucent.
The protruding cyst wall was dissected using a 5 mm laparoscopic vessel sealer/divider device (Figure 3) and the part of the cyst lining that was in contact with the hepatic parenchyma was left in situ. The portion dissected of the cyst was removed from the abdomen through one of the portals and was submitted for histological study. Because the cyst capsule was not completely removed, an omentopexy within the residual cavity of the cyst was performed using 4-0 USP braided absorbable material (Polyglactin 910) (Figure 4) in a simple interrupted pattern. The three portals were removed, and abdominal incisions were closed in three layers using a 3/0 USP monofilament absorbable material (glycolic acid).
Figure 3.
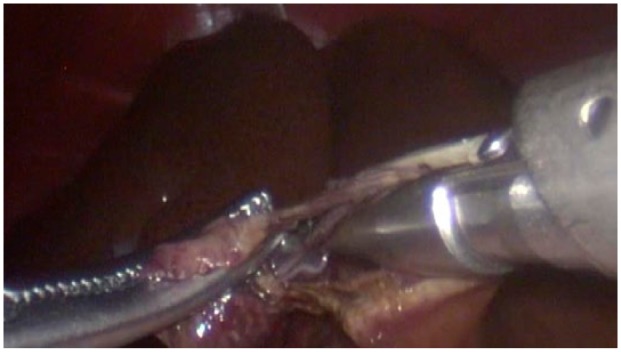
Cyst dissection using a 5 mm laparoscopic vessel sealer/divider device
Figure 4.
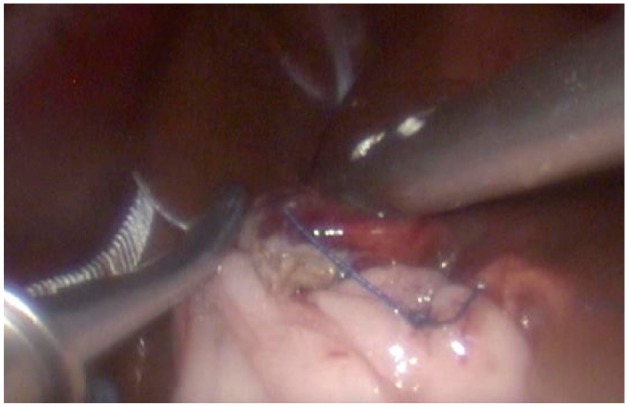
Omentopexy of the residual cystic wall using 4-0 USP in a simple interrupted pattern
The anaesthetic recovery was uneventful and the cat was hospitalised for 12 h. Postoperative care in our hospital included close monitoring, Ringer’s lactate fluid therapy, methadone 0.2 mg/kg SC q6h, which was changed to 20 µg/kg buprenorphine SL q8h for 3 days after discharge, and continuation of amoxicillin–clavulanic acid 20 mg/kg PO q12h for 4 weeks for the urinary infection.
At follow-up examination 5 days later, the patient was bright and alert, physical examination was normal and abdominal palpation was not painful.
Histopathological study showed a cyst wall covered internally by a flattened epithelial layer, supported by a thin band of loose connective tissue, and small clusters of vacuolised hepatocytes, with distended sinusoidal walls. These findings confirmed the diagnosis of a liver epithelial cyst, excluding a neoplastic lesion.
At the 6 month follow-up after surgery, there was no evidence of abdominal pain or other clinical signs. The abdominal ultrasonography revealed no recurrence of the liver cyst. The small liver cyst seen during the laparoscopy was stable and measured 4.9 mm × 10.6 mm, but the cyst near the diaphragm had increased to 2.8 cm × 1 cm.
Discussion
Liver cysts are uncommon in cats and clinical signs are not usually present, but in some cases a variety of signs may occur, such as abdominal pain, vomiting or jaundice. Treatment decisions should be taken bearing in mind the size of the lesion and the clinical signs. In this case, surgical intervention was considered necessary owing to the enlargement of the cyst accompanied by severe abdominal pain and partial obstruction of the biliary duct.
Currently the most successful treatment options described in veterinary medicine for liver cysts are partial or complete excision combined with omentalisation or ultrasound-assisted drainage and alcoholisation of hepatic cysts.2,4 Although successful ultrasound-assisted drainage and alcoholisation of cysts has been reported in veterinary medicine, the median size of cysts treated by this technique is around 2 cm in cats – which is much smaller than our case.
In human medicine, open fenestration was the most widely used technique, but there is a high risk of symptomatic recurrence and abdominal adhesion development. More recently, laparoscopic fenestration has been described as a safe and effective alternative in patients with a solitary cyst. The advantages include minimal surgical trauma, rapid postoperative recovery and reduced adhesion formation.5,6
Laparoscopic procedures in veterinary surgery are becoming widely applied, although further studies are needed for full evaluation of the advantages and disadvantages of minimally invasive procedures. Some comparative studies of laparoscopic and open ovariohysterectomy have shown decreased pain, less risk of dehiscence and haemorrhage, and less risk of postoperative wound complications with laparoscopic procedures. Other advantages may include decreased postoperative pain and shortened hospitalisation and convalescence times.7–9
There has also been a study in dogs demonstrating that resolution of clinical signs was quicker for patients undergoing laparoscopic cholecystectomy compared with open surgery.10 People also have faster convalescence and shorter hospital stays after laparoscopic cholecystectomy.10
In all cases, the main disadvantages of laparoscopic surgery are longer surgical time and the risk of conversion to open surgery. The first of these may partially relate to the experience of the surgeon and the severity of disease. The second may be associated with inappropriate case selection and lack of clinical experience, as noted in human surgery.
The known advantages of laparoscopic procedures meant this was the choice for management of the liver (cyst resection) and subsequent omentalisation in this case.
Laparoscopic hepatic resection has been described in people, especially for the treatment of hydatid liver cysts, whereas laparoscopic hepatic cyst fenestration has become one of the main management in cases of symp tomatic congenital hepatic cysts. Thus, surgical approach mostly depends on cyst aetiology.11
The technique used in hydatid liver cysts does not describe omentalisation, as total epithelial lining of the cyst is removed. In our case, owing to the different aetiology, we only removed the free cyst capsule leaving a small portion of cyst lining in contact with the hepatic parenchyma, and we sealed the cavity left with omentum. Omentopexy is then performed to prevent postoperative adhesions, cyst recurrence and to drain the fluid secreted by the remaining cystic lining.4 The cyst fluid is usually aspirated intraoperatively to avoid the risk of contamination of the abdomen.12 Fluid analysis is recommended to rule out abscesses or parasitic cysts.13 Unfortunately, cyst fluid was not analysed in the present case.
Laparoscopic resection of the hepatic cyst resulted in a very good outcome. Conversion to open surgery was not needed and no complications were found during either the surgery or 6 month follow-up, at the end of which there was no evidence of recurrence.
Minimally invasive surgery is gaining widespread acceptance within the veterinary community because of its benefits, but more techniques should be described and studied for increasing its applications.
Conclusions
To our knowledge, this is the first case report describing laparoscopic liver cystectomy and omentopexy in veterinary medicine. This case demonstrates that the technique can be performed successfully and with a good long-term outcome. To establish precise recommendations and indications for this technique further prospective studies are necessary.
Footnotes
Accepted: 9 November 2018
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for there search, authorship, and/or publication of this article.
References
- 1. Watson PJ. Hepatobiliary diseases in the cat. In Nelson RW, Couto CG. (eds). Small animal internal medicine. 5th ed. St. Louis, Missouri: Elsevier, 2014, pp 536–558. [Google Scholar]
- 2. Zatelli A, D’Ippolito P, Bonfanti U, et al. Ultrasound-assisted drainage and alcoholization of hepatic and renal cysts: 22 cases. J Am Anim Hosp Assoc 2007; 43: 112–116. [DOI] [PubMed] [Google Scholar]
- 3. Eaton KA, Biller DS, DiBartola SP, et al. Autosomal dominant polycystic kidney disease in Persian and Persian-cross cats. Vet Pathol 1997; 34: 117–126. [DOI] [PubMed] [Google Scholar]
- 4. Fried EJ, Niles JD, Williams JM. Omentalisation of congenital liver cysts in a cat. Vet Rec 2001; 149: 275–276. [DOI] [PubMed] [Google Scholar]
- 5. Qiu J, Wu H, Jiang H, et al. Laparoscopic fenestration vs open fenestration in patients with congenital hepatic cysts: a meta-analysis. World J Gastroenterol 2011; 17: 3359–3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pantè S, Di Dio V, Putorti A, et al. Laparoscopic cyst fenestration in the treatment of polycystic liver disease. Ann Ital Chir 2014; 85: 298–303. [PubMed] [Google Scholar]
- 7. Mayhem P. Advanced laparoscopic procedures (Hepastobiliary, Endocrine) in dogs and cats. Vet Clin Small Anim 2009; 39: 925–939. [DOI] [PubMed] [Google Scholar]
- 8. Davidson EB, Moll HD, Payton ME. Comparison of laparoscopic ovariohysterectomy and ovariohisterctomy in dogs. Vet Surg 2004; 33: 62–69. [DOI] [PubMed] [Google Scholar]
- 9. Devitt CM, Cox RE, Hailey JJ. Duration, complication, stress and pain of open ovariohysterectomy versus a simple method of laparoscopic-assisted ovariohysterectomy in dogs. J Am Vet Med Assoc 2005; 227: 921–927. [DOI] [PubMed] [Google Scholar]
- 10. Scott J, Singh A, Mayhew P, et al. Perioperative complications and outcome of laparoscopic cholecystectomy in 20 dogs. Vet Surg 2016; 45 S1: O49–O59. [DOI] [PubMed] [Google Scholar]
- 11. Li H, Shao Y, Aji T, et al. Laparoscopic approach for total cystectomy in treating hepatic cystic echicococcosis. Parasite 2014; 21: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Klinger PJ, Gadenstätter M, Schmid T, et al. Treatment of hepatic cyst in the era of laparoscopic surgery. Br J Surg 1997; 84: 438–444. [PubMed] [Google Scholar]
- 13. Proverbio D, Spada E, Faverzani S, et al. Multiple hepatic vascular cysts in a young ragdoll cat. Vet Rec 2008; 163: 748–749. [PubMed] [Google Scholar]