Abstract
Mindfulness meditation interventions – which train skills in monitoring present-moment experiences with a lens of acceptance – have shown promise for increasing positive emotions. Using a theory-based approach, we hypothesized that learning acceptance skills in mindfulness interventions helps people notice more positive experiences in daily life, and tested whether removing acceptance training from mindfulness interventions would eliminate intervention-related boosts in positive affect. In two randomized controlled trials (RCTs) of stressed community adults, mindfulness skills were dismantled into two structurally equivalent interventions: (1) training in both monitoring and acceptance (Monitor+Accept) and (2) training in monitoring only (Monitor Only) without acceptance training. Study 1 tested 8-week group-based Monitor+Accept and Monitor Only interventions compared to a no treatment control group. Study 2 tested 2-week smartphone-based Monitor+Accept and Monitor Only interventions compared to an active control training. In both studies, end-of-day and momentary positive affect and negative affect were measured in daily life for three days pre- and post-intervention using ambulatory assessments. As predicted, across two RCTs, Monitor+Accept training increased positive affect compared to both Monitor Only and control groups. In Study 1, this effect was observed in end-of-day positive affect. In Study 2, this effect was found in both end-of-day and momentary positive affect outcomes. In contrast, all active interventions in Studies 1 and 2 decreased negative affect. These studies provide the first experimental evidence that developing an orientation of acceptance toward present-moment experiences is a central mechanism of mindfulness interventions for boosting positive emotions in daily life.
Keywords: mindfulness, positive affect, acceptance, mechanisms, ambulatory assessment
“When you observe things through the lens of mindfulness… you invariably begin to appreciate things in a new way because your very perceptions change.” – Kabat-Zinn (1990)
Happiness is a fundamental value pursued by people across time and culture (Kesebir & Diener, 2008). Key to happiness is the experience of positive emotions, which encourage better relationships, career success, and longer, healthier lives (Lyubomirsky, King, & Diener, 2005). For example, positive affect – independent of negative affect – encourages meaning in life (King, Hicks, Krull, & Del Gaiso, 2006) and satisfaction with life (Cohn, Fredrickson, Brown, Mikels, & Conway, 2009), fosters resilience to stress (Ong, Bergeman, Bisconti, & Wallace, 2006), and promotes a broad range of mental and physical health outcomes (e.g., reduced risk for depression, acute illness, systemic inflammation, cardiovascular incidents, and mortality; Wichers et al., 2010; Cohen, Alper, Doyle, Treanor, & Turner, 2006; Cohen, Doyle, Turner, Alper, & Skoner, 2003; Moreno, Moskowitz, Ganz, & Bower, 2016; K. W. Davidson, Mostofsky, & Whang, 2010; Steptoe, Owen, Kunz-Ebrecht, & Brydon, 2004; for reviews, see Marsland, Pressman, & Cohen, 2007; Pressman & Cohen, 2005). Yet paradoxically, the more a person values and seeks happiness, the greater the chance for disappointment, and the less likely happiness is attained (Gruber, Mauss, & Tamir, 2011). At the same time, although not all psychological interventions designed to increase positive affect have been successful (see Parks & Biswas-Diener, 2013), there are several evidence-based interventions for improving happiness (for reviews, see Bolier et al., 2013; Sin & Lyubomirsky, 2009). Particularly promising are interventions that promote hypo-egoic states (e.g., spending money on others, expressing gratitude, performing acts of kindness, practicing lovingkindness meditation; Dunn, Aknin, & Norton, 2008; Emmons & McCullough, 2003; Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008; for reviews, see Brown & Leary, 2016; Sin & Lyubomirsky, 2009).
Among these, mindfulness meditation, which has been described as a practice of (1) monitoring present-moment experiences (2) with an orientation of acceptance (Bishop et al., 2004), has been shown to increase positive affect in daily life (Davis & Zautra, 2013; Fredrickson et al., 2017; Garland, Geschwind, Peeters, & Wichers, 2015; Geschwind, Peeters, Drukker, van Os, & Wichers, 2011). Although mindfulness meditation does not involve intentionally generating positive thoughts and feelings, recent theorizing posits that positive affect, growth, and flourishing can emerge following mindfulness practice (Garland, Farb, Goldin, & Fredrickson, 2015a). Still, little is known about the underlying mechanisms of mindfulness training that promote positive affective experience. How do commonly used mindfulness interventions, which train skills in monitoring and acceptance of present-moment experience, enhance positive affect?
Monitor and Acceptance Theory (MAT) is a new theoretical account that offers two competing predictions about how the basic components of mindfulness interventions – monitoring and acceptance skills – interact to impact affective outcomes (Lindsay & Creswell, 2017). This account proposes that on one hand, monitoring by itself might be enough to boost positive affect: practice in maintaining ongoing awareness of present-moment sensory and perceptual experiences might enhance the vividness of affective stimuli, both positive and negative (the Monitor Only hypothesis). On the other hand, both monitoring and acceptance may be necessary: practice in orienting toward all momentary sensory experiences with acceptance, openness, and receptivity may facilitate a broadened scope of awareness that affords greater access to positive experience (the Monitor + Accept hypothesis). The opening quote echoes this latter hypothesis, emphasizing how an open and accepting lens changes perceptions in ways that encourage greater appreciation of experiences (Kabat-Zinn, 1990), thus boosting positive affect. To test these competing mechanistic predictions, we conducted two three-arm randomized controlled trials (RCTs) that each compare a full mindfulness intervention (Monitor+Accept) to a mindfulness intervention without acceptance skills training (Monitor Only) and a control intervention (Study 2) or no treatment (Study 1). These studies are the first to experimentally dismantle the underlying mechanisms of mindfulness interventions for promoting positive affect, specifically testing whether training in monitoring skills only is sufficient for increasing positive affect (the Monitor Only hypothesis) or whether training in both monitoring and acceptance are necessary (the Monitor + Accept hypothesis, our primary hypothesis).
Mindfulness and Emotional Experience
Positive emotions serve an important function independent of negative emotions. Positive emotions broaden the scope of attention (Fredrickson & Branigan, 2005), allow for more flexible thoughts and behaviors, and build personal resources that translate to better health, personal fulfillment, and more positive emotions (Fredrickson, 1998). The evolutionary function of positive emotions is thought to be this capacity to build resources, including knowledge, skills, and social connections that improve one’s long-term odds of survival and flourishing (Fredrickson, 1998). Importantly, the presence of positive emotions is more predictive of resilience, life satisfaction, and physical health than the absence of negative emotions (e.g., Cohen et al., 2006; Cohn et al., 2009). Further, the absence or reduction of negative emotions does not necessarily lead to the generation of positive emotions (Watson & Clark, 1997), and negative and positive emotions often exist simultaneously in daily life. For example, in contexts that elicit negative emotions, the ability to access and experience positive affect can buffer against stress (Aschbacher et al., 2012; Ong et al., 2006), aid in the emotional and physiological recovery from stress (Fredrickson & Levenson, 1998; Tugade & Fredrickson, 2004), and promote resilience (Cohn et al., 2009; Folkman & Moskowitz, 2000). All of these outcomes serve to further encourage positive emotions, and positive emotions tune the attentional system to perceive more positive cues (Fredrickson & Joiner, 2002; Garland, Farb, Goldin, & Fredrickson, 2015b). Altogether, interventions that effectively promote positive emotions are of considerable value for supporting health and well-being.
Yet a person’s trait level of positive emotionality may be difficult to change (see Lyubomirsky, Sheldon, & Schkade, 2005). First, there is substantial genetic heritability (~40-50%) in a person’s set level of happiness (e.g., Bartels & Boomsma, 2009). Second, acute changes in happiness in response to external events often return to this set point, an effect known as the ‘hedonic treadmill’ (Brickman & Campbell, 1971; Diener, Lucas, & Scollon, 2006). Despite these challenges to increasing positive emotions, longitudinal evidence suggests that a subset of people do report increases in happiness (including positive emotional experience) over time (Fujita & Diener, 2005).
Promisingly, mindfulness interventions have shown initial efficacy for increasing positive affect. However, there are some methodological limitations within this small body of literature (Goyal et al., 2014). Evidence that mindfulness interventions increase positive affect largely relies on retrospective reporting of global positive affect (e.g., Bower et al., 2015; Chang et al., 2004; Howells, Ivtzan, & Eiroa-Orosa, 2016; Nyklicek & Kuijpers, 2008; Schroevers & Brandsma, 2010) and few of these studies are well-controlled (cf. Jain et al., 2007; Zautra et al., 2008). Yet retrospective report of global affect is often an inaccurate reflection of experienced emotional states, with negative emotions tending to outweigh positive emotions in memory (Thomas & Diener, 1990). In contrast, ambulatory assessment approaches (Smyth, Juth, Ma, & Sliwinski, 2017) suffer much less from retrospective memory biases, tap affective experiences in real world contexts, and are more predictive of health outcomes (Conner & Feldman Barrett, 2012). To date, three studies have shown that 6- to 8-week mindfulness-based interventions can increase positive affect in daily life in patient populations (depressive symptoms: Geschwind et al., 2011; fibromyalgia: Davis & Zautra, 2013) and in healthy adults (Fredrickson et al., 2017). The current studies extend these findings in two stressed community adult samples. For three days at pre- and post-intervention, a smartphone ambulatory assessment approach was used to measure positive affect in daily life using both ecological momentary assessments (EMA) and diary assessments. Specifically, momentary affective states were assessed repeatedly throughout the day using EMA (e.g., “how positive are you feeling right now?”). Second, specific types of positive affect (happiness, calm, vigor) experienced throughout the day were assessed each evening using end-of-day diaries.
In the same assessment battery, we also tested secondary predictions about how the components of mindfulness training impact momentary negative affect and specific types of negative affect (depression, anxiety, hostility) experienced in daily life. A larger body of research has investigated the effects of mindfulness interventions on decreasing negative affect, with evidence that mindfulness practice from 5 minutes to 8 weeks reduces negative affectivity (Keng, Smoski, & Robins, 2011; Khoury et al., 2013; Schumer, Lindsay, & Creswell, in press). However, some well-controlled studies suggest that mindfulness interventions are no more effective than active control interventions for reducing negative affect (e.g., Davis & Zautra, 2013). It is possible that mindfulness interventions might reduce reactivity to negative emotional experience (e.g., Brown, Goodman, & Inzlicht, 2013), thus reducing negative affect in daily life, but it is also possible that mindfulness interventions have no relative advantage over placebo-matched active control interventions for reducing negative affect. We aimed to address this open question in Study 2.
Psychological Mechanisms: How Monitoring and Acceptance Impact Affective Experience
Mindfulness is a practice of monitoring ongoing experiences as they occur in the present moment (i.e., monitoring), and approaching these experiences with openness, curiosity, and equanimity (i.e., acceptance). Although there are many ways to practice mindfulness, one common illustrative mindfulness meditation practice involves focusing attention on body sensations. Participants are first invited to monitor their momentary body experiences: detecting each sensation as it arises, unfolds, and passes; noting the qualities of each sensation (e.g., muscular, breath, skin, or other physical sensations; emotional sensations of tension or excitement; pressure, pain, or itch; tingling, radiating, or pulsing; patterns of movement or stability); noticing when attention wanders away from body sensations (e.g., to thoughts or external stimuli); and bringing attention back to monitoring body sensations. It is common for the mind to drift away from focusing on the body, and practice in repeatedly bringing attention back to the body develops skill in monitoring. It is also common for monitoring practice to be effortful, uncomfortable, or frustrating as attention continues to wander or narrow in on feelings of agitation or discomfort in the body. When these emotional reactions and evaluations occur, participants are trained to bring an accepting orientation to their experience, allowing these distractions to occur in the background while gently refocusing attention on present-moment body experience. Acceptance is described as a permission to fully experience what’s happening as it happens without getting caught up in or attached to the content of what’s happening (i.e., non-interference with pleasant and unpleasant sensory experience alike; Desbordes et al., 2015; Young, 2016). Practice involves welcoming all types of body sensations into awareness with a detached interest; allowing each sensation to occur, unfold, and pass without evaluating or trying to change it; and maintaining an attitude of gentle matter-of-factness when attention wanders away and is brought back to the body. Acceptance is a middle way between suppression (i.e., attempting to avoid or deny unpleasant experiences like itches or pain) and identification (i.e., fixating or holding on to certain experiences) with sensory experiences. Metaphorically, acceptance is the psychological equivalent of reducing friction in a mechanical system, reducing resistance in an electrical circuit, or reducing stiffness in a spring (Young, 2016). Experientially, orienting toward one’s experience with acceptance creates a sense of openness, broadening the scope of awareness and freeing attention to notice and savor pleasant experiences in the moment.
In addition to formal meditation practice, monitoring and acceptance skills can also be intentionally practiced in daily life by bringing receptive attention to ongoing experience while doing a routine activity (e.g., washing dishes). Over time, this way of mindfully relating to experiences may begin to arise automatically. Mindfulness skills contrast with common tendencies to become lost in thought (in opposition to present-focused monitoring skills) and to evaluate and engage with the content of thoughts and feelings (in opposition to acceptance skills). Indeed, rather than approaching all experiences with openness and acceptance regardless of their valence (Desbordes et al., 2015), people often attempt to chase after or prolong positive experiences and fixate on or suppress negative experiences in accordance with their self-views (e.g., Swann, 1983). These tendencies are magnified during periods of stress, which tends to narrow attention to focus on stress-relevant stimuli to the exclusion of pleasant and neutral stimuli (Derryberry & Tucker, 1994). In all of these cases, acceptance begins to transform how one relates to present-moment experiences, ultimately changing the scope of attention and the nature of experience. By not over- or under-identifying with affective experiences, acceptance facilitates a broadening of awareness to include a wide array of positive stimuli that can be monitored and appreciated in the moment. Mindfulness is not about chasing happiness, but this lack of attachment to emotion-enhancing goals may be precisely why it is effective.
Attention monitoring and acceptance are the two basic components described in numerous scientific definitions of mindfulness (e.g., Bishop et al., 2004) and the two unique elements of mindfulness interventions that distinguish them from other therapeutic interventions (Lindsay & Creswell, 2017). Although mindfulness is canonically described as a state of clear awareness (Quaglia, Brown, Lindsay, Creswell, & Goodman, 2014), acceptance training is considered an integral part of third-wave acceptance- and mindfulness-based interventions (Hayes, 2004; Mennin, Ellard, Fresco, & Gross, 2013). The present dismantling studies are the first to experimentally test the role of acceptance training on affective processes by removing acceptance instruction from mindfulness interventions.
MAT offers two competing predictions about how monitoring and acceptance skills impact affective experience: the Monitor Only hypothesis and the Monitor + Accept hypothesis. First, the Monitor Only hypothesis posits that learning to monitor present-moment experiences by itself enhances both positive and negative affect (Lindsay & Creswell, 2017). By bringing greater awareness to present-moment sensory experiences (e.g., body sensations, mental images and dialogue, sounds in the environment), attention monitoring has been theorized to intensify both positive and negative affective experiences (Lindsay & Creswell, 2017). The self-reported trait tendency to monitor present experiences, operationalized as scoring higher on the “Observing” subscale of the Five Facet Mindfulness Questionnaire (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006), has been associated with greater psychological distress among non-meditators (e.g., Brown, Bravo, Roos, & Pearson, 2015; Desrosiers, Vine, Curtiss, & Klemanski, 2014; Hamill, Pickett, Amsbaugh, & Aho, 2015; Pearson, Lawless, Brown, & Bravo, 2015). In some cases, however, this tendency has also been associated with positive happiness-related outcomes (e.g., higher satisfaction with life and personal growth; Chopko & Schwartz, 2009; Christopher & Gilbert, 2010). Moreover, at the within-person level, at moments when people report focusing on the present, they report higher concurrent positive affect (Felsman, Verduyn, Ayduk, & Kross, 2017; Killingsworth & Gilbert, 2010). Still, it is possible that the reverse is also true; positive affect may encourage greater focus on the present moment. Overall, evidence on the affective consequences of monitoring is mixed, linking self-reported monitoring skills to both positive and negative affective outcomes, and highlighting the need for experimental manipulation of monitoring training in isolation. In sum, if the Monitor Only hypothesis is true, learning monitoring skills alone should increase both positive and negative affect relative to control groups, with no added advantage of acceptance skills training for increasing positive affect.
A second possibility – and our primary prediction – is that learning to accept one’s present-moment experiences (i.e., monitoring with acceptance) is key for increasing positive affect through mindfulness interventions (the Monitor + Accept hypothesis). The term “acceptance” is used in a variety of ways in scholarly literature, but as conceptualized here, it is defined as a receptive and nonreactive orientation toward momentary experiences, an attitude that allows all inner and outer experiences—pleasant, unpleasant, or neutral—to arise and pass without interference. There is some indication that experiential acceptance promotes positive emotional experience (Kashdan, Barrios, Forsyth, & Steger, 2006; Kashdan & Breen, 2007; Kratz, Davis, & Zautra, 2007), although acceptance by itself may not be sufficient for enhancing positive affect (Ford, Lam, John, & Mauss, 2017). Instead, MAT posits that monitoring and acceptance skills work synergistically to boost positive emotions (Lindsay & Creswell, 2015). Bringing an attitude of acceptance and receptivity toward momentary experiences may broaden awareness and open individuals to the many positive stimuli available in daily life, increasing positive affect overall. Indeed, though many people report a higher proportion of positive than negative affective experiences in daily life (Carstensen et al., 2011), the tendency to be experientially avoidant or judgmental can reduce one’s capacity to notice and enjoy positive emotions (Machell, Goodman, & Kashdan, 2015). Furthermore, without training in acceptance, practice in monitoring present moment experience may narrow the focus of attention onto negative thoughts and feelings while excluding neutral and pleasant cues that are otherwise available (Derryberry & Tucker, 1994; Farb et al., 2010). Likewise, the desire to prolong positive experiences can also narrow attention in the attempt to cling to remnants of positive moments, again to the exclusion of spontaneous pleasant stimuli (Lindsay & Creswell, 2015). In both cases, attentional biases disrupt the natural flow of affective experience. In contrast, orienting toward all experiences with receptivity, openness, and acceptance may reduce these attentional biases (Kiken & Shook, 2011), broaden awareness (Garland, Hanley, Goldin, & Gross, 2017), and afford greater access to positive stimuli that might otherwise go unnoticed. Allowing oneself to engage and disengage with positive, negative, and neutral experiences equally may make negative experiences less overpowering (Catalino, Arenander, Epel, & Puterman, 2017), and subtle pleasant somatic sensations and emotions may become more perceptible (Farb et al., 2010). Overall, the Monitor + Accept hypothesis predicts that training in both monitoring and acceptance skills should increase positive affect and decrease negative affect relative to monitoring skills training alone and control groups.
Overview of experimental approach
The present studies employed a dismantling paradigm, an approach that has been recommended to identify the active components of mindfulness interventions (Britton et al., 2017; Davidson & Dahl, 2017; Williams et al., 2014; Williams, Russell, & Russell, 2008). Here we experimentally dismantled acceptance training from standard mindfulness interventions to clarify the underlying mechanisms of mindfulness training for increasing positive affective experience. Informed by MAT, we offer two competing predictions. First, our primary prediction is that training in both monitoring and acceptance skills will increase positive affect (and decrease negative affect) compared to training in monitoring skills only, with no advantage of monitoring skills training only over control groups (the Monitor + Accept hypothesis). Alternatively, training in monitoring skills only may be sufficient for increasing positive affect relative to control groups (but may also increase negative affective experiences), with no added benefit of training in both monitoring and acceptance skills for increasing positive affect (the Monitor Only hypothesis).
We concurrently conducted two RCTs to test these hypotheses. In both RCTs, mindfulness instructions were dismantled into two structurally equivalent interventions: (1) Monitor + Accept (MA), which modeled commonly used, secular mindfulness training with instruction in both monitoring and acceptance, and (2) Monitor Only (MO), which involved instruction in monitoring but not acceptance techniques. In Study 1, the interventions were adapted from the 8-week group-based Mindfulness-Based Stress Reduction program (MBSR; Kabat-Zinn, 1982, 1990) and compared to a No Treatment control condition (NT control). In Study 2, we developed three matched 2-week smartphone interventions; MA and MO were based on the Unified Mindfulness system (Young, 2016) and were compared with an active control program that instructed neither monitoring or acceptance (Coping control). This smartphone format provided maximal experimental control in isolating the components of mindfulness training and further controlled for many non-mindfulness-specific treatment components (e.g., placebo expectancies, daily time and effort, instructor effects, social environment).
Both studies used a two-pronged ambulatory assessment approach to assess momentary positive and negative affective states via EMA and discrete types of positive and negative affect (happiness, calm, and vigor; depression, anxiety, and hostility) experienced throughout the day via end-of-day diary. This approach is sensitive to dynamic affective processes that occur in a person’s natural environment, and tested for changes in both momentary and end-of-day positive and negative affect from pre- to post-intervention.
Taken together, these studies allow us to explore questions surrounding theoretically-guided mechanisms of mindfulness training (the role of acceptance in promoting positive affect), training length (whether 2- and 8-week mindfulness trainings produce similar effects), and context (whether at-home smartphone-based mindfulness training is similarly effective as in-person group-based mindfulness training).
Study 1
Study 1 dismantled monitoring and acceptance training components in the standardized 8-week MBSR program, with MA emphasizing acceptance content and acceptance instruction removed from MO. Stressed community adults were randomly assigned to one of three conditions: (1) MA, with instruction in both monitoring and acceptance, (2) MO, with instruction in monitoring only, or (3) NT control, an eight-week waiting period between assessments with no training. Positive and negative affect were assessed in daily life for three days before and after the intervention period using both momentary assessments and end-of-day diaries. Our primary Monitor+Accept prediction was that MA participants would show increases in positive affect relative to MO and NT participants, whereas MO would not differ from NT control participants.
Methods
Participants
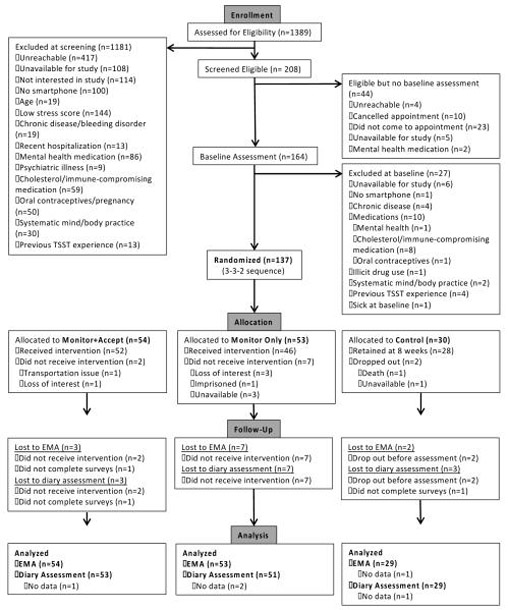
There were 137 stressed community adults between the ages of 18-67 (Mage=381, SD=13) enrolled in the study (see Table 1A for baseline characteristics). Participants were recruited via participant registries, community advertisements, and mass emails to local organizations for a study testing an 8-week training program for stress reduction and well-being. Of the 137 randomized participants, 124 completed at least one post-intervention daily diary and 125 completed at least one post-intervention momentary assessment (see Figure 1A for CONSORT flow chart). N=133 participants were included in diary analyses and 136 were included in momentary assessment analyses.
Table 1.
| A. Baseline characteristics of participants randomized in Study 1. | |||||
|---|---|---|---|---|---|
| Characteristic | Full Sample (N=137) | Monitor + Accept (N=54) | Monitor Only (N=53) | No Treatment (N=30) | Condition Difference |
| Age in yearsa | 37.68 (13.43) | 36.02 (14.35) | 37.58 (12.60) | 40.83 (12.95) | F(2,133)=1.25 |
| Sex | χ2(2)=0.96 | ||||
| Female | 92 (67.15%) | 34 (62.96%) | 36 (67.92%) | 22 (73.33%) | |
| Male | 45 (32.85%) | 20 (37.04%) | 17 (32.08%) | 8 (26.67%) | |
| Race | χ2(8)=7.56 | ||||
| American Indian/Alaska Native | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Asian | 14 (10.22%) | 7 (12.96%) | 6 (11.32%) | 1 (3.33%) | |
| Black/African American | 21 (15.33%) | 10 (18.52%) | 7 (13.21%) | 4 (13.33%) | |
| White/Caucasian | 91 (66.42%) | 33 (61.11%) | 36 (67.92%) | 22 (73.33%) | |
| Bi- or Multi-Racial | 6 (4.38%) | 2 (3.70%) | 1 (1.89%) | 3 (10.00%) | |
| Other | 5 (3.65%) | 2 (3.70%) | 3 (5.66%) | 0 (0.00%) | |
| Ethnicityb | χ2(2)=1.70 | ||||
| Hispanic or Latino | 6 (4.41%) | 3 (5.56%) | 3 (5.66%) | 0 (0.00%) | |
| Not Hispanic or Latino | 130 (95.59%) | 51 (94.44%) | 50 (94.34%) | 29 (96.67%) | |
| Education Level | χ2(16)=11.18 | ||||
| No High School Diploma | 1 (0.73%) | 0 (0.00%) | 1 (1.89%) | 0 (0.00%) | |
| GED | 2 (1.46%) | 1 (1.85%) | 1 (1.89%) | 0 (0.00%) | |
| High School Diploma | 10 (7.30%) | 4 (7.41%) | 3 (5.66%) | 3 (10.00%) | |
| Technical Training | 2 (1.46%) | 0 (0.00%) | 1 (1.89%) | 1 (3.33%) | |
| Some College, no degree | 18 (13.14%) | 9 (16.67%) | 4 (7.55%) | 5 (16.67%) | |
| Associate Degree | 10 (7.30%) | 3 (5.56%) | 5 (9.43%) | 2 (6.67%) | |
| Bachelor’s Degree | 41 (29.93%) | 19 (35.19%) | 17 (32.08%) | 5 (16.67%) | |
| Master’s Degree | 40 (29.20%) | 12 (22.22%) | 17 (32.08%) | 11 (36.67%) | |
| MD, PhD, JD, PharmD | 13 (9.49%) | 6 (11.11%) | 4 (7.55%) | 3 (10.00%) | |
| B. Baseline characteristics of participants randomized in Study 2. | |||||
|---|---|---|---|---|---|
| Characteristic | Full Sample (N=153) | Monitor + Accept (N=58) | Monitor Only (N=58) | Control (N=37) | Condition Difference Statistic |
| Age in years | 32.42 (13.68) | 32.76 (14.21) | 32.64 (12.93) | 31.54 (14.31) | F(2,150)=0.10 |
| Sex | χ2(2)=0.75 | ||||
| Female | 103 (67.32%) | 39 (67.24%) | 41 (70.69%) | 23 (62.16%) | |
| Male | 50 (32.68%) | 19 (32.76%) | 17 (29.31%) | 14 (37.84%) | |
| Race | χ2(8)=14.49 | ||||
| American Indian/Alaska Native | 1 (0.65%) | 0 (0.00%) | 0 (0.00%) | 1 (2.70%) | |
| Asian | 33 (21.57%) | 15 (25.86%) | 13 (22.41%) | 5 (13.51%) | |
| Black/African American | 33 (21.57%) | 14 (24.14%) | 16 (27.59%) | 3 (8.11%) | |
| White/Caucasian | 81 (52.94%) | 28 (48.28%) | 28 (48.28%) | 25 (67.57%) | |
| Bi- or Multi-Racial | 5 (3.27%) | 1 (1.72%) | 1 (1.72%) | 3 (8.11%) | |
| Ethnicity | χ2(2)=1.40 | ||||
| Hispanic or Latino | 7 (4.58%) | 2 (3.45%) | 2 (3.45%) | 3 (8.11%) | |
| Not Hispanic or Latino | 146 (95.42%) | 56 (96.56%) | 56 (96.56%) | 34 (91.89%) | |
| Education Level | χ2(14)=14.26 | ||||
| GED | 3 (1.96%) | 1 (1.72%) | 1 (1.72%) | 1 (1.72%) | |
| High School Diploma | 20 (13.07%) | 9 (15.52%) | 10 (17.24%) | 1 (2.70%) | |
| Technical Training | 1 (0.65%) | 1 (0.65%) | 0 (0.00%) | 0 (0.00%) | |
| Some College | 41 (26.80%) | 15 (25.86%) | 12 (20.69%) | 14 (37.84%) | |
| Associate Degree | 10 (6.54%) | 4 (6.90%) | 2 (3.45%) | 4 (10.81%) | |
| Bachelor’s Degree | 48 (31.37%) | 15 (25.86%) | 21 (36.21%) | 12 (32.43%) | |
| Master’s Degree | 26 (16.99%) | 10 (17.24%) | 11 (18.97%) | 5 (13.51%) | |
| MD, PhD, JD, PharmD | 4 (2.61%) | 3 (5.17%) | 1 (1.72%) | 0 (0.00%) | |
Note: Data are reported as means (SD) or numbers (%).
Age missing from one participant in the Monitor Only condition (N=136).
Ethnicity missing from one participant in the No Treatment condition (N=136).
p<.05
Figure 1.
A. Study 1 CONSORT flow chart.
B. Study 2 CONSORT flow chart.
Note: EMA = Ecological Momentary Assessment.
The study design and outcomes described here were pre-registered with Clinical Trials identifier NCT02502227; hypotheses were guided by MAT (Lindsay & Creswell, 2015, 2017). This report describes positive and negative affect outcome data from ambulatory assessments at baseline and post-intervention. Eligible participants were fluent English-speaking smartphone owners (Android or iPhone) between the ages of 18-70 years who scored >5 on the 4-item Perceived Stress Scale (reflecting higher-than-average perceived stress; Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988; Warttig, Forshaw, South, & White, 2013). As blood and saliva samples were collected in the parent trial, participant exclusion criteria included: chronic mental or physical disease; hospitalization for mental or physical illness in the past 3 months; medication use that interferes with hypothalamic-pituitary-adrenal axis (HPA) or immune system functioning; current antibiotic, antiviral, or antimicrobial treatment; current oral contraceptive use or pregnancy; recreational drug use; and bloodborne pathogen risk due to travel to countries on the CDC travel alert list in the past 6 months. Finally, in order to test the effects of developing mindfulness skills in a novice population, those reporting a regular systematic mindfulness meditation or related mind-body practice (>2 times per week or >90 minutes per week) were excluded. Written informed consent was obtained from all participants, and all study procedures were approved by the Carnegie Mellon University IRB. Study data was collected between August 2015 and November 2016. Trial enrollment concluded as planned following the launch of the third cohort because recruitment goals had been reached.
The sample size was determined based on power calculations for primary stress reduction outcomes of the larger trial. Specifically, previous mindfulness interventions have demonstrated medium-large effect sizes (~η2=0.06-0.18) for both daily stress (pre-post 8-week mindfulness intervention: Carson, Carson, Gil, & Baucom, 2004) and stress reactivity outcomes (post 3-session mindfulness vs. active control intervention: Creswell, Pacilio, Lindsay, & Brown, 2014). Based on pilot data available at the time of grant writing that compared brief MA vs. MO interventions (Rahl, Lindsay, Pacilio, Brown, & Creswell, 2017), we conservatively estimated a small effect size (η2=0.02) for comparing the two active mindfulness training programs on changes in psychological stress (i.e., a group × time interaction). We estimated a pre-post correlation of .60 and a conservative two-tailed Type I error rate of .05. To achieve 90% power, G*Power calculated a total of N=120 participants needed to test the primary study aims using omnibus tests. The ambulatory assessment data reported here were not analyzed until the complete dataset was collected.
Additionally, power was maximized by encouraging adherence to the interventions and compliance to the outcome assessments. Adherence was encouraged through reminder phone calls and text messages, as well as monetary incentives. Participants in the intervention programs received $50 for attending 4 classes, $75 for attending 6 classes, $125 for attending 8 classes. To encourage compliance with ambulatory assessments, participants received $15 base compensation plus an additional maximum of $15 for compliance with the ambulatory assessment protocols at baseline and $45 base compensation plus an additional maximum of $25 for compliance at post-intervention.
Procedure
Overview
As part of a three-arm randomized controlled trial, interested participants completed screenings for eligibility both via telephone and at an in-person baseline appointment. During this baseline appointment, eligible participants provided a dried blood spot (DBS) sample, completed a questionnaire and task battery, and were oriented to the study’s schedule and activities. Participants then completed three consecutive days of pre-intervention ecological momentary assessments (EMA) and daily diary assessments (see Measures). Next, participants were allocated into one of three study conditions using a computerized random number generator in simple randomization with a 3:3:2 ratio, with the ratios corresponding to MA, MO, and NT, respectively. Randomization procedures were implemented separately for each cohort (N=42; N=55; N=40). Allocation sequence was concealed, such that only author AGCW had access to the sequence and otherwise was not involved with the running of the study and had no contact with participants other than to assign them to the next condition in the randomization sequence. At the end of classes 1, 4 and 8 of the intervention, participants in the active treatment groups completed a questionnaire battery that included a measure of Treatment Expectancies (see Measures). Immediately following the last class of the 8-week intervention period (see Intervention Programs), participants completed three consecutive days of post-intervention EMA and diary assessments. Finally, participants returned to the laboratory for a post-intervention assessment and to be debriefed, informed of the study’s primary aims, and compensated for their participation. Other outcomes from this trial will be reported in separate papers.
Ecological Momentary Assessment and Diary Assessments
Ambulatory assessment approaches sample participants’ experiences in their natural environment, and are sensitive to dynamic and transient affective processes in daily life (Shiffman, Stone, & Hufford, 2008). A two-pronged ambulatory assessment approach was used to measure both momentary affective states (EMA) and end-of-day positive and negative affect (diary). EMA provided snapshots of state affect in real time whereas daily diary assessments measured specific types of positive and negative affect experienced throughout the day (see Measures).
Both EMA and daily diary assessments were administered on participants’ personal smartphones using Qualtrics software delivered through SurveySignal text links (Cohort 1; Cohorts 2 & 3 post-intervention surveys) or MetricWire software (Cohorts 2 & 3 baseline surveys) 2. Participants were prompted to complete EMA surveys at five quasi-random times each day (yielding up to 30 momentary assessments in total across the pre- and post-intervention period). Text links were sent during each of five 2-hour blocks distributed between 9:00am and 7:00pm, with links expiring after 45 minutes. Participants were prompted to complete daily diary surveys at 8:30pm each day (providing up to 6 daily diary assessments in total across pre- and post-intervention); links were sent at 8:30pm and remained active until 11:30pm. Participants were trained on how to complete ambulatory assessment items during the baseline study appointment. For both pre- and post-intervention ambulatory assessments, sampling began on a Wednesday and concluded on a Friday.
Materials
Intervention Programs
Participants were randomly assigned to one of three study conditions: 8-week Monitor+Accept MBSR intervention (MA; the standard MBSR intervention), 8-week Monitor Only modified MBSR intervention (MO), or a no treatment control condition (NT). The MA and MO intervention programs are described in detail below.
The study was run in three cohorts ranging in size from 40-55 participants. Intervention class sizes ranged from 15-22 participants. All classes were taught by two instructors (authors CG and DB) who were counterbalanced across cohorts (MA was taught by DB in Cohorts 1 and 3 and by CG in Cohort 2; MO was taught by CG in Cohorts 1 and 3 and by DB in Cohort 2). Both instructors maintained their own personal meditation practice (23 years, 10 years) and were Certified (CG) or Qualified (DB) MBSR teachers who had completed all MBSR teacher-training programs at the University of Massachusetts Center for Mindfulness (see “Center for Mindfulness - UMass Medical School”). Together, they had 16 years of experience teaching MBSR. Because the instructors also developed the modified MO program, they were not completely blind to the general study hypotheses, but were unaware of the specific measures used to test hypotheses.
Monitor & Accept (MA):
The MA program adhered to the MBSR curriculum except for the length of each class, which was 2 hours. MBSR is a standardized group-based program consisting of 8 weekly 2.5-3-hour group sessions, 1 day-long retreat during the sixth week, and approximately 45 minutes of guided home practice six days per week. During each group session, an MBSR instructor leads guided mindfulness meditations intended to (1) foster the ability to intentionally pay attention to, or monitor, one’s present-moment experiences (including pleasant, unpleasant, and neutral experiences), and (2) cultivate an open, accepting, and nonjudgmental attitude while doing so (e.g., “Noticing what is present now, in body sensations, emotions, or thoughts… and allowing it to be there as best we can… not trying to change or improve what is present”). Guidance and group discussions also encourage purposeful attention monitoring with an open, non-interfering attitude in everyday life; over time, unhelpful habits of reacting to stress may be recognized and monitored non-judgmentally (including the habit of self-judgment). Home practice recordings guide participants through body awareness, mindful movement, seated meditation, and brief awareness exercises during daily life. In this study, and in standard MBSR, the instructors followed scripts to record their own home practice audios so that participants could be guided by their regular teacher.
Monitor Only (MO):
The MO program was adapted from the standard MBSR program. Monitoring, or training oneself to sense and observe one’s experience, is explicitly taught in standard MBSR and in the MO intervention in this study. Participants were invited to focus their attention on an aspect of their present moment experience (e.g., breathing or other body sensations). They were asked to notice when their attention wandered, and to return it to the direct perception of the focus object. The MO adaptations of the MBSR program consisted primarily of 1) changes in language and 2) an emphasis on concentration practices rather than open awareness meditation practices. First, changes in language included avoiding use of the phrases: allow, accept, acceptance, being with, letting go of judgment, non-judgment, non-interference, and instead referring to: direct perception, observe, monitor, return to the anchor (e.g., of breath sensation). Second, the MO program emphasized concentration and the development of focused attention and reorienting skills when aware of distraction (e.g., anchoring to breath or body sensation to ‘return home’ to the present moment). Focused attention was also discussed as a resource for coping with stressful events. Choiceless awareness and lovingkindness meditation, practices in the standard MBSR curriculum that emphasize an attitude of acceptance and openness, were not included in the MO program. The amount of class time spent in meditation practice was equivalent in MA and MO programs. MO participants also completed a retreat day and 45 minutes of home practice each day, again guided by standardized recordings from their class instructor. Of note, although the language and practices associated with acceptance were excised as much as possible from MO, the teachers embodied the acceptance and inclusion that are essential to cultivating a safe learning environment for participants.
The MO program was adapted from standard MBSR curriculum by coauthors (CG, DB) in consultation with a former senior teacher at the UMass Center for Mindfulness (Melissa Myozen Blacker, MA, Roshi) and utilizing meditation literature (Foust, 2014; Goenka, 1994; Trungpa, 2005; Young, 2016). To minimize contamination (i.e., acceptance content), a MO curriculum guide was used by both teachers that included learning intentions, themes, session activities, and facilitator intentions. The curriculum guide included specific reminders regarding language and focus on concentration and monitoring practices. The MO teachers recorded meditations for home practice that did not include acceptance language (e.g., letting go of judgment, allowing, accepting, opening to, being with, non-interference). Teachers met briefly prior to each session in order to review curriculum.
No Treatment (NT):
Participants assigned to the no treatment control group completed assessments at baseline and post-intervention (compliance was encouraged through check-in phone calls), and did not receive an intervention program.
Measures
Ecological Momentary Assessment of State Positive and Negative Affect:
Momentary positive and negative affect in daily life were assessed on participants’ smartphones five times daily for three days pre- and three days directly post-intervention. Positive and negative affect were assessed independently using a single item each (“Just before this survey, how [positive/negative] was your emotional state or mood?”). Responses were provided on a 1 (not at all) to 7 (extremely) Likert scale. Higher values indicate higher positive affect or higher negative affect.
Positive and Negative Affect Diary:
Positive and negative affect were assessed in greater detail at the end of each day for three days both pre- and post-intervention using a previously validated scale (Cohen et al., 2003; Usala & Hertzog, 1989). Using a seven-point Likert scale ranging from 1 (not at all) to 7 (extremely), participants rated how well each of 18 adjectives (9 positive adjectives, 9 negative adjectives) described how they felt on average across the entire day. Positive affect adjectives were divided into three subscales: happiness (happy, pleased, cheerful), calm (calm, at-ease, relaxed), and vigor (lively, full-of-pep, energetic). Negative affect adjectives were also divided into three subscales: anxiety (on edge, nervous, tense), depression (sad, depressed, unhappy), and hostility (hostile, resentful, angry). Eight composite affect scales were created: an overall positive affect scale, the average of all nine positive adjectives (average Cronbach’s α=.94 across six daily diary days); an overall negative affect scale, the average of all nine negative adjectives (average α=.88); three positive adjective subscales (average happiness α=.90; average calm α=.88; average vigor α=.89); and three negative affect subscales (average anxiety α=.77; average depression α=.88; average hostility α=.79). Higher values reflect higher positive or negative affect.
Intervention and Home Practice Adherence:
Attendance at each of the eight classes and the day-long retreat was recorded via sign-in sheet. This was used to calculate the total number of classes attended for each participant. Home practice audio files were distributed each day using Qualtrics links that automatically recorded the duration of time each link was open. Durations longer than each audio recording were considered outliers, and were replaced with the actual duration of the audio recording (45 minutes). These daily durations were summed across the eight-week intervention to calculate the total amount of home practice. In addition, the total number of Qualtrics practice sessions was summed to create a second home practice outcome.
Treatment Expectancies:
To evaluate whether the training programs produced equivalent perceived treatment benefits, participants completed an adapted 6-item Credibility/Expectancy Questionnaire (Devilly & Borkovec, 2000) to assess their beliefs about the efficacy of the training program after class at Weeks 1, 4, and 8. Cognitive (e.g., “how successful do you think this program will be in reducing your stress symptoms?”) and emotional (e.g., “how much improvement in your symptoms do you think will occur?”) subscales were averaged to create an overall measure of positive treatment expectancies (Cronbach’s α=.91, .92, and .91 at Weeks 1, 4, and 8 respectively).
Analyses
Overview
Analyses were conducted using SPSS Statistics 24.0 (IBM, Armonk, New York) and Stata 14.2 software (StataCorp, College Station, Texas). Preliminary analyses conducted in SPSS tested for condition differences in demographics and other baseline characteristics using chi-square (for categorical variables) and ANOVA tests (for continuous variables). Cohort (1, 2, or 3) and instructor (0=NT, 1=DB, or 2=CG) were included as covariates in all models; because instructor is collinear with condition in the No Treatment group, the linear form of the instructor variable was entered into models. Treatment expectancies, treatment and homework adherence, and ambulatory assessment compliance were evaluated as covariates using ANOVA to test for significant condition differences.
Ambulatory assessment analyses
To test primary ambulatory assessment predictions, multilevel mixed-effect linear models (MLMs) tested for time (pre or post) × condition (MA, MO, or NT) differences on the primary outcomes using the Stata Mixed procedure. These MLMs also calculate MA vs. MO, MA vs. NT, and MO vs. NT contrasts, which we report following significant time × condition interactions. Ambulatory assessment data have a nested structure; diary outcomes involve multiple observations (level 1) clustered within the same individual (level 2), and momentary assessment outcomes have multiple observations (level 1) collected within day (level 2) clustered within individual (level 3). MLMs are able to capture variability from all sources (within-individual, within-day, and between-individual). MLMs model all available data and provide unbiased estimates for data missing at random; thus, MLMs are robust to missing data.
The assumption of dependence in the data (i.e., that substantial variance exists at each level: within-individual, within-day, between-individual) was tested using unconditional models and examining intraclass correlations (ICCs). For diary-assessed positive and negative affect outcomes, empty 2-level models showed that 33-55% of the total variance occurred between individuals, while 45-67% of the variance occurred within individuals. For EMA affect outcomes, 20-36% of the total variance occurred between individuals, 5-7% was explained at the day-level, and 58-75% of the variance occurred within individuals. The substantial variance present at each level confirmed the dependent nature of the data. Thus, 2-level models were used for daily diary data and 3-level models were used for EMA data. Restricted Maximum Likelihood (REML) estimation was used for all models.
In sum, the diary outcome models followed the general equation:
Level 1:
Level 2:
Reduced from:
with β0i reflecting the intercept of affect for the reference group (MA) at pre-intervention compared to MO and NT, and β1i accounting for time (pre or post) and time × condition interactions. Study condition, cohort, and instructor (which varied at the individual level) were modeled at Level 2. The rti and u0i terms reflect error at the within- and between-subjects levels, respectively.
EMA outcome models followed the general 3-level equation below, which also accounted for the clustering of observations within days. Time of day (first, second, third, fourth, or fifth survey), which varied at the observation level, was included at Level 1 to account for temporal dependency between proximal observations. Study condition, cohort, and instructor were modeled at Level 3. The rtdi, u0di, and u00i terms reflect error at the within-subject, within-day, and between-subject levels, respectively.
Level 1:
Level 2:
Level 3:
Reduced form:
Within-group Cohen’s d effect sizes were calculated by dividing the pre-post mean difference in each condition by that condition’s pre-intervention standard deviation (Morris, 2008) adjusted to account for the overall pre-post correlation for each outcome (see equation 8 in Morris & DeShon, 2002; Wiseheart, 2013). Between-group Hedges’ g effect sizes and confidence intervals were calculated using a bias-corrected equation that divides the differences between two group means (pre-post intervention mean differences) by the pooled standard deviation (using a calculator provided from the Centre for Evaluation & Monitoring, 2018).
Results
Preliminary Analysis
First, success of randomization on major demographic characteristics in the full randomized sample (N=137) was evaluated. There were no baseline differences in age, sex, race, ethnicity, or education between the three conditions (see Table 1A).
Second, condition differences in study attrition, treatment adherence, compliance with the ambulatory assessment protocol, treatment expectancies, and pre-intervention positive and negative affect were tested (see Table 2A). First, 92% of randomized participants completed the study, with no condition differences in number of drop-outs (χ2(2)=3.37, p=.186). Of the 107 participants assigned to one of the two study interventions, 98 completed the intervention (91.6%). Participants who completed the intervention were highly adherent, with no condition differences in the number of classes attended (F(1,96)=0.00, p=.983). On average, participants attended 7.44 of the 9 possible classes (8 weekly classes plus the day-long retreat). Moreover, 81 of 98 participants (82.7%) attended at least 6 of the 9 possible classes and only 9 participants (9.2%) attended fewer than half of the classes. MA participants tended to practice at home more than MO participants over the course of the 8-week intervention (Mdiff = 2.85 hours), but home practice did not significantly differ between conditions (F(1,96)=2.97, p=.088). On average, participants logged 12 hours of home practice (in 26 practice sessions) during the 8-week intervention period. Controlling for total duration of home practice (in minutes) or frequency of home practice (in days) did not impact the results reported below.
Table 2.
| A. Adherence, treatment expectancies, and pre-intervention outcomes of participants in Study 1. | |||||
|---|---|---|---|---|---|
| Characteristic | Full Sample (N=137) | Monitor + Accept (N=54) | Monitor Only (N=53) | Control (N=30) | Condition Difference Statistic |
| Intervention Drop-outs | 11 (8.03%) | 2 (3.70%) | 7 (13.21%) | 2 (6.67%) | χ2(2)=3.37 |
| Intervention Adherence (sessions)a | 7.44 (1.72) | 7.44 (1.66) | 7.43 (1.80) | -- | F(1,96)=0.00 |
| Home Practice Adherence (minutes)a | 728.9 (491.6) | 814.5 (490.7) | 643.3 (490.7) | -- | F(1,96)=2.97 |
| Home Practice Adherence (sessions)a | 25.66 (10.72) | 27.08 (10.69) | 24.24 (10.70) | -- | F(1,96)=1.72 |
| Week 1 Treatment Expectancies b | 6.31 (1.70) | 6.24 (1.70) | 6.38 (1.73) | -- | F(1,98)=0.15 |
| Week 4 Treatment Expectancies c | 6.26 (1.77) | 6.17 (1.76) | 6.36 (1.79) | -- | F(1,93)=0.25 |
| Week 8 Treatment Expectancies d | 6.95 (1.58) | 6.90 (1.67) | 7.00 (1.48) | -- | F(1,93)=0.10 |
| Pre-Intervention Diary Compliance e | 1.80 (1.44) | 1.64 (1.38) | 1.92 (1.39) | 1.83 (1.39) | F(2,130)=0.54 |
| Pre-Intervention EMA Compliance f | 8.39 (5.96) | 8.94 (5.72) | 9.17 (5.72) | 7.07 (5.72) | F(2,133)=1.40 |
| Post-Intervention Diary Compliance e | 2.61 (0.86) | 2.76 (0.83) | 2.55 (0.83) | 2.52 (0.83) | F(2,130)=1.10 |
| Post-Intervention EMA Compliance f | 11.56 (4.44) | 12.41 (4.26) | 10.49 (4.27) | 11.79 (4.27) | F(2,133)=2.77 |
| Pre-Intervention Diary PA (overall)e | 3.35 (1.17) | 3.24 (1.20) | 3.56 (1.39) | 3.18 (1.78) | χ2(2)=1.76 |
| Pre-Intervention EMA PA f | 3.77 (1.06) | 3.79 (1.08) | 3.76 (1.23) | 3.77 (1.66) | χ2(2)=0.03 |
| Pre-Intervention Diary NA (overall)e | 2.38 (0.85) | 2.45 (0.88) | 2.37 (1.03) | 2.25 (1.26) | χ2(2)=0.70 |
| Pre-Intervention EMA NA f | 2.23 (0.72) | 2.26 (0.72) | 2.16 (0.84) | 2.32 (1.11) | χ2(2)=0.56 |
| B. Adherence, treatment expectancies, and pre-intervention outcomes of randomized participants in Study 2. | |||||
|---|---|---|---|---|---|
| Characteristic | Full Sample (N=153) | Monitor + Accept (N=58) | Monitor Only (N=58) | Control (N=37) | Condition Difference Statistic |
| Intervention Drop-outs | 3 (1.96%) | 1 (1.72%) | 2 (3.45%)) | 0 (0.00%) | χ2(2)=1.42 |
| Intervention Adherence (lessons)g | 13.49 (1.20) | 13.44 (1.52) | 13.60 (0.91) | 13.39 (1.04) | F(2,146)=0.40 |
| Treatment Expectancies h | 5.37 (1.90) | 5.71 (1.77) | 5.26 (2.02) | 5.05 (1.86) | F(2,146)=1.55 |
| Pre-Intervention Diary Compliance i | 2.87 (0.43) | 2.81 (0.43) | 2.91 (0.42) | 2.89 (0.43) | F(2,149)=0.90 |
| Pre-Intervention EMA Compliance | 10.81 (1.35) | 10.71 (1.32) | 10.90 (1.32) | 10.84 (1.32) | F(2,150)=0.31 |
| Post-Intervention Diary Compliance i | 2.80 (0.62) | 2.76 (0.60) | 2.83 (0.60) | 2.81 (0.60) | F(2,149)=0.19 |
| Post-Intervention EMA Compliance | 10.14 (2.41) | 9.98 (2.36) | 10.02 (2.36) | 10.41 (2.36) | F(2,150)=0.42 |
| Ambulatory Assessment Counterbalance | χ2(2)=3.10 | ||||
| Pre: Thurs-Sat; Post: Sun-Tues | 103 (67.32%) | 44 (75.86%) | 36 (62.07%) | 23 (62.16%) | |
| Pre: Sun-Tues; Post: Thurs-Sat | 50 (32.68%) | 14 (24.14%) | 22 (37.95%) | 14 (37.84%) | |
| Pre-Intervention Diary PA (overall)i | 3.40 (1.01) | 3.40 (1.00) | 3.31 (1.00) | 3.54 (1.00) | χ2(2)=1.20 |
| Pre-Intervention EMA PA | 3.90 (0.96) | 3.95 (0.96) | 3.81 (0.95) | 3.96 (0.95) | χ2(2)=0.89 |
| Pre-Intervention Diary NA (overall)i | 2.18 (0.78) | 2.10 (0.77) | 2.31 (0.77) | 2.11 (0.77) | χ2(2)=2.62 |
| Pre-Intervention EMA NA | 2.16 (0.70) | 2.08 (0.70) | 2.24 (0.70) | 2.16 (0.70) | χ2(2)=1.57 |
Note: Data are reported as means (SD) or numbers (%). Intervention Drop-outs is reported as number of drop-outs at the completion of the intervention period. Ambulatory Assessment Compliance is reported as number of surveys completed; in Study 1, there were 15 possible EMA surveys and 3 possible diary surveys at pre- and post-intervention, and in Study 2, there were 12 possible EMA surveys and 3 possible diary surveys at pre- and post-intervention. EMA = Ecological Momentary Assessment, PA = Positive Affect, NA = Negative Affect.
N=98 (MA N=52; MO N=46).
N=100 (MA N=52; MO N=48).
N=95 (MA N=50; MO N=45).
N=95 (MA N=51; MO N=44).
N=133 (MA N=53; MO N=51; NT N=29).
N=136 (MA N=54; MO N=53; NT N=29).
N=150 (MA N=57; MO N=56; Control N=37).
N=149 (MA N=56; MO N=56; Control N=37).
N=152 (MA N=58; MO N=57; Control N=37).
p<.05
There were no condition differences in compliance with the ambulatory assessment protocols at baseline (F(2,133)=0.91, p=.404) or post-intervention (F(2,133)=2.49, p=.087). In total, participants included in analyses completed 58% of surveys at baseline and 79% at post-intervention. Conditions were equivalent in baseline EMA and diary-assessed positive and negative affect ratings (Table 2A). Finally, treatment expectancy data was available from 93% of MA and MO participants at Week 1, 89% at Week 4, and 89% at Week 8. There were no differences in treatment expectancies between MA and MO participants at any time point (Week 1: F(1,98)=0.15, p=.700; Week 4: F(1,93)=0.25, p=.617; Week 8: F(1,93)=0.10, p=.758), indicating that both groups had similar perceptions of treatment benefits throughout the intervention period.
Primary Analysis
This study predicted that MA participants would show increases in positive affect (primary Monitor + Accept hypothesis) and decreases in negative affect (secondary Monitor + Accept hypothesis) in daily life compared to MO and NT participants, and that MO and NT participants would not differ. To evaluate these predictions, we used MLMs to test for time × condition interactions on end-of-day diary-assessed affect composites and momentary affect using all available data. When significant time × condition interactions were present, we report MA vs. MO, MA vs. NT, and MO vs. NT contrasts.
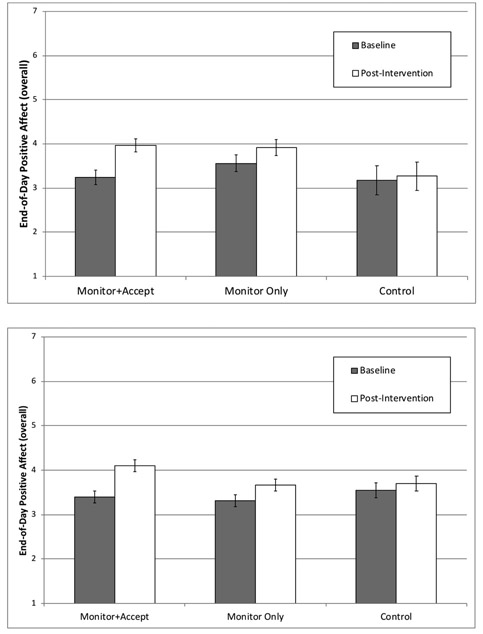
Positive affect
In end-of-day diary analyses, an MLM revealed a significant main effect of time (χ2(1)=25.01, p<.0005), no main effect of study condition across time points (χ2(2)=1.48, p=.477), and, consistent with predictions, a significant time × condition interaction for overall positive affect (χ2(2)=10.82, p=.005). Figure 2A depicts this interaction (see Table 3A for full MLM results). Both MA- and MO-trained participants showed significant increases in overall positive affect from baseline to post-intervention (MA mean change=0.71, p<.0005, d=.70; MO mean change=0.36, p=.003, d=.32) whereas control participants did not (NT mean change=0.08, p=.583, d=.06) (see Table 5A). As predicted by the Monitor+Accept hypothesis, MA participants showed significantly greater increases in overall positive affect compared to MO (χ2(1)=4.12, p=.043, g=.40) and NT participants (χ2(1)=10.35, p=.001, g=.73) (see Figure 3), whereas MO and NT participants did not differ (χ2(1)=2.02, p=.155, g=.33).
Figure 2.
A. Study 1 diary-assessed positive affect (overall) at baseline and post-intervention by study condition.
B. Study 2 diary-assessed positive affect (overall) at baseline and post-intervention by study condition.
Table 3.
| A. Multilevel mixed effects linear model results for diary-assessed Positive and Negative Affect (overall) in Study 1. | ||||
|---|---|---|---|---|
| Positive Affecta B (SE) | z | Negative Affecta B (SE) | z | |
| Interceptb (γ00) | 3.32 (.35) | 9.49* | 2.59 (.24) | 10.82* |
| Time (pre vs. post) (γ10) | 0.71 (.12) | 5.86* | −0.54 (.11) | −4.91* |
| Condition | ||||
| MA vs. MO (γ01) | 0.32 (.24) | 1.31 | −0.07 (.18) | −0.41 |
| MA vs. NT (γ02) | −0.06 (.39) | −0.16 | −0.20 (.27) | −0.74 |
| Condition × Time | ||||
| MA vs. MO × pre vs. post (γ11) | −0.35 (.17) | −2.03* | 0.25 (.16) | 1.59 |
| MA vs. NT χ pre vs. post (γ12) | −0.63 (.20) | −3.22* | 0.52 (.18) | 2.93* |
| Cohort | ||||
| 2 (γ03) | 0.01 (.22) | 0.05 | 0.09 (.15) | 0.60 |
| 3 (γ04) | 0.21 (.22) | 0.95 | 0.01 (.15) | 0.03 |
| Instructor (γ05) | −0.13 (.21) | −0.61 | −0.14 (.15) | −0.92 |
| Estimate | 95% CI | (.15) Estimate | 95% CI | |
| Within-subjects error (rti) | 0.63 (.04) | 0.55, 0.72 | 0.53 (.04) | 0.46, 0.60 |
| Between-subjects error (u0i) | 0.88 (.13) | 0.65, 1.18 | 0.35 (.06) | 0.25, 0.49 |
| B. Multilevel mixed effects linear model results for diary-assessed Positive and Negative Affect (overall) in Study 2. | ||||
|---|---|---|---|---|
| Positive Affectc B (SE) | z | Negative Affectc B (SE) | z | |
| Interceptd (γ00) | 3.31 (.15) | 21.76* | 2.13 (.12) | 17.85* |
| Time (pre vs. post) (γ10) | 0.70 (.10) | 6.77* | −0.31 (.08) | −3.66* |
| Condition | ||||
| MA vs. MO (γ01) | −0.09 (.19) | −0.46 | 0.21 (.14) | 1.47 |
| MA vs. control (γ02) | 0.15 (.21) | 0.69 | 0.00 (.16) | 0.03 |
| Condition × Time | ||||
| MA vs. MO × pre vs. post (γ11) | −0.35 (.14) | −2.48* | 0.03 (.12) | 0.27 |
| MA vs. control × pre vs. post (γ12) | −0.54 (.16) | −3.39* | 0.22 (.13) | 1.64 |
| Day of Week | ||||
| Monday (γ20) | −0.12 (.10) | −1.16 | 0.00 (.09) | 0.04 |
| Tuesday (γ30) | −0.02 (.10) | −0.23 | −0.13 (.09) | −1.46 |
| Thursday (γ40) | 0.05 (.11) | 0.43 | 0.07 (.09) | 0.80 |
| Friday (γ50) | 0.21 (.11) | 1.97* | 0.02 (.09) | 0.21 |
| Saturday (γ60) | 0.40 (.11) | 3.72* | −0.14 (.09) | −1.56 |
| Estimate | 95% CI | Estimate | 95% CI | |
| Within-subjects error (rti) | 0.77 (.04) | 0.69, 0.86 | 0.52 (.03) | 0.47, 0.58 |
| Between-subjects error (u0i) | 0.72 (.10) | 0.55, 0.95 | 0.40 (.06) | 0.30, 0.54 |
N=129.
Reference group: condition: MA; time: Pre; cohort: 1; instructor: NT.
N=152.
Reference group: condition: MA; time: Pre; day of week: Sunday.
p<.05
Table 5.
| A. Ecological Momentary Assessment (EMA) and diary-assessed Positive Affect (PA) and Negative Affect (NA) in Study 1. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Monitor + Accept (N=54)a | Monitor Only (N=53)b | Control (N=29) | Time × Condition Difference | ||||||
| Pre | Post | d | Pre | Post | d | Pre | Post | d | ||
| Diary Positive Affect | 3.24 (.17) | 3.96 (.15) | .70 | 3.56 (.19) | 3.92 (.18) | .32 | 3.18 (.33) | 3.27 (.32) | .06 | χ2(2)=10.82* |
| Diary PA: Happiness | 3.37 (.18) | 4.06 (.17) | .58 | 3.70 (.22) | 3.98 (.19) | .20 | 3.26 (.36) | 3.40 (.35) | .08 | χ2(2)=6.74* |
| Diary PA: Calm | 3.14 (.18) | 3.94 (.17) | .75 | 3.41 (.21) | 3.99 (.19) | .48 | 2.77 (.36) | 3.01 (.35) | .15 | χ2(2)=6.29* |
| Diary PA: Vigor | 3.24 (.18) | 3.86 (.17) | .56 | 3.56 (.21) | 3.81 (.19) | .20 | 3.51 (.36) | 3.41 (.35) | −.06 | χ2(2)=11.23* |
| EMA Positive Affect | 3.79 (.15) | 4.40 (.14) | .61 | 3.76 (.17) | 4.25 (.16) | .43 | 3.77 (.17) | 3.85 (.30) | .09 | χ2(2)=15.23* |
| Diary Negative Affect | 2.45 (.12) | 1.91 (.11) | .58 | 2.37 (.14) | 2.08 (.12) | .27 | 2.25 (.23) | 2.22 (.23) | .02 | χ2(2)=8.70* |
| Diary NA: Anxiety | 3.05 (.16) | 2.26 (.14) | .58 | 2.94 (.19) | 2.32 (.16) | .39 | 2.94 (.31) | 2.74 (.30) | .10 | χ2(2)=6.85* |
| Diary NA: Depression | 2.22 (.15) | 1.86 (.13) | .31 | 2.18 (.18) | 2.01 (.15) | .12 | 2.11 (.29) | 2.08 (.28) | .02 | χ2(2)=2.23 |
| Diary NA: Hostility | 2.07 (.12) | 1.60 (.11) | .51 | 2.00 (.15) | 1.92 (.12) | .07 | 1.70 (.24) | 1.86 (.23) | −.12 | χ2(2)=11.64* |
| EMA Negative Affect | 2.26 (.10) | 1.86 (.10) | .48 | 2.16 (.11) | 1.95 (.11) | .23 | 2.32 (.21) | 2.14 (.20) | .14 | χ2(2)=4.75 |
| B. Ecological Momentary Assessment (EMA) and diary-assessed Positive Affect (PA) and Negative Affect (NA) in Study 2. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Monitor + Accept (N=58) | Monitor Only (N=58)c | Control (N=37) | Time × Condition Difference | ||||||
| Pre | Post | d | Pre | Post | d | Pre | Post | d | ||
| Diary Positive Affect | 3.40 (.13) | 4.10 (.13) | .70 | 3.31 (.13) | 3.66 (.13) | .35 | 3.54 (.16) | 3.70 (.17) | .16 | χ2(2)=12.67* |
| Diary PA: Happiness | 3.48 (.15) | 4.23 (.15) | .65 | 3.47 (.15) | 3.76 (.15) | .25 | 3.65 (.18) | 3.77 (.18) | .11 | χ2(2)=14.88* |
| Diary PA: Calm | 3.37 (.14) | 4.12 (.14) | .67 | 3.25 (.14) | 3.60 (.14) | .31 | 3.67 (.17) | 3.79 (.17) | .11 | χ2(2)=13.08* |
| Diary PA: Vigor | 3.36 (.15) | 3.95 (.15) | .52 | 3.22 (.15) | 3.62 (.15) | .36 | 3.31 (.18) | 3.55 (.18) | .22 | χ2(2)=3.88 |
| EMA Positive Affect | 3.95 (.13) | 4.31 (.13) | .39 | 3.81 (.13) | 3.95 (.13) | .15 | 3.96 (.16) | 3.97 (.16) | .01 | χ2(2)=11.13* |
| Diary Negative Affect | 2.10 (.10) | 1.79 (.10) | .40 | 2.31 (.10) | 2.03 (.10) | .36 | 2.11 (.13) | 2.01 (.13) | .12 | χ2(2)=2.96 |
| Diary NA: Anxiety | 2.38 (.12) | 2.10 (.12) | .27 | 2.72 (.12) | 2.28 (.12) | .42 | 2.23 (.15) | 2.15 (.15) | .08 | χ2(2)=4.32 |
| Diary NA: Depression | 2.11 (.12) | 1.75 (.12) | .41 | 2.27 (.12) | 2.10 (.12) | .19 | 2.17 (.15) | 2.08 (.15) | .10 | χ2(2)=3.66 |
| Diary NA: Hostility | 1.82 (.10) | 1.52 (.11) | .38 | 1.94 (.10) | 1.71 (.11) | .30 | 1.91 (.13) | 1.80 (.13) | .13 | χ2(2)=1.66 |
| EMA Negative Affect | 2.08 (.09) | 1.82 (.09) | .38 | 2.24 (.09) | 1.96 (.09) | .41 | 2.16 (.11) | 2.00 (.12) | .24 | χ2(2)=1.62 |
Note: Data are reported as means (SE) adjusted for cohort, instructor, and time of day (for EMA).
Note: Data are reported as means (SE) adjusted for day of week and time of day (For EMA). d = Cohen’s d effect size estimate. EMA = Ecological Momentary Assessment.
N=53 for diary outcome analyses.
N=51 for diary outcome analyses.
N=57 for diary outcome analyses.
p<.05
Figure 3.
Effect size estimates (Hedges’ g) and 95% Confidence Intervals in Studies 1 & 2 for primary intervention comparisons.
Note: MA = Monitor + Accept. MO = Monitor Only. PA = Positive Affect. NA = Negative Affect. EMA = Ecological Momentary Assessment.
Exploratory sensitivity analyses then evaluated whether there were condition differences in subcategories of positive affect. Both MA and MO participants showed significant increases in feelings of calm (MA mean change=0.80, p<.0005, d=.75; MO mean change=0.58, p<.0005, d=.48), whereas only MA participants showed significant increases in happiness (MA mean change=0.69, p<.0005, d=.58; MO mean change=0.28, p=.059, d=.20) and vigor (MA mean change=0.63, p<.0005, d=.56; MO mean change=0.25, p=.068, d=.20). NT control participants did not show increases on any of these subtypes of positive affect (happiness mean change=0.14, p=.435, d=.08; calm mean change=0.24, p=.159, d=.15; vigor mean change=−0.10, p=.557, d=−.06). There was a significant advantage of MA over MO in increasing happiness (χ2(1)=4.08, p=.043, g=.39), with no significant differences on increasing feelings of vigor (χ2(1)=3.71, p=.054, g=.37) or calm (χ2(1)=1.28, p=.257, g=.22). MA participants showed significantly greater increases on all positive affect subscales compared to NT participants (happiness: χ2(1)=5.55, p=.019, g=.52; vigor: χ2(1)=10.96, p=.001, g=.73; calm: χ2(1)=6.29, p=.012, g=.56). MO and NT participants did not differ on any of these diary-assessed positive affect subscales (all ps>.10).
MLM analyses of momentary positive affect revealed a main effect of time across study conditions (χ2(1)=57.46, p<.0005), no main effect of study condition across baseline and post-intervention time points (χ2(2)=0.81, p=.666), and a significant time × condition interaction (χ2(2)=15.23, p=.001) (see Table 4A for full MLM results). Both MA- and MO-trained participants showed significant increases in momentary positive affect from baseline to post-intervention (MA mean change=0.61, p<.0005, d=.61; MO mean change=0.49, p<.0005, d=.43) whereas control participants did not (NT mean change=0.09, p=.434, d=.09) (see Table 5A). Although the magnitude of positive affect change was greater following MA compared to MO, there were no time × condition differences between these conditions (χ2(1)=1.25, p=.263, g=.22) (see Figure 3). MA participants showed significantly greater increases in state positive affect compared to NT participants (χ2(1)=15.10, p<.0005, g=.95), as did MO participants relative to NT participants (χ2(1)=8.48, p=.004, g=.68).
Table 4.
| A. Multilevel mixed effects linear model results for Ecological Momentary Assessment Positive and Negative Affect in Study 1. | ||||
|---|---|---|---|---|
| Positive Affecta | Negative Affecta | |||
| B (SE) | z | B (SE) | z | |
| Interceptb (γ000) | 3.60 (.33) | 10.81* | 2.38 (.22) | 10.99* |
| Time (pre vs. post) (γ010) | 0.61 (.07) | 8.24* | −0.40 (.07) | −5.84* |
| Condition | ||||
| MA vs. MO (γ001) | −0.03 (.21) | −0.16 | −0.10 (.14) | −0.69 |
| MA vs. NT (γ002) | −0.03 (.36) | −0.07 | 0.06 (.24) | 0.25 |
| Condition × Time | ||||
| MA vs. MO × pre vs. post (γ011) | −0.12 (.11) | −1.12 | 0.19 (.10) | 1.87 |
| MA vs. NT × pre vs. post (γ012) | −0.52 (.13) | −3.89* | 0.22 (.12) | 1.74 |
| Time of Day (γ100) | 0.04 (.02) | 2.28* | −0.03 (.01) | −2.07* |
| Cohort | ||||
| 2 (γ003) | 0.00 (.20) | 0.00 | 0.07 (.13) | 0.54 |
| 3 (γ004) | 0.28 (.22) | 1.28 | −0.08 (.14) | −0.61 |
| Instructor (γ005) | 0.01 (.20) | 0.07 | 0.03 (.13) | 0.23 |
| Estimate | 95% CI | Estimate | 95% CI | |
| Within-subjects error (rtdi) | 1.31 (.04) | 1.24, 1.39 | 1.13 (.03) | 1.07, 1.20 |
| Day level error (uodi) | 0.13 (.03) | 0.09, 0.21 | 0.09 (.02) | 0.05, 0.15 |
| Between-subjects error (u00i) | 0.85 (.12) | 0.64, 1.12 | 0.31 (.05) | 0.23, 0.43 |
| B. Multilevel mixed effects linear model results for Ecological Momentary Assessment Positive and Negative Affect in Study 2. | ||||
|---|---|---|---|---|
| Positive Affectc B (SE) | z | Negative Affectc B (SE) | z | |
| Interceptd (γ000) | 3.72 (.15) | 25.19* | 2.15 (.12) | 18.61* |
| Time (pre vs. post) (γ010) | 0.36 (.07) | 4.96* | −0.26 (.06) | −3.95* |
| Condition | ||||
| MA vs. MO (γ001) | −0.14 (.18) | −0.81 | 0.16 (.13) | 1.25 |
| MA vs. control (γ002) | 0.01 (.20) | 0.07 | 0.08 (.15) | 0.57 |
| Condition × Time | ||||
| MA vs. MO × pre vs. post (γ011) | −0.22 (.10) | −2.22* | −0.03 (.09) | −0.31 |
| MA vs. control × pre vs. post (γ012) | −0.36 (.11) | −3.23* | 0.09 (.10) | 0.96 |
| Day of Week | ||||
| Monday (γ020) | −0.22 (.08) | −2.57* | 0.14 (.08) | 1.80 |
| Tuesday (γ030) | −0.02 (.08) | −0.19 | 0.02 (.08) | 0.20 |
| Thursday (γ040) | −0.07 (.08) | −0.94 | −0.01 (.07) | −0.10 |
| Friday (γ050) | 0.06 (.09) | 0.64 | 0.05 (.08) | 0.67 |
| Saturday (γ060) | 0.21 (.09) | 2.38* | −0.17 (.08) | −2.11* |
| Time of Day (γ100) | 0.10 (.02) | 5.03* | −0.03 (.02) | 1.68 |
| Estimate | 95% CI | Estimate | 95% CI | |
| Within-subjects error (rtdi) | 1.41 (.04) | 1.34, 1.48 | 1.12 (.03) | 1.07, 1.19 |
| Day level error (u0di) | 0.12 (.03) | 0.08, 0.19 | 0.11 (.02) | 0.07, 0.16 |
| Between-subjects error (u00i) | 0.73 (.10) | 0.57, 0.95 | 0.34 (.05) | 0.26, 0.46 |
N=136.
Reference group: condition: MA; time: Pre; time of day: first survey (9:00-11:00am); cohort: 1; instructor: NT.
Note: N=153.
Reference group: condition: MA; time: Pre; day of week: Sunday; time of day: first survey (9-11:30am).
p<.05
Negative affect
In analyses of end-of-day overall negative affect, an MLM revealed a significant main effect of time (χ2(1)=16.61, p<.0005), no main effect of study condition across time points (χ2(2)=0.17, p=.918), and a significant time × condition interaction (χ2(2)=8.70, p=.013) (see Table 3A for full MLM results). Both MA- and MO-trained participants showed significant decreases in overall negative affect from baseline to post-intervention (MA mean change=−0.54, p<.0005, d=.58; MO mean change=−0.29, p=.008, d=.27), whereas control participants did not (NT mean change=−0.02, p=.859, d=.02). MA and MO participants did not significantly differ on change in overall negative affect (χ2(1)=2.54, p=.111, g=.31) (see Figure 3). However, MA participants showed significantly greater decreases in overall negative affect compared NT participants (χ2(1)=8.59, p=.003, g=.66), whereas MO and NT participants did not significantly differ (χ2(1)=2.29, p=.130, g=.35).
Consistent with changes in overall negative affect, both MA and MO participants showed significant decreases in anxiety (MA mean change=−0.79, p<.0005, d=.58; MO mean change=−0.62, p<.0005, d=.39) whereas control participants did not (NT mean change=−0.19, p=.281, d=.10). MA participants also showed significant decreases in depression (MA mean change=−0.36, p=.011, d=.31) and hostility (MA mean change=−0.48, p<.0005, d=.51), whereas neither MO or control participants showed significant decreases in depression (MO mean change=−0.18, p=.214, d=.12; control mean change=−0.03, p=.881, d=.02) or hostility (MO mean change=−0.08, p=.506, d=.07; control mean change=0.15, p=.309, d=−.12). These MLMs suggest that the advantage of MA over MO was specific to hostility (χ2(1)=5.33, p=.021, g=.45) rather than anxiety (χ2(1)=0.65, p=.420, g=.16) and depression (χ2(1)=0.82, p=.365, g=.18). MA showed an advantage over NT specifically for hostility (χ2(1)=10.75, p=.001, g=.73) and anxiety (χ2(1)=6.70, p=.010, g=.58) but not feelings related to depression (χ2(1)=2.16, p=.142, d=.33). MO did not significantly differ from NT on any negative affect subtype (anxiety: χ2(1)=3.50, p=.061, g=.42; depression: χ2(1)=0.44, p=.508, g=.15; hostility: χ2(1)=1.49, p=.222, g=.27).
For momentary negative affect, there was a main effect of time across study conditions (χ2(1)=30.53, p<.0005) such that all conditions on average showed significant decreases in negative affect from baseline to post-intervention (mean change=−0.28, p<.0005, d=.35). There was no main effect of study condition across baseline and post-intervention time points (χ2(2)=0.54, p=.764), and no time × condition interaction (χ2(2)=4.75, p=.093) (see Tables 4A and 5A).
Summary & Discussion
Study 1 provides the first indication that acceptance skills are an important component of mindfulness training for enhancing positive affect. Although both MA and MO participants showed significant increases in positive affect, end-of-day positive affect was enhanced significantly more following MA compared to MO training, and MO and NT participants did not differ. MA was particularly effective for elevating feelings of happiness (i.e., feeling happy, pleased, and cheerful). In contrast, there were no differences between MA and MO on momentary assessments of positive affect, although the pattern of this effect was consistent with end-of-day diary reports. It is possible that this EMA effect was smaller due to greater within-person variability in momentary positive affect throughout the day (compared to end-of day reports), less sensitivity to detect pre- to post-intervention condition differences on a one-item positive affect measure (compared to a nine-item composite), or an added effect of acceptance on the endurance of positive emotions (e.g., monitoring might increase awareness of positive affective states, and acceptance training might additionally enhance the recall and/or impact of positive emotions experienced throughout the day). Overall, though, the evidence suggests that the inclusion of acceptance training more effectively boosts positive affect, with medium-large effects attributed to MA (ds=.61-.70) and small-medium effects attributable to MO (ds=.32-.43).
In contrast, there was little difference between MA and MO interventions on change in negative affect. Both MA and MO interventions decreased momentary negative affect and end-of-day diary negative affect from pre- to post-intervention. However, MA showed a significant advantage over MO for decreasing diary-assessed hostility, suggesting some additive benefit of acceptance skills training on negative affect.
Overall, Study 1 provides initial support for the primary Monitor + Accept hypothesis, showing that the inclusion of acceptance skills training has added benefit for boosting positive affect in mindfulness interventions. Interestingly, these effects were most robust for end-of-day reports of happiness, consistent with outside observer ratings of greater happiness among experienced meditators (Choi, Karremans, & Barendregt, 2012). In contrast, both MA and MO training decreased negative affect, with less evidence that the inclusion of acceptance training appreciably reduces negative affect. One open question not addressed in Study 1 is whether this reduction in negative affect is specific to mindfulness interventions or nonspecific factors (e.g., placebo expectancies), as we did not include an active treatment control condition in this RCT. Likewise, it is possible that increases in positive affect following both interventions were influenced by increases in social contact in this group-based format; social integration has been shown to promote positive affect (Cohen, 2004). The group-based format also introduces the possibility that acceptance themes emerged through monitoring practice and were introduced through group discussion, a potential source of contamination in isolating monitoring and acceptance instruction. A second limitation of Study 1 was participants’ lower than ideal compliance with survey completion, although participants did provide an average of 14 data points at post-intervention. We sought to address these concerns in an active treatment-controlled replication trial.
Study 2
Study 2 extends the findings of Study 1 in several important ways. First, although every effort was made to control the content of the 8-week MO intervention, the group discussion format opens the possibility for contamination to occur around the theme of acceptance. For example, participants may have shared meditation experiences of sitting with physical or emotional discomfort and allowing it to be present without trying to push it away. By using smartphone interventions that deliver carefully isolated monitoring and acceptance content to individuals, Study 2 eliminates the possibility that acceptance themes were unintentionally instructed in the MO program. This smartphone format also isolates the basic skills of mindfulness from contextual factors that might play an active but nonspecific role in promoting mindfulness intervention benefits (e.g., social contact, which is a central feature of MBSR but not a conceptual feature of mindfulness). Moreover, Study 2 controls for other nonspecific intervention factors, including treatment expectancies and placebo effects, daily time and effort dedicated to a practice goal, and instructor effects, by comparing MA and MO training to a structurally matched active control program. This Coping control program provided guidance in free-ranging reflection, analytic thinking and reappraisal, and problem-solving strategies; these elements encouraged past and future focus rather than present-moment monitoring, and active change strategies in contrast to acceptance skills. Finally, by testing the effects of 2-week interventions on positive affect, Study 2 begins to address questions about context and training length, such as whether an abbreviated dose of smartphone mindfulness training can produce comparable positive affect increases as 8-week group-based MBSR.
To test whether acceptance training plays a central role in increasing positive affect after two weeks of training, stressed adults were randomly assigned to receive one of three structurally equivalent smartphone programs: (1) MA, which modeled standard secular mindfulness training with instruction in both monitoring and acceptance techniques; (2) MO, which instructed monitoring techniques only; or (3) Coping control, which instructed coping techniques and did not develop monitoring or acceptance skills. As in Study 1, positive and negative affect were assessed in daily life via momentary assessments and end-of-day diaries for three days before and after the intervention period. Study 2 tested the primary Monitor + Accept prediction that MA mindfulness training would increase positive affect in daily life compared to MO and control trainings, with no differences between MO and control, largely consistent with Study 1 findings. Study 2 also evaluated whether MA training would decrease daily life negative affect compared to MO and control trainings (the Monitor + Accept hypothesis), or whether all active stress management programs would be effective for decreasing negative affect (as suggested by Study 1 findings).
Methods
Participants
Enrolled participants were 153 stressed adults (Mage=32 years, SD=14; see Table 1B for baseline characteristics) recruited from the Pittsburgh community via participant registries, community advertisements, and mass emails to local organizations for a study testing smartphone training programs for managing stress. Primary study analyses are reported using all available baseline and post-intervention data. Of 153 participants (for all of whom baseline data was available), 150 completed the intervention, 149 completed post-intervention EMA, 148 provided post-intervention diary data, and 149 provided data at a post-intervention lab assessment. See Figure 1B for CONSORT flow chart.
The study design and outcomes described here were pre-registered with Clinical Trials identifier NCT02433431; hypotheses were guided by MAT (Lindsay & Creswell, 2015, 2017). This report describes positive and negative affect outcome data from ambulatory assessments (secondary trial outcomes). As in Study 1, eligible participants were English-speaking smartphone owners (Android or iPhone) between the ages of 18-70 years who scored >5 on the 4-item Perceived Stress Scale. Participant exclusion criteria were identical to those in Study 1. Written informed consent was obtained from all participants, and all study procedures were approved by the Carnegie Mellon University IRB. Study data was collected between February 2015 and April 2016. Trial recruitment was stopped when the goal of enrolling 150 participants was reached; participants partway through the screening process at this time were included in the study if eligible.
Sample size was determined for primary stress reduction outcomes in the larger clinical trial (Lindsay, Young, Smyth, Brown, & Creswell, 2018). Specifically, effect size estimates were based on medium-large pre-post 8-week mindfulness intervention vs. waitlist control effects on stress reactivity outcomes (d=.63: Nyklíček, Mommersteeg, Van Beugen, Ramakers, & Van Boxtel, 2013) and small-medium pre-post 2-week online mindfulness intervention vs. waitlist control effects on general stress perceptions (d=.37-.46: (Cavanagh et al., 2013; Glück & Maercker, 2011). A medium effect size was estimated for this trial (d=.52), with plans to boost treatment adherence and participant retention through standardized study reminders, individual contact during the intervention period, and cash bonuses for high adherence (participants received $15 base compensation plus a $15 bonus for completing at least 13 of 15 surveys at baseline and at post-intervention, and $25 base compensation for completing the intervention portion of the study, plus a $40 bonus for completing at least 13 of the 14 lessons). Using G*Power, we estimated a total of N=147 participants were needed to detect post-intervention omnibus differences between three study conditions at 80% power using ANOVAs (the primary trial outcome), and N=120 were needed to detect group × time interactions estimating a pre-post correlation of .60 and a two-tailed Type I error rate of .05 (Faul et al., 2007). The ambulatory assessment data reported here were not analyzed until the complete dataset was collected.
Procedure
Overview
Briefly, as part of the larger three-arm parallel trial, interested participants were pre-screened for eligibility by telephone, then further screened at an in-person baseline assessment. Subject IDs were assigned sequentially, and author EKL used a computerized random number generator to pre-assign one of three condition codes to each ID in blocks of 8, 16, or 24 using a 3:3:2 randomization sequence (MA:MO:control). Trained study staff enrolled eligible participants and instructed participants to download their assigned intervention by code. All participants were blind to study condition, and study staff were blind to condition in 76% of baseline sessions3. Enrolled participants provided a dried blood spot (DBS) sample, completed a questionnaire and task battery, and were oriented to the at-home ambulatory assessments and intervention. During three weeks of at-home study activities, participants completed three consecutive days of pre-intervention momentary and diary assessments (see Measures), a 14-day intervention period (see Materials), and three consecutive days of post-intervention momentary and diary assessments immediately following the intervention period. Participants received standardized study reminder texts and phone calls throughout the at-home period, and were able to call or text the study hotline to ask questions or resolve technical issues. Participants returned for a post-intervention assessment an average of 4.66 days (SD=1.88 days) after the completion of training. At that session, they provided a DBS sample (to be reported elsewhere), completed questionnaires and tasks (including a measure of Treatment Expectancies), and underwent the Trier Social Stress Task and assessments (reported in Lindsay et al., 2018). After all outcome measures were collected, participants were funnel debriefed, informed of the primary aims of the study – namely, to test the active ingredients of mindfulness training – were given access to the training program of their choice, and were compensated for their time.
Ecological Momentary Assessments and Diary Assessments
As in Study 1, a two-pronged ambulatory assessment approach was used to measure momentary affective states and end-of-day positive and negative affect (see Measures). In this study, momentary and diary assessments were administered on participants’ own smartphones using Qualtrics surveys delivered through SurveySignal text links. EMA surveys were administered at four quasi-random times each day (totaling 24 surveys across 3 days pre- and 3 days post-intervention); text links were sent during each of four 2.5-hour blocks distributed between 9:00am and 7:00pm, with links expiring after 45 minutes. Links for daily diary surveys (6 surveys in total across pre- and post-intervention) were sent at 8:30pm and remained active until 11:30pm. Participants were trained on how to complete ambulatory assessment items during the baseline study appointment.
Depending on the day of their baseline study appointment, participants began baseline ambulatory assessments on either a Thursday or a Sunday. Those who completed baseline ambulatory assessments on a Thursday-Saturday schedule began the 2-week intervention on Sunday and completed post-intervention ambulatory assessments Sunday-Tuesday; participants who completed baseline ambulatory assessments on a Sunday-Tuesday schedule began the intervention on Thursday and completed post-intervention ambulatory assessments Thursday-Saturday. This counterbalance distributed weekdays and weekend days equally between baseline and post-intervention assessments and enabled the collection of post-intervention ambulatory assessments immediately following the intervention.
Materials
Intervention Programs
Participants were randomly assigned to receive one of three 14-lesson smartphone-based interventions (described below): MA, MO, or Coping control. To maximize experimental control in isolating the effects of monitoring and acceptance instruction, all three interventions were delivered by the same female instructor (who was blind to hypotheses) and were matched on attentional demand (i.e., active listening and guided practice), length of each lesson, lesson structure (i.e., proportion of time devoted to didactics, guidance, and silent practice), and delivery tone of voice. To equalize expectancies at the baseline appointment, all participants viewed the same 5-minute introductory video explaining how to prepare for and what to expect in the training program, and “mindfulness” was not mentioned during the study period. During the 14-day intervention period, participants were expected to complete one 20-minute guided audio lesson each day, plus brief unguided homework practice (3-10 minutes per day). Participants were required to complete lessons in order and could not skip or repeat lessons. Each lesson trained specific techniques through didactic explanation (what the technique was and how it would help) and formal guided practice (i.e., meditation practice in the MA and MO interventions and guided thinking in the control intervention). The lessons in all three conditions included an average of 5 minutes of didactics (an average of 26% of each lesson), 12.5 minutes of guided practice (including 7 minutes of silence; 62% of the lessons), and 2.5 minutes of instruction about home practice (12% of the lessons). An unblinded study manager contacted all participants by phone on Days 3 and 9 of the intervention program to answer training-specific questions, address difficulties, and encourage program adherence. After the 14-day intervention period, the training program was deactivated (although a training program of choice was provided to participants at the completion of the study).
The intervention programs were developed in collaboration with leading mindfulness teacher Shinzen Young and were based on his Unified Mindfulness system (Young, 2016). The instructor who voiced the programs had 15 years of teaching experience with this system. The two mindfulness meditation programs were designed to systematically parse mindfulness instruction in (1) attention monitoring and (2) acceptance. The content of each intervention is detailed in Lindsay et al. (2018). Full intervention scripts are available for research purposes by request.
Monitor + Accept (MA):
MA participants first learned foundational concentration skills, which enabled them to (1) monitor their present-moment body experience (in the lessons, this skill was referred to as ‘sensory clarity’) while (2) welcoming and accepting each experience (referred to as ‘equanimity’). Specifically, concentration was described as an intrinsically rewarding state of stable attention (Csikszentmihalyi, 2000) on the intended target. In this intervention, the focus of all meditations was physical and emotional body experiences.
Monitoring (‘sensory clarity’) was explained in terms of two dimensions: (a) resolution, referring to discriminating types of experiences, such as whether pleasant, unpleasant, or neutral; physical vs. emotional; level of intensity; locations and movement patterns of sensations; and (b) sensitivity, referring to detecting subtle sensations, including faint sensations related to pleasant activities and emotions, and fleeting waves of unpleasant emotions. Acceptance (‘equanimity’) was trained through three tangible strategies that embody the attitude of acceptance: participants were encouraged to (a) maintain a state of global body relaxation; (b) mentally welcome all physical and emotional body experiences; and (c) use a gentle, matter-of-fact tone of voice (an ‘equanimity tone’) while labeling these experiences. Although positive emotional states were neither encouraged nor discouraged, participants were instructed to notice and differentiate pleasant, unpleasant, and neutral emotional body sensations (monitoring) and to greet each type of sensation with equanimity (acceptance). In the context of emotional sensations, equanimity was described as a sort of permission for each sensation to unfold in its own time. At the end of each lesson, participants were prompted to notice and tune into any rewarding sensations that were present.
Monitor Only (MO):
The MO program trained participants only to concentrate on and (1) monitor physical and emotional body experience during each meditation practice (as described above), with no instruction on acceptance. As in MA, positive emotional states themselves were not encouraged or discouraged, but the focus was on noticing and differentiating pleasant, unpleasant, and neutral emotional body sensations, and participants were prompted to notice any rewarding sensations present at the end of each lesson.
Coping control:
The Coping control training program, referred to in the lessons as ‘MyTime,’ was developed to parallel the structure of MA and MO without encouraging focus on or acceptance of present experience. Instead, participants were instructed to: (a) freely reflect and let their minds drift (in contrast to concentration developed in MA and MO); (b) reframe or reappraise past and anticipated events (with past and future emphasis contrasting present-focused monitoring, and change strategies contrasting acceptance strategies); and (c) analyze and solve personal problems (again encouraging active change rather than acceptance of momentary experiences). Throughout the lessons, participants were encouraged to mind-wander between pleasant, unpleasant, or neutral topics as they pleased. Guidance in two lessons involved reflecting on past positive experiences and imagining future positive experiences. Similar to MA and MO, control participants were prompted to carry any positive effects of each practice session into their daily lives. Overall, the Coping control program was designed to be useful for managing stress by reinforcing common reappraisal and coping strategies (see Carver et al., 1989; Ochsner & Gross, 2005) without training mindfulness, and was included to control for nonspecific effects of undergoing an active training program, such as treatment expectancies and daily practice toward the goal of reducing stress.
Measures
Ecological Momentary Assessment of State Positive and Negative Affect:
Assessments of momentary positive and negative affect in daily life were identical to those described in Study 1, except surveys were prompted four times daily.
Positive and Negative Affect Diary:
Specific types of positive and negative affect were assessed at the end of each day for three days pre- and immediately post-intervention, as described in Study 1. Again, eight composite affect scales were created from the 18 items: an overall positive affect scale (average Cronbach’s α=.94 across 6 diary days) and three positive affect subscales: happiness (α=.90), calm (α=.88), and vigor (α=.89); and an overall negative affect scale (average α=.90) and three negative affect subscales: anxiety (α=.83), depression (α=.89), and hostility (α=.81).
Treatment Adherence:
The smartphone training application automatically timestamped the initiation and completion of each lesson in the 14-day at-home training period. This electronic timestamp was used to calculate the total number of at-home lessons completed for each individual.
Treatment Expectancies:
As in Study 1, participants completed an adapted 6-item Credibility/Expectancy Questionnaire (Devilly & Borkovec, 2000) to assess their beliefs about the efficacy of the training program at post-intervention (but before beginning the TSST procedures). Cognitive and emotional subscales were averaged to create an overall measure of positive treatment expectancies (α=.95).
Analyses
Overview
Analyses were conducted with SPSS Statistics 21.0 (IBM, Armonk, New York) and Stata 14.2 software (StataCorp, College Station, Texas). Preliminary analyses conducted in SPSS tested for condition differences in demographics and other baseline characteristics using chi-square (for categorical variables) and ANOVA tests (for continuous variables). Treatment expectancies, treatment adherence, EMA compliance, and EMA counterbalance were evaluated as covariates using ANOVA to test for significant condition differences.
Ambulatory assessment analyses
As in Study 1, MLMs were used to test for time (pre or post) × condition (MA, MO, or control) differences and between-group contrasts on the primary outcomes using the Stata Mixed procedure with REML estimation. The assumption of dependence in the data was confirmed in unconditional models. For diary-assessed positive and negative affect outcomes, empty 2-level models showed that 34-48% of the total variance occurred between individuals, whereas 52-66% of variance occurred within individuals. For momentary positive and negative affect outcomes, 21-32% of the total variance occurred between individuals, 5-7% was explained at the day level, and 63-72% occurred within individuals. Thus, 2-level models were used for diary data and 3-level models were used for EMA data.
In sum, the diary outcome models followed this general equation:
Level 1:
Level 2:
Reduced form:
with β0i reflecting the intercept of affect for the reference group (MA) at pre-intervention compared to MO and control groups, and β1i accounting for time (pre or post) and time × condition interactions. Time and day of week were modeled at Level 1, while study condition was modeled at Level 2; rti and u0i represented error at the within- and between-subject levels, respectively.
EMA data was modeled in 3-level equations, which additionally accounted for the clustering of observations within day. Time of day (first, second, third, or fourth survey), which varied at the observation level, was included at Level 1 to account for temporal dependency between proximal observations. Time (pre or post) and day of week, which varied at the day level, were included at Level 2. The rtdi, u0di, and u00i terms reflect error at the within-subject, within-day, and between-subject levels, respectively.
Level 1:
Level 2:
Level 3:
Reduced form:
Effect sizes were calculated as in Study 1.
Results
Preliminary Analyses
First, success of randomization on major demographic characteristics in the full randomized sample (N=153) was evaluated. There were no pre-existing condition differences on age, sex, race, ethnicity, or education (see Table 1B).
Second, condition differences in study attrition, intervention adherence, ambulatory assessment compliance, ambulatory assessment counterbalance, and pre-intervention positive and negative affect were tested (see Table 2B). Study attrition was low, with a 2% participant drop-out rate and no condition differences in study drop-outs (χ2(2)=1.42, p=.491). Likewise, participants in all conditions were highly adherent to the training programs, with no condition differences in treatment adherence (F(2,146)=0.40, p=.670). On average, participants completed 13.49 of the 14 lessons, and 75% of participants completed all 14 lessons (1.3% of participants completed fewer than 10 lessons). Similarly, participants in all conditions were adequately adherent to both baseline and post-intervention ambulatory assessments, on average completing 91% of baseline surveys and 86% of post-intervention surveys. There were no condition differences in the counterbalance of ambulatory assessment days (χ2(2)=3.10, p=.21). But there was a relationship between day of the week and positive and negative affect in this sample; there was a main effect of day of week on momentary positive affect (χ2(5)=16.10, p=.007), on diary-assessed positive affect (χ2(5)=15.01, p=.010), and on diary-assessed negative affect (χ2(5)=13.72, p=.018). Thus, day of week was included as a covariate in all EMA analyses. There were no pre-intervention condition differences on EMA or diary-assessed positive or negative affect ratings (Table 2B). Finally, the post-intervention assessment took place an average of 4.66±1.88 days after the end of the intervention, with no differences between conditions (F(2,146)=1.03, p=.360). At this assessment, there were no condition differences in treatment expectancies (F(2,146)=1.55, p=.22), indicating similar perceptions of treatment benefits across all three training conditions.
Primary analyses
As with Study 1, we predicted that MA training would increase positive affect (primary Monitor + Accept hypothesis) and decrease negative affect (secondary Monitor + Accept hypothesis) in daily life compared to MO and control training, and that MO and control would not differ. To evaluate these hypotheses, MLMs focused on time × condition interactions in end-of-day diary-assessed affect composites and momentary affect (using all available data). When significant time × condition interactions were present, we tested for differences in MA vs. MO, MA vs. control, and MO vs. control contrasts.
Positive affect
In diary assessment analyses, an MLM revealed a significant main effect of time (χ2(1)=38.02, p<.0005), no main effect of study condition across time (χ2(2)=2.25, p=.325), and, as predicted, a significant time × condition effect on overall positive affect (χ2(2)=12.67, p=.002). Figure 2B depicts this interaction (see Table 3B for full MLM results). Both MA- and MO-trained participants showed significant increases in overall positive affect from pre- to post-intervention (MA mean change=0.70, p<.0005, d=.70; MO mean change=0.35, p<.0005, d=.35) whereas control participants did not (control mean change=0.16, p=.206, d=.16) (see Table 5B). Supporting the primary hypothesis, MA-trained participants showed significantly higher overall positive affect from pre- to post-intervention compared to MO-trained (χ2(1)=6.17, p=.013, g=.46) and control-trained (χ2(1)=11.49, p=.001, g=.71) participants (see Table 5B and Figure 3), whereas MO and control participants did not differ (χ2(1)=1.45, p=.228, g=.25).
Consistent with changes in overall positive affect, both MA and MO participants showed significant increases in happiness (MA mean change=0.75, p<.0005, d=.65; MO mean change=0.29, p=.011, d=.25), calm (MA mean change=0.75, p<.0005, d=.67; MO mean change=0.35, p=.002, d=.31), and vigor (MA mean change=0.59, p<.0005, d=.52; MO mean change=0.41, p<.0005, d=.36), whereas control participants did not show increases in any of these types of positive affect (happiness mean change=0.12, p=.410, d=.11; calm mean change=0.12, p=.393, d=.11; vigor mean change=0.23, p=.104, d=.22). Positive affect subscale MLM analyses suggested that the advantage of MA over both MO and control was specific to happiness (MA vs. MO: χ2(1)=8.70, p=.003, g=.54; MA vs. control: χ2(1)=12.53, p<.0005, g=.72) and calm (MA vs. MO: χ2(1)=6.24, p=.013, g=.45; MA vs. control: χ2(1)=11.93, p=.001, g=.70) rather than feelings of vigor (MA vs. MO: χ2(1)=1.28, p=.258, g=.21; MA vs. control: χ2(1)=3.79, p=.052, g=.40) (see Table 5B). MO and control participants did not differ on any diary-assessed positive affect subscales (all ps>.20).
On momentary positive affect, MLM results showed a significant main effect of time across study conditions (χ2(1)=13.60, p=.0002), no main effect of study condition across baseline and post-intervention time points (χ2(2)=2.25, p=.324), and, consistent with predictions, a significant time × condition interaction (χ2(2)=11.13, p=.004) (see Table 4B for full MLM results). Both MA- and MO-trained participants showed significant increases in momentary positive affect from pre- to post-intervention (MA mean change=0.36, p<.0005, d=.39; MO mean change=0.14, p=.044, d=.15) whereas control participants did not (control mean change=0.004, p=.960, d=.01) (see Table 5B). Again supporting the primary Monitor + Accept hypothesis, this increase in positive affect was significantly greater after MA training than after MO (χ2(1)=4.91, p=.027, g=.41) and control trainings (χ2(1)=10.40, p=.001, g=.66) (see Table 4B and Figure 3). MO and control interventions did not differ (χ2(1)=1.55, p=.213, g=.25).
Negative affect
An MLM revealed a significant main effect of time for diary-assessed negative affect overall (χ2(1)=18.08, p<.0005), with participants on average showing lower overall negative affect at post- compared to pre-intervention (mean change=−0.25, p<.0005, d=.32). There was no main effect of condition across time (χ2(2)=2.93, p=.231) and no significant time × condition interaction (χ2(2)=2.96, p=.227) (see Tables 3B and 5B). For each diary-assessed negative affect subscale, MLMs showed significant main effects of time, but revealed no time × condition differences on depression (χ2(2)=3.66, p=.160), anxiety (χ2(2)=4.32, p=.115), or hostility (χ2(2)=1.66, p=.435) subscales (see Table 5B).
On momentary negative affect, there was a significant main effect of time across study conditions (χ2(1)=32.77, p<.0005), such that participants on average showed significant decreases in negative affect from pre- to post-intervention (mean change=−0.24, p<.0005, d=.33; see Table 5B). There was no main effect of study condition (χ2(2)=1.67, p=.434) and no time × condition interaction (χ2(2)=1.62, p=.446) (see Table 4B).
Summary & Discussion
Study 2 provides the first well-controlled experimental evidence that just 14 days of smartphone-based mindfulness training boosts positive affect in daily life, and supporting the Monitor + Accept hypothesis, acceptance training appears to be a key ingredient for this effect. When acceptance training was not included in the mindfulness intervention, positive affect benefits were significantly reduced. Specifically, although both MA and MO participants showed higher positive affect at post- compared to pre-intervention, MA training boosted end-of-day and state positive affect significantly more than MO and control trainings, and MO did not differ from control training. Medium-large effects were observed after MA training (ds=.39-.70), small-medium effects after MO training (ds=.15-.36), and very small effects after control training (ds=.01-.22). The inclusion of acceptance training was particularly important for increasing feelings of happiness and calm. Overall, by comparing structurally matched interventions that control for non-mindfulness-specific treatment components, Study 2 demonstrates that acceptance training is a central component of mindfulness interventions for increasing positive affect after two weeks of daily training.
In contrast, all three active interventions were effective for decreasing negative affect on average, and there were no differences between MA and MO training. This finding is notable because, although there is ample evidence that mindfulness interventions can reduce negative affect (for reviews, see Keng et al., 2011; Khoury et al., 2013), some questions remain about whether mindfulness programs are more effective than active placebo controlled programs (e.g, Rosenkranz et al., 2013). The present results indicated that a 14-day mindfulness intervention provides equivalent negative affect reductions as a coping control training. This study suggests that mindfulness interventions uniquely enhance positive affect but may have little relative benefit for reducing negative affect above and beyond other placebo-controlled active treatments. It is also possible that negative affective states, as measured here, do not closely correspond to states of distress and other negative emotions assessed in clinical populations, with whom much research examining mindfulness training effects on affective outcomes has been conducted.
Notable strengths of Study 2 include its use of well-controlled and structurally equivalent intervention programs to isolate the active ingredients of mindfulness training and its high rates of participant retention (98%) and treatment adherence (96%) compared to longer group-based mindfulness interventions. Thus, these findings provide strong evidence that acceptance plays a key role in increasing positive affect following mindfulness training, and they demonstrate the efficacy and value of short-term smartphone-based mindfulness interventions for increasing well-being in populations who may not have access to in-person mindfulness programs. Indeed, smartphone-based mindfulness training approaches may reduce some of the practical and psychological barriers associated with more intensive group-based mindfulness interventions, while delivering similar benefits for positive emotions.
General Discussion
Happiness is known to improve personal relationships, career satisfaction, health, and overall satisfaction with life (Lyubomirsky, King, et al., 2005; Pressman & Cohen, 2005). Here we provide evidence from two pre-registered trials that mindfulness training interventions boost positive affect—and happiness in particular—in daily life. Notably, the affective benefits of mindfulness training compared to active control training were most robust for positive affect. In particular, although reductions in negative affect were observed following mindfulness training, Study 2 showed no relative advantage of mindfulness interventions for reducing negative affect compared to a placebo-controlled active treatment comparison group. Second, the present work contributes to a mechanistic understanding of how mindfulness interventions increase positive affect. In support of the Monitor + Accept hypothesis, removing acceptance skills training from mindfulness interventions significantly reduced positive affect benefits (approximately halving the magnitude of effects). This work offers the first experimental evidence that acceptance is a key mechanism of mindfulness interventions for boosting positive affect in daily life.
Specifically, the primary aim of the present studies was to test how the basic components of mindfulness training (monitoring and acceptance) increase positive affect in daily life. Across two RCTs, the inclusion of acceptance skills training (MA) increased daily life positive affect to a greater degree than training in monitoring momentary experience only (MO). These differences were magnified in end-of-day reports and were specific to feelings of happiness (i.e., happy, pleased, cheerful) across the two trials. As Kabat-Zinn (1990) intimates in the opening quote of this paper, the orientation of acceptance may be a key mechanism that broadens one’s awareness of affective cues so that positive stimuli may be accessed, monitored, and appreciated.
Comparing the effects of the two parallel studies also begins to offer clues about effective training length and delivery of mindfulness interventions for enhancing positive emotion. The two studies showed similar medium-to-large effect sizes on positive affect outcomes (ds=.70 for diary-assessed positive emotions; ds=.61 and .39 for momentary positive affect), indicating that just two weeks of mindfulness training without a “live” instructor was sufficient for boosting positive affect in daily life. The Study 2 results, in particular, also support the claim that it is the mindfulness-specific elements of training (monitoring and acceptance) that enhanced positive affect rather than positive expectations (placebo) or the influence of a supportive social environment.
How does practice in monitoring and accepting momentary experiences boost positive affect in daily life after mindfulness interventions? There are multiple component processes that drive these benefits. First, acute effects of mindfulness meditation practice (e.g., tranquility, happiness, appreciation, and joy; Garland, Farb, et al., 2015a; Moyer et al., 2011), are known to carry over into daily life (Shoham, Goldstein, Oren, Spivak, & Bernstein, 2017). Specifically, formal mindfulness practice focuses on noticing momentary emotions, thoughts, and sensations (i.e., monitoring) and observing each experience with equal receptivity regardless of affective content (i.e., acceptance); maintaining this equanimous, even-tempered attitude can trigger subtle pleasant emotions that carry over into daily life. The types of emotions thought to arise from mindfulness practice overlap with the specific types of positive affect impacted by the MA interventions investigated here, particularly happiness, cheer, calm, and ease. Second, previous studies indicate that brief mindfulness practice increases attention to positive stimuli (Kiken & Shook, 2011) and magnifies positive affective experience (Erisman & Roemer, 2010); it is possible that the acute positive emotions resulting from meditation practice may begin to retune the attentional system toward positive cues in the environment (Todd, Cunningham, Anderson, & Thompson, 2012). Indeed, positive emotions themselves are known to propagate more positive emotions (Wadlinger & Isaacowitz, 2006). Third, practicing nonreactivity toward one’s inner experiences may begin to retrain habitual reactivity to affective stimuli in the environment, further encouraging the attunement of attention to positive cues and experiences of positive affect in daily life. Fourth, when all affective experiences are treated with acceptance and equanimity, an array of subtle pleasant emotions and sensations can be savored as they unfold in each moment (Bryant, Chadwick, & Kluwe, 2011; Kiken, Lundberg, & Fredrickson, 2017) without being disrupted by a desire to prolong or cling to positive experiences. Finally, it is possible that the types of positive affect fostered through mindfulness training may broaden one’s attention, thoughts, and behaviors in ways that build lasting resources and reinforce positive states (Fredrickson, 1998, 2013). These pathways explaining how monitoring and acceptance increase positive affect were not directly tested here, but should be evaluated in future research, with the intriguing possibility that mindfulness practices can contribute to a self-reinforcing cycle of positive emotions over time.
These findings have basic research and applied implications for social, health, clinical, and positive psychology, and for contemplative science, domains in which mindfulness training is of active interest. In social psychology, positive emotional experience is known to have important influences on social behavior and relationships, career success, decision making, satisfaction with life, and resilience (Lyubomirsky et al., 2005), suggesting potential benefits of mindfulness training in a wide range of domains. This work also spurs additional theoretical questions about how mindfulness skill development links with social psychological perspectives on the self, emotion, and emotion regulation. First, changes in self processes may be an important pathway linking mindfulness skills with positive emotions and other intra- and interpersonal outcomes (Vago & Silbersweig, 2012). For example, developing mindful acceptance skills might promote a more stable sense of self-worth (Crocker & Knight, 2005) by reducing self-evaluative processing (Farb et al., 2007) and ego-involvement with present-moment experience (Brown & Leary, 2016). Further, this self-transcendence may encourage greater connection with others (Lindsay & Creswell, 2014), promoting compassion and prosocial behaviors (Berry et al., 2018; Condon, Desbordes, Miller, & DeSteno, 2013). Second, future work might explore whether mindfulness training decreases the disparity between desired affect and experienced affect (Tsai, 2007); in general, people want to be happier than they are, but acceptance skills may reduce this craving for ever-greater positive affect and allow for contentment with actual affective experience (Young, 2016). Finally, in the domain of emotion regulation, this work extends previous research showing that both acceptance and cognitive change (i.e., reappraisal; Ochsner & Gross, 2005) strategies are effective for regulating negative emotions, but that mindful acceptance strategies may be more useful for boosting positive emotions.
From a health psychology perspective, reductions in distress are one important pathway linking mindfulness training with improvements in physical health (Creswell & Lindsay, 2014), but the presence of positive emotions is a second important pathway that may independently promote physical health outcomes (for a review, see Pressman & Cohen, 2005). Thus, learning to accept present-moment experiences may initiate both stress reduction (Lindsay et al., 2018) and positive affect gains with downstream benefits for physical health. Similarly, though a large literature shows that mindfulness training is effective for reducing psychological distress (Keng et al., 2011) and symptoms of stress, depression, and anxiety in normative and clinical populations (Khoury et al., 2013), the present findings contribute to a second, less explored pathway highlighting the capacity for mindfulness to generate positive affect (Garland, Farb, et al., 2015a) and potentially promote mental health and well-being. For example, positive emotions may reduce the risk of depression relapse (Wichers et al., 2010), suggesting that mindfulness training with an emphasis on acceptance techniques might help to reduce relapse risk. Indeed, clinical research and theory has likewise described how an objective and decentered perspective toward experiences can be an important mechanism of change following mindfulness-based therapy (Fresco et al., 2007; Segal, Williams, & Teasdale, 2002; van der Velden et al., 2015). Providing concrete techniques for training acceptance skills, as done in these studies, may further encourage such adjuvant treatment. These findings also contribute to the evidence base of positive psychological interventions by helping to establish the effectiveness of mindfulness training for increasing positive emotions and identifying key features of this intervention (i.e., acceptance) that promote these effects (Ivtzan & Lomas, 2016).
Finally, these findings are important for theory and practice in contemplative science, where the contributions of the active components of mindfulness interventions to affective experience are unknown. The importance of acceptance in contemporary mindfulness interventions is the topic of ongoing debate among mindfulness intervention researchers and contemplative scientists (e.g., Bodhi, 2011; Dreyfus, 2011; Dunne, 2011; Grossman & Van Dam, 2011). A number of Buddhist practice traditions that include mindfulness training do not include acceptance as an explicit element (Bodhi, 2011), yet secular mindfulness-based interventions include both awareness and acceptance training (Lindsay & Creswell, 2017). Here we show that explicit instruction in acceptance is important for beginning meditators to reap the maximal benefits of mindfulness interventions on positive affect.
Although the study findings supported the Monitor + Accept hypothesis concerning increases in positive emotions, there was not compelling support for the secondary hypothesis concerning the contribution of acceptance training on reducing daily life negative affect. Instead, all active interventions were effective for reducing negative affect in daily life. Specifically, although Study 1 showed an advantage of MA training over MO training for decreasing hostility in daily life, both of these interventions reduced anxious affect and momentary negative affect. Likewise, reductions in negative affect were observed across all three interventions in Study 2, with no advantage of MA training over MO or active placebo-controlled training. Thus, reductions in negative affect in these studies appeared to be non-mindfulness-specific treatment effects; indeed, the negative affect results in particular may have been influenced by high treatment expectancies across all interventions, as the trainings were described to participants as stress management programs. Or, the negative affect measures reported here could have been relatively insensitive to changes in appraisal processes surrounding the experience of negative emotion that monitoring and acceptance skills might target (e.g., negative affect is experienced as less problematic). It is also possible that the studies lacked power to detect small differential effects of the interventions on negative affect; across both studies, MA tended to decrease negative affect more than MO, and MO tended to be superior to both active and no treatment control groups. Although post-hoc power analyses suggest that Study 1’s sample size was large enough to detect time × condition interactions on negative affect with a No Treatment control design (diary power=86%; EMA power=64%) (and both studies were powered for diary and EMA positive affect effects, ranging from 88-99% power), Study 2 was underpowered to detect small time × condition effects on negative affect comparing three active interventions (diary power=36%; EMA power=22%). Of course, it is also plausible that different forms of mindfulness training and coping skills training are equally effective in reducing negative affect; attention regulation (trained in the MA and MO programs), acceptance (trained in the MA program), and reappraisal (trained in the Coping control program) are all considered effective emotion regulation strategies for reducing negative affectivity (e.g., Wadlinger & Isaacowitz, 2006; Wolgast, Lundh, & Viborg, 2011; for a review, see Kohl, Rief, & Glombiewski, 2012). Indeed, the mindfulness interventions were not ineffective for reducing negative affect; the magnitude of pre- to post-MA-intervention change in both studies was comparable to negative affect reductions on a similar daily life measure following 8-week Mindfulness-Based Cognitive Therapy (Geschwind et al., 2011). Given the novelty of these training comparisons, further research is required to address these questions.
Although the evidence here supports the Monitor + Accept hypothesis, showing a benefit of MA over MO training for boosting positive affect across Studies 1 and 2, there is also some indication that training in Monitoring Only is moderately effective for increasing positive affect and reducing negative affect. There was no evidence that training in monitoring skills intensified negative affectivity, an important revision to MAT (Lindsay & Creswell, 2017). Although the trait tendency to monitor present experience has been linked with negative affectivity (e.g., Desrosiers et al., 2014; Pearson et al., 2015), meditation practice that develops monitoring skills is not detrimental and may instead lead to adaptive outcomes (Lindsay et al., 2018). By detecting and untangling emotions and sensations in the present moment, monitoring practice by itself may promote clarity and reduce sensory overload. Further, it is possible that, over longer periods of practice, systematic training in monitoring momentary experience becomes equally as effective as explicitly learning to monitor these experiences with acceptance. Practice in monitoring may begin to engender an implicit attitude of acceptance and equanimity toward experiences that both reduces the potency of negative emotions and allows positive stimuli to be noticed more frequently and savored in the moment.
One natural question that arises from these findings is whether training in attention monitoring is necessary for the effects of mindfulness interventions on boosting positive affect, or whether acceptance training alone is sufficient. Theoretically, monitoring and acceptance skills work together to boost positive emotions; acceptance may allow more positive stimuli to enter awareness, but monitoring is also necessary to deeply attend to and appreciate these stimuli in the present moment (Lindsay & Creswell, 2015). Consistent with this idea that acceptance alone may not be sufficient, recent evidence suggests that, although acceptance by itself is linked with lower negative affect, it is unrelated to positive affect (Ford et al., 2017). Practically, it may be challenging (or impossible) to develop acceptance skills without concurrently developing the ability to monitor present moment experiences. In the context of mindfulness interventions, acceptance is defined in relation to present-moment experiences; while attention monitoring can be practiced without explicit acceptance training, practicing an accepting attitude toward momentary body sensations and emotions fundamentally relies on first bringing attention to these experiences. Thus, monitoring and acceptance likely play complementary and synergistic roles in enhancing positive emotional experience.
Limitations and Future Research
The findings reported here are likely generalizable to adults motivated to engage in a stress management program. Two large pre-registered clinical trials conceptually replicated the basic finding that mindfulness interventions can increase positive emotions in diverse samples of stressed adults, with acceptance skills being particularly important for promoting these effects. These findings were consistent across different lengths of training (2 weeks vs. 8 weeks), different delivery methods (in-person group-based vs. individual smartphone-based), and different instructors and instructional techniques (MBSR-based instruction vs. Unified Mindfulness instruction). Moreover, the study samples included men and women across a wide range of ages, from 18-67 years in Study 1 and 18-65 years in Study 2, and the other demographic characteristics were generally representative of the larger Pittsburgh metropolitan area.
A few features of the study samples may affect generalizability. First, we recruited participants who reported an above average level of perceived stress. It is possible that stressed populations might have more room for intervention-related improvements in positive affect, although participants in both studies reported moderate baseline levels of positive affect on average. Still, stress tends to narrow attentional focus to threat-relevant features (e.g., Chajut & Algom, 2003; Derryberry & Tucker, 1994), limiting the ability to notice positive cues; mindfulness training, and acceptance skills in particular, may help to reduce fixation on stressful stimuli, broaden the scope of awareness, and allow greater access to positive stimuli specifically among stressed adults (Garland, Farb, et al., 2015a). Relatedly, not only were participants stressed, they also self-selected into a study intended to help manage stress; an interesting question is if people less motivated to engage in a stress management program are less responsive to mindfulness training (e.g., Lyubomirsky, Dickerhoof, Boehm, & Sheldon, 2011). Second, cultural differences in desired affective states could also impact motivation to seek out mindfulness interventions; promisingly, these studies provide evidence that mindfulness training boosts both high-arousal positive states (valued more in Western cultures) and low-arousal positive states (valued more in East Asian cultures) (Tsai, 2007), and thus may have cross-cultural appeal. Moreover, this research was conducted in a Western cultural context that values positive self-representation; Monitor+Accept mindfulness intervention effects may be more pronounced in East Asian cultural contexts where people are more prone to self-criticism (Heine & Hamamura, 2007), a tendency that acceptance training targets (e.g., Gilbert & Procter, 2006). Third, educational attainment was higher than the national average particularly in Study 1, a factor that may relate to higher adherence or motivation toward intervention content. Fourth, participants were smartphone owners, which may have limited our ability to reach a representative sample of lower SES and older adults (e.g., Poushter, 2016), although smartphone ownership is very high and continues to rise in these populations (e.g., Smith, 2015, 2017). As such, although we see these results as important and robust, there are additional research opportunities in testing these studies’ hypotheses in low stress populations, among stressed adults who may be less motivated to volunteer for research studies or engage in mindfulness training, in different cultural contexts, and among lower SES and older adult populations who may not own smartphones. Finally, it is important to acknowledge that mindfulness training is not the sole route to happiness, and it is currently unclear whether mindfulness training would have similar benefits for people who are high in trait positive emotionality, optimism, extraversion, self-esteem, or self-enhancement (Diener, Suh, Lucas, & Smith, 1999).
We note several additional limitations to address in future research. First, more work is needed to develop manipulation checks of monitoring and acceptance skill development in mindfulness interventions, given current debates about whether existing self-report measures of mindfulness skills have suitable discriminant validity (e.g., Goldberg et al., 2016; Visted, Vøllestad, Nielsen, & Nielsen, 2014). Second, neither study included a long-term follow-up assessment; increases in positive affect following mindfulness training might remain stable, continue to build, or decrease over time. Further research is required to assess the stability of positive affect gains observed here, as well as to explore positive affectivity outcomes using additional methods beyond self-report (e.g., observer- or peer-rated happiness: Choi et al., 2012; Sandvik, Diener, & Seidlitz, 1993; changes in positive vs. negative cognitive bias: Kiken & Shook, 2011) and to link these changes in positive affect with downstream social and health outcomes (e.g., healthcare utilization and symptoms, physiological markers, disease risk and progression; Creswell & Lindsay, 2014). Finally, it is unclear whether continued mindfulness practice is necessary for maintaining these benefits. Promisingly, mindfulness intervention RCTs suggest that certain benefits of training last through to follow-up even without continued formal practice (e.g., Creswell et al., 2016), perhaps due to integration of mindfulness skills into daily life via recursive processes (Cohen & Sherman, 2014; Walton, 2014). Indeed, mindfulness interventions—and acceptance training in particular—foster a new lens through which to view one’s experiences in daily life, which may alter attitudes and behaviors in ways that build positive emotions and provide feedback to reinforce this mindful perspective (Walton & Wilson, in press). However, the ability to implement mindfulness skills in daily life may fade without continued practice; formal meditation practice may be necessary to preserve training-based increases in mindfulness skills and positive affect over an extended time. In this regard, smartphone-based delivery of mindfulness instruction offers a convenient and, as such, promising means to promote ongoing practice.
Conclusion
Guided by a novel theoretical account, we conducted two pre-registered dismantling trials to test how the basic components of mindfulness interventions boost positive affect among stressed community adults. Across training length and delivery format, these studies provide the first experimental evidence that acceptance training is a key component of mindfulness interventions for increasing positive affect in daily life. Together, the studies emphasize the importance of learning to accept present-moment experiences for enhancing happiness, and suggest that mindfulness interventions may be tailored toward boosting positive emotions and their associated benefits.
Footnotes
We declare one potential conflict of interest, which has not influenced the authorship or content of this article: author Shinzen Young owns a portion of 01 Expert Systems, which will be releasing a modified and extended version of Study 2’s Monitor+Accept mindfulness intervention as a commercial app.
Age was missing from one participant; age average based on N=136 participants.
A portion of scheduled baseline surveys were never delivered to participants in Cohort 2 due to a technical problem with MetricWire software, resulting in data missing completely at random (MCAR).
Study managers who contacted participants during the intervention period were not blind to condition code. Study managers also infrequently served as experimenters in cases when blind research assistants were unavailable (e.g., during semester breaks). Including baseline experimenter blinding status as a covariate did not impact any of the results.
Trial Registration: Both RCTs are registered on clinicaltrials.gov (Study 1: NCT02502227; Study 2: NCT02433431).
References
- Aschbacher K, Epel E, Wolkowitz OM, Prather AA, Puterman E, & Dhabhar FS(2012). Maintenance of a positive outlook during acute stress protects against pro-inflammatory reactivity and future depressive symptoms. Brain, Behavior, and Immunity, 26(2), 346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using Self-Report Assessment Methods to Explore Facets of Mindfulness. Assessment, 13(1), 27–45. [DOI] [PubMed] [Google Scholar]
- Bartels M, & Boomsma DI (2009). Born to be Happy? The Etiology of Subjective Well-Being. Behavior Genetics, 39(6), 605–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry DR, Cairo AH, Goodman RJ, Quaglia JT, Green JD, & Brown KW (2018). Mindfulness increases prosocial responses toward ostracized strangers through empathic concern. Journal of Experimental Psychology: General, 147(1), 93. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G (2004). Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice, 11(3), 230–241. [Google Scholar]
- Bodhi B. (2011). What does mindfulness really mean? A canonical perspective. Contemporary Buddhism, 12(1), 19–39. [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013).Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health, 13(1), 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, Ganz PA (2015). Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer, 121(8), 1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brickman P, & Campbell DT (1971). Hedonic relativism and planning the good society. In Appley MH (Ed.), Adaptation level theory: A symposium (pp. 287–302). New York: Academic Press. [Google Scholar]
- Britton WB, Davis JH, Loucks EB, Peterson B, Cullen BH, Reuter L, Lindahl JR (2017). Dismantling Mindfulness-Based Cognitive Therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour Research and Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DB, Bravo AJ, Roos CR, & Pearson MR (2015). Five Facets of Mindfulness and Psychological Health: Evaluating a Psychological Model of the Mechanisms of Mindfulness. Mindfulness, 6(5), 1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Goodman RJ, & Inzlicht M (2013). Dispositional mindfulness and the attenuation of neural responses to emotional stimuli. Social Cognitive and Affective Neuroscience, 8(1), 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, & Leary MR (2016). The Oxford Handbook of Hypo-egoic Phenomena. Oxford University Press. [Google Scholar]
- Bryant FB, Chadwick ED, & Kluwe K (2011). Understanding the Processes that Regulate Positive Emotional Experience: Unsolved Problems and Future Directions for Theory and Research on Savoring. International Journal of Wellbeing, 1(1). [Google Scholar]
- Carson JW, Carson KM, Gil KM, & Baucom DH (2004). Mindfulness-based relationship enhancement. Behavior Therapy, 35(3), 471–494. [Google Scholar]
- Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, Samanez-Larkin GR, Nesselroade JR (2011). Emotional Experience Improves With Age: Evidence Based on Over 10 Years of Experience Sampling. Psychology and Aging, 26(1), 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalino LI, Arenander J, Epel E, & Puterman E (2017). Trait acceptance predicts fewer daily negative emotions through less stressor-related rumination. Emotion, 17(8), 1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh K, Strauss C, Cicconi F, Griffiths N, Wyper A, & Jones F (2013). A randomised controlled trial of a brief online mindfulness-based intervention. Behaviour Research and Therapy, 51(9), 573–578. [DOI] [PubMed] [Google Scholar]
- Center for Mindfulness - UMass Medical School. (n.d.). Retrieved from https://www.umassmed.edu/cfm [Google Scholar]
- Centre for Evaluation & Monitoring. (2018). Effect Size Calculator. Retrieved from https://www.cem.org/effect-size-calculator [Google Scholar]
- Chajut E, & Algom D (2003). Selective attention improves under stress: implications for theories of social cognition. Journal of Personality and Social Psychology, 85(2), 231. [DOI] [PubMed] [Google Scholar]
- Chang VY, Palesh O, Caldwell R, Glasgow N, Abramson M, Luskin F, Koopman C (2004). The effects of a mindfulness-based stress reduction program on stress, mindfulness self-efficacy, and positive states of mind. Stress and Health, 20(3), 141–147. [Google Scholar]
- Choi Y, Karremans JC, & Barendregt H (2012). The happy face of mindfulness:Mindfulness meditation is associated with perceptions of happiness as rated by outside observers. The Journal of Positive Psychology, 7(1), 30–35. [Google Scholar]
- Chopko B, & Schwartz R (2009). The Relation Between Mindfulness and Posttraumatic Growth: A Study of First Responders to Trauma-Inducing Incidents. Journal of Mental Health Counseling, 31(4), 363–376. [Google Scholar]
- Christopher MS, & Gilbert BD (2010). Incremental Validity of Components of Mindfulness in the Prediction of Satisfaction with Life and Depression. Current Psychology, 29(1), 10–23. [Google Scholar]
- Cohen GL, & Sherman DK (2014). The Psychology of Change: Self-Affirmation and Social Psychological Intervention. Annual Review of Psychology, 65(1), 333–371. [DOI] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. American Psychologist, 59(8), 676. [DOI] [PubMed] [Google Scholar]
- Cohen S, Alper CM, Doyle WJ, Treanor JJ, & Turner RB (2006). Positive Emotional Style Predicts Resistance to Illness After Experimental Exposure to Rhinovirus or Influenza A Virus. Psychosomatic Medicine, 68(6), 809–815. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Turner RB, Alper CM, & Skoner DP (2003). Emotional Style and Susceptibility to the Common Cold. Psychosomatic Medicine, 65(4), 652–657. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385. [PubMed] [Google Scholar]
- Cohen S, & Williamson G (1988). Perceived stress in a probability sample of the US. In Spacapam S & Oskamp S (Eds.), The social psychology of health: Claremont symposium on applied social psychology (pp. 31–67). Newbury Park, CA: Sage. [Google Scholar]
- Cohn MA, Fredrickson BL, Brown SL, Mikels JA, & Conway AM (2009).Happiness Unpacked: Positive Emotions Increase Life Satisfaction by Building Resilience. Emotion; (Washington, D.C.), 9(3), 361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condon P, Desbordes G, Miller WB, & DeSteno D (2013). Meditation Increases Compassionate Responses to Suffering. Psychological Science, 24(10), 2125–2127. [DOI] [PubMed] [Google Scholar]
- Conner TS, & Feldman Barrett L (2012). Trends in Ambulatory Self-Report: The Role of Momentary Experience in Psychosomatic Medicine. Psychosomatic Medicine, 74(4), 327–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, & Lindsay EK (2014). How Does Mindfulness Training Affect Health? A Mindfulness Stress Buffering Account. Current Directions in Psychological Science, 23(6), 401–407. [Google Scholar]
- Creswell JD, Pacilio LE, Lindsay EK, & Brown KW (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Taren AA, Lindsay EK, Greco CM, Gianaros PJ, Fairgrieve A, Ferris JL (2016). Alterations in resting state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biological Psychiatry, 80(1), 53–61. [DOI] [PubMed] [Google Scholar]
- Crocker J, & Knight KM (2005). Contingencies of self-worth. Current Directions in Psychological Science, 14(4), 200–203. [Google Scholar]
- Davidson KW, Mostofsky E, & Whang W (2010). Don’t worry, be happy: positive affect and reduced 10-year incident coronary heart disease: The Canadian Nova Scotia Health Survey. European Heart Journal, 31(9), 1065–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, & Dahl CJ (2017). Varieties of Contemplative Practice. JAMA Psychiatry, 74(2), 121–123. [DOI] [PubMed] [Google Scholar]
- Davis MC, & Zautra AJ (2013). An Online Mindfulness Intervention Targeting Socioemotional Regulation in Fibromyalgia: Results of a Randomized Controlled Trial. Annals of Behavioral Medicine, 46(3), 273–284. [DOI] [PubMed] [Google Scholar]
- Derryberry D, & Tucker DM (1994). Motivating the focus of attention. In Niedenthal PM & Kitayama S (Eds.), The heart’s eye: Emotional influences in perception and attention (pp. 167–196). San Diego, CA, US: Academic Press. [Google Scholar]
- Desbordes G, Gard T, Hoge EA, Hölzel BK, Kerr C, Lazar SW, Vago DR (2015). Moving Beyond Mindfulness: Defining Equanimity as an Outcome Measure in Meditation and Contemplative Research. Mindfulness, 6(2), 356–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desrosiers A, Vine V, Curtissue J, & Klemanski DH (2014). Observing nonreactively: A conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. Journal of Affective Disorders, 165, 31–37. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, & Borkovec TD (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry, 31(2), 73–86. [DOI] [PubMed] [Google Scholar]
- Diener E, Suh EM, Lucas RE, & Smith HL (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125(2), 276. [Google Scholar]
- Dreyfus G (2011). Is mindfulness present-centred and non-judgmental? A discussion of the cognitive dimensions of mindfulness. Contemporary Buddhism, 12(1), 41–54. [Google Scholar]
- Dunn EW, Aknin LB, & Norton MI (2008). Spending money on others promotes happiness. Science, 319(5870), 1687–1688. [DOI] [PubMed] [Google Scholar]
- Dunne J (2011). Toward an understanding of non-dual mindfulness. Contemporary Buddhism, 12(01), 71–88. [Google Scholar]
- Emmons RA, & McCullough ME (2003). Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology, 84(2), 377–389. [DOI] [PubMed] [Google Scholar]
- Erisman SM, & Roemer L (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion, 10(1), 72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Anderson AK, Mayberg H, Bean J, McKeon D, & Segal ZV (2010). Minding one’s emotions: Mindfulness training alters the neural expression of sadness. Emotion, 10(1), 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, & Anderson AK (2007). Attending to the Present: Mindfulness Meditation Reveals Distinct Neural Modes of Self-Reference. Social Cognitive and Affective Neuroscience, 2(4), 313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felsman P, Verduyn P, Ayduk O, & Kross E (2017). Being present: Focusing on the present predicts improvements in life satisfaction but not happiness. Emotion, 17(7), 1047. [DOI] [PubMed] [Google Scholar]
- Folkman S, & Moskowitz JT (2000). Positive affect and the other side of coping. American Psychologist, 55(6), 647–654. [DOI] [PubMed] [Google Scholar]
- Ford BQ, Lam P, John OP, & Mauss IB (2017). The Psychological Health Benefits of Accepting Negative Emotions and Thoughts: Laboratory, Diary, and Longitudinal Evidence. Journal of Personality and Social Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foust J (2014). Body-Centered Inquiry; Louisville, CO: Sounds True. Retrieved from https://www.soundstrue.com/store/body-centered-inquiry-5896.html [Google Scholar]
- Fredrickson BL (1998). What Good Are Positive Emotions? Review of General Psychology, 2(3),300–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2013). Positive Emotions Broaden and Build. In Devine P & Plant A (Eds.),Advances in Experimental Social Psychology (Volume. 47, pp. 1–53). Burlington: Academic Press. [Google Scholar]
- Fredrickson BL, Boulton AJ, Firestine AM, Van Cappellen P, Algoe SB, Brantley MM, Salzberg S (2017). Positive Emotion Correlates of Meditation Practice: a Comparison of Mindfulness Meditation and Loving-Kindness Meditation. Mindfulness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Branigan C (2005). Positive emotions broaden the scope of attention and thought-action repertoires. Cognition & Emotion, 19(3), 313–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, & Finkel SM (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Joiner T (2002). Positive Emotions Trigger Upward Spirals Toward Emotional Well-Being. Psychological Science, 13(2), 172–175. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, & Levenson RW (1998). Positive Emotions Speed Recovery from the Cardiovascular Sequelae of Negative Emotions. Cognition & Emotion, 12(2), 191–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, van Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, & Williams JMG (2007). Initial Psychometric Properties of the Experiences Questionnaire: Validation of a Self-Report Measure of Decentering. Behavior Therapy, 38(3), 234–246. [DOI] [PubMed] [Google Scholar]
- Fujita F, & Diener E (2005). Life Satisfaction Set Point: Stability and Change. Journal of Personality and Social Psychology, 88(1), 158–164. [DOI] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin PR, & Fredrickson BL (2015a). Mindfulness Broadens Awareness and Builds Eudaimonic Meaning: A Process Model of Mindful Positive Emotion Regulation. Psychological Inquiry, 26(4), 293–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Farb NA, Goldin PR, & Fredrickson BL (2015b). The Mindfulness-to-Meaning Theory: Extensions, Applications, and Challenges at the Attention–Appraisal–Emotion Interface. Psychological Inquiry, 26(4), 377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Geschwind N, Peeters F, & Wichers M (2015). Mindfulness training promotes upward spirals of positive affect and cognition: multilevel and autoregressive latent trajectory modeling analyses. Frontiers in Psychology, 6, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Hanley AW, Goldin PR, & Gross JJ (2017). Testing the mindfulness-to-meaning theory: Evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLOS ONE, 12(12), e0187727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Drukker M, van Os J, & Wichers M (2011). Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 618–628. [DOI] [PubMed] [Google Scholar]
- Gilbert P, & Procter S (2006). Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 13(6), 353–379. [Google Scholar]
- Glück TM, & Maercker A (2011). A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry, 11(1), 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenka SN (1994). Discourse summaries: Evening Discourses by Goenka S.N. from a Ten-Day Course of Vipassana. Onalaska, WA: Pariyatti Publishing. [Google Scholar]
- Goldberg SB, Wielgosz J, Dahl C, Schuyler B, MacCoon DS, Rosenkranz M, Davidson RJ (2016). Does the Five Facet Mindfulness Questionnaire measure what we think it does? Construct validity evidence from an active controlled randomized clinical trial. Psychological Assessment, 28(8), 1009–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga E, Gould N, Rowland-Seymour A, Sharma R, Haythornthwaite J (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P, & Van Dam NT (2011). Mindfulness, by any other name: trials and tribulations of sati in western psychology and science. Contemporary Buddhism, 12(1), 219–239. [Google Scholar]
- Gruber J, Mauss IB, & Tamir M (2011). A Dark Side of Happiness? How, When, and Why Happiness Is Not Always Good. Perspectives on Psychological Science, 6(3), 222–233. [DOI] [PubMed] [Google Scholar]
- Hamill TS, Pickett SM, Amsbaugh HM, & Aho KM (2015). Mindfulness and acceptance in relation to Behavioral Inhibition System sensitivity and psychological distress. Personality and Individual Differences, 72, 24–29. [Google Scholar]
- Hayes SC (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35(4), 639–665. [DOI] [PubMed] [Google Scholar]
- Heine SJ, & Hamamura T (2007). In search of East Asian self-enhancement. Personality and Social Psychology Review, 11(1), 4–27. [DOI] [PubMed] [Google Scholar]
- Howells A, Ivtzan I, & Eiroa-Orosa FJ (2016). Putting the ‘app’ in Happiness: A Randomised Controlled Trial of a Smartphone-Based Mindfulness Intervention to Enhance Wellbeing. Journal of Happiness Studies, 17(1), 163–185. [Google Scholar]
- Ivtzan I, & Lomas T (2016). Mindfulness in Positive Psychology: The Science of Meditation and Wellbeing. Routledge. [Google Scholar]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, & Schwartz GER. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33(1), 11–21. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: The program of the stress reduction clinic at the University of Massachusetts Medical Centre. New York: Dell. [Google Scholar]
- Kashdan TB, Barrios V, Forsyth JP, & Steger MF (2006). Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behaviour Research and Therapy, 44(9), 1301–1320. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, & Breen WE (2007). Materialism and Diminished Well–Being: Experiential Avoidance as a Mediating Mechanism. Journal of Social and Clinical Psychology, 26(5), 521–539. [Google Scholar]
- Keng S-L, Smoski MJ, & Robins CJ (2011). Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review, 31(6), 1041–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesebir P, & Diener E (2008). In Pursuit of Happiness: Empirical Answers to Philosophical Questions. Perspectives on Psychological Science, 3(2), 117–125. [DOI] [PubMed] [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Hofmann SG (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. [DOI] [PubMed] [Google Scholar]
- Kiken LG, Lundberg KB, & Fredrickson BL (2017). Being Present and Enjoying It:Dispositional Mindfulness and Savoring the Moment Are Distinct, Interactive Predictors of Positive Emotions and Psychological Health. Mindfulness, 8(5), 1280–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiken LG, & Shook NJ (2011). Looking Up: Mindfulness Increases Positive Judgments and Reduces Negativity Bias. Social Psychological and Personality Science, 2(4), 425–431. [Google Scholar]
- Killingsworth MA, & Gilbert DT (2010). A Wandering Mind Is an Unhappy Mind. Science, 330(6006),932–932. [DOI] [PubMed] [Google Scholar]
- King LA, Hicks JA, Krull JL, & Del Gaiso AK (2006). Positive affect and the experience of meaning in life. Journal of Personality and Social Psychology, 90(1), 179–196. [DOI] [PubMed] [Google Scholar]
- Kohl A, Rief W, & Glombiewski JA (2012). How effective are acceptance strategies? A meta-analytic review of experimental results. Journal of Behavior Therapy and Experimental Psychiatry, 43(4), 988–1001. [DOI] [PubMed] [Google Scholar]
- Kratz AL, Davis MC, & Zautra AJ (2007). Pain Acceptance Moderates the Relation Between Pain and Negative Affect in Osteoarthritis and Fibromyalgia Patients. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine, 33(3), 291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2014). Helping the self help others: Self-affirmation increases self-compassion and pro-social behaviors. Frontiers in Psychology, 5, 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2015). Back to the Basics: How Attention Monitoring and Acceptance Stimulate Positive Growth. Psychological Inquiry, 26(4), 343–348. [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review, 51, 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Smyth JM, Brown KW, & Creswell JD (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology, 87, 63–73. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Dickerhoof R, Boehm JK, & Sheldon KM (2011). Becoming happier takes both a will and a proper way: An experimental longitudinal intervention to boost well-being. Emotion, 11(2), 391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, & Diener E (2005). The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin, 131(6), 803–855. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Sheldon KM, & Schkade D (2005). Pursuing happiness: The architecture of sustainable change. Review of General Psychology, 9(2), 111. [Google Scholar]
- Machell KA, Goodman FR, & Kashdan TB (2015). Experiential avoidance and well-being: A daily diary analysis. Cognition and Emotion, 29(2), 351–359. [DOI] [PubMed] [Google Scholar]
- Marsland AL, Pressman S, & Cohen S (2007). Positive affect and immune function. In Ader R (Ed.), Psychoneuroimmunology (pp. 761–779). [Google Scholar]
- Mennin DS, Ellard KK, Fresco DM, & Gross JJ (2013). United We Stand: Emphasizing Commonalities Across Cognitive-Behavioral Therapies. Behavior Therapy, 44(2), 234–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno PI, Moskowitz AL, Ganz PA, & Bower JE (2016). Positive affect and inflammatory activity in breast cancer survivors: examining the role of affective arousal. Psychosomatic Medicine, 78(5), 532–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. [Google Scholar]
- Morris SB, & DeShon RP (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 7(1), 105. [DOI] [PubMed] [Google Scholar]
- Nyklicek I, & Kuijpers KF (2008). Effects of Mindfulness-Based Stress ReductionIntervention on Psychological Well-being and Quality of Life: Is Increased Mindfulness Indeed the Mechanism? Annals of Behavioral Medicine, 35(3), 331–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyklíček I, Mommersteeg PMC, Van Beugen S, Ramakers C, & Van Boxtel GJ (2013). Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychology, 32(10), 1110–1113. [DOI] [PubMed] [Google Scholar]
- Ochsner K, & Gross J (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9(5), 242–249. [DOI] [PubMed] [Google Scholar]
- Ong AD, Bergeman CS, Bisconti TL, & Wallace KA (2006). Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology, 91(4), 730–749. [DOI] [PubMed] [Google Scholar]
- Parks AC, & Biswas-Diener R (2013). Positive interventions: Past, present and future. In Kashdan TB & Ciarrochi J (Eds.), Bridging acceptance and commitment therapy and positive psychology: A practitioner’s guide to a unifying framework. Oakland, CA: New Harbinger. [Google Scholar]
- Pearson MR, Lawless AK, Brown DB, & Bravo AJ (2015). Mindfulness and emotional outcomes: Identifying subgroups of college students using latent profile analysis. Personality and Individual Differences, 76, 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poushter J (2016). Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies. Pew Research Center. [Google Scholar]
- Pressman SD, & Cohen S (2005). Does positive affect influence health? Psychological Bulletin, 131(6), 925–971. [DOI] [PubMed] [Google Scholar]
- Quaglia JT, Brown KW, Lindsay EK, Creswell JD, & Goodman RJ (2014). From Conceptualization to Operationalization of Mindfulness. In Handbook of mindfulness: Theory, research, and practice. New York: Guilford. [Google Scholar]
- Rahl HA, Lindsay EK, Pacilio LE, Brown KW, & Creswell JD (2017). Brief Mindfulness Meditation Training Reduces Mind Wandering: the Critical Role of Acceptance Training. Emotion, 17(4), 224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenkranz MA, Davidson RJ, MacCoon DG, Sheridan JF, Kalin NH, & Lutz A (2013). A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity, 27, 174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandvik E, Diener E, & Seidlitz L (1993). Subjective well-being: The convergence and stability of self-report and non-self-report measures. Journal of Personality, 61(3), 317–342. [Google Scholar]
- Schroevers MJ, & Brandsma R (2010). Is learning mindfulness associated with improved affect after mindfulness-based cognitive therapy? British Journal of Psychology, 101(1), 95–107. [DOI] [PubMed] [Google Scholar]
- Schumer MC, Lindsay EK, & Creswell JD (in press). Brief Mindfulness Training for Negative Affectivity: A Systematic Review and Meta-Analysis. Journal of Consulting and Clinical Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2002). Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. Guilford Press. [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Annual Review of Clinical Psychology, 4(1), 1–32. [DOI] [PubMed] [Google Scholar]
- Shoham A, Goldstein P, Oren R, Spivak D, & Bernstein A (2017). Decentering in the process of cultivating mindfulness: An experience-sampling study in time and context. Journal of Consulting and Clinical Psychology, 85(2), 123. [DOI] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. [DOI] [PubMed] [Google Scholar]
- Smith A (2015). U.S. Smartphone Use in 2015. Retrieved from http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/ [Google Scholar]
- Smith A (2017, January 12). Record shares of Americans have smartphones, home broadband. Retrieved from http://www.pewresearch.org/fact-tank/2017/01/12/evolumeution-of-technology/ [Google Scholar]
- Smyth JM, Juth V, Ma J, & Sliwinski M (2017). A slice of life: Ecologically valid methods for research on social relationships and health across the life span. Social and Personality Psychology Compass, 11(10), e12356. [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, & Brydon L (2004). Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology, 29(5), 593–611. [DOI] [PubMed] [Google Scholar]
- Swann WB (1983). Self-verification: Bringing social reality into harmony with the self. Social Psychological Perspectives on the Self, 2, 33–66. [Google Scholar]
- Thomas DL, & Diener E (1990). Memory accuracy in the recall of emotions. Journal of Personality and Social Psychology, 59(2), 291–297. [Google Scholar]
- Todd RM, Cunningham WA, Anderson AK, & Thompson E (2012). Affect-biased attention as emotion regulation. Trends in Cognitive Sciences, 16(7), 365–372. [DOI] [PubMed] [Google Scholar]
- Trungpa C (2005). Training the Mind & Cultivating Loving-kindness. Boston: Shambhala Publications. [Google Scholar]
- Tsai JL (2007). Ideal affect: Cultural causes and behavioral consequences. Perspectives on Psychological Science, 2(3), 242–259. [DOI] [PubMed] [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient Individuals Use Positive Emotions to Bounce Back From Negative Emotional Experiences. Journal of Personality and Social Psychology, 86(2), 320–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vago DR, & Silbersweig DA (2012). Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience, 6, 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Piet J (2015). A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review, 37, 26–39. [DOI] [PubMed] [Google Scholar]
- Visted E, Vøllestad J, Nielsen MB, & Nielsen GH (2014). The Impact of Group-Based Mindfulness Training on Self-Reported Mindfulness: a Systematic Review and Meta-analysis. Mindfulness, 6(3), 501–522. [Google Scholar]
- Wadlinger HA, & Isaacowitz DM (2006). Positive mood broadens visual attention to positive stimuli. Motivation and Emotion, 30(1), 87–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton GM (2014). The new science of wise psychological interventions. Current Directions in Psychological Science, 23(1), 73–82. [Google Scholar]
- Walton GM, & Wilson TD (in press). Wise interventions: Psychological remedies for social and personal problems. Psychological Review. [DOI] [PubMed] [Google Scholar]
- Warttig SL, Forshaw MJ, South J, & White AK (2013). New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). Journal of Health Psychology, 18(12), 1617–1628. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1997). Measurement and Mismeasurement of Mood: Recurrent and Emergent issueues. Journal of Personality Assessment, 68(2), 267–296. [DOI] [PubMed] [Google Scholar]
- Wichers M, Peeters F, Geschwind N, Jacobs N, Simons CJP, Derom C, van Os J (2010). Unveiling patterns of affective responses in daily life may improve outcome prediction in depression: A momentary assessment study. Journal of Affective Disorders, 124(1–2), 191–195. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, Von Rohr IR (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82(2), 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Russell I, & Russell D (2008). Mindfulness-based cognitive therapy: further issueues in current evidence and future research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiseheart M (2013). Effect Size Calculator. Retrieved from http://www.cognitiveflexibility.org/effectsize/ [Google Scholar]
- Wolgast M, Lundh L-G, & Viborg G (2011). Cognitive reappraisal and acceptance: An experimental comparison of two emotion regulation strategies. Behaviour Research and Therapy, 49(12), 858–866. [DOI] [PubMed] [Google Scholar]
- Young S (2016). What Is Mindfulness? A Contemplative Perspective. In Schonert-Reichl KA & Roeser RW (Eds.), Handbook of Mindfulness in Education (pp. 29–45). Springer New York. [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassario P, Tennen H, Finan P, Irwin MR (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology, 76(3), 408–421. [DOI] [PubMed] [Google Scholar]