Abstract
Purpose
To report the clinical findings and management of a case of occipital lobe infarction with homonymous quadrantanopia in a patient treated with vitamins and coenzyme Q10.
Observations
A currently 69-years-old patient presenting in 2007 left inferior quadrantanopia following a right occipital lobe stroke with initial visual field index of 82% and 79% in the right and left eyes, respectively. From 2007 to 2010 was treated with vitamin and antioxidant complexes, without specific signs of changes observed in the visual field (81% right eye, 79% left eye). In 2011 was treated for the first time with coenzyme Q10 (Active complex® Q10 Gold 100 mg) in addition to the vitamin and antioxidant supplementation. A promptly slight improvement of the visual field in both eyes was observed. In 2013, a remarkable improvement was noticed observing a slight scotoma where previously presented the quadrantanopia. Thereafter, in the successive one-year follow-up examinations the patient experienced an exponential improvement in the visual field with gradually fading of the scotoma. Currently the patient no longer presents any sign of quadrantanopia, with normal visual field in both eyes (99% right eye, 98% left eye).
Conclusion and importance
Spontaneous improvement more than 6 months after stroke is thought to be unlikely. However, we observed, for the first time, an amelioration of the visual field after 10 years of an occipital lobe stroke. The combination of vitamins and coenzyme Q10 (100 mg) improved the prognosis with significant recovery of the visual field, which is impossible to recover under current knowledge.
Keywords: Stroke, Occipital lobe, Homonymous quadrantanopia, Vitamins, Coenzyme Q10
1. Introduction
Visual field defects following cerebral insults are very prevalent, with frequencies ranging from 8.3 to 25%. 1, 2 When homonymous visual field defects occurs following damage to the neural visual pathway, specifically damage posterior to the optic chiasma, the same part of the visual field is affected in both eyes. Homonymous hemianopia is a visual field defect involving either two right or the two left halves of the visual field of both eyes, while the loss of one quarter of visual field on one side in both eyes is referred to as homonymous quadrant hemianopia or quadrantanopia. Hemianopia and quadrantanopia are consequence of injuries mainly in the occipital, the parietal and the temporal lobes,3 with high impact upon the quality of life of individuals.4
Approximately 60% of patients could experience spontaneous improvement in the visual field, usually within the first month after brain injury. However, the spontaneous improvement in the first 6 months decreases progressively with every successive month, while complete recovery is rare and beyond 6 months is unlikely.5, 6, 7 Therefore, any documented improvement in the visual field of treated patients, with signs of quadrantanopia after 6 months post-injury, would be a sign of therapeutic efficacy. We report a case of occipital lobe infarction with homonymous quadrantanopia in a patient treated with vitamins and coenzyme Q10, with significant visual field recovery, 10 years after the cerebral insult.
2. Case report
A currently 69-years old male patient suffered in 2007 a right occipital lobe stroke with left inferior homonymous quadrantanopia (retrochiasmal lesion of the visual pathway). Magnetic resonance imaging of the brain at the time of his stroke demonstrated an infarct in the right occipital lobe (see Fig. 1, panel a). He had no significant past ocular history, nor did he report history of autoimmune disorder, or neurological disorders. Visual acuities were 20/20 in each eye. OCT analysis, retinography and fundus examination were normal. The patient did not receive restorative training, optical aids, or compensatory training. Diagnostic was carried out using the Humphrey field analyzer (HFA) instrument and 30-2 testing algorithm. The visual field index (VFI) was obtained to evaluate the percentage of the remaining visual field of the right eye (OD) and the left eye (OS), respectively.
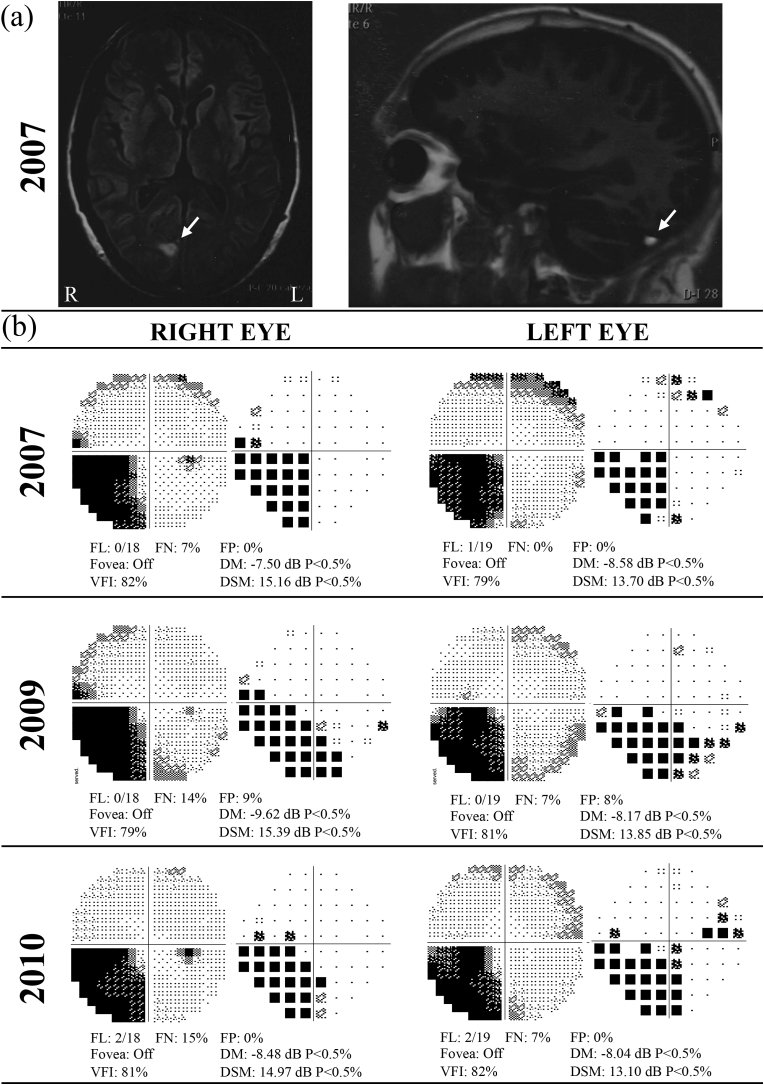
Fig. 1.
(a) Brain magnetic resonance imaging (MRI) at the time of the stroke revealed an infarct in the right occipital lobe (white arrow). (b) Visual field test using the Humphrey field analyzer (HFA) and 30-2 algorithm, from 2007 to 2010. Rows represents the right and left visual fields of each respective eye. In 2007 the patient presented left inferior homonymous quadrantanopia. From 2007 to 2010 was treated with Visan, Hidroxil and Acfol, with no changes in the visual field index were observed.
Upon initial examination in 2007, the patient presented VFI of 82% (OD) and 79% (OS), as shown Fig. 1 (panel b). A systemic treatment consisting of Adiro 300 (Bayer, Germany), Visan (Théa laboratories, France), Hidroxil (Almirall, Spain) and Acfol (Italfarmaco, Italy) was prescribed. Every other month the patient took Hidroxil B12, B6, B1 (1 tablet each breakfast, lunch and dinner) and Acfol (1 tablet at breakfast), while in the rest month took Visan (1 tablet at breakfast), for a year. The active ingredient of Adiro 300 is acetylsalicylic acid and is used for stroke (antiplatelet). Hidroxil active ingredients include vitamins B1 (250 mg thiamin), B6 (250 mg pyridoxine) and B12 (500 mg cyanocobalamin). Acfol active ingredient is folic acid (5 mg). Visam nutritional supplement contains trace elements (e.g. zinc, copper, selenium, manganese), vitamins (A, C, E, B1—B12), lutein, zeaxanthin, glutathione, flavonoids and low levels of coenzyme Q10 (2.5 mg).
At two-year follow-up, i.e., 2009, according to Fig. 1 no changes were observed in the VFI (79% OD, 81% OS), maintaining the same treatment prescribed. We observed signs of peripheral cortical cataract (OD) and nuclear sclerosis of the lens (OI), presenting normal optic papilla, macula and retinal vascularization. In 2010 no significant changes were observed in the VFI (81% OD, 82% OS), as shown in Fig. 1 (panel b), and the same treatment was prescribed. Sign of cataracts in OD and OI was observed, while optic papilla, macula, retinal neovascularization and retinal periphery were normal.
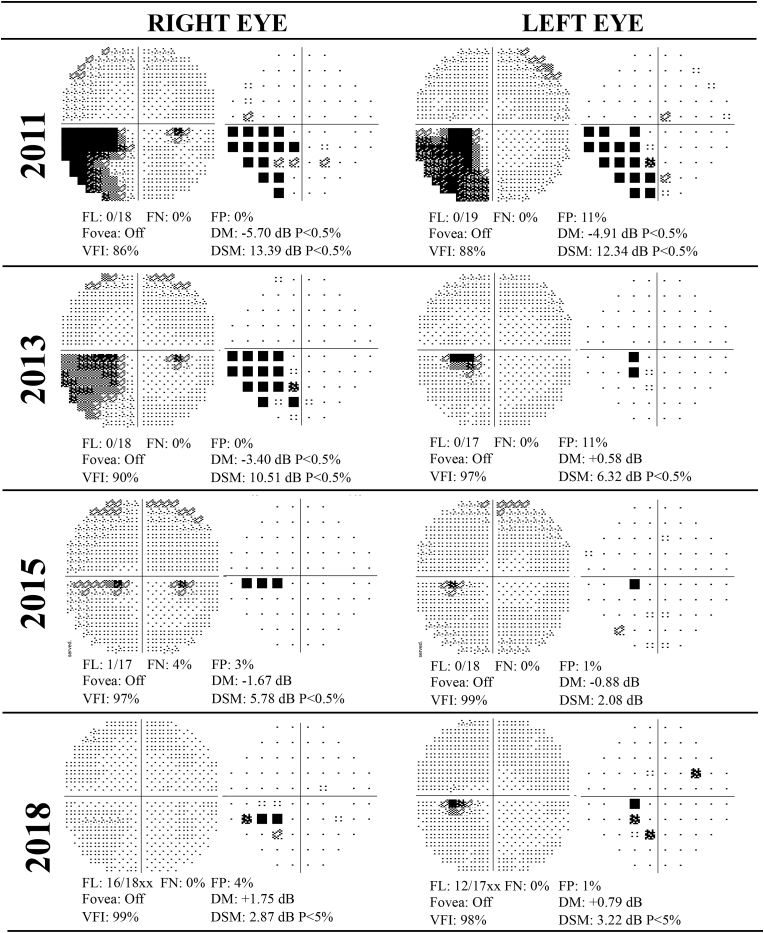
In 2011 Active complex® Q10 Gold 100 mg (Pharma Nord, Dennmark), containing 100 mg of CoQ10 and 25 mg of vitamin C, was prescribed in alternate months (1 tablet at lunch, following manufacturer dosage guidelines), additional to Hidroxil, Acfol and Visan supplements, over a period of one year. As shown Fig. 2, the VFI in 2011 presented a promptly slight improvement of the visual field in both eyes (86% OD, 88% OS). At one-year follow up of the patient a remarkable improvement was observed in the visual field index of both eyes (91% OD, 96% OS), presenting minimal inferonasal quadrantanopia with central scotoma in the right eye and minimal inferotemporal quadrantanopia with small scotoma in the left eye. The remaining ocular parameters were normal.
Fig. 2.
Visual field test using the Humphrey field analyzer (HFA) and 30-2 algorithm, from 2011 to 2018. Rows represents the right and left visual fields of each respective eye. In 2007 the patient presented left inferior homonymous quadrantanopia. In 2011 was treated for the first time with coenzyme Q10 (Active complex® Q10 Gold 100 mg). The visual field index improved progressively until now.
In 2013 (Fig. 2), the VFI was notably improved, reaching 90% (OD) and 96% (OS). In the left eye a slight scotoma was present where the quadrantanopia was previously observed. In the right an inferonasal quadrantanopia was still present with minimum scotoma and minimal alteration in the RPE, while optic papilla, macula, retinal vascularization and periphery were normal. Medical prescription was virtually maintained, but one tablet of Active complex® Q 10 Gold 100 mg was prescribed for daily treatment along all the successive months.
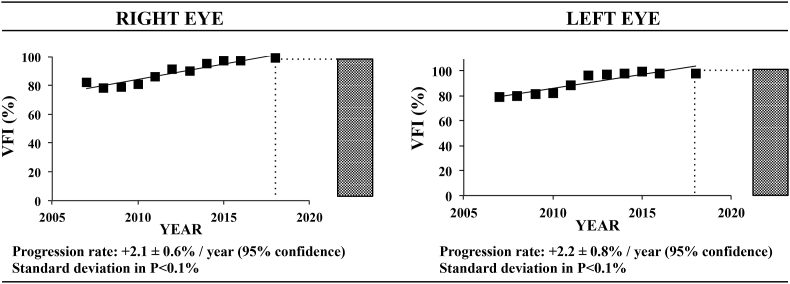
In the successive one-year follow up examinations (2014–2018), the patient experimented an exponential improvement in the visual field with gradually removal of the scotoma. At present time, the patient no longer shows any sign of quadrantanopia, with normal visual field index in both eyes (99% OD, 98% OS). Summarizing, the VFI of right and left eyes are plotted in Fig. 3, from 2007 (stroke event) to 2018. The patient presented a progression rate of +2.1 ± 0.6% per year in the OD, and +2.2 ± 0.8% per year in the OS, at 95% confidence, with significant enhancement of the visual field maintaining the prescribed treatment, which includes daily CoQ10 supplementation.
Fig. 3.
The visual field index (VFI) of right and left eyes plotted from 2007 (stroke event) to 2018. Progression rates at 95% confidence are shown.
3. Discussion
Visual field defects are common after stroke, trauma, tumor, brain surgery, and demyelinating lesions, affecting specifically up to 25% of all stroke survivors.1,8 The impact on daily activities is significant, with poor mobility, collisions, impaired reading and driving skills, and increased dependence and disability.9 Lesions affecting postchiasmal afferent nerve pathways generally produce homonymous visual field loss, which may be a hemianopia or quadrantanopia depending on the location of the lesion. The term hemianopia describes visual defects that occupy about one-half of an eye's visual field, while quadrantanopia describes defects confined mostly to about one-fourth of an eye's visual field.10 The exact type of homonymous defect depends on the specific location of the injury, its extent and the presence of other lesions.11 Our patient presented a right occipital lobe stroke with left inferior homonymous quadrantanopia, which is the most common location of the lesion (45% of cases).6
Spontaneous visual field improvement or restoration is common and occurs in early weeks to few months,5 probably mediated by the removal of the cerebral edema with concomitant restitution of surrounding non-infarcted penumbral tissue, with reports ranging from 7% to 85% of clinical cases.12,13 The recovery is variable, depending on the degree of neuronal death and stunning in the damaged visual pathways, as well as the resolution of the initial effects of the acute injury.14 Approximately 60% of patients could experience spontaneous improvement, usually within the first month after injury, and in some case a few months later but does not extend thereafter.7 In a recent study on the natural history of homonymous hemianopia, spontaneous improvement of the visual field defect has been observed in 38% of patients.15 The approximate maximal period of spontaneous recovery is typically 3 months.14 In our case, the improvement in the visual field of the patient began to occur more than 4 years after the lesion, with significant recovery 10 years later, and therefore is not likely as a result of spontaneous recovery.
Visual field improvement is usually defined as an amelioration of the field defect with significant changes in mean and pattern deviations in Humphrey visual fields. The percentage of field recovery is variable and depends upon individual.16 No other factor including age seems to affect significantly the visual field improvement. The natural history of visual field recovery is fundamental when evaluating claims of improvement by potential rehabilitation therapy or treatments for homonymous hemianopia or quadrantanopia.17 We observed an amelioration in the visual field, along the ten years of follow-up of our patient, from 82% (OD) and 79% (OS) in 2007 to 99% (OD) and 98% (OS) in 2018 with progression rates >2% per year in both eyes.
Post stroke treatment includes the identification of the stroke etiology, the modification of risk factors to prevent reoccurrences, and the initiation of an early and intensive rehabilitation therapy allowing functional outcomes and improving the disability.18,19 Interventions in patients diagnosed with homonymous quadrantanopia or hemianopia are focused on their rehabilitation through optical therapies, compensatory therapies, and visual field restitution therapies based on the hypothesis of plasticity, which has been attracted increasing attention in recent years.2,12,20,21 The use of optical aids pursues to expand artificially the visual field, the compensatory training attempts to alleviate the resulting disability by teaching patients to make more efficient eye-movements, and the restorative therapy aims to reduce the visual field loss through prolonged training.12 However, our patient did not receive any of those interventions, and therefore the improvement in the visual field observed was not as the result of improved neither compensation nor rehabilitation therapy.
The use of nutritional supplements in the treatment of visual field defects including quadrantanopia is widely recommended, although there is a lack of standard pharmacological treatments or broadly accepted nutritional recommendations. Nutritional supplements including vitamins (A, C, E and B) and antioxidants are commonly used but available evidence of their effectiveness is scarce and inconsistent. Among the supplements suggested, coenzyme Q10 (CoQ10 or ubiquinone) has been extensively used to treat aging, stroke, retinal diseases, but no effects on homonymous quadrantanopia has been published to date.22 Our patient was prescribed from 2007 to 2010 with vitamin, folic acid and antioxidant supplements, with no changes in the visual field were observed. In 2011, the treatment was complemented with Active complex® Q10 Gold 100 mg at high doses, i.e., containing 100 mg of CoQ10. While the recovery progression rate of the visual field of the patient remained constant from 2007 to 2010, we observed a great improvement of the recovery since the patient was prescribed with CoQ10 treatment in 2011 until present.
Given that spontaneous improvement has not been noted in patients with stroke after 6 months and that our patient did not receive any formal visual field training or optical aids, the improvement seen by our patient is most likely as result of CoQ10 treatment. CoQ10, also known as ubiquinone, ubidecarenone or coenzyme Q, is a 1,4-benzoquinone where Q refers to the quinone chemical group, and 10 refers to the number of isoprenyl chemical subunits in its tail. CoQ10, the most common coenzyme Q in humans, is an essential cofactor of the electron transport chain and acts by maintaining the mitochondrial membrane potential, supporting ATP synthesis and inhibiting reactive oxygen species generation for protecting neuronal cells against oxidative stress in neurodegenerative diseases.23,24
Various mechanisms for the beneficial effects of CoQ10 have been suggested including its neuroprotective role, which underlying pathways may involve a dual function, acting as a free radical scavenger and activating the mitochondrial function.25,26 Pretreatment with CoQ10 may protect neuronal cells against oxidative stress stabilizing the mitochondrial membrane and reduced the amount of mitochondrial reactive oxidative species generation.22,27 Moreover, the antioxidant function of CoQ10 is of great importance in the plasma membrane by reducing vitamins C and E.28 Recent studies in animal models showed that pretreatment with CoQ10 ameliorated ischemic injury by regulating the antioxidant defense and mitochondrial function.29,30
Overall, CoQ10 may play a significant role in treating neurological conditions, including visual field loss following stroke, as in our case. However, since visual field recovery may involve both, improved function of injured tissue and recruitment of additional cortical structures to assume the function of the permanently damaged centers, we cannot ruled out that the plasticity in the visual system may intervene, underlying behavioral compensatory strategies.31, 32, 33 Moreover, this case report has several limitations hinder confirming the beneficial effect of CoQ10 supplement, including discontinuation of the treatment or anatomic and physiologic evidences to observe deterioration and improvement in the visual field.
4. Conclusions
We describe a case of a patient presenting right occipital lobe stroke with left inferior homonymous quadrantanopia and more than 10 years of follow-up. We did not observe any spontaneous recovery of the visual field nor the patient received any rehabilitating therapy. After the initiation of CoQ10 treatment, the patient demonstrated improved visual field after a remote ischemic stroke, four years before, with almost complete recovery at present. Considering that spontaneous recovery is extremely unlikely 5 years after the stroke and the improvement was temporally related to the initiation of the CoQ10 supplementation, we assume that the CoQ10 treatment had beneficial effects in our patient.
Patient consent
Consent to publish the case report was not obtained. All information contained within this report has been made anonymous in compliance with institutional policies.
Conflicts of interest
The following authors have no financial disclosures: BFV, HGI, JAV, JN, AFV.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgments and Disclosures
The Instituto Oftalmológico Fernández-Vega and Fundación de Investigación Oftalmológica acknowledge financial support from the Fundación Rafael del Pino (http://www.frdelpino.es) through the “Cátedra Rafael del Pino”. BFV and HGI thank Fabiola Fernández Andrés for its inestimable help.
Contributor Information
Beatriz Fernández-Vega, Email: beatriz@fernandez-vega.com.
Héctor González-Iglesias, Email: h.gonzalez@fio.as.
References
- 1.Gilhotra J.S., Mitchell P., Healey P.R., Cumming R.G., Currie J. Homonymous visual field defects and stroke in an older population. Stroke. 2002;33:2417–2420. doi: 10.1161/01.str.0000037647.10414.d2. [DOI] [PubMed] [Google Scholar]
- 2.Romano J.G. Progress in rehabilitation of hemianopic visual field defects. Cerebrovasc Dis. 2009;27(1):187–190. doi: 10.1159/000200458. [DOI] [PubMed] [Google Scholar]
- 3.Grunda T., Marsalek P., Sykorova P. Homonymous hemianopia and related visual defects: restoration of vision after a stroke. Acta Neurobiol Exp. 2013;73(2):237–249. doi: 10.55782/ane-2013-1933. [DOI] [PubMed] [Google Scholar]
- 4.Schuett S., Kentridge R.W., Zihl J., Heywood C.A. Are hemianopic reading and visual exploration impairments visually elicited? New insights from eye movements in simulated hemianopia. Neuropsychologia. 2009;47:733–746. doi: 10.1016/j.neuropsychologia.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Gray C.S., French J.M., Bates D., Cartlidge N.E., Venables G.S., James O.F. Recovery of visual fields in acute stroke: homonymous hemianopia associated with adverse prognosis. Age Ageing. 1989;18:419–421. doi: 10.1093/ageing/18.6.419. [DOI] [PubMed] [Google Scholar]
- 6.Zhang X., Kedar S., Lynn M.J., Newman N.J., Biousse V. Homonymous hemianopias: clinical-anatomic correlations in 904 cases. Neurology. 2006;66:906–910. doi: 10.1212/01.wnl.0000203913.12088.93. [DOI] [PubMed] [Google Scholar]
- 7.Frolov A., Feuerstein J., Subramanian P.S. Homonymous hemianopia and vision. Restoration therapy. Neurol Clin. 2017;35(1):29–43. doi: 10.1016/j.ncl.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin D. Homonymous hemianopia: challenges and solutions. Clin Ophthalmol. 2014;8:1919–1927. doi: 10.2147/OPTH.S59452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kerkhoff G. Restorative and compensatory therapy approaches in cerebral blindness—a review. Restor Neurol Neurosci. 1999;15:255–271. [PubMed] [Google Scholar]
- 10.Eggenberger E.R., Pula J.H. Aminoff's Neurology and General Medicine. fifth ed. Elsevier Inc; 2014. Neuro-ophthalmology in medicine; pp. 479–502. [Google Scholar]
- 11.Matsubara J.A., Boyd J.D. Overview of the central visual pathways. In: Levin L.A., Nilsson S.F.E., Ver Howeve J., editors. Adler's Physiology of the Eye. eleventh ed. Saunders Elservier; Philadelphia: 2001. [Google Scholar]
- 12.Lane A.R., Smith D.T., Schenk T. Clinical treatment options for patients with homonymous visual field defects. Clin Ophthalmol. 2008;2(1):93–102. doi: 10.2147/opth.s2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kasten E., Poggel D.A., Müller-Oehring E., Gothe J., Schulte T., Sabel B.A. Restoration of vision II: residual functions and training-induced visual fi eld enlargement in brain-damaged patients. Restor Neurol Neurosci. 1999;15:273–287. [PubMed] [Google Scholar]
- 14.Pambakian A.L., Kennard C. Can visual function be restored in patients with homonymous hemianopia? Br J Ophthalmol. 1997;81:324–328. doi: 10.1136/bjo.81.4.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang X., Kedar S., Lynn M.J., Newman N.J., Biousse V. Natural history of homonymous hemianopia. Neurology. 2006;66:901–905. doi: 10.1212/01.wnl.0000203338.54323.22. [DOI] [PubMed] [Google Scholar]
- 16.Zihl J., Kennard C. Disorders of higher visual function. In: Brandt T., Caplan L.R., Dichgans J., editors. Neurological Disorders: Course and Treatment. Academic Press; California: 1996. pp. 201–212. 1996. [Google Scholar]
- 17.Kedar S., Ghate D., Corbett J.J. Visual fields in neuro-ophthalmology. Indian J Ophthalmol. 2011;59(2):103–109. doi: 10.4103/0301-4738.77013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han L., Law-Gibson D., Reding M. Key neurological impairments influence function-related group outcomes after stroke. Stroke. 2002;33:1920–1924. doi: 10.1161/01.str.0000019792.59599.cc. [DOI] [PubMed] [Google Scholar]
- 19.Turner-Stokes L., Pick A., Nair A., Wade D.T. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst Rev. 2015;12:CD004170. doi: 10.1002/14651858.CD004170.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Obuchowska I., Mariak Z. Homonymous hemianopsia. Klin Oczna. 2012;114(3):226–229. [PubMed] [Google Scholar]
- 21.Guo X., Jin Z., Feng X., Tong S. Enhanced effective connectivity in mild occipital stroke patients with hemianopia. IEEE Trans Neural Syst Rehabil Eng. 2014;22(6):1210–1217. doi: 10.1109/TNSRE.2014.2325601. [DOI] [PubMed] [Google Scholar]
- 22.Salama M., Yuan T.F., Machado S. Co-enzyme Q10 to treat neurological disorders: basic mechanisms, clinical outcomes, and future research direction. CNS Neurol Disord - Drug Targets. 2013;12(5):641–664. doi: 10.2174/18715273113129990071. [DOI] [PubMed] [Google Scholar]
- 23.Littarru G.P., Tiano L. Bioenergetic and antioxidant properties of coenzyme Q10: recent developments. Mol Biotechnol. 2007;37:31–37. doi: 10.1007/s12033-007-0052-y. [DOI] [PubMed] [Google Scholar]
- 24.Somayajulu M., Mc Carthy S., Hung M., Sikorska M., Borowy-Borowski H., Pandey S. Role of mitochondria in neuronal cell death induced by oxidative stress; neuroprotection by coenzyme Q10. Neurobiol Dis. 2005;18:618–627. doi: 10.1016/j.nbd.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 25.Beal M.F. Therapeutic effects of coenzyme Q10 in neurodegenerative diseases. Methods Enzymol. 2004;382:473–487. doi: 10.1016/S0076-6879(04)82026-3. [DOI] [PubMed] [Google Scholar]
- 26.Nucci C., Tartaglione R., Cerulli A. Retinal damage caused by high intraocular pressure-induced transient ischemia is prevented by coenzyme Q10 in rat. Int Rev Neurobiol. 2007;82:397–406. doi: 10.1016/S0074-7742(07)82022-8. [DOI] [PubMed] [Google Scholar]
- 27.Russo R., Cavaliere F., Rombolà L. Rational basis for the development of coenzyme Q10 as a neurotherapeutic agent for retinal protection. Prog Brain Res. 2008;173:575–582. doi: 10.1016/S0079-6123(08)01139-4. [DOI] [PubMed] [Google Scholar]
- 28.Hernández-Camacho J.D., Bernier M., López-Lluch G., Navas P. Coenzyme Q10 supplementation in aging and disease. Front Physiol. 2018;9:44. doi: 10.3389/fphys.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu C.J., Guo Y.Z., Zhang Y. Coenzyme Q10 ameliorates cerebral ischemia reperfusion injury in hyperglycemic rats. Pathol Res Pract. 2017;213(9):1191–1199. doi: 10.1016/j.prp.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 30.Lee D., Kim K.Y., Shim M.S. Coenzyme Q10 ameliorates oxidative stress and prevents mitochondrial alteration in ischemic retinal injury. Apoptosis. 2014;19(4):603–614. doi: 10.1007/s10495-013-0956-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huxlin K.R. Perceptual plasticity in damaged adult visual systems. Vis Res. 2008;48:2154–2166. doi: 10.1016/j.visres.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 32.Das A., Huxlin K.R. New approaches to visual rehabilitation for cortical blindness: outcomes and putative mechanisms. Neuroscientist. 2010;16:374–387. doi: 10.1177/1073858409356112. [DOI] [PubMed] [Google Scholar]
- 33.Dilks D.D., Serences J.T., Rosenau B.J., Yantis S., McCloskey M. Human adult cortical reorganization and consequent visual distortion. J Neurosci. 2007;27:9585–9594. doi: 10.1523/JNEUROSCI.2650-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]