Abstract
Introduction
Errors are frequent in health care and Emergency Departments are one of the riskiest areas due to frequent changes of team composition, complexity and variety of the cases and difficulties encountered in managing multiple patients. As the majority of clinical errors are the results of human factors and not technical in nature or due to the lack of knowledge, a training focused on these factors appears to be necessary. Crisis resource management (CRM), a tool that was developed initially by the aviation industry and then adopted by different medical specialties as anesthesia and emergency medicine, has been associated with decreased error rates.
The aim of the study
To assess whether a single day CRM training, combining didactic and simulation sessions, improves the clinical performance of an interprofessional emergency medical team.
Material and Methods
Seventy health professionals with different qualifications, working in an emergency department, were enrolled in the study. Twenty individual interprofessional teams were created. Each team was assessed before and after the training, through two in situ simulated exercises. The exercises were videotaped and were evaluated by two assessors who were blinded as to whether it was the initial or the final exercise. Objective measurement of clinical team performance was performed using a checklist that was designed for each scenario and included essential assessment items for the diagnosis and treatment of a critical patient, with the focus on key actions and decisions. The intervention consisted of a one-day training, combining didactic and simulation sessions, followed by instructor facilitated debriefing. All participants went through this training after the initial assessment exercises.
Results
An improvement was seen in most of the measured clinical parameters.
Conclusion
Our study supports the use of combined CRM training for improving the clinical performance of an interprofessional emergency team. Empirically this may improve the patient outcome.
Keywords: interprofessional, clinical performance, training, crisis resource management, emergency department
Introduction
In the recent years, the need to enhance patient safety has become a priority as the majority of clinical errors (approximately 70%) are the results of human factors [1] and not technical in nature or due to the lack of knowledge (failure in team communication, situational awareness, resource utilization and leadership) [2]. Efforts are necessary to improve the quality of the medical care provided and the patient outcome, especially in high risk areas as emergency medicine, anesthesia, surgery and intensive care.
How can we achieve this if just improving the knowledge is not enough? Steps were taken by adopting and adapting the Crises Resource Management (CRM) training, a tool that is oriented towards human factors and was initially developed by the aviation industry. CRM training is considered to be responsible for the decrease in aircraft accidents over the last four decades [3].
The primary objectives of CRM training are to improve team dynamics, to identify and help change mental models that create barriers in adopting effective communication, effective task management, healthy leadership and fellowship behaviors and an increasing awareness [4].
Anesthesia was one of the first specialties to adopt the CRM training and an improvement of team performance and a reduced risk of errors during medical and surgical crisis in the operating room has been shown [5].
Early interest in this type of training was demonstrated also by the emergency medicine specialty.
Morey et al. (2002), in their evaluation of MedTeams Project’s results found that formal teamwork training was effective in improving team behaviors and in reducing errors in Emergency Departments (ED) [6]. Despite this, human factors training is not widely disseminated through professionals working in ED and most studies focused only on emergency medicine residents and interdisciplinary trauma teams.
According to Chiniara (2003), simulation training is most suitable for low frequency high-risk situations that are potentially harmful for the patient [7]. These types of situations are those where crises arise, and CRM training may play an important role. As crises events are rare in real practice, the simulation room is an ideal setting for teaching CRM principles [7] and simulation-based CRM training was shown to be effective and relevant for the emergency medicine residents’ practice [2].
Different scales were developed to assess the nontechnical skills/behavioral performance and many studies reported on the reaction of participants toward the training, the acquisition of knowledge and the changes in attitude in non-clinical settings. Only a limited number of studies focused on transfer of the learning to the working place and even less measured the effect on patient outcomes [8].
As morbidity and mortality are indicators difficult to track in prospective studies, surrogates such as time to disposition, delays in achieving tasks in a timeframe, number of errors [9] have been used as well as checklists, to assess the clinical performance.
This study is aimed at assessing whether a single day CRM oriented team training combining didactic and simulation sessions improves the clinical performance of interprofessional emergency medicine teams.
Methods
Study design
The study took place in the emergency department of the Tirgu-Mures Emergency Clinical County Hospital, Romania between March and July 2016. The hospital has an emergency medicine residency training program and is the site of an affiliated emergency and disaster medicine simulation center that focuses on multidisciplinary and inter-professional training. The emergency department’s annual census is around 77,000 patients, approximately 10% of them being “critically ill”.
Emergency department clinical staff without prior CRM training were invited to participate. Residents with less than three months clinical experience in the emergency department were excluded. Twenty board-certified emergency medicine (EM) physicians, ten emergency medicine residents, and forty nurses volunteered for the study.
The study protocol was approved by the Ethics Committee of the Tirgu-Mures Emergency Clinical County Hospital. Written informed consent was obtained from all study participants. Twenty mixed teams were constructed according to participants’ work schedules.
Each team utilized an attending EM physician, an EM resident and two nurses, a structure we consider ideal for the management of a single critically ill patient in our ED. Because the number of eligible attending physicians was greater than the number of residents, each resident participated in two teams.
Two sets of scenarios were designed, consisting of two scenarios each: a medical case and a trauma case.
The first set consisted of:
Medical patient A - A patient with an acute COPD exacerbation complicated by severe pneumonia, initially requiring noninvasive and subsequently invasive ventilation. Due to patient physiognomy as well as a history of prior tracheostomy, a difficult intubation needed to be anticipated.
Trauma patient A - A trauma patient with severe brain injury complicated by hemorrhagic shock secondary to intra-abdominal bleeding requiring activation of the massive transfusion protocol and emergent surgery.
The second set consisted of:
Medical patient B - A patient with COPD now presenting with a pulmonary embolism necessitating thrombolysis due to clinical instability.
Trauma patient B - A patient with a difficult airway, a severe, but surgically amenable intra-cranial injury, as well as long bones fractures, overall resulting in hypotension.
Both medical cases had signs of β2 mimetics overuse (tremor, tachycardia, hypokalemia).
Sets were chosen pseudo-randomly, as participating residents were intended to be exposed to all cases and not to repeat scenarios. Simulations were performed in the ED resuscitation room during work hours. Scenarios utilized a high-fidelity manikin as well as the usual medical equipment and documentation forms from the resuscitation room. The role of different specialties doctors who were called for advice/help was played by one of the instructors, as well as the role of paramedics. The role of the radiologist was played by the radiologist on duty that day. Both a fixed camera, placed on the ceiling of the resuscitation room, as well as a mobile camera recorded all of the exercises. No debriefings took place after the assessment scenarios were completed.
We then held single day (6 to 7 hours) training sessions over a period of ten days. Participants chose the day for their training session at their convenience. Training sessions took place in a recreation of the ED resuscitation room in the simulation center. Each training session started with a lecture focusing on medical errors and CRM principles. No medical teaching was provided. After the lecture, participants had the opportunity to familiarize themselves with the manikin and the simulation setting.
Each training session involved two multi-professional teams, each team consisting of one EM attending physician, one EM resident and two nurses. During the training sessions participants were permitted to change teams as long as the multi-professional composition remained the same. We utilized six critical patient scenarios (two trauma cases and four medical cases), different from those used in the initial assessment. One team completed a scenario while the other team observed the exercise remotely via a high-resolution real time video transmission system. Either as participants or observers, each team was exposed to all cases.
The simulation was run by two instructors (one doctor and one nurse) with CRM background training and one IT technician. Each scenario was followed by an instructor facilitated debriefing. Both technical and non-technical issues relating to team performance and team work were discussed. Identified clinical errors were addressed by either the participants or the instructors. Members of the team who had completed the scenario had priority in providing feedback, but both observers and participants were involved in debriefings.
Two months after receiving training, a final assessment was performed consisting of the same scenarios, teams and setting used in the initial assessment. As in the initial assessment, the scenarios were video-recorded, and no briefing was provided.
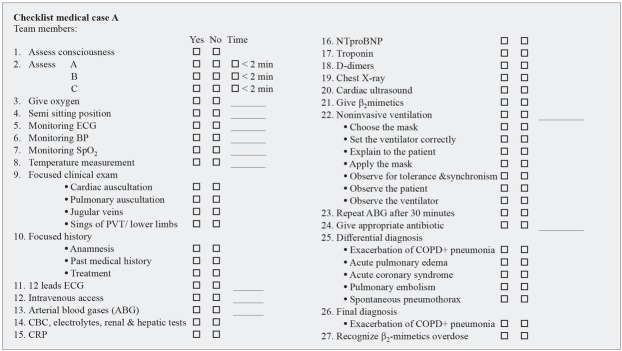
Objective measurement of clinical team performance was performed through a checklist that was designed for each scenario (Figure 1). The checklist included essential assessment items for the diagnosis and treatment of a critical patient, with the focus on key actions and decisions. The number of times a critical procedure was performed, as well as time to completion of the critical steps where appropriate, were recorded.
Fig. 1.
Example of a checklist used for the assessment of clinical performance
The video recordings were analyzed, and the checklists completed by an assessor blinded to whether the scenarios analyzed were the initial or final assessment.
Statistical analysis
The collected data were organized into several SPSS data files. The variables obtained were binary type and continuous type. For binary data analysis, the likelihood ratio was used to assess the difference in proportions. Continuous variables were tested for normality using Kolmogorov-Smirnov test. Our data followed a non-gaussian distribution, therefore a non-parametric test was used to compare the central tendency for the data series. Wilcoxon signed rank test was used, since we analyzed paired data. The significance level used in all tests was 0.05.
Results
Seventy participants were enrolled in the study and 69 completed the study. One nurse participant resigned her position and she was not available for the final assessment scenario. She was replaced by another nurse who had attended the training. The initial nurse was excluded from the final analysis and the nurse who replaced her was analyzed only once with the team to whom she was allocated at the beginning of the study.
The male: female ratio was 13:17 for doctors and 11:29 for nurses. Professional experience was variable (average 70 months, minimum 8 and maximum 300 months).
A checklist was completed for each scenario and each team. A total of 40 checklists were collected, 20 for the initial assessment and 20 the for the final one.
For the medical case A, the patient with acute COPD exacerbation complicated by severe pneumonia, critical elements where considered: oxygen administration, sitting position, establishing an intravenous access, appropriate investigations- especially ECG and arterial blood gases, recognition of the need for non-invasive ventilation, recognition of β2 sympatico-mimetics overdose, appropriate antibiotic administration. Results are reported in table 1 and table 2. A trend towards improvement was seen for these elements. Concerning the time until the procedure was performed, a statistically significant value was reached only for intravenous access. In terms of number of procedures performed, β2 sympatico-mimetics overdose recognition and assessment of efficiency of NIV through repeated ABG 30 minutes after initiation of it, reached significance level.
Table 1.
Checklist results for medical case A
| Element | Number of teams “Yes”/initial | Number of teams “Yes”/final | Number of teams “No”/initial | Number of teams “No”/final | Likelihood Ratio* | |
|---|---|---|---|---|---|---|
| Consciousness |
10 |
10 |
0 |
0 |
||
| ABC evaluation < 2 minutes |
10 |
10 |
0 |
0 |
||
| Oxygen administration ** |
10 |
10 |
0 |
0 |
||
| Siting position ** |
10 |
10 |
0 |
0 |
||
| Monitoring | Electrocardiogram |
10 |
10 |
0 |
0 |
|
| Blood pressure |
10 |
10 |
0 |
0 |
||
| Oxygen saturation |
10 |
10 |
0 |
0 |
||
| Temperature |
8 |
9 |
2 |
1 |
0.528 |
|
| Focused clinical | Cardiac auscultation |
1 |
2 |
9 |
1 |
0.528 |
| examination | Pulmonary auscultation |
10 |
10 |
0 |
0 |
|
| Jugular veins |
0 |
1 |
10 |
9 |
||
| Signs of PVT/edema |
5 |
10 |
5 |
0 |
||
| Focused history | Anamnesis |
10 |
10 |
0 |
0 |
|
| Past medical history |
10 |
10 |
0 |
0 |
||
| Treatment |
8 |
10 |
2 |
0 |
||
| 12-lead electrocardiogram ** |
6 |
10 |
4 |
0 |
||
| Intravenous line ** |
10 |
10 |
0 |
0 |
||
| Arterial blood gases (ABG) ** |
10 |
10 |
0 |
0 |
||
| Lab tests | CBC, electrolytes, Renal &hepatic tests |
9 |
10 |
1 |
0 |
|
| C-reactive protein |
1 |
0 |
9 |
10 |
||
| NTproBNP |
8 |
2 |
8 |
2 |
1.000 |
|
| Troponin |
2 |
4 |
8 |
6 |
0.326 |
|
| D-dimers |
6 |
8 |
4 |
2 |
0.326 |
|
| Chest radiography |
10 |
10 |
0 |
0 |
||
| Cardiac ultrasound |
1 |
1 |
9 |
9 |
1.000 |
|
| Give β2mimetics |
9 |
3 |
1 |
7 |
0.004 |
|
| Noninvasive ventilation ** |
10 |
10 |
0 |
0 |
||
| Choose the mask |
8 |
7 |
2 |
3 |
0.605 |
|
| Set the ventilator correctly |
8 |
9 |
2 |
1 |
0.528 |
|
| Explain to the patient |
8 |
10 |
2 |
0 |
0.112 |
|
| Apply the mask |
10 |
10 |
0 |
0 |
||
| Observe for tolerance & synchronism |
6 |
9 |
4 |
1 |
0.112 |
|
| Observe the patient |
9 |
9 |
1 |
1 |
1.000 |
|
| Observe the ventilator |
7 |
9 |
3 |
1 |
0.255 |
|
| Repeat ABG after 30 minutes |
4 |
9 |
6 |
1 |
0.015 |
|
| Give appropriate antibiotic |
8 |
10 |
2 |
0 |
||
| Differential | Exacerbation of COPD+ pneumonia |
10 |
10 |
0 |
0 |
|
| diagnosis | Acute pulmonary edema |
4 |
10 |
6 |
0 |
|
| Acute coronary syndrome |
0 |
3 |
10 |
7 |
||
| Pulmonary embolism |
7 |
10 |
3 |
0 |
||
| Spontaneous pneumothorax |
2 |
6 |
8 |
4 |
0.063 |
|
| Correct diagnosis |
10 |
10 |
0 |
0 |
||
| Recognize β2mimetics overdose |
1 |
7 |
9 |
3 |
0.004 |
|
Chi-Square Tests; ** Time to achievement recorded; ABC- airway, breathing, circulation, PVT-profound venous thrombosis, CBC- complete blood count, NTproBNP- N-terminal pro b-type natriuretic peptide, COPD-chronic obstructive pulmonary disease
Table 2.
Results for medical case A – Time to achievement of critical steps
| Initial | Final | ||||
|---|---|---|---|---|---|
| Time to…. (seconds) | Median | IQR | Median | IQR | P value* |
| Oxygen administration |
65 |
80 |
39.5 |
63 |
0.203 |
| Sitting position |
17 |
113 |
6 |
18 |
0.074 |
| 12 leads electrocardiogram |
56 |
121 |
136.5 |
111 |
0.463 |
| Intravenous line |
123.5 |
114 |
58.5 |
54 |
0.013 |
| Arterial blood gases |
142.5 |
99 |
70.5 |
99 |
0.169 |
| Noninvasive ventilation |
308 |
304 |
215.5 |
124 |
0.386 |
Wilcoxon Signed Ranks Test
For medical case B, the patient with COPD now presenting with a pulmonary embolism, critical elements where: oxygen administration, semi-sitting position, establishing an intravenous access, appropriate investigations- especially ECG, arterial blood gases, angioCT scan/ cardiac ultrasound, recognition of the need for and initiation of thrombolysis, request for cardiologic advice and recognition of β2 sympatico-mimetics overdose. Results are reported in table 3 and table 4. As for the medical case A, an improvement was seen for most of the elements. Significance level was reached in terms of number of procedures performed for cardiac ultrasound requested and β2 sympatico-mimetics overdose recognition. Concerning the time until the procedure was performed, significance level was reached for oxygen administration and sitting position. For time until a cardiac ultrasound was requested, the p value couldn’t be calculated as the test was requested during the initial assessment scenario only by two teams.
Table 3.
Checklist results for medical case B
| Element | Number of teams “Yes”/initial | Number of teams “Yes”/final | Number of teams “No”/initial | Number of teams “No”/final | Likelihood Ratio* |
|---|---|---|---|---|---|
| Consciousness |
10 |
10 |
0 |
0 |
|
| ABC evaluation < 2 minutes |
10 |
10 |
0 |
0 |
|
| Oxygen administration ** |
10 |
10 |
0 |
0 |
|
| Sitting position ** |
9 |
10 |
1 |
0 |
|
| Monitoring Electrocardiogram |
10 |
10 |
0 |
0 |
|
| Blood pressure |
10 |
10 |
0 |
0 |
|
| Oxygen saturation |
10 |
10 |
0 |
0 |
|
| Temperature |
6 |
1 |
4 |
9 |
0.015 |
| Focused clinical Cardiac auscultation |
4 |
8 |
6 |
2 |
0.063 |
| examination Pulmonary auscultation |
9 |
8 |
1 |
2 |
0.528 |
| Jugular veins |
1 |
3 |
9 |
7 |
0.255 |
| Signs of PVT/edema |
9 |
10 |
1 |
0 |
|
| Focused history Anamnesis |
10 |
10 |
0 |
0 |
|
| Past medical history |
10 |
10 |
0 |
0 |
|
| Treatment |
10 |
10 |
0 |
0 |
|
| 12-lead electrocardiogram** |
10 |
10 |
0 |
0 |
|
| Intravenous line ** |
10 |
10 |
0 |
0 |
|
| Arterial blood gases (ABG) |
10 |
10 |
0 |
0 |
|
| Lab tests CBC, electrolytes, Renal &hepatic tests |
10 |
10 |
0 |
0 |
|
| CRP |
0 |
0 |
10 |
10 |
|
| NT-proBNP |
8 |
9 |
2 |
1 |
0.528 |
| Troponin |
9 |
8 |
1 |
2 |
0.528 |
| D-dimers |
9 |
10 |
1 |
0 |
|
| Chest radiography |
6 |
4 |
4 |
6 |
0.369 |
| Fluids bolus |
2 |
9 |
8 |
1 |
0.001 |
| Give β2mimetics |
8 |
2 |
2 |
8 |
0.005 |
| Request angioCT scan ** |
10 |
8 |
0 |
2 |
|
| Angio-CT scan performed |
6 |
2 |
4 |
6 |
0.132 |
| Request cardiac ultrasound ** |
2 |
7 |
8 |
3 |
0.021 |
| Request venous Doppler ultrasound |
2 |
0 |
8 |
10 |
|
| Decide to thrombolysis ** |
9 |
10 |
1 |
0 |
|
| Verify contraindications to thrombolysis |
2 |
7 |
8 |
3 |
0.021 |
| Start thrombolysis ** |
9 |
10 |
1 |
0 |
|
| Ask for cardiologic advise ** |
10 |
10 |
0 |
0 |
|
| Differential Exacerbation of COPD+ pneumonia |
6 |
9 |
4 |
1 |
0.112 |
| diagnosis Acute pulmonary edema |
4 |
5 |
6 |
5 |
0.653 |
| Acute coronary syndrome |
5 |
10 |
5 |
0 |
|
| Pulmonary embolism |
10 |
10 |
0 |
0 |
|
| Spontaneous pneumothorax |
5 |
8 |
5 |
2 |
0.155 |
| Correct diagnosis |
10 |
10 |
0 |
0 |
|
| Recognize β2mimetics overdose |
2 |
8 |
8 |
2 |
0.005 |
Chi-Square Test; ** Time to achievement recorded; ABC- airway, breathing, circulation, PVT-profound venous thrombosis, CBC- complete blood count, NT-proBNP- N-terminal pro b-type natriuretic peptide, COPD-chronic obstructive pulmonary disease
Table 4.
Results for medical case B – Time to achievement of critical steps
| Time to…. (seconds) | Initial | Final | P value* | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Oxygen administration |
76 |
81 |
51.5 |
29 |
0.022 |
| Siting position |
20 |
245 |
6.5 |
15 |
0.012 |
| 12 leads electrocardiogram |
160 |
125 |
120 |
30 |
0.221 |
| intravenous line |
115 |
116 |
105 |
48 |
0.859 |
| Arterial blood gases |
159 |
73 |
128 |
144 |
0.767 |
| AngioCT scan |
345 |
369 |
501 |
NA |
NA |
| Cardiac ultrasound |
790 |
NA |
520 |
450 |
NA |
| Thrombolysis decision |
515 |
233 |
510 |
394 |
0.515 |
| Start thrombolysis |
570 |
673 |
606.5 |
410 |
0.678 |
| Request cardiologic advice |
336 |
280 |
300 |
580 |
0.333 |
Wilcoxon Signed Ranks Test; NA- not available
Critical elements for the trauma case A, the patient with severe brain injury complicated by hemorrhagic shock secondary to intra-abdominal bleeding, were considered: 2 intravenous access, FAST ultrasound examination, administration of fluid bolus and O negative PRBCs, recognition of a shock patient requiring urgent surgery (request for surgeon advise early, transfer to the
operating theatre), recognition of the need to intubate and anticipation of a difficult airway, recognition and initiation of treatment for increased ICP. Results are reported in table 5 and table 6. There was a trend towards improvement in all the elements, though not statistically significant, except for recognition and initiation of treatment of high ICP, and the time until airway was secured.
Table 5.
Checklist results for trauma case A
| Element | Number of teams “Yes”/initial | Number of teams “Yes”/final | Number of teams “No”/initial | Number of teams “No”/final | Likelihood Ratio* |
|---|---|---|---|---|---|
| Consciousness |
10 |
10 |
0 |
0 |
|
| A-airway |
6 |
10 |
4 |
0 |
|
| B-breathing |
9 |
10 |
1 |
0 |
|
| Primary survey C-circulation |
9 |
10 |
1 |
0 |
|
| (ABC < 2 minutes) D GCS |
9 |
10 |
1 |
0 |
|
| (DE < 5 minutes) Motor response |
7 |
10 |
3 |
0 |
|
| Pupillary exam |
9 |
10 |
1 |
0 |
|
| E-exposure |
10 |
10 |
0 |
0 |
|
| Oxygen administration |
10 |
10 |
0 |
0 |
|
| Electrocardiogram |
10 |
10 |
0 |
0 |
|
| Blood pressure |
10 10 |
10 10 |
0 0 |
0 0 |
|
| Monitoring Oxygen saturation |
10 |
10 |
0 |
0 |
|
| Temperature |
1 |
5 |
9 |
5 |
0.044 |
| Anamnesis |
10 |
10 |
0 |
0 |
|
| Past medical history |
1 |
0 |
9 |
10 |
|
| Allergies |
0 |
0 |
10 |
10 |
|
| Focused history Treatment |
0 |
1 |
10 |
9 |
|
| Mechanism of injury |
7 |
10 |
3 |
0 |
|
| Time from injury |
0 |
7 |
10 |
3 |
|
| Last meal |
0 |
1 |
10 |
9 |
|
| Insert an intravenous line ** |
10 |
10 |
0 |
0 |
|
| ABO+ Rhesus |
10 |
10 |
0 |
0 |
|
| Glucose level |
2 |
1 |
8 |
9 |
0.528 |
| CBC, electrolytes, renal &hepatic, coagulation tests, creatine kinase, arterial blood gases |
10 |
10 |
0 |
0 |
|
| Fluids bolus ** |
7 |
10 |
3 |
0 |
|
| FAST ultrasound exam ** |
10 |
10 |
0 |
0 |
|
| 12-lead electrocardiogram ** |
3 |
4 |
7 |
6 |
0.639 |
| Insert a second intravenous line ** |
10 |
10 |
0 |
0 |
|
| Recognize signs of shock |
10 |
10 |
0 |
0 |
|
| Transfusion of O negative PRBCs |
6 |
9 |
4 |
1 |
0.121 |
| Recognize signs of increased ICP |
6 |
10 |
4 |
0 |
|
| Recognize the need for intubation ** |
10 |
10 |
0 |
0 |
|
| Anticipate a difficult airway |
3 |
7 |
7 |
3 |
0.070 |
| Airway secured ** |
10 |
10 |
0 |
0 |
|
| Request the surgeon advise ** |
10 |
10 |
0 |
0 |
|
| Request for a CT scan |
3 |
3 |
7 |
7 |
1.000 |
| Request the neurosurgeon advise |
5 |
8 |
5 |
2 |
0.155 |
| Treat high ICP |
2 |
7 |
8 |
3 |
0.021 |
| Immobilize the fracture |
5 |
10 |
5 |
0 |
|
| Perform the logroll |
1 |
3 |
9 |
7 |
0.255 |
| Perform a complete secondary survey |
1 |
0 |
9 |
10 |
|
| Transfer the patient to the operating room ** |
9 |
10 |
1 |
0 |
|
| IOT checklist completed verified |
0 |
2 |
10 |
8 |
Chi-Square Tests; ** Time to achievement recorded; D-disability, CBC-complete blood count, a FAST-focused assessment with Sonography in Trauma, PRBCs-packed red blood cells, ICP-intracranial pressure
Table 6.
Results for trauma case A – Time to achievement of critical steps
| Time to…. (seconds) | Initial | Final | P value* | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| First intravenous line |
65 |
49 |
43.5 |
45 |
0.139 |
| Fluids bolus |
208 |
258 |
116.5 |
114 |
0.128 |
| FAST ultrasound exam |
174 |
177 |
160.5 |
160 |
0.721 |
| 12 leads electrocardiogram |
658 |
NA |
114 |
52 |
0.109 |
| Second intravenous line |
174 |
352 |
158.5 |
190 |
0.646 |
| Recognize the need for IOT |
149 |
116 |
109 |
199 |
0.203 |
| Airway secured |
401 |
210 |
317 |
78 |
0.017 |
| Request the surgeon advise |
339.5 |
215 |
247.5 |
247 |
0.241 |
| Transfer into the operating room |
580 |
295 |
605 |
70 |
0.374 |
Wilcoxon Signed Ranks Test; NA- not available; FAST-focused assessment with ultrasound in trauma, IOT-orotracheal intubation
The trauma case B, the patient with a difficult airway, severe TBI and long bones fractures resulting in hypotension, had the following elements: intravenous access, administration of fluid bolus, FAST ultrasound examination, recognition of severe brain injury requiring urgent measures to decrease the ICP, performance of the CT scan and early involvement of the neurosurgeon, recognition of the need to intubate, anticipation of a difficult airway and management of a “cannot ventilate, cannot intubate “ situation (number of direct laryngoscopies, call for help, decide and perform a cricothyroidotomy).
Results are given in table 7 and table 8. An improvement was seen in most of the elements. Significant improvement was shown in the elements corelated with severe TBI and difficult airway management, in terms of number of procedures performed (recognition and treatment of increased ICP, anticipation of difficult airway) and time until procedure was completed (request for neurosurgeon advice, first attempt to intubate, decision for cricothyroidotomy, airway secured).
Table 7.
Checklist results for trauma case B
| Element | Number of teams “Yes”/initial | Number of teams “Yes”/final | Number of teams “No”/initial | Number of teams “No”/final | Likelihood Ratio* |
|---|---|---|---|---|---|
| Consciousness |
10 |
10 |
0 |
0 |
|
| A-airway |
9 |
10 |
1 |
0 |
|
| B-breathing |
9 |
10 |
1 |
0 |
|
| Primary survey C-circulation |
9 |
10 |
1 |
0 |
|
| (ABC < 2 minutes) D GCS |
8 |
10 |
2 |
0 |
|
| (DE < 5 minutes) Motor response |
7 |
10 |
3 |
0 |
|
| Pupillary exam |
8 |
10 |
2 |
0 |
|
| E-exposure |
10 |
10 |
0 |
0 |
|
| Oxygen administration |
8 |
10 |
2 |
0 |
|
| Electrocardiogram |
10 |
10 |
0 |
0 |
|
| Blood pressure |
10 |
10 |
0 |
0 |
|
| Monitoring Oxygen saturation |
10 |
10 |
0 |
0 |
|
| Temperature |
0 |
5 |
10 |
5 |
|
| Anamnesis |
10 |
10 |
0 |
0 |
|
| Past medical history |
1 |
5 |
9 |
5 |
0.044 |
| Allergies |
0 |
7 |
10 |
3 |
|
| Focused history Treatment |
0 |
1 |
10 |
9 |
|
| Mechanism of injury |
7 |
10 |
3 |
0 |
|
| Time from injury |
5 |
10 |
5 |
0 |
|
| Last meal |
0 |
0 |
10 |
10 |
|
| Insert an intravenous line ** |
10 |
10 |
0 |
0 |
|
| ABO+ Rhesus |
10 |
10 |
0 |
0 |
|
| Glucose level |
2 |
3 |
8 |
7 |
0.605 |
| CBC, electrolytes, renal &hepatic& coagulation tests, creatine kinase, arterial blood gases |
10 |
10 |
0 |
0 |
|
| Fluids bolus ** |
3 |
3 |
7 |
7 |
1.000 |
| FAST ultrasound exam ** |
5 |
7 |
5 |
3 |
0.359 |
| 12-lead electrocardiogram |
1 |
4 |
9 |
6 |
0.112 |
| Insert a second intravenous line ** |
8 |
8 |
2 |
2 |
1.000 |
| Request for CT scan |
9 |
10 |
1 |
0 |
|
| Request the neurosurgeon ** |
9 |
10 |
1 |
0 |
|
| Recognize signs of increased ICP |
3 |
9 |
7 |
1 |
0.004 |
| Recognize the need for intubation ** |
10 |
10 |
0 |
0 |
|
| Anticipate a difficult airway |
5 |
9 |
5 |
1 |
0.044 |
| Number of direct laryngoscopy atempts (more than two) |
6 |
0 |
4 |
10 |
|
| Ventilation achieved between intubation attempts |
10 |
10 |
0 |
0 |
|
| Ask for help ** |
5 |
5 |
5 |
5 |
1.000 |
| Use of alternative techniques for intubation |
5 |
0 |
5 |
10 |
|
| Decide for cricothyroidotomy ** |
10 |
10 |
0 |
0 |
|
| Airway secured ** |
10 |
10 |
0 |
0 |
|
| Treat high ICP |
4 |
9 |
6 |
1 |
0.015 |
| Immobilize the fracture |
8 |
9 |
2 |
1 |
0.528 |
| Give antibiotic |
4 |
10 |
6 |
0 |
|
| Perform the logroll |
4 |
8 |
6 |
2 |
0.063 |
| Perform a complete secondary survey |
3 |
1 |
7 |
9 |
0.255 |
| IOT checklist completed verified |
0 |
2 |
10 |
8 |
Chi-Square Test; ** Time to achievement recorded; D-disability, CBC-complete blood count, a FAST-focused assessment with Sonography in Trauma, ICP-intracranial pressure, IOT-orotracheal intubation
Table 8.
Results for trauma case B – Time to achievement of critical steps
| Time to…. (seconds) | Initial | Final | P value* | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| First intravenous line |
66 |
85 |
69.5 |
80 |
0.674 |
| Fluids bolus |
245 |
703 |
114 |
188 |
0.317 |
| FAST ultrasound exam |
170 |
875 |
240 |
510 |
0.715 |
| Second intravenous line |
150 |
207 |
195 |
552 |
0.917 |
| Request for neurosurgeon |
1200 |
338 |
580 |
465 |
0.008 |
| Recognize the need for IOT |
240 |
175 |
145 |
80 |
0.017 |
| First IOT atempt |
512 |
179 |
355 |
147 |
0.007 |
| Call for help |
682 |
356 |
520 |
186 |
0.655 |
| Decide for cricothyroidotomy |
790 |
195 |
446,5 |
262 |
0.005 |
| Airway secured |
1030 |
304 |
602 |
250 |
0.005 |
Wilcoxon Signed Ranks Test; FAST-focused assessment with ultrasound in trauma, IOT-orotracheal intubation
Discussion
CRM trainings are addressing a set of nontechnical skills, “the cognitive, social and personal resource skills that complement technical skills, and contribute to safe and efficient task performance” [10]. These nontechnical skills can be divided into four domains essential for an effective team: teamwork, task management, decision making and situational awareness, all of them being linked by communication [11]
The CRM key principles that act as a framework for teaching teamwork skills to emergency residents, according to GABA [5] and modified by Carne [12] are:
Know your environment
Anticipate, share and review the plan
Ensure leadership and role clarity
Communicate effectively
Call for help early
Allocate attention wisely- avoid fixation
Distribute the workload-monitor and support team members.
In our study we assessed whether a single-day training on CRM principles combining didactic and high-fidelity simulated session may improve the clinical performance (objectively measured through a checklist) of an interprofessional emergency team. We found that most of the measured clinical parameters improved. We hypothesize this is due to an improvement of non-technical skills, as we didn’t teach the clinical skills in the simulation cases explicitly. Also, in each team we had an experienced attending physician, the mean experience for the EM attendings being 149 months (minimum 72 and maximum 300 months), so lack of knowledge was unlikely.
Many of the clinical decisions as well as the evaluation of the patient include the correct usage of CRM principles.
The cases were chosen in such a way that they were typical for an average acute ED patient, but still strongly dependent on correct application of CRM principles. E.g., when dealing with a difficult airway, in our case a “cannot ventilate cannot intubate” situation, the team should anticipate, share the same mental model, distribute the workload and plan ahead while staying alert for sudden changes of situation. All the required skills correspond to CRM principles and indeed improved significantly after the training as shown by the number of teams who anticipated the difficult airway (p=0.044), number of attempts to intubate by direct laryngoscopy, the time until decision to perform a cricothyroidotomy was taken and the airway was secured.
Managing a polytrauma patient with hemorrhagic shock, requiring damage control surgery and massive transfusion protocol activation, requires to: anticipate, share the plan, ensure leadership and role clarity, communicate effectively, distribute the workload, call for help early and maintain standards. An improvement was seen in the present study, reflected by number of teams that administrate fluids bolus and O negative PRBCs from the ED storage, monitored the temperature as hypothermia is one of the components of the lethal triad in bleeding patients [13], time until they insert the intravenous lines, gave the fluids bolus, performed the FAST exam, call for surgeon.
Also, the recognition of a condition such as β2 sympatico-mimetics overdose, in a patient presenting with respiratory distress, where signs as tachycardia and agitation might have different causes, request situational awareness and wise allocation of attention. In both medical cases, a significant improvement was seen after the training (p=0.004 for case A and p=0.005 for case B).
Avoiding fixation error was important in order to avoid a wrong diagnosis in medical cases as
they had a similar history and almost the same clinical presentation, except for the blood pressure that was
lower but still in normal range initially, for the patient with PE. Their final diagnosis was correct before and after the training, but more differential diagnoses were considered during the final assessment.
The idea of team skills training being associated with better clinical performance and empirically with better patient outcome was already raised by Wright et al [14]. In their study on medical students, run in two settings: a classroom-based and a high-fidelity simulated environment, they found a strong correlation between team skills rating and objective performance measures within the high fidelity simulated environment, but no correlation on the classroom- based environment.
Very few studies measured the impact of CRM training on patient outcome [8]. One of these found a significant decrease in mortality for in hospital pediatric cardiac arrest after simulation CRM training. [15].
A positive association between better teamwork, better nontechnical skills and disposition time and risk for delays to patient care was demonstrated by Pucher et al, on a study carried on fifty real trauma cases [9].
Similar to our study, the efficiency of a relatively brief (4 hours) teamwork training, including a one-hour web didactic session followed by a human patient simulator-based session, on clinical performance of an interdisciplinary trauma team was shown by Steinmann et al [16]. This improvement was seen on simulated cases as well as on real trauma cases.
The effectiveness of teamwork training on clinical performance of an interprofessional team (surgeons, nurses), reflected by the decrease in time from arrival to CT scanner, endotracheal intubation and operating room, was demonstrated also by Capella et al [17]. As in the previously mentioned study, these results were obtained from real cases.
The present study has several limitations. The study was run in a single center and this limited the number of participants. Due to the very small number of EM residents available during the study period, they were exposed twice to the initial and final assessment in two different teams. Although we used two sets of scenarios and we did not perform a debriefing afterwards, we cannot exclude that their experience with the first team influenced their performance with the second one. It is difficult to appreciate if this had an impact the team clinical performance.
Participants were evaluated two months after the training. We did not assess them immediately after the training, so we do not know if their performance improved or declined over this time period.
Ideally, after a CRM training the actual patient outcome would be measured. This was our initial intention when we implemented this study. Unfortunately, we encountered a technical problem when we tried to analyze real cases. The quality of the image returned by the fixed camera was good, but the quality of the sound was too poor to permit a proper evaluation.
Conclusion
Our study supports the use of combined CRM training for improving clinical performance of an interprofessional emergency team. Empirically this may improve the patient outcome, but further research is necessary to establish the ideal length of the training, the real impact on patient outcome, the length of the decay phase and the optimal method and time for refresher training.
Acknowledgements
The authors thank all the participants in the study. Special thanks to Oana Mates, Andreea Soceanu and Bogdan Posteuca for their help in collecting the data.
Footnotes
Conflict of Interest None to declare
References
- 1.Rovamo L, Nurmi E, Mattila MM. Effect of a simulation-based workshop on the multidisciplinary teamwork of newborn emergencies: an interventional study. BMC Res Notes. 2015;8:671. doi: 10.1186/s13104-015-1654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hicks MC, Kiss A, Bandiera WG. Crisis Resources for Emergency Workers (CREW II): results of a pilot study and simulation-based crisis resource management course for emergency medicine residents. CJEM. 2012;14(6):354–62. doi: 10.2310/8000.2012.120580. [DOI] [PubMed] [Google Scholar]
- 3.Petrosoniak A, Hicks CM. Beyond crisis resource management: new frontiers in human factors training for acute care medicine. Curr Opin Anesthesiol. 2013;26:699–706. doi: 10.1097/ACO.0000000000000007. [DOI] [PubMed] [Google Scholar]
- 4.Rall M, Gaba D- Human Performance, Patient Safety, Miller RD. Miller’s Anesthesia. Philadelphia: Elsevier Churchill Livingstone; 2005. pp. 3021–72. [Google Scholar]
- 5.Gaba D, Howard S, Fish K. Simulation-based training in anesthesia crisis resource management (ACRM): a decade of experience. Simul Gaming. 2001;32:175–93. [Google Scholar]
- 6.Morey JC, Simon R, Jay GD. Error Reduction and Performance Improvement in the Emergency Department through Formal Teamwork Training: Evaluation Results of the MedTeams Project. Health Serv Res. 2002;37(6):1553–81. doi: 10.1111/1475-6773.01104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chiniara G, Cole G, Brisbin K. Simulation in healthcare: a taxonomy and a conceptual framework for instructional design and media selection. Med Teach. 2013;35(8):e1380–95. doi: 10.3109/0142159X.2012.733451. [DOI] [PubMed] [Google Scholar]
- 8.Boet S, Bould MD, Fung L. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anesth. 2014;61:571–82. doi: 10.1007/s12630-014-0143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pucher PH, Aggarwal R, Batrick N. Nontechnical skills performance and care processes in the management of the acute trauma patient. Surgery. 2014;155(5):902–9. doi: 10.1016/j.surg.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Flin R, O’Connor R, Crichton M. Safety at the Sharp End: A Guide to Nontechnical Skills. Farnham, UK: Ashgate; 2008. [Google Scholar]
- 11.Bleetman A, Sanusi S, Dale T, Brace S. Human factors and error prevention in emergency medicine. Emerg Med J. 2012;29:389–93. doi: 10.1136/emj.2010.107698. [DOI] [PubMed] [Google Scholar]
- 12.Carne B, Kennedy M, Gray T. Crisis resource management in emergency medicine. Emerg Med Australas. 2012;24:7–13. doi: 10.1111/j.1742-6723.2011.01495.x. [DOI] [PubMed] [Google Scholar]
- 13.Simmons JW, Powell MF. Acute traumatic coagulopathy: pathophysiology and resuscitation. Br J Anaesth. 2016;117(3):iii31–iii43. doi: 10.1093/bja/aew328. [DOI] [PubMed] [Google Scholar]
- 14.Wright MC, Phillips-Bute BG, Petrusa ER, Grifin KL, Hobbs GW, Taekman JM. Assessing teamwork in medical education and practice: relating behavioural teamwork ratings and clinical performance. Med Teach. 2009;31:30–8. doi: 10.1080/01421590802070853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andreatta P, Saxton E, Thompson M, Annich G. Simulation-based mock codes significantly correlate with improved pediatric cardiopulmonary arrest survival rates. Pediatr Crit Care Med.. 2011;12:33–8. doi: 10.1097/PCC.0b013e3181e89270. [DOI] [PubMed] [Google Scholar]
- 16.Steinemann S, Berg B, Skinner A. In situ-multidisciplinary, simulated-based teamwork training improves early trauma care. J Surg Educ. 2011;68:472–7. doi: 10.1016/j.jsurg.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Capella J, Smith S, Philp A. Teamwork training improves the clinical care of trauma patients. J Surg Educ. 2010;67:43943. doi: 10.1016/j.jsurg.2010.06.006. [DOI] [PubMed] [Google Scholar]