Abstract
Objectives.
Using subsequent all-cause mortality as a yardstick for retrospective health, this study assessed the comparability of self-rated health (SRH) between non-Hispanic whites and Hispanics.
Methods.
Based on longitudinal data from 6,870 white and 886 Hispanic respondents aged between 51 and 61 in the 1992 Health and Retirement Study, we related SRH in 1992 to risk of mortality in the 1992–2008 period. Logit models were used to predict white–Hispanic differences in reporting fair or poor SRH. Survival curves and cox proportional hazard models were estimated to assess whether and the extent to which the SRH–mortality association differs between non-Hispanic whites and Hispanics.
Results.
Hispanic respondents reported worse SRH than whites at the baseline, yet they had similar risk of mortality as whites in the 1992–2008 period. Overall, Hispanics rated their health more pessimistically than whites. This was especially the case for Hispanics who rated their health fair or poor at the baseline, whereas their presumed health conditions, as reflected by subsequent risk of mortality, should be considerably better than their white counterparts.
Discussion.
Health disparities between whites and Hispanics aged between 51 and 61 will be overestimated if the assessment has been solely based on differences in SRH between the two groups. Findings from this study call for caution in relying on SRH to quantify and explain health disparities between non-Hispanic whites and Hispanics in the United States.
Keywords: Hispanics, Mortality, Self-Rated Health, Whites.
Self-rated health (SRH) has been widely used as a measure of health status in health surveys and studies. The global measure of SRH typically consists of a single item, asking respondents to rate their current health by selecting one out of five standard categories including excellent, very good, good, fair, and poor. Relative to biomedical measures of health, SRH tends to be more comprehensive in that individuals evaluate their own health not only in terms of diseases and physical functioning but also in terms of psychosocial well-being (Idler & Benyamini, 1997; Kaplan, & Camacho, 1983; Liang et al., 2010). Analytical results from different studies have consistently shown that SRH is a valid health measure as indicated by its robust association with subsequent mortality (Benyamini & Idler, 1999; DeSalvo, Fan, McDonell, & Fihn, 2005; Franks, Gold, & Fiscella, 2003; Idler & Angel, 1990; Kaplan, Barell, & Lusky, 1988; Mossey & Shapiro, 1982) and disability (Idler & Kasl, 1995; Kaplan & Keil, 1993).
The established validity of SRH as a global measure of overall health, however, does not necessarily mean that the conception of SRH categories is comparable across different social groups. In essence, this issue of comparability concerns whether, and the extent to which, the differences in SRH across social groups are true reflections of corresponding differences in health status or they are more of a result of differential perceptions or response bias of health status by social groups. These two scenarios correspond, respectively, with what has been termed as “spontaneous assessment” and “enduring self-concept” in SRH (Balis et al., 2003). If individuals of different gender, socioeconomic status (SES), or racial and ethnic groups have systematically different expectations or standards when they are prompted to evaluate their own health, reporting differences, labeled as “reporting heterogeneity,” in SRH may arise (Dowd and Todd, 2011). This reporting heterogeneity in SRH can also depend on group differences in health pessimism or optimism (Boardman, 2004; Krause & Jay, 1994; Spencer et al., 2009) and tendency to incorporate social and emotional well-being when self-assessing health (Finch, Hummer, Reindl, & Vega, 2002).
Racial and ethnic minorities in the United States on average report poorer SRH than non-Hispanic whites (Bzostek, Goldman, & Pebley, 2007; Cagney, Browning, & Wen, 2005; Liang et al., 2010). This minority disadvantage in SRH is particularly intriguing in the case of Hispanics. Despite their relatively poorer SRH, Hispanics tend to fare at least similarly to and or even better than whites in terms of longevity (Hummer, Powers, Pullum, Gossman, & Frisbie, 2007; Markides & Coreil, 1986; Markides & Eschbach, 2005, 2011). The average life expectancy at birth for the U.S. Hispanic population in 2006 was 80.6 years compared with 78.1 years for non-Hispanic whites (Arias, 2010). This seeming paradox has motivated studies that seek to understand the cognitive and cultural processes in which Hispanics evaluate their own health (Idler & Benyamini, 1997; Kaplan & Camacho, 1983; Liang et al., 2010).
There is evidence that Spanish-speaking Hispanics reported lower levels of SRH than those more fluent in English (Angel, Buckley, & Finch, 2001; Angel & Guarnaccia, 1989; Bzostek et al., 2007; DuBard & Gizlice, 2008; Franzini & Fernandez-Esquer, 2004; Kandula, Lauderdale, & Baker, 2007; Phillips, Hammock, & Blanton, 2005; Shetterly, Baxter, Mason, & Hamman, 1996), lending support to the idea of a cultural orientation among Hispanics to be less likely to rate one’s own health highly (Shetterly et al., 1996). None the less, controlling for proxy factors of these cultural orientations, such as nativity status, age at migration, and language use, Hispanics who were interviewed in Spanish still reported poorer health than those who were interviewed in English (Viruell-Fuentes, Morenoff, Williams, & House, 2011), pointing to a possible linguistic reason why Hispanics interviewed in Spanish in health surveys reported lower SRH than expected by objective health. Specifically, it was noted that the translation of “fair” in English to “regular” in Spanish makes this response category of SRH less negative, resulting in respondents interviewed in Spanish more likely to select the “fair” category despite their “better-than-fair” health status (Bzostek et al., 2007; Viruell-Fuentes, Morenoff, Williams, & House, 2011).
In search of clues for the relatively pessimistic ratings of health by Hispanics, another plausible explanation lies in a process called “somatization”—expressing health complaints that are indicative of personal or social problems (Angel & Guarnaccia, 1989; Finch et al., 2002; Hulme, 1996). Based on data from the Hispanic Health and Nutrition Examination Survey, Angel and Guarnaccia (1989) investigated the issue of somatization among Mexican Americans and Puerto Ricans. Using the physician’s assessment as a control, Angel and Guarnaccia examined the association between depressive affect and self-perceptions of health for individuals with similar evaluated health levels. Their findings reveal rather dramatic discrepancies between individual’s assessments of their health and physicians’ evaluations. In addition, the data reveal that, net of the physician’s evaluation, individuals’ assessments of their overall health status are significantly influenced by their affective states.
It could also be the case that Hispanics, relative to whites, have less access to health care and may thus be less aware of health conditions lacking professional diagnoses (Ferraro & Kelley-Moore, 2001). The relative economic advantages of whites may allow them to have better management of chronic conditions; and therefore, health problems experienced by whites may be controlled well with potentially long symptom-free periods (e.g., asthmas and diabetes)—so they tend to rate health better in spite of the presence of objective health conditions. Of course, different racial/ethnic groups may also differ in the frame of reference used when responding to the global SRH question, as suggested by an earlier small qualitative study (Krause & Jay, 1994), but the findings are not conclusive.
Despite the various explanations proposed to explain Hispanic–white disparities in SRH, the comparability between the two groups in terms of SRH has not been adequately examined. Although the literature on SRH has proliferated in the past two decades, the bulk of the studies do not pay attention to group differences in SRH validity (Idler & Benyamini, 1997). More recently, studies have emerged to compare the predictive utility of SRH on mortality across United States ethnic groups but mainly focused on black–white differences with mixed findings (Ferraro & Kelley-Moore, 2001; Gibson, 1991; Johnson & Wolinsky, 1994). Studies examining Hispanic–white disparities in SRH validity have been limited by local samples (Bzostek et al., 2007; Shetterly et al., 1996), cross-sectional design (Bzostek et al., 2007; Viruell-Fuentes et al., 2011), or older data (Finch et al., 2002; Franks et al., 2003; McGee, Liao, Cao, & Cooper, 1999). One longitudinal study is noteworthy. McGee and colleagues (1999) compared the predictive utility of SRH on mortality between Hispanics and whites using data from the pooled 1986–1994 data from the National Health Interview Survey. The findings suggest strong associations between SRH and subsequent mortality in all five racial/ethnic groups—native Americans, Asian/Pacific Islanders, blacks, whites, and Hispanics—but the effect sizes, or predictive powers of SRH for mortality, seem stronger among whites and Asian/Pacific Islanders than among blacks and Hispanics. Despite its unique contribution, this study was not focused on ethnic disparities in SRH validity, did not control for key variables, such as language of interview and nativity, and used relatively dated data. More recent data are needed to investigate this issue considering that growth and changes in the Hispanic population in the United States may have had an impact on the SRH of these groups (Stroup-Benham, Markides, Espino, & Goodwin, 1999). Assuming mortality is one legitimate metric for SRH validity, a longitudinal analysis of the predictive power of SRH on subsequent mortality in a nationally representative sample would shed more light on this issue (Franks et al., 2003).
Using data from a nationally representative longitudinal sample, our study extends previous research on Hispanic–white disparities in SRH by assessing if differences in self-perceptions of health status between non-Hispanic whites and Hispanics, as reflected by SRH, correspond well with differences in subsequent mortality between the two groups. Specifically, by using the subsequent all-cause mortality as a yardstick for retrospective health, this study aims to reveal whether and the extent to which Hispanics rate their health differently from whites. We also offer a broader range of controls to provide a more stringent test on the SRH–mortality relationship. The use of subsequent mortality as a yardstick of retrospective health is based on three premises: (a) there is an intrinsic relationship between general health status for the time being and risk of mortality in the future—better current health should be associated with a lower risk of subsequent mortality; (b) if whites and Hispanics perceive their health the same way, differences in SRH between the two groups should correspond well with observed differences in subsequent risk of mortality between the two groups; and (c) if whites and Hispanics perceive SRH differently from one another, examining the inconsistency between SRH and subsequent risk of mortality and its distribution in the two groups should tell which group more positively or negatively rate their health compared with the other group holding the underlying “true health” constant.
Data, Measures, and Methodology
Data: The Health and Retirement Study
The Health and Retirement Study (HRS) is an ongoing longitudinal study funded by the National Institute on Aging that collects information on demographics, health, disabilities, health behaviors, health care, employment, housing, assets, and other retirement-related factors. The incorporated questions cover a wide array of topics including demographics, economic and financial conditions, health status, health behaviors, and changes in these profiles over time. To ensure its representativeness, the HRS utilizes a national area probability sample of households in the contiguous United States, with oversamples of blacks and Hispanics. Institutionalized persons are excluded from the survey population (Heeringa & Connor, 1995).
The first wave of data collection started in 1992, soliciting information from 9,771 respondents who were born between 1931 and 1941. The response rate was 81.6% (Kapteyn, Michaud, Smith, & Soest, 2006). These respondents were then followed every other year for updated information. By the year of 2008, 2,021 or 20.7% of the baseline sample died (passive attrition) and 893 or 9.1% were lost for follow-up (active attrition). The active attrition rates among whites and Hispanics were 8.7% and 9.9%, respectively. Cao and Hill (2005) examined sample attrition in the HRS from 1992 to 2002 and compared between those remaining in the sample and those lost due to active attrition. They found that these two groups were very similar to each other in terms of health status, household income, assets, and labor market status at the 1992 baseline.
The longitudinal design of the HRS allows for the merging of the 1992 baseline data with the 2008 tracker and exit file for information on vital status and its timing. In our analysis, we focus on the relationship between SRH at the baseline and subsequent mortality among whites and Hispanics. The working sample in this study contains 6,248 white and 806 Hispanic respondents who were aged between 51 and 61 in 1992 and who were followed through 2008 with complete information on vital status and its timing.
Measures
The key measures we used in our analysis include SRH at the 1992 baseline and risk of mortality during the 1992–2008 period. Besides these two measures, we also incorporated in our analysis a range of control variables on demographics, SES, health status, and health behaviors at the baseline, as described subsequently.
Mortality after the 1992 baseline.—
The HRS updates information on vital status and its timing at each wave. In the event where death was reported, an exit interview rather than a core interview was attempted. The exit interview was most often accomplished with the widow(er) or with another close relative of the deceased respondent (Kapteyn et al., 2006). Records on mortality and its timing can be verified by linking the HRS data to the National Death Index. This makes it possible for HRS to maintain quality records on reported deaths and its timing since the 1992 baseline.
Health and health behaviors at the 1992 baseline.—
In the 1992 HRS, information on SRH was captured by the question:
“Would you say that your health is excellent, very good, good, fair, or poor?” The same five response categories were also listed for the question: “What about your emotional health—how good you feel or how stressed, anxious or depressed you feel?”
Besides SRH and emotional well-being, the HRS data also contain information on chronic conditions and functional limitations. Respondents were asked if they were told by their physicians if they had hypertension, diabetes, cancer, heart diseases, stroke, chronic lung diseases, arthritis or rheumatism, and other chronic conditions. Based on this information, we created a dummy variable denoting whether a respondent reported any chronic condition. Respondents were also asked if they had any difficulty dealing with a variety of activities such as running, jogging, walking, sitting, climbing stairs, carrying things, and so forth. We collapsed these variables into a single dummy variable indicating if a respondent reported any functional limitation or not.
We used current smoking status and physical activities to characterize health behaviors at the baseline. In the HRS, respondents were asked if they were currently smoking. They were also asked about their participation in physical activities at different levels. These physical activities were classified into three categories including vigorous, moderate/mild, and none.
The 1992 HRS also collects information on height and weight based on respondents’ self-report. We used the height and weight information to calculate BMI and incorporated these anthropometrics as control variables in our multivariate analysis of the effect of baseline SRH on subsequent mortality.
Race and ethnicity.—
Respondents in the HRS were asked to identify their own racial and ethnic background from the following seven categories: (1) white/Caucasian; (2) black/African American; (3) American Indian or Alaskan Native (including combination of 1 and 2); (4) Asian or Pacific Islander; (5) Hispanic/Latino; (6) brown, “Moreno”; trigueno, “de color” (of color), combination of black and American Indian; and (7) others (specify). The working HRS sample in this study selected only those who identified with “1” or “5” in the racial and ethnic categories listed.
Acculturation.—
The two measures we used to capture acculturation are nativity and language of interview. These measures have been widely used in previous research as indicators of acculturation, particularly in studies examining the relationship between acculturation and health behaviors (Abraído-Lanza, Chao, & Flórez, 2005; Leclere, Jensen, & Biddlecom, 1994; Singh & Siahpush, 2002; Su, Li, & Pagán, 2008; Zambrana, Breen, Fox, & Gutierrez-Mohamed, 1999). Most respondents in the HRS were interviewed in English; however, for Hispanic respondents with no or limited English proficiency, they were interviewed in Spanish if preferred. Despite the team translation approach adopted by the HRS to reduce errors and discrepancies in the translation process (Tirodkar, Song, Chang, Dunlop, & Chang, 2008), subtle differences between the two versions of the questionnaires might still exist, which could potentially influence how the respondents report their health. In particular, the five standard response categories for SRH are conventionally translated into Spanish as excelente (excellent), muy buena (very good), buena (good), regular (fair), and mala (poor). Because the Spanish word “regular” connotes more positive ratings than “fair” does in English, the translation of this response option may downwardly bias estimates of SRH status for Hispanics (Viruell-Fuentes et al., 2011). Therefore, it is important to consider the effect of language of interview in assessing the comparability of SRH between Hispanics and non-Hispanics.
Socioeconomic status.—
We used four variables to characterize SES at the 1992 baseline including marital status, years of education, annual household income, and health insurance status. Household income was calculated by adding income from all sources including salary and wages, dividends, rent, interests, and other sources. Because these variables were used only as the control variables in the regression analyses, we did not code them in more detailed categories.
Methodology
We first calculated descriptive statistics comparing between Hispanics and whites at the 1992 baseline in terms of selected variables on demographics, SES, health, and health behavior. We then estimated a series of logit models to assess the robustness of the observed white–Hispanic differences in SRH controlling for selected variables on demographics, SES, health, and health behavior at the baseline. In particular, the incorporation of language of interview as one of the controlled variables allows us to examine the extent to which whites and Hispanics differ from each other in terms of SRH after the effect of language of interview has been taken into consideration.
We then adopted the life table method to estimate survival curves from 1992 to 2008 by SRH categories at the baseline, respectively, among whites and Hispanics. Comparisons of these survival curves across the two groups are expected to reveal whether and the extent to which one group had more positively or negatively evaluated their own health status than the other.
To verify these findings in a multivariate framework, we then ran a series of cox proportional hazards (CPH) models (Cox and Oakes, 1984), respectively, among white and Hispanic respondents. The dependent variable is the hazard rate of dying at any time after the 1992 baseline, which is modeled as a function of SRH in 1992 and controlled variables on demographics, SES, anthropometrics, health conditions, and health behaviors at the baseline. We examined the SRH gradients in mortality among whites and Hispanics, respectively, by incorporating these controlled variables step by step in order to evaluate the sensitivity of the observed SRH–mortality association to the incorporation of additional variables.
We calculated z statistics to denote if the differences between white and Hispanic respondents in the SRH gradients in mortality are statistically significant. The use of z or t statistics has been fairly common in testing if the effect of a given explanatory variable on the focal-dependent variable is invariant across groups (Paternoster, Brame, Mazerolle, & Piquero, 1998). In our study, we estimated z using the formula proposed by Paternoster and colleagues as indicated subsequently:
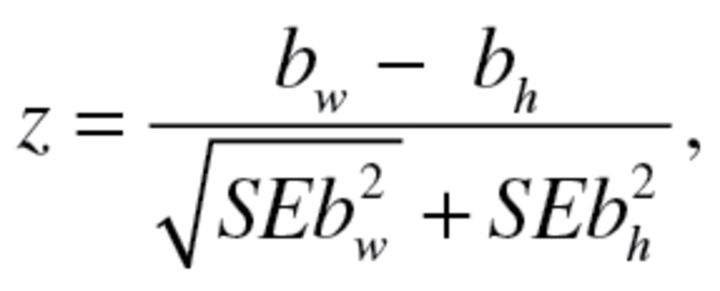 |
where bw is the hazard rate of dying associated with a certain SRH category among white respondents during the 1992–2008 period; bh is the hazard rate of dying associated with the same SRH category among Hispanic respondents during the 1992–2008 period;  and
and  are the coefficient variances associated with the hazard rate coefficients among whites and Hispanics, respectively.
are the coefficient variances associated with the hazard rate coefficients among whites and Hispanics, respectively.
Results
A Comparative Description of Whites and Hispanics in the 1992 HRS
Results in Table 1 present a description of the variables used in the analysis and the white–Hispanic differences in these variables. In terms of demographics, a notable difference between the two groups lies in nativity. About 53% of Hispanics in the 1992 HRS were foreign born compared with 4.3% among whites. The use of Spanish as the language of interview was virtually all for Hispanic respondents. About 45% of Hispanic respondents were interviewed in Spanish and 54.6% were interviewed in English.
Table 1.
Description of the Health and Retirement Sample (HRS) at the 1992 Baseline (Mean or %)
| Variables | Whites | Hispanics | Total |
|---|---|---|---|
| Demographics | |||
| Age | 55.8 | 55.5 | 55.7 |
| Gender | |||
| Male | 49.0 | 46.0 | 48.7 |
| Female | 51.0 | 54.0 | 51.3 |
| Nativity | |||
| Native born | 95.7 | 46.8 | 90.1 |
| Foreign born | 4.3 | 53.2 | 9.9 |
| Language of interview | |||
| English | 99.9 | 54.6 | 94.7 |
| Spanish | 0.1 | 45.4 | 5.3 |
| Socioeconomic status | |||
| Marital status | |||
| Married | 79.4 | 70.1 | 78.4 |
| Unmarried | 20.6 | 29.9 | 21.6 |
| Years of education | 12.7 | 8.4 | 12.2 |
| Annual household, $ (log transformed) | 10.6 | 9.9 | 10.5 |
| Health insurance | |||
| Insured | 90.1 | 65.1 | 87.3 |
| Uninsured | 9.9 | 34.9 | 12.7 |
| Baseline health/health behavior | |||
| Self-rated health (SRH) | |||
| Excellent | 24.5 | 14.6 | 23.4 |
| Very good | 31.2 | 14.4 | 29.3 |
| Good | 26.6 | 31.6 | 27.2 |
| Fair | 11.0 | 25.8 | 12.7 |
| Poor | 6.6 | 13.5 | 7.4 |
| Emotional well-being | |||
| Excellent | 21.0 | 14.5 | 20.3 |
| Very good | 31.1 | 19.6 | 29.8 |
| Good | 31.9 | 39.5 | 32.7 |
| Fair | 11.9 | 21.8 | 13.1 |
| Poor | 4.1 | 4.6 | 4.1 |
| Height (inches) | 67.3 | 64.7 | 67.0 |
| BMI | 26.8 | 27.9 | 27.2 |
| Chronic disease | |||
| Yes | 67.1 | 65.5 | 66.9 |
| No | 32.9 | 34.5 | 33.1 |
| Functional limitation | |||
| Yes | 40.3 | 40.1 | 40.3 |
| No | 59.7 | 59.9 | 59.7 |
| Currently smoking cigarettes | |||
| Yes | 27.3 | 24.1 | 27.7 |
| No | 72.7 | 75.9 | 72.3 |
| Physical exercises | |||
| Vigorous | 54.7 | 30.1 | 51.9 |
| Moderate/mild | 26.8 | 36.5 | 27.9 |
| None | 18.5 | 33.4 | 20.2 |
| Number of cases at the baseline | 6,248 | 806 | 7,054 |
| Number of deaths (1992–2008) | 1,374 | 176 | 1,550 |
| Percentage of deaths | 22.0 | 21.8 | 22.0 |
Note. The Health and Retirement Study.
There are also substantial differences in SES between Hispanic and white respondents in the 1992 HRS. Relative to their white counterparts, Hispanic respondents were less likely to be married, had lower level of education and household income, and were much less likely to have health insurance coverage.
Hispanic respondents in the HRS reported worse SRH than whites. The percentage of poor SRH among Hispanics is 13.5, more than double the 6.6% for whites. This gap becomes even more apparent in the case of fair SRH with 25.8% for Hispanics and 11% for whites. Combining the poor and fair SRH categories, 39.3% of Hispanics rated their health to be poor or fair compared with 17.6% among whites. Similar differences, though to a lesser extent, can also be observed in the case of emotional well-being.
Despite the substantial differences in SRH between whites and Hispanics, the two groups were comparable in terms of the prevalence of chronic diseases and functional limitations at the 1992 baseline. The two groups also had similar mortality rates. About 22% of white respondents died between 1992 and 2008 compared with 21.8% of Hispanics.
Assessing White–Hispanic Differences in SRH in a Multivariate Framework
We assessed white–Hispanic differences in SRH validity by estimating three logit models, where we related selected explanatory variables to the odds of reporting fair or poor health. Results presented in Table 2 confirm that Hispanics were more likely than whites to report fair or poor health after adjusting for differences in selected variables on demographics, SES, health, and health behavior at the baseline. For instance, based on results from Model 1, the odds of reporting fair or poor health among Hispanics is 24% higher (p < .001) than among whites after controlling for the effect of age, gender, nativity, and language of interview. The magnitude of this Hispanic–white gap in the odds of reporting fair or poor health becomes mitigated in Models 2 and 3, where additional variables were incorporated into the analysis, but the difference remains statistically significant (p < .05 in Model 2 and p < .001 in Model 3).
Table 2.
Selected Predictors of Reporting Poor/Fair Health at the 1992 Baseline Expressed as Odds Ratios (ORs)
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Demographics | |||
| Ethnicity | |||
| Whites | 1.00 | 1.00 | 1.00 |
| Hispanics | 1.24*** (1.18, 1.31) | 1.08* (1.02, 1.15) | 1.17*** (1.09, 1.26) |
| Age | 1.05*** (1.03, 1.07) | 1.03* (1.01, 1.05) | 1.02 (0.99, 1.04) |
| Gender | |||
| Male | 1.00 | 1.00 | 1.00 |
| Female | 1.12 (1.00, 1.26) | 0.95 (0.83, 1.08) | 0.79* (0.63, 0.99) |
| Nativity | |||
| Native born | 1.00 | 1.00 | 1.00 |
| Foreign born | 0.76* (0.59, 0.98) | 0.82(0.62, 1.08) | 0.93 (0.67, 1.29) |
| Language of interview | |||
| English | 1.00 | 1.00 | 1.00 |
| Spanish | 2.28*** (1.65, 3.15) | 0.93 (0.64, 1.34) | 1.28 (0.83, 1.98) |
| Socioeconomic status | |||
| Marital status | |||
| Married | 1.00 | 1.00 | |
| Unmarried | 1.21* (1.03, 1.41) | 1.02 (0.85, 1.24) | |
| Years of education | 0.86*** (0.84, 0.88) | 0.92*** (0.90, 0.95) | |
| Annual household, $ (log transformed) | 0.59*** (0.56, 0.64) | 0.71*** (0.65, 0.77) | |
| Health Insurance | |||
| Insured | 1.00 | 1.00 | |
| Uninsured | 0.93 (0.78, 1.12) | 0.89 (0.71, 1.10) | |
| Baseline health/health behavior | |||
| Emotional well-being | |||
| Excellent | 1.00 | ||
| Very good | 1.00 (0.76, 1.32) | ||
| Good | 1.75*** (1.36, 2.25) | ||
| Fair | 6.69*** (5.11, 8.76) | ||
| Poor | 13.01*** (8.89, 19.08) | ||
| Height (inches) | 0.99 (0.97, 1.02) | ||
| BMI | 1.02* (1.00, 1.03) | ||
| Chronic disease | |||
| No | 1.00 | ||
| Yes | 4.86*** (3.87, 6.10) | ||
| Functional limitation | |||
| No | 1.00 | ||
| Yes | 3.67*** (3.11, 4.32) | ||
| Currently smoking cigarettes | |||
| No | 1.00 | ||
| Yes | 1.40*** (1.18, 1.65) | ||
| Physical exercises | |||
| Vigorous | 1.00 | ||
| Moderate/mild | 1.42*** (1.18, 1.71) | ||
| None | 2.37*** (1.96, 2.88) | ||
| Number of cases | 7,054 | 6,980 | 6,980 |
Note. The Health and Retirement Study. *p < .05. ***p < .001.
Results from Table 2 also provide evidence regarding the effect of language of interview on SRH and how the effect changes across models. Based on results from Model 1, being interviewed in Spanish was associated with a higher odds of reporting fair or poor health after controlling for the effect of ethnicity, age, gender, and nativity (odds ratio [OR] = 2.28, p < .001). This effect, however, becomes insignificant in Models 2 and 3 where explanatory variables characterizing SES and baseline health and health behavior have been incorporated into the analysis.
SRH and Subsequent Mortality Among Whites and Hispanics
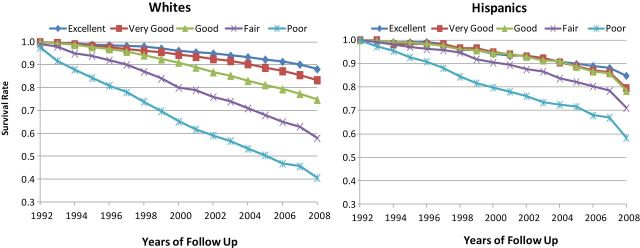
Figure 1 shows the survival curves during the period of 1992–2008 by SRH categories among whites and Hispanics. A comparison between the two sets of survival curves reveals that the association between SRH and subsequent mortality differs substantially between Hispanics and whites. In both groups, mortality is reduced as SRH improves, yet the SRH gradient in mortality turns out to be much smaller among Hispanics than among whites. At the end of the 16 years of follow-up, the mortality gap between those who rated their health excellent and those who rated their health poor at the baseline was about 25% among Hispanics compared with roughly 50% for whites. Among Hispanics, mortality differences associated with excellent, very good, and good SRH did not unfold until almost the end of the follow-up. Before 2004, there were virtually no mortality differences across the three survival curves. This is different from the survival curves associated with whites, where mortality differences across excellent, very good, and good SRH were more pronounced. Similar differences between Hispanics and whites can also be observed in the survival curves associated with poor and fair SRH, where the survival gap between the two curves was much smaller among Hispanics.
Figure 1.
Self-rated health (SRH) in 1992 and subsequent survival curves among whites and Hispanics. Source: The Health and Retirement Study.
Figure 1 also reveals a notable Hispanic advantage in mortality among those who rated their health poor or fair at the baseline. Among white respondents, who rated their health poor at the 1992 baseline, 41% survived by 2008. The corresponding percentage among Hispanics is 58. Similar findings also hold in the case of fair SRH. The survival rate was 58% among whites compared with 71% among Hispanics.
SRH in 1992 and Subsequent Risk of Mortality Among Whites and Hispanics: A Multivariate Analysis
We next assessed in a multivariate framework if the relation between SRH and subsequent mortality differs between white and Hispanic respondents based on results from three CPH models. An important assumption of the CPH analysis is the proportionality of hazard, that is, the effect of changing values for a certain explanatory variable on the hazard rate is constant, independent of time. This assumption was tested for all the explanatory variables in the CPH models by relating the Schoenfeld residuals to time (Allison, 2010). The results of this testing confirmed that the proportionality assumption was upheld (results not shown here).
Table 3 shows the hazard ratios of mortality associated with each of the SRH categories among the white and Hispanic respondents in the HRS. Overall, the results indicate a patterned SRH gradient in risk of mortality: mortality risk becomes smaller as SRH improves. Relative to the SRH gradient in Model 1, where only the effects of demographics are adjusted for, the range of the gradient becomes increasingly smaller in Models 2 and 3. This is because the effect of SRH on subsequent mortality is correlated to the effect of SES, baseline health, and health behaviors. Once these confounding factors have been taken into consideration, the SRH effect becomes less salient.
Table 3.
Self-Rated Health (SRH) in 1992 and Relative Mortality Risk in the 1992–2008 Period: A Comparison Between Whites and Hispanics
| SRH | Whites | Hispanics | z statisticsa |
|---|---|---|---|
| Model 1: Adjusting only for demographicsb | |||
| Excellent | 1.00 | 1.00 | |
| Very good | 1.44*** (1.19, 1.74) | 1.33 (0.69, 2.58) | 0.22 |
| Good | 2.27*** (1.89, 2.72) | 1.54 (0.86, 2.73) | 1.27 |
| Fair | 4.27*** (3.52, 5.18) | 2.20** (1.25, 3.89) | 2.16 > 1.96 |
| Poor | 7.35*** (6.03, 8.98) | 4.11*** (2.26, 7.46) | 1.82 |
| Model 2: Adjusting for demographics and SESc | |||
| Excellent | 1.00 | 1.00 | |
| Very good | 1.43*** (1.18, 1.73) | 1.35 (0.70, 2.60) | 0.17 |
| Good | 2.18*** (1.81, 2.62) | 1.52 (0.85, 2.71) | 1.17 |
| Fair | 3.82*** (3.12, 0.94) | 2.00* (1.12, 3.58) | 2.06 > 1.96 |
| Poor | 6.11*** (4.93, 7.57) | 3.45*** (1.85, 6.55) | 1.65 |
| Model 3: Adjusting for demographics, SES, and baseline health/health behaviorsd | |||
| Excellent | 1.00 | 1.00 | |
| Very good | 1.25* (1.02, 1.53) | 1.19 (0.61, 2.34) | 0.15 |
| Good | 1.67*** (1.37, 2.05) | 1.12 (0.61, 2.07) | 1.19 |
| Fair | 2.69*** (2.14, 3.39) | 1.24 (0.65, 2.34) | 2.21 > 1.96 |
| Poor | 4.30*** (3.33, 5.56) | 1.99 (0.99, 4.02) | 1.97 > 1.96 |
Notes. SES = socioeconomic status. The Health and Retirement Study (N = 8,578). Numbers in the brackets are 95% confidence intervals.
aTo denote if the hazard ratios associated with SRH are significantly different between whites and Hispanics.
bControlling for the effect of age, gender, nativity, and language of interview.
cControlling for the effect of age, gender, nativity, language of interview, marital status, education, annual household income, and health insurance status.
dControlling for the effect of age, gender, nativity, language of interview, marital status, education, annual household income, and health insurance status, emotional well-being, height, BMI, chronic diseases, functional limitations, physical exercises, and current smoking status.
*p < .05. **p < .01. ***p < .001 (two-tailed test).
It should be noted, however, that this patterned SRH–mortality gradient generally fits better among whites than among Hispanics. This is especially the case in Model 3, where all selected explanatory variables have been incorporated in the analysis. The results indicate a notable difference between whites and Hispanics in terms of the SRH–mortality association: while the SRH gradients in mortality are well patterned and statistically significant among whites, the corresponding gradients among Hispanics are neither statistically significant and nor as well patterned.
Based on the z statistics, the major difference between whites and Hispanics in terms of the association between SRH at the baseline and subsequent mortality lies in the case of fair SRH and to a lesser extent in the case of poor SRH. The mortality gap between those who reported excellent health and those who reported fair health at the baseline is substantially smaller among Hispanics than among whites. In all three models, this white–Hispanic difference is statistically significant (z > 1.96). Similar findings can also be observed in the case of poor SRH in Model 3. Consistent with the survival curves as revealed in Figure 1, the hazard ratios in Table 3 also show that the SRH gradients in mortality are more pronounced among whites than among Hispanics.
Limitations of the Study
Due to data constraints, several limitations of this study are worth noting. First, since the age range of the 1992 HRS sample is between 51 and 61, our findings are more relevant for this age group than for other age groups. Future studies can assess whether and the extent to which the Hispanic exception in SRH as revealed in this study still holds in other age groups or birth cohorts.
Second, despite the fact that HRS oversamples Hispanics, the number of Hispanics in the sample is much smaller than that of whites. This could have potentially contributed to the less salient impact of baseline SRH on subsequent survival among Hispanics than among whites. Moreover, the relatively modest sample size of Hispanics in the HRS also makes it difficult to assess heterogeneities by country of origin within Hispanics in terms of perceptions of health status (Angel & Angel, 1992; Angel & Guarnaccia, 1989; Markides, Rudkin, Angel, & Espino, 1997).
Third, the longitudinal design of HRS implies that sample attrition and its distribution needs to be taken into account for a more robust assessment of the comparability of SRH between whites and Hispanics. Based on their analysis of the mortality and sample attrition records between 1992 and 2008 in the HRS, Zhivan and colleagues (2012) used a competing risks model to examine racial/ethnic differences in sample attrition and their explanatory factors. Their findings reveal that chances of attrition associated with health conditions were greater for Mexican Americans than that for white counterparts. It was also reported that among those who ranked their health poor or fair at the baseline, the probability of attrition is, respectively, 14.9% and 11.2% among whites and Hispanics. A related issue here concerns the selective return of less healthy Hispanics to their country of birth or the so-called salmon bias hypothesis in explaining the Hispanic paradox in mortality (Pablos-Méndez, 1994). Based on mortality records in Social Security data, Turra and Elo (2008) examined the effect of salmon bias on the Hispanic mortality advantage among those aged 65 and older. Their study confirmed the existence of salmon bias, yet concluded that the effect was of too small a magnitude to be a primary explanation for the lower mortality of Hispanics in the sample. These findings do not necessarily negate our results, but they highlight the relevance of sample attrition in more reliable estimates of white–Hispanic disparities in mortality using panel data. It would be a further step for future studies to test the sensitivity of our results in the face of sample attrition.
Finally, because information on causes of death is masked in the publicized version of the HRS data, we could only rely upon all-cause mortality as a yardstick for baseline health. If information on causes of deaths is available, it would be valuable to relate baseline SRH to subsequent cause-specific mortality. Such a further step would make it possible to pinpoint the specific causes of death that are closely related to baseline health, which could potentially lead to more clues for ethnic differences in perceptions of health status and their contributing factors.
Discussion
Ethnic disparities in SRH validity are important because SRH is routinely included in health surveys, is widely recognized as a valid measure of objective health, and is often used as a barometer of health disparities across social groups. There is, however, potential response bias in SRH for Hispanic respondents (Bzostek et al., 2007) who tend to rate their health lower than what would be expected from objective health measures (Borrell & Dallo, 2008; Cho, Frisbie, Hummer, & Rogers, 2004; Kandula et al., 2007; Viruell-Fuentes et al., 2011). The question of whether Hispanics’ SRH operates as a valid measure of objective health has important policy and research implications if we are interested in using SRH as a reliable measure to assess the extent and determinants of disparities in health status and health care.
One of the key findings of this study is that when subsequent mortality was used as a yardstick to assess the validity of SRH at the baseline, Hispanics tended to rate their health more pessimistically than whites. This was especially the case for Hispanics who rated their health fair or poor at the baseline, whereas their presumed health conditions, as reflected by subsequent risk of mortality, should be considerably better than their white counterparts. These findings call for caution in relying on SRH to quantify and explain health disparities across racial and ethnic groups in the United States (Dowd and Todd, 2011). Our results indicate that health disparities between whites and Hispanics will be overestimated if the assessment has been solely based on differences in SRH between the two groups.
Our study rests on the premise that subsequent mortality can serve as a more objective measure of retrospective health status than SRH. Such a premise essentially rules out the possibility for Hispanics to actually have poorer health than whites at the baseline yet nonetheless have lower mortality afterward. Empirical evidence from the HRS provides little support to this possibility. Results in Table 1 indicate that the prevalence of chronic conditions, functional limitations, and smoking were pretty close between Hispanics and whites at the 1992 baseline.
It should be noted that the Hispanic exception in the predictive utility of SRH, however, does not necessarily mean that SRH is no longer a valid health measure among Hispanics. On the contrary, the survival curves in Figure 1 and the SRH gradients in mortality in Table 3 all point to the validity of SRH as an overall health indicator that differentiates health status among Hispanics. The problem arises when SRH is used to compare between Hispanics and whites in terms of health status. Our findings indicate that the variations in health that SRH captures turn out to be much smaller among Hispanics than among whites, suggesting a weaker SRH–mortality link. In other words, relative to whites, the substantially lower risk of mortality associated with fair SRH among Hispanics suggests that fair SRH may not presage the same mortality force for Hispanics as for whites.
Although language of interview is important in understanding the different perceptions of health between Hispanics and non-Hispanics, linguistic bias is only one of the explanatory factors. As indicated by the results from the multivariate CPH analysis, even after adjusting for the effects of language of interview, the relative mortality risk associated with fair SRH is still much lower among Hispanics than among whites. Moreover, the robustness of this Hispanic exception in SRH despite controlling for selected variables on demographics, SES, and baseline health, and health behaviors suggests that other nonincorporated factors need to be considered to better account for the Hispanic exception in SRH.
Findings from our study point to the need to assess the role of ethnicity and its associated cultural background in SRH. Ethnic groups may differ in how they weigh health dimensions and how they prioritize components of health when reporting health. Whites, for instance, may tend to use physical functioning as a frame of reference of overall health (Krause & Jay, 1994), whereas Hispanics may think more about emotional health when interpreting SRH (Spencer et al., 2009). Such a difference has important implications regarding the relatively weak linkage between SRH and mortality among Hispanics as observed in this study. The weaker linkage between SRH and objective health among Hispanics might be related to somatization—expressing health complaints that are indicative of economic disadvantages or hardships that most Hispanic immigrants have to overcome in the process of immigration and settlement in the receiving community (Angel & Guarnaccia, 1989; Finch et al., 2002; Hulme, 1996; Finch, Kolody, & Vega, 2000; Vega & Amaro, 1994). It is possible that objectively healthy Hispanics can underestimate their health if they feel marginalized in the society. On the other hand, the alarmingly high rates of uninsurance among Hispanics (34.9% in this study) imply that objectively unhealthy Hispanics might be unreasonably optimistic about their health if they are not aware of undiagnosed illnesses if they have any. Although both scenarios can help explain the relatively weak SRH–mortality association among Hispanics, more information is needed to assess the relative importance of either one.
Previous studies have documented a close linkage between the identification with collectivist culture and a tendency to select midpoints of general scales among Asian Americans (Chen, Lee, & Stevenson, 1995; Iwata & Higuchi, 2000; Kitayama, Markus, Matsumoto, & Norasakkunkit, 1997). These studies also report that Asian Americans, in particular Japanese, tend to avoid selecting extreme positive scales when reporting their emotions. In their study of SRH among Asian Americans, Erosheva and coauthors (Erosheva, Walton, & Takeuchi, 2007) explain how the native culture of immigrants and their acculturation into the United States can influence their perceptions of health:
Collectivist societies tend to encourage self-criticism, understatement of personal virtues, and diffidence in individual behavior. Accordingly, individuals in these societies may be more likely to avoid extreme ratings, either positive or negative, in describing their behavior and emotions. On the other hand, the cultural environment of the United States rewards self-enhancement, and individuals may be more likely to use the full range of options in rating their own behavior and emotions (p. 80).
It remains to be seen to what extent this cultural interpretation can be used to explain the Hispanic exception in SRH. There is evidence that Hispanics are more unwilling to select “excellent/very good” categories of SRH because they tend to be shy away from “boasting” or “being optimistic” about their health (Shetterly et al., 1996). To verify this explanation, more qualitative information is needed, such as the references, if any, Hispanics use in evaluating their own health, what these SRH categories exactly mean to them (Idler & Benyamini, 1997; Viruell-Fuentes et al., 2011), and how Hispanics differ from whites in the way sociodemographic factors affect SRH (Franks et al., 2003). Examining these issues would presumably provide new insights into social and cultural differences in defining health and illness (Bzostek et al., 2007), enhance our understanding of the root causes of Hispanic–white disparities in SRH (Viruell-Fuentes et al., 2011), and advance research on racial/ethnic disparities in health in general (Anderson, Bulatao, & Cohen, 2004).
Funding
This study was supported by a grant from Centers for Disease Control and Prevention (grant number: 1H75DP001812-02).
Acknowledgments
The authors would like to thank anonymous reviewers designated by Journal of Gerontology: Social Sciences (JGSS), Merril Silverstein, and Megan Kelly for their comments. All authors substantially contributed to the conceptualization, research design, literature review, and writing of the article. Data analysis was solely completed by Dejun Su. Views and opinions endorsed by the authors in this study do not reflect those of the funding agency.
References
- Abraído-Lanza A. F., Chao M. T., Flórez K. R. 2005. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine (1982), 61, 1243–1255. doi:10.1016/j.socscimed.2005.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison P. D. 2010. Survival analysis using SAS: A practical guide (2nd ed). Cary, NC: SAS Press. [Google Scholar]
- Anderson N. B., Bulatao R. A., Cohen B. (Eds.). 2004. Critical perspectives on racial and ethnic differences in Health in late life. Washington DC: National Academies Press. [PubMed] [Google Scholar]
- Angel J. L., Angel R. J. 1992. Age at migration, social connections, and well-being among elderly Hispanics. Journal of Aging and Health, 4, 480–499. doi:10.1177/089826439200400402 [DOI] [PubMed] [Google Scholar]
- Angel J. L., Buckley C. J., Finch B. K. (2001). Nativity and self-assessed health among pre-retirement age Hispanics and non-Hispanic whites. International Migration Review, 35, 784–803. doi:10.1111/j.1747-7379.2001.tb00041.x [Google Scholar]
- Angel R., Guarnaccia P. J. 1989. Mind, body, and culture: Somatization among Hispanics. Social Science & Medicine (1982), 28, 1229–1238. doi:10.1016/0277-9536(89)90341–9 [DOI] [PubMed] [Google Scholar]
- Arias E. 2010. United States life tables by Hispanic origin. National Center for Health Statistics.Vital Health Stat 2(152). [PubMed] [Google Scholar]
- Ballis D. S, Segall A, Chipperfield J. G. (2003). Two views of self-rated general health status. Social Science and Medicine, 56, 203–217. [DOI] [PubMed] [Google Scholar]
- Benyamini Y., Idler E. L. 1999. Community studies reporting association between self-rated health and mortality: Additional studies, 1995–1998. Research on Aging, 21, 392–401. doi:10.1177/0164027599213002 [Google Scholar]
- Boardman J. D. (2004). Health pessimism among black and white adults. The role of interpersonal and institutional maltreatment. Social Science & Medicine 59, 2523–2533. [DOI] [PubMed] [Google Scholar]
- Borrell L. N., Dallo F. J. 2008. Self-rated health and race among Hispanic and non-Hispanic adults. Journal of Immigrant and Minority Health, 10, 229–238. [DOI] [PubMed] [Google Scholar]
- Bzostek S., Goldman N., Pebley A. 2007. Why do Hispanics in the USA report poor health? Social Science & Medicine (1982), 65, 990–1003. doi:10.1016/j.socscimed.2007.04.028 [DOI] [PubMed] [Google Scholar]
- Cagney K. A., Browning C. R., Wen M. 2005. Racial disparities in self-rated health at older ages: What difference does the neighborhood make? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, S181–S190. doi:10.1093/geronb/60.4.S181 [DOI] [PubMed] [Google Scholar]
- Cao H., Hill D. H. 2005. Active versus passive sample attrition: The Health Retirement Study. Ann Arbor, MI: Institute for Social Research, University of Michigan. [Google Scholar]
- Chen C, Lee S., Stevenson H. W. 1995. Response style and cross-cultural comparisons of rating scales among East Asian and North American students. Psychological Science, 6, 170–175. doi: 10.1111/ j.1467-9280.1995.tb00327.x [Google Scholar]
- Cho Y., Frisbie W. P., Hummer R. A., Rogers R. G. 2004. Nativity, duration of residence, and the health of Hispanic adults in the United States. International Migration Review, 38, 184–211. doi:10.1111/ j.1747-7379.2004.tb00193.x [Google Scholar]
- Cox D. R., Oakes D. 1984. Analysis of survival data. London: Chapman & Hall. [Google Scholar]
- DeSalvo K. B., Fan V. S., McDonell M. B., Fihn S. D. 2005. Predicting mortality and healthcare utilization with a single question. Health Services Research, 40, 1234–1246. doi:10.1111/j.1475- 6773.2005.00404.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd J. B, Todd M. (2011). Does Self-reported Health Bias the Measurement of Health Inequalities in US Adults? Evidence Using Anchoring Vignettes From the Health and Retirement Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 66(4), 478–489. [DOI] [PubMed] [Google Scholar]
- DuBard C. A., Gizlice Z. 2008. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. American Journal of Public Health, 98, 2021–2028. doi:10.2105/AJPH.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erosheva E., Walton E. C., Takeuchi D. T. 2007. Self-rated health among foreign- and U.S.-born Asian Americans: a test of comparability. Medical Care, 45, 80–87. doi:10.1097/01.mlr.0000241114.90614.9c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro K. F., Kelley-Moore J. A. 2001. Self-rated health and mortality among black and white adults: examining the dynamic evaluation thesis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56, S195–S205. doi:10.1093/geronb/56.4.S195 [DOI] [PubMed] [Google Scholar]
- Finch B. K., Hummer R. A., Reindl M., Vega W. A. 2002. Validity of self-rated health among Latino(a)s. American Journal of Epidemiology, 155, 755–759. doi:10.1093/aje/155.8.755 [DOI] [PubMed] [Google Scholar]
- Finch B. K., Kolody B., Vega W. A. 2000. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior, 41, 295–313. [PubMed] [Google Scholar]
- Franks P., Gold M. R., Fiscella K. 2003. Sociodemographics, self-rated health, and mortality in the US. Social Science & Medicine (1982), 56, 2505–2514. [DOI] [PubMed] [Google Scholar]
- Franzini L., Fernandez-Esquer M. E. 2004. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Social Science & Medicine (1982), 59, 1629–1646. [DOI] [PubMed] [Google Scholar]
- Gibson R. C. 1991. Race and the self-reported health of elderly persons. Journal of Gerontology, 46, S235–S242. [DOI] [PubMed] [Google Scholar]
- Heeringa S. G., Connor J. H. 1995. Technical description of the Health and Retirement Survey sample design. Ann Arbor, MI: Institute for Social Research. University of Michigan. [Google Scholar]
- Hulme P. A. 1996. Somatization in Hispanics. Journal of Psychosocial Nursing and Mental Health Services, 34, 33–37. [DOI] [PubMed] [Google Scholar]
- Hummer R. A., Powers D. A., Pullum S. G., Gossman G. L., Frisbie W. P. 2007. Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography, 44, 441–457. doi:10.1353/dem.2007.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L., Angel R. J. 1990. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. American Journal of Public Health, 80, 446–452. doi:10.2105/ajph.80.4.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. L., Benyamini Y. 1997. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37. [PubMed] [Google Scholar]
- Idler E. L., Kasl S. V. 1995. Self-ratings of health: Do they also predict change in functional ability? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 50, S344–S353. doi:10.1093/geronb/50B.6.S344 [DOI] [PubMed] [Google Scholar]
- Iwata N., Higuchi H. R. 2000. Responses of Japanese and American university students to the STAI items that assess the presence or absence of anxiety. Journal of Personality Assessment, 74, 48–62. doi:10.1207/s15327752jpa740104 [DOI] [PubMed] [Google Scholar]
- Johnson R. J., Wolinsky F. D. 1994. Gender, race, and health: The structure of health status among older adults. The Gerontologist, 34, 24–35. [DOI] [PubMed] [Google Scholar]
- Kandula N. R., Lauderdale D. S., Baker D. W. 2007. Differences in self-reported health among Asians, Latinos, and non-Hispanic whites: The role of language and nativity. Annals of Epidemiology, 17, 191–198. [DOI] [PubMed] [Google Scholar]
- Kaplan G. A., Camacho T. 1983. Perceived health and mortality: A nine-year follow-up of the human population laboratory cohort. American Journal of Epidemiology, 117, 292–304. [DOI] [PubMed] [Google Scholar]
- Kaplan G., Barell V., Lusky A. 1988. Subjective state of health and survival in elderly adults. Journal of Gerontology, 43, S114–S120. doi:10.1093/geronj/43.4.S114 [DOI] [PubMed] [Google Scholar]
- Kaplan G. A., Keil J. E. 1993. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation, 88, 1973–1998. [DOI] [PubMed] [Google Scholar]
- Kapteyn A., Michaud P., Smith J. P., Soest A. V. (Cartographer). 2006. Effects of attrition and non-response in the Health and Retirement Study (Working paper series # 2246). Retrieved from http://www.rand.org/content/dam/rand/pubs/working_papers/2006/RAND_WR407.pdf
- Kitayama S., Markus H. R., Matsumoto H., Norasakkunkit V. 1997. Individual and collective processes in the construction of the self: Self-enhancement in the United States and self-criticism in Japan. Journal of Personality and Social Psychology, 72, 1245–1267. doi:10.1037/0022-3514.72.6.1245 [DOI] [PubMed] [Google Scholar]
- Krause N. M., Jay G. M. 1994. What do global self-rated health items measure? Medical Care, 32, 930–942. [DOI] [PubMed] [Google Scholar]
- Leclere F. B., Jensen L., Biddlecom A. E. 1994. Health care utilization, family context, and adaptation among immigrants to the United States. Journal of Health and Social Behavior, 35, 370–384. [PubMed] [Google Scholar]
- Liang J., Quiñones A. R., Bennett J. M., Ye W., Xu X., Shaw B. A., Ofstedal M. B. 2010. Evolving self-rated health in middle and old age: How does it differ across Black, Hispanic, and White Americans? Journal of Aging and Health, 22, 3–26. doi:10.1177/ 0898264309348877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K. S., Coreil J. 1986. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Reports (Washington, DC: 1974), 101, 253–265. [PMC free article] [PubMed] [Google Scholar]
- Markides K. S., Eschbach K. 2005. Aging, migration, and mortality: Current status of research on the Hispanic paradox. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 68–75. doi:10.1093/geronb/60.Special_Issue_2.S68 [DOI] [PubMed] [Google Scholar]
- Markides K. S., Eschbach K. 2011. Hispanic Paradox in adult mortality in the United States. In Rogers R. G., Crimmins E. M. (Eds.), International Handbook of Adult Mortality (pp. 227–240). New York, NY: Springer. [Google Scholar]
- Markides K. S., Rudkin L., Angel R. J., Espino D. V. 1997. Health status of Hispanic elderly. In Martin L. G., Soldo B. J. (Eds.), Racial and ethnic differences in the health of older Americans (pp. 285–300). Washington DC: National Academy Press. [Google Scholar]
- McGee D. L., Liao Y., Cao G., Cooper R. S. 1999. Self-reported health status and mortality in a multiethnic US cohort. American Journal of Epidemiology, 149, 41–46. [DOI] [PubMed] [Google Scholar]
- Mossey J. M., Shapiro E. 1982. Self-rated health: A predictor of mortality among the elderly. American Journal of Public Health, 72, 800–808. doi:10.2105/ajph.72.8.800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pablos-Méndez A. 1994. Mortality among Hispanics. Journal of the American Medical Association, 271, 1237. [PubMed] [Google Scholar]
- Paternoster R., Brame R., Mazerolle P., Piquero A. 1998. Using the correct statistical test for the equality of regression coefficients. Criminology, 36, 859–866. [Google Scholar]
- Phillips L. J., Hammock R. L., Blanton J. M. 2005. Predictors of self-rated health status among Texas residents. Preventing Chronic Disease, 2, 1–9. [PMC free article] [PubMed] [Google Scholar]
- Shetterly S. M., Baxter J., Mason L. D., Hamman R. F. 1996. Self-rated health among Hispanic vs non-Hispanic white adults: the San Luis Valley Health and Aging Study. American Journal of Public Health, 86, 1798–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G. K., Siahpush M. 2002. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: An analysis of two national data bases. Human Biology, 74, 83–109. [DOI] [PubMed] [Google Scholar]
- Spencer S, et al. (2009). Racial Differences in Self-Rated Health at Similar Levels of Physical Functioning: An Examination of Health Pessimism in the Health, Aging, and Body Composition Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences 64(1), 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup-Benham C. A., Markides K. S., Espino D. V., Goodwin J. S. 1999. Changes in blood pressure and risk factors for cardiovascular disease among older Mexican-Americans from 1982–1984 to 1993–1994. Journal of the American Geriatrics Society, 47, 804–810. [DOI] [PubMed] [Google Scholar]
- Su D., Li L., Pagán J. A. 2008. Acculturation and the use of complementary and alternative medicine. Social Science & Medicine (1982), 66, 439–453. doi:10.1016/j.socscimed.2007.08.023 [DOI] [PubMed] [Google Scholar]
- Tirodkar M. A., Song J., Chang R. W., Dunlop D. D., Chang H. J. 2008. Racial and ethnic differences in activities of daily living disability among the elderly: The case of Spanish speakers. Archives of Physical Medicine and Rehabilitation, 89, 1262–1266. doi:10.1016/j.apmr.2007.11.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turra C. M., Elo I. T. 2008. The impact of salmon bias on the hispanic mortality advantage: New evidence from social security data. Population Research and Policy Review, 27, 515–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega W. A., Amaro H. 1994. Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health, 15, 39–67. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes E. A., Morenoff J. D., Williams D. R., House J. S. 2011. Language of interview, self-rated health, and the other Latino health puzzle. American Journal of Public Health, 101, 1306–1313. doi:10.2105/ajph.2009.175455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrana R. E., Breen N., Fox S. A., Gutierrez-Mohamed M. L. 1999. Use of cancer screening practices by Hispanic women: Analyses by subgroup. Preventive Medicine, 29, 466–477. doi:10.1006/pmed.1999.0566 [DOI] [PubMed] [Google Scholar]
- Zhivan N. A., Ang A., Amaro H., Vega W. A., Markides K. S. 2012. Ethnic/race differences in the attrition of older American survey respondents: Implications for health-related research. Health Services Research, 47, 241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]