Abstract
Background
Combined abdominal and breast surgery presents a convenient and relatively cost-effective approach for accomplishing both procedures.
Objectives
This study is the largest to date assessing the safety of combined procedures, and it aims to develop a simple pretreatment risk stratification method for patients who desire a combined procedure.
Methods
All women undergoing abdominoplasty, panniculectomy, augmentation mammaplasty, and/or mastopexy in the TOPS database were identified. Demographics and outcomes for combined procedures were compared to individual procedures using χ2 and Student's t-tests. Multiple logistic regression provided adjusted odds ratios for the effect of a combined procedure on 30-day complications. Among combined procedures, a logistic regression model determined point values for pretreatment risk factors including diabetes (1 point), age over 53 (1), obesity (2), and 3+ ASA status (3), creating a 7-point pretreatment risk stratification tool.
Results
A total of 58,756 cases met inclusion criteria. Complication rates among combined procedures (9.40%) were greater than those of aesthetic breast surgery (2.66%; P < .001) but did not significantly differ from abdominal procedures (9.75%; P = .530). Nearly 77% of combined cases were classified as low-risk (0 points total) with a 9.78% complication rates. Medium-risk patients (1 to 3 points) had a 16.63% complication rate, and high-risk (4 to 7 points) 38.46%.
Conclusions
Combining abdominal and breast procedures is safe in the majority of patients and does not increase 30-day complications rates. The risk stratification tool can continue to ensure favorable outcomes for patients who may desire a combined surgery.
Level of Evidence
4 Risk
Risk
The popularity of both breast and abdominal plastic surgery has increased greatly over the years with more than half a million procedures in 2013 alone.1 It is not uncommon for patients who are unhappy with the appearance of their breasts to also desire an abdominal procedure, and patients desiring an abdominal procedure may also want the appearance of their breasts changed. Consequently, requests for combining breast and abdominal procedures, so called “mommy makeovers,” are fairly common. This strategy decreases overall recovery time, may reduce costs, and eliminates the need to undergo a second surgical procedure. Although this is common practice for many surgeons, there is a paucity of published data available on the relative safety of combined procedures.
Many studies to date have demonstrated the relative safety of combined plastic surgery procedures in carefully selected patients.2-6 Only recently, however, have a few studies specifically explored cosmetic breast surgery combined with abdominal procedures.7-9 Stevens et al8 compared 151 combined procedures to 264 abdominoplasties and concluded that the addition of breast surgery did not seem to significantly increase major or minor complication rates. These findings were later corroborated in an updated cohort of 268 additional combined procedures.7 Stokes and Williams9 independently reached the same conclusion in a single surgeon, private practice experience. Most recently, Saad et al analyzed a California ambulatory surgery database and found similar complication rates following an abdominoplasty with or without breast surgery.10
These benchmark studies have guided our approach to combined procedures for years. Nonetheless, even their results are limited by sample size and single-center perspectives. The Tracking Operations and Outcomes for Plastic Surgeons (TOPS) database was established to collect high powered, multi-center samples in order to assess surgical trends and outcomes relevant to the plastic surgery community.11 Using the TOPS registry, this study is the largest to date aiming to assess the safety of combined abdominal surgery, including abdominoplasty and/or panniculectomy, with cosmetic breast surgery, augmentation mammaplasty and/or mastopexy, and to develop a simple pretreatment risk stratification method for patients who desire a combined procedure.
METHODS
Data Acquisition and Patient Selection
The TOPS registry has tracked patient demographics and 30-day outcomes in plastic surgery since 2002 and currently contains over one million plastic surgery procedures logged by 684 plastic surgeons across the Unites States. TOPS utilizes an electronic data capture interface through which surgeons may voluntarily report patient/procedural data and surgical outcomes.12 This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The TOPS registry was queried in May 2014 for patients undergoing one or more cosmetic procedures without any concurrent surgical reconstruction since 2002. All patients with a male or missing gender, as well as those without a valid case-id were eliminated. The “Procedure Description” variable was queried for all patients undergoing at least one of the following: mastopexy, augmentation mammaplasty, abdominoplasty, and panniculectomy. Duplicate cases were eliminated based on case-id.
Pretreatment Variables and Outcomes
Pretreatment variables collected by the TOPS registry included age, body mass index (BMI), active or former smoking, diabetes, inpatient/outpatient status, American Society of Anesthesiologists (ASA) class, race, and the presence of additional surgical procedures.
The primary outcome of interest was the presence of any complication within 30-days of the surgical procedure. Complications included mortality, readmission, return to operating room or emergency room, medical complications, and surgical complications. Medical complications included cardiac arrest, myocardial infarction, coma, peripheral nerve injury, stroke, ventilator use greater than 48 hours, pneumonia, unplanned intubation, sepsis, septic shock, systemic inflammatory response syndrome, acute renal insufficiency, progressive renal insufficiency, urinary tract infection, deep vein thrombosis, and pulmonary embolism. Surgical complications included seroma, hematoma, superficial or deep wound disruption, superficial incisional, deep incisional, or organ/space surgical site infection, posttreatment IV or PO antibiotic use, total or partial flap loss, implant/prosthesis loss, and blood loss requiring greater than 4 units of blood transfusion.
Statistical Analysis
Descriptive statistics were calculated for the study populations using Pearson's χ2 or Fisher's exact tests for categorical variables and Student's t-tests for continuous variables. A multiple logistic regression model was developed in order to control for the influence of potential confounding variables on the relationship between combined procedures and 30-day complication rates.
Multiple logistic regression among patients undergoing a combined procedure resulted in adjusted odds ratios for the development of any 30-day complication. All available pretreatment variables were included in this model with the exception of additional procedures due to its non-specific definition. Continuous variables were converted to binary form in order to simplify risk stratification. The BMI was divided based on the World Health Organization's cutoff for obesity13 and age via recursive partitioning. Adjusted odds ratios were converted to weighted risk coefficients, and the sum of these coefficients (maximum 7 points) defined a risk score. Patients undergoing a combined procedure with complete demographic data were stratified based on the risk score into low (0 points), medium (1 to 3 points), or high (4 to 7 points) risk.
RESULTS
Patient Demographics
A total of 58,756 females who underwent cosmetic breast and/or abdominal surgery were identified in the TOPS registry. Of these, there were a total of 44,623 aesthetic breast procedures, 10,440 abdominal procedures, and 3693 combined aesthetic breast and abdominal procedures. In general, the abdominal surgery cohort had a greater comorbidity burden than the aesthetic breast cohort, while the combined procedures cohort fell in the range between. Table 1 shows a complete record of patient demographic and clinical characteristics. On average, patients undergoing combined surgery were 40.05 years of age with a BMI of 25.54 kg/m2, while those undergoing only breast procedures tended to be younger (36.85 years, P < .001) and thinner (23.19 kg/m2, P < .001), and those undergoing only abdominal procedures were older (43.25 years, P < .001) and heavier (26.9654 kg/m2, P < .001). Furthermore, aesthetic breast cases underwent fewer concurrent procedures (35.81% vs 68.56%, P < .001), while abdominal procedures did not significantly differ.
Table 1.
Patient Demographics in Females Undergoing Breast and/or Abdominal Procedures
| Combined Procedures | Breast |
Abdomen |
|||
|---|---|---|---|---|---|
| (n = 3693) | (n = 44,623) | P-value | (n = .440) | P-value | |
| Age, years | 40.05 ± 9.24 | 36.85 ± 12.02 | < .001 | 43.25 ± 9.24 | < .001 |
| Body mass index (BMI), kg/m2 | 25.54 ± 4.19 | 23.19 ± 4.25 | < .001 | 26.96 ± 5.13 | < .001 |
| Diabetes | 1.62% | 0.85% | < .001 | 2.25% | .051 |
| Smoking | < .001 | < .001 | |||
| Never Smoker | 83.54% | 82.07% | 85.66% | ||
| Former Smoker | 8.68% | 6.71% | 8.80% | ||
| Current Smoker | 7.78% | 11.23% | 5.54% | ||
| Outpatient Procedure | 93.13% | 97.78% | < .001 | 90.94% | < .001 |
| ASA class 3 or 4 | 0.73% | 0.84% | .540 | 1.78% | < .001 |
| Race | < .001 | < .001 | |||
| White | 76.36% | 79.58% | 68.86% | ||
| Black of African-American | 3.09% | 2.86% | 6.01% | ||
| Asian | 1.46% | 2.37% | 1.74% | ||
| Hispanic or Latino | 9.04% | 7.28% | 11.16% | ||
| Other/Unknown | 10.05% | 7.91% | 12.23% | ||
| Additional Procedures | 68.56% | 35.81% | < .001 | 65.37% | .597 |
Unadjusted Outcomes
A total of 2770 patients (4.7%) experienced at least one posttreatment complication. A complete record of complication rates is shown in Table 2. Of the 3693 patients who underwent a combined aesthetic breast and abdominal procedure, 9.40% experienced an adverse event within 30 days. Importantly, this rate did not significantly differ from those undergoing only abdominal surgery (9.75%, P = .530) but was significantly higher than those who underwent only aesthetic breast surgery (2.66%, P < .001). Furthermore, when compared to breast procedure alone, combined procedures had significantly higher rates of readmission (0.79% vs 0.19%, P < .001), emergency room visits (0.41% versus 0.14%, P < .001) and return to the operating room (1.33% versus 0.87%, P = .006). Incidence of mortality was extremely rare and did not differ significantly across cohorts.
Table 2.
Complication Rates in Females Undergoing Breast and/or Abdominal Procedures
| Combined Procedures | Breast |
Abdomen |
|||
|---|---|---|---|---|---|
| (n = 3693) | (n = 44,623) | P-value | (n = 10,440) | P-value | |
| Mortality | 0.00% | 0.01% | 1.000 | 0.07% | .201 |
| Any Complication | 9.91% | 3.01% | < .001 | 10.14% | .686 |
| Medical Complication | |||||
| Cardiac Arrest requiring CPR | 0.00% | 0.01% | 1.000 | 0.00% | 1.000 |
| Myocardial Infarction | 0.00% | 0.00% | 1.000 | 0.00% | – |
| Coma > 24 hours | 0.00% | 0.00% | – | 0.01% | 1.000 |
| Peripheral Nerve Injury | 0.00% | 0.00% | – | 0.00% | |
| Stroke | 0.00% | 0.00% | – | 0.01% | 1.000 |
| On ventilator > 48 hrs | 0.00% | 0.00% | – | 0.01% | 1.000 |
| Pneumonia | 0.00% | 0.01% | 1.000 | 0.07% | .201 |
| Unplanned intubation | 0.00% | 0.00% | – | 0.03% | .572 |
| Sepsis | 0.00% | 0.00% | – | 0.00% | – |
| Septic Shock | 0.00% | 0.00% | – | 0.00% | – |
| Systemic Inflammatory Response Syndrome (SIRS) | 0.00% | 0.01% | 1.000 | 0.00% | – |
| Acute Renal Insufficiency | 0.00% | 0.00% | – | 0.01% | 1.000 |
| Progressive Renal Insufficiency | 0.00% | 0.00% | – | 0.00% | – |
| Urinary Tract Infection | 0.03% | 0.01% | .214 | 0.02% | 1.000 |
| Deep Vein Thrombosis | 0.22% | 0.01% | < .001 | 0.16% | .504 |
| Pulmonary Embolism | 0.08% | 0.01% | .019 | 0.30% | .019 |
| Surgical Complications | |||||
| Seroma | 2.84% | 0.26% | < .001 | 3.59% | .031 |
| Hematoma | 1.22% | 0.86% | .028 | 0.72% | .003 |
| Wound Disruption Superficial | 2.55% | 0.68% | < .001 | 2.32% | .436 |
| Wound Disruption Deep/Fascia | 0.32% | 0.11% | < .001 | 0.47% | .250 |
| Superficial Incisional Surgical Site Infection | 0.73% | 0.22% | < .001 | 0.79% | .746 |
| Deep Incisional Surgical Site Infection | 0.41% | 0.14% | < .001 | 0.55% | .305 |
| Organ/Space Surgical Site Infection | 0.03% | 0.01% | .429 | 0.02% | 1.000 |
| Infection Requiring Intravenous Antibiotics | 0.38% | 0.15% | .001 | 0.42% | .729 |
| Infection Requiring Oral Antibiotics | 2.41% | 0.70% | < .001 | 2.63% | .460 |
| Total Flap Loss (>90%) | 0.00% | 0.01% | 1.000 | 0.01% | 1.000 |
| Partial Flap Loss (10% - 90%) | 0.08% | 0.07% | .749 | 0.18% | .229 |
| Implant/Prosthesis Loss | 0.08% | 0.21% | .122 | – | – |
| Transfusion, > 4 U RBC | 0.00% | 0.00% | – | 0.01% | 1.000 |
| Return to Emergency Room | 0.41% | 0.14% | < .001 | 0.57% | .226 |
| Readmission | 0.79% | 0.19% | < .001 | 0.88% | .586 |
| Return to Operating Room | 1.33% | 0.87% | .006 | 1.01% | .106 |
Table 3 stratifies total complication rates between different aesthetic breast or abdominal procedures alone and combined with one another. Across all three breast procedure and both abdominoplasty and panniculectomy, the risk for a 30-day complication did not significantly vary when combined with abdominal surgery (Table 3).
Table 3.
Total Complication Rates Stratified by Breast or Abdominal Procedure
| Breast or Abdominal Procedure Alone | Combined Procedurea | |
|---|---|---|
| Augmentation | 2.14% (N = 34,164) | 8.29% (N = 1629) |
| Mastopexy | 4.55% (N = 5849) | 10.89% (N = 1331) |
| Augmentation-Mastopexy | 3.90% (N = 4610) | 9.14% (N = 733) |
| Abdominoplasty | 9.80 (N = 2367) | 9.73% (N = 2487) |
| Panniculectomy | 9.59% (N = 8073) | 8.71% (N = 1206) |
aχ2-test P value for the column is not significant (P = .054 for breast procedures and P = .317).
Adjusted Outcomes
After adjusting for patient comorbidities and additional procedures using multivariate logistic regression modeling, breast surgery alone was associated with lower complication rates than combined procedures (OR 0.31, 95% confidence interval [CI] 0.27-0.36, P < .001). In contrast, abdominal surgery alone did not differ significantly from combined abdominal and breast procedures (OR 0.87, 95% CI 0.75-1.01, P = .076). The full review of the adjusted odds ratios from the multiple logistic regression models is available in Table 4.
Table 4.
Adjusted Odds Ratios for the Development of any 30-day Complication
| Variable | OR | 95% Confidence Interval |
P-value | |
|---|---|---|---|---|
| Combined Procedure | Reference | |||
| Abdomen | 0.87 | 0.75 | 1.01 | .076 |
| Breast | 0.31 | 0.27 | 0.36 | < .001 |
| Active Smoking | 1.56 | 1.35 | 1.81 | < .001 |
| Diabetes | 1.27 | 0.94 | 1.73 | .123 |
| ASA 3 or 4 | 1.77 | 1.31 | 2.38 | < .001 |
| BMI | 1.08 | 1.07 | 1.09 | < .001 |
| Age | 1.01 | 1.01 | 1.02 | < .001 |
| Outpatient | 0.67 | 0.56 | 0.81 | < .001 |
| Additional Procedure | 1.29 | 1.17 | 1.43 | < .001 |
Risk Stratification
Pretreatment risk factors for complication within the combined procedure cohort were converted into weighted risk coefficients based on the magnitude of their adjusted odds ratios: current smoker (0); age over 53 (1); diabetes (1); body mass index (2); and ASA 3 or 4 (3). (Table 5) Although smoking significantly increased the risk for complication within the overall cohort (Table 4), within the smaller combined procedures cohort the adjusted odds ratio (OR = .98) did not confer a clinically significant increase on risk likely because of low prevalence and significant overlap with other variables, and was assigned a weight of 0. Nearly 77% of patients undergoing a combined procedure were classified as low-risk (0 points), and only 0.5% high-risk (4 to 7 points). Table 6 breaks down the classification of all patients into risk categories. Low, medium and high-risk patients undergoing a combined procedure demonstrated complication rates of 9.78%, 16.63%, and 38.46%, respectively (Figure 1). The risk of a combined procedure is not significantly different than that of an abdominoplasty in the low and medium-risk cohorts (P > .05). There is a non-significant trend towards increased complications with a combined procedure compared to abdominal procedures in the high-risk cohort, however this sub-group is poorly powered (β = .775) to detect a significant difference.
Table 5.
Risk Factors Among Patients With Combined Procedures and Coefficients Used to Risk Stratify Patients
| Risk Factor | Adjusted Odds Ratio | Weighted Coefficient |
|---|---|---|
| Active Smoking | 1.08 | Not Assigned |
| Age over 53 | 1.39 | 1 |
| Diabetes | 1.53 | 1 |
| BMI ≥30 | 2.04 | 2 |
| ASA class 3 or 4 | 2.37 | 3 |
Table 6.
Complication Rates Across Risk Categories
| Sample size, n (%a) | Complication, % | P-value | |
|---|---|---|---|
| Low Risk (0 points) | |||
| Abdomen | 3981 (62.75%) | 9.44% | .924 |
| Breast | 27,502 (84.69%) | 2.28% | < .001 |
| Combined | 1911 (76.96%) | 9.37% | Reference |
| Medium Risk (1-3 points) | |||
| Abdomen | 2233 (35.20%) | 13.61% | .235 |
| Breast | 4746 (14.61%) | 5.60% | < .001 |
| Combined | 559 (22.51%) | 15.56% | Reference |
| High Risk (4-7 points) | |||
| Abdomen | 130 (2.05%) | 23.07% | .307 |
| Breast | 227 (0.70%) | 15.42% | .046 |
| Combined | 13 (0.53%) | 38.46% | Reference |
aRefers to the percentage of each procedure within a given risk category, ie, the percentage of all breast procedures that are classified as low, medium, or high-risk.
Figure 1.
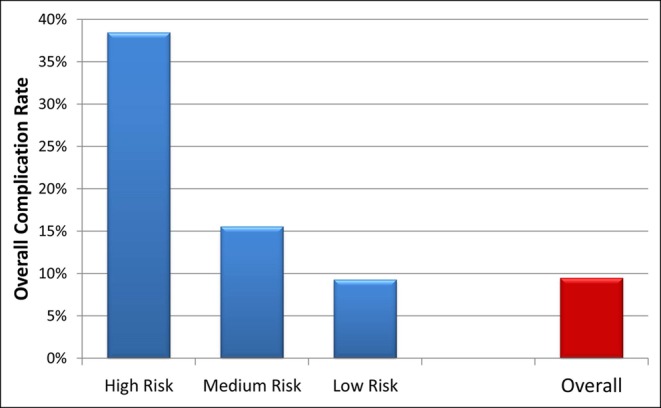
Complication rates among low, medium, and high-risk patients undergoing combined breast and abdominal procedures. The complication rates are 9.78%, 16.63%, and 38.46% for low, medium, and high-risk procedures, respectively. The overall complication rate for combined procedures is 9.91%.
DISCUSSION
This retrospective review of 58,756 patients, including 3693 combined procedures, is the largest to date assessing the safety of combining aesthetic breast procedures with abdominal surgery. On the whole, our complication rates are lower than those previously reported for abdominal procedures alone or combined procedures.7,8,14-16 Although this may be at least in part due to TOPS's voluntary data reporting, this discrepancy can be accounted for by the 30-day nature of TOPS outcomes data, as our results are similar to those found using other national, 30-day registries.17-19 A similar trend was noted in mastopexies and augmentation mammaplasties.12,20,21
Importantly, like previous studies of combined breast and abdominal procedures, we found no significant difference in complication rates between abdominal surgery and combined procedures.7-10 To our knowledge, however, this is the first study to also compare combined breast and abdominal procedures to aesthetic breast surgery alone.
Our results demonstrate a nearly 4-fold increase in 30-day complications with combined procedures when compared to breast surgery alone, (Table 2) regardless of the particular breast or abdominal procedure (Table 3). This difference in complication rates can be explained by both inherent procedural and demographic differences between the cohorts. It has been hypothesized that the presence of large, poorly adhering surfaces following abdominoplasty as well as the disruption of local lymphatic structures provide a potential space and shearing force that drive elevated rates of seroma formation.22 Combined with the unique distribution of wound tension and quite simply a larger wound, it is not surprising that abdominal procedures had greater complication rates than aesthetic breast surgery.23,24 Furthermore, compared to the breast surgery cohort, patients undergoing an abdominal procedure on average had more comorbidities, with the exception of active smoking, and underwent more concurrent surgical procedures (Table 1). Even after controlling for this difference in demographic variables, the trend in complication rates remained the same – abdominal procedures are inherently more prone to 30-day complications than cosmetic breast surgery (Table 4).
The question is—does combining aesthetic breast surgery with abdominal procedures result in multiplicative or additive risk? Compared to abdominal surgery alone, a combined procedure does not confer any increased risk. Compared to an augmentation mammaplasty and/or mastopexy alone, concomitant abdominal surgery increases the risk for complications, but only inasmuch as patients assume the inherently greater risk associated with an abdominal procedure instead. The calculated 30-day risk of one or more complications associated with undergoing both procedures independently would be 12.15% [P = 1 – (1–.0975)(1–.0266)]. These results provide further evidence for the safety of combining abdominal procedures, including abdominoplasty and panniculectomy, with aesthetic breast surgery.
The benefits of a combined procedure may not necessarily apply to every patient. Unfortunately, no study to date has promulgated guidelines as to when it may be beneficial and/or appropriate to combine aesthetic breast surgery with an abdominal procedure. Nonetheless, within our series, those patients undergoing a combined surgery were younger and had on average fewer comorbidities than their abdominal surgery counterparts, (Table 1) suggesting an intuitive predilection among plastic surgeons for selecting a healthier subset of patients as candidates for a combined procedure.
We developed the first easy-to-use risk stratification tool for patients undergoing combined abdominal and aesthetic breast surgery by examining the adjusted effect of 5 commonly measured pretreatment variables on the incidence of 30-day complications. Many of the pretreatment variables identified in this study to increase the risk of complication, including ASA class, age, BMI and diabetes, have been previously described as risk factors across a broad range of outcomes and surgical procedures.17,18,25,26 Impressively, over 75% of the combined procedures within our cohort were classified into the low-risk category, and only less than 1% high-risk, (Table 6) again a testament to the prudent decision-making among plastic surgeons with regards to this elective procedure.
Overall, the incidence of a 30-day complication among combined procedures rapidly increased from 9.78% in low-risk patients to 16.63% and over 38% in medium and high-risk patients, respectively (Figure 1). Low and medium-risk patients enjoyed similar complication rates with a combined or abdominal procedure, whereas high-risk patients experienced a nearly 150% increase in complications undergoing a combined procedure (Table 6). For the low-risk patient, the benefits of a combined procedure appear to outweigh the drawbacks, sparing the patient a second surgery without increasing morbidity. For the high-risk patient, however, the danger of complication very quickly becomes prohibitive. Although the 38.5% risk of a combined procedure is similar to the 34.9% risk calculated for two independent surgeries, both of these are prohibitively high for an elective procedure. For this small cohort we would advise against surgery altogether; at the least it would be prudent to minimize the risk for complications by deciding with the patient on the single most important procedure towards achieving her goal, and proceeding cautiously with either breast or abdominal surgery alone. The medium-risk patient again requires a careful discussion regarding her goals. Breast surgery alone carries a significantly deceased complication rate, and may perhaps be more safely combined with liposuction or other alternatives to abdominal surgery. However, when the inherently elevated risk of an abdominal procedure cannot be avoided, breast surgery may be performed concurrently without a significantly increased risk of complication, precluding the need for a second operation.
This study is not without its limitations, at least in part stemming from TOPS data collection methodologies. As we have alluded to before, TOPS captures complications for only 30-days posttreatment, likely underestimating the true total complication rate. This is particularly true for long-term breast complications including implant-related infections and/or implant loss and capsular contracture. Although the presence of additional surgical procedures is tracked in TOPS, the specific nature of the procedures is not necessarily clear. Concomitant liposuction would explain the trend towards increased procedures within the abdominal and combined cohorts; however, more data is required to test properly this hypothesis. Furthermore, at this time TOPS does not widely capture cosmetic outcomes or patient satisfaction. Despite the large volume of cases included in this analysis, the data was collected over 13 years from 2002 to 2014 and represents a relatively small proportion of all breast and abdominal procedures over this time period. There is also concern that the self-reported nature of TOPS may result in under-reporting of complication and bias our results; however, many of TOPS's 30-day complication rates have been previously shown to be similar to those reported by other studies using national registries.17,18,20 When compared to the validated National Surgical Quality Improvement Program (NSQIP) registry, TOPS has been shown to effectively capture outcomes, including those specifically relevant to plastic surgeons, in a broader patient population that includes both private and academic practices.19 Finally, while our risk stratification tool effectively identified at risk patients within the TOPS database, its utility in clinical practice must ultimately be judged externally with a prospective cohort of patients.
CONCLUSION
As the demand for both abdominal procedures and cosmetic breast surgery continues to increase, a combined procedure presents a convenient and relatively cost-effective approach for accomplishing both. This retrospective review comparing the safety of such combined and individual surgeries is the largest to date and the first to include patients from multiple private and academic practices across the country. Our results add to the growing evidence supporting the safety of a combined procedure, particularly in a carefully selected patient population. Using a simple risk stratification tool to identify low and medium-risk patients based on diabetes, age, BMI, and ASA status, we can continue to ensure favorable outcomes for women who may desire a combined surgery.
Disclosures
Dr Kim receives research funding from and is on the advisory board for the Musculoskeletal Transplant Foundation. Mr Hume and Mr Simmons are employed by the American Society of Plastic Surgeons (ASPS), who developed the registry database utilized in this article, and Dr Murphy is the current president of the ASPS. The other authors have nothing to disclose.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Supplementary Material
REFERENCES
- 1. Cosmetic Surgery National Data Bank: Statistics 2013. Aesthet Surg J. 2014;34(1 suppl):1S-22S. [DOI] [PubMed] [Google Scholar]
- 2. Dillerud E. Abdominoplasty combined with suction lipoplasty: a study of complications, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990;255:333-338; discussion 339-343. [DOI] [PubMed] [Google Scholar]
- 3. Hester TR, Jr., Baird W, Bostwick J, 3rd, Nahai F, Cukic J. Abdominoplasty combined with other major surgical procedures: safe or sorry? Plast Reconstr Surg. 1989;836:997-1004. [DOI] [PubMed] [Google Scholar]
- 4. Savage RC. Abdominoplasty combined with other surgical procedures. Plast Reconstr Surg. 1982;704:437-443. [DOI] [PubMed] [Google Scholar]
- 5. Stevens WG, Cohen R, Vath SD, Stoker DA, Hirsch EM. Does lipoplasty really add morbidity to abdominoplasty? Revisiting the controversy with a series of 406 cases. Aesthet Surg J. 2005;254:353-358. [DOI] [PubMed] [Google Scholar]
- 6. Stevens WG, Vath SD, Stoker DA. "Extreme" cosmetic surgery: a retrospective study of morbidity in patients undergoing combined procedures. Aesthet Surg J. 2004;244:314-318. [DOI] [PubMed] [Google Scholar]
- 7. Stevens WG, Repta R, Pacella SJ, et al. Safe and consistent outcomes of successfully combining breast surgery and abdominoplasty: an update. Aesthet Surg J. 2009;292:129-134. [DOI] [PubMed] [Google Scholar]
- 8. Stevens WG, Cohen R, Vath SD, Stoker DA, Hirsch EM. Is it safe to combine abdominoplasty with elective breast surgery? A review of 151 consecutive cases. Plast Reconstr Surg. 2006;1181:207-212; discussion 213-204. [DOI] [PubMed] [Google Scholar]
- 9. Stokes RB, Williams S. Does concomitant breast surgery add morbidity to abdominoplasty? Aesthet Surg J. 2007;276:612-615. [DOI] [PubMed] [Google Scholar]
- 10. Saad AN, Parina R, Chang D, Gosman AA. Risk of adverse outcomes when plastic surgery procedures are combined. Plast Reconstr Surg. 2014;1346:1415-1422. [DOI] [PubMed] [Google Scholar]
- 11. Hume KM, Crotty CA, Simmons CJ, Neumeister MW, Chung KC. Medical specialty society-sponsored data registries: opportunities in plastic surgery. Plast Reconstr Surg. 2013;1321:159e-167e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alderman AK, Collins ED, Streu R, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;1246:2127-2133. [DOI] [PubMed] [Google Scholar]
- 13. Organization WH. Fact sheet N311: Obesity and overweight. 2015; http://www.who.int/mediacentre/factsheets/fs311/en/ Accessed March 4, 2015.
- 14. Simon S, Thaller SR, Nathan N. Abdominoplasty combined with additional surgery: a safety issue. Aesthet Surg J. 2006;264:413-416. [DOI] [PubMed] [Google Scholar]
- 15. Staalesen T, Elander A, Strandell A, Bergh C. A systematic review of outcomes of abdominoplasty. J Plast Surg Hand Surg. 2012;46(3-4):139-144. [DOI] [PubMed] [Google Scholar]
- 16. Neaman KC, Armstrong SD, Baca ME, Albert M, Vander Woude DL, Renucci JD. Outcomes of traditional cosmetic abdominoplasty in a community setting: a retrospective analysis of 1008 patients. Plast Reconstr Surg. 2013;1313:403e-410e. [DOI] [PubMed] [Google Scholar]
- 17. Mioton LM, Buck DW, 2nd, Gart MS, Hanwright PJ, Wang E, Kim JY. A multivariate regression analysis of panniculectomy outcomes: does plastic surgery training matter? Plast Reconstr Surg. 2013;1314:604e-612e. [DOI] [PubMed] [Google Scholar]
- 18. Mioton LM, Alghoul MS, Kim JY. A comparative analysis of readmission rates after outpatient cosmetic surgery. Aesthet Surg J. 2014;342:317-323. [DOI] [PubMed] [Google Scholar]
- 19. Khavanin N, Gutowski KA, Hume KM, et al. The use of patient registries in breast surgery: a comparison of the tracking operations and outcomes for plastic surgeons and national surgical quality improvement program data sets. Ann Plast Surg. 2015;742:157-162. [DOI] [PubMed] [Google Scholar]
- 20. Hanwright PJ, Hirsch EM, Seth AK, et al. A multi-institutional perspective of complication rates for elective nonreconstructive breast surgery: an analysis of NSQIP data from 2006 to 2010. Aesthet Surg J. 2013;333:378-386. [DOI] [PubMed] [Google Scholar]
- 21. Khavanin N, Jordan SW, Rambachan A, Kim JYS. A systematic review of single-stage augmentation-mastopexy. Plast Reconstr Surg. 2014;1345:922-931. [DOI] [PubMed] [Google Scholar]
- 22. Rangaswamy M. Minimising complications in abdominoplasty: An approach based on the root cause analysis and focused preventive steps. Indian J Plast Surg. 2013;462:365-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Khan S, Teotia SS, Mullis WF, et al. Do progressive tension sutures really decrease complications in abdominoplasty? Ann Plast Surg. 2006;561:14-20; discussion 20-11. [DOI] [PubMed] [Google Scholar]
- 24. Pollock H, Pollock T. Reducing abdominoplasty complications. Aesthet Surg J. 2002;225:475-476. [DOI] [PubMed] [Google Scholar]
- 25. Kim JY, Khavanin N, Jordan SW, et al. Individualized Risk of Surgical Site Infection: An application of the Breast Reconstruction Risk Assessment (BRA) Score. Plast Reconstr Surg. 2014;1343:351e-362e. [DOI] [PubMed] [Google Scholar]
- 26. Mlodinow AS, Fine NA, Khavanin N, Kim JY. Risk factors for mastectomy flap necrosis following immediate tissue expander breast reconstruction. J Plast Surg Hand Surg. 2014;485:322-326. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


