Abstract
Background: The service needs of people with human immunodeficiency virus (HIV) in low-income settings are wide-ranging. Service provision in a community is often disjointed among a variety of providers. We sought to reduce unmet patient needs by increasing referral coordination for HIV and family planning, measured as network density, with an organizational network approach.
Methods: We conducted organizational network analysis on two networks in sub-cities of Addis Ababa, Ethiopia. There were 25 organizations in one sub-city network and 26 in the other. In one of them we sought to increase referrals through three network strengthening meetings. We then conducted the network analysis again in both sub-cities to measure any changes since baseline. We also quantitatively measured reported client service needs in both sub-cities before and after the intervention with two cross-sectional samples of face-to-face interviews with clients (459 at baseline and 587 at follow-up).
Results: In the sub-city with the intervention, the number of referral connections between organizations, measured as network density, increased 55%. In the control community, the density decreased over the same period. Reported unmet client service needs declined more consistently across services in the intervention community.
Discussion: This quasi experiment demonstrated that (1) an organizational network analysis can inform an intervention, (2) a modest network strengthening intervention can enhance client referrals in the network, (3) improvement in client referrals was accompanied by a decrease in atient-reported unmet needs and (4) a series of network analyses can be a useful evaluation tool.
Keywords: Family planning, global health, HIV/AIDS, integration, network analysis, quasi-experiment
Key Messages
Services for people living with human immunodeficiency virus/acquired immune deficiency syndrome in low- to middle-income countries are poorly coordinated or integrated.
An organizational network analysis provides useful information to guide a network strengthening intervention.
A modest and affordable intervention can enhance client referrals in the network, and reduce client unmet needs.
Introduction
Urban communities in developing countries host a wide array of services for their lower income residents. They address health, housing, education, income generation and much more. In many instances, services are most effective when received in combination with other services for related needs. The importance of service integration and coordination are highlighted in several of the US Government’s Global Health Initiative (GHI) principles (US Global Health Initiative); and are among the recommendations in the US Institute of Medicine evaluation of the President’s Emergency Program for AIDS Relief ( IOM 2013 ).
The call for integration is not a new one. There has long been recognition of siloed funding and uncoordinated service delivery ( Spicer et al. 2010 ). Lack of coordination between service providers creates inefficiencies that lessen impact and increase costs. It is important to realize as many benefits as possible from deployed resources before deploying more. Ensuring that organizations and programs already in place coordinate their efforts is an important step towards this end. Studies have demonstrated that implementation of integrated health services is feasible across contexts, populations and interventions ( Lindegren et al. 2012 ). Integrated human immunodeficiency virus (HIV) and family planning services improve quality of care, increases uptake of services and results in positive effects on outcomes such as contraceptive use and pregnancy incidence, although there are few evaluations of scalable strategies ( Wilcher et al. 2013 ).
The primary recommended means of integration are a broadened array of services offered by a provider, creating ‘one stop shopping’ for clients, and better systems of referral for services needed but not provided by a particular provider. ‘One stop’ opportunities are convenient when the services under consideration are narrowly circumscribed, as with clinical services for example. But the needs of people with HIV are not narrowly circumscribed. They are instead vast, including housing, mental health, family counselling, income opportunities, civil rights and more. The instances in which all relevant services can be housed under one roof are rare. More commonly, each provider needs to refer clients to other providers for additional services.
Numerous efforts have been made to improve client referrals, including mechanisms (e.g. referral notes, escorted referral; Baumgartner et al. 2013 ), and gathering organization representatives to work together towards improved collaboration ( Provan et al. 2003 ). The importance of evaluating efforts to strengthen interactions between organizations has been recognized but rarely implemented ( Provan and Milward 2001 ; Provan et al. 2005 ).
We identified and described networks of organizations providing services for HIV care or family planning in two of Addis Ababa’s 10 sub-cities. In one of them, we conducted an intervention to strengthen the network, leaving the other untouched. In Valente’s classification of three types of network interventions (segmentation, induction and alteration), enhancing network referrals is an alteration in which links are added ( Valente 2012 ). We followed the intervention with a second network assessment to see how the two networks had changed. Our objectives were to see (1) if an organizational network analysis (ONA) could inform an intervention, (2) if a modest network development intervention could enhance client referrals in the network, as measured by network density, (3) if changes in network referral density would be reflected in a decrease of patient-reported unmet needs and (4) if a follow-up network analysis would be a useful evaluation tool.
Materials and methods
Identification of networks
As described elsewhere( Valente 2012 ), the two sub-cities of Addis Ababa, Kirkos and Kolfe Keranyo, were selected because they were similar in demographic composition yet not contiguous. We identified all organizations that provided HIV care and support and/or family planning services to women living with HIV between the ages 18 and 49 living in one of the two sub-cities. The sub-cities had nearly identical numbers of organizations in their networks (25 and 26, respectively). The selection of Kirkos as the intervention community was based on information from the baseline network analysis that showed Kirkos as having a lower referral density, or number of actual inter-organizational connections as a proportion of all possible connections (Kirkos = 0.115, Kolfe Keranyo = 0.155), thus having more room for improvement. In addition, compared with the network in Kolfe Keranyo, the Kirkos network was less centralized around one organization (centralization scores of 0.192 and 0.525, respectively). With higher centralization, the success or failure of the intervention could depend too heavily on one organization.
Kolfe Keranyo served as the control sub-city in this quasi experiment. The organizations in Kolfe Keranyo were not informed that we would be implementing a network strengthening intervention in Kirkos. However, representatives from organizations in Kolfe Keranyo had participated in a meeting in which the baseline descriptions of both sub-city networks were presented.
Network strengthening
We chose a modest, low dose intervention over an expensive, high dose one so that, if shown effective, replication would be more affordable and likely. The intervention consisted of three 2-day meetings attended by representatives of the organizations providing HIV or family planning services in Kirkos sub-city. The meetings were spaced ∼2 months apart; with three occurring between March and July 2012. To carry out the meetings we worked in collaboration with FHI 360 in Addis Ababa. The meeting content was conceived by one of the co-authors (X.A.), and adapted from organizational development materials developed by Management Sciences for Health. The content was delivered in collaboration with FHI 360 by local coaches with training in organizational development. Amharic was the principal language in the meetings, with translation between English and Amharic done by the Ethiopian facilitators and a designated translator.
At the beginning of the first meeting, we reviewed the network results, including a ‘gap analysis’ showing each organization the HIV or family planning services they reported providing, the organizations they had referred to, and the organizations they had not referred to but could in the future. HIV services considered were 13 in number, ranging from testing and treatment to nutritional and social support services. The participants were also given a directory of the organizations in their sub-city, with contact information and which HIV or family planning services were offered. After considering the benefits of and challenges to client referral, the participants were guided through a visioning and performance improvement process in which they selected for themselves a 6-month goal. They chose to increase the referrals by 50%, as measured by the number of organizations linked by referrals across the network. In the case of Kirkos, this would be an increase in network density from 0.115 to 0.173. They were then led through a process of deciding how to achieve the goal. In subsequent meetings, we administered a brief questionnaire, asking participants whether a referral to a new organization had occurred since the previous meeting, what steps had been taken to increase referrals, and what barriers to referral they had encountered. They then engaged in planning for the next 2-month period.
Apart from personnel, the meeting costs included rental of a hotel meeting room, tea served twice a day, lunch and 50 Ethiopian Birr (just under US$3.00) for participant travel to and from the meeting.
Each of our meetings built off of the previous ones, so consistent attendance by the same people was important. To facilitate this, a letter describing the project and the importance of consistent attendance was delivered to the director of each organization several weeks before the first meeting. At the first meeting, we asked for the cell phone numbers of the participants. For the second and third meetings, we sent them a text message several days in advance of the meeting to confirm the date and location.
Follow-up network survey
The follow-up ONA was conducted in September 2012, 19 months after the baseline ONA, 6 months after the first intervention meeting and 2 months after the last intervention meeting. The methods for the baseline ONA have been described elsewhere ( Thomas et al. 2014 ). The same methods were used for the follow-up in both Kirkos and Kolfe Keranyo sub-cities, but we did not conduct a new enumeration of organizations. Rather, we collected data from the same organizations visited at baseline.
Baseline and follow-up client surveys
To understand how female clients perceived the provision of services by organizations in the network we interviewed two cross-sectional samples of women aged 18–49. They were the clients of a large non-governmental organization (NGO) providing home based care services for people living with HIV in Addis Ababa, including Kirkos and Kolfe Keryano sub-cities. Questions for both the baseline and follow-up surveys pertained to clients’ sociodemographic characteristics, perceived quality of care, their met or unmet HIV care and family planning needs, and some of their behaviours (such as ART adherence) and quality of life. Interview response categories were almost exclusively close-ended and were conducted by a trained interviewer. All questionnaires (including those for the organizations) were translated into Amharic and then back into English to ensure correct translation.
A desired sample size of 480 (for the two sub-cities together) was based on an assumption that one-third of all clients had an unmet need for contraception, a desire for 95% confidence interval of ± 0.046 for an unmet need proportion and an anticipated refusal rate of 20%. Clients were interviewed in April–May 2011 for the baseline and September–October 2012 for the follow-up. The baseline and follow-up samples were independent cross-sections of all clients of the NGO on the respective dates.
Ten research assistants participated in a 4-day training for this study. Topics included research ethics and pilot testing of data collection instruments. All research assistants were Ethiopian nationals and spoke fluent Amharic in addition to English. They were young professionals working health or social research. All had previous experience as data collectors.
Nurse supervisors and volunteer caregivers from the NGO were oriented to the study and hired to help with coordinating logistics for data collection with clients. We randomly sampled clients from the client list. The supervisors and volunteers then contacted them, which they already did on a regular basis for their work, and provided information about how to participate in the interview. Interviews were conducted in the offices of the NGO near the clients’ respective communities, in a room with auditory privacy. No NGO staff was present during the interviews. Clients who presented for an interview received a nominal transportation stipend of 50 Ethiopian Birr, regardless of whether they consented to the interview. All respondents were informed of the participation risks and benefits, and consented to participate.
Analyses
Two analyses were conducted: one of network density; the other of unmet client needs. Two data entry specialists entered the organizational and client data into Epidata, a data management program. The organizational data were then exported into R version 2.14.0 (Vienna, Austria) for analysis. Differences in referral densities were calculated by subtracting the baseline density from the follow-up density in each of the sub-cities. The statistical significance of changes in network density were assessed with bootstrap-assisted paired sample t-tests using UCINet software, version 6.528 ( Snijder and Borgatti 1999 ; Borgatti et al. 2002 ).
Client data were exported to STATA version 12.1 (College Station, TX) for analysis. ART non-adherence was based on the Simplified Medication Adherence Questionnaire and defined as a positive response to one or more of six questions: ‘ever forget meds’, ‘careless at times about taking meds’, ‘stop meds when feeling worse’, ‘last weekend, did not take any meds’, ‘more than 2 doses missed over the past week’ or ‘over 2 days of total non-medication during the past 3 months’ ( Knobel et al. 2002 ). Satisfaction with health care was measured based on the responses to the question ‘Do you feel that your health needs are being met?’ A dichotomous measure was created where ‘yes’ combined the responses ‘all’ and ‘most’, and ‘no’ combined ‘some’, ‘very few’ or ‘none’. Family planning use was a dichotomous measure based on clients’ response to the question ‘Are you currently using a pregnancy prevention method’.
Health service needs were documented in response to the question ‘What kinds of care and services do you feel you need but do not yet have, or are not getting sufficiently?’ Categories were pre-identified and the interviewer chose the category closest to the response. Where it was not possible for the interviewer to code the response, s/he wrote down the response verbatim and this was coded into grouped categories later in data analysis. The most common responses are reported here and include social services (e.g. household help, legal services, loans, education, small business or job opportunity or training, housing/shelter, transportation, clothes or toilet), nutrition (includes money for food, water), medical treatment (includes pain killers), ART assessment or follow-up, care for other diseases and health problems (e.g. nausea, rash, malaria, TB, mental health), counselling services and spiritual services.
Results
Network strengthening
Of the 25 organizations in Kirkos, 21 (84%) participated in at least one of the three network strengthening meetings; 12 (48%) were represented at all three. Across the three meetings there were 36 unique participants from the 21 organizations. Sixteen of those 36 (44%) participants attended all three meetings, 5 (14%) attended two and 15 (42%) attended one meeting.
In the second meeting, nine organizations present reported having made a referral since the last meeting to an organization they had not referred to before. Seven organizations reported receiving a referral from an organization they had not received referrals from before. At the third and final meeting, eight organizations reported referring to new organizations and the same eight also reported receiving referrals from new organizations.
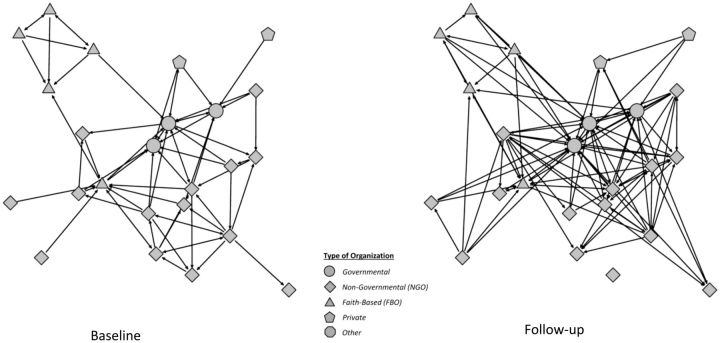
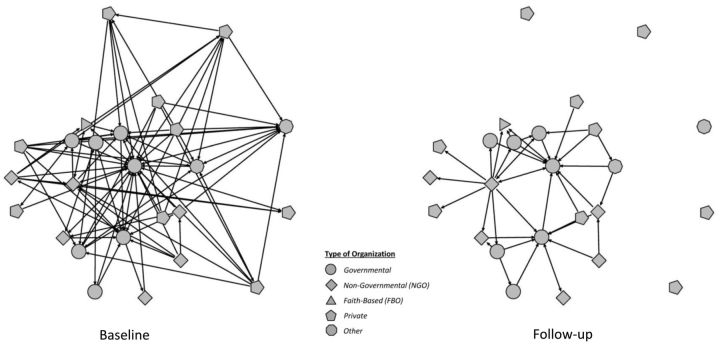
Network changes
In each of the sub-cities, there was one less organization at follow-up than at baseline ( Table 1 ). In each case, they had stopped providing the services that made them eligible for our network, and declined to participate when approached for the follow-up survey. Even so, compared with baseline, there were 32 more referral ties at follow-up between organizations in Kirkos, whereas there were 61 fewer in Kolfe Keranyo. The sociograms for each sub-city, before and after, are depicted in Figures 1 and 2 . These sizable and opposite changes are reflected in other network characteristics. The Kirkos organizations slightly surpassed their goal of a 50% increase in the referral density. In contrast, the Kolfe Keranyo network density experienced a loss of 60% of their referral ties. These changes were statistically significant in both Kirkos ( P < 0.05) and Kolfe Keranyo ( P < 0.01). At the time of follow-up, five organizations in Kolfe Keranyo reported not sending or receiving any referrals to others in the network in the previous 3 months.
Table 1.
Relational characteristics of the organizational networks at baseline (2011) and follow-up (2012) in Kirkos and Kolfe Keranyo sub-cities of Addis Ababa, Ethiopia
| Network characteristic | Kirkos (intervention) |
Kolfe Keranyo (comparison) |
||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Organizations | 25 | 24 | 26 | 25 |
| Links | 69 | 101 | 101 | 40 |
| Density | 0.115 | 0.183 | 0.155 | 0.067 |
| Centralization | 0.19 | 0.27 | 0.53 | 0.22 |
| Degree centrality | 5.52 | 8.42 | 7.77 | 3.20 |
| Reciprocity | 0.83 | 0.72 | 0.78 | 0.89 |
Figure 1.
Sociograms of client referrals in Kirkos sub-city of Addis Ababa, Ethiopia at baseline (April 2011) and follow-up (September 2012)
Figure 2.
Sociograms of client referrals in Kolfe Keranyo sub-city of Addis Ababa, Ethiopia at baseline (April 2011) and follow-up (September 2012)
Network centralization increased marginally in the Kirkos network whereas it decreased markedly in Kolfe Keranyo. At baseline, the centralization of the Kolfe Keranyo network was nearly three times that of Kirkos, but by the time of the follow-up, Kirkos’s was slightly greater than Kolfe Keranyo’s.
The number of referrals sent and received by an organization is measured by degree centrality. The Kirkos average degree centrality increased by folding in nearly three organizations over the study period, whereas in Kolfe Keranyo it decreased by losing more than four organizations ( Table 1 ). The increased reciprocity in Kolfe Keranyo indicates that as the number of referrals decreased, the remaining connections were more likely to occur between organizations referring to each other. In Kirkos, the reciprocity of referrals decreased slightly, signifying that new referrals were with organizations that did not necessarily refer clients back, as could happen when referring for specific services.
Client characteristics
In Kirkos and Kolfe Keranyo, respectively, 234 and 225 clients participated in the baseline interview; 293 and 294 participated in the follow-up interview. Of clients who were located, 96% at baseline and 98% at follow-up agreed to participate. At baseline, the two sub-city samples were similar in terms of mean age, employment and the proportion not wanting any more children ( Table 2 ). Compared with Kirkos, twice as many in Kolfe Keranyo had never attended school, and half as many had no toilet in their home. Higher proportions in Kolfe Keranyo lived with a sexual partner, had sex in the previous 6 months, and used a pregnancy prevention method. The most common methods were condoms and the injectable (results not shown). Most women in both sub-cities learned their HIV positive status over 2 years ago, were on ART, and had been on ART for over 2 years. These rates were even higher at follow-up. Just over half of those on ART were adherent at baseline in Kirkos and Kolfe Keranyo; the proportions were slightly higher in both sub-cities at follow-up. General quality of life was low, ranging between ‘poor’ and ‘neither good nor poor’ in both sub-cities at both time points.
Table 2.
Client characteristics (percent) at baseline (2011) and follow-up (2012) in Kirkos and Kolfe-Keranyo sub-cities of Addis Ababa, Ethiopia
| Characteristic | Kirkos (intervention) |
Kolfe Keranyo (comparison) |
||
|---|---|---|---|---|
| Baseline( n = 234) | Follow-up ( n = 293) | Baseline ( n = 225) | Follow-up ( n = 294) | |
| Age (mean) | 33.9 | 34.0 | 32.1 | 33.5 |
| Never attended school | 16.7 | 17.4 | 32.4 | 30.3 |
| Worked last year | 83.3 | 85.7 | 78.2 | 81.3 |
| Rent home (vs own) | 82.5 | 67.2 | 73.3 | 70.6 |
| Public/share toilet (vs private) | 80.3 | 84.0 | 41.3 | 53.7 |
| Live with sexual partner | 28.6 | 30.5 | 42.7 | 34.4 |
| Sex in last 6 months | 28.6 | 37.2 | 45.3 | 37.9 |
| Use a pregnancy prevention method | 29.9 | 34.6 | 44.6 | 31.3 |
| Don’t want more children (or undecided) | 74.4 | 84.5 | 69.6 | 83.5 |
| More than 2 years since HIV diagnosis | 88.3 | 93.9 | 84.4 | 96.6 |
| On ART | 89.7 | 91.5 | 85.3 | 87.1 |
| On ART more than 2 years a | 78.5 | 84.9 | 70.8 | 84.9 |
| ART adherent a | 54.6 | 63.8 | 59.5 | 66.1 |
| General QOL b | 2.24 | 2.01 | 2.09 | 1.95 |
a Kirkos ( n = 210) at baseline and ( n = 268) at follow-up. Kolfe ( n = 192) at baseline and ( n = 256) at follow-up.
b Measured in response to the question, ‘How would you rate your overall quality of life?’ where 1 = very poor, 2 = poor, 3 = neither good nor poor, 4 = good and 5 = very good.
Many of the respondent characteristics remained the same in the follow-up sample. Notable exceptions included a decrease in the proportion of respondents in Kirkos who rented their homes and an increase in the proportion in Kolfe Keranyo that used a public/shared toilet. Also, in Kirkos the proportion living with a sexual partner, having sex in the last 6 months and using a pregnancy prevention method increased, whereas the proportions in Kolfe Keranyo all decreased.
Unmet client needs
At baseline, sizable proportions of women reported having unmet service needs in both sub-cities ( Table 3 ). Social services were the most frequently needed, reported by nearly half of all respondents in Kirkos and one-third in Kolfe Keranyo.
Table 3.
Clients’ reports of care and needed services (percent) at baseline (2011) and follow-up (2012) in Kirkos and Kolfe-Keranyo sub-cities of Addis Ababa, Ethiopia
| Service | Kirkos (intervention) |
Kolfe-Keranyo (comparison) |
||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Difference | Baseline | Follow-up | Difference | |
| Social a | 46.6 | 27.3 | −19.3 | 33.9 | 43.5 | +9.6 |
| Counselling b | 23.1 | 4.8 | −18.3 | 15.2 | 10.3 | −4.9 |
| ART c | 22.2 | 7.5 | −14.7 | 27.8 | 12.0 | −15.8 |
| Pain d | 18.4 | 5.5 | −12.9 | 32.1 | 4.8 | −27.3 |
| Other medical e | 5.1 | 2.7 | −2.4 | 12.1 | 5.8 | −6.3 |
| Nutrition f | 29.5 | 13.7 | −15.8 | 26.3 | 17.9 | −8.5 |
| Spiritual g | 23.5 | 1.0 | −22.5 | 26.8 | 7.9 | −18.9 |
a Includes household help, legal services, loans, education, small business or job opportunity or training, housing/shelter, transportation, clothes and toilet.
b Includes counselling services, individual or group.
c Includes ART assessment or follow-up.
d Includes treatment for pain or pain killers.
e Includes care for other diseases and health problems (e.g. nausea, rash, malaria, TB and mental health).
f Includes food and nutrition advice or support, money for food and water.
g Includes spiritual services and guidance.
At follow-up, unmet social service needs in Kirkos had decreased by 40% compared with baseline, whereas in Kolfe Keranyo they had increased 26% ( Table 3 ). Unmet needs for counselling, ART, and nutrition counselling decreased in both sub-cities, but more so in Kirkos. Unmet medical needs in Kirkos decreased dramatically to the same low level experienced at baseline and follow-up in Kolfe Keranyo, the only sub-city of the two that had a hospital in its network.
Discussion
The intervention to strengthen the Kirkos inter-organizational network shows clear promise. The number of referral links and the network density increased markedly following the three meetings of organization representatives, whereas the links and density of the control community decreased over the same time. The referral density increase in Kirkos was twice that observed over a 1-year period of network strengthening among organizations addressing chronic disease outcomes in a rural Arizona community (55% vs 25%) ( Provan et al. 2003 ). However, the markedly different contexts of Ethiopia and Arizona make it difficult to compare these two.
We cannot account for the network deterioration in Kolfe Keranyo. Networks are highly dynamic, with many factors affecting connections, such as changes in personnel, funding or policies. Any changes were likely specific to that sub-city, however, because Kirkos did not have the same experience. We noted above that Kolfe Keranyo had a higher degree of centralization, which could make the whole network susceptible to changes in the central organization. The striking network deterioration in Kolfe Keranyo may reflect such an occurrence.
The association between the intervention and the network strengthening in Kirkos is highly suggestive but it is not definitive proof of a causal connection. The results suggest that the organization network approach can generate data that guide efforts to improve referrals between organizations. A stronger study design with multiple intervention and control communities would help validate the results and understand with greater precision the effect of the ONA approach on strengthened referrals. Similarly, a more representative sample of all clients served by the organization would help elucidate the effect on services received, health care needs and other outcomes such as ART adherence or contraceptive use. There is some chance that the respondents to the follow-up survey in Kirkos had been sensitized to referrals by the intervention and thus recognized more of them in their organization (i.e. detection bias); or they reported what they knew the researchers were looking for. However, our presentation of the baseline network data to both the intervention and control networks alike would mitigate the effects of such reporting biases.
Limiting the follow-up network analysis to the baseline organizations prevented us from detecting new links with organizations outside of the network. For example, organizations in Kirkos, a sub-city without a hospital, may have begun referring to the hospital in Kolfe Keranyo. In this particular instance, however, referrals in both sub-cities would have increased (one sending and the other receiving), thereby not markedly changing the differences between them. Another way that new links could have gone undetected is if a new organization were to appear in one of the sub-cities. We believe, however, that the chances of starting a new organization and making links with others in 15 months—the time between our baseline and follow-up—are relatively low.
The changes in client unmet needs in Kirkos are also suggestive but not definitive proof of a causal link with the intervention. The changes were greater and more consistently positive in the intervention community, but perceptions of need are influenced by many factors, including the addition of services within an organization (lessening the need for referral). Moreover, we had two cross-sections rather than a cohort of clients. There were a few differences in the two cross-sections (e.g. desire to have a baby), that could have been related to perceived unmet needs. We should also note that the respondents represent clientele of one NGO and they are not necessarily representative of all women living with HIV in the two sub-cities. However, this particular NGO is large and with a wide reach throughout the city. Thus, we believe that any effects of the intervention on these respondents would likely reflect changes experienced more broadly in Kirkos.
To our knowledge, this is the first quantitatively evaluated network strengthening in a developing country, and the first anywhere with a control network for comparison. Moreover, ONAs with client outcomes are rare ( Provan et al. 2003 ). This is the first known to us reporting changes in client outcomes related to HIV or family planning. The study provided us with answers to our objectives: a network analysis provides useful information to guide a network strengthening intervention; a modest and affordable intervention can enhance client referrals in the network and a follow-up network analysis is a useful evaluation tool for such an intervention. With additional applications and research, we anticipate enhancing the impact of services already deployed and improving the health of populations through greater organizational collaboration.
Acknowledgements
The authors also thank the staff and clients of Hiwot Integrated Development Association (HIDA) (formerly Hiwat HIV and AIDS Prevention, Care and Support Association [HAPCSA]). Thank you to the staff and consultants of FHI 360’s Addis Ababa office, in particular Teklu Mulugeta Badwaza, who managed and supervised data collection and entry for the follow-up.
Funding
This study was supported by the US Agency for International Development (USAID) through the MEASURE Evaluation project and cooperative agreement GHA-A-00-08-00003-00. The views expressed in this publication do not necessarily reflect the views of USAID or the US government.
Conflict of interest statement. None declared.
References
- Baumgartner JN, Green M, Weaver MA, et al. . 2013. . Integrating family planning services into HIV care and treatment clinics in Tanzania: evaluation of a facilitated referral model . Health Policy and Planning 29 : 570 – 9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti SP, Everett MG, Freeman LC . 2002. . UCINet 6 for Windows: Software for Social Network Analysis . Harvard: : Analytic Technologies; . [Google Scholar]
- IOM (Institute of Medicine) . 2013. . Evaluation of PEPFAR. Washington, DC: The National Academies Press, 431ff. http://books.nap.edu/catalog.php?record_id=18256 , accessed 11 November 2013 .
- Knobel H, Alonso J, Casado JL, et al. . 2002. . Validation of a simplified medication adherence questionnaire in a large cohort of HIV-infected patients: the GEEMA study . AIDS 16 : 605 – 13 . [DOI] [PubMed] [Google Scholar]
- Lindegren ML, Kennedy CE, Bain-Brickley D et al . 2012. . Integration of HIV/AIDS services with Maternal, Neonatal and Child Health, Nutrition, and Family Planning Services. Cochrane Database of Systematic Reviews Issue 9. Art. No.: CD010119 . [Google Scholar]
- Provan KG, Milward HB . 2001. . Do networks really work? A framework for evaluating public-sector organizational networks . Public Administration Review 61 : 414 – 23 . [Google Scholar]
- Provan KG, Nakama L, Veazie MA, et al. . 2003. . Building community capacity around chronic disease services through a collaborative interorganizational network . Health Education and Behaviour 30 : 646 – 62 . [DOI] [PubMed] [Google Scholar]
- Provan KG, Veazie MA, Staten LK . 2005. . The use of network analysis to strengthen community partnerships . Public Administration Review 65 : 603 – 13 . [Google Scholar]
- Snijder TAB, Borgatti SP . 1999. . Non-parametric standard errors and tests for network statistics . Connections 22 : 61 – 70 . [Google Scholar]
- Spicer N, Aleshkin J, Biesma R, et al. . 2010. . National and subnational HIV/AIDS coordination: Are global health initiatives closing the gap between intent and practice? Globalization and Health 6 : 3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JC, Reynolds HW, Bevc C, et al. . 2014. . Integration opportunities for HIV and family planning services in Addis Ababa, Ethiopia: an organizational network analysis . BMC Health Services Research 14 : 22 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Government . GHI Principle Paper on Integration in the Health Sector. 2012. Available online at http://www.ghi.gov/principles/docs/principlePaperIntegration.pdf , accessed 15 June 2015 .
- Valente TW . 2012. . Network interventions . Science 337 : 49 – 53 . [DOI] [PubMed] [Google Scholar]
- Wilcher R, Hoke T, Adamchak SE, Cates W, Jr . 2013. . Integration of family planning into HIV services: a synthesis of recent evidence . AIDS 27 ( Suppl 1 ): S65 – 75 . [DOI] [PubMed] [Google Scholar]