Abstract
Purpose To replicate and extend O’Mahar and colleagues’ (O'Mahar, K., Holmbeck, G. N., Jandasek, B., & Zuckerman, J. [2010]. A camp-based intervention targeting independence among individuals with spina bifida. Journal of Pediatric Psychology, 35, 848–856) findings in a new and larger sample of youth and young adults with spina bifida who participated in a modified camp-based intervention targeting independence and social skills. Moderators of intervention effectiveness and clinical significance were examined. Method In all, 119 campers aged 7–41 years participated in an intervention that included goal setting and interactive workshops. Campers and parents completed measures of campers’ goal attainment, independence, and social functioning at preintervention and postintervention; counselors reported on campers’ goal attainment daily throughout the intervention. Results Parents and campers reported improvements in campers’ goal attainment, management of health-related self-care, and independence. Although benefits were found for most campers, cognitive functioning and family income moderated some outcomes. Campers who improved most on their social goals perceived the intervention to be more effective. Conclusions Further support is provided for the effectiveness of a camp-based intervention targeting independence and social skills for individuals with spina bifida. More attention should be directed toward those with cognitive difficulties and low-income backgrounds.
Keywords: camp, independence, intervention, social functioning, spina bifida
Camp-based programs for youth and young adults with chronic health conditions have become increasingly popular in the United States (American Camping Association, 2010). These programs have the capacity to address children’s medical needs, promote positive psychosocial adjustment and independence, and allow campers to socialize with peers with similar health conditions. For individuals with physical disabilities, such as youth with spina bifida (SB), summer camps also provide an accessible setting where campers can participate in modified recreational activities that may not be available in programs for typically developing youth.
SB occurs in roughly three out of every 10,000 live births (Centers for Disease Control and Prevention, 2011) and is caused by the failed closure of the neural tube during gestation. This disorder is associated with an array of health complications, including orthopedic impairments, weakened bowel and bladder functions, and hydrocephalus. In addition, deficits in executive functioning, abstract reasoning, and attention (including higher rates of attention deficit-hyperactivity disorder [ADHD]; Burmeister et al., 2005) pose unique challenges to children with SB (Dennis, Landry, Barnes, & Fletcher, 2006). Relative to their typically developing peers, youth with SB also face various obstacles related to their psychosocial development, particularly in the domains of social functioning and independence development (Davis, Shurtleff, Walker, & Seidel, 2006; Friedman, Holmbeck, DeLucia, Jandasek, & Zebracki, 2009; Holmbeck, et al., 2010), and these difficulties appear to endure into adulthood (Zukerman, Devine, & Holmbeck, 2011). Socially, youth with SB tend to possess fewer and less intimate friendships, have lower levels of social acceptance, and are more immature and withdrawn in social interactions (Blum, Resnick, Nelson, & St. Germaine, 1991; Devine, Holmbeck, Gayes, & Purnell, 2012). Adolescents with SB also lag behind their peers in certain aspects of independence development (e.g., behavioral autonomy; Davis et al., 2006; Friedman, et al., 2009). The attainment of independence with medical care tasks may be especially difficult for individuals with SB, as cognitive difficulties may impact their ability to follow medical regimens. Clearly, youth and young adults with SB are in need of effective interventions that facilitate social skills while promoting independence, but few interventions have been implemented for this population. Among those interventions that have targeted psychosocial outcomes, findings have been mixed, and research designs have been limited by small sample sizes (Briery & Rabian, 1999; Engelman, Loomis, & Kleiback, 1994; Sherman, Berling, & Oppenheimer, 1985).
Summer camp programs present an optimal setting for implementing interventions for individuals with SB who may face accessibility barriers at other locations. Campers can practice their new social skills with other campers, and independence may be more salient when they are living away from family and caregivers. Our previous work has demonstrated the effectiveness of a camp-based intervention for youth and young adults with SB that specifically targeted the participants’ difficulties with independence and social functioning. Specifically, O’Mahar et al. (2010) found that both campers and parents observed significant improvements in social and health-related self-care goals postintervention and at a 1-month follow-up. Although this intervention possessed a number of strengths (e.g., group discussions were developed to be sensitive to campers’ cognitive abilities), the program has since been modified in an attempt to improve outcomes. For instance, updated manuals helped us target more developmentally appropriate social skills (e.g., managing sibling conflicts for younger children and navigating romantic relationships for older adolescents and young adults) and health-related self-care issues (e.g., the transition to adult medical care in young adults). Interactive activities were also included in place of more lecture-based psychoeducational lessons. Additionally, a brief neurocognitive battery was administered to each camper to examine interactions between cognitive abilities and program effectiveness.
The first objective of the current study was to examine the effectiveness of this modified camp-based intervention targeting independence in health-related self-care and social functioning in children, adolescents, and young adults with SB. As the intervention was modified by increasing social development content, incorporating more developmentally appropriate interactive activities, and re-arranging the format of topics covered, we aimed to replicate and extend O’Mahar et al. (2010) findings in a new sample of campers. Our primary outcomes focused on changes in social and health-related self-care goals attainment, as goal setting to improve skills in these domains was a major component of the intervention. Secondary outcomes included changes in overall independence, management of health-related self-care tasks, and social skills. Based on the findings of O’Mahar et al. (2010), it was expected that parents, campers, and counselors would report camper improvement on social and health-related self-care goal attainment and independence. Evaluation of changes in social functioning was new to the present study. Owing to the additional emphasis on social skills in the intervention curriculum and the opportunities to practice these skills with their peers, campers were expected to improve on measures of social functioning.
A second objective of this study was to identify conditions and participant characteristics that moderated intervention effectiveness (Holmbeck, Devine, & Bruno, 2010). Such variables can be targeted to improve future iterations of the intervention. Demographic and neurocognitive moderators were chosen based on past research that highlighted their role in social and independence development of youth with SB. While all campers were expected to show improvement, it was hypothesized that these improvements would depend on the camper’s neurocognitive functioning (i.e., IQ, ADHD symptoms, number of shunt revisions, and emotion recognition abilities), and demographic characteristics (i.e., socioeconomic status [SES] and gender).
In particular, children with higher IQs were expected to show the greatest improvements in social functioning and independence, given that children with SB and low verbal intelligence have shown a slower growth rate in emotional independence (Friedman et al., 2009). Consistent with studies that have found negative correlations between number of shunt surgeries and IQ (Hetherington et al., 1999), it was expected that campers with fewer shunt revisions would demonstrate greater improvements in social functioning and independence. Furthermore, youth without clinically significant ADHD symptoms were expected to show greater improvements relative to their peers with clinically significant symptoms, as they may be expected to pay less attention to the intervention content and tend to display difficulties retaining information (Cutting, Koth, Mahone, & Denckla, 2003). It was also hypothesized that campers with higher emotional recognition abilities would report more treatment gains in social goals and responsibilities. In accordance with research demonstrating higher levels of independence in girls with SB compared with boys (Friedman et al., 2009), it was expected that female campers would demonstrate more improvement in the independence and social domains. Campers from higher SES households were expected to demonstrate the greatest improvements in social and independence domains (Rieppi et al., 2002). Further, we expected campers who enjoyed the intervention and perceived the intervention to be more effective would benefit more than campers who felt less positively about camp.
In addition, treatment gains were expected to be similar across intervention variables (i.e., age group, year of camp, or interventionist) and camper ethnicity. No differences were expected based on age-group because the treatment followed a developmentally sensitive manualized protocol. Further, we predicted that the extensive manual-based training of interventionists implemented in both years would make differences across interventionist and year unlikely. Because previous studies of treatment effectiveness have not found ethnicity to be a moderator of outcomes (e.g., Silverman et al., 1999), we did not expect to find significant moderator effects for ethnicity.
Finally, as part of our secondary analyses, we aimed to investigate the link between changes in social and health-related self-care goals and perceptions of intervention effectiveness and satisfaction. Given the expectation that campers would improve on their goals selected for the intervention, these analyses would provide support for the notion that campers would find the intervention more enjoyable and effective if they had noticeably improved on their intervention goals. Thus, these analyses provide a more subjective evaluation of the intervention from the point of view of the campers themselves. We predicted a direct association between changes in social and health-related self-care goals and camper reports of intervention satisfaction and effectiveness.
Method
Participants
Participants were 119 individuals (aged 7–41 years; Mean [M] = 16.16, standard deviation [SD] = 6.50) attending an overnight summer camp in northern Illinois in either 2009 or 2010. Camp Independence exclusively serves individuals with SB and is conducted in week-long consecutive sessions segmented by camper age. Individuals with SB aged ≥7 years are eligible to apply to Camp Independence. Those with severe allergies or unpredictable health conditions (e.g., uncontrolled seizures) were ineligible. Placements in camp sessions were reserved on a first come first serve basis, and families were encouraged to apply for scholarship assistance if needed. Group A targeted youths aged 7–12 years (N = 44, M = 10.48, SD = 1.72), Group B targeted youths aged 13–18 years (N = 41, M = 15.41, SD = 2.05), and Group C targeted adults aged ≥19 years (N = 34, M = 24.38, SD = 5.36). See Figure 1 for more details.
Figure 1.
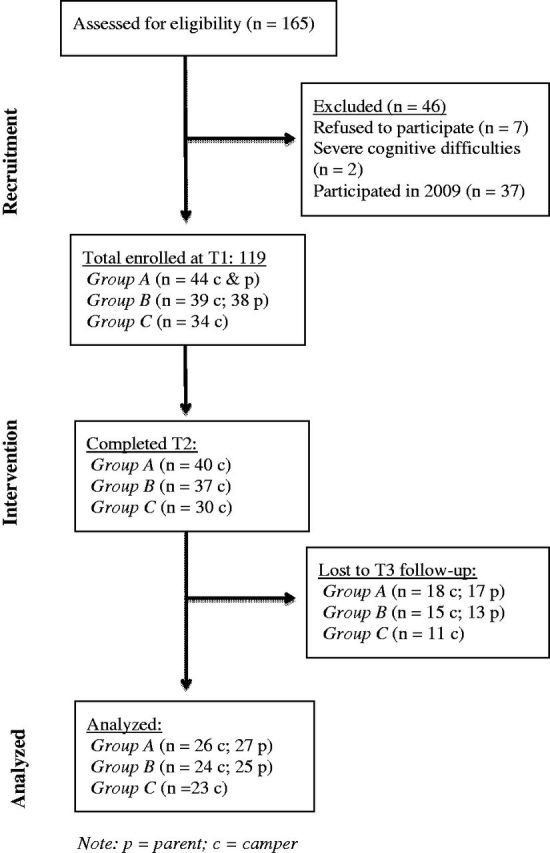
Study participant flow.
The current study included three data collection points: Time 1 (T1; preintervention); Time 2 (T2; daily throughout the intervention and the last day of camp); and Time 3 (T3; 1-month follow-up). Data were collected from parents of campers in Groups A and B at T1 and T3, as parents did not participate in the camp. Every camper was approached to participate in the study. Figure 1 illustrates the progression of participants in the treatment study. As shown, 165 children were assessed for eligibility and 46 were excluded (37 of whom were returning campers in 2010 who participated in 2009). Because the daily-intervention workshops were embedded into camp sessions, all campers participated in the intervention regardless of their decision to complete questionnaires. Collapsing across groups, the attrition rate for campers from T1 to T2 was 8.5% and from T2 to T3 was 31.8%; from T1 to T3, attrition rates were 37.6% and 36.6% for campers and parents, respectively. Participants completing measures at T2 did not differ from those who declined at T3 on any demographic or physical status characteristics, including age, gender, ethnicity, family income, and number of shunt surgeries. Participant descriptive data are provided in Table I.
Table I.
Demographic and Clinical Characteristics
| Characteristic | N (%) or M (SD) |
|---|---|
| Camper age (years) | 16.16 (6.50); range = 7–41 |
| Gender | |
| Male | 49 (41.2%) |
| Female | 70 (58.8%) |
| Ethnicity | |
| Caucasian | 75 (63.0%) |
| African American | 15 (12.6%) |
| Hispanic | 18 (15.1%) |
| Asian | 1 (0.8%) |
| Other | 7 (5.9%) |
| Missing | 3 (2.5%) |
| Family incomea | |
| <$29,999 | 14 (11.8%) |
| $30,000–69,999 | 31 (26.1%) |
| $70,000–99,999 | 16 (13.4%) |
| >$100,000 | 20 (16.8%) |
| Missing | 4 (10.9%) |
| Type of SB | |
| Myelomeningocele | 99 (83.2%) |
| Meningocele | 4 (3.4%) |
| Lipomeningocele | 1 (0.8%) |
| Occulta/myelocystocele | 2 (1.7%) |
| Missing | 13 (4.7%) |
| Lesion level | |
| Sacral | 21 (17.6%) |
| Lumbar | 71 (59.7%) |
| Lumbar–sacral | 2 (1.7%) |
| Thoracic | 11 (9.2%) |
| Missing | 14 (11.8%) |
| Number of shunt surgeries | 5.14 (8.92); range = 0–53 |
| Type of ambulation assistive deviceb | |
| Ankle–foot | 54 (45.4%) |
| Knee–ankle–foot | 14 (11.8%) |
| Hip–knee–ankle–foot | 2 (1.7%) |
| Wheelchair | 40 (43.7%) |
| None | 5 (4.2%) |
| Missing | 11 (9.2%) |
Note. M = mean; SB = spina bifida; SD = standard deviation.
a N = 85; income data were only provided by parents of campers aged ≤18 years.
bCategories are not discrete; several campers used multiple types of ambulation aids.
Procedure
This study was approved by the Institutional Review Board at Loyola University Chicago. To market the camp program, families received information about the camp through contact with their health care professionals and various print and online information from a local SB organization. Financial subsidies and sliding scale fees were available for families who could not afford to pay. Camper consent/assent, caregiver consent (for campers aged ≤18 years), and T1 questionnaires were completed via mail before the start of camp or during camp orientation on the first day of camp. Questionnaires for T2 were completed throughout the week by campers and counselors. T3 questionnaires were sent to parent and child participants approximately one month postintervention via mail with prepaid envelopes. Follow-up phone calls were made at T1 and T3 to ensure receipt of all study materials and to answer any questions. Parents and campers received monetary compensation for completion of materials.
At T1, campers and their parents completed measures assessing camper functioning, medical information, and demographic information. At T2, campers and counselors completed measures assessing campers’ social and health-goal progress and social function. Neurocognitive tests were administered by trained research assistants during camp. Across all three camper groups, 98.3% of camp counselors completed the goal progress report. At T3, both campers and parents completed measures assessing camper functioning as well as feedback about the camp and the intervention. See Table II for additional details regarding measures collected at each time point.
Table II.
Measures Collected From Each Informant at Each Data Collection Point
| Time 1 | Time 2 | Time 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤18 years | >19 years | ≤18 years | >19 years | ≤18 years | >19 years | ||||
| Measures | C | P | C | C | CC | C | C | P | C |
| Medical and demographics | X | X | |||||||
| Social skills measure | X | X | |||||||
| Social acceptance (SPP-C; SPP-A; SPP-YA) | X | X | X | X | X | X | |||
| Goal attainment | X | X | X | X | X | X | X | X | X |
| SOSBMR | X | X | X | X | X | X | |||
| Independence (SBIS) | X | X | |||||||
| Intervention evaluation | X | X | X | ||||||
| Neurocognitive measures | |||||||||
| WASI | X | X | |||||||
| DANVA | X | X | |||||||
| SNAP-IV | X | ||||||||
Note. For campers >18 years of age, parent report was not collected.
C = camper report; CC = camp counselor report; DANVA = Diagnostic Analysis of Nonverbal Accuracy; P = parent report; SPP = self perception profile; SOSBMR = sharing of spina bifida management responsibilities; SBIS = spina bifida independence survey; WASI = Wechsler Abbreviated Scale of Intelligence; SNAP-IV = Swanson, Nolan, and Pelham Parent Rating Scale.
Intervention
The 2006 version of the intervention was described by O’Mahar et al. (2010); it has since undergone changes and improvements as described above. In general, the original version of the intervention was designed to address the social and independence difficulties specific to youth and young adults with SB that have been identified in the literature. The current study combines data collected from the 2009 and 2010 summer camp sessions. The intervention was embedded within a typical camp program, which included swimming, arts and crafts, and physical activities. The intervention has three main components: (1) goal-setting, (2) counselor monitoring of these goals, and (3) 1-hr daily workshops. Before the start of camp, parents and campers collaborated to identify one health-related self-care goal and one social goal for campers to work on throughout the camp session. Camp counselors monitored these camper goals daily and collaborated with campers to accomplish the following tasks: (1) review goals, (2) review steps to achieve goals (and revise if necessary), and (3) discuss barriers to goal achievement.
In addition to goal-setting and monitoring, campers participated in daily 1-hr group workshops. Workshops included psychoeducation and strategies (e.g., problem-solving and communication) that targeted cognitive deficits believed to impede independence and social development. Workshops implemented multiple interactive activities, such as group and partner discussions, art projects, games, workbook exercises, and role plays. In place of the diaries described by O’Mahar et al. (2010), campers were provided with workbooks to use throughout the week, which they then took home with them. Two interventionists led the workshops by following a manualized curriculum for each session (Essner, Kelly, & Holmbeck, 2010). Both interventionists were postbaccalaureate research assistants in a health-related field and were trained by masters-level study coordinators. Each day, a different topic was addressed based on common health and social goals identified in a pilot study conducted in 2005: (1) building friendships and communication skills, (2) self-esteem and emotional wellness, (3) living with SB (e.g., personal and outside reactions to SB), and (4) health-related self-care. Three versions of the intervention manual were used to ensure developmentally appropriate content and activities for each age group. For example, the intervention manual for Group A (aged 7–12 years) focused on family-related issues, whereas the manual for Group B (aged 13–18 years) contained more content on peer relationships.
Measures
Primary Outcomes
Goal Attainment (T1, T2, T3)
Health-related self-care and social goals were assessed using a goal attainment scale (Joyce, Rockwood, & Mate-Kole, 1994; Malec, 1999) that was developed for this study. At T1, campers and parents chose one social goal and one health-related self-care goal from a comprehensive list. Parents, campers, and counselors then independently rated current camper goal attainment status using a 5-point scale (1 = “not at all reaching this goal” to 5 = “completely reaching this goal”). Data on camper goal attainment was collected from parents at T1 and T3. Campers reported on their goals at all three time points. Counselors reported on goal attainment for four consecutive days during the camp session (i.e., T2).
Secondary Outcomes
Social Skills (T1 and T3)
A 26-item measure, the Social Skills Measure, was developed for this study to measure campers’ social skills that were specifically targeted in the intervention (McLone & Ito, 1998; Wills, 1993). Parents rated how often campers demonstrated important verbal and nonverbal interpersonal skills (e.g., “Stays on topic during conversations” and “Maintains appropriate eye contact”) using a 5-point Likert scale (1 = Never to 5 = Always). In the current sample, internal consistency was adequate (α = .86).
Social Acceptance (T1, T2, T3)
The Social Acceptance subscale from Harter’s Self Perception Profile (Harter, 1985, 1988) was used to assess campers’ social acceptance by peers. Developmentally appropriate versions of this measure (i.e., Child, Adolescent, and Young Adult) were provided for each age group. A total score was computed by averaging all items with higher scores indicating greater social acceptance. In the current sample, reliability coeffecients were .16, .67, and .76 for the child, adolescent, and young adult versions, respectively. Scores from the child version were not included in subsequent analyses owing to poor internal consistency.
Sharing of SB Management Responsibilities (T1, T3)
The Sharing of SB Management Responsibilities (SOSBMR) was closely adapted from the Diabetes Family Responsibility Questionnaire, a measure that has shown adequate internal consistency and concurrent validity (Anderson, Auslander, Jung, Miller, & Santiago, 1990). The SOSBMR was used to assess changes in responsibility for SB tasks across several domains (e.g., health appointments, communication about SB, medications). Campers and parents indicated who was responsible for 34 tasks (1 = parent, 2 = shared, 3 = camper or “N/A”). Mean scores were computed for all subscales as well as the total score, with higher scores indicating greater camper responsibility. The SOSBMR total score and subscales displayed adequate reliability (α = .66–.95 camper report; α = .67–.94 parent report).
SB Independence Survey (T1, T3)
The 48-item SB Independence Survey (SBIS) was closely adapted from the Diabetes Independence Survey, a measure that has shown adequate construct and concurrent validity (Wysocki et al., 1996). Parents responded “yes,” “no,” “not sure,” or “N/A” regarding their child’s mastery of disease-related skills, such as medication management and catheterization. Ratio scores of “yes” responses to the total number of item responses were calculated to determine the degree to which a camper had mastered condition-related tasks, with higher scores indicating better mastery of tasks. Internal consistency for the SBIS was excellent (α = .98).
Intervention-Related Variables (T3)
Campers’ evaluations of the intervention were assessed by a measure created for this study asking them to rate their satisfaction with the intervention and their perception of intervention effectiveness using a 6-point Likert rating scale (1 = Strongly Disagree to 6 = Strongly Agree). Reliability for this sample was adequate for the satisfaction subscale (α = .65) and the perception of effectiveness subscale (α = .81).
Moderators
Medical and Demographic Moderators (T1)
Parents completed a demographics form assessing their children’s age, gender, ethnicity, and their total household income. Parents also completed a medical history form assessing lesion level, type of SB, number of shunt surgeries, and ambulation status. Owing to the nature of the grouped analyses (see below), two groups were created that fell above and below the median cut point of three total shunt surgeries (i.e., two or fewer surgeries; three or more surgeries). Similarly, two income groups were formed for the purposes of data analyses: families with a combined income of ≤$70,000 per year, and >$70,000 per year (e.g., Herring et al., 2008).
Neurocognitive Moderators (T1)
To assess neurocognitive functioning, trained research assistants administered measures of cognitive ability and emotion recognition, and parents provided data on their child’s ADHD symptoms. If already administered within the past 2 years, IQ and emotion recognition data were extracted from previous camp evaluations or from an ongoing longitudinal study that used the same measures (e.g., Devine et al., 2012).
Cognitive ability
Cognitive ability was assessed using the Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999). The Vocabulary and Matrix Reasoning subtests were administered to campers, yielding an estimated Full-Scale IQ score (FSIQ). Consistent with Wechsler’s (2003) guidelines of youth intellectual functioning, a FSIQ cutoff point of 80 was used to create two groups: campers with lower (≤80) and higher (>80) cognitive abilities.
Emotion recognition
Emotion recognition was measured using the Child Facial Expression subtest of the Diagnostic Analysis of Nonverbal Accuracy 2 (Nowicki, 2003). Nonverbal accuracy–scaled scores were computed according to normative data. For the purpose of this study, a conservative cutoff point of 85 (corresponding to one SD below the mean standard score) was used to create two groups: (1) campers with scores <85, indicating lower emotion recognition ability, and (2) campers with scores of ≥85, indicating greater emotion recognition ability.
ADHD symptoms
ADHD symptoms were measured using the Swanson, Nolan, and Pelham Parent Rating Scale (SNAP-IV; 2001). Using a 4-point Likert scale (0 = not at all to 3 = very much), parents answered 18 items on the extent to which their child has demonstrated DSM-IV criteria-based symptoms of inattention and impulsivity/hyperactivity. Average subscale scores were calculated for inattention and impulsivity/hyperactivity, and scores at or above the 95th percentile were used to determine whether a camper had clinically significant symptoms of ADHD (Swanson et al., 2001). This measure’s reliability was acceptable in the current sample (α = .88).
Results
Preliminary Analyses
Power analyses were conducted using G*Power 3 (Faul, Erdfelder, Lang, & Buchner, 2007) to determine whether our sample size was adequate to detect a medium to large effect size. Because several variables included data from three time points, repeated measures analyses of variances (ANOVAs) were used to test the hypotheses. Assuming a medium effect size f = .25, power = .95, and α = .05, a total sample size of 66 was required for the most complicated analysis (within-subjects main effect across three time points and two-way interactions). Based on a large effect size f = .40, power = .95, and α = .05, a total sample size of 30 was required for the within-subjects main effect and two-way interactions. Thus, our sample size of 74–117 was sufficient to detect medium to large effect sizes (Cohen, 1988).
Before running the analyses, the outcome variables were examined for outliers and skewness (Tabachnick & Fidell, 2001). A total of seven outlier data points from five outcomes were removed. Skewness analyses were conducted for all outcome variables at each (Tabachnick & Fidell, 2001). Skewed variables were transformed using a log transformation after a square root transformation failed to sufficiently reduce skewness. The following variables were transformed: SOSBMR Appointment subscale (parent and child report; positive skew), SOSBMR Self-care subscale (camper report; negative skew), SOSBMR Catheterization subscale (camper report; negative skew), and the SBIS (positive skew).
Thirty-seven campers who participated in 2009 returned to the camp intervention program in 2010. Because it was assumed that earlier participation in the intervention may be less biased by practice effects, data from these campers’ second sessions (i.e., 2010) were removed from the analyses (see Figure 1). Thus, we analyzed data from the earliest time point of all participating campers, resulting in 75 campers included in analyses using data from T1, T2, and T3 and 119 campers included in analyses using counselor-reported data at T2.
Hypothesis 1
It was expected that campers’ goal achievement, independence, and social competence would increase over time for all campers. Results of the tests of main effects are presented in Table III. Mauchly’s tests indicated that the assumption of sphericity was violated for the within-subjects main effect of time for camper reports of social goals [χ2(5) = 38.67, p < .001] and health-related goals [χ2(5) = 18.27, p < .01]. In other words, the variances of the differences between campers’ data across the three time points were unequal. Thus, degrees of freedom were corrected for these measures using Greenhouse–Geisser estimates of sphericity (ε = .76 and ε = .88 for social and health-related self-care goals, respectively).
Table III.
Repeated Measures Analyses of Variance for Main Effects
| Outcome | Reporter | Time 1 M (SD) | Time 2 M (SD) | Time 3 M (SD) | F | df | Partial η2 |
|---|---|---|---|---|---|---|---|
| Social skills | (p)a,b | 3.46 (0.51) | 3.54 (0.58) | 1.61 | 1, 50 | .03 | |
| Harter social acceptance | (c)b,c | 2.84 (0.77) | 3.02 (0.84) | 2.85 (0.81) | 1.64 | 2, 74 | .04 |
| Individual social goals | (p)a,b | 2.62 (0.66) | 3.21 (0.95) | 13.83** | 1, 41 | .25 | |
| (c)a,b,c | 2.86 (1.03) | 3.80 (0.88) | 3.66 (1.10) | 19.02*** | 2, 86 | .31 | |
| (cc)m,t,w,th | 3.03 (1.0) | 4.00 (0.87)d | 49.83*** | 3, 213 | .35 | ||
| Individual health goals | (p)a,b | 2.14 (0.78) | 2.93 (0.97) | 27.21*** | 1, 41 | .40 | |
| (c)a,b,c | 2.58 (1.12) | 3.78 (1.06) | 3.24 (1.19) | 16.37*** | 2, 88 | .27 | |
| (cc)m,t,w,th | 2.95 (1.18) | 3.52 (0.97)d | 20.18*** | 3, 206 | .21 | ||
| SOSBMR: appointmentsd | (p)a,b | 0.07 (0.08) | 0.09 (0.10) | 1.81 | 1, 45 | .04 | |
| (c)a,b,c | 1.35 (0.32) | 1.40 (0.40) | 1.10 | 1, 67 | .02 | ||
| SOSBMR: communication | (p)a,b | 1.83 (0.59) | 2.12 (0.59) | 14.32*** | 1, 48 | .23 | |
| (c)a,b,c | 2.24 (0.55) | 2.33 (0.57) | 1.98 | 1, 69 | .03 | ||
| SOSBMR: medication | (p)a,b | 1.56 (0.55) | 1.70 (0.64) | 3.27 | 1, 45 | .07 | |
| (c)a,b,c | 1.95 (0.71) | 2.00 (0.67) | 0.56 | 1, 69 | .01 | ||
| SOSBMR: ambulation | (p)a,b | 2.30 (0.55) | 2.44 (0.48) | 4.35* | 1, 47 | .09 | |
| (c)a,b,c | 2.55 (0.44) | 2.61 (0.39) | 1.89 | 1, 65 | .03 | ||
| SOSBMR: needs, self-cared | (p)a,b | 2.40 (0.67) | 2.56 (0.58) | 4.26* | 1, 49 | .08 | |
| (c)a,b,c | 0.11 (0.16) | 0.13 (0.18) | 0.72 | 1, 69 | .01 | ||
| SOSBMR: skin care | (p)a,b | 1.94 (0.56) | 2.13 (0.52) | 10.31** | 1, 48 | .18 | |
| (c)a,b,c | 2.15 (0.72) | 2.27 (0.66) | 2.36 | 1, 68 | .03 | ||
| SOSBMR: exercise and diet | (p)a,b | 2.06 (0.73) | 2.17 (0.66) | 0.56 | 1, 34 | .02 | |
| (c)a,b,c | 2.48 (0.75) | 2.40 (0.78) | 0.34 | 1, 39 | .01 | ||
| SOSBMR: catheterizingd | (p)a,b | 2.24 (0.68) | 2.39 (0.65) | 11.00** | 1, 48 | .19 | |
| (c)a,b,c | 0.16 (0.16) | 0.14 (0.16) | 5.92* | 1, 69 | .08 | ||
| SOSBMR: bowel program | (p)a,b | 1.76 (0.56) | 1.98 (0.53) | 12.81** | 1, 50 | .20 | |
| (c)a,b,c | 2.20 (0.60) | 2.20 (0.64) | 0.01 | 1, 71 | .00 | ||
| SOSBMR: total | (p)a,b | 1.92 (0.42) | 2.12 (0.41) | 43.68*** | 1, 50 | .47 | |
| (c)a,b,c | 2.21 (0.44) | 2.28 (0.45) | 8.15** | 1, 72 | .10 | ||
| SBIS independence | (p)a,b | 0.50 (0.35) | 0.59 (0.38) | 6.62* | 1, 41 | .14 |
Note. (p) = parent report; (c) = child report; (cc) = camp counselor report; M = mean; SBIS = Spina Bifida Independence Survey; SD = standard deviation; SOSBMR = Sharing of Spina Bifida Management Responsibilities.
aGroup A (aged 7–12 years).
bGroup B (aged 13–18 years).
cGroup C (aged ≥19 years).
dVariable was log-transformed. m, t, w, th Monday, Tuesday, Wednesday, Thursday (i.e., each intervention day in a week-long session).
*p < .05, **p < .01, ***p < .001.
As hypothesized, significant main effects in the expected directions were found for the following outcomes: social goals (parent, camper, and counselor report); health goals (parent, camper, and counselor report); child responsibility for tasks involving communication (parent report), ambulation (parent report), general self-care (parent report), skin care (parent report), catheterizing (parent and child report), and bowel program (parent report); total responsibility for SB-related tasks (parent and child report); and level of SB independence (parent report). All significant changes over time were in the positive direction, except for child-reported management of catheterizing, which decreased over time (see Table III). Improvements in social and health-related goals reported by all informants yielded large effects (i.e., partial η2 ≥ .14), as did most significant parent reports of management of health-related self-care tasks and overall independence. Medium effects (i.e., partial η2 = .06) were observed for the other outcomes.
Clinically significant change on statistically significant outcome measures was determined by comparing changes in values from T1 and T3 with the corresponding SDs at T1. Using the criteria of a large change of two SDs (Kazdin, 2003), none of the statistically significant findings attained clinical significance. As smaller changes can still have a meaningful impact on the campers’ everyday functioning (Kazdin, 2003), improvements of one SD were also investigated. Changes of approximately one standard were found for parent-reported health-related goal attainment and counselor-reported social goal attainment. For campers, improvements in social and health-related self-care goals were greater than or equal to one SD at T2 but not at T3. Statistically significant changes on the secondary outcome measures were all smaller than one SD.
Hypothesis 2
It was expected that improvements in campers’ level of social competence and independence would be greatest for campers in the following groups: females, campers with higher family income, campers with higher intelligence, campers with higher emotion-recognition ability, campers with fewer ADHD symptoms, and campers with fewer shunt revisions. Repeated measures ANOVAs were used to examine interactions to determine whether changes in outcome measures depended on each potential moderator. Results of the significant interactions are presented in Table IV.
Table IV.
Repeated Measures Analyses of Variance for Significant Interactions
| Interaction, outcome | Interaction F | Group | N | Time 1 M (SD) | Time 3 M (SD) | Main effect F | d |
|---|---|---|---|---|---|---|---|
| IQ × time, individual SB goals (cc) | 3.84* | Low IQ | 38 | 3.32 (1.14) | 3.82 (1.11)d | 2.53 | 0.42 |
| High IQ | 32 | 2.50 (1.05) | 3.78 (1.07)d | 23.47*** | 1.14 | ||
| IQ × time, SOSBMR total (c)a,b,c | 4.71* | Low IQ | 32 | 2.18 (0.45) | 2.18 (0.44) | 0.01 | 0.01 |
| High IQ | 35 | 2.32 (0.38) | 2.43 (0.41) | 9.30** | 0.24 | ||
| No. of shunt surgeries × time, SOSBMR total (c)a,b,c | 7.86** | <3 | 34 | 2.10 (0.45) | 2.23 (0.44) | 16.40*** | 0.28 |
| ≥3 | 36 | 2.29 (0.42) | 2.30 (0.46) | 0.09 | 0.02 | ||
| Income × time, social skills (p)a,b | 8.05** | Low income | 23 | 3.46 (0.56) | 3.73 (0.59) | 8.12** | 0.43 |
| High income | 25 | 3.52 (0.46) | 3.47 (0.48) | 0.67 | −0.10 | ||
| Ethnicity × time, social skills (p)a,b | 6.98* | Caucasian | 35 | 3.46 (0.55) | 3.44 (0.54) | 0.17 | −0.03 |
| Other | 16 | 3.45 (0.45) | 3.75 (0.64) | 5.93* | 0.48 |
Note. (p) = parent report; (c) = child report; (cc) = camp counselor report; M = mean; SB = spina bifida; SD = standard deviation; SOSBMR = Sharing of SB management responsibilities.
aGroup A (aged 7–12 years).
bGroup B (aged 13–18 years).
cGroup C (aged ≥19 years).
*p < .05, **p < .01, ***p < .001.
Three of the eight hypothesized moderators resulted in a significant interaction for at least one outcome. Results suggest that a child’s level of intelligence moderated his/her success with counselor-reported SB goals [F(3, 204) = 3.84, p = .01] and overall management of SB-related tasks [F(1, 65) = 4.71, p = .03]. Specifically, children with higher intelligence showed a significant increase in these outcomes, while those with lower intelligence did not (see Table IV). Improvements in the overall management of SB-related tasks also depended on the number of shunt surgeries a child had undergone, F(1, 62) = 7.86, p = .01. Contrary to our expectations, children with fewer shunt revisions demonstrated significant improvements, a small effect. The family’s level of income was found to moderate changes in social skills [F(1, 43) = 8.05, p = .01], such that children from families with a lower income showed significant improvement in social skills (a small-to-medium effect; see Table IV).
Hypothesis 3
It was hypothesized that the intervention would be equally effective for campers in different intervention variables and for campers of different ethnicities. This hypothesis was tested by examining the following variables as possible moderators: age group (A, B, or C), interventionist (two different interventionists), year in which the camp took place (2009 or 2010), and camper ethnicity. A Group × Time interaction was examined for each combination of moderator and outcome, resulting in 44 analyses. As the number of significant findings (i.e., 1/44 = 2.2%) was no more than what would be expected by chance, these results are not reported further.
Hypothesis 4
It was predicted that campers who improved most on their social and health-related self-care goals would report the intervention to be more satisfying and effective. Before conducting analyses, residual variables were computed for both parent report and camper report of the change in social and health-related self-care goal attainment from T1 to T3. To examine the hypothesis, four regressions were conducted, with either camper perception of intervention effectiveness or intervention satisfaction entered as the dependent variable and the residual variables of either parent or camper report of changes in goal attainment entered as independent variables. One of the four regressions produced significant findings. Specifically, improvements in parent-reported social goals predicted higher camper ratings of intervention effectiveness (β = .444, p < .05).
Discussion
The current study sought to replicate findings of a previous study demonstrating the effectiveness of a summer camp intervention intended to promote independence and social skills in individuals with SB (O’Mahar et al., 2010). Consistent with our hypotheses and the results of our previous work (O’Mahar et al., 2010), parents, campers, and counselors reported significant improvement in social and health goal attainment and management of SB-related health responsibilities. The large effects found across all reporters for goal attainment support the use of goal setting activities in similar interventions, while small-to-medium effects of more distal outcome measures provide evidence for the potential diffuse impact of the intervention. We also examined moderators of intervention effects. Intervention outcomes tended not to differ according to year, interventionist, age group, or ethnicity. Partially supporting our predictions, several indices of camper improvement were moderated in the predicted directions by neurocognitive functioning, while income had an effect on improvements in the opposite direction.
The intervention effects reported by multiple informants (i.e., campers, parents, and counselors) are stronger than those first reported by O’Mahar et al. (2010), lending additional support to the utility of a brief, camp-based intervention using workshops and goal setting focused on improvement of independence and social skills in individuals with SB. Although significant improvements in social and health-related self-care goals were found across all informants, effects for camper reports were smaller in magnitude compared with parent reports, suggesting campers perceived less improvement in responsibility for SB-related tasks. This discrepancy is consistent with previous findings demonstrating high rates of disagreement between youth with SB and their parents regarding the transfer of responsibilities, with youth generally reporting more responsibility (Devine, Wasserman, Gershenson, Holmbeck, & Essner, 2011; Sawin et al., 2006). Put another way, it is likely that campers’ perceived a relatively high level of independence that was maintained over the span of camp (i.e., a ceiling effect), whereas parents noticed significant improvements in their campers’ abilities after camp.
As a new area of focus relative to our previous work (O’Mahar et al., 2010), the lack of improvement found across measures of general social functioning is notable. Although campers’ social goal attainment increased after the intervention, these specific improvements may not have generalized to other social skills. Given that youth with SB spend less time with peers (Devine et al., 2012) and that campers may have fewer opportunities to interact with peers over the summer, campers may not have had sufficient opportunities to demonstrate improvements in social skills. Alternatively, the social skills component of the intervention curriculum may require modification and improvement. For example, it may be beneficial to view and discuss videotaped models of adaptive and maladaptive social interactions (Gresham & Nagle, 1980). In fact, a social skills video modeling component is planned for upcoming Camp Independence sessions.
The expected moderators of intervention outcomes were only partially confirmed by this study, with effect sizes for significant moderators being small-to-medium. Income played an unexpected role in intervention effectiveness. Parents of campers in the lower income group reported greater improvement in social skills and progress in health goals. Lower SES campers are more likely to disagree with their parents about who is responsible for SB tasks (Devine et al., 2011), and they may not have access to resources that build social skills and goal-oriented behavior at school and at home. Thus, the intervention may be more stimulating and salient to them compared with children from higher SES backgrounds, and it may help them to improve communication with their parents about their SB responsibilities (also see Rieppi et al., 2002; Rhee, Belyea, Hunt, & Brasch, 2011). These results suggest that summer camps with similar intervention programs should be made affordable for families from lower socioeconomic backgrounds. Given that IQ level significantly influenced intervention effects, it may be necessary to provide more support to campers with lower intellectual functioning during intervention sessions. The importance of treatment protocols sensitive to varying cognitive-developmental levels has recently received increased attention in the field (Holmbeck, Devine, & Bruno, 2010).
In general, campers were satisfied with the intervention, and many campers perceived the intervention to be effective. Of note, improvements in health-related self-care goals did not seem to influence campers’ beliefs that the intervention had helped them or their overall enjoyment of the program. However, parents’ ratings of improvement on social goals predicted campers’ perceptions of effectiveness. In other words, it appears that campers who felt the intervention had helped them to become more independent tended to show improvement on their specific social goals. Perhaps improvements in specific social skills had a greater influence on campers’ everyday lives. It is also possible that campers valued their social goal improvements and were more motivated to work on these goals during camp. Given the relatively high satisfaction with the intervention overall, there may have been inadequate variability in satisfaction ratings to yield significant results.
Despite several strengths, including a focus on moderators of intervention improvement, use of multiple reporters, and implementation of a developmentally gauged manual-based intervention protocol, there were also several limitations. First, sample sizes were somewhat small, resulting in insufficient power to detect small effects. This was partially due to low response rates at 1 month after intervention. The small sample precluded the examination of three-way interactions involving multiple moderators. Second, the construct validity of the Social Skills Measure has not yet been established. Third, follow-up data were only available 1 month after intervention; long-term effects should be studied in future work. Fourth, counselors, campers, and parents were not blind to the goals of the study, increasing the likelihood of response bias. Finally, owing to the lack of a control group, this study could not rule out overall camp experiences as possible explanations for intervention effects.
Several clinical implications emerge from our findings. First, the intervention evaluated in this study may help a larger number of individuals with SB if it is disseminated to other health-related summer camps. Use of straightforward, detailed treatment manuals likely facilitates the process of implementing the intervention at other sites (Addis, 1997). Further, goal-setting that targets an individual’s personal social and health-related self-care difficulties is a simple and inexpensive component of this intervention that may be beneficial when included in routine clinic appointments with physicians, nurses, and other health care professionals. Second, by targeting social and independence development, youth and young adults with SB may experience both immediate and long-term improvements, such as improving the quality of their social interactions, taking on more self-care responsibilities, and developing the skills and confidence to become less dependent on their families. The observed significant differences are encouraging, but it should be noted that evidence of clinically significant change is limited. Improvements in social and health-related goal attainment satisfied a modified indicator of clinical significance, suggesting the primary aims of the intervention had a noticeable impact on campers’ functioning. However, campers appeared to perceive that their progress in social and health-related goal attainment decreased as time passed following the conclusion of the intervention. It is possible that the therapeutic process of the intervention (i.e., learning how to set goals, acquiring strategies for assertive communication, making friends, eliciting emotional support, etc.) may have been greater or equal in importance to the measured intervention outcomes (Kazdin, 2003). Additional research is necessary to further evaluate the clinical impact of the present findings and ways in which clinically significant goal improvements can be maintained over time. Third, individuals from lower SES backgrounds appear to especially benefit in these domains, so scholarships or sliding scale fees should be made available to allow such individuals to attend camp.
Overall, our results complement those described by O’Mahar et al. (2010) by exploring additional outcomes and providing support for the effectiveness of a camp-based intervention targeting social skills and independent self-care skills in youth and young adults with SB. More generally, our findings corroborate previous positive results from other camp programs developed for youth with disabilities (Sherman et al., 1985; Briery & Rabian, 1999). Also, the present study expands on the work of O’Mahar et al. (2010) by examining for whom the intervention is most helpful. In general, most campers benefited from the intervention, although certain camper characteristics (i.e., IQ, number of shunt surgeries, and income) influenced increases in goal attainment, social functioning, and independence from preintervention to follow-up. Investigating moderators of treatment outcomes also informs future intervention planning and aids in identifying campers who may require more support. Future studies may also investigate whether this camp-based intervention model could be successfully adapted to other chronic health conditions (e.g., cerebral palsy, traumatic brain injury).
Funding
Completion of this manuscript was supported in part by a research grant from the Spastic Paralysis Research Foundation: Illinois—Eastern Iowa District of Kiwanis International.
Conflicts of interest: None declared.
Acknowledgments
The authors would like to thank the Spastic Paralysis Research Foundation: Illinois—Eastern Iowa District of Kiwanis International, Camp Independence, YMCA Camp Duncan, the Illinois Spina Bifida Association, Renae Alvarez, Laurie Gayes, and the undergraduate and graduate research assistants who assisted with camp procedures and data management. The authors would also like to extend their appreciation to the campers and parents who contributed their time and effort to this study.
Authors C.M., A.P., and R.W.: their contributions were equivalent. Authors B.E. and L.O.: their contributions were equivalent.
References
- Addis M E. Evaluating the treatment manual as a means of disseminating empirically validated psychotherapies. Clinical Psychology: Science and Practice. 1997;4:1–11. [Google Scholar]
- American Camping Association. 2010 Retrieved from http://www.acacamps.org/ [Google Scholar]
- Anderson B J, Auslander W F, Jung K C, Miller J P, Santiago J V. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15:477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Blum R W, Resnick M D, Nelson R, St. Germaine A. Family and peer issues among adolescents with spina bifida and cerebral palsy. Pediatrics. 1991;88:280–285. [PubMed] [Google Scholar]
- Briery B G, Rabian B. Psychosocial changes associated with participation in a pediatric summer camp. Journal of Pediatric Psychology. 1999;24:183–190. doi: 10.1093/jpepsy/24.2.183. [DOI] [PubMed] [Google Scholar]
- Burmeister R, Hannay H J, Copeland K, Fletcher J, Boudousquie A, Dennis M. Attention problems and executive functions in children with spina bifida and hydrocephalus. Child Neuropsychology. 2005;11:265–283. doi: 10.1080/092970490911324. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Neural tube defect ascertainment project. 2011 Retrieved from http://www.nbdpn.org. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cutting L E, Koth C E, Mahone E M, Deckla M B. Evidence for unexpected weaknesses in learning in children with attention-deficit/hyperactivity disorder without reading disabilities. Journal of Learning Disabilities. 2003;36:259–269. doi: 10.1177/002221940303600305. [DOI] [PubMed] [Google Scholar]
- Davis B E, Shurtleff D B, Walker W O, Seidel K D. Acquisition of autonomy skills in adolescents with myelomeningocele. Developmental Medicine and Child Neurology. 2006;48:253–258. doi: 10.1017/S0012162206000569. [DOI] [PubMed] [Google Scholar]
- Dennis M, Landry S H, Barnes M, Fletcher J M. A model of neurocognitive function in spina bifida over the life span. Journal of the International Neurocognitive Society. 2006;12:285–296. doi: 10.1017/S1355617706060371. [DOI] [PubMed] [Google Scholar]
- Devine K A, Holmbeck G N, Gayes L, Purnell J Q. Friendships of children and adolescents with spina bifida: Social adjustment, social performance, and social skills. Journal of Pediatric Psychology. 2012;37:220–231. doi: 10.1093/jpepsy/jsr075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine K A, Wasserman R M, Gershenson L S, Holmbeck G N, Essner B S. Mother-adolescent agreement regarding decision-making autonomy: A longitudinal comparison of families of adolescents with and without spina bifida. Journal of Pediatric Psychology. 2011;36:277–288. doi: 10.1093/jpepsy/jsq093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelman B E, Loomis J W, Kleiback L. A psychoeducational group addressing self-care, self-esteem, and social skills in children with spina bifida. European Journal of Pediatric Surgery. 1994;4:38–39. [PubMed] [Google Scholar]
- Essner B, Kelly L, Holmbeck G. Camp ability: A camp curriculum addressing independence, social skills, emotional wellness, and self-care. 2nd ed. 2010. Unpublished manual. [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Friedman D, Holmbeck G N, DeLucia C, Jandasek B, Zebracki K. Trajectories of autonomy development across the adolescent transition in children with spina bifida. Rehabilitation Psychology. 2009;54:16–27. doi: 10.1037/a0014279. [DOI] [PubMed] [Google Scholar]
- Gresham F M, Nagle R J. Social skills training with children: Responsiveness to modeling and coaching as a function of peer orientation. Journal of Consulting and Clinical Psychology. 1980;48:718–729. doi: 10.1037//0022-006x.48.6.718. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for self-perception profile for children: Revision of the perceived competence scale for children. Denver, CO: University of Denver; 1985. [Google Scholar]
- Harter S. Manual for the Self-Perception profile for adolescents. Denver, CO: University of Denver; 1988. [Google Scholar]
- Herring S S J, Rich-Edwards J W, Oken E, Rifas-Shiman S L, Kleinman K P, Gillman M W. Association of postpartum depression with weight retention 1 year after childbirth. Obesity (Silver Spring, Md.) 2008;16:1296–1301. doi: 10.1038/oby.2008.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington R, Dennis M, Barnes M, Drake J, Gentili F. Functional outcome in young adults with spina bifida. Journal of Neurology, Neurosurgery & Psychiatry. 1999;67:591–595. [Google Scholar]
- Holmbeck G N, DeLucia C, Essner B, Kelly L, Zebracki K, Friedman D, Jandasek B. Trajectories of psychosocial adjustment in adolescents with spina bifida: A 6-year, four-wave longitudinal follow-up. Journal of Consulting and Clinical Psychology. 2010;78:511–525. doi: 10.1037/a0019599. [DOI] [PubMed] [Google Scholar]
- Holmbeck G N, Devine K A, Bruno E F. Developmental issues and considerations in research and practice. In: Weisz J R, Kazdin A E, editors. Evidence-based psychotherapies for children and adolescents. 2nd ed. New York, NY: The Guilford Press; 2010. pp. 28–39. [Google Scholar]
- Joyce B M, Rockwood K J, Mate-Kole C C. Use of goal attainment scaling in brain injury in a rehabilitation hospital. American Journal of Physical Medicine & Rehabilitation/Association of Academic Physiatrists. 1994;73:10–14. [PubMed] [Google Scholar]
- Kazdin A E. Clinical significance: Measuring whether interventions make a difference. In: Kazdin A E, editor. Methodological issues & strategies in clinical research. 3rd ed. Washington, DC: American Psychological Association; 2003. pp. 691–710. [Google Scholar]
- Malec J J F. Goal attainment scaling in rehabilitation. Neurocognitive Rehabilitation. 1999;9:253–275. [Google Scholar]
- McLone D G, Ito J. An introduction to spina bifida. Chicago, IL: Children’s Memorial Spina Bifida Team; 1998. [Google Scholar]
- Nowicki S. Manual for the receptive tests of the diagnostic analysis of nonverbal accuracy 2: DANVA2. Atlanta, GA: Department of Psychology, Emory University; 2003. [Google Scholar]
- O'Mahar K, Holmbeck G N, Jandasek B, Zuckerman J. A camp-based intervention targeting independence among individuals with spina bifida. Journal of Pediatric Psychology. 2010;35:848–856. doi: 10.1093/jpepsy/jsp125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee H, Belyea M J, Hunt J F, Brasch J. Effects of a peer-led asthma self-management program for adolescents. Archives of Pediatrics & Adolescent Medicine. 2011;165:513–519. doi: 10.1001/archpediatrics.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieppi R, Greenhill L L, Ford R E, Chuang S, Wu M, Davies M, Abikoff H B, Arnold L E, Conners C K, Elliott G R, Hechtman L, Hinshaw S P, Hoza B, Jensen P S, Kraemer H C, March J S, Newcorn J H, Pelham W E, Severe J B, Swanson J M, Vitiello B, Wells K C, Wigal T. Socioeconomic status as a moderator of ADHD treatment outcomes. Journal of American Academy of Child and Adolescent Psychiatry. 2002;41:269–277. doi: 10.1097/00004583-200203000-00006. [DOI] [PubMed] [Google Scholar]
- Sawin K J, Bellin M H, Builta E, Vasel L, Buran C F, Brei T J. Cross-informant agreement between adolescents with myelomeningocele and their parents. Developmental Medicine & Child Neurology. 2006;48:188–194. doi: 10.1017/S0012162206000417. [DOI] [PubMed] [Google Scholar]
- Sherman R G, Berling B S, Oppenheimer S. Increasing community independence for adolescents with spina bifida. Adolescence. 1985;20:1–13. [PubMed] [Google Scholar]
- Silverman W K, Kurtines W M, Ginsburg G S, Weems C F, Lumpkin P W, Carmichael D H. Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- Swanson J M, Kraemer H C, Hinshaw S P, Arnold L E, Conners C K, Abikoff H B, Clevenger W, Davies M, Elliott G R, Greenhill L L, Hechtman L, Hoza B, Jensen P S, March J S, Newcorn J H, Owens E B, Pelham W E, Schiller E, Severe J B, Simpson S, Vitiello B, Wells K, Wigal T, Wu M. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- Tabachnick B G, Fidell L S. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001. Using multivariate statistics. [Google Scholar]
- Wechsler D. Wechsler abbreviated scales of intelligence (WASI) San Antonia, TX: Psychological Corporation; 1999. [Google Scholar]
- Wechsler D. WISC-IV technical and interpretive manual. San Antonia, TX: Psychological Corporation; 2003. [Google Scholar]
- Wills K K W. Neurocognitive functioning in children with spina bifida and/or hydrocephalus. Journal of Clinical Child Psychology. 1993;22:247–265. [Google Scholar]
- Wysocki T, Meinhold P M, Taylor A, Hough B S, Barnard M U, Clarke W L, Bellando B J, Bourgeois M J. Psychometric properties and normative data for the parent version of the Diabetes Independence Survey. The Diabetes Educator. 1996;22:587–591. doi: 10.1177/014572179602200606. [DOI] [PubMed] [Google Scholar]
- Zukerman J M, Devine K A, Holmbeck G N. Adolescent predictors of emerging adult milestones in youth with spina bifida. Journal of Pediatric Psychology. 2011;36:265–276. doi: 10.1093/jpepsy/jsq075. [DOI] [PMC free article] [PubMed] [Google Scholar]


