Abstract
Among sexual minorities, bisexuals are at the greatest risk for poor health, due in part to prejudice and stigma. This research examined associations of bisexual-specific minority stress and health among cisgender (non-transgender) and transgender adults with bisexual orientation. Participants were 488 adults (378 cisgender women, 49 cisgender men, 61 transgender individuals), age 18–66 years, with bisexual orientation based on identity and/or attractions to multiple genders. Participants completed an online survey. Hierarchical linear regression analyses were conducted with sexual minority stress and bisexual-specific minority stress as the predictors and physical health (measured by the SF-36) as the outcome. Models controlled for demographic variables. Moderation analyses were conducted to test for gender differences. Greater bisexual-specific minority stress significantly predicted poorer overall physical health (β=−0.16), greater pain (β=−0.16), and poorer general health (β=−0.25) above and beyond the effects of sexual minority stress. Gender moderated the association between bisexual-specific minority stress and health, such that bisexual-specific minority stress predicted overall physical health and role limitations for transgender individuals, but not for cisgender women. Addressing bisexual-specific minority stress is necessary to improve the health and well-being of bisexual individuals.
Keywords: sexual minority, bisexual, prejudice, minority stress, SF-36
A growing body of literature has demonstrated worse mental and physical health outcomes among sexual minority (e.g., lesbian, gay, bisexual) adults compared to heterosexual adults, with bisexuals at the greatest risk for poor health. Specifically, bisexuals are at greater risk than heterosexuals of depression, obesity, and impairments in functioning due to pain (Bostwick, Hughes, & Everett, 2015; Case et al., 2004; Cochran & Mays, 2007; Conron, Mimiaga, & Landers, 2010). Minority stress theory proposes that sexual minorities experience prejudice and discrimination related to their stigmatized identity, which negatively affects health via a psychological stress response pathway (Brooks, 1981; Hatzenbuehler, 2009; Meyer, 1995, 2003). Bisexuals may experience unique prejudice related to bisexuality (i.e., bisexual-specific minority stress) (Bradford, 2004; Brewster & Moradi, 2010; Friedman et al., 2014; Mohr & Rochlen, 1999; Mulick & Wright, 2002; Ochs, 1996). Although some research has found evidence for negative effects of sexual minority stress on health among sexual minorities (Frost, Lehavot, & Meyer, 2015; Mereish & Poteat, 2015), few studies have examined how bisexual-specific minority stress affects health among bisexuals. In addition, previous research on bisexual-specific minority stress has been limited to cisgender (non-transgender) individuals. This research examined associations of bisexual-specific minority stress and physical health among cisgender and transgender adults with bisexual orientation, and tested for gender differences.
Sexual orientation can be defined as a multidimensional construct including sexual orientation identity, romantic and sexual attractions, and sex/gender of sexual partners (Institute of Medicine, 2011). Similarly, bisexuality can be defined and measured based on multiple dimensions: bisexual identity, attractions to more than one gender, and having sexual partners of more than one sex/gender (Mereish, Katz-Wise, & Woulfe, 2016). Sexual orientation dimensions may not be consistent within an individual person; for example, a woman may have attractions to more than one gender (bisexual orientation based on attractions), but identify as lesbian. Data from a 2009 national probability sample of U.S. adults ages 18 to 70 years found that 3.6% of women and 2.6% of men identified their sexual orientation as bisexual, with more women and men reporting past sexual partners of more than one gender (bisexual orientation based on sexual partners) than identifying as bisexual (Herbenick et al., 2010b). In the current study, bisexual orientation was defined based on both bisexual identity and attractions to more than one gender. Among sexual minorities, more individuals identify as bisexual than as lesbian or gay (Herbenick et al., 2010a), but the majority of research on sexual minority health has focused on the experiences of lesbian and gay individuals rather than bisexuals. Research is needed that specifically examines health-related experiences among individuals with bisexual orientation.
Previous research has demonstrated that when sexual minorities are compared to heterosexuals, bisexuals have the most adverse physical health outcomes, with bisexual women at even greater risk than bisexual men for poor health (Bostwick et al., 2015; Case et al., 2004; Cochran & Mays, 2007; Conron et al., 2010). A study using data from the California Quality of Life Survey found numerous sexual orientation group differences in health, with sexual minorities generally reporting worse health outcomes than heterosexuals (Cochran & Mays, 2007). Greater sexual orientation health disparities were found among “homosexually experienced heterosexual” women and men (heterosexually-identified with a history of same-gender sexual partners; i.e., bisexual orientation based on sexual partners) and bisexually-identified women compared to heterosexual women and men. For instance, compared to heterosexual women, bisexual women were more likely to report digestive complaints, back problems, and chronic fatigue syndrome (Cochran & Mays, 2007). A study of sexual orientation and gender differences in health using multiple waves of data from the Massachusetts Behavioral Risk Factor Surveillance found similar results, with bisexuals reporting poorer health than heterosexual and lesbian/gay respondents (Conron et al., 2010). Finally, a study using data from the Nurses’ Health Study II found that compared with heterosexual women, bisexual women reported impairment in functioning due to pain (assessed with the SF-36) and had a lower perception of their overall health (Case et al., 2004). Although these health disparities have been established, more research is needed to understand factors associated with bisexual individuals’ physical health while also considering gender differences.
Minority stress theory has been used to conceptualize sexual orientation health disparities. This theory proposes that experiences of prejudice and discrimination based on sexual minority status (i.e., “sexual minority stress,” such as heterosexist harassment, discrimination, or rejection (Szymanski, 2006)) and internalization of heterosexist stigma adversely affect physical and mental health via a psychological stress response pathway (Brooks, 1981; Hatzenbuehler, 2009; Meyer, 1995, 2003). Indeed, recent research among sexual minorities found that sexual minority stress was associated with physical health problems (Frost et al., 2013), including distressing physical symptoms (Mereish & Poteat, 2015). However, these two studies did not report results specifically for individuals with bisexual orientation or examine bisexual-specific minority stress.
Under the purview of a sexual minority stress framework, particularly in terms of experiences of prejudice and discrimination, bisexuals may experience a unique form of prejudice related to their bisexual orientation, termed “biphobia” (Bradford, 2004; Ochs, 1996) or “anti-bisexual prejudice” (Mohr & Rochlen, 1999). In this paper, the term “bisexual-specific minority stress” is synonymous with other terms used to describe prejudice and stigma related to bisexual orientation. Individuals with bisexual orientation based on identity (identifying as bisexual) and bisexual orientation based on other sexual orientation dimensions (e.g., having multiple gender attractions or sexual partners of multiple genders) may experience this unique type of prejudice. Anti-bisexual prejudice is thought to have two underlying dimensions: the perception of bisexuality as an unstable and illegitimate sexual orientation, and hostility toward bisexuality and bisexual persons (Mohr & Rochlen, 1999). Previous research on anti-bisexual prejudice has found that bisexual individuals experience this type of prejudice from both heterosexuals and other sexual minorities (Brewster & Moradi, 2010; Mulick & Wright, 2002).
Bisexual-specific minority stress occurs within a societal context of stigma related to bisexuality. Research on attitudes toward bisexual individuals has found that both heterosexual and lesbian and gay individuals hold negative attitudes toward bisexual individuals (de Bruin & Arndt, 2010; Herek, 2002; Yost & Thomas, 2012), and that bisexual men are perceived more negatively than bisexual women (Eliason, 2001; Yost & Thomas, 2012). A recent study illustrated the extent of negative attitudes toward bisexual individuals, finding that heterosexuals and lesbians and gay men were less willing to be romantic or sexual with bisexual partners than were bisexual individuals (Feinstein, Dyar, Bhatia, Latack, & Davila, 2014). Some research has found that bisexuals report experiencing more victimization (e.g., physical violence, sexual victimization) than lesbians and gay men (Hequembourg, Livingston, & Parks, 2013; Katz-Wise & Hyde, 2012), although other research has found the opposite pattern (Baams, Grossman, & Russell, 2015; Ybarra, Mitchell, Kosciw, & Korchmaros, 2015). Although research on bisexual-specific minority stress is growing, no studies have examined whether this type of minority stress may affect the health of individuals with bisexual orientation independently from sexual minority stress.
Another limitation of the extant anti-bisexual research is its limited focus on cisgender individuals. Cisgender refers to individuals for whom their current gender identity matches their sex assigned at birth, whereas transgender refers to individuals who identify with a different gender from their sex assigned at birth. Some transgender individuals identify with binary (woman, man) gender identities, such as transmasculine spectrum (assigned female at birth and now identify as men or transgender/trans men) and transfeminine spectrum (assigned male at birth and now identify as women or transgender/trans women), whereas other transgender individuals use identity labels that reflect non-binary gender identities, such genderqueer or agender. Research on sexual orientation identities among transgender individuals has found that many transgender individuals use labels that reflect sexual orientation toward more than one gender, such as bisexual and queer (Katz-Wise, Reisner, Hughto, & Keo-Meier, 2016). Transgender individuals also report substantial prejudice and discrimination related to their transgender identity (Grant et al., 2011), which has been explained using a minority stress framework (Hendricks & Testa, 2012).
Research with transgender individuals has not often considered the unique experiences of transgender individuals who also have a bisexual orientation. Alexander and Yescavage (2003) identified a number of intersections between transgender and bisexual individuals’ experiences: 1) marginalization within the lesbian, gay, bisexual, and transgender (LGBT) community; 2) perceptions that bisexual and transgender individuals are unwilling to commit to one sexual orientation or gender identity; 3) perceptions of bisexuality and transgender as impermanent; and 4) expectations for disclosure by bisexual and transgender individuals of both past and present genders and partners’ genders. These intersections may also be experienced within individuals who are both transgender and bisexual. Considering the prevalence of stigma related to transgender identity (Grant et al., 2011), transgender individuals with a bisexual orientation may be more likely to experience negative health affects related to bisexual-specific minority stress than cisgender individuals with a bisexual orientation. To our knowledge, this is the first study to examine bisexual-specific minority stress among transgender individuals and associations with physical health.
The aim of the current study was to examine associations of bisexual-specific minority stress (specifically, anti-bisexual prejudice) and physical health among cisgender and transgender adults with bisexual orientation. We hypothesized that greater bisexual-specific minority stress would be associated with poor physical health above and beyond sexual minority stress (specifically, heterosexist harassment and rejection). Considering that bisexual women are at the greatest risk for poor health compared to other sexual minorities (Bostwick et al., 2015; Case et al., 2004; Cochran & Mays, 2007; Conron et al., 2010) and that transgender individuals experience substantial stigma related to their transgender identity (Grant et al., 2011) and also have poor health outcomes compared to cisgender individuals (Institute of Medicine, 2011), we hypothesized that gender would moderate the associations between bisexual-specific minority stress and health. Specifically, we hypothesized that women and transgender individuals will have the strongest association between bisexual-specific minority stress and health.
Method
Participants
Participants were from an online sample of 488 adults (378 cisgender women, 49 cisgender men, and 61 transgender individuals), age 18–66 years (M = 28.44; SD = 9.68). The sample was primarily White (80.3%) and low income (annual income ≤ $19,999; 55.9%), with 38.1% students. Most of the participants identified as bisexual (73.3%); participants who were not bisexually-identified endorsed attraction to multiple genders. Detailed participant demographic information is presented in Table 1.
Table 1.
Sociodemographic Characteristics of Adults with Bisexual Orientation (N = 488)
| Measures | Total Sample |
|---|---|
|
M (SD) |
|
| Age | 28.44 (9.68) |
|
% (n) |
|
| Gender Identity | |
| Cisgender women | 77.5 (378) |
| Cisgender men | 10.0 (49) |
| Transgender, binary | 3.1 (15) |
| Transgender, non-binary/other | 9.4 (46) |
| Race/Ethnicity | |
| Asian/Pacific Islander | 2.7 (13) |
| Black or African American | 2.5 (12) |
| Hispanic/Latina/o | 3.7 (18) |
| Middle Eastern/Arab American | 0.8 (4) |
| Native American/American Indian/Alaska Native | 0.4 (2) |
| White (non-Hispanic) | 80.3 (392) |
| Biracial or Multi-racial | 8.2 (40) |
| Other | 1.4 (7) |
| Education | |
| High school degree/GED or less | 34.0 (166) |
| College degree | 38.5 (188) |
| Graduate degree | 27.5 (134) |
| Employment | |
| Full-time | 33.8 (165) |
| Part-time | 11.7 (57) |
| Student | 38.1 (186) |
| Unemployed | 10.5 (51) |
| Other | 5.9 (29) |
| Individual Income | |
| ≤ $9,999 | 42.2 (206) |
| $10,000 to $19,999 | 13.7 (67) |
| $20,000 to $29,999 | 13.1 (64) |
| $30,000 to $49,999 | 12.5 (61) |
| $50,000 to $69,999 | 8.0 (39) |
| ≥ $70,000 | 9.0 (44) |
| Geographical Region | |
| Northeastern U.S. | 23.8 (116) |
| Midwestern U.S. | 17.4 (85) |
| Northwestern U.S. | 3.5 (17) |
| Southern U.S. | 9.0 (44) |
| Southwestern U.S. | 6.8 (33) |
| Western U.S. | 10.5 (51) |
| Other U.S. Territory | 0.2 (1) |
| International/non-U.S. Territory | 28.7 (140) |
Measures
Bisexual-specific minority stress.
Bisexual-specific minority stress was assessed using the Anti-Bisexual Experiences Scale (ABES) (Brewster & Moradi, 2010), which measured anti-bisexual prejudice from heterosexual people (ABES-H; 17-items) and from lesbian/gay people (ABES-LG; 17-items). Sample items are “When I have disclosed my sexual orientation to others, they have continued to assume that I am really heterosexual or gay/lesbian” and “People have treated me as if I am likely to have an STD/HIV because I identify as bisexual.” Response options are on a 6-point scale, ranging from 1 (never) to 6 (almost all of the time). For this study, the Cronbach alpha reliability coefficients for the ABES-H and ABES-LG scales were 0.95 and 0.97, respectively. Given the high correlation between the two subscales (r = .84, p < .01), a total scale score was computed to assess overall bisexual-specific minority stress, as conducted in prior research (Brewster, Moradi, Deblaere, & Velez, 2013).
Sexual minority stress.
Sexual minority stress was assessed using the 7-item Harassment and Rejection subscale of the Heterosexist Harassment, Rejection, and Discrimination Scale (HHRDS) (Szymanski, 2006), which measured the frequency with which participants experienced sexual minority prejudice in the past year. Sample items are “How many times have you been called a heterosexist name?” and “How many times have you been verbally insulted because of you are a lesbian/gay/bisexual person?” Item response options are on a 6-point frequency scale, ranging from 1 (the event has never happened to you) to 6 (the event happened almost all the time [more than 70% of the time]). The scale’s psychometric properties were examined and validated with sexual minority samples, and high alpha reliability coefficients were found in previous samples of sexual minorities (Lehavot & Simoni, 2011; Szymanski & Sung, 2010; Szymanski, 2006). For this study, the Cronbach alpha reliability was 0.85.
Physical health.
Four dimensions of physical health were assessed with the Medical Outcomes Study Short Form Health Survey (SF-36) (McHorney, Ware, & Raczek, 1993): physical functioning, role limitation due to physical health, pain, and overall general health. The standardized scoring protocol for the SF-36 was used to compute scores for the subscales (McHorney et al., 1993), ranging from 0 to 100. With the exception of the general health subscale, the other subscales are a measure of the absence of disability, with a score of 100 indicating no disability is endorsed; i.e., higher scores indicate better health. The general health subscale assesses both positive and negative health, with a score of 100 indicating good health. We also computed a total score of physical health; with higher scores indicating positive self-perceived health. For this investigation, the Cronbach alpha reliability coefficients were physical functioning (α = 0.89), role limitation due to physical health (α = 0.84), pain (α = 0.83), and overall general health (α = 0.81).
Sociodemographic characteristics.
Participants’ gender identity was assessed with the following response options: male/man; female/woman; transgender; and other. Some participants selected other and indicated that their gender identity is non-binary (e.g., agender, gender fluid, non-binary). Assigned sex at birth was not assessed. Three dimensions of sexual orientation were assessed: sexual orientation identity (“How would you describe your sexual orientation?”), sexual attractions (“People are different in their sexual attraction to other people. Which best describes your feelings?”), and sexual behaviors in the past year (“During the past year, which whom have you had sex?”) and lifetime (“With whom have you had sex in your lifetime?”). Participants’ age (in years), race/ethnicity, education, employment, annual individual income, and geographical region were also assessed. The specific categories for sociodemographic characteristic are listed in Tables 1 and 2.
Table 2.
Sexual Orientation Dimensions by Gender Identity Among Adults with Bisexual Orientation (N = 488)
| Measures | Cisgender Women | Cisgender Men | Transgender Individuals | Total Sample |
|---|---|---|---|---|
| Sexual Orientation Identity | ||||
| Bisexual | 74.5 (280) | 79.6 (39) | 61.3 (38) | 73.2 (357) |
| Gay | 0.3 (1) | 2 (1) | 0 (0) | 0.8 (4) |
| Lesbian | 0.5 (2) | 0 (0) | 0 (0) | |
| Heterosexual/straight | 0.8 (3) | 6.1 (3) | 0 (0) | 1.2 (6) |
| Queer | 17.3 (65) | 4.1 (2) | 27.4 (17) | 17.2 (84) |
| Pansexual | 2.7 (10) | 2 (1) | 9.7 (6) | 3.5 (17) |
| Other | 4 (15) | 6.1 (3) | 1.6 (1) | 3.9 (19) |
| Past year sex partners | ||||
| Men only | 33.2 (125) | 12.2 (6) | 29 (18) | 30.5 (149) |
| Women only | 9.8 (37) | 30.6 (15) | 12.9 (8) | 12.3 (60) |
| Transgender and/or genderqueer individuals only | 2.1 (8) | 0 (0) | 8.1 (5) | 2.7 (13) |
| Men and women only | 17.2 (65) | 22.4 (11) | 4.8 (3) | 16.2 (79) |
| Men, women, transgender, and/or genderqueer | 8.5 (32) | 14.3 (7) | 19.4 (12) | 10.5 (51) |
| Did not have sex during the past year | 29.2 (110) | 20.4 (10) | 25.8 (16) | 27.9 (136) |
| Lifetime sex partners | ||||
| Men only | 12.2 (46) | 10.2 (5) | 17.7 (11) | 12.7 (62) |
| Women only | 3.2 (12) | 12.2 (6) | 1.6 (1) | 3.9 (19) |
| Transgender and/or genderqueer individuals only | 0.5 (2) | 0 (0) | 0 (0) | 0.4 (2) |
| Men and women only | 41.1 (155) | 34.7 (17) | 16.1 (10) | 37.3 (182) |
| Men, women, transgender, and/or genderqueer | 26.5 (100) | 32.7 (16) | 56.6 (35) | 30.9 (151) |
| Did not have sex in lifetime | 16.4 (62) | 10.2 (5) | 8.1 (5) | 14.8 (72) |
| Sexual Attraction | ||||
| Only attracted to men/trans men | 0.3 (1) | 0 (0) | 0 (0) | 0.2 (1) |
| Mostly attracted to men/trans men | 15.6 (59) | 14.3 (7) | 6.5 (4) | 14.3 (70) |
| Equally attracted to men/trans men and women/trans women | 51.2 (193) | 36.7 (18) | 43.5 (27) | 48.8 (238) |
| Mostly attracted to women/trans women | 19.4 (73) | 30.6 (15) | 16.1 (10) | 20.1 (98) |
| Only attracted to women/trans women | 0 (0) | 4.1 (2) | 0 (0) | 0.4 (2) |
| Not sure | 5 (19) | 8.2 (4) | 4.8 (3) | 5.3 (26) |
| Other | 8.5 (32) | 6.1 (3) | 29 (18) | 10.9 (53) |
Procedure
A sample of adults with bisexual orientation was recruited. Inclusion criteria were age 18 years or older and identifying as bisexual or having attractions to more than one gender. Participants were recruited using web-based community sampling by contacting sexual minority and bisexual-specific online groups and listservs. Internet recruitment of participants has been identified as a successful and common method to reach sexual minority populations that have been previously overlooked (Moradi, Mohr, Worthington, & Fassinger, 2009). All potential participants received a link to the data collection website, on which they provided informed consent, completed an online survey, and had the option of being entered into a raffle to win one of five $25 prizes as a monetary incentive for their participation. At the end of the survey, participants were presented with a list of online resources providing sexual minority-specific mental health support and services. The study was approved by the researchers’ Institutional Review Board.
An initial 961 participants clicked the survey link or initiated the online survey. Of those participants, 548 were removed for terminating their participation in the online survey prematurely or having stopped taking the survey all together prior to completing any of the items of the main measures of the study (i.e., 234 were removed for not having any data for the SF-36 scale, 138 for the ABES scales, and 56 for the HHRDS scale). This data cleaning procedure and the degree of missingness is consistent with prior online studies of sexual minorities (Brewster et al., 2013). An additional 45 participants were removed for not providing data for age, resulting in a final sample of 488 participants. Of the 488 participants included in this study, some had missing data on the item level; however, no item had 1.8% item-level missingness or more, which is considered a very small amount of missingness (Parent, 2012). We conducted available item analysis procedures to address these missing data points, which is recommended over mean substitution and performs equally to multiple imputation procedures (Parent, 2012). Internet Provider (IP) addresses were reviewed and cases from repeated IP addresses were removed to ensure data quality.
Analytic Method
We conducted a MANOVA to test for gender differences on the study measures. To reduce the inflation of a Type 1 error, we utilized a Bonferroni adjustment of the alpha value for follow-up ANOVAs. Effect sizes were calculated using Cohen’s d. We conducted five hierarchical linear regression analyses to examine the effects of bisexual-specific minority stress on physical health outcomes. We accounted for age, gender, education, income, and race/ethnicity on the first step of each regression model, entered sexual minority stress on the second step, and entered bisexual-specific minority stress on the third step. The criterion variables were each of the four physical health subscale scores and a total physical health score.
We then conducted a series of hierarchical linear regression analyses to test the moderating effects of gender on the associations of bisexual-specific minority stress and the physical health outcomes. To test for the moderating effects of gender, we created three sets of gender dummy variables to allow for examination of all possible comparisons: cisgender women vs. cisgender men; cisgender women vs. transgender individuals; and cisgender men vs. transgender individuals; each was coded as 0 and 1, respectively. We followed the commonly used procedures for testing moderation (Aiken & West, 1991). We standardized the bisexual-specific minority stress variable to reduce the effects of multicolinearity. We accounted for age, education, income, and race/ethnicity, and sexual minority stress, and entered these variables on Step 1. We entered the main effects on Step 2 (i.e., bisexual-specific minority stress and respective gender dummy variable), the two-way interactions of bisexual-specific minority stress and the respective gender comparison on Step 3. To aid in the interpretation of the two-way moderating effect, we computed simple slope regressions (Aiken & West, 1991). We split participants based on their gender identification (cisgender women vs. transgender individuals).
Results
Sociodemographic characteristics are reported in Table 1. Sexual orientation dimensions are reported by gender identity in Table 2. Correlations among the measures are reported in Table 3. Descriptive statistics of all measures are reported in Table 3. Scores for overall physical health ranged from 50.97 for transgender individuals to 66.20 for cisgender men (Table 4). Results from linear regression analyses are reported in Table 5, and moderation results are in Table 6.
Table 3.
Correlations Between the Measures Among Adults with Bisexual Orientation
| Full Sample | 1 | 2 | 3 |
|---|---|---|---|
| 1. Bisexual-specific minority stress | --- | ||
| 2. Sexual minority stress | .59* | --- | |
| 3. Overall physical health (total scale) | −.25* | −.21* | --- |
| Cisgender Women | 1 | 2 | 3 |
| 1. Bisexual-specific minority stress | --- | ||
| 2. Sexual minority stress | .60** | --- | |
| 3. Overall physical health (total scale) | −.20** | −.16** | --- |
| Cisgender Men | 1 | 2 | 3 |
| 1. Bisexual-specific minority stress | --- | ||
| 2. Sexual minority stress | .32* | --- | |
| 3. Overall physical health (total scale) | −.13 | −.26 | --- |
| Transgender Individuals | 1 | 2 | 3 |
| 1. Bisexual-specific minority stress | --- | ||
| 2. Sexual minority stress | .65* | --- | |
| 3. Overall physical health (total scale) | −.43* | −.22* | --- |
p < 0.05
p < 0.01
Table 4.
Descriptive Statistics for All Measures among Adults with Bisexual Orientation
| Measures | Total Sample | Cisgender Women (n = 377) | Cisgender Men (n = 49) | Transgender Individuals (n = 62) | Gender Differences | EffectSize | Result |
|---|---|---|---|---|---|---|---|
| Predictors | M (SD) | M (SD) | M (SD) | M (SD) | p-value | Cohen’s d | |
| Bisexual-specific minority stress | 2.63 (1.09) | 2.65 (1.11) | 2.18 (0.85) | 2.83 (1.11) | .01 | .30 | CM<CW, T |
| Sexual minority stress | 1.73 (0.77) | 1.70 (0.73) | 1.57 (0.59) | 2.07 (1.01) | .001 | .36 | CW, CM<T |
| Outcomes | |||||||
| Overall physical health (total scale) | 73.15 (18.97) | 73.96 (18.17) | 79.85 (15.86) | 62.91 (22.34) | .000 | .46 | T<CW, CM |
| Physical functioning | 87.51 (17.40) | 88.37 (16.41) | 92.24 (13.77) | 78.58 (22.45) | .000 | .42 | T<CW, CM |
| Role limitation due to physical health | 74.08 (35.47) | 75.60 (34.44) | 82.14 (32.27) | 58.47 (39.97) | .000 | .36 | T<CW, CM |
| Pain | 71.68 (20.27) | 72.11 (19.49) | 78.57 (19.95) | 63.63 (22.86) | .001 | .36 | T<CW, CM |
| General health | 59.33 (21.80) | 59.78 (20.99) | 66.23 (19.15) | 50.97 (26.03) | .000 | .35 | T<CW, CM |
Note. The range for the predictors was 1-6; the range for the outcomes was 0–100. CW = cisgender women; CM = cisgender men; T = transgender individuals.
Table 5.
Results from Linear Regression Analyses with Bisexual-Specific Minority Stress Predicting Health Outcomes Among Adults with Bisexual Orientation
| Overall Physical Health (Total Scale) | Physical Functioning | Role Limitations due to Physical Health | Pain | General Health | |
|---|---|---|---|---|---|
| Models | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) |
| Step 1 | |||||
| Age | −.32 (0.11)*** | −.33 (0.10)*** | −.28 (0.21)*** | −.30 (0.12)*** | −.13 (0.13)* |
| Gender | −.19 (1.18)*** | −.20 (1.06)*** | −.15 (2.24)** | −.16 (1.27)** | −.12 (1.39)* |
| Education | .09 (1.26) | .11 (1.14)* | .03 (2.39) | .07 (1.36) | .10 (1.49) |
| Income | .21 (0.59)*** | .15 (0.54)* | .18 (1.24)** | .17 (0.64)** | .15 (0.70)* |
| Race | .00 (0.51) | .03 (0.46) | .02 (0.97) | .01 (0.55) | −.05 (0.60) |
| R2= .10 | R2= .10 | R2= .07 | R2= .08 | R2= .05 | |
| Step 2 | |||||
| Sexual minority stress | −.21 (1.09)*** | −.10 (1.00)* | −.16 (2.09)* | −.18 (1.19)*** | −.21 (1.29)*** |
| R2= .14 | R2= .11 | R2= .10 | R2= .11 | R2= .09 | |
| Δ R2 = .04** | Δ R2 = .01* | Δ R2 = .02** | Δ R2 = .03** | Δ R2 = .04** | |
| Step 3 | |||||
| Sexual minority stress | −.11 (1.37) | −.06 (1.27) | −.12 (2.64)* | −.08 (1.49) | −.06 (1.60) |
| Bisexual-specific minority stress | −.16 (0.95)** | −.07 (0.88) | −.07 (1.83) | −.16 (1.03)** | −.25 (1.11)*** |
| Δ R2 = .02** | Δ R2 = .003 | Δ R2 = .003 | Δ R2 = .02** | Δ R2 = .04*** | |
Note. Δ R2 = change in percent variance accounted for between Steps 2 and 3. β = standardized beta coefficient; SE = standardized error.
p < 0.05
p < 0.01
p < .001
Table 6.
Results from Analyses to Test for Moderation by Gender Among Adults with Bisexual Orientation
| Overall Physical Health (Total Scale) | Physical Functioning | Role Limitation due to Physical Health | Pain | General Health | |
|---|---|---|---|---|---|
| Models | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) |
| Step 1 – Covariates | |||||
| Age | −.34 (0.12)*** | −.34 (0.11)*** | −.29 (.22)*** | −.33 (.12)*** | −.15 (0.14)** |
| Education | .10 (1.34) | .13 (1.26)* | .02 (2.54) | .09 (1.42) | .12 (1.57)* |
| Income | .15 (0.64)* | .11 (0.61)+ | .14 (1.22)* | .11 (0.68) | .10 (0.75) |
| Race | .00 (0.55) | .02 (0.52) | −.01 (1.04) | .03 (.58) | −.04 (0.65) |
| Sexual minority stress | −.22 (1.14)*** | −.07 (1.21)* | −.18 (2.17)*** | −.20 (1.21)*** | −.21 (1.34)*** |
| Step 2 – Main Effects | |||||
| Bisexual-specific minority stress | −.17 (1.00)** | −.08 (0.95) | −.06 (1.93) | −.16 (1.07)** | −.28 (1.17)*** |
| Cisgender women vs. transgender | −.18 (2.48)*** | −.19 (2.35)*** | −.16 (4.77)** | −.13 (2.66)** | −.11 (2.91)* |
| Step 3 – Interaction | |||||
| Bisexual-specific minority stress x gender | −.30 (2.22)* | −.12 (2.12) | −.35 (4.27)** | −.16 (2.39) | −.24 (2.61)+ |
| R2 = .18 | R2 = .12 | R2 = .12 | R2 = .13 | R2 = .14 | |
Note. β = standardized beta coefficient; SE = standardized error. Cisgender women were coded as 0 and transgender individuals were coded as 1. Bisexual-specific minority stress was centered in the moderation analyses.
p = 0.06;
p < 0.05;
p < 0.01;
p < .001;
Gender Differences
Results of analyses to test for gender differences indicated that there was a significant effect for gender, Wilks’s Λ = .91, F (12, 960) = 3.87, p < .001, = .05. Follow-up ANOVAs revealed significant gender differences on all the measures (Table 4). Cisgender men reported less bisexual-specific minority stress than cisgender women and transgender individuals. Cisgender women and men reported less sexual minority stress than transgender individuals. Significant gender differences were also found for all physical health outcomes, with transgender individuals reporting lower physical health scores than cisgender women and cisgender men. Effect sizes for significant differences ranged from small to medium (Table 4).
Effects of Bisexual-Specific Minority Stress on Physical Health
Correlations among the measures for each gender group and the total sample are reported in Table 3. Results of analyses to test for associations between bisexual-specific minority stress and physical health indicated that all of the regression models were statistically significant: overall physical health (i.e., total physical health score): F (7, 473) = 12.54, p < .001; physical functioning: F (7, 487) = 8.6, p < .001; role limitations: F (7, 473) = 8.56, p < .001; pain: F (7, 473) = 9.58, p < .001; and general health: F (7, 473) = 9.86, p < .001. When accounting for demographic variables and sexual minority stress, bisexual-specific minority stress uniquely predicted some of the physical health measures over and above sexual minority stress, as indicated by the significant change in r-squared (Table 3). Specifically, bisexual-specific minority stress significantly predicted overall physical health (β = −.16, p < .01; Δ R2 = .02), pain (β = −.16, p < .01; Δ R2 = .02), and general health (β = −.25, p < .001; Δ R2 = .04; Table 5). Although bisexual-specific minority stress was significantly associated with these outcomes, the levels of additional explained variances due to bisexual-specific minority stress were between 2% to 4%.
Moderation Effect of Gender on Bisexual-Specific Minority Stress and Physical Health
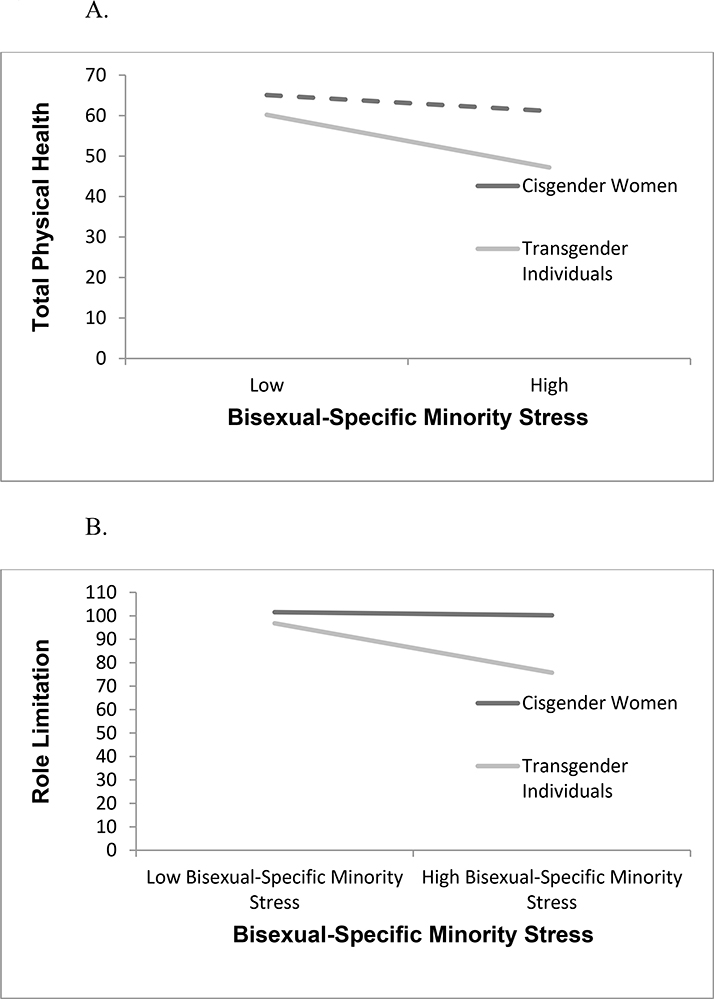
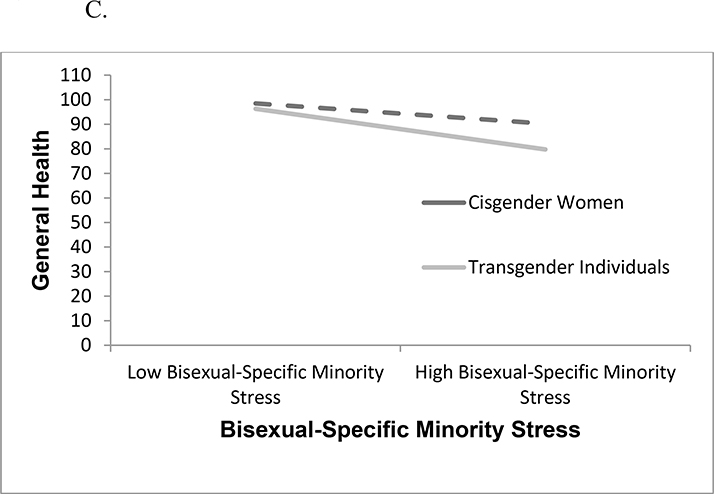
Results of analyses to test for overall gender differences indicated that neither the moderation effect comparing cisgender women vs. cisgender men nor the moderation effect comparing cisgender men vs. transgender individuals was significant in predicting any of the physical health outcomes. However, the moderating effect comparing cisgender women vs. transgender individuals was significant for two physical health outcomes: overall physical health: F (8, 433) = 11.25, p < .001 and role limitations: F (8, 433) = 7.46, p < .001; and marginally significant for general health: F (8, 433) = 8.30, p < .001. Given their statistical significance, the results for these moderating effects are presented in Table 6 and Figure 1A-1C.
Figure 1.
Results of analyses to test for specific gender differences indicated that bisexual-specific minority stress was associated with the total physical health score (β = −.46, p <.01) and role limitations (β = −.40, p <.05) for transgender individuals, but not for cisgender women. Bisexual-specific minority stress was associated with general health for both cisgender women (β = −.24, p <.001) and transgender individuals (β = −.47, p <.01).
Discussion
The focus of this study was to examine associations of bisexual-specific minority stress and physical health among cisgender and transgender adults with bisexual orientation and to test for gender differences in this association. Among adults with bisexual orientation in the current study, significant gender differences were found for all physical health outcomes, with transgender individuals reporting poorer health than cisgender women and cisgender men for all outcomes. Evidence from the growing body of literature on transgender health indicates that transgender individuals consistently report worse health outcomes than cisgender individuals (Institute of Medicine, 2011); findings from the current study are consistent with this research.
In the current study, greater bisexual-specific minority stress was associated with poorer health, which provides support for minority stress theory (Brooks, 1981; Hatzenbuehler, 2009; Meyer, 1995, 2003). This is consistent with previous research drawing a link between sexual minority stress and adverse physical health among sexual minorities (Mereish & Poteat, 2015). Findings from the current study provide further evidence for the utility of using minority stress theory to predict physical health outcomes in sexual minorities (Institute of Medicine, 2011) and transgender individuals (Hendricks & Testa, 2012). This study also indicates that this theory can be extended to understand the impact of bisexual-specific minority stress on the health of individuals with bisexual orientation. In addition, the current study moves the field forward in demonstrating that bisexual-specific minority stress is a distinct form of prejudice that may have a negative effect on bisexual health above and beyond experiences of sexual minority stress.
Previous research with sexual minorities has focused primarily on cisgender lesbian women and gay men. Although this has begun to change in recent years to include other sexual orientation groups, such as bisexual and mostly heterosexual, studies rarely include both transgender and cisgender individuals. In the current study, gender differences were found regarding the association between bisexual-specific minority stress and physical health. However, gender was found to moderate the association between bisexual-specific minority stress and health only for the comparison between cisgender women and transgender individuals. The adverse effects of bisexual-specific minority stress on health were stronger among transgender individuals than among cisgender women. These results could be understood from an intersectional framework, which emphasizes the way multiple social identities (e.g., gender, race, sexual orientation identity) intersect to construct individuals’ experiences – particularly with regard to their experiences within interlocking systems of privilege and oppression (Bowleg, 2012). Crenshaw’s (1991) foundational article on intersectionality, focused upon the way in which racism and sexism intersect to uniquely affect woman of color in ways that neither white women or men of color experience. Similarly, transgender individuals with bisexual orientation experience prejudice and discrimination based on both their transgender identity and their bisexual orientation, in addition to other identities and social positions, such as race/ethnicity or socioeconomic status. Further research must be done to better understand how macro level factors such as structural cissexism and biphobia may result in greater vulnerability to minority stress generally, as well as the possible association between this vulnerability and physical health outcomes.
In addition to health outcomes, transgender individuals were at the greatest risk for experiencing bisexual-specific minority stress and sexual minority stress, compared to cisgender women and men. A national U.S. survey of transgender adults found that experiences of prejudice and discrimination were substantial and across numerous environments, including school, employment, housing, public accommodations, health care, family, and police interactions (Grant et al., 2011). Findings from the current study suggest that transgender individuals with bisexual orientation may be experiencing additional prejudice based on their sexual orientation identity. To our knowledge this is the first study of bisexual health to include transgender individuals and to examine this group separately in analyses. Future research, particularly qualitative research on the lived experiences of transgender individuals with bisexual orientation, may provide further insight into the finding that transgender individuals are at greater risk than cisgender individuals for bisexual-specific minority stress and sexual minority stress.
In addition to transgender individuals, cisgender women also experienced bisexual-specific minority stress than cisgender men. This was surprising in light of previous research demonstrating that attitudes toward bisexual men tend to be more negative than attitudes toward bisexual women, particularly when evaluated by heterosexual men (Eliason, 2001; Herek, 2002). From a minority stress perspective, bisexual men may be expected to have poorer outcomes than bisexual women, but previous research has found that among sexual minorities, bisexual women have the poorest health compared to other sexual minority subgroups for many outcomes (Bostwick et al., 2015; Case et al., 2004; Cochran & Mays, 2007; Conron et al., 2010). Some studies have noted that although bisexuality is more “accepted” in women, often this acceptance takes the form of sexualizing bisexual women (Yost & Thomas, 2012), which may be considered part of the hypersexualization that bisexual individuals experience as part of the “sexual irresponsibility” dimension of anti-bisexual prejudice (Brewster & Moradi, 2010). Returning to an intersectionality framework, another possibility is that the intersections of structural sexism and anti-bisexual prejudice interact to create more vulnerability. For example, structural sexism, such as pay inequality may affect other protective factors such as SES that may buffer some experiences of anti-bisexual prejudice. As a whole, this pattern of results indicates that gendered experiences of bisexual-specific minority stress may be more complicated than originally thought and deserve further investigation.
Implications for Health Care Practice
Findings from this study have critical implications for practice. Health care providers should be aware that poor health among patients with bisexual orientation may be related to bisexual-specific minority stress, and that this unique form of prejudice may affect the health of bisexual individuals more so than other forms of sexual minority stress. To address and reduce health disparities for bisexual individuals, health care providers must focus on not only reducing homophobia and heterosexism in medical practice and systems, but specifically reducing bisexual-specific minority stress.
Previous literature has outlined some possible mechanisms of bisexual health disparities, including additional stress related to bisexual invisibility, in which individuals with bisexual orientation are assumed to be heterosexual or lesbian gay; actual and perceived anti-bisexual prejudice from medical providers, and less access to bisexual-specific resources that may affect health, such as sexual education that affirms bisexual experiences and bisexual-specific support groups (Ebin, 2012; Quinn et al., 2015). Health care providers can address these barriers in several ways. Providers can regularly inquire about patients’ sexual orientation and gender identity (SOGI) as part of routine care and use this information to initiate conversation about health risk-factors, such as exposure to bisexual-specific minority stress and depression (Cahill & Makadon, 2014). Providers can work to examine their own anti-bisexual prejudice and affirm bisexuality in patients by avoiding assumptions about their sexual orientation, such as assuming that patients with bisexual orientation are ‘really’ heterosexual or lesbian/gay, or equating sexual behavior with partners of multiple genders with bisexual identity. Providers can also be aware of unique health risks that do apply to bisexual individuals, such as bisexual women being at a higher likelihood for depression compared to heterosexual and lesbian women (Bostwick et al., 2015; Case et al., 2004). Finally, providers can be aware of and refer patients to, bisexual-specific specialty care that may in turn promote health, such as sexual education that affirms bisexual experiences and bisexual-specific support groups (Ebin, 2012; Quinn et al., 2015).
Study Limitations
While making important contributions to existing literature, this study had several limitations related to design and sampling. This study used a cross-sectional design; consequently, we cannot assume causality. Although the findings suggest that exposure to bisexual-specific minority stress leads to poorer physical health outcomes, it is also possible that those with poorer physical health are in turn exposed to more bisexual-specific minority stress. Further, a third unmeasured variable could be related to both bisexual-specific minority stress and poor physical health outcomes. Future research could examine the temporality of these associations using a longitudinal study design.
This study also has limited representation of racial/ethnic, gender, and socioeconomic diversity. The majority (80.5%) of the sample was White and there was a relatively small sample size (12.1%) of transgender participants. In addition, we had unequal sample sizes across gender groups, and the sample of cisgender men may have been underpowered to detect significant differences. In particular, the small sample sizes for binary vs. non-binary transgender individuals necessitated combining these two groups, which likely obscured important distinctions between them. Thus, the generalizability of these findings to other transgender individuals and race/ethnicities is limited. Further, the sampling strategy involved reaching out to LGBTQ-specific listservs, which limited the sample to participants who identify themselves as members of the LGBTQ community. This may limit generalizability to those participants whose attractions or behavior might include them in the bisexual community, but who do not identify as such. The choice to recruit participants online may have contributed to a less racial/ethnically diverse sample (Scheim, Bauer and Colman, 2015). Further, researcher-driven studies such as this one may have less success engaging with communities, including the transgender community and communities of color, that have historical legacies of research-related violence (Martin & Meezan, 2003). Given the history of exploitative research in transgender and communities of color (Martin & Meezan, 2003), research methodologies that emphasize transparency and community participation in various aspects of the research process (e.g., community based participatory research; Minkler & Wallerstein, 2011) may be more successful at developing trust with, and participation in research endeavors.
Future research must continue to use the recommended recruitment strategies to reach out to LGBTQ people of color and transgender communities that were used by this research team (e.g., oversampling LGBTQ communities of color and transgender communities, reaching out to racial/ethnic minority- and transgender-specific online communities). Additional efforts should include adding more recruitment strategies to reach these communities (e.g., reaching out to racial/ethnic minority sites that are not LGBTQ specific and meeting administrators of online sites in more personal ways to create increased buy-in) and perhaps incorporating strategies from other research approaches from the participatory action research tradition (Minkler & Wallerstein, 2011), such as developing longer term research collaborations with organizations that serve these communities and collaborating with and developing ways to make the process and products of the research more accessible to these communities.
This study focused on bisexual-specific minority stress, and therefore did not assess other types of prejudice, such as anti-transgender prejudice or prejudice based on other social positions, such as race/ethnicity or socioeconomic status. Finally, this study did not specifically examine the mechanisms by which stigma affects physical health. Minority stress theory proposes that both distal (external) minority stressors and proximal (internal) minority stressor affect health (Meyer, 1995, 2003). The current study focused on exposure to distal sources of minority stress by assessing anti-bisexual prejudice. Further, recent research has explored how exposure to stigma-related stress may affect general psychological processes such as emotion regulation (Hatzenbuehler, 2009). Future research could expand upon these findings by examining both distal and proximal stressors, and general psychological processes that may be affected by chronic discrimination to better understand how bisexual-specific minority stress contributes to poor physical health outcomes.
Conclusions
Bisexual-specific minority stress was associated with poor physical health of adults with bisexual orientation above and beyond sexual minority stress. In addition, transgender individuals were at the greatest risk of bisexual-specific minority stress, sexual minority stress, and adverse physical health outcomes, compared to cisgender women and men. Health care providers should be aware that poor health among bisexual patients may be related to bisexual-specific minority stress. Addressing this distinct type of prejudice is necessary to improve the health and well-being of individuals with bisexual orientation.
Acknowledgments
We would like to thank the Sexual Orientation and Gender Identity and Expression (SOGIE) working group at Boston Children’s Hospital and the participants who contributed data to this study. Dr. Katz-Wise was supported in part by a grant from the National Institute of Child Health and Human Development (K99HD082340) and Dr. Mereish was supported in part by the National Institute on Drug Abuse (T32DA016184).
Contributor Information
Sabra L. Katz-Wise, Division of Adolescent/Young Adult Medicine, Boston Children’s Hospital and Department of Pediatrics, Harvard Medical School, Boston, MA
Ethan H. Mereish, Department of Health Studies, American University, Washington, DC
Julie Woulfe, Department of Counseling, Developmental, and Educational Psychology, Boston College, Boston, MA.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage Publications. [Google Scholar]
- Alexander J, Yescavage K (2003). Bisexuality and transgenderism: InterSEXions of the others. Journal of Bisexuality, 3, 1–23. doi:0.1300/J159v03n03_01 [Google Scholar]
- Baams L, Grossman AH, & Russell ST (2015). Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Developmental Psychology, 51, 688–696. doi:10.1037/a0038994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality – an important theoretical framework for public health. American Journal of Public Health, 102, 1267–73. doi:10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Hughes TL, & Everett B (2015). Health behavior, status, and outcomes among a community-based sample of lesbian and bisexual women. LGBT Health, 2, 121–126. doi:10.1089/lgbt.2014.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford M (2004). The bisexual experience: Living in a dichotomous culture. Journal of Bisexuality, 4, 7–23. doi:10.1300/J159v04n01 [Google Scholar]
- Brewster ME, & Moradi B (2010). Perceived experiences of anti-bisexual prejudice: Instrument development and evaluation. Journal of Counseling Psychology, 57, 451–468. doi:10.1037/a0021116 [DOI] [PubMed] [Google Scholar]
- Brewster ME, Moradi B, Deblaere C, & Velez BL (2013). Navigating the borderlands: the roles of minority stressors, bicultural self-efficacy, and cognitive flexibility in the mental health of bisexual individuals. Journal of Counseling Psychology, 60, 543–56. doi:10.1037/a0033224 [DOI] [PubMed] [Google Scholar]
- Brooks VR (1981). Minority stress and lesbian women. Lexington, MA: Lexington Books. [Google Scholar]
- Cahill S, & Makadon H (2014). Sexual orientation and gender Identity data collection in clinical settings and in electronic health records: A key to ending LGBT health disparities. LGBT Health, 1, 34–41. doi:10.1089/lgbt.2013.0001 [DOI] [PubMed] [Google Scholar]
- Case P, Austin SB, Hunter DJ, Manson JE, Malspeis S, Willett WC, & Spiegelman D (2004). Sexual orientation, health risk factors, and physical functioning in the Nurses’ Health Study II. Journal of Women’s Health, 13, 1033–1047. doi:10.1089/jwh.2004.13.1033 [DOI] [PubMed] [Google Scholar]
- Cochran SD, & Mays VM (2007). Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexual individuals: results from the California Quality of Life Survey. Journal of Public Health, 97, 2048–2055. doi:10.2105/AJPH.2006.087254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. doi:10.2105/AJPH.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 1241–1299. doi:10.2307/1229039 [Google Scholar]
- de Bruin K, & Arndt M (2010). Attitudes toward bisexual men and women in a university context: Relations with race, gender, knowing a bisexual man or woman and sexual orientation. Journal of Bisexuality, 10, 233–252. doi:10.1080/15299716.2010.500955 [Google Scholar]
- Ebin J (2012). Why bisexual health? Journal of Bisexuality, 12, 168–177. doi:10.1080/15299716.2012.674854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliason M (2001). The stigma facing bisexual men. Journal of Bisexuality, 1, 137–154. doi:10.1300/J159v01n02 [Google Scholar]
- Feinstein BA, Dyar C, Bhatia V, Latack JA, & Davila J (2014). Willingness to engage in romantic and sexual activities with bisexual partners: Gender and sexual orientation differences. Psychology of Sexual Orientation and Gender Diversity, 1, 255–262. doi:10.1037/sgd0000047 [Google Scholar]
- Friedman MR, Dodge B, Schick V, Herbenick D, Hubach RD, Bowling J, … Krier S (2014). From bias to bisexual health disparities: Attitudes toward bisexual men and women in the United States. LGBT Health, 2, 1–10. doi:10.1089/lgbt.2014.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, Lehavot K, & Meyer IH (2013). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 1–8. doi:10.1007/s10865-013-9523-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, & Keisling M (2011). Injustice at every turn: A report of the National Transgender Discrimination Survey. Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force. [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135, 707–730. doi:10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychology: Research and Practice, 43, 460–467. doi:10.1037/a0029597 [Google Scholar]
- Hequembourg AL, Livingston JA, & Parks KA (2013). Sexual victimizaton and associated risks among lesbian and bisexual women. Violence Against Women, 19, 634–657. doi:10.1177/1077801213490557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Schick V, Sanders S. a., Dodge B, & Fortenberry JD (2010a). An event-level analysis of the sexual characteristics and composition among adults ages 18 to 59: Results from a national probability sample in the United States. Journal of Sexual Medicine, 7, 346–361. doi:10.1111/j.1743-6109.2010.02020.x [DOI] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Schick V, Sanders S. a., Dodge B, & Fortenberry JD (2010b). Sexual behavior in the United States: Results from a national probability sample of men and women ages 14–94. Journal of Sexual Medicine, 7, 255–265. doi:10.1111/j.1743-6109.2010.02012.x [DOI] [PubMed] [Google Scholar]
- Herek GM (2002). Heterosexuals attitudes toward bisexual men and women in the United States. Journal of Sex Research, 39, 264–274. doi:10.1080/00224490209552150 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. The National Academies Press; Washington, DC. [PubMed] [Google Scholar]
- Katz-Wise SL, & Hyde JS (2012). Victimization experiences of lesbian, gay, and bisexual individuals: A meta-analysis. Journal of Sex Research, 49, 142–167. doi:10.1080/00224499.2011.637247 [DOI] [PubMed] [Google Scholar]
- Katz-Wise SL, Reisner SL, Hughto JW, & Keo-Meier CL (2015). Differences in sexual orientation diversity and sexual fluidity in attractions among gender minority adults in Massachusetts. Journal of Sex Research, 53, 74–84. doi:10.1080/00224499.2014.1003028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. doi:10.1037/a0022839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JI, & Meezan W (2003). Applying ethical standards to research and evaluations involving lesbian, gay, bisexual, and transgender populations. Journal of Gay & Lesbian Social Services, 15, 181–201. doi:10.1300/J041v15n01_12 [Google Scholar]
- McHorney CA, Ware JE, & Raczek AE (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31, 247–63. [DOI] [PubMed] [Google Scholar]
- Mereish EH, Katz-Wise SL, & Woulfe J (2016). We’re here and we’re queer: Sexual orientation and sexual fluidity differences between bisexual and queer women. Journal of Bisexuality. Advance online publication. doi:10.1080/15299716.2016.1217448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, & Poteat VP (2015). A relational model of sexual minority mental and physical health: The negative effects of shame on relationships, loneliness, and health. Journal of Counseling Psychology, 62, 425. doi:10.1037/cou0000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38–56. [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. doi:10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, & Wallerstein N (Eds.). (2011). Community-based participatory research for health: From process to outcomes. San Francisco, CA: John Wiley & Sons. [Google Scholar]
- Mohr JJ, & Rochlen AB (1999). Measuring attitudes regarding bisexuality in lesbian, gay male, and heterosexual populations. Journal of Counseling Psychology, 46, 353–369. doi:10.1037/0022-0167.46.3.353 [Google Scholar]
- Moradi B, Mohr JJ, Worthington RL, & Fassinger RE (2009). Counseling psychology research on sexual (orientation) minority issues: Conceptual and methodological challenges and opportunities. Journal of Counseling Psychology, 56, 5–22. [Google Scholar]
- Mulick PS, & Wright LW (2002). Examining the existence of biphobia in the heterosexual and homosexual populations. Journal of Bisexuality, 2, 45–64. doi:10.1300/J159v02n04_03 [Google Scholar]
- Ochs R (1996). Biphobia: It goes more than two ways In Firestein BA (Ed.), Bisexuality: The psychology and politics of an invisible minority (pp. 217–239). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Parent MC (2012). Handling item-level missing data: Simpler is just as good. The Counseling Psychologist, 41, 568–600. doi:10.1177/0011000012445176 [Google Scholar]
- Quinn GP, Sutton SK, Winfield B, Breen S, Canales J, Shetty G, … Schabath MB (2015). Lesbian, gay, bisexual, transgender, queer/questioning (LGBTQ) perceptions and health care experiences. Journal of Gay & Lesbian Social Services, 27, 246–261. doi:10.1080/10538720.2015.1022273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheim AI, Bauer GR, & Coleman TA (2015). Sociodemographic differences by survey mode in a respondent-driven sampling study of transgender people in Ontario, Canada. LGBT Health. doi:10.1089/lgbt.2015.004 [DOI] [PubMed] [Google Scholar]
- Szymanski DM (2006). Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles, 54, 227–234. doi:10.1007/s11199-006-9340-4 [Google Scholar]
- Szymanski DM, & Sung MR (2010). Minority stress and psychological distress among Asian American sexual minority persons. The Counseling Psychologist, 38, 848–872. doi:10.1177/0011000010366167 [Google Scholar]
- Ybarra ML, Mitchell KJ, Kosciw JG, & Korchmaros JD (2015). Understanding linkages between bullying and suicidal ideation in a national sample of LGB and heterosexual youth in the United States. Prevention Science, 16, 451–462. doi:10.1007/s11121-014-0510-2 [DOI] [PubMed] [Google Scholar]
- Yost MR, & Thomas GD (2012). Gender and binegativity: men’s and women’s attitudes toward male and female bisexuals. Archives of Sexual Behavior, 41, 691–702. doi:10.1007/s10508-011-9767-8 [DOI] [PubMed] [Google Scholar]