Abstract
Aim: To evaluate the impact of a stress management program on weight loss, depression, anxiety and stress as well as on the adoption of healthy lifestyle in adults with obesity. Methods: Adults with obesity who sought help for weight loss at a medical obesity clinic were consecutively enrolled in the study and were randomly assigned to the intervention or control group. All participants received standard instructions for a healthy lifestyle. The intervention group attended an 8-week stress management program that comprised diaphragmatic breathing, progressive muscle relaxation, guided visualization and instructions about healthy nutrition/dietary habits. Anthropometric parameters were assessed and several questionnaires were completed by all participants, at the beginning and at the end of the study. Results: A total of 45 adults (mean age±SD 45.7±10.55 years) with obesity were enrolled in the study; 22 in the intervention group and 23 in the control group. Participants in the two groups were matched for age and BMI. Participants in the intervention group achieved a significantly larger reduction in BMI compared to the control group (ΔBMI −3.1 vs. −1.74 kg/m2 respectively, P<0.001). In addition, they displayed ameliorated depression and anxiety scores and a reduction in the health locus of control based on chance.
Introduction
People in modern societies are subject to high levels of stress. Over the years several definitions have been used for stress. A key concept in attempting to define stress is homeostasis, the complex and dynamic balance which substantially contributes to the maintenance of life. From this perspective, stress can be defined as a status of threat or perceived threat to homeostasis, which is counterbalanced through a complex web of behavioral and physiological responses in order for the body to adapt. The response to stress is regulated by the stress system, which is localized in both the central nervous system and in peripheral organs. One of the main effects of stress is the increase of cortisol, therefore, high levels of saliva and blood cortisol are considered the best biological indicators of stress (Chrousos 2009, Nicolaides et al. 2015).
The stress that people face has been shown to cause physical, behavioral and psychological harm i.e. headaches, constipation, smoking, alcohol abuse, poor diet, sleep disturbances and obesity. Under stress people display a behavioral shift to a more westernized dietary pattern i.e. emotional overeating, overconsumption of high-fat, -salt, -sugar foods and less intake of fruits and vegetables (Chaplin & Smith 2011). This dietary pattern, in the context of a stressful lifestyle has led, among other factors, to the global increase in the prevalence of obesity. Stress related chronic cortisol hypersecretion favors fat storage in the abdominal region more than the hips (Daubenmier et al. 2011, Donoho et al. 2011, Speaker & Fleshner 2012). Abdominal (visceral) fat deposition, frequently termed as “toxic fat”, is associated with the development of cardiovascular disease, including coronary heart disease and ischemic stroke. Therefore, stress management could play an important role in weight loss, amelioration of body composition and prevention of various comorbidities.
Studies of the effects of stress management techniques in addition to dietary interventions for weight loss are scarce. Christaki et al. (2013) applied relaxation techniques in overweight and obese women for eight weeks with significant results on weight loss, but not on perceived stress levels. Furthermore, the progressive muscle relaxation technique for stress management has been associated with better compliance to a dietary program (Wynd 2006). Another study in obese Latinos found that the use of the stress management technique of guided visualization led to the adoption of healthy dietary choices (Weigensberg et al. 2003). Manzoni et al (Manzoni et al. 2009) observed that the application of a 3-week relaxation program decreased the levels of stress and depression and the need for emotional eating in a sample of women. In a more recent study (Stavrou et al. 2016), overweight and obese children and adolescents that underwent a stress-management intervention, demonstrated statistically significant weight loss and decrease in the levels of stress and depression, as well as in internalizing and externalizing problems.
The purpose of this study was to evaluate the impact of an 8-week stress management program, comprising diaphragmatic breathing, progressive muscle relaxation, guided visualization and instructions on healthy nutrition and dietary habits, on body weight, mental health and lifestyle indices of adults with obesity.
Materials and Methods
Setting
This randomized controlled study was conducted over a period of two years (from October 2014 to October 2016), at the outpatient Obesity Clinic of the Laiko General Hospital, one of the largest hospitals in Athens, the capital of Greece. The research protocol was approved by the Ethics Committee of the Laiko General Hospital.
Participants and randomization
Patients were eligible to enter the study if they had obesity i.e. body mass index (BMI) ≥30 Kg/m2, age >18 years, permanent residence in Athens and literacy in the Greek language. Exclusion criteria included the presence of mental illness, use of corticosteroids in the past month, use of benzodiazepines, neuroleptics or other psychiatric medication, as well as engagement in any other stress management technique. Patients who deemed eligible were fully informed in writing about the purposes and process of the research and signed a written consent form prior to participation. Patients were consecutively enrolled in the study and randomized to the intervention or the control group with the use of an online random number generator (random.org). No concealment was used between the groups.
Measures
Participants were assessed upon entry to the study for their social and demographic characteristics i.e. gender, age, education level, marital and employment status. Each patient underwent anthropometric measurements at baseline and at the end of the study period. Body weight was recorded to the nearest 0.1 Kg, with participants standing on a digital scale, without shoes and in minimal clothing. Height was recorded to the nearest 1 cm, with participants standing on a stadiometer bare-foot with feet together, heels, buttocks and shoulder blades positioned against the stick and head in the Frankfurt plane. BMI was calculated by dividing weight (in Kg) with height squared (in m2).
Depression, anxiety, stress and health related life quality were evaluated at baseline and the end of the two-month study period with the use of the following questionnaires:
Healthy Lifestyle and Personal Control Questionnaire (HLPCQ)
The HLPCQ (Darviri et al. 2014) records a set of daily behaviors and habits relating to the adoption of healthy dietary choices, avoidance of incorrect eating habits, daily routine, organized physical activity, social support and mental control. The frequency of adoption of these habits is rated on a scale of 1 (rarely or never) to 4 (always).
Perceived Stress Scale (PSS) 14
The Greek version of the PSS 14 (Cohen et al. 1983, Andreou et al. 2011) was used to assess participants’ stress levels by measuring the degree to which situations in one's life were deemed as stressful. It is a self-report instrument that consists of 14 elements rating the frequency of emotions and thoughts in the past month on a 5-point Likert-type scale (0=never to 4=very often). There are seven positive and seven negative elements and the total score is calculated by summing the scores of each element, after positive elements have been reversed (minimum score=0, total maximum score=56). Higher scores indicate higher levels of perceived stress during the past month. This measure has performed well in terms of its psychometric properties in a Greek sample, with good initial and final internal consistency (Cronbach's a: 0.82 and 0.87, respectively).
Multidisciplinary Health Locus of Control (MHLC) FORM A
The MHLC FORM A questionnaire (Wallston et al. 1978) uses the Health Control Housing scale, which consists of 18 elements. Respondents express their level of agreement with 18 statements on a six-point Likert-type scale (1=strongly disagree to 6=strongly agree). The scale comprises three subscales, namely the "Internal Health Locus of Control (HLC-INT)", the "External Health Locus of Control (HLC-EXT)" and "Health Locus of Control by Chance (HLC-CHANCE)", each of which consists of six statements. The HLC-INT measures the degree to which a person believes that he/she is responsible for his/her health. The HLC-EXT and HLC-CHANCE, represent the extent to which other people (such as doctors) or chance, respectively, are perceived by a person as the main determinants of one’s health. Summing up the answers for each subscale, higher scores indicate a higher strength for each type of health beliefs (total score ranges from 6 to 36, for each subscale). The instrument has been standardized for the Greek population (Karademas 2009) and the internal validity for each subscale has been found to be satisfactory for the initial and final measurements (Cronbach’s a: baseline HLC-INT 0.76, HLC-EXT 0.8, HLC-CHANCE 0.76 and final HLC-INT 0.66, HLC-EXT 0.77, HLC-CHANCE 0.7).
Food Frequency Questionnaire (FFQ)
The Greek version of the FFQ (Manios 2006) was used to assess eating habits; the questionnaire includes all food items, next to which the proposed amounts of consumption are displayed. Individuals rate the frequency with which they consume these foods in the proposed amount, in a scale of >2 times/day, once/day, 3-6 times/week, 1-2 times/week, 1-3 times/month, rarely or never.
Beck Depression Inventory (BDI)
The BDI-II scale (Beck et al. 1996) is a self-report questionnaire with 21 questions that measure the severity of depression in adults and adolescents over 13 years of age. With the use of the Greek version (Giannakou et al. 2013), individuals were asked to evaluate how true the 21 questions (each of which corresponds to a symptom) were, considering their mood over the past two weeks. The total score consists of the sum of all responses and ranges from 0 to 63 points.
Routine-Daily Life Questionnaire
The Routine-Daily Life questionnaire includes items about demographic characteristics (such as age, educational level, marital status), height, weight and daily routine habits and has been developed in the Greek language (Darviri et al. 2012). It consists of many scales but only one was used, the "Life Satisfaction Scale". The "Life Satisfaction Scale" includes 18 items; 8 items for life satisfaction and general daily satisfaction, 5 items for relationship satisfaction and 5 items for job satisfaction. Participants’ satisfaction in various areas, such as work, self, relationships with friends and colleagues, other interpersonal relationships, support from friends, leisure, appearance and overall outward self-image, were measured by a 5-point Likert-type scale from 1=not at all (extremely dissatisfied) to 5=very much (extremely satisfied).
Study Interventions
Patients in the intervention group attended the stress management program for eight weeks. Program sessions were held by a health professional specialized in stress management techniques and comprised progressive muscle relaxation, diaphragmatic breathing and guided visualization as well as instructions on progressively shifting one’s way of thinking by replacing incorrect perceptions about nutrition with healthier food habits and choices. Participants were informed in detail about the aforementioned techniques, were given a compact disk with recorded instructions and were encouraged to perform the techniques once a week. Furthermore, patients were given diaries detailing the nature of the intervention and were encouraged to contact the investigators for any clarification. The intervention diaries were returned at the end of the two-month study period and were used to assess proper implementation of the stress management techniques. Participants in the control group received standard dietary and physical activity instructions.
Outcome Measures
Primary outcome measures were the differences in BMI, depression, anxiety, stress and health-related life quality indices, before and after implementation of the stress management program, in the intervention and control groups.
Statistical analysis
Continuous variables are displayed using descriptive statistics (mean values ± standard deviations) and categorical variables are shown as frequencies and percentages. Comparisons between the intervention and control groups were performed using the chi-square test (x2) or the non-parametric Mann-Whitney U test. The intervention effect size was evaluated by the formula rho = Z/N0.5, where rho is the effect size of the study (<0.3 small, 0.3-0.5 medium, >0.5 great degree of effect), Z is the score of each Mann-Whitney U test and N is the sample of the study. The level of statistical significance was set at P < 0.05. Analyses were performed using the SPSS 22.0 software.
Results
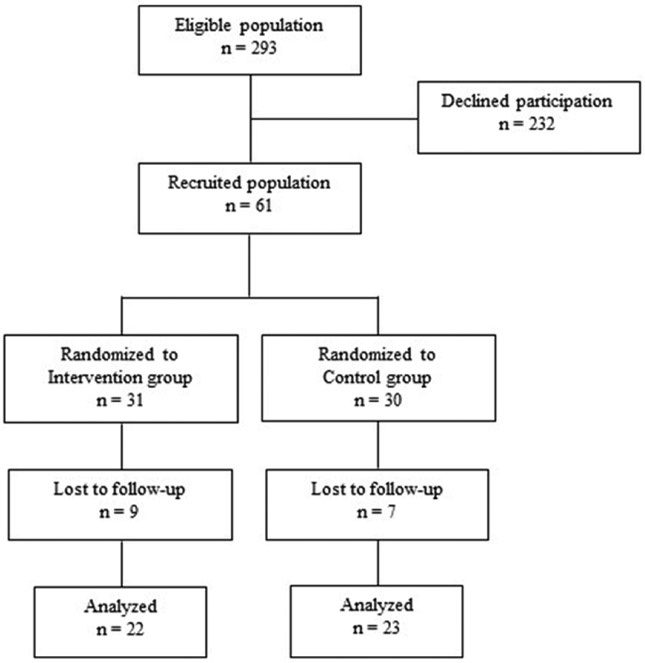
During the 2-year period, 367 individuals were screened for eligibility and 293 were considered eligible to participate. A total of 61 adults gave consent to enter the study; of these 16 were excluded after randomization, as they were considered drop-outs. Consequently, 22 patients were allocated to the intervention group and 23 to the control group. The participants’ flow chart is shown in Figure 1. Participants’ demo-graphic characteristics and baseline measurements are shown in Table 1.
Figure 1.
Study participants' flowchart, depicting the eligible and recruited populations and the subsequent intervention and control groups.
Table 1.
Participants’ demographic characteristics and baseline measurements. BMI: Body Mass Index, BDI: Beck Depression Inventory, PSS: Perceived Stress Scale, HLC-INT: Internal Health Locus of Control, HLC-EXT: External Health Locus of Control, HLC-CHANCE: Health Locus of Control by Chance, DHC: Dietary Healthy Choices, DHA: Dietary Harm Avoidance, DR: Daily Routine, OPE: Organized Physical Exercise, SSMC: Social Support and Mental Control. Results are presented as mean ± Standard Deviation.
| Variable | Intervention group (N=22) | Control group (N=23) | P value |
|---|---|---|---|
| Age | 46.91 ± 10.98 | 44.48 ± 10.12 | 0.413 |
| Men, N (%) | 10 (45.4) | 12 (52.2) | 0.768 |
| Women, N (%) | 12 (54.5) | 11 (47.8) | 0.897 |
| Married, N (%) | 18 (81.8) | 18 (78.3) | 1.0 |
| Higher education, N (%) | 19 (86.4) | 19 (82.6) | 1.0 |
| BMI | 35.54 ± 2.98 | 34.86 ± 2.86 | 0.742 |
| BDI | 33.68 ± 4.85 | 29.57 ± 2.79 | 0.001* |
| PSS | 28.14 ± 4.76 | 29.35 ± 1.90 | 0.292 |
| HLC-INT | 25.05 ± 3.63 | 21.30 ± 2.03 | <0.001* |
| HLC-EXT | 19.59 ± 5.11 | 16.04 ± 2.84 | 0.007* |
| HLC-CHANCE | 9.5 ± 2.15 | 9.61 ± 1.31 | 0.296 |
| DHC | 12.41 ± 3.13 | 11.52 ± 1.86 | 0.325 |
| DHA | 6.95 ± 0.84 | 6.96 ± 1.02 | 0.793 |
| DR | 18.77 ± 1.85 | 18.04 ± 1.52 | 0.118 |
| OPE | 2.36 ± 0.85 | 2.22 ± 0.42 | 0.961 |
| SSMC | 12.77 ± 1.93 | 11.48 ± 1.27 | 0.010* |
| Frequency of Consumption | |||
| Dairy products | 16.23 ± 3.09 | 15.43 ± 1.59 | 0.678 |
| Fruits and vegetables | 31.32 ± 4.96 | 28.61 ± 1.67 | 0.050* |
| Fish eggs and poultry | 13.09 ± 1.97 | 12.39 ± 0.84 | 0.225 |
| Red meat | 20.82 ± 4.29 | 18.78 ± 2.89 | 0.051 |
| Fast food | 39.82 ± 8.78 | 37.13 ± 3.88 | 0.048* |
| Alcohol | 6.68 ± 2.03 | 6.52 ± 1.65 | 0.809 |
| Other beverages | 20.86 ± 3.69 | 20.43 ± 2.25 | 0.403 |
| Foods with carbohydrates | 50.23 ± 5.23 | 45.74 ± 1.96 | <0.001* |
| Foods with fat | 20.91 ± 2.91 | 19.04 ± 1.58 | 0.001* |
P < 0.05.
The majority of participants were married or had reached higher educational level. Statistically significant differences between the intervention and control groups were observed at baseline for the following variables: depression, internal and external HLC, social support and frequency of eating habits such as consumption of fruits and vegetables, fast food, carbohydrates and fat.
Comparisons of the differences, pre- and post-intervention, in measured variables between the two groups are shown in Table 2. Statistically significant differences between groups were observed for the changes in BMI, perceived stress levels, depression levels, internal and external HLC, several eating habits, daily routine, organized physical activity and social support.
Table 2.
Comparisons of pre- and post- intervention differences in measured variables between groups. Δ: Difference BMI: Body Mass Index, BDI: Beck Depression Inventory, PSS: Perceived Stress Scale, HLC-INT: Internal Health Locus of Control, HLC-EXT: External Health Locus of Control, HLC-CHANCE: Health Locus of Control by Chance, DHC: Dietary Healthy Choices, DHA: Dietary Harm Avoidance, DR: Daily Routine, OPE: Organized Physical Exercise, SSMC: Social Support and Mental Control. Results are presented as mean ± Standard Deviation.
| Outcomes | Intervention group (n=22) |
Control group (n=23) | P value | Effect size rho |
|---|---|---|---|---|
| ΔBMI | −3.1 ± 0.62 | −1.74 ± 0.62 | <0.001* | 0.84 |
| ΔPSS | −11.23 ± 2.39 | −1.22 ± 1.31 | <0.001* | 0.86 |
| ΔBDI | −8.50 ± 3.20 | −2.09 ± 1.68 | <0.001* | 0.79 |
| ΔHLC-INT | 2.95 ± 1.43 | 0.96 ±0.82 | <0.001* | 0.65 |
| ΔHLC-EXT | 3.41 ± 2.74 | 0.35 ± 0.71 | <0.001* | 0.58 |
| ΔHLC-CHANCE | −2.18 ± 1.01 | −0.26 ± 0.86 | <0.001* | 0.75 |
| ΔDHC | 5.36 ± 0.95 | 2.83 ± 1.07 | <0.001* | 0.78 |
| ΔDHA | 3.59 ± 0.67 | 1.13 ± 0.81 | <0.001* | 0.85 |
| ΔDR | 5.00 ± 1.27 | 1.35 ± 1.15 | <0.001* | 0.82 |
| ΔOPE | 1.36 ± 0.58 | 0.61 ± 0.58 | <0.001* | 0.55 |
| ΔSSMC | 3.64 ± 1.14 | 0.96 ± 0.82 | <0.001* | 0.80 |
| Δdairy products | −1.32 ± 2.10 | −0.74 ± 1.14 | 0.423 | 0.12 |
| Δfruits and vegetables | 7.05 ± 3.29 | 6.00 ± 2.13 | 0.224 | 0.18 |
| Δfish eggs and poultry | −0.45 ± 1.77 | −0.43 ± 0.95 | 0.852 | 0.03 |
| Δred meat | −5.14 ± 2.40 | −2.57 ± 1.44 | <0.001* | 0.59 |
| Δjunk food | −10.55 ± 4.19 | −8.52 ± 1.70 | 0.010* | 0.38 |
| Δalcohol | −1.05 ± 1.13 | −0.83 ± 1.03 | 0.582 | 0.08 |
| Δother beverages | −2.55 ± 1.22 | −1.48 ± 1.41 | 0.007* | 0.41 |
| Δfoods with carbohydrate | −2.55 ± 2.91 | −0.65 ± 1.90 | 0.011* | 0.38 |
| Δfoods with fat | −2.27 ± 1.83 | −1.13 ± 1.18 | 0.012* | 0.38 |
P < 0.05.
Table 3 presents the significantly different percentages of participants between the two groups who reported improvement of satisfaction in various areas i.e. work, self, interpersonal relationships with friends and colleagues, support from friends, leisure time and manner of its disposal, and self-appearance.
Table 3.
Percentage of participants in intervention and control groups who reported improvement of satisfaction.
| Domains | Intervention group (n=22) | Control group (n=23) | P value |
|---|---|---|---|
| Work | 83.3 | 16.7 | 0.007* |
| Self | 65.4 | 34.6 | 0.016* |
| Relationships with friends | 75.0 | 25.0 | 0.013* |
| Relationships with colleagues | 82.4 | 17.6 | 0.001* |
| Intrapersonal relationships | 93.3 | 6.7 | <0.001* |
| Support by friends | 65.2 | 34.8 | 0.038* |
| Time | 84.2 | 15.8 | <0.001* |
| Mood | 69.0 | 31.0 | <0.001* |
| Self-image | 68.0 | 32.0 | 0.007* |
P < 0.05.
Discussion
In this randomized clinical trial, we evaluated the effect of an 8-week stress management program on weight loss in obese patients vs. age- and BMI-matched control patients who received standard lifestyle instructions. Both groups experienced significant reductions in BMI, perceived stress, level of depression, HLC based on chance, increases in internal and external HLC, as well as positive changes regarding dietary habits, physical activity, daily routine, and social support. The intervention group displayed better results regarding reduction of weight, perceived stress and depression levels.
This study is one of few in the literature to implement an integrated program of stress management relaxation techniques, that included diaphragmatic breathing, progressive muscle relaxation and guided visualization, for eight weeks to overweight and obese adults. In another study (Christaki et al. 2013) of the same duration, where similar stress management techniques were applied to overweight and obese women, a statistically significant weight loss was also evident, but no such effect on perceived stress levels, as in our study. In a more recent study (Stavrou et al. 2016), examining a sample of overweight and obese children and adolescents, stress management resulted in a significant reduction in BMI and perceived stress levels, as in the present study. Finally, in three other studies the application of a relaxation technique (progressive muscle relaxation or guided visualization) led to improved compliance with a dietary intervention and adoption of healthy dietary choices (Manzoni et al. 2009, Weigensberg et al. 2003, Wynd 2006). The results of the present study suggest that this comprehensive stress management intervention targeting both males and females could be useful for the prevention and management of obesity in adulthood.
It is well known that a reciprocal relationship between stress and depression exists. In support of this, our study demonstrated a statistically significant reduction in the levels of perceived stress accompanied by a similar decrease in the levels of depression. The association of stress with obesity is also undeniable. In particular, the more stress one has, the greater amount of cortisol is produced in the body leading to accumulation of fat in the abdominal area, namely abdominal or visceral obesity (Daubenmier et al. 2011, Donoho et al. 2011, Speaker & Fleshner 2012). In turn, decreased levels of perceived stress are associated with lower cortisol secretion, which could contribute to reduction of abdominal fat. This mechanism could provide a possible explanation for the increased weight loss of the intervention group in our study.
On the other hand, stress is known to affect the eating behavior per se; current living conditions with work overload and constant lack of time, lead to the consumption of easy fast food choices and abandonment of the healthy Mediterranean style diet. The reduction in perceived stress levels in the intervention group, could have led to the adoption of healthier dietary habits and subsequent weight loss.
This study has several limitations. The study sample was small and not representative of the general population, thus generalizability of the results is not feasible. Furthermore, there were some significant differences between groups at baseline. To overcome this limitation, groups’ comparisons were performed with respect to the change of measures during follow-up and not to the final outcome measures. In addition, despite the existence of a diary, there is a subjective element when recording improvement of symptoms and compliance to a stress management program, especially in this non-blind study where individuals in the intervention group knew they underwent a more complex intervention.
In conclusion, the implementation of a comprehensive stress management program in overweight and obese adults led to significant decreases in their levels of perceived stress and depression as well as to their adoption of healthier dietary patterns. Stress management could be adopted as an adjunct to traditional methods of treating obesity, namely lifestyle interventions, drugs and bariatric surgery. Future studies are needed to confirm these findings, in larger population samples.
Footnotes
Conflict of interest
Authors have no conflicts of interest.
References
- Andreou E, Alexopoulos EC, Lionis C, Varvogli L, Gnardellis C, Chrousos GP & Darviri C 2011. Perceived Stress Scale: reliability and validity study in Greece. Int J Environ Res Public Health 8 3287–3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK 1996. Manual for the Beck Depression Inventory. San Antonio, T.X: Psychological Corporation [Google Scholar]
- Chaplin K & Smith AP 2011. Breakfast and snacks: associations with cognitive failures, minor injuries, accidents and stress. Nutrients 3 515–528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christaki E, Kokkinos A, Costarelli V, Alexopoulos EC, Chrousos GP & Darviri C 2013. Stress management can facilitate weight loss in Greek overweight and obese women: a pilot study. J Hum Nutr Diet 26 132–139 [DOI] [PubMed] [Google Scholar]
- Chrousos GP 2009. Stress and disorders of the stress system. Nat Rev Endocrinol 5 374–381 [DOI] [PubMed] [Google Scholar]
- Cohen S, Mermelstein K & Kamarck T 1983. A global measure of perceived stress. J Health Soc Behav 24 385–396 [PubMed] [Google Scholar]
- Darviri C, Alexopoulos EC, Artemiadis AK, Tigani X, Kraniotou C, Darvyri P & Chrousos GP 2014. The Healthy Lifestyle and Personal Control Questionnaire (HLPCQ): a novel tool for assessing self-empowerment through a constellation of daily activities. BMC Public Health 24 995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darviri C, Fouka G, Gnardellis C, Artemiadis AK, Tigani X & Alexopoulos EC 2012. Determinants of self-rated health in a representative sample of a rural population: a cross-sectional study in Greece. Int J Environ Res Public Health 9 943–954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M, Jhaveri K, Lustig RH, Kemeny M, Karan L & Epel E 2011. Mindfulness Intervention for Stress Eating to Reduce Cortisol and Abdominal Fat among Overweight and Obese Women: An Exploratory Randomized Controlled Study. J Obes 2011 651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donoho CJ, Weigensberg MJ, Emken BA, Hsu JW & Spruijt-Metz D 2011. Stress and abdominal fat: preliminary evidence of moderation by the cortisol awakening response in Hispanic peripubertal girls. Obesity (Silver Spring) 19 946–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannakou M, Roussi P, Kosmidou M, Kioseoglou G, Adamopoulou A & Garyfalos G 2013. Adjustment of the Beck-II depression scale to the Greek population. Hellenic Journal of Psychology 10 120–146 [Google Scholar]
- Karademas EC 2009. Effects of exposure to the suffering of unknown persons on health-related cognitions, and the role of mood. Health (London) 13 491–504. [DOI] [PubMed] [Google Scholar]
- Manios Y. Nutritional Evaluation: Dietetic and Medical History, Somatometric, Clinical and Bio-chemical Indices, Paschalidis Publications 2006 [Google Scholar]
- Manzoni GM, Pagnini F, Gorini A, Preziosa A, Castel-nuovo G, Molinari E & Riva G 2009. Can relaxation training reduce emotional eating in women with obesity? An exploratory study with 3 months of follow-up. J Am Diet Assoc 109 1427–1432 [DOI] [PubMed] [Google Scholar]
- Nicolaides NC, Kyratzi E, Lamprokostopoulou A, Chrousos GP & Charmandari E 2015. Stress, the stress system and the role of glucocorticoids. Neuroimmuno-modulation 22 6–19 [DOI] [PubMed] [Google Scholar]
- Speaker KJ & Fleshner M 2012. Interleukin-1 beta: a potential link between stress and the development of visceral obesity. BMC Physiol 12 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavrou S, Nicolaides NC, Papageorgiou I, Papadopoulou P, Terzioglou E, Chrousos GP, Darviri C & Charmandari E 2016. The effectiveness of a stress-management intervention program in the management of overweight and obesity in childhood and adolescence. J Mol Biochem 5 63–70 [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS & DeVellis R 1978. Development of the multidimensional health locus of control scale. Health Education Monographs 6 160–170 [DOI] [PubMed] [Google Scholar]
- Weigensberg MJ, Lane CJ, Winners O, Wright T, Nguyen-Rodriguez S, Goran MI & Spruijt-Metz D 2003. Acute effects of stress-reduction Interactive Guided Imagery (SM) on salivary cortisol in overweight Latino adolescents. J Altern Complement Med 15 297–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynd CA 2006. Relaxation imagery used for stress reduction in the prevention of smoking relapse. J Adv Nurs 17 294–302 [DOI] [PubMed] [Google Scholar]