Abstract
Objective:
This study was conducted to identify factors contributing to health satisfaction outcomes among emerging adults (ages 18–25) with diabetes.
Method:
SEARCH for Diabetes in Youth study participants whose diabetes was prevalent in 2001 and were ≥18 years of age when they completed a 2008–2009 follow-up survey (n = 340) were included. We developed a health resilience model (HRM) to identify potentially modifiable factors (anticipatory guidance, social support, physical activity, quality of life) associated with health outcomes (satisfaction with health care, overall personal health, self-report of hemoglobin A1c [HbA1c]). Proportional odds logistic regression models were used to examine relationships between modifiable factors and health outcomes while adjusting for predetermined characteristics; linear regression models were used for reported HbA1c. Comparison of participants who reported HbA1c versus nonreporters was conducted.
Results:
A majority (70%) of participants rated satisfaction with health care ≥7 out of 10, and most (71%) rated overall health as good, very good, or excellent. Satisfaction with health care was independent of change in provider between the ages of 17 and 24. After controlling for predetermined characteristics, we found that the odds of increased satisfaction with health care and overall personal health were 1.3 and 1.2 greater, respectively, when participants discussed additional diabetes-related anticipatory guidance topics with a provider and 1.3 and 2.1, respectively, for each 10-unit change in quality of life score. Relationship between HbA1c level and modifiable factors was not significant; however, participants reporting HbA1c had higher ratings of health care and overall health versus nonreporters.
Conclusions:
HRM describes relationships between modifiable factors and patient-reported outcomes of satisfaction with health care and overall personal health among a cohort of ethnically and racially diverse emerging adults with longstanding diabetes, over half of whom experienced a change in provider. HRM may discern candidate areas for intervention, such as effective anticipatory guidance that can impact satisfaction with health care and overall health, to promote positive health outcomes.
Keywords: Type 1 diabetes mellitus, transition to adult care, resilience, adolescent
Emerging adulthood (age 18–25 years) is defined as a developmental stage during which individuals explore a variety of educational, occupational, social, emotional, and financial opportunities and challenges (Arnett, 2000). During this period, individuals with diabetes assume increased responsibility for management of their condition. Competing priorities often result in interrupted medical care, placing these individuals at risk for poor outcomes, such as suboptimal glycemic control, early onset of diabetes-related chronic complications, and premature mortality (Bryden et al., 2001; Garvey, Markowitz, & Laffel, 2012; Garvey, Wolpert, et al., 2012; Lotstein et al., 2013; Peters, Laffel, & the American Diabetes Association Transitions Working Group, 2011; Weissberg-Benchell, Wolpert, & Anderson, 2007; Wills et al., 2003). Although previous studies have identified a number of factors predicting poor diabetes outcomes (Bernstein, Stockwell, Gallagher, Rosenthal, & Soren, 2013; Bryden, Dunger, Mayou, Peveler, & Neil, 2003; Feltbower et al., 2008; Grey, Whittemore, & Tamborlane, 2002; Hilliard, Herzer, Dolan, & Hood, 2011; Hood et al., 2006; Kovacs, Goldston, Obrosky, & Bonar, 1997; Lotstein et al., 2013; Peters, Laffel, & the American Diabetes Association Transitions Working Group, 2011; Rydall, Rodin, Olmsted, Devenyi, & Daneman, 1997), little is known about those individuals who succeed in maintaining a high level of overall health, as defined by favorable clinical or patient reported outcomes during the transition to adulthood (Hilliard, Harris, & Weissberg-Benchell, 2012).
Resilience is defined as a positive adaptation despite adversity that may involve multiple protective factors (individual, familial, social, and cultural or contextual; Hilliard et al., 2012; Hilliard, McQuaid, Nabors, & Hood, 2015; Luthar, Cicchetti, & Becker, 2000; Yi, Vitaliano, Smith, Yi, & Weinger, 2008). When applied to youth with diabetes, resilience is associated with positive diabetes outcomes (Yi-Frazier et al., 2015) and diabetes-specific protective processes (e.g., self-efficacy, family communication, social competence, and health appraisals; Hilliard et al., 2012). To date, the role of modifiable factors, including provider-mediated factors that contribute to resilience, have not been studied among emerging adults with diabetes.
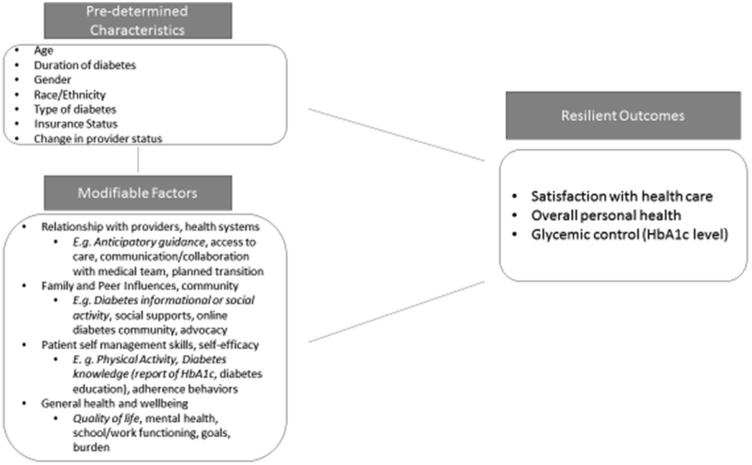
Informed by the social–ecological model of transition readiness (SMART; Pierce & Wysocki, 2015; Schwartz, Tuchman, Hobbie, & Ginsberg, 2011), which conceptualizes interrelated constructs that influence transfer to adult care, the authors attempted to address gaps in the resilience literature for emerging adults with diabetes by developing a health resilience model (HRM). The HRM represents the relationship among predetermined characteristics less amenable to intervention, modifiable factors that are candidates for intervention, and positive health outcomes in an emerging adult population with diabetes (see Figure 1). Predetermined characteristics include things such as age and duration and type of diabetes, which cannot be changed. Modifiable factors could include patient, family, provider, health system, and community considerations. Examples of modifiable factors of interest in the current study include diabetes-related anticipatory guidance of adult screening guidelines, diabetes informational or social activities, frequency of physical activity, and quality of life. The construct of quality of life was treated as a modifiable factor in the model because of the potential for targetable interventions within each domain included in the measure (physical, emotional, social, and work or school functioning). Positive health outcomes of interest include rating of satisfaction with the health care received in the previous 12 months (Li, Yuan, Wu, Luan, & Hao, 2013; Pascoe, 1983), current overall health, and glycemic control as measured by self-reported glycated hemoglobin A1c (HbA1c).
Figure 1.
Health resilience model (HRM) for emerging adults with diabetes. The HRM acknowledges pre-determined characteristics that are difficult to change and highlights proposed modifiable factors that are predicted to promote favorable health outcomes. Modifiable factors in italic font are considered for analysis in this study. Brief description of terms; see methods section for operational definitions: Pre-determined characteristics: demographic and clinical features that are fixed. Change in provider was considered pre-determined for the sake of analysis in this study. Modifiable factors: opportunities for interventions; broad categories of theoretical factors are listed with specific variables included in current study noted by italics. Glycemic control: self-report of most recent hemoglobin HbA1c. Satisfaction with health care: rating of health care received within the past 12 months. Overall health: rating of current personal health. HbA1c = hemoglobin A1c.
The purpose of this cross-sectional study was to use the proposed HRM to identify the association of potentially modifiable factors with positive health outcomes (higher satisfaction with health care and personal overall health ratings and lower self-reported HbA1c levels) for emerging adults with diabetes, rather than examining risk factors for negative health outcomes, as has been the primary focus of research thus far in this population.
Method
SEARCH for Diabetes in Youth Study Procedures
The SEARCH for Diabetes in Youth study has been conducting population-based ascertainment of youth clinically diagnosed with either Type I or Type 2 diabetes before the age of 20 since 2001(Hamman et al., 2014; SEARCH Study Group, 2004). Cases of diabetes were identified in four geographically defined populations in Ohio, Colorado, South Carolina, and Washington and among Indian Health Service beneficiaries and health plan enrollees in California. The institutional review boards for all sites approved the study protocol. Youth who identified as having diabetes were then invited to participate in an initial in-person visit, where informed consent was obtained; physical measurements and fasting samples were obtained from participants in metabolically stable condition, and questionnaires were completed.
Participants
This study population was drawn from 2,543 pediatric SEARCH participants whose diabetes was prevalent in 2001. From this group, all racial minorities (n = 770) and a 10% random sample of non-Hispanic Whites (n = 174) were selected and invited to complete the SEARCH Quality of Care survey (Waitzfelder et al., 2011) and the generic Young Adult version of the Pediatric Quality of Life Inventory (PedsQL; Varni & Limbers, 2009). Of the 944 selected individuals, 613 (65%) completed these surveys over the telephone or via the Internet or completed and mailed a printed survey between September 2008 and March 2009. Of the 613 who completed the surveys, 340 were ≥18 years of age at the time of survey completion and are included in these analyses.
Measures
The SEARCH Quality of Care survey was designed to solicit information about conformity with standards of diabetes care as recommended by the American Diabetes Association, access to care, self-care practices, satisfaction with care, and quality of life (Waitzfelder et al., 2011). Participants age 18 and older consented and completed the survey independent of parent or guardian. All surveys were available in English and Spanish.
Measurement of predetermined factors.
Predetermined characteristics available from the SEARCH study data set that were used in the analyses include date of birth, duration of diabetes, gender, race or ethnicity, diabetes type (on the basis of health care provider reports), change in provider, and insurance type. Age and diabetes duration were calculated on the basis of the date of survey completion in relation to participants’ date of birth and date of diagnosis. Information regarding their self-reported change in diabetes care provider between the ages of 17 and 24 (see the Appendix in the online supplemental materials) and responsibility for diabetes care was collected as part of the survey.
Measurement of potentially modifiable factors.
Diabetes-related anticipatory guidance, diabetes informational or social activity, exercise frequency, and quality of life were the key potentially modifiable factors studied under our proposed HRM (see the Appendix in the online supplemental materials for further details of survey items).
Anticipatory guidance was defined as having ever received information from a health care provider about recommended frequency of the following: eye and foot examinations, blood pressure checks, urine test for kidney function, blood test for cholesterol, HbA1c test, and (among women), importance of glycemic control prior to pregnancy. For each survey item, responses were coded as 1 (yes) and 0 (no) or (don’t know/unsure). Summation of total positive responses resulted in a variable with a range of 0–6 for men and 0–7 for women.
Diabetes informational or social activity was defined as having ever attended a diabetes camp, support group for diabetes, diabetes expo or fair, or a diabetes walk-a-thon or bike-a-thon. Participation in each of the diabetes informational or social activity was coded as positive. Summation of positive responses resulted in a variable with a range from 0 to 4.
Exercise frequency was measured as the number of days within the past week in which the participant engaged in moderate or vigorous physical activity for at least 20 min. Frequency was coded as a variable with a range from 0 to 7 days/week.
Quality of life was measured with the generic Pediatric Quality of Life Inventory (Young Adult Version) [PedsQL]. The PedsQL is a multidimensional measure of health-related quality of life that includes four domains (physical, emotional, social. and work or school functioning) that distinguish between young adults with and without chronic conditions (Varni & Limbers, 2009). A summation score for all domains was treated as a continuous variable with a range from 0 to 100. Higher scores indicate an overall higher quality of life.
Measurement of positive health outcomes.
Health Satisfaction was assessed on the basis of responses to two questions: (1) satisfaction with health care and (2) overall personal health. Participants were asked to rate satisfaction with the health care that they received in the previous 12 months (range = 0–10) and their current overall personal health (excellent, very good, good, fair, poor). The raw scores are presented in Table 1 and 2. In order to fit the analytic model, we then grouped scores for participants’ satisfaction with their health care as 0–4 (n = 38), 5–6 (n = 58), 7–8 (n = 117), or 9–10 (n = 124). Qualitative responses to overall personal health ratings were recoded numerically as 1 (poor), 2 (fair), 3 (good), 4 (very good), and 5 (excellent). Outcomes were then grouped as poor or fair (n = 96), good (n = 131), or very good or excellent (n = 112). Scores for health care and personal health were analyzed as separate outcomes. Higher scores indicated more satisfaction with health care and better rating of overall personal health, respectively. Proportional odds regression model for grouped responses are reported in Table 3.
Table 1.
Participant Predetermined Characteristics, Modifiable Factors, and Outcome Variables, Overall and by Diabetes Type
| Overall (N = 340) |
Type 1 (n = 246) |
Type 2 (n = 94) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predetermined factor | M | SD | Range | M | SD | Range | M | SD | Range | pa |
| Age (in years) at survey completion | 21.9 | 2.4 | 18.0–27.1 | 21.6 | 2.3 | 18.0–26.7 | 22.9 | 2.4 | 18.1–27.1 | <.0001 |
| Duration (in years) of DM | 11.4 | 3.7 | 6.2–24.0 | 12.3 | 3.9 | 6.5–24.0 | 8.9 | 1.7 | 6.2–13.7 | <.0001 |
|
N |
% |
n |
% |
n |
% |
|||||
| Gender | .0127 | |||||||||
| Female | 191 | 56.2 | 118 | 48.0 | 63 | 67.0 | ||||
| Male | 149 | 43.8 | 128 | 52.0 | 31 | 33.0 | ||||
| Race | ||||||||||
| Hispanic | 117 | 34.4 | 101 | 41.1 | 16 | 17.0 | ||||
| Black | 106 | 31.2 | 59 | 24.0 | 47 | 50.0 | ||||
| White | 69 | 20.3 | 67 | 27.2 | 2 | 2.1 | ||||
| Native American | 33 | 9.7 | 6 | 2.4 | 27 | 28.7 | ||||
| Asian/Pacific Islander | 14 | 4.1 | 12 | 4.9 | 2 | 2.1 | ||||
| Other | 1 | .3 | 1 | .4 | 0 | .0 | ||||
| Provider change | .8086 | |||||||||
| Yes | 187 | 57.0 | 133 | 56.6 | 54 | 58.1 | ||||
| No | 141 | 43.0 | 102 | 43.4 | 39 | 41.9 | ||||
| HbA1cc reported | <.0001 | |||||||||
| Yes | 179 | 52.7 | 152 | 61.8 | 27 | 28.7 | ||||
| No | 161 | 47.4 | 94 | 38.2 | 67 | 71.3 | ||||
| Health insurance | <.0001 | |||||||||
| Medicaid or Medicare | 80 | 23.9 | 49 | 20.3 | 31 | 33.3 | ||||
| None | 47 | 14.0 | 25 | 10.3 | 22 | 23.7 | ||||
| Private | 154 | 46.0 | 129 | 53.3 | 25 | 26.9 | ||||
| Other | 54 | 16.1 | 39 | 16.1 | 15 | 16.1 | ||||
|
M |
SD |
M |
SD |
M |
SD |
|||||
| Patient outcomes | ||||||||||
| HbA1c levelb (%) | 8.5 | 1.9 | 5.2–15.2 | 8.3 | 1.7 | 5.2–15.0 | 9.5 | 2.8 | 5.3–15.2 | .0049 |
| Satisfaction with health care (past 12 months) | 7.4 | 2.3 | .0–10.0 | 7.8 | 2.0 | .0–10.0 | 6.3 | 2.8 | .0–10.0 | <.0001 |
| Overall personal health (current) | 3.0 | 1.0 | 1.0–5.0 | 3.2 | .9 | 1.0–5.0 | 2.6 | 1.0 | 1.0–5.0 | <.0001 |
| Modifiable factors | ||||||||||
| Anticipatory guidance | 4.4 | 2.0 | .0–7.0 | 4.5 | 1.9 | .0–7.0 | 4.0 | 2.1 | .0–7.0 | .0307 |
| Physical activity | 2.7 | 2.1 | .0–7.0 | 2.8 | 2.0 | .0–7.0 | 2.5 | 2.1 | .0–7.0 | .2602 |
| Social support | .9 | 1.1 | .0–4 | 1.1 | 1.1 | .0–4 | .4 | .8 | .0–4 | <.0001 |
| Total PedsQL score | 80.8 | 16.5 | 2.2–100 | 82.9 | 14.1 | 16.3–100 | 76.6 | 20.2 | 2.2–100 | .0071 |
Note. Differences by diabetes type were assessed using analysis of variance for continuous variables and chi-square tests for categorical variables. DM = diabetes mellitus; HbA1c = hemoglobin A1c; PedsQL = Pediatric Quality of Life Inventory (Young Adult version).
Assessed by Fisher’s exact test.
Per self-report of value.
Table 2.
Predetermined Factors and Report of Recent HbA1c (Yes/No) by Satisfaction With Health Care Total Scores and Overall Personal Health Ratings
| Predetermined factors and value |
Satisfaction with health carea |
Overall personal healthb |
||||
|---|---|---|---|---|---|---|
| M | SD | p | M | SD | p | |
| Age (in years) at survey | ||||||
| <22 | 7.8 | 2.2 | .0008 | 3.0 | .9 | .6372 |
| ≥22 | 7.0 | 2.4 | c | 3.0 | 1.0 | c |
| Duration of DM (in years) | ||||||
| <10 | 7.0 | 2.5 | .003 | 2.8 | 1.0 | .0017 |
| ≥10 | 7.8 | 2.1 | c | 3.2 | 1.0 | c |
| Gender | ||||||
| Female | 7.4 | 2.4 | .7701 | 2.8 | .9 | <.0001 |
| Male | 7.4 | 2.2 | c | 3.3 | .9 | c |
| Race2 | ||||||
| Hispanic | 7.5 | 2.3 | .54 | 3.0 | 1.0 | .0054 |
| Black | 7.4 | 2.5 | .3287 | 2.7 | 1.0 | <.0001 |
| White | 7.7 | 2.1 | c | 3.4 | .8 | c |
| Other | 6.8 | 2.5 | .0286 | 3.1 | .9 | .0694 |
| Type of DM | ||||||
| Type 1 | 7.8 | 2.0 | <.0001 | 3.2 | .9 | <.0001 |
| Type 2 | 6.3 | 2.8 | c | 2.6 | 1.0 | c |
| Provider change | ||||||
| Yes | 7.2 | 2.5 | .1474 | 2.9 | 1.0 | .019 |
| No | 7.6 | 2.2 | c | 3.2 | .9 | c |
| Recent HbA1c report | ||||||
| Yes | 7.8 | 2.0 | .0011 | 3.2 | .9 | <.0001 |
| No | 7.0 | 2.6 | c | 2.8 | .9 | c |
| Health insurance | ||||||
| Medicaid or Medicare | 7.7 | 2.2 | .5648 | 2.8 | .9 | .0001 |
| None | 5.2 | 3.1 | <.001 | 2.7 | 1.2 | .0002 |
| Private | 7.9 | 1.8 | c | 3.2 | 1.0 | c |
| Other | 7.6 | 1.9 | .333 | 3.1 | .7 | .3552 |
Note. N = 340. HbA1c = hemoglobin A1c; DM = diabetes mellitus.
Rated over the past 12 months, with a range of 0–10, and additional statistically significant pairwise comparisons existed between insurance types: Medicaid or Medicare vs. None and None vs. Other (both p < .0001). No pairwise race comparisons were significant other than those already presented.
Rated current health, with a range of 0–5, and additional statistically significant pairwise comparisons existed between insurance types: Medicaid or Medicare vs. Other and None vs. Other (p = .0293 and .0162, respectively). Additional statistically significant pairwise comparisons for race existed between African American and Other, and African American and Hispanic (p = .0213 and .018, respectively). Other includes Asian, Pacific Islander, Native American, and Other.
Comparison to reference range.
Table 3.
Proportional Odds Regression Model for Satisfaction With Health Care and Overall Health Rating
| Satisfaction with health carea |
Overall personal healthb |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR | Lower 95% CI | Upper 95% CI | p | OR | Lower 95% CI | Upper 95% CI | p |
| Predetermined factors and value | ||||||||
| Age at survey completion | 1.0 | .8 | 1.1 | .4254 | 1.0 | .9 | 1.1 | .9001 |
| Duration of DM | 1.0 | .9 | 1.1 | .977 | 1.0 | .9 | 1.1 | .9554 |
| Gender | ||||||||
| Female | 2.5 | 1.4 | 4.3 | .0013 | .4 | .2 | .8 | .004 |
| Male | ||||||||
| Race | ||||||||
| Hispanic | 1.0 | .5 | 2.2 | .9908 | .4 | .2 | .8 | .0155 |
| Black | 2.1 | 1.0 | 4.5 | .0448 | .3 | .2 | .8 | .009 |
| White | ||||||||
| Other | .9 | .4 | 2.1 | .7444 | .6 | .2 | 1.6 | .2941 |
| Type of DM (Type 2) | .5 | .2 | 1.1 | .0829 | .8 | .3 | 1.7 | .5468 |
| Provider change (yes) | .7 | .4 | 1.3 | .2692 | .8 | .5 | 1.4 | .4721 |
| Report of recent HbA1c (yes) | 2.6 | 1.5 | 4.7 | .0009 | 1.7 | .9 | 3.2 | .0821 |
|
Modifiable variables | ||||||||
| Anticipatory guidance | 1.3 | 1.2 | 1.5 | <.0001 | 1.2 | 1.1 | 1.5 | .0072 |
| Physical activity | 1.1 | .9 | 1.2 | .309 | 1.0 | .8 | 1.1 | .7376 |
| Social support | .9 | .7 | 1.1 | .2456 | 1.2 | .9 | 1.5 | .2725 |
| Total PedsQL per 10-unit change | 1.3 | 1.1 | 1.5 | .0052 | 2.1 | 1.6 | 2.6 | <.0001 |
Note. Results are presented from the proportional odds regression models. Models were first adjusted for predetermined variables and then additionally by modifiable variables. Odds ratios greater than 1 indicate an increased likelihood for higher health satisfaction scores or overall health rating. OR = odds ratio; CI = confidence interval; DM = diabetes mellitus; HbA1c = hemoglobin A1c; PedsQL = Pediatric Quality of Life Inventory (Young Adult version).
Rated over the past 12 months, comparing 0–4 vs. 5–6 vs. 7–8 or 9–10.
Rated current health, comparing poor or fair vs. good vs. very good or excellent.
Hemoglobin A1c level was based on self-report of most recent HbA1c level prior to the time of completing the survey. A second dichotomous variable was created to indicate whether participants reported their most recent HbA1c (yes or no).
Statistical Analyses
Statistical analyses were conducted using SAS Version 9.3. Continuous data are expressed as mean plus or minus standard deviation, and categorical data are presented as counts and percentages. Predetermined variables and modifiable factors were summarized overall and by diabetes type; differences by diabetes type were assessed using analysis of variance (ANOVA) for continuous variables and chi-squared tests or Fisher’s exact tests for categorical variables. Additionally, we compared participants’ predetermined factors by report of HbA1c using ANOVA and chi-squared tests.
Univariate associations between the positive health outcomes (self-reported HbA1c level, satisfaction of health care, and overall personal health) and independent variables were evaluated using ANOVA and Pearson’s correlations. To examine the relationship between positive health outcomes and modifiable variables after adjustment for predetermined characteristics, we conducted multivariate linear regression with self-reported HbA1c level as the outcome variable. Then, proportional odds logistic regression models were conducted for the two health satisfaction outcome variables: satisfaction with health care and overall personal health. This approach was chosen over linear regression because these outcomes are ordinal and because changes are not uniform across the entire distribution of the outcomes. Score tests for the nonproportionality assumption were all nonsignificant. Regression models were initially adjusted for only predetermined demographic and clinical variables. Then, the potential modifiable factors were added to the regression models. All statistical tests were two-sided, with p < .05 considered statistically significant.
Results
Population Description
The 340 emerging adults with diabetes had a mean age of 21.9 ± 2.4 years (range = 18–27), were predominately female (56%), and were of diverse race and ethnicity (34.4% Hispanic, 31.2% Black, 20.3% White, 9.7% Native American, 4.1% Asian-Pacific Islander), and 46% were privately insured. Their mean duration of diabetes was 11.4 ± 3.7 years (range = 6.2–24.0), and the majority (72%) had Type 1 diabetes (see Table 1). A majority (76%) reported being the person primarily responsible for their diabetes care, with over 95% reporting being responsible for glucose monitoring and medication administration. All participants were within an age range of anticipated transition from pediatric to adult care services; 57% reported that they had changed providers between the ages of 17 and 24. Participants with Type 1 diabetes were more likely to be male, be of Hispanic (41.1%) or White (27.2%) origin, and have higher levels of satisfaction with health care and overall personal health, anticipatory guidance, social support, and quality of life than were participants with Type 2 diabetes (see Table 2).
Potentially Modifiable Factors
Anticipatory guidance.
The mean number of anticipatory guidance topics the participants reported receiving was 4.4 ± 2.0 out of a maximum score of 6 for men (4.2 ± 2.0) and 7 for women (4.4 ± 1.9). Most emerging adults reported ever receiving information from a health care provider about having a dilated eye examination (85%), HbA1c testing (84%), blood pressure measurement (71%), blood test for cholesterol (64%), urine test for kidney function (60%), and foot examination (59%). Among women, 34% reported counseling regarding the importance of glucose control prior to pregnancy. Only 22% of the emerging adults surveyed reported receiving anticipatory guidance on all of these topics.
Diabetes informational or social activity.
The mean number of diabetes information or social activities reported was 0.9 ± 1.1 per respondent (range = 0–4). Emerging adults reported attendance at diabetes camp or participation in a diabetes walk-a-thon as 29% and 28%, respectively. Attendance at a diabetes support group was 22%, and 14% reported attending a diabetes expo or fair. About half (54%) of responders reported that they had ever participated in any of the diabetes-related informational or social activities.
Physical activity.
The mean number of physical activity days reported by respondents was 2.7 ± 2.1 in the previous week. Whereas 51% of emerging adults reported exercising ≥3 days out of the previous week, 20% did not exercise at all in the previous week.
Quality of life.
The mean total score on the PedsQL was 80.8 ± 16.5 (range = 2.2–100).
Positive Health Outcomes
Satisfaction with health care.
Satisfaction rating with health care received in the previous 12 months was positively correlated with the three modifiable factors: anticipatory guidance (r = .24, p < .0001), social supports (r = .16, p = .0031), and PedsQL total score (r = .23, p = .0005).
The odds of reporting higher satisfaction with health care received (score of 7–8 or 9–10) were significantly higher among women Blacks, and those who reported their most recent HbA1c compared to the remainder of the study population. There was no significant difference of modifiable factors when stratified by type of diabetes. When significant predetermined factors were held constant (e.g., gender, ethnicity, type of diabetes, change in provider), the odds of being more satisfied with one’s health care were 1.3 times higher for each additional anticipatory guidance topic that participants reported discussing with a health care provider and 1.3 times higher for each 10-unit increase in total PedsQL score (see Table 3). The odds ratios for frequency of physical activity and diabetes informational or social activity were 1.1 and 0.9, respectively, which were not statistically significant.
Overall personal health.
Ratings of personal health were positively correlated with all four modifiable factors: anticipatory guidance (r = .20, p = .002), diabetes informational or social activity (r = .11, p = .03), physical activity (r = .17, p = .0014), and PedsQL total score (r = .53, p < .0001).
The odds of reporting better overall personal health (good or very good/excellent) were significantly higher for men than women and Whites than other racial or ethnic groups. When significant predetermined factors were held constant, the odds of better personal health ratings were 1.2 times higher if the participant received anticipatory guidance and 2.1 times higher for each 10-unit increase in total PedsQL (see Table 3). The odds ratios for frequency of physical activity and diabetes informational or social activity were 1.0 and 1.2, respectively, which were not statistically significant.
Hemoglobin A1c.
Approximately half the sample (53%, n = 179) reported their most recent HbA1c when answering the survey. When comparing HbA1c reporters to those who did not report their HbA1c, there were no statistically significant differences in age, gender, or change in health care provider. However, reporters of their recent HbA1c were more likely to have Type 1 diabetes (p < .0001), longer duration of diabetes (11.9 ± 3.8 vs. 10.8 ± 3.6 years, p = .0057), and be non-Hispanic White (p < .0001). Reporters also had significantly higher satisfaction rating of health care received (7.8 ± 2.0 vs. 7.0 ± 2.6, p = .001) and overall personal health rating (3.2 ± 0.9 vs. 2.8 ± 0.9, p < .0001).
The HbA1c level among the subset of participants who reported their most recent HbA1c was evaluated in additional analysis. A small percentage (8.8%) met target HbA1c < 7.0% (American Diabetes Association, 2016). Reported HbA1c level was not associated with provider change (p = .11). For participants who did not change provider, mean HbA1c was 8.2% (SD = 1.88). For those who did change provider, mean HbA1c was 8.7% (SD = 2.0). Among reporters, HbA1c level was inversely correlated with two of the four modifiable factors: anticipatory guidance (r = −0.21, p < .01) and PedsQL total score (r = −0.23, p < .05). However, after adjustment for predetermined characteristics (age, duration of diabetes, gender, race or ethnicity, diabetes type, provider change), there were no significant relationships between the reported HbA1c values and any of the four studied modifiable factors. Overall personal health ratings were inversely related to HbA1c level (r = −.40, p < .0001).
Discussion
Although it is recognized that emerging adults with diabetes are at risk for lapses in care and deteriorating glycemic control (Garvey, Wolpert, et al., 2012; Lyons, Becker, & Helgeson, 2014; Peters, Laffel, & the American Diabetes Association Transitions Working Group, 2011), in this study a majority (70%) of participants rated satisfaction with health care ≥7 out of 10 and most (71%) rated overall health as good, very good, or excellent. Previous studies have focused on associations between morbidity and mortality and nonmodifiable risk factors (gender, socioeconomic status, type and duration of diabetes; Bryden et al., 2003; Garvey, Markowitz, & Laffel, 2012; Lotstein et al., 2013; Peters, Laffel, & the American Diabetes Association Transitions Working Group, 2011; Rydall et al., 1997). In contrast, the current study uses a resilience model to describe relationships between potentially modifiable factors and patient-reported outcomes of high satisfaction with health care and overall health among a cohort of ethnically and racially diverse emerging adults with longstanding diabetes, over half of whom had experienced a change in provider between the ages of 17 and 24, when transfer to adult care providers is anticipated.
In the HRM, modifiable factors that result in better-than-anticipated outcomes are protective and considered buffering factors. After controlling for relevant predetermined characteristics, we found that the odds of having increased levels of satisfaction with both health care and overall personal health ratings were greater when the participants received more anticipatory guidance and had higher PedsQL scores. Satisfaction with health care was independent of whether the emerging adults reported a change in provider between the ages of 17 and 24, suggesting that transfer of care is not necessarily a determinant of this component of health satisfaction. Overall personal health ratings were lower for participants with a change in provider despite no differences in HbA1c levels associated with provider change, which is consistent with the view that overall health is a broader construct than is a single measure of glycemic control. Further investigation into preparation for transition, lapses in services between leaving pediatrics and establishing adult care, and receivership into adult practices are all potential areas for study to better define the process of provider change. The SMART model of transition readiness has been applied to survivors of childhood cancer (Schwartz et al., 2011) and sickle-cell disease (Mulchan, Valenzuela, Crosby, & Diaz Pow Sang, 2016) and could prove a useful framework for diabetes transition research and clinical practice. Results of the current study suggest that clinical interventions that focus on anticipatory guidance and quality of life may mitigate the deterioration in care and clinical outcomes often reported among emerging adults during transition and post transfer to adult care.
Anticipatory guidance is a mechanism by which emerging adults may become knowledgeable about health-promoting opportunities (e.g., maintenance of blood pressure control, glucose control prior to pregnancy; Committee on Practice and Ambulatory Medicine & Bright Futures Periodicity Schedule Workgroup, 2014; Irwin, Adams, Park, & Newacheck, 2009). This study found a positive relationship between greater levels of anticipatory guidance and both increased satisfaction with health care and ratings of overall personal health. However, only 22% of participants reported receiving anticipatory guidance on all surveyed diabetes topics. Specifically, fewer than 65% of responders reported that a health care provider had ever discussed the need for urine tests for kidney function, blood test for cholesterol monitoring, foot exams, or (among women) the importance of glucose control prior to pregnancy. Although it is possible that recall of discussed topics underestimates anticipatory guidance provided, there remains an opportunity to improve the delivery of consistent and effective anticipatory guidance for emerging adults with diabetes as well as evidence to suggest that doing so can promote positive health outcomes. For example, both pediatric and adult clinicians can improve anticipatory guidance through individualized assessment of knowledge, referral to relevant diabetes education classes or resources, routine discussion of screening and prevention expectations at clinic visits, list of external specialist resources, and handouts or online materials that reinforce verbal education and outline various diabetes topics.
The PedsQL is a composite measure of quality of life including multiple domains of physical, emotional, social, and work or school functioning (Varni & Limbers, 2009). Each of these domains may provide an important arena for intervention to promote health outcomes. As may be expected, higher total PedsQL scores correlated with higher satisfaction regarding health care received and overall current health. Of note, previous SEARCH studies have indicated that among youth with Type 2 diabetes, health-related quality of life is lower compared to those with Type 1 diabetes (e.g., Naughton et al., 2008). These findings highlight that demographic or other predetermined factors, such as type of diabetes, are interrelated with modifiable factors and health outcomes.
Diabetes informational or social activity and exercise frequency were hypothesized to be positively associated with the two health satisfaction outcomes; however, these factors were not statistically significant in the proportional odds regression analyses. The lack of a significant association of either diabetes information or social activity or exercise with health outcomes may be due to the wording of the survey items rather than the absence of a true effect. For example, the measure of diabetes informational or social activity did not include aspects of peer, family, or community support or participation in the diabetes online community, which may be more significant contributors than is participation in a diabetes walk-a-thon (see the Appendix in the online supplemental materials for full item details). Beneficial effects of exercise among those with diabetes are described in numerous studies (e.g., Riddell, Miadovnik, Simms, Li, & Zisser, 2013), but reported days of exercise within the past week did not correlate to health satisfaction ratings in this analysis. Therefore, reported days of activity may not be the most accurate mechanism to measure the construct of exercise.
Poor HbA1c recall has been associated with unhealthy eating behaviors, low levels of exercise, worse glycemic control, and lower patient activation scores (Willaing, á Rogvi, Bogelund, Almdal, & Schiotz, 2013). In the current study, participants who reported their most recent HbA1c had higher health care satisfaction scores and overall personal health ratings. This suggests that, consistent with prior studies, recall of HbA1c may reflect a proxy for level of patient engagement that contributes to health-promoting behaviors. Indeed, accurate knowledge and recall of one’s personal and target HbA1c level may be another important modifiable buffering factor.
This study includes a large and diverse sample of participants drawn from the SEARCH study that provides a unique opportunity to explore positive health outcomes among a wide variety of emerging adults with diabetes, particularly subpopulations with historically high risk for worse outcomes. Understanding modifiable factors that may help high-risk groups succeed could have a significant impact for intervention development. This study has several limitations. The potentially modifiable factors included in the proposed HRM were derived from survey responses in a data set of emerging adults with Type 1 or Type 2 diabetes and do not reflect a comprehensive consideration of all possible influences. The study is cross-sectional and reflects one point in time along the trajectory of a chronic condition. Responses are self-reported and comparison to medical records for validation was not available. In addition, there are missing data, in particular to the question about participants’ most recent HbA1c level. The latter limits the power for the regression analysis in which glycemic control was the outcome variable. However, lack of report of the most recent HbA1c is also present in prior studies, in which 47%−77% of queried patients with diabetes did not know their most recent HbA1c level and few accurately reported the level (Beard, Clark, Hurel, & Cooke, 2010; Guirguis, Kieser, Chewning, & Kanous, 2007; Harwell et al., 2002; Heisler, Piette, Spencer, Kieffer, & Vijan, 2005). It is uncertain whether poor recall of HbA1c in this cohort reflects length of time from last visit or lack of knowledge or engagement.
Findings from this study highlight that future research into a more comprehensive recognition of modifiable factors within health delivery systems, social networks, and self-management practices and promotion of general health and wellbeing could inform the design of effective interventions aimed at improving health care and outcomes for emerging adults with diabetes. Development of meaningful patient-reported outcome measures that complement existing clinical measures is an important area for ongoing research to define multifaceted outcomes that are relevant to patients, clinicians, and researchers.
Conclusions
The proposed HRM seeks to reframe the study of emerging adults with longstanding diabetes from one of risk factors and morbidity to that of buffering factors and resilience. The HRM distinguishes predetermined characteristics from modifiable factors associated with positive patient-reported health outcomes in order to discern candidate areas for potential interventions. Recognition of modifiable factors associated with higher satisfaction with health care and overall health, including more consistent and effective anticipatory guidance, may contribute to future studies of resilience promoting interventions aimed at improving clinical and psychosocial outcomes for emerging adults with diabetes.
Supplementary Material
Acknowledgments
This study was conducted for the SEARCH for Diabetes in Youth Study group, which is indebted to the many youth and their families, as well as their health care providers, whose participation made this study possible. SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Site Contract Numbers: Kaiser Permanente Southern California (U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Kuakini Medical Center (U58CCU919256 and U01 DP000245), Children’s Hospital Medical Center (Cincinnati) (U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01 DP000254, and U18DP002708), University of Washington School of Medicine (U58/CCU019235-4, U01 DP000244, and U18DP002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01 DP000250, and 200-2010-35171).
The authors wish to acknowledge the involvement of General Clinical Research Center at the South Carolina Clinical & Translational Research Institute at the Medical University of South Carolina (NIH/NCRR Grant UL1RR029882); Seattle Children’s Hospital (NIH CTSA Grant UL1 TR00423 of the University of Washington); University of Colorado Pediatric Clinical and Translational Research Center (Grant UL1 TR000154) and the Barbara Davis Center at the University of Colorado at Denver (DERC NIH P30 DK57516); the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8 UL1 TR000077; and the Children with Medical Handicaps program managed by the Ohio Department of Health.
The authors acknowledge the editorial assistance and contributions of Ronny A. Bell of the Department of Epidemiology and Prevention, Wake Forest School of Medicine.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Parts of this study were presented in abstract form at the 73rd Scientific Sessions of the American Diabetes Association, Chicago, IL, June 2013.
Supplemental materials: http://dx.doi.org/10.1037/hea0000419.supp
Contributor Information
Sarah D. Corathers, Division of Endocrinology, Children’s Hospital Medical Center, Cincinnati, Ohio
Jessica C. Kichler, Division of Behavioral Medicine and Clinical Psychology, Children’s Hospital Medical Center, Cincinnati, Ohio
Nora F. Fino, Department of Bio-statistical Sciences, Wake Forest School of Medicine
Wei Lang, Department of Bio-statistical Sciences, Wake Forest School of Medicine.
Jean M. Lawrence, Department of Research & Evaluation, Kaiser Permanente Southern California, Pasadena, California
Jennifer K. Raymond, The Barbara Davis Center for Childhood Diabetes, University of Colorado
Joyce P. Yi-Frazier, Department of Pediatrics, University of Washington School of Medicine
Dana Dabelea, Department of Epidemiology, Colorado School of Public Health.
Angela D. Liese, Department of Epidemiology and Biostatistics and Center for Research in Nutrition and Health Disparities, University of South Carolina
Sharon H. Saydah, Division of Diabetes Translation, Centers for Disease Control and Prevention, Atlanta, Georgia
Michael Seid, Division of Pulmonary Medicine and the Anderson Center for Health Systems Excellence, Children’s Hospital Medical Center, Cincinnati, Ohio.
Lawrence M. Dolan, Division of Endocrinology, Children’s Hospital Medical Center, Cincinnati, Ohio
References
- American Diabetes Association. (2016). 5. Glycemic targets. Diabetes Care, 39(Suppl. 1), S39–S46. 10.2337/dc16-S008 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Beard E, Clark M, Hurel S, & Cooke D (2010). Do people with diabetes understand their clinical marker of long-term glycemic control (HbA1c levels) and does this predict diabetes self-care behaviours and HbA1c? Patient Education and Counseling, 80, 227–232. 10.1016/j.pec.2009.11.008 [DOI] [PubMed] [Google Scholar]
- Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, & Soren K (2013). Mental health issues in adolescents and young adults with type 1 diabetes: Prevalence and impact on glycemic control. Clinical Pediatrics, 52, 10–15. 10.1177/0009922812459950 [DOI] [PubMed] [Google Scholar]
- Bryden KS, Dunger DB, Mayou RA, Peveler RC, & Neil HAW (2003). Poor prognosis of young adults with type 1 diabetes: A longitudinal study. Diabetes Care, 26, 1052–1057. 10.2337/diacare.26.4.1052 [DOI] [PubMed] [Google Scholar]
- Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, & Dunger DB (2001). Clinical and psychological course of diabetes from adolescence to young adulthood: A longitudinal cohort study. Diabetes Care, 24, 1536–1540. 10.2337/diacare.24.9.1536 [DOI] [PubMed] [Google Scholar]
- Committee on Practice and Ambulatory Medicine & Bright Futures Periodicity Schedule Workgroup. (2014). 2014 recommendations for pediatric preventive health care. Pediatrics, 133, 568–570. 10.1542/peds.2013-4096 [DOI] [PubMed] [Google Scholar]
- Feltbower RG, Bodansky HJ, Patterson CC, Parslow RC, Stephenson CR, Reynolds C, & McKinney PA (2008). Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: Results from the Yorkshire Register of diabetes in children and young adults. Diabetes Care, 31, 922–926. 10.2337/dc07-2029 [DOI] [PubMed] [Google Scholar]
- Garvey KC, Markowitz JT, & Laffel LM (2012). Transition to adult care for youth with type 1 diabetes. Current Diabetes Reports, 12, 533–541. 10.1007/s11892-012-0311-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Wolpert HA, Rhodes ET, Laffel LM, Kleinman K, Beste MG, … Finkelstein JA (2012). Health care transition in patients with type 1 diabetes: Young adult experiences and relationship to glycemic control. Diabetes Care, 35, 1716–1722. 10.2337/dc11-2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey M, Whittemore R, & Tamborlane W (2002). Depression in Type 1 diabetes in children: Natural history and correlates. Journal of Psychosomatic Research, 53, 907–911. 10.1016/S0022-3999(02)00312-4 [DOI] [PubMed] [Google Scholar]
- Guirguis LM, Kieser MA, Chewning BA, & Kanous NL (2007). Recall of A1C, blood pressure, and cholesterol levels among community pharmacy patients with diabetes. Journal of the American Pharmacists Association, 47, 29–34. 10.1331/1544-3191.47.1.29.Guirguis [DOI] [PubMed] [Google Scholar]
- Hamman RF, Bell RA, Dabelea D, D’Agostino RB Jr., Dolan L, Imperatore G, … Saydah S (2014). The SEARCH for Diabetes in Youth study: Rationale, findings, and future directions. Diabetes Care, 37, 3336–3344. 10.2337/dc14-0574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwell TS, Dettori N, McDowall JM, Quesenberry K, Priest L, Butcher MK, … Gohdes D (2002). Do persons with diabetes know their (A1C) number? Diabetes Educator, 28, 99–105. 10.1177/014572170202800111 [DOI] [PubMed] [Google Scholar]
- Heisler M, Piette JD, Spencer M, Kieffer E,& Vijan S (2005). The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care, 28, 816–822. 10.2337/diacare.28.4.816 [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Harris MA, & Weissberg-Benchell J (2012). Diabetes resilience: A model of risk and protection in type 1 diabetes. Current Diabetes Reports, 12, 739–748. 10.1007/s11892-012-0314-3 [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Herzer M, Dolan LM, & Hood KK (2011). Psychological screening in adolescents with type 1 diabetes predicts outcomes one year later. Diabetes Research and Clinical Practice, 94, 39–44. 10.1016/j.diabres.2011.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, McQuaid EL, Nabors L, & Hood KK (2015). Resilience in youth and families living with pediatric health and developmental conditions: Introduction to the special issue on resilience. Journal of Pediatric Psychology, 40, 835–839. 10.1093/jpepsy/jsv072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood KK, Huestis S, Maher A, Butler D, Volkening L, & Laffel LM (2006). Depressive symptoms in children and adolescents with type 1 diabetes: Association with diabetes-specific characteristics. Diabetes Care, 29, 1389–1391. 10.2337/dc06-0087 [DOI] [PubMed] [Google Scholar]
- Irwin CE Jr., Adams SH, Park MJ, & Newacheck PW (2009). Preventive care for adolescents: Few get visits and fewer get services. Pediatrics, 123(4), e565–e572. 10.1542/peds.2008-2601 [DOI] [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Obrosky DS, & Bonar LK (1997). Psychiatric disorders in youths with IDDM: Rates and risk factors. Diabetes Care, 20, 36–44. 10.2337/diacare.20.1.36 [DOI] [PubMed] [Google Scholar]
- Li J, Yuan L, Wu Y, Luan Y, & Hao Y (2013). The Chinese version of the Pediatric Quality of Life Inventory™ (PedsQL™) Healthcare Satisfaction Generic Module (Version 3.0): Psychometric evaluation. Health and Quality of Life Outcomes, 11, 113 10.1186/1477-7525-11-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotstein DS, Seid M, Klingensmith G, Case D, Lawrence JM, Pihoker C, … Waitzfelder B (2013). Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics, 131(4), e1062–e1070. 10.1542/peds.2012-1450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71, 543–562. 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons SK, Becker DJ, & Helgeson VS (2014). Transfer from pediatric to adult health care: Effects on diabetes outcomes. Pediatric Diabetes, 15, 10–17. 10.1111/pedi.12106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulchan SS, Valenzuela JM, Crosby LE, & Diaz Pow Sang C (2016). Applicability of the SMART model of transition readiness for sickle-cell disease. Journal of Pediatric Psychology, 41, 543–554. 10.1093/jpepsy/jsv120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naughton MJ, Ruggiero AM, Lawrence JM, Imperatore G, Klingensmith GJ, Waitzfelder B,… SEARCH for Diabetes in Youth Study Group. (2008). Health-related quality of life of children and adolescents with type 1 or type 2 diabetes mellitus: SEARCH for Diabetes in Youth study. Archives of Pediatrics & Adolescent Medicine, 162, 649–657. 10.1001/archpedi.162.7.649 [DOI] [PubMed] [Google Scholar]
- Pascoe GC (1983). Patient satisfaction in primary health care: A literature review and analysis. Evaluation and Program Planning, 6(3–4): 185–210. 10.1016/0149-7189(83)90002-2 [DOI] [PubMed] [Google Scholar]
- Peters A, & Laffel L, & the American Diabetes Association Transitions Working Group. (2011). Diabetes Care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care, 34, 2477–2485. 10.2337/dc11-1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce JS,& Wysocki T (2015). Topical review: Advancing research on the transition to adult care for type 1 diabetes. Journal of Pediatric Psychology, 40, 1041–1047. 10.1093/jpepsy/jsv064 [DOI] [PubMed] [Google Scholar]
- Riddell MC, Miadovnik L, Simms M, Li B, & Zisser H (2013). Advances in exercise, physical activity, and diabetes mellitus. Diabetes Technology & Therapeutics, 15(Suppl. 1), S96–S106. 10.1089/dia.2013.1511 [DOI] [PubMed] [Google Scholar]
- Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, & Daneman D (1997). Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. New England Journal of Medicine, 336, 1849–1854. 10.1056/NEJM199706263362601 [DOI] [PubMed] [Google Scholar]
- Schwartz LA, Tuchman LK, Hobbie WL, & Ginsberg JP (2011). A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child: Care, Health and Development, 37, 883–895. 10.1111/j.1365-2214.2011.01282.x [DOI] [PubMed] [Google Scholar]
- SEARCH Study Group. (2004). SEARCH for Diabetes in Youth: A multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Controlled Clinical Trials, 25, 458–471. 10.1016/j.cct.2004.08.002 [DOI] [PubMed] [Google Scholar]
- Varni JW, & Limbers CA (2009). The PedsQL 4.0 Generic Core Scales Young Adult Version: Feasibility, reliability and validity in a university student population. Journal of Health Psychology, 14, 611–622. 10.1177/1359105309103580 [DOI] [PubMed] [Google Scholar]
- Waitzfelder B, Pihoker C, Klingensmith G, Case D, Anderson A, Bell RA,… Seid M (2011). Adherence to guidelines for youths with diabetes mellitus. Pediatrics, 128, 531–538. 10.1542/peds.2010-3641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Wolpert H, & Anderson BJ (2007). Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care, 30, 2441–2446. 10.2337/dc07-1249 [DOI] [PubMed] [Google Scholar]
- Willaing I, á Rogvi SA, Bøgelund M, Almdal T, & Schiøtz M (2013). Recall of HbA1c and self-management behaviours, patient activation, perception of care and diabetes distress in Type 2 diabetes. Diabetic Medicine, 30(4), e139–e142. 10.1111/dme.12121 [DOI] [PubMed] [Google Scholar]
- Wills CJ, Scott A, Swift PG, Davies MJ, Mackie AD, & Mansell P (2003). Retrospective review of care and outcomes in young adults with type 1 diabetes. British Medical Journal, 327, 260–261. 10.1136/bmj.327.7409.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi JP, Vitaliano PP, Smith RE, Yi JC, & Weinger K (2008). The role of resilience on psychological adjustment and physical health in patients with diabetes. British Journal of Health Psychology, 13, 311–325. 10.1348/135910707X186994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi-Frazier JP, Yaptangco M, Semana S, Buscaino E, Thompson V, Cochrane K, … Rosenberg AR (2015). The association of personal resilience with stress, coping, and diabetes outcomes in adolescents with type 1 diabetes: Variable- and person-focused approaches. Journal of Health Psychology, 20, 1196–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.