Abstract
Background:
It has been reported that women have higher 30-day readmission rates than men following acute coronary syndrome (ACS). However, readmission after percutaneous coronary intervention (PCI) for ACS is a distinct subset of patients in whom gender differences have not been adequately studied.
Methods:
Hawaii statewide hospitalization data from 2010–2015 were assessed to compare gender differences in 30-day readmission rates among patients hospitalized with ACS who received PCI during the index hospitalization. Readmission diagnoses were categorized using an aggregated version of the Centers for Medicare and Medicaid Services Condition Categories. Multivariable logistic regression was applied to evaluate the effect of gender on 30-day readmission rate.
Results:
A total of 5,354 patients (29.4% women) who were hospitalized with a diagnosis of ACS and received PCI were studied. Overall, women were older with more identified as Native Hawaiian, and had a higher prevalence of cardiovascular risk factors compared to men. Thirty-day readmission rate was 13.9% in women and 9.6% in men (p<0.0001). In the multivariable model, female gender (OR [95% CI]: 1.32 [1.09, 1.60]), Medicaid (1.48 [1.07, 2.06]), Medicare (1.72 [1.35, 2.19]), heart failure (1.88 [1.53, 2.33]), atrial fibrillation (1.54 [1.21, 1.95]), substance use (1.88 [1.27, 2.77]), history of gastrointestinal bleeding (2.43 [1.29, 4.58]), and chronic kidney disease (1.78 [1.42, 2.22]) were independent predictors of 30-day readmissions. Readmission rates were highest during day 1–6 (peak: day 3) after discharge. The top three cardiac causes of readmissions were heart failure, recurrent angina, and recurrent ACS.
Conclusion:
In conclusion, the female gender is an independent predictor for 30-day readmissions after ACS that requires PCI. Our finding suggests women are at a higher risk of post-ACS cardiac events such as heart failure and recurrent ACS, and further gender specific intervention is needed to reduce 30-day readmission rate in women following ACS.
INTRODUCTION
Reducing early hospital readmissions is considered an important goal for healthcare systems, as readmission rate is often proposed as a marker for quality of care (Ashton, Del Junco, Souchek, Wray, & Mansyur, 1997; Ashton, Kuykendall, Johnson, Wray, & Wu, 1995; Ashton & Wray, 1996; Jencks, 2010). Acute coronary syndrome (ACS) is a crucial target in this effort since it affects approximately 625,000 people each year in the United States, of whom an estimated 363,000 are men and 262,000 are women (Benjamin et al., 2017), (Berger et al., 2009). ACS patients who are readmitted within 30 days have higher morbidity and incur greater healthcare costs than patients who are not readmitted (Dharmarajan et al., 2017; McManus et al., 2012). There have been substantial recent efforts to identify ACS patients who are at risk for 30-day readmission (O’Brien et al., 2017; Ranasinghe et al., 2014), in the hope that identifying these patients in advance of discharge can improve outcomes, reduce costs, and improve health care quality.
Gender differences in outcomes such as mortality, length of stay, and readmission after ACS have been previously described, with a higher rate of readmission in women when compared to men (Dreyer, Dharmarajan, Kennedy, et al., 2017; Dreyer et al., 2015; Hess et al., 2017; Izadnegahdar et al., 2014; O’Brien et al., 2017). However, these studies include a heterogeneous population of ACS patients regardless of whether percutaneous coronary intervention (PCI) was performed during the index hospitalization. PCI utilization defines a subset of patients with relative homogeneous pathophysiology, including potentially treatable lesions and sufficiently good health to be a candidate for the procedure. Therefore, we sought to assess gender differences in the rate of 30-day readmissions in patients with admission diagnosis of ACS who required PCI.
METHODS
We received approval from the University of Hawaii Institutional Review Board to conduct a retrospective study on all patients hospitalized in the state of Hawaii between January 1, 2010 and December 31, 2015. The data were obtained from the Hawaii Health Information Corporation (HHIC). HHIC compiles patient-level discharge data for all acute care hospitalizations in Hawaii by all payers. The data set included patient demographics (such as insurer, age, gender, and home address), International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) primary diagnosis, secondary diagnosis, and procedure codes. Race/ethnicity information was categorized based on self-report.
Inclusion criteria for this study consisted of patients with a discharge ICD-9-CM primary diagnosis code of acute myocardial infarction and/or acute coronary syndrome (ICD-9-CM 411.1x and 410.xx). Patients with ICD-9-CM codes of 410.x2 were excluded, as these codes indicate an old myocardial infarction. For inclusion, patients must have also received PCI during the index hospitalization, which was defined as ICD-9-CM code of 00.66, 36.01, 36.02, 36.05, 36.06, 36.07. All inpatients in the state of Hawaii discharged with the diagnosis of AMI/ACS who received a PCI between January 1, 2010 and December 31, 2015 were identified.
We excluded patients who were hospitalized at the Department of Defense hospital in Hawaii, as detailed race/ethnicity data were not available. Patients who were not residents of Hawaii were also excluded from this study, as we expect that many of these patients would return to their home state or country following discharge from the initial hospitalization and therefore be lost to follow up. Patients who expired during the index hospitalization or were transferred to another facility or hospice were also excluded.
Control variables
The following factors were selected a priori to be included in the multivariable models: age (<50 year old, 50–79 year old, and ≥80 year old), insurance (Medicaid, Medicare, private, and others), race/ethnicity (Chinese, Filipino, Japanese, Native Hawaiian, Pacific islanders, White, and other race), discharge diagnosis of hypertension, hyperlipidemia, diabetes mellitus, cigarette smoking, obesity, coronary artery disease, coronary arterial bypass grafting (CABG) surgery, heart failure, atrial fibrillation, peripheral artery disease, depression, other mental illness, gastrointestinal bleed, chronic kidney disease, pneumonia, stroke, and CABG surgery during index hospitalization. The risk factors for coronary artery disease at presentation of the index hospitalization were derived from the secondary discharge diagnosis codes. Other mental illness is defined as psychoses, neurotic disorders, personality disorders, other nonpsychotic mental disorders, and mental disorders related to pregnancy (ICD-9-CM code 295.xx – 302.xx, 306.xx – 314.xx, and 648.4x).
Outcome variables
Thirty-day readmission was defined as the first admission occurring within 30 days from the index hospitalization for any cause. Additional hospitalizations within the 30-day period were not counted as additional readmissions. Subsequent hospitalizations occurring after 30 days from the index hospitalization were counted as a separate independent index admission if the inclusion criteria are met (ACS with PCI). The readmission principle diagnoses were also derived from the ICD-9-CM codes from the readmission hospitalization. The diagnoses were then re-categorized into 30 modified condition categories, using an aggregated version of the Centers for Medicare and Medicaid Services Condition Categories, which assemble the diagnoses into more meaningful clinical categories. The timing of readmission was calculated from the day after discharge.
Statistical Analysis
Baseline characteristics were compared using Chi-squared tests or Fisher’s exact tests for demographic and clinical variables. Multivariable adjusted odds ratios (OR) and their 95% confidence intervals were obtained with a logistic regression model. To assess potential gender differences in the timing of 30-day readmission, a log-rank test was performed and a multivariable cox proportional hazards regression model was used to control the demographic or clinical factors. A secondary analysis assessed whether there was an interaction between gender and age group. All data analyses were performed in SAS 9.3 (Cary, N.C., 2011). A two-tailed p-value of less than 0.05 was regarded as statistically significant.
RESULTS
We evaluated 5,354 patients with index hospitalizations with the diagnosis of ACS who underwent PCI. The clinical characteristics of the 5,354 patients are shown in Table 1. Of the 5,354 hospitalizations, 1578 (29%) were women and 3,776 (71%) were men. Women in this study were older than men (≥80 years: 19.2% vs. 10.1%; 50–79 years: 70.3% vs. 74.6%; <50 years: 10.5% vs. 15.3%, p<0.0001). There were also more Native Hawaiian women (18.9% vs. 12.4%) and fewer Caucasian women (23.5% vs. 32.6%) (chi-square of racial/ethnic groups, p<0.0001). Women also had a higher prevalence of hypertension (82.5% vs. 73.6%, p<0.0001), diabetes mellitus (47.9% vs. 35.6%, p<0.0001), obesity (16.6% vs. 13.7%, p=0.006), heart failure (21.2% vs. 15.9%, p<0.0001), depression (3.4% vs 2.2%, p=0.01), other mental illness (9.1% vs. 6.6%, p=0.002), and chronic kidney disease (20.7% vs. 16.7%, p=0.0005); and a lower prevalence of smoking (36.1% vs. 43.8%, <0.0001) and substance use (2.5% vs. 5.2%, p<0.0001).
Table 1.
Clinical Characteristics, by Gender
| Female N = 1578 | Male N = 3776 | P-value | |
|---|---|---|---|
| Age | <0.0001 | ||
| <50 | 166 (10.5%) | 578 (15.3%) | |
| 50–79 | 1,109 (70.3%) | 2,816 (74.6%) | |
| 80+ | 303 (19.2%) | 382 (10.1%) | |
| Insurance | <0.0001 | ||
| Private | 396 (25.1%) | 1,487 (39.4%) | ref |
| Medicaid | 192 (12.2%) | 432 (11.4%) | <0.0001 |
| Medicare | 907 (57.5%) | 1,505 (39.9%) | <0.0001 |
| Others | 83 (5.3%) | 352 (9.3%) | 0.3700 |
| Race | <0.0001 | ||
| White | 371 (23.5%) | 1,231 (32.6%) | ref |
| Chinese | 64 (4.1%) | 167 (4.4%) | 0.1300 |
| Filipino | 290 (18.4%) | 634 (16.8%) | <0.0001 |
| Japanese | 295 (18.7%) | 710 (18.8%) | 0.0004 |
| Native Hawaiian | 298 (18.9%) | 469 (12.4%) | <0.0001 |
| Pacific Islander | 89 (5.6%) | 218 (5.8%) | 0.0029 |
| Other race | 171 (10.8%) | 347 (9.2%) | <0.0001 |
| Medical history | |||
| Hypertension | 1,302 (82.5%) | 2,781 (73.6%) | <0.0001 |
| Diabetes | 756 (47.9%) | 1,343 (35.6%) | <0.0001 |
| Hyperlipidemia | 1,175 (74.5%) | 2,793 (74.0%) | 0.7066 |
| Smoking | 570 (36.1%) | 1,652 (43.8%) | <0.0001 |
| Obesity | 262 (16.6%) | 517 (13.7%) | 0.0059 |
| Coronary artery disease | 1,475 (93.5%) | 3,509 (92.9%) | 0.4745 |
| History of CABG | 56 (3.5%) | 167 (4.4%) | 0.1445 |
| Heart Failure | 335 (21.2%) | 599 (15.9%) | <0.0001 |
| Atrial fibrillation | 177 (11.2%) | 444 (11.8%) | 0.5725 |
| Peripheral artery disease | 24 (1.5%) | 57 (1.5%) | 0.9752 |
| Depression | 53 (3.4%) | 82 (2.2%) | 0.0115 |
| Other mental illness | 144 (9.1%) | 251 (6.6%) | 0.0016 |
| Substance use | 39 (2.5%) | 197 (5.2%) | <0.0001 |
| History of GI bleeding | 18 (1.1%) | 34 (0.9%) | 0.4138 |
| Chronic kidney disease | 326 (20.7%) | 629 (16.7%) | 0.0005 |
| Index hospitalization | |||
| CABG procedure | 15 (1.0%) | 52 (1.4%) | 0.2005 |
| Stroke | 17 (1.1%) | 23 (0.6%) | 0.0697 |
| Pneumonia | 64 (4.1%) | 147 (3.9%) | 0.7802 |
There were 583 30-day readmissions in this study (11% of subjects). The readmission rate for women was 13.9%, compared to 9.6% for men (p<0.0001). In univariate analyses, as shown in Table 2, a higher proportion of patients with 30-day readmission were 80 years old and above (18.9% vs. 12.1%, p<0.0001). Also, a higher proportion of patients with 30-day readmission had Medicare insurance compared to other types of insurance coverage (61.2% vs 43.1%, p<0.0001). No statistically significant differences were seen between race/ethnicity in 30-day readmission after ACS. Patients with 30day readmission had higher prevalence of hypertension (82.2% vs 75.5%, p<0.0004), diabetes mellitus (49.6% vs 37.9%, p<0.0001), heart failure (33.8% vs 15.4%, p<0.0001), atrial fibrillation (20.4% vs 10.5%, p<0.0001), peripheral artery disease (3.1% vs 1.3%, p<0.001), chronic kidney disease (33.4% vs 15.9%, p<0.0001), gastrointestinal bleed (2.7% vs 0.8%, p<0.0001), substance use (6.5% vs 4.2%, p=0.0086), and other mental illness (10.3% vs 7.0%, p=0.0044) than those who did not have 30-day readmission.
Table 2.
Clinical and Demographic Characteristics, by Readmission Status
| No 30-day readmission N = 4771 | 30-day readmission N = 583 | P-value | |
|---|---|---|---|
| Gender | <0.0001 | ||
| Female | 1,359 (28.5%) | 219 (37.6%) | |
| Male | 3,412 (71.5%) | 364 (62.4%) | |
| Age | <0.0001 | ||
| <50 | 690 (14.5%) | 54 (9.3%) | |
| 50–79 | 3,506 (73.5%) | 419 (71.9%) | |
| 80+ | 575 (12.1%) | 110 (18.9%) | |
| Insurance | <0.0001 | ||
| Medicaid | 557 (11.7%) | 67 (11.5%) | |
| Medicare | 2,055 (43.1%) | 357 (61.2%) | |
| Others | 400 (8.4%) | 35 (6.0%) | |
| Private | 1,759 (36.9%) | 124 (21.3%) | |
| Race/ethnicity | 0.1362 | ||
| Chinese | 203 (4.3%) | 28 (4.8%) | 0.2168 |
| Filipino | 821 (17.2%) | 103 (17.7%) | 0.1956 |
| Japanese | 884 (18.5%) | 121 (20.8%) | 0.0443 |
| Native Hawaiian | 669 (14.0%) | 98 (16.8%) | 0.0162 |
| Other race | 472 (9.9%) | 46 (7.9%) | 0.6513 |
| Pacific Islander | 273 (5.7%) | 34 (5.8%) | 0.4063 |
| Caucasian | 1,449 (30.4%) | 153 (26.2%) | ref |
| Medical history | |||
| Hypertension | 3,604 (75.5%) | 479 (82.2%) | 0.0004 |
| Diabetes | 1,810 (37.9%) | 289 (49.6%) | <0.0001 |
| Hyperlipidemia | 3,558 (74.6%) | 410 (70.3%) | 0.0269 |
| Smoking | 1,968 (41.2%) | 254 (43.6%) | 0.2835 |
| Obesity | 689 (14.4%) | 90 (15.4%) | 0.5197 |
| Coronary artery disease | 4,438 (93.0%) | 546 (93.7%) | 0.5694 |
| History of CABG | 195 (4.1%) | 28 (4.8%) | 0.4143 |
| Heart Failure | 737 (15.4%) | 197 (33.8%) | <0.0001 |
| Atrial fibrillation | 502 (10.5%) | 119 (20.4%) | <0.0001 |
| Peripheral artery disease | 63 (1.3%) | 18 (3.1%) | 0.0009 |
| Depression | 117 (2.5%) | 18 (3.1%) | 0.3558 |
| Other mental illness | 335 (7.0%) | 60 (10.3%) | 0.0044 |
| Substance use | 198 (4.2%) | 38 (6.5%) | 0.0086 |
| History of GI bleeding | 36 (0.8%) | 16 (2.7%) | <0.0001 |
| Chronic kidney disease | 760 (15.9%) | 195 (33.4%) | <0.0001 |
| Index hospitalization | |||
| CABG procedure | 64 (1.3%) | 3 (0.5%) | 0.0857 |
| Stroke | 33 (0.7%) | 7 (1.2%) | 0.1779 |
| Pneumonia | 169 (3.5%) | 42 (7.2%) | <0.0001 |
In the multivariable model, as shown in Table 3, female gender (OR [95% CI]: 1.32 [1.09, 1.60]), Medicaid (1.48 [1.07, 2.06]), Medicare (1.72 [1.35, 2.19]), heart failure (1.88 [1.53, 2.33]), atrial fibrillation (1.54 [1.21, 1.95]), substance use (1.88 [1.27, 2.77]), gastrointestinal bleeding (2.43 [1.29, 4.58]), and chronic kidney disease (1.78 [1.42, 2.22]) were independent predictors of 30-day readmissions. There was no significant interaction between gender and age groups (p=0.80).
Table 3.
Multivariable Analyses for 30-day Readmission
| Odds Ratio | 95% CI | ||
|---|---|---|---|
| Female | 1.32 | 1.09 | 1.60 |
| Age group | |||
| <50 | 0.78 | 0.51 | 1.17 |
| 50–79 | 0.93 | 0.72 | 1.21 |
| ≥80 (reference) | - | - | - |
| Race | |||
| Cascasian (reference) | - | - | - |
| Chinese | 1.18 | 0.76 | 1.85 |
| Filipino | 0.97 | 0.73 | 1.28 |
| Japanese | 1.10 | 0.84 | 1.43 |
| Native Hawaiian | 1.13 | 0.84 | 1.50 |
| Pacific Islander | 0.89 | 0.58 | 1.37 |
| Other race | 0.83 | 0.58 | 1.18 |
| Insurance | |||
| Private (reference) | - | - | - |
| Medicaid | 1.48 | 1.07 | 2.06 |
| Medicare | 1.72 | 1.35 | 2.19 |
| Other insurance | 1.21 | 0.81 | 1.80 |
| Medical history | |||
| Hypertension | 1.00 | 0.78 | 1.27 |
| Diabetes | 1.15 | 0.94 | 1.40 |
| Smoking | 1.15 | 0.96 | 1.38 |
| Obesity | 1.01 | 0.78 | 1.31 |
| Coronary artery disease | 0.93 | 0.65 | 1.34 |
| History of CABG | 0.90 | 0.59 | 1.37 |
| Heart failure | 1.89 | 1.53 | 2.33 |
| Atrial fibrillation | 1.54 | 1.21 | 1.95 |
| Peripheral artery disease | 1.65 | 0.94 | 2.88 |
| Depression | 1.21 | 0.72 | 2.05 |
| History of substance use | 1.88 | 1.27 | 2.77 |
| History of GI bleeding | 2.43 | 1.29 | 4.58 |
| Chronic kidney disease | 1.78 | 1.42 | 2.22 |
| Index hospitalization | |||
| CABG procedure | 0.33 | 0.10 | 1.07 |
| Stroke | 1.05 | 0.45 | 2.45 |
| Pneumonia | 1.16 | 0.80 | 1.68 |
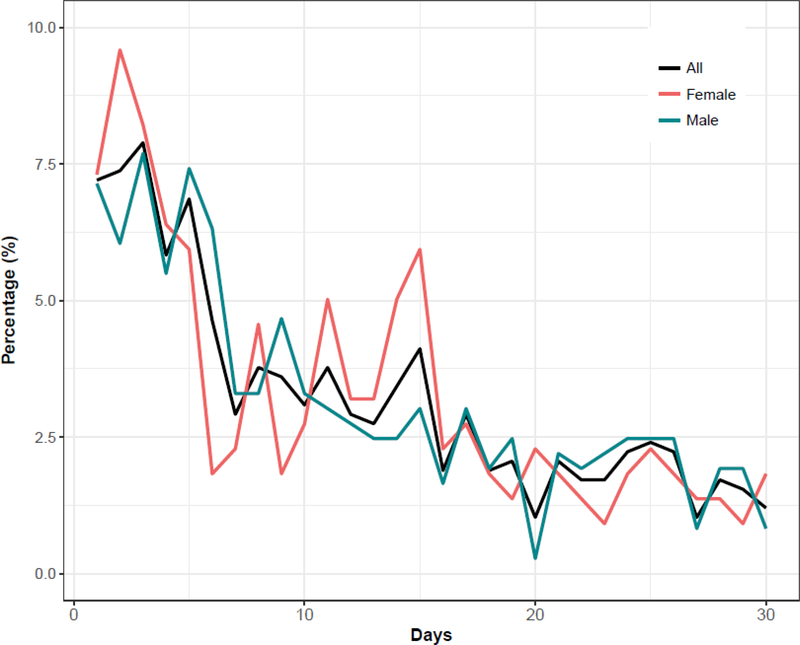
A list of the reasons for readmission, categorized into 30 modified condition categories, is shown in Table 4. The top three cardiac causes of readmission were heart failure, chronic angina, and recurrent ACS. Cardiac-related diagnoses accounted for 49.7% of the 30-day readmission diagnoses. The distribution of the causes of readmission differed by gender (p=0.044). As shown in Figure 1, readmission rates were highest during day 1–6 (peak: day 3) after discharge, accounting for 43.1% of 30-day readmissions. However, we did not find any significant difference of the timing of 30-day readmissions between women and men (p=0.98 from log-rank test; p=0.42 from cox regression model).
Table 4.
Top 15 Condition Categories for 30-day Readmission
| Diagnosis categories | Total N = 583 | Female N = 219 | Male N = 364 |
|---|---|---|---|
| Other | 90 (15.4%) | 38 (17.4%) | 52 (14.3%) |
| Heart failure | 83 (14.2%) | 36 (16.4%) | 47 (12.9%) |
| Chronic angina and coronary artery disease | 74 (12.7%) | 21 (9.6%) | 53 (14.6%) |
| Acute coronary syndrome | 70 (12.0%) | 31 (14.2%) | 39 (10.7%) |
| Arrhythmias and conduction disorder | 37 (6.4%) | 10 (4.6%) | 27 (7.4%) |
| Chest pain | 34 (5.8%) | 13 (5.9%) | 21 (5.8%) |
| Gastrointestinal hemorrhage | 24 (4.1%) | 11 (5.0%) | 13 (3.6%) |
| Pneumonia | 23 (4.0%) | 3 (1.4%) | 20 (5.5%) |
| Septicemia/Shock | 23 (4.0%) | 7 (3.2%) | 16 (4.4%) |
| Complications of care | 22 (3.8%) | 7 (3.2%) | 15 (4.1%) |
| Acute stroke/transient ischemic attack | 16 (2.7%) | 7 (3.2%) | 9 (2.5%) |
| Renal disorders (renal failure | 12 (2.1%) | 4 (1.8%) | 8 (2.2%) |
| Cardio-respiratory failure | 9 (1.5%) | 4 (1.8%) | 5 (1.4%) |
| Cellulitis | 8 (1.4%) | 5 (2.3%) | 3 (0.8%) |
| Diabetes and its complications | 8 (1.4%) | 6 (2.7%) | 2 (0.6%) |
| Other lung disorders | 8 (1.4%) | 2 (0.9%) | 6 (1.7%) |
| Other peripheral vascular disease | 8 (1.4%) | 6 (2.7%) | 2 (0.6%) |
Figure 1:
Timing of readmission after ACS and PCI between men and women
DISCUSSION
In this study, we compared the 30-day readmission rates between women and men of all ages after ACS hospitalization that required PCI. The overall 30-day readmission rate in our study was 11%, which is consistent with prior studies (Dreyer et al., 2015; Dunlay et al., 2012; Nuti et al., 2016). Our results suggest that after adjusting for confounders, women have a higher 30-day readmission rate compared to men in all age ranges, as supported by the lack of interaction between gender and age groups in the secondary analyses. Our analyses demonstrate that a higher proportion of those belonging to the older age group among women was not the major contributor for the higher readmissions among women. This is consistent with a number of previous studies (Dreyer et al., 2015; Khera et al., 2017). Overall, our analyses show that the female gender is an independent predictor for 30-day readmissions after ACS that requires PCI.
The top three diagnoses of readmissions (excluding the “other” category) were heart failure, recurrent angina, and recurrent ACS. In our data, women exhibited a higher rate of heart failure and recurrent ACS readmission diagnoses compared to men. This finding supports the possibility that women are at a higher risk for recurrent acute cardiac events following PCI for ACS. These cardiac events resulting in readmissions are likely from either natural sequelae post-ACS and complications from PCI procedures. For example, a delay in PCI resulting in ventricular dysfunction could lead to a heart failure readmission within days following discharge for ACS. Complications from PCI, such as coronary dissection or stent under-expansion, can result in recurrent ACS readmission, also within days following discharge for ACS. Indeed, some studies suggest women are more likely to have delayed PCI (Nguyen, Saczynski, Gore, & Goldberg, 2010) and PCI complications (Numasawa et al., 2015) for ACS. These findings also support other studies that showed a trend towards increasing length of stay and in-hospital mortality from recurrent cardiac events among women after ACS compared to men (Mehta et al., 2016) (Gupta et al., 2014).
Early readmission is an important concern in the United State healthcare system today, as national initiatives are focusing on improving quality of care by reducing preventable readmissions (Jencks, 2010; Kocher & Adashi, 2011). In our study, we found a peak of readmission during the first week out of hospital at day 3 for both women and men, which is similar to previous studies (Dharmarajan et al., 2013; Dreyer, Dharmarajan, Hsieh, et al., 2017). In our study, approximately half of the readmission diagnoses were cardiac-related. Early post-discharge intervention such as post-discharge telephonic follow up may help to reduce post-ACS readmission (Harrison, Hara, Pope, Young, & Rula, 2011). This study suggests, however, that earlier intervention within 3 days of discharge is critical in preventing readmission after ACS.
Our findings may be due to the healthcare disparities in care for women after ACS with PCI that other investigators have reported. Women have been shown to be more likely to delay seeking medical care longer than men (Nguyen et al., 2010), which may result in delays in revascularization and, subsequently, a higher rate of post-ACS complications and readmissions. Following ACS with PCI, women are also less likely to receive angiotensin-converting enzyme inhibitors, beta blockers, and statins on discharge (Shah et al., 2015). Women are also less likely to adhere to medications compared to men following ACS (Lauffenburger, Robinson, Oramasionwu, & Fang, 2014). These healthcare disparities are potential targets for healthcare systems to reduce rates of readmission following ACS and provide a higher quality of care.
This study has several limitations. First, the diagnosis of ACS and co-morbidities were derived from an administrative database, which may include inaccuracies in diagnostic coding. Many of the ICD-9-CM codes used to identify co-morbidities have not been verified by chart review and may have resulted in inaccurate representation. Further indepth clinical observational studies may elucidate the reasons for gender differences in readmission after ACS. Second, the patient’s risk factors for coronary artery disease were derived from the secondary discharge diagnosis codes, which may not necessarily reflect the patient’s risk factors upon admission. However, we speculate that most risk factors present at discharge are chronic conditions that are likely present on admission as well. Third, our data is limited to the state of Hawaii, which is comprised of an unusually diverse multiethnic population and may not be generalizable to the mainland United States or other countries. At the same time, the diverse population in Hawaii provides useful evidence for an increasingly multicultural US population, particularly including often understudied heterogeneous Asian and Pacific Islander populations. Fourth, readmissions occurring outside of Hawaii were not captured and thus additional readmission cases were potentially not included in the model. However, we speculate that these numbers are relatively small, and the exclusion of non-Hawaii residents from the study would not influence the generalizability to Hawaii residents. Fifth, without outpatient data, we could not assess the effects of outpatient accessibility and medication adherence factors in our model. Sixth, planned re-admissions for CABG and staged PCI cannot be excluded as they are not identified separately in our data. However, we speculate that the number of planned readmissions is relatively small compared to unplanned readmissions. Finally, variables that could have affected 30-day readmission rate, such as medication at the time of infarction and treatment for cardiac co-morbidities, cannot be accounted for.
CONCLUSIONS
Female gender is an independent predictor for 30-day readmissions after acute coronary syndrome that requires percutaneous intervention. This difference persists after extensive adjustment for clinical variables. Our finding suggests women are at a higher risk of post-ACS cardiac events such as heart failure and recurrent ACS, and that further gender-specific intervention is needed to reduce the 30-day readmission rate in women following ACS.
IMPLICATIONS FOR PRACTICE AND/OR POLICY
Readmission rate is frequently used by hospital administrations as an indicator of the quality of inpatient care. Early readmission, typically defined as readmission within 30 days of index hospitalization, is frequently equated with relatively low/substandard quality of care. However, our findings suggest that gender plays a role in readmission rate. This complicates the use of readmission rate as a sole parameter of the quality of care provided by inpatient practitioners, as practitioners who see a higher percentage of women may have a higher readmission rate. The study also highlights potential healthcare disparities in the care of women diagnosed with ACS undergoing PCI. Prompt referral to cardiology for PCI revascularization, appropriate medical treatment at discharge, and improvement in medication adherence through early post-discharge follow-up within 3 days are some potential targets for improving quality of care and reducing 30-day readmission after ACS for women.
Acknowledgements:
Sources of Funding: The research described was supported by National Institute on Minority Health and Health Disparities (NIMHD) grant P20MD000173, U54MD007584 and U54MD00760131, National Institute of General Medical Sciences (NIGMS) grant GM103341, and GM113134, and Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. grant RO1HS019990.
Footnotes
Conflict of Interest/Disclosure: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Ashton CM, Del Junco DJ, Souchek J, Wray NP, & Mansyur CL (1997). The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care, 35(10), 1044–1059. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Kuykendall DH, Johnson ML, Wray NP, & Wu L (1995). The association between the quality of inpatient care and early readmission. Ann Intern Med, 122(6), 415–421. [DOI] [PubMed] [Google Scholar]
- Ashton CM, & Wray NP (1996). A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med, 43(11), 1533–1541. [DOI] [PubMed] [Google Scholar]
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, … Stroke Statistics, S. (2017). Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation, 135(10), e146–e603. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, … Douglas PS (2009). Sex differences in mortality following acute coronary syndromes. JAMA, 302(8), 874–882. doi: 10.1001/jama.2009.1227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, … Krumholz HM (2013). Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA, 309(4), 355–363. doi: 10.1001/jama.2012.216476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharmarajan K, Wang Y, Lin Z, Normand ST, Ross JS, Horwitz LI, … Krumholz HM (2017). Association of Changing Hospital Readmission Rates With Mortality Rates After Hospital Discharge. JAMA, 318(3), 270–278. doi: 10.1001/jama.2017.8444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreyer RP, Dharmarajan K, Hsieh AF, Welsh J, Qin L, & Krumholz HM (2017). Sex Differences in Trajectories of Risk After Rehospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia. Circ Cardiovasc Qual Outcomes, 10(5). doi: 10.1161/CIRCOUTCOMES.116.003271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreyer RP, Dharmarajan K, Kennedy KF, Jones PG, Vaccarino V, Murugiah K, … Krumholz HM (2017). Sex Differences in 1-Year All-Cause Rehospitalization in Patients After Acute Myocardial Infarction: A Prospective Observational Study. Circulation, 135(6), 521–531. doi: 10.1161/CIRCULATIONAHA.116.024993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreyer RP, Ranasinghe I, Wang Y, Dharmarajan K, Murugiah K, Nuti SV, … Krumholz HM (2015). Sex Differences in the Rate, Timing, and Principal Diagnoses of 30-Day Readmissions in Younger Patients with Acute Myocardial Infarction. Circulation, 132(3), 158–166. doi: 10.1161/CIRCULATIONAHA.114.014776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, & Roger VL (2012). Thirty-day rehospitalizations after acute myocardial infarction: a cohort study. Ann Intern Med, 157(1), 11–18. doi: 10.7326/0003-4819-157-1-201207030-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, … Krumholz HM (2014). Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol, 64(4), 337–345. doi: 10.1016/j.jacc.2014.04.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison PL, Hara PA, Pope JE, Young MC, & Rula EY (2011). The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag, 14(1), 27–32. doi: 10.1089/pop.2009.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess CN, Kaltenbach LA, Doll JA, Cohen DJ, Peterson ED, & Wang TY (2017). Race and Sex Differences in Post-Myocardial Infarction Angina Frequency and Risk of 1-Year Unplanned Rehospitalization. Circulation, 135(6), 532–543. doi: 10.1161/CIRCULATIONAHA.116.024406 [DOI] [PubMed] [Google Scholar]
- Izadnegahdar M, Singer J, Lee MK, Gao M, Thompson CR, Kopec J, & Humphries KH (2014). Do younger women fare worse? Sex differences in acute myocardial infarction hospitalization and early mortality rates over ten years. J Womens Health (Larchmt), 23(1), 10–17. doi: 10.1089/jwh.2013.4507 [DOI] [PubMed] [Google Scholar]
- Jencks SF (2010). Defragmenting care. Ann Intern Med, 153(11), 757–758. doi: 10.7326/0003-4819-153-11-201012070-00010 [DOI] [PubMed] [Google Scholar]
- Khera R, Jain S, Pandey A, Agusala V, Kumbhani DJ, Das SR, … Girotra S (2017). Comparison of Readmission Rates After Acute Myocardial Infarction in 3 Patient Age Groups (18 to 44, 45 to 64, and >/=65 Years) in the United States. Am J Cardiol. doi: 10.1016/j.amjcard.2017.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocher RP, & Adashi EY (2011). Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA, 306(16), 1794–1795. doi: 10.1001/jama.2011.1561 [DOI] [PubMed] [Google Scholar]
- Lauffenburger JC, Robinson JG, Oramasionwu C, & Fang G (2014). Racial/Ethnic and gender gaps in the use of and adherence to evidence-based preventive therapies among elderly Medicare Part D beneficiaries after acute myocardial infarction. Circulation, 129(7), 754–763. doi: 10.1161/CIRCULATIONAHA.113.002658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus DD, Nguyen HL, Saczynski JS, Tisminetzky M, Bourell P, & Goldberg RJ (2012). Multiple cardiovascular comorbidities and acute myocardial infarction: temporal trends (1990–2007) and impact on death rates at 30 days and 1 year. Clin Epidemiol, 4, 115–123. doi: 10.2147/CLEP.S30883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, … Outcomes R (2016). Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation, 133(9), 916–947. doi: 10.1161/CIR.0000000000000351 [DOI] [PubMed] [Google Scholar]
- Nguyen HL, Saczynski JS, Gore JM, & Goldberg RJ (2010). Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes, 3(1), 82–92. doi: 10.1161/CIRCOUTCOMES.109.884361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Numasawa Y, Kohsaka S, Miyata H, Noma S, Suzuki M, Ishikawa S, … Fukuda K (2015). Gender differences in in-hospital clinical outcomes after percutaneous coronary interventions: an insight from a Japanese multicenter registry. PLoS One, 10(1), e0116496. doi: 10.1371/journal.pone.0116496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuti SV, Qin L, Rumsfeld JS, Ross JS, Masoudi FA, Normand SL, … Krumholz HM (2016). Association of Admission to Veterans Affairs Hospitals vs Non-Veterans Affairs Hospitals With Mortality and Readmission Rates Among Older Men Hospitalized With Acute Myocardial Infarction, Heart Failure, or Pneumonia. JAMA, 315(6), 582–592. doi: 10.1001/jama.2016.0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien C, Valsdottir L, Wasfy JH, Strom JB, Secemsky EA, Wang Y, & Yeh RW (2017). Comparison of 30-Day Readmission Rates After Hospitalization for Acute Myocardial Infarction in Men Versus Women. Am J Cardiol. doi: 10.1016/j.amjcard.2017.06.046 [DOI] [PubMed] [Google Scholar]
- Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, & Krumholz HM (2014). Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med, 11(9), e1001737. doi: 10.1371/journal.pmed.1001737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah AS, Griffiths M, Lee KK, McAllister DA, Hunter AL, Ferry AV, … Mills NL (2015). High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ, 350, g7873. doi: 10.1136/bmj.g7873 [DOI] [PMC free article] [PubMed] [Google Scholar]