Abstract
SUMMARY
Objective:
Approximately 50% of patients with severe symptomatic MR are deemed too high risk for surgery. The MitraClip procedure is a viable option for this population. Our goal was to assess outcomes and survival of patients who underwent the MitraClip procedure at an institution where mitral valve surgery is routinely performed.
Methods:
A retrospective study of patients undergoing the MitraClip procedure was performed. Baseline characteristics, perioperative outcomes and follow-up echocardiographic and clinical outcomes were examined. Primary endpoint was survival. Secondary endpoints included technical failure (residual 3/4+ MR), reoperation, NYHA symptoms, 30 day mortality, and other clinical outcomes. Predictors of mortality were determined using multivariable regression analysis.
Results:
Fifty consecutive patients underwent the MitraClip procedure during the four year period. The average age was 83, mean STS PROM was 9.4%, 88% (44/50) had NYHA III/IV symptoms, 86% (43/50) had 4+ MR, and 72% (36/50) had degenerative mitral disease etiology. Echocardiographic data (median follow-up 43[IQR: 26,392]) showed that 86% (43/50) of patients had ≤ 2+ mitral regurgitation. 60% (24/40) had NYHA I/II symptoms at last followup. Predictors of mortality were higher STS PROM (p=0.042, HR 1.098) and previous cardiac surgery (p=0.013, HR 3.848). Survival at 1 and2years was 75% and 63%, respectively.
Conclusions:
Many patients with mitral valve regurgitation who are high risk for open surgery can be treated with the MitraClip procedure. In our study, the majority (86%) of patients had a technically successful operation and postoperative outcomes including survival were acceptable.
Keywords: Mitral valve, MitraClip, Mitral regurgitation
BACKGROUND
There are currently few treatment options for patients with symptomatic mitral regurgitation (MR) who are at high risk for conventional mitral valve repair or who are deemed inoperable due to severe comorbidities. The MitraClip procedure, a newer promising technology which has been shown to reduce MR, can be performed on patients whose symptoms are not improved with optimal medical management. This transcatheter edge-to-edge mitral valve repair has emerged as a safe and effective alternative therapy to open heart surgery (1,2). To date, over 45,000 patients deemed to have prohibitive surgical risk have undergone mitral valve repair using this approach (3). However, the vast majority have been done on patients who are low or moderate risk for conventional surgery.
For individuals with moderate to severe MR, American Heart Association/American College of Cardiology (AHA/ACC) guidelines endorse mitral valve repair or replacement. However, only 60% of these patients present as candidates for surgery (4). The MitraClip procedure has shown to be an effective approach with less perioperative morbidity and mortality than conventional surgery. There are reported improvements in New York Heart Association (NYHA) class as well as MR grade following the procedure (5,6). According to the AHA/ACC guidelines, MitraClip is recommended for patients with degenerative mitral regurgitation who are too high risk for surgery, while the European Society of Cardiology guidelines endorse MitraClip placement in patients with functional mitral regurgitation (1).
Our goal was to assess outcomes of patients deemed high risk for surgery with either functional or degenerative MR who underwent MitraClip placement at a single institution where surgical mitral valve replacement is the preferred treatment.
METHODS
A retrospective review of all patients undergoing the MitraClip procedure was conducted between 2014 and 2017 using medical records and established databases. No patients were excluded from the study. Patients were initially seen in clinic by a cardiac surgeon or cardiologist. Those who were deemed high risk for surgery were then presented at a multidisciplinary meeting with multiple cardiologists and surgeons present. Patients who were low or moderate risk for surgery had conventional mitral valve surgery. Those patients deemed high risk due to high STS scores, frailty, or anatomical considerations (e.g. MAC) were considered for MitraClip. The primary endpoint was intermediate-term survival. Secondary endpoints included technical failure (3/4+ mitral regurgitation) following the procedure, 30 day mortality, reoperation for MitraClip failure, postoperative NYHA class, postoperative atrial fibrillation (POAF), sepsis, stroke, acute kidney injury, and readmission to the hospital within 30 days. Echocardiograms were performed postoperatively as standard patient follow up and in patients who were involved in studies as part of the routine protocols.
Continuous data are reported as mean ± SD, or median [Interquartile range] as appropriate. Survival estimates were generated using the Kaplan-Meier method. Survival data were obtained for all patients through interrogation of institutional medical records, databases, and obituaries. Operative mortality was defined as death that occurred during the index hospitalization or within 30 days of the operation. Survival data included death from all causes. Univariate and multivariate analyses were used to determine preoperative and intraoperative risk factors that were predictors of mortality and are expressed as hazard ratios (HR). Statistics were done with SPSS Version 23.0 (IBM Corp, Armonk, NY, USA). A P-value of ≤0.05 was considered statistically significant. The study was approved by Washington University IRB committee.
RESULTS:
Fifty consecutive patients underwent the MitraClip procedure during the four year period. The average age was 83±7. Average STS predicted risk of mortality was 9.4±4%. Forty-four (88%) had NYHA III/IV heart failure symptoms. Severe (4+) MR was present in 86% (43/50), and 72% (36/50) had degenerative mitral regurgitation (Table 1).
Table 1:
Baseline characteristics
| Variable | |
|---|---|
| Male gender No, % | 27 (54) |
| Age, Mean | 83.2 ±7.1 |
| BMI, mean | 28.1±6.7 |
| Diabetes No, % | 15 (30) |
| Chronic Kidney Disease No, % | 22 (44) |
| Hypertension No, % | 47 (94) |
| Chronic Lung Disease No, % | 14 (34) |
| Peripheral Vascular Disease No, % | 5 (10) |
| Prior Stroke No, % | 11 (22) |
| NYHA 3 or 4 No, % | 44 (88) |
| Urgent operation No, % | 5 (10) |
| Prior Myocardial Infarction No, % | 8 (16) |
| Arrhythmia No, % | 35 (70) |
| Ischemic Mitral Valve etiology No, % | 14 (28) |
| Preop LVED volume, mL | 141 ±47 |
| Ejection Fraction, % | 59.0 ±14 |
| STS PROM | 9.4±4 |
| STS Predicted Morbidity and Mortality | 37.2±13 |
BMI: Body mass index, NYHA: New York Heart Association, LVED: Left ventricular end diastolic, STS: Society of Thoracic Surgeons
Thirty day mortality was 4% (2/50). One patient was discharged and returned with severe heart failure symptoms and PEA arrest and one patient died from cardiogenic shock. One patient suffered an ischemic stroke, but recovered strength on the same day. Three patients (6%) had to have surgery for mitral valve replacement following clip placement. In one patient the clip had a deployment malfunction and was operated on immediately. One patient developed severe mitral regurgitation after 8 months, and one patient developed severe mitral stenosis leading to mitral valve replacement 3 months following the MitraClip. Median length of stay was 3 [2,5] days. Sixteen percent (8/50) of patients were readmitted within thirty days.
Echocardiographic follow-up (mean 0.6±0.1 years) showed 86% (43/50) of patients had either 2+ or less mitral regurgitation at last follow up (Table 3, Figure 1 and 2). Sixty percent (24/40) had NYHA I/II symptoms at last followup (Figure 3). Survival at 1 and 2 years was 75%,and63%,, respectively (Figure 4). Left ventricular diastolic volume decreased from 141 mL preoperatively to 120mL following MitraClip placement (p=0.002). Predictors of mortality were higher STS PROM (p=0.042, HR 1.098) and previous cardiac surgery (p=0.013, HR 3.848).
Tables 3:
Perioperative echocardiograph and NYHA data
| Outcome | Preoperative, No (%) | Postoperative, No (%) |
|---|---|---|
| Mitral Regurgitation None Trace Mild Moderate Severe |
N/A N/A N/A 7 (14) 43 (86) |
5(10) 6(12) 23 (46) 9 (18) 7 (14) |
| Time to echo (yrs) | 0.6 ± 0.1 | |
| NYHA III or IV | 44 (88) | 16 (32) |
| LVED volume (mL) | 141 ± 47 | 120 ± 47 |
| Ejection Fraction | 59 ±14 | 54 ± 13 |
LVED: Left ventricular end diastolic, NYHA: New York Heart Association
Figure 1:
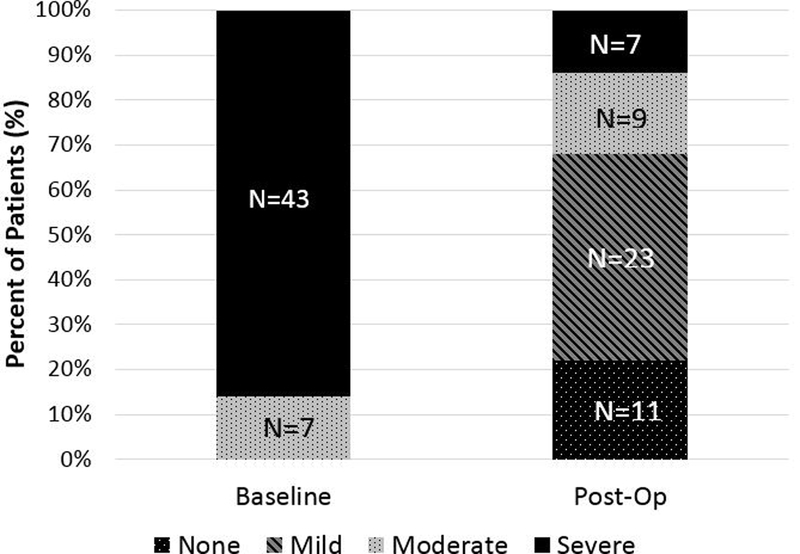
Perioperative mitral regurgitation grade in patients undergoing MitraClip placement.
Figure 2:
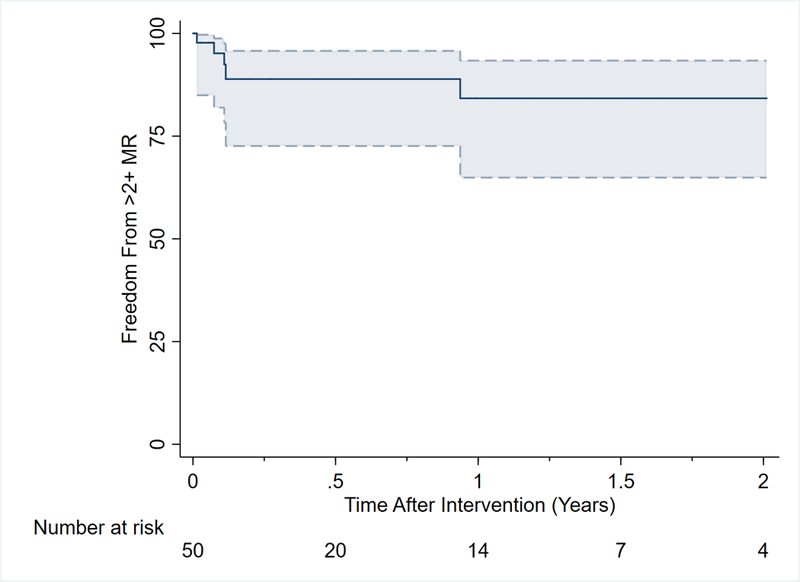
Kaplan Meier analysis showing freedom from 2+ mitral regurgitation postoperatively.
Figure 3:
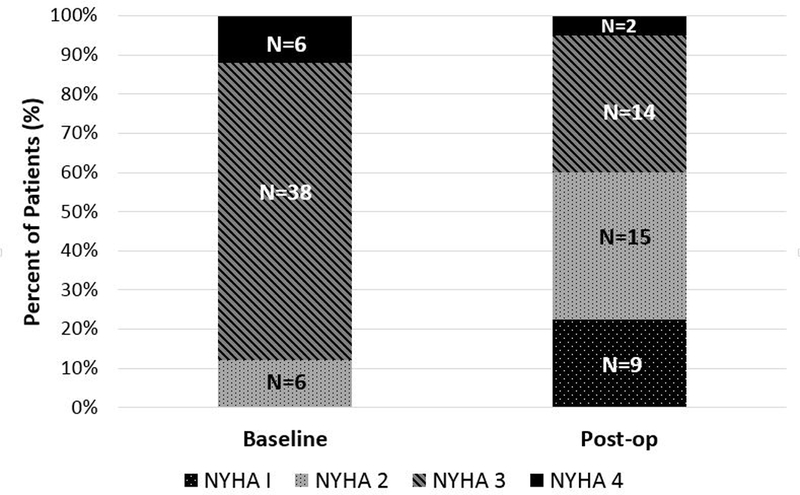
Perioperative NYHA functional status in patients undergoing MitraClip placement.
Figure 4:
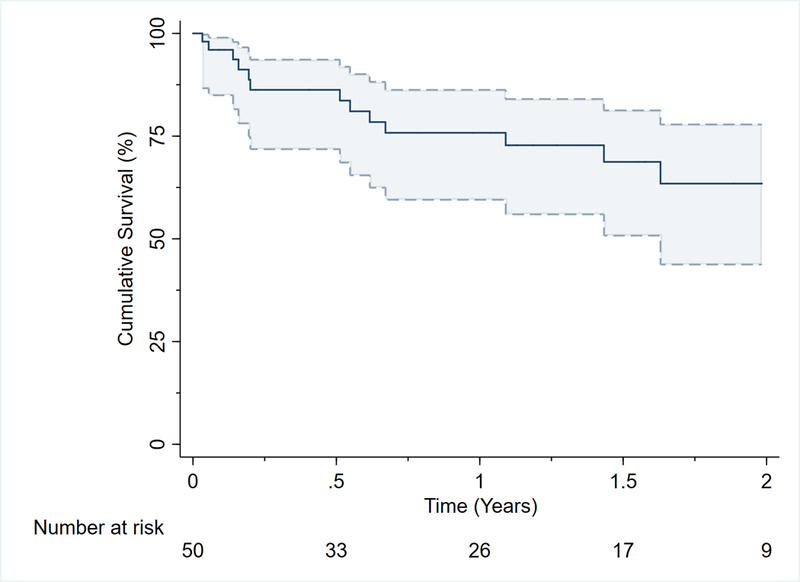
Kaplan Meier survival curve showing 2 year survival following MitraClip placement.
DISCUSSION:
MitraClip placement is feasible to offer patients that are deemed too high risk to undergo surgery. Survival was acceptable in our study, and the majority (86%) of patients had technically successful procedures performed as demonstrated by mitral regurgitation grade post-operatively.
Our institution performs mitral valve surgery whenever feasible and only patients deemed too high risk for surgery undergo MitraClip placement. During this same time period, 918 mitral valve surgeries were performed with standard cardiac surgery techniques. This is important as the majority of published studies on the MitraClip procedure are on lower risk populations who may not have necessarily been too high risk to undergo a surgical operation, and this cohort are much high risk for surgery, as those with low risk were offered standard surgery. Baseline preoperative characteristics were different in our cohort compared to other studies including the EVEREST II trial (7). The average age in this review was 83±7 years old compared to 67±13 in the EVEREST II Trial. Furthermore, average STS PROM was 9±4, and 88% (44/50) patients had NYHA III or IV heart failure symptoms prior to the procedure. In the EVEREST trial, only 50% (89/178) of patients had NYHA III or IV symptoms prior to MitraClip placement (7). Despite these high risks, perioperative complications remained acceptable.
The majority of patients experienced an improvement in NYHA functional status following placement of the MitraClip. At baseline, 88% (44/50) of patient’s had NYHA class III or IV heart failure symptoms. After clip placement the majority had class I and II NYHA symptoms (24/40). Echocardiographic followup showed that at 0.6±0.1 years following clip placement, the majority (86%) of patients had ≤2+ MR indicating a technically successful procedure. This is similar to the lower risk cohort in the EVEREST trial which found that 82% of patients had ≤2+ MR at one year (7). Significant improvement in left ventricular dimensions were noted after MitraClip placement as demonstrated by a decrease in left ventricular diastolic volume from 141 mL to 120 mL post operatively (p=0.002). Studies have shown that the majority of patients undergoing MitraClip placement showed reverse remodeling as demonstrated by a reduction in LVEDV. This is important as this data reflects the unloading effect of mitral valve repair (8).
Three patients required surgery after their initial procedure. There was a clip deployment malfunction in one patient which resulted in an emergency mitral valve replacement and then a subsequent redo mitral valve replacement 3 months later. The company has since made modifications to the steps in releasing the clip, and no further issues have been encountered with release of the clip. The second patient developed severe mitral stenosis and subsequently underwent mitral valve replacement 3 months after clip placement, and the third patient developed severe MR and underwent mitral valve replacement 6 months following placement of the MitraClip. A fourth patient underwent clip placement, had initial improvement of MR from 4+ to 2+, and subsequently developed severe MR leading to a second MitraClip placement 8 months later.
Survival was similar to previously published studies (5). Overall we found that at 1 and 2 survival was 75% and 63%, respectively (Figure 3). This was considerably worse survival than the EVEREST II trial, which was presumably the result of a higher risk cohort (7). Notably, 30 day mortality was 4 %( 2/50) which is in line with isolated mitral valve surgery. O’Brien et al. showed that 30 day mortality in this population was 5.7% in over 21,000 patients (9). Twenty-eight percent of our cohort had functional mitral regurgitation, but this cohort becomes increasingly important to consider for MitraClip procedure, specifically when considering the favorable outcomes reported from the COAPT trial where they showed that death or rehospitalization for heart failure at 2 years was 45.7% in patients who underwent the MitraClip procedure vs 67.9% in the medical therapy arm (10).
Limitations of this study include that it was retrospective in nature and thus subject to the threats inherent to this design. The sample size of our study was limited and likely affected by surgeon bias as only two surgeons routinely performed the procedure. Follow up is relatively short compared to surgical series, however in this high risk cohort prolonged survival would be surprising given the multitude of comorbidities in each patient. Additionally, while it would be interesting to compare MitraClip patients to a medically managed or surgical cohort, we did not have this data available to us.
In conclusion, the majority of patients in our study underwent a technically successful MitraClip procedure and benefited from improved NYHA functional status. Postoperative complications and intermediate-term survival were acceptable; therefore, in patients deemed too high risk for surgery the MitraClip remains a feasible option.
Table 2:
Postoperative outcomes following MitraClip placement
| Outcome | No (%) |
|---|---|
| Postoperative Atrial Fibrillation | 3 (6) |
| Sepsis | 5 (10) |
| Stroke | 1(2) |
| Deep wound infection | 0 (0) |
| Acute Kidney Injury | 4 (8) |
| Length of Stay | 3 [2,5] |
| Reoperation for valve | 3 (6) |
| 30 Day Mortality | 2 (4) |
| 30 Day Readmission | 8 (20) |
Acknowledgments
Conflict of Interest and Source of Funding: Ralph J. Damiano- Atricure: Speaker and receives research funding, LivaNova: Speaker. Medtronic: Consultant, Edwards: Speaker. Funding from: 1) T32-HL007776, and 2) Barnes Jewish Hospital Foundation
Poster presentation at the Annual Scientific Meeting of the International Society for Minimally Invasive Cardiothoracic Surgery, June 13–16, 2018, Vancouver, BC Canada
REFERENCES
- 1.Chiarito M, Pagnesi M, Martine EA, et al. Outcome after percutaneous edge-to-edge mitral repair for functional and degenerative mitral regurgitation: a systematic review and meta-analysis. Heart. 2017; 0:1–7 [DOI] [PubMed] [Google Scholar]
- 2.Mendirichaga R, Singh V, Blumer V, et al. Transcatheter Mitral Valve Repair With MItraClip for Symptomatic Functional Mitral Valve Regurgitation. Am J Cardiol. 2017;120:708–15. [DOI] [PubMed] [Google Scholar]
- 3.Orban M, Hausleiter J,. Edge-to-edge mitral valve repair: solid data and a prosperous future. Heart. 2018;104:280–281 [DOI] [PubMed] [Google Scholar]
- 4.Wu A, Aaronson K, Bolling S, et al. Impact of mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. J Am Coll Cardiol. 2005;45:381–387 [DOI] [PubMed] [Google Scholar]
- 5.Volker R, Malgorzata K, Franzen O, Schluter M, et al. Echocardiographic and Clinical Outcomes of MItraClip Therapy in Patients Not Amenable to Surgery. Journal of the American College of Cardiology. 2011; 58:2190–95 [DOI] [PubMed] [Google Scholar]
- 6.Ailawadi G, Lim S, Kron I, et al. Mitraclip for Functional Mitral Regurgitation: Outcomes in Over 600 Patients. Circulation. 2018; 132:A13513 [Google Scholar]
- 7.Feldman T, Foster E, Glower DG, et al. Percutaneous repair of surgery for mitral regurgitation. N Engl J Med 2011; 364:1395–406 [DOI] [PubMed] [Google Scholar]
- 8.Brouwer HJ, Heijer MC, Paelinck BP, et al. Left ventricular remodelling patterns after MitraClip implantation in patients with severe mitral valve regurgitation: mechanistic insights and prognostic implications. European heart journal. 2018; 00:1–7 [DOI] [PubMed] [Google Scholar]
- 9.O’Brien SM, Shahian DM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2—isolated valve surgery. Ann Thorac Surg 2009;88 Suppl:S23–42 [DOI] [PubMed] [Google Scholar]
- 10.Stone G, Abraham W, Lindenfeld J, et al. Cardiovascular outcomes assessment of MitraClip Therapy in Heart Failure Patients with Functional Mitral Regurgitation (The COAPT Trial): Baseline Characteristics and Preliminary 30-day and 1-year outcomes of the Roll-in Cohort. JACC 2016;68: B255–256 [Google Scholar]


