Abstract
Background:
Balloon expulsion test (BET) and high resolution anorectal manometry (HRM) are used in diagnosis of rectal evacuation disorders (RED); their performance characteristics are suboptimal.
Methods:
We audited records of 449 consecutive patients with chronic constipation (CC). We documented: anal sphincter tone and contraction, puborectalis tenderness, and perineal descent on digital rectal exam (DRE); maximum resting and squeeze pressures, and rectoanal pressure gradient on HRM; weight or time to balloon expulsion; colonic transit, and area of rectal area on radiograph (RASF). We based the diagnosis of RED on ≥2 abnormalities on both DRE and HRM, excluding results of BET, since the performance of BET is being investigated. Results of RED vs. non-RED, and results obtained using tbBET vs. wbBET groups were compared. We used multivariate logistic regressions to identify predictors of RED using different diagnostic modalities.
Key Results:
Among 449 individuals, 276 were included (74 RED and 202 non-RED). Predominant exclusions were for no HRM (n=79) or use of low resolution anorectal manometry (n=77). Logistic regression models for abnormal tbBET showed time >60 seconds, RASF and age predicted RED. For tbBET, the current cut-off of 60 seconds had sensitivity of 39.0% and specificity 93.0% to diagnose RED; on the other hand, applying the cut-off at 22 seconds, the sensitivity was 77.8% and specificity 69.8%.
Conclusions/Inferences:
The clinical diagnosis of RED in patients with CC is achieved with combination of DRE, HRM and an optimized, time-based BET. Prospective studies are necessary to confirm the proposed 22 second cut-off for tbBET.
Keywords: constipation, pelvic floor, dyssynergia, examination
Graphical Abstract
Abbreviated abstract: Balloon expulsion test (BET) and high resolution anorectal manometry (HRM) are used in diagnosis of rectal evacuation disorders (RED); their performance characteristics are suboptimal. The clinical diagnosis of RED in patients with CC is achieved with combination of DRE, HRM and an optimized, time-based BET. Prospective studies are necessary to confirm the proposed 22 second cut-off for tbBET.
Introduction
Three categories of primary chronic constipation are not associated with an underlying disorder: rectal evacuation disorders (RED), slow transit constipation, and normal transit constipation. Differentiation is based on examination, colonic transit, and anorectal function assessment.1 RED is primarily characterized by impaired rectal evacuation in the absence of structural obstruction, with normal or delayed colonic transit. In Olmsted County, MN, the age- and sex-adjusted incidence rate of clinically diagnosed RED was 19.3 per 100,000 person-years.2 Constipation in patients with RED may not respond to laxatives, and biofeedback therapy is usually necessary.3,4
There is no current “gold standard” to confirm the diagnosis of RED.3 Given considerable disagreement between the results of various tests used to diagnose evacuation disorders, Palit et al. recommended incorporating symptoms, findings on a digital rectal examination, and two diagnostic tests to define the condition.5 However, symptoms have insufficient ability to distinguish functional constipation from rectal evacuation disorders. Thus, four of the six Rome IV criteria for functional constipation are highly suggestive of rectal evacuation disorders, especially when they occur in >25% of defecations: straining, sensation of incomplete evacuation, sensation of anorectal obstruction/blockage and manual maneuvers to facilitate defecation.6
Digital rectal exams (DRE) are operator dependent and, when performed correctly, have a high sensitivity and positive predictive value in detecting RED compared to high resolution anorectal manometry (HRM).7 Rome III8 and Rome IV3 criteria for defecatory disorders do not include DRE, despite the evidence from multiple reports.7,9,10
HRM has been utilized as an indirect measure and the balloon expulsion test (BET) as a direct measure for RED. Diverse parameters measured on HRM show a wide range of specificity and sensitivity for diagnosing RED; HRM was considered to be of limited diagnostic utility in distinguishing patients with functional constipation and healthy controls.11 Timed BET (using the 60 second cut-off as abnormal) has a specificity of 90% in diagnosing RED,12 but the sensitivity is 27%.13
Until January 2015, our center performed weight-based BET (wbBET); after that date, we transitioned to a time-based BET (tbBET). It is considered that the wbBET overcomes passive resistance to expulsion provided by the pelvic floor and anal sphincters, whereas the tbBET, in seated position, may test active expulsive forces. A comparison between the wbBET and the tbBET within the same participant showed modest inter-rater agreement [κ=0.44 (95% CI 0.30–0.57)] between the wbBET and the tbBET among participants with normal (n=141) or abnormal (n=32) rectal balloon expulsion in 62 healthy and 158 women with chronic constipation, and there was only modest correlation in the results between the balloon expulsion times (in seated position) and weights (in left lateral position) expressed as continuous variables (r = 0.46, p < 0.0001).14 Given all the above considerations, we used a combination of DRE and HRM criteria to categorize RED in this study.
The primary aim of the current study was to compare the wbBET or the tbBET in diagnosing RED in patients evaluated for chronic constipation by a single gastroenterologist. Secondary aims were comparison between DRE findings and anorectal manometry parameters, and identification of predictors of a diagnosis of RED, including rectal area of gas on scout abdominal film (RASF),15 colonic transit, and the tbBET or the wbBET. The ultimate objective of this audit was to generate the preliminary data in support of the hypothesis that, in patients with chronic constipation, the diagnosis of RED can be optimized for sensitivity and specificity with combination of DRE, HRM and an optimized timed-based BET. Future research could then test this hypothesis and, particularly, to identify the time cut-off on tbBET that provides optimal specificity and sensitivity for diagnosing RED.
Methods
Study Population and Data Extraction
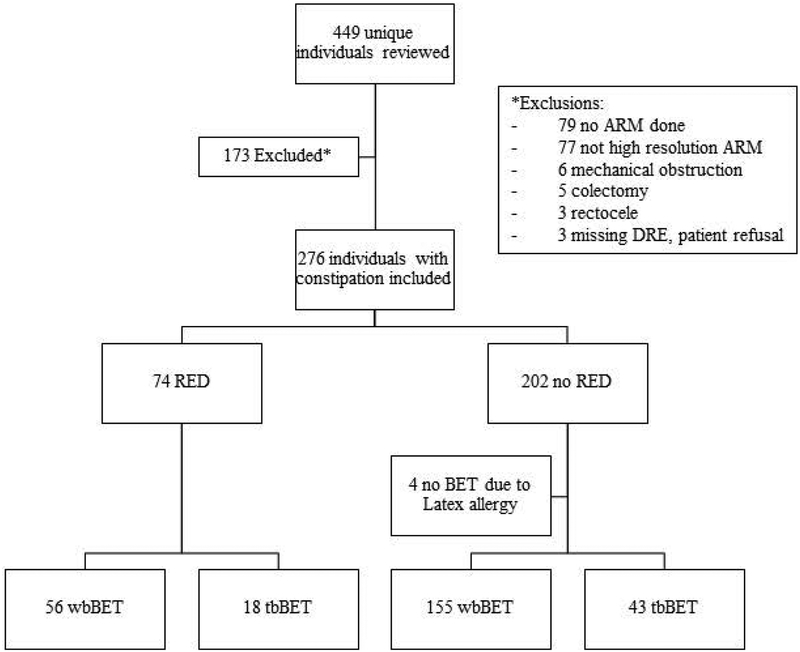
We reviewed the Mayo Clinic Rochester electronic medical records of adult patients who had previously given their consent for use of medical records for research. Mayo Clinic Institutional Review Board approved the study (IRB #17–008852). Patients were evaluated for chronic constipation by a single gastroenterologist (M.C.) between January 1, 2007 and January 30, 2018. Exclusion criteria are summarized in the Results section and Figure 1.
Figure 1.
CONSORT flow chart of our cohort referred to a single gastroenterologist. ARM, anorectal manometry; DRE, digital rectal exam; RED, rectal evacuation disorders; BET, balloon expulsion tests; wbBET, weight-based balloon expulsion test; tbBET, time-based balloon expulsion test
We extracted the following information: basic demographics [body mass index (BMI), age, and sex], detailed DRE, HRM, time or weight added to balloon expulsion, colonic transit, current narcotic use, obstetric history, prior abdominal surgeries, and hysterectomies.
Criteria Used for Diagnosis of Rectal Evacuation Disorders in Evaluation of Outcomes in Anorectal Testing
Given the lack of a gold standard diagnostic test, the lack of validation of proportion emptied by defecography and our objective to characterize the tbBET in order to optimize its performance, we identified the cases of RED from our cohort of patients with chronic constipation based on Rome III diagnostic criteria for functional constipation,16 with symptom criteria met in the last 3 months and symptom onset at least 6 months before diagnosis: 1) symptoms suggestive of functional constipation, 2) features of impaired evacuation on anorectal manometry. In addition to these criteria, we included the findings on digital rectal exam (DRE). Thus, individuals were diagnosed with RED if they had two abnormal DRE findings and two abnormal HRM measures. Abnormal high resolution anorectal manometry (HRM) measures were: (1) high resting anal sphincter pressure (maximum resting pressure >104mmHg, based on upper limit of data from patients with normal balloon expulsion);13 (2) high anal squeeze pressure (maximum squeeze pressure >260mmHg;16 and (3) rectoanal pressure gradient more negative than −50mmHg based on controls and patients with normal balloon expulsion.16
Digital Rectal Exam
The DRE was performed by a single gastroenterologist (M.C.) and documented in a standardized way in the medical records: resting anal tone, squeeze pressure (both designated as increased, decreased or normal), sphincter relaxation (impaired relaxation, paradoxical contraction, normal), puborectalis tenderness (present or absent) and perineal descent (<2cm absent, 2–4 cm normal, >4 cm excessive) estimated by visual inspection by the single observer.
High Resolution Anorectal Manometry
Details of the HRM procedure16–18 included: performance by a trained nurse one hour after a sodium phosphate enema (Fleet®, Lynchburg, VA, USA), left lateral position, use of a transanal solid-state, high resolution probe (4.2mm outer diameter; Sierra Scientific Instruments, Los Angeles, CA, USA) with closely spaced solid-state sensors (16 channels at each level) and measurements in mmHg. HRM parameters were computed in a standardized protocol utilizing ManoView AR v.3.0 (Sierra Scientific Instruments, Los Angeles, CA, USA). This high resolution, solid-state manometry has been previously validated in comparison to water-perfused manometry.19 We extracted from the reports the maximum resting pressure, squeeze anal pressure, and the rectoanal pressure gradient.
Balloon Expulsion Test
Between 2007 and 2014 at our center, we used the wbBET.14 After anorectal manometry was completed and with the patient in the left lateral position, a latex balloon was inserted into the rectum and filled with 50mL water at room temperature. If the patient was unable to spontaneously expel the balloon, weights were added to a basket tied to the balloon catheter and suspended over a pulley; sequentially, weights were added in increments of 47g up to a maximum of 564g.
From 2015, the tbBET was adopted. After the anorectal manometry study was completed, the patient attempted to expel the inserted latex balloon while sitting in private on a bedside commode, and the time to expulsion was recorded or censored at >60 seconds, if expulsion was not achieved. For further hypothesis generation, we conducted regression analyses dividing groups based on the time to expulsion: <15 sec, 15–60 sec, or >60 sec.
Unfortunately, the performance characteristics of balloon expulsion time, and different parameters observed on HRM are suboptimal.10–12 Therefore, while most laboratories determine that time for balloon expulsion >60sec is diagnostic of RED (specificity >90%),12 the sensitivity using the current cut-off of 60 seconds is only 27% compared to MR defecography.13 In addition, while weight required for balloon expulsion >200g is deemed abnormal, this test is no longer performed, even at Mayo Clinic, which originally championed the test.20
Colonic Transit
Evaluation of colonic transit has been previously validated and published by our group and is described in detail elsewhere.17,21 In this analysis of patients with chronic constipation, we focused on colonic transit assessed by calculating the geometric center (GC) at 24 hours and 48 hours (GC24 and GC48). The GC is expressed as the sum of the weighted proportion of 111In counts in each of 5 colonic regions [ascending colon (AC), transverse colon (TC), descending colon (DC), rectosigmoid (RS), and stool] at a given time.
Participants were not taking any prescription or over the counter medications for the 48 hours prior to and during the testing of gastrointestinal and colonic transit. Colonic transit measurements were compared to laboratory normal values: median (5th, 95th%iles) GC 24h: 2.3 (1.3, 4.4) and GC48h: 3.8 (1.9, 5.0).22
Rectal Area of Gas on Abdominal Scout Film
The method for measuring the rectal area of gas on scout film (RASF) of an abdominal computed tomography (CT) scan has been previously published and validated relative to the estimated rectal gas volume measured by the same CT scan after 3-dimensional reconstruction.15,23 From our previous studies, we used mean RASF >9 cm2 (92.3% specificity and 68.8% positive predictive value) as the cut-off to diagnose RED.23
For estimating the RASF, we identified the most recent radiograph (within 1 year) from the date of evaluation in the GI clinic. We adopted a standardized approach to identify rectal gas, based on the bony landmarks (from the lower aspect of the sacroiliac joint to the lower aspect of the pubic symphysis) to define the margins of vertical extent of the rectal gas.15,23 The surface area of rectal gas was outlined by using a manually operated region of interest (ROI) approach. The software, Quick Query Radiographs and Photographs, Electronic Analysis and Display Station (QREADs version 5.9.3.2, Mayo Clinic, Rochester, MN, USA), automatically calculated the area of rectal gas on the 2-dimensional abdominal film (RASF) in cm2. RASF was measured by a single operator (V.C.) who was trained on how to identify and measure RASF,15,23 and who was blinded to the information on DRE and HRM at the time when the RASF was being estimated.
Statistical Analysis
Data were expressed as median values with the interquartile range [IQR: 25th-75th percentile] or mean values with standard error of the mean (SEM) where applicable.
Identification and Comparison of RED and Non-RED
Latent class analysis to identify RED on DRE and ARM tests
We used two abnormal findings on DRE and two abnormal findings on ARM to diagnose RED. This approach was necessitated by the absence of a generally accepted ‘gold standard’ for the diagnosis of RED in the literature. For example, in the Rome III criteria, the symptoms (e.g., 25% straining or sense of incomplete evacuation) are included in both criteria of functional constipation and dyssynergic defecation. The Rome III criteria recommend two abnormal findings on ARM and abnormal balloon expulsion test to diagnose RED, but we were unable to include the BET in our diagnosis of RED because we were testing the validity of these parameters. Given that ARM alone does not suffice for diagnosis of DRE, we supplemented these criteria with findings on DRE.
Using latent class analysis (LCA), our cohort was best fit into two clusters (RED and no RED) based on the individual DRE parameters. The LCA identified that the following parameters suggest rectal evacuation disorder: Reduced perineal descent (effect size [ES] 0.90; paradoxical contraction ES 0.65; presence of puborectalis tenderness ES 0.35; increased anal sphincter resting tone ES 0.19; and increased anal squeeze pressure 0.09). Any two or more abnormalities among these five parameters on DRE were accepted as complementary to the findings on ARM for the diagnosis of RED.
Comparison of RED to non-RED
Continuous variables in the groups with or without RED were compared using independent two-sample t-test or Wilcoxon Rank Sum test. Proportions were compared using Chi-square test of independence or Fisher’s exact test. Statistical significance was defined based on a two-sided α value of <0.05. Analysis of variance (ANOVA) on ranks was utilized to compare anorectal manometry parameters in three groups (low, normal, or high) based on the report documented on anal examination in the DRE results. If there was a significant difference based on ANOVA on ranks, we utilized Dunn’s method for all pairwise comparisons, corrected for multiple comparisons.
Comparison of wbBET and tbBET
The cohort was further subdivided into those who underwent the wbBET or the tbBET. Our primary endpoint was the diagnosis of RED. In each subgroup (wbBET and tbBET), a univariate analysis was conducted with a priori selected set of seven predictor variables: sex, age, BMI, GC24, GC48, RASF (cm2), and balloon weight or balloon time for expulsion. Variables that were statistically significant were then entered in a multivariate model to determine predictors of RED. Sensitivity and specificity of tbBET were calculated. These parameters are not presented for wbBET, since it is no longer being used as a diagnostic test.
Statistical analysis was conducted using (JMP® PRO Version 13.0.0, Cary, NC, USA). The same statistical software was utilized to create receiver operating curves (ROC) to determine the association of the predictor variables with a diagnosis of RED.
Results
Demographics and Characteristics of Participants
Figure 1 describes the flow chart of all individuals included in our study: 449 records of consecutive, unique individuals referred to Mayo Clinic were reviewed; 276 were included (74 RED and 202 non-RED). We excluded records that did not include HRM (n=79) or DRE (patient refusal, n=3), or when anorectal manometry was not high resolution (n=77). Four individuals did not have a balloon expulsion test due to latex allergy. Table 1 shows demographics and results of colonic transit, balloon expulsion test, and rectal area on scout film (RASF) in patients evaluated for constipation with RED and no RED. The colonic transit profile at 24 and 48 hours in the RED and non-RED groups are shown in Table 1. Among patients with RED, 4/61 had slow colonic transit at 24h (GC24 <1.3) and 6/42 at 48h (GC48 <1.9); among patients without RED, 11/163 had slow colonic transit at 24h and 5/119 at 48h. At 48h, there was a significantly higher proportion of patients with RED with slow colonic transit compared to patients without RED (p=0.03).
Table 1.
Demographics and results of colonic transit, balloon expulsion test, and rectal area on scout film (RASF) in patients evaluated for constipation with rectal evacuation disorder (RED) and no RED.
| Characteristics | RED (n=74) | No RED (n=202) | P value |
|---|---|---|---|
| Age, years | 30.5 [25; 42.3] | 45 [28; 56.3] | |
| Sex (female) | 50 (67.5) | 172 (85.2) | |
| Body mass index (kg/m2) | 21.8 [18.9; 25.0] | 22.2 [19.3; 25.4] | |
| Current narcotic use | 7 (9.5) | 33 (16.3) | |
| Prior hysterectomy | 3 (7.9) | 24 (18.3) | |
| Prior delivery | 7 (14.6) | 74 (48.1) | |
| Number of births | |||
| • None | 41 (82.0) | 80 (47.9) | |
| • One | 1 (2.0) | 24 (14.4) | |
| • Two | 6 (12) | 40 (23.9) | |
| • Three or more | 2 (4) | 23 (13.8) | |
| Digital Rectal Examination | |||
| Absent perineal descent | 62 (88.6) | 96 (51.1) | <0.001 |
| Puborectalis tenderness | 40 (54.0) | 58 (28.7) | <0.001 |
| Increased resting anal tone | 41 (56.2) | 42 (21.6) | <0.001 |
| Increased anal squeeze | 15 (22.1) | 2 (1.1) | <0.001 |
| Paradoxical contraction | 41 (68.3) | 83 (45.1) | <0.001 |
| Impaired anal relaxation | 7 (11.7) | 6 (3.3) | <0.001 |
| Colonic transit | |||
| Geometric center 24 hours | 1.8 [1.5; 2.4], n=61 | 1.9 [1.6; 2.3], n=163 | 0.47 |
| Slow colonic transit at 24h (<1.3) | 4/61 | 11/163 | 0.9 |
| Geometric center 48 hours | 2.7 [2.0; 3.7], n=42 | 2.7 [2.2; 3.9], n=119 | 0.84 |
| Slow colonic transit at 48h (<1.9) | 6/42 | 5/119 | 0.03 |
| Balloon expulsion test | |||
| Balloon weight (g) n=211 | 564 [384; 564] | 0 [0; 564] | <0.001 |
| Balloon time (sec) n=61 | 31 [20; 60] | 13 [7; 23] | 0.003 |
| Rectal area | |||
| Rectal area on scout film (cm2) | 9.48 ± 1.99, n=38 | 6.09 ± 0.93, n=103 | 0.13 |
| RASF >9cm2 | 15/38 (39.5%) | 27/103 (26.2 %) | 0.15 |
Data presented as N (%); median [interquartile range]; or mean±SEM.
Normal colonic transit data based on measurements in 145 females and 75 males for geometric center (GC) 24, and 136 females and 63 males for GC 48:
Median (5th, 95th %) GC 24h: 2.3 (1.3, 4.4)
GC48h: 3.8 (1.9, 5.0)
Among patients who underwent wbBET, 14/175 had slow colonic transit at 24h (GC24 <1.3) and 10/113 at 48h (GC48 <1.9); among patients who underwent tbBET, 1/47 had slow colonic transit at 24h and at 48h. The proportions of slow colonic transit in the two groups of patients were not statistically different.
Identification of RED, and Comparisons of RED and Non-RED Groups
Table 1 shows the baseline demographics of our cohort comparing those with the diagnosis of RED to those with no RED. Individuals with RED were younger, with a median age of 30.5 years [IQR 25; 42.25] compared to 45 years [IQR 28; 56.3] in the non-RED group (p<0.001). A total of 141 patients (38 with RED and 103 with non-RED) had abdominal x-rays available to measure RASF. For the RED group, the mean RASF was 9.48±1.99 cm2 in comparison with 6.09±0.93 cm2 for the non-RED group (p=0.13).
Among the group who had the wbBET, those with RED had a median added weight of 564g [IQR 384; 564] compared to 0g [IQR 0; 564] in the non-RED group (p<0.001) (Table 1). Additionally, among those who underwent the tbBET, those with RED were able to expel the balloon in 31 seconds [IQR 20; 60, with the 60 seconds being a censored value] compared to 13 seconds [IQR 7; 23] in the non-RED group (p=0.003).
Table 2 describes the characteristics of the groups who underwent the wbBET or the tbBET, showing no differences in the two groups except for the rectoanal pressure gradient on anorectal manometry, which was significantly more negative in the wbBET group compared to the tbBET group [−26.2mmHg (IQR −44.1; −7.7) vs. −41.0mmHg (−71.3; −13.4); p=0.0016].
Table 2.
Demographics and results of digital rectal exam, high resolution anorectal manometry, colonic transit, balloon expulsion test, and rectal area on scout film (RASF) in patients evaluated for constipation based on patients who underwent weight- or time-based balloon expulsion tests (wbBET or tbBET).
| Characteristics | wbBET (n=211) | tbBET (n=61) | p value |
|---|---|---|---|
| Females, N (%) | 165 (78.2) | 53 (86.9) | 0.12 |
| Age (years) | 40 [27; 53] | 40 [27; 56] | 0.85 |
| Body mass index (kg/m2) | 21.7 [19.2; 24.8] | 22.7 [19.2; 26.8] | 0.27 |
| Rectal evacuation disorder, N (%) | 43 (21.7) | 18 (29.5) | 0.64 |
| Digital rectal exam findings | |||
| Absent perineal descent | 116 (59.5) | 38 (64.4) | 0.50 |
| Puborectalis tenderness | 73 (34.6) | 24 (39.3) | 0.50 |
| Increased resting anal tone | 63 (30.7) | 19 (32.2) | 0.94 |
| Decreased resting anal tone | 27 (13.2) | 8 (13.8) | |
| Increased anal squeeze | 12 (6.3) | 5 (9.6) | 0.64 |
| Decreased anal squeeze | 36 (18.9) | 11 (21.2) | |
| Paradoxical contraction | 96 (52.8) | 26 (44.1) | 0.50 |
| Impaired anal relaxation | 9 (4.9) | 3 (5.1) | |
| Colonic transit on scintigraphy^ | |||
| Geometric center 24 hours | 1.9 [1.6; 2.4] | 1.8 [1.6; 2.2] | 0.37 |
| Slow colonic transit at 24h | 14/175 | 1/47 | 0.10 |
| Geometric center 48 hours | 2.7 [2.1; 3.8] | 2.7 [2.1; 3.7] | 0.90 |
| Slow colonic transit at 48h | 10/113 | 1/47 | 0.10 |
| Anorectal manometry parameters | |||
| Max resting pressure (mmHg) | 95.2 [77.1;112.9] | 97.0 [82.4;114.8] | 0.52 |
| Max squeeze pressure (mmHg) | 161.7 [120.2;207.9] | 187.5 [134.6;227.4] | 0.13 |
| Recto-anal pressure gradient(mmHg) | −26.2 [−44.1;−7.7] | −41.0 [−71.3;−13.4] | 0.002 |
| Rectal area | |||
| RASF (cm2) | 2.1 [0; 10.0] | 3.3 [0; 10.0] | 0.28 |
Data presented as N (%); median [interquartile range].
Normal colonic transit data based on measurements in 145 females and 75 males for geometric center (GC) 24, and 136 females and 63 males for GC 48:
Median (5th, 95th %) GC 24h: 2.3 (1.3, 4.4)
GC48h: 3.8 (1.9, 5.0)
Comparison of DRE Findings to Anorectal Manometry Parameters
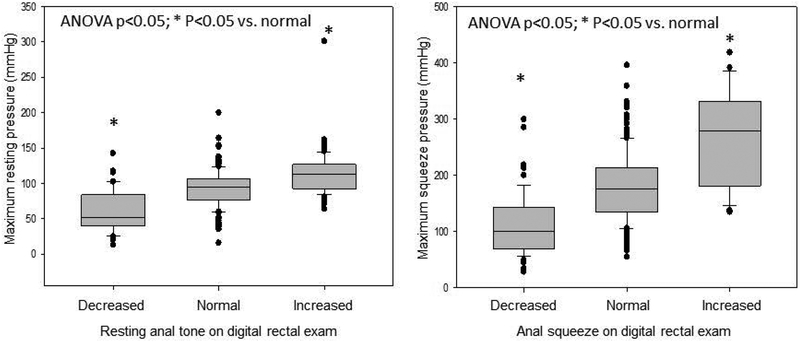
Figure 2 shows the DRE findings and anorectal manometry parameters. There was an overall difference in the maximum resting pressure on HRM according to the determination by the DRE (p<0.001 on ANOVA). Indeed, all pairwise comparisons showed significant differences in pressures between the 3 groups (corrected Dunn’s test p<0.05). Similarly, the overall differences in maximum squeeze pressures among the 3 groups based on DRE (ANOVA on ranks p<0.001) and all pairwise comparisons (corrected p<0.05). Table 3 further characterizes the relation between each finding on the digital rectal exam and the objective parameters on anorectal manometry, balloon weight, balloon expulsion test (BET) and rectal area on scout film (RASF).
Figure 2.
Comparing digital rectal exam findings to anorectal manometry (ARM) parameters: maximum resting and squeeze sphincter pressures. ANOVA comparing the means of three groups were statistically significant (p<0.05), Dunn’s method comparing each pair was also statistically significant (p<0.05).
Table 3.
Relationship between each finding on the digital rectal exam (DRE) and the objective parameters on anorectal manometry, balloon weight, balloon expulsion test (BET) and rectal area on scout film (RASF).
| Maximum resting pressure (mmHg) | p | Maximum squeeze pressure (mmHg) | p | Recto-anal pressure gradient (mmHg) | p | Balloon Weight (g) | p | Balloon Expulsion Time (sec) | p | RASF (cm2) | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resting Pressure* | <0.001 | <0.001 | 0.2 | 0.2 | 0.6 | |||||||
| Increased** | 112.9 [82.4;144.9] |
<0.001 | −38.3 [−90.5; −6.1] |
0.02 | 470 [0; 564] |
0.6 | 16.0 [4.0; 60.0] |
0.6 | 1.1 [0.0; 17.7] |
0.8 | ||
| Decreased** | 52.4 [23.9;107.4] |
<0.001 | −5.2 [−30.7; 8.5] |
0.008 | 0 [0; 564] |
0.3 | 12.0 [3.0; 29.0] |
0.4 | 5.1 [0.0; 17.7] |
0.7 | ||
| Squeeze* | <0.001 | 0.001 | 0.9 | 0.2 | 0.9 | |||||||
| Increased** | 279.2 [137.3;396.6] |
<0.001 | −70.7 [−173.8; 10.3] |
0.004 | 470break/>[0; 564] | 0.9 | 37.0 [14.0; 60.0] |
0.1 | 2.0 [0.0; 33.8] |
0.8 | ||
| Decreased** | 103.6 [75.0; 156.1] |
<0.001 | −14.1 [−58.1; 11.1] |
0.2 | 435 [0; 564] |
0.9 | 20.0 [2.0; 60.0] |
0.8 | 2.7 [0.0; 39.2] |
0.9 | ||
| Sphincter Relaxation* | 0.5 | 0.8 | 0.009 | <0.001 | 0.05 | 0.3 | ||||||
| Paradoxical Contraction** | 94.7 [56.7; 134.7] |
0.5 | 161.5 [91.9; 213.3] |
0.9 | −30.6 [−89.0; 0.2] |
0.01 | 547 [0; 564] |
<0.001 | 22.0 [5.4; 33.7] |
0.6 | 2.5 [0.0; 25.4] |
0.9 |
| Impaired Relaxation** | 95.0 [64.7; 118.8] |
0.9 | 159.8 [76.4; 310.3] |
0.7 | −47.0 [−97.8; 24.1] |
0.07 | 564 [0; 564] |
0.003 | 60.0 [20.0; 60.0] |
0.03 | 7.8 [8.6; 48.5] |
0.2 |
| Puborectalis Tenderness$ | 99.8 [70.9; 137.8] |
0.001 | 167.6 [95.9; 280.0] |
0.5 | −37.1 [−83.8; −1.8] |
0.002 | 547 [0; 564] |
<0.001 | 15.0 [4.0; 60.0] |
0.6 | 3.2 [0.0; 25.1] |
0.3 |
| Absent Perineal Descent$ | 94.8 [56.5; 135.6] |
0.1 | 164.8 [84.4; 285.5] |
0.6 | −34.6 [−83.6; 0.0] |
<0.001 | 547 [0; 564] |
<0.001 | 22.0 [5.9; 60.0] |
0.2 | 2.7 [0.0; 24.2] |
0.9 |
p value compares DRE findings using ANOVA followed by Dunnett’s test (**) for comparison with normal result; or 2-tailed t-test ($) for presence or absence of the other parameters
Univariate and Multivariate Analyses to Identify Factors Predicting Diagnosis of RED
Weight-based BET group
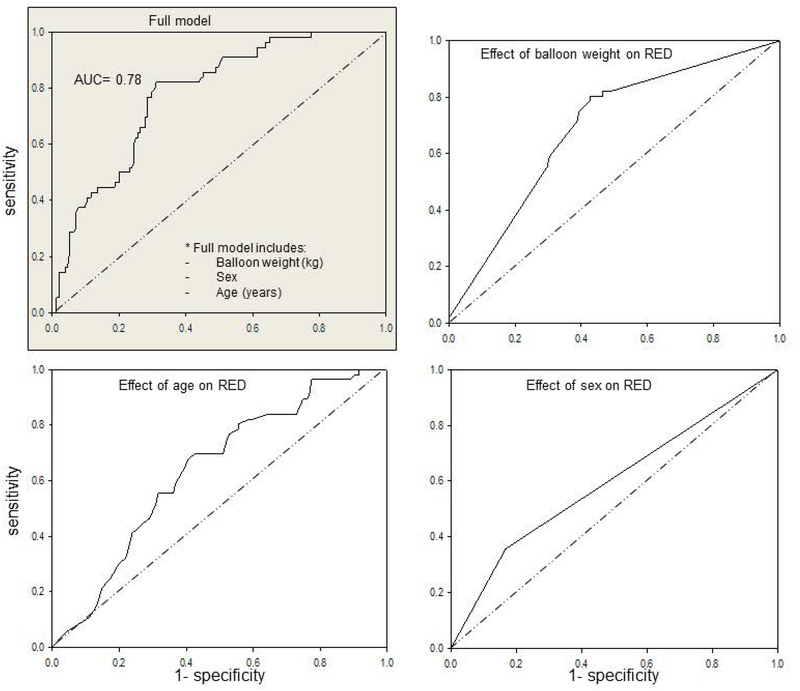
Univariate analysis was statistically significant for age, sex, and balloon weight (p<0.01) (Table 4) in the wbBET group. In the multivariate analysis, the odds ratio for age (per year), sex, and balloon weight (per g added) were significant in the model (p<0.001; for ORs, see Table 4). The ROC curve for the full model to predict RED had an AUC of 0.78 (Figure 3). The ROC curves for the independently significant factors (age, sex, weight added) are also shown in Figure 3. Thus, for every 50-gram increase in balloon weight required for expulsion, there was a 16% increase in the odds ratio of a patient with constipation to have RED when using the wbBET. For every 10-year increase in age, there was a 30% decrease in the odds ratio of RED.
Table 4.
Univariate, multivariate predictors of rectal evacuation disorder(RED) with wbBET
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Characteristic | N | OR (95% CI) | LR p value | OR (95% CI) | LR p value |
| Balloon weight (g) | 211 | 1.003 (1.001–1.004) | <0.001 | 1.003 (1.002–1.004) | <0.001 |
| Age | 211 | 0.97 (0.95–0.99) | <0.001 | 0.96 (0.94–0.99) | 0.001 |
| Sex | 211 | ||||
| Male | 46 | 1.0 | reference | 1.0 | reference |
| Female | 165 | 0.36 (0.18–0.72) | 0.004 | 0.27 (0.12–0.59) | <0.001 |
| BMI (kg/m2) | 209 | 1.02 (0.96–1.08) | 0.61 | AUC=0.78 | |
| GC24 | 180 | 1.09 (0.77–1.55) | 0.61 | ||
| GC48 | 115 | 0.91 (0.62–1.34) | 0.64 | ||
| RASF (cm2) | 101 | 0.99 (0.99–1.00) | 0.68 | ||
AUC = area under the curve; CI = confidence interval; GC= colonic geometric center; LR = likelihood ratio; OR= odds ratio; RASF= rectal area on scout film
Figure 3.
Receiver operating characteristic (ROC) curves for the wbBET group based on the full model (multivariate analysis) of predictors of rectal evacuation disorders (RED) shown in upper left panel; and univariate models for balloon weight, age, and sex and their effects on RED. Note that the full model is significant (p=0.001) and the major univariate contribution to the AUC is provided by the weight added to the balloon; however, age and gender are also univariately significant and contribute to the overall significance of the full model.
Time-based BET group
Table 5 shows the univariate analysis with the pre-specified variables in the tbBET group; age (p=0.002), rectal gas RASF (p=0.008), and time for expulsion >60seconds (p<0.001) were statistically significant (for ORs, see Table 5). However, only 18/61 patients had tbBET >60 seconds, suggesting relatively low sensitivity among 61 patients with RED.
Table 5.
Univariate predictors of rectal evacuation disorder (RED) with tbBET
| Univariate Analysis | |||
|---|---|---|---|
| Characteristic | N | OR (95% CI) | LR p value |
| Timed subgroups | 61 | ||
| ≤15 sec | 28 | 1.0 | Reference |
| 16–59 sec | 23 | 2.63 (0.66–10.45) | 0.16 |
| ≥60 sec | 10 | 14 (2.51–77.99) | 0.001 |
| Age | 61 | 0.94 (0.90–0.98) | 0.002 |
| Sex Male | 8 | 1.0 | Reference |
| Sex Female | 53 | 0.36 (0.08–1.63) | 0.19 |
| BMI (kg/m2) | 59 | 0.90 (0.80–1.02) | 0.07 |
| GC24 | 48 | 1.32 (0.63–2.78) | 0.46 |
| GC48 | 47 | 1.2 (0.62–2.29) | 0.60 |
| RASF (cm2) | 36 | 1.001 (1.0001–1.002) | 0.008 |
CI = confidence interval; GC= colonic geometric center; LR = likelihood ratio; OR= odds ratio; RASF= rectal area on scout film
Sensitivity and Specificity of Time-Based Balloon Expulsion Tests to Diagnose RED
In order to appraise the potential effect of different cut-offs with tbBET and provide preliminary data for future hypothesis-testing studies, we assessed different cut-offs for both methods, as shown in Table 6.
Table 6.
Diagnostic accuracy by time-based balloon expulsion test (tbBET) at different cut-off values
| tbBET cut-off | Sensitivity (95% CI) |
Specificity (95% CI) |
PPV (95% CI) |
NPV (95% CI) |
|---|---|---|---|---|
| 15 sec | 83% (58.6%−96.4%) |
51.6% (35.5%−66.7%) |
41.7% (33.1%−50.8%) |
88.0% (71.5%−95.6%) |
| 22 sec | 77.8% (52.4%−93.6%) |
69.8% (53.9%−82.8%) |
51.9% (39.1%−64.4%) |
88.2% (75.6%−94.8%) |
| 60 sec* | 39.0% (17.3%−64.2%) |
93.0% (80.9%−98.5%) |
70.0% (40.4%−88.9%) |
78.4% (71.4%−84.1%) |
indicates current cut-offs for balloon expulsion test
CI = confidence interval; NPV, negative predictive value; PPV, positive predictive value
For the tbBET, the currently used cut-off in many laboratories is 60 seconds, and this had a sensitivity of 39.0% (17.3%−64.2%) and specificity of 93.0% (80.9%−98.5%) to diagnose RED in our cohort. If the cut-off was changed to 15 seconds, the sensitivity improved to 83% (58.6%−96.4%) and specificity to 51.6% (35.5%−66.7%). In order to achieve the best combination of sensitivity and specificity, the “optimal” cut-off for tbBET was 22 seconds (sensitivity 77.8% [52.4%−93.6%], and specificity 69.8% [53.9%−82.8%]).
Discussion
Our study evaluated two techniques of balloon expulsion tests for diagnosing RED: weight-based and time-based. We included findings of the DRE, anorectal manometry, colonic transit, rectal gas area on scout film, and BET. We have shown the association between individual DRE findings and parameters on ARM, balloon expulsion and RASF.
In our analysis, we used latent class analysis to justify the incorporation of DRE parameters to the diagnosis of RED, in addition to two abnormal ARM parameters. We have also assessed the associations between each parameter on DRE and findings on ARM and showed that, in addition to the correlation between DRE and ARM findings, the combination of DRE and ARM helps in better identifying individuals with RED.
We diagnosed RED utilizing symptom criteria consistent with Rome III for functional defecation disorders,16 in addition to findings on DRE and on HRM. We did not use parameters related to BET because of the questionable accuracy as reported in the literature10–12 and the fact that we were exploring optimization of the balloon expulsion test itself.
The prevalence of RED in individuals with constipation presenting to our tertiary care center cohort was 74/276 (26.8%). This is similar to previous studies reporting a prevalence of RED around 20–30%.17,20,24 Among our patients with RED, there were some patients with evidence of slow colonic transit at 24 or 48h based on the validated scintigraphic method. This is consistent with prior studies showing that RED may be associated with secondary delay in colonic transit; our previous studies showed that about 25% of patients with RED had delayed colonic transit at 24 and 48h, and colonic transit was significantly slower in females than males with RED.25
We did not use defecography as the gold standard in view of reported methodological differences and poor inter-observer agreement, which have limited its overall usefulness;26 in addition, the evacuation of liquid contrast may not necessarily reflect the passage of solid stool. Impaired rectal emptying on proctography is included among diagnostic tests for RED. However, methodological differences and poor inter-observer agreement have limited the overall usefulness of rectal emptying studies.26 Structural disorders contributing to abnormal defecation may result from abnormalities such as enteroceles, rectoceles and rectal mucosal or full thickness intussusception. Clearly, a structural study is usually necessary to identify such structural disorders, although a recent retrospective analysis of patients assessed by high resolution manometry (HRM) suggested that measurements by HRM alone or HRM together with anorectal descent during evacuation may identify rectal prolapse and large rectoceles.13 Unfortunately, defecographic findings in the majority of patients with possible evacuation disorders show a high incidence of rectocele, sigmoidocele, and intussusception, and experienced colorectal experts have cautioned not to treat patients strictly based on radiographic findings.4 Moreover, participants with normal defecation may show features during defecography that are often considered pathological, such as a broad ranges of anorectal angle, excessive pelvic floor descent (up to 57mm in men and 59mm in women) and formation of rectocoeles (>1cm deep in 48% of women) or enteroceles (~10% of women).27 In up to 10% of healthy women, there is descent of the bladder base or uterus 4 cm or more below the pubococcygeal line, or a rectocele measuring 4 cm or larger based on MRI defecography.28
Therefore, despite the very recent consensus assessment that “in comparison with other tests of evacuatory function, defecography provides better overall evaluation of the defecatory process and structure and/or function of the anorectum”29 there are still many pitfalls in the diagnostic interpretation of defecography in patients with impaired rectal evacuation. In fact, the 2014 American College of Gastroenterology Clinical Guideline documents that defecography or MR defecography are used as an adjunct test when anorectal manometry and balloon expulsion tests are equivocal.30 Overall, defecography is associated with high cost, lack of availability, and low sensitivity to detect rectal intussusception,31,32 and it has not been recommended as a gold standard for RED.
The wbBET has been replaced by the tbBET in many centers. The reported benefit of the tbBET is that it is performed in the more physiological seated position, similar to defecation, as opposed to the wbBET, which is done in the left lateral position.14 Our current study showed that the wbBET was a significant predictor of RED in comparison to the tbBET. We showed that, with every 50-gram increase in balloon weight required for balloon expulsion, the odds ratio of RED increased by 16%. The wbBET (at a cut-off of 200g) identified cases of RED with a higher sensitivity than the tbBET (at 60 seconds and 22 seconds cut-offs). One potential explanation might be that the wbBET patients had more severe evacuation disorder than the patients who underwent tbBET. However, it turned out that the wbBET group had a rectoanal pressure gradient of −26.2mmHg (IQR −44.1; −7.7 mmHg) which was lower (not as negative) than the gradient of −41.0mmHg (−71.3; −13.4 mmHg) in the tbBET group. Therefore, the greater sensitivity of wbBET compared to tbBET (based on 60 second cut-off) cannot be explained by the greater disorder of rectal evacuation in the wbBET patients.
On the other hand, the tbBET had a higher specificity in diagnosing RED at the cut-off of 60 seconds, which has been validated in previous studies.3,12,33 Results from this audit support the hypothesis that, in patients with chronic constipation, the diagnosis of RED could be optimized for sensitivity and specificity with combinations of DRE, HRM and either wbBET or an optimized timed-based BET. Depending on the clinical setting, if the BET is meant to be used as a screening test for RED, then the wbBET (with higher sensitivity) might be a better option than the tbBET; however, the wbBET is no longer performed at our institution. Therefore, an alternative approach is to optimize the cut-off for the tbBET to diagnose RED. The mean time needed to expel the balloon in the RED group in our study was 31 seconds compared to 13 seconds in the non-RED group. A study by Lee et al. also showed that the tbBET is not useful for screening for RED, which is consistent with our findings.33 Minguez et al. showed similar results, suggesting that the tbBET is good to screen individuals without RED.12 Ratuapali et al. showed a modest agreement between the tbBET and the wbBET,14 and they suggested that, in an individual with constipation and high clinical suspicion for RED, the wbBET can be pursued if the tbBET was normal.14 Our regression models suggest the hypothesis that the optimal time cut-off may be 15 or 22 seconds, and this needs to be confirmed by further research in a prospective cohort.
While the DRE is not included in the Rome criteria, it is an essential and inexpensive tool performed in the clinic to assist with the diagnosis of RED in individuals with constipation. When performed by a trained specialist, DRE has been shown to have a high sensitivity and positive predictive value when compared to anorectal manometry.7,9 Unfortunately, many clinicians are inadequately trained to perform a sufficient and comprehensive DRE.9,10 We have further evaluated the association between resting anal tone and squeeze findings on DRE and high resolution anal sphincter pressure measurements. In those with increased resting tone, the median maximum resting pressure on HRM was 112.9mmHg, which is above the 104mmHg reported previously as the upper limit of normal.13,16,18 Similarly, the DRE was able to determine those with increased squeeze pressures; those patients had a median maximum squeeze pressure of 279.2mmHg on HRM, also consistent with abnormal pressures relative to the upper limit of 265mmHg.16,18 Our data further validate the utility of the DRE and suggest that, if adequately trained, providers can detect RED in a cohort with constipation by utilizing history and DRE34 to increase the pre-test probability prior to pursuing further expensive testing such as HRM or defecography.
We also included RASF in our evaluation of individuals with constipation. While RASF was not statistically different between the RED and non-RED groups in this cohort, the mean RASF for the RED group was higher than that of the non-RED group. Park et al. previously validated this technique with a cut-off of 9cm2, which was indicative of RED, with 17.5% sensitivity and 92.3% specificity.23 In our study, RASF was a good predictor of RED in the univariate analysis in the tbBET subgroup. With every increase in rectal gas RASF by 1cm2, there was an 8% increase in the odds ratio of RED. Additionally, since RASF is a predictor of RED in the tbBET subgroup with constipation, the data suggest that tbBET may detect the more severe cases of RED, which also result in rectal gas retention.
Both DRE and RASF (which could also be measured on a plain abdominal radiograph) are inexpensive and noninvasive indirect measurements of defecatory function which may be used in identifying patients with RED in clinical practice. This is particularly useful for providers practicing at centers that do not have access to specialized tests of defecatory function such as high resolution manometry, balloon expulsion or MRI defecography.
In our cohort, those with RED were younger in age than those without RED. In the Olmsted County, Minnesota cohort study by Noelting et al., the incidence per 100,000 of RED in women was greatest between the ages of 20 and 29 years, and declined with age, with a second peak between the ages of 80 and 89 years.2 This is consistent with our logistic regression model, which showed that, in both, wbBET and tbBET subgroups, the odds ratio of RED decreased by 30–47% with every 10-year increase in age. Our cohort did not include individuals above the age of 80 years and, hence, we were not able to confirm the second peak described by Noelting et al.2 Similar to previously published data, we found no difference in BMI in the RED and non-RED groups.17
Limitations and Strengths
We recognize that our study has limitations. The patients in this retrospective study underwent either tbBET or wbBET, and there were more patients with wbBET (assessed between 2007 and 2014) than tbBET (assessed between 2015–2018); the latter restricted the number of associated features that could be tested in the regression model. The investigators performing statistical analysis also performed data acquisition from the medical records. However, the categorization of RED and non-RED for this research study utilized simple criteria for the diagnosis of RED based on objective findings extracted from the medical records. Our cohort was referred to a single gastroenterologist, increasing the risk of referral bias, but currently the majority of patients with RED are seen at tertiary care referral centers. A final limitation is that there is no established gold standard and therefore the reference standard used is empirical; however, we tried to overcome any bias by including parameters based on consensus symptom-based Rome III (and IV) criteria, and at least 2 findings on both DRE and HRM.
Despite these limitations, we believe our current study identified simpler modalities to screen for RED, such as the DRE, RASF, and tbBET >22seconds. If replicated, we believe these simpler tests would constitute a clinically relevant advance in the diagnosis of RED, which is a frequently misdiagnosed condition that is eminently treatable. In addition, our audit achieved the objective to generate the preliminary data in support of the hypothesis that, in patients with chronic constipation, the diagnosis of RED can be optimized for sensitivity and specificity with combination of DRE, HRM and an optimized timed-based BET.
Conclusion
We have identified different predictors that can assist in the diagnosis of RED, which is achieved with high sensitivity assessments with a combination of the DRE and HRM. The tbBET with cut-off of 60 seconds was specific, but not sensitive for diagnosing RED in our cohort. Further prospective research is warranted to test the hypothesis that an optimal time cut-off for tbBET (e.g., 22 seconds, based on our logistic regression analysis) can be identified to diagnose RED with the highest combination of specificity and sensitivity.
KEY POINTS
Current Knowledge
High resolution anorectal manometry (HRM) and balloon expulsion test (BET) are standard approaches to evaluation of defecatory function in patients with chronic constipation. There is no “gold standard” to confirm diagnosis of rectal evacuation disorder (RED).
Results of Current Paper
A combination of digital rectal exam (DRE) and HRM can identify RED with high sensitivity in chronic constipation.
Importance of These Results
Exploring new time cut-offs for BET can improve sensitivity and specificity of diagnosing RED.
Acknowledgement:
The authors thank Mrs. Cindy Stanislav for excellent secretarial assistance.
Funding: Dr. Camilleri is funded by grants R01-DK67071 and R01-DK115950 from National Institutes of Health.
Abbreviations:
- ANOVA
analysis of variance
- ARM
Anorectal manometry
- AUC
area under the curve
- BET
Balloon Expulsion Test
- BMI
Body Mass Index
- CT
colonic transit
- GC
geometric center
- HRM
High-Resolution anorectal manometry
- In
Indium
- IQR
interquartile range
- RASF
Rectal area of gas on scout film
- RED
Rectal Evacuation Disorders
- ROC
Receiver-operating curve
- SD
Standard Deviation
- tbBET
Time-based balloon expulsion test
- wbBET
Weight-based balloon expulsion test
Footnotes
Disclosures: The authors have no conflicts of interest.
REFERENCES
- 1.Camilleri M, Ford AC, Mawe GM, et al. Chronic constipation. Nat Rev Dis Primers 2017;3:17095. [DOI] [PubMed] [Google Scholar]
- 2.Noelting J, Eaton JE, Choung RS, et al. The incidence rate and characteristics of clinically diagnosed defecatory disorders in the community. Neurogastroenterol Motil 2016;28:1690–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A. Functional anorectal disorders. Gastroenterology 2016;150:1430–1442, e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agachan F, Pfeifer J, Wexner SD. Defecography and proctography. Results of 744 patients. Dis Colon Rectum 1996;39:899–905. [DOI] [PubMed] [Google Scholar]
- 5.Palit S, Thin N, Knowles CH, Lunniss PJ, Bharucha AE, Scott SM. Diagnostic disagreement between tests of evacuatory function: a prospective study of 100 constipated patients. Neurogastroenterol Motil 2016;28:1589–1598. [DOI] [PubMed] [Google Scholar]
- 6.Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel disorders. Gastroenterology 2016;150:1393–1407. [DOI] [PubMed] [Google Scholar]
- 7.Soh JS, Lee HJ, Jung KW, et al. The diagnostic value of a digital rectal examination compared with high-resolution anorectal manometry in patients with chronic constipation and fecal incontinence. Am J Gastroenterol 2015;110:1197–1204. [DOI] [PubMed] [Google Scholar]
- 8.Bharucha AE, Wald A, Enck P, et al. Functional anorectal disorders. Gastroenterology 2006;130:1510–1518. [DOI] [PubMed] [Google Scholar]
- 9.Tantiphlachiva K, Rao P, Attaluri A, et al. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clin Gastroenterol Hepatol 2010;8:955–960. [DOI] [PubMed] [Google Scholar]
- 10.Caetano AC, Santa-Cruz A, Rolanda C. Digital rectal examination and balloon expulsion test in the study of defecatory disorders: are they suitable as screening or excluding tests? Can J Gastroenterol Hepatol 2016;2016:8654314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grossi U, Carrington EV, Bharucha AE, et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 2016;65:447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minguez M, Herreros B, Sanchiz V, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62. [DOI] [PubMed] [Google Scholar]
- 13.Prichard DO, Lee T, Parthasarathy G, et al. High-resolution anorectal manometry for identifying defecatory disorders and rectal structural abnormalities in women. Clin Gastroenterol Hepatol 2017;15:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ratuapli S, Bharucha AE, Harvey D, et al. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil 2013;25:e813–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park S-Y, Khemani D, Nelson AD, et al. Rectal gas volume measured by computerized tomography identifies evacuation disorders in patients with constipation. Clin Gastroenterol Hepatol 2017;15:543–552. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ratuapli SK, Bharucha AE, Noelting J, et al. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology 2013;144:314–322, e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nullens S, Nelsen T, Camilleri M, et al. Regional colon transit in patients with dys-synergic defaecation or slow transit in patients with constipation. Gut 2012;61:1132–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noelting J, Ratuapli SK, Bharucha AE, et al. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol 2012;107:1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones MP, Post J, Crowell MD. High-resolution manometry in the evaluation of anorectal disorders: a simultaneous comparison with water-perfused manometry. Am J Gastroenterol 2007;102:850–855. [DOI] [PubMed] [Google Scholar]
- 20.Pemberton JH, Rath DM, Ilstrup DM. Evaluation and surgical treatment of severe chronic constipation. Ann Surg 1991;214:403–411; discussion 411–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deiteren A, Camilleri M, Bharucha AE, et al. Performance characteristis of scintigraphic colon transit measurement in health and irritable bowel syndrome and relationship to bowel functions. Neurogastroenterol Motil 2010;22:415–e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kolar GJ, Camilleri M, Burton D, Nadeau A, Zinsmeister AR. Prevalence of colonic motor or evacuation disorders in patients presenting with chronic nausea and vomiting evaluated by a single gastroenterologist in a tertiary referral practice. Neurogastroenterol Motil 2014;26:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park SY, Khemani D, Acosta A, et al. Rectal gas volume: Defining cut-offs for screening for evacuation disorders in patients with constipation. Neurogastroenterol Motil 2017;29:e13044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skardoon GR, Khera AJ, Emmanuel AV, et al. Review article: dyssynergic defaecation and biofeedback therapy in the pathophysiology and management of functional constipation. Aliment Pharmacol Ther 2017;46:410–423. [DOI] [PubMed] [Google Scholar]
- 25.Shin A, Camilleri M, Nadeau A, Nullens S, Rhee JC, Jeong ID, Burton DD. Interpretation of overall colonic transit in defecation disorders in males and females. Neurogastroenterol Motil 2013;25:502–508, e369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Videlock EJ, Lembo A, Cremonini F. Diagnostic testing for dyssynergic defecation in chronic constipation: meta-analysis. Neurogastroenterol Motil 2013;25:509–520. [DOI] [PubMed] [Google Scholar]
- 27.Shorvon PJ, McHugh S, Diamant NE, et al. Defecography in normal volunteers: results and implications. Gut. 1989;30:1737–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tirumanisetty P, Prichard D, Fletcher JG, Chakraborty S, Zinsmeister AR, Bharucha AE. Normal values for assessment of anal sphincter morphology, anorectal motion, and pelvic organ prolapse with MRI in healthy women. Neurogastroenterol Motil. 2018. March 2. doi: 10.1111/nmo.13314. [Epub ahead of print]). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrington EV, Scott SM, Bharucha A, Mion F, Remes-Troche JM, Malcolm A, Heinrich H, Fox M, Rao SS; International Anorectal Physiology Working Group and the International Working Group for Disorders of Gastrointestinal Motility and Function. Expert consensus document: Advances in the evaluation of anorectal function. Nat Rev Gastroenterol Hepatol. 2018. May;15(5):309–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wald A, Bharucha AE, Cosman BC, et al. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol 2014;109:1141–57; (Quiz) 1058. [DOI] [PubMed] [Google Scholar]
- 31.Pilkington SA, Nugent KP, Brenner J, et al. Barium proctography vs magnetic resonance proctography for pelvic floor disorders: a comparative study. Colorectal Dis 2012;14:1224–30. [DOI] [PubMed] [Google Scholar]
- 32.Schreyer AG, Paetzel C, Furst A, et al. Dynamic magnetic resonance defecography in 10 asymptomatic volunteers. World J Gastroenterol 2012;18:6836–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee J, Hong KS, Kim JS, et al. Balloon Expulsion Test Does Not Seem to Be Useful for Screening or Exclusion of Dyssynergic Defecation as a Single Test. Journal of Neurogastroenterology and Motility 2017;23:446–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lembo A, Camilleri M. Chronic constipation. N Engl J Med 2003;349:1360–8. [DOI] [PubMed] [Google Scholar]