Abstract
Castleman's disease is an uncommon benign B-cell lymphoproliferative disorder. According to lymph nodes distribution, there are two distinct subtypes of disease: unicentric and multicentric. Unicentric Castleman's disease is more common, localized to one site, and locally treated. On the contrary, multicentric form is a rare systemic disease characterized by diffuse lymphadenopathy and inflammatory symptoms. We report three cases of persons that were initially suspected to have a lymphoma but were later histologically confirmed to have Multicentric Castleman's Disease. In addition, our work aims to investigate the role of fluorodeoxyglucose (FDG) PET/CT in evaluation of this rare condition.
Keywords: Multicentric Castleman's disease, Hyaline vascular type, FDG PET/CT
Background
Castleman's disease (CD) is a heterogeneous group of lymphoproliferative disorders of unknown cause presenting with lymphadenopathy. This clinicopathologic entity, also known as angiofollicular lymph node hyperplasia and giant lymph node hyperplasia, is a rare relatively benign process characterized by nonclonal lymphocyte proliferation. CD is a condition histologically and prognostically distinct from malignant lymph-node hyperplasia.
The disease may present as a localized or multicentric form. The localized form is often asymptomatic and is characterized by an isolated enlarged lymph node that regresses without sequelae after surgical excision. Multicentric Castleman's disease (MCD) is always symptomatic and is characterized by polyadenopathy and general signs [1]. Symptoms, primarily a consequence of elevated Interleukin-6 production, are asthenia, weight loss, and fever. Splenomegaly is common. The prognosis of the latter form is much less favorable and treatment often requires chemotherapy [2]. Diagnosis of CD is histologic, made upon biopsy of an excised lymph-node. There are three histologic variants of disease: hyaline vascular type (the most common), plasma cell type, and mixed type [[3], [4]]. CD was first described in a group of patients with localized hyperplastic lymph-nodes in 1956 by Benjamin Castleman [5]. He reported 13 cases of unicentric hyaline vascular CD of the chest and described the classic pathologic features of hypervascular lymph nodes with hyalinization of vessels, which form concentric arrangements somewhat reminiscent of Hassall corpuscles. MCD was described by Gaba in 1978 [6]. The etiology of CD remains unknown but several reports have indicated the role of human herpesvirus 8, especially in multicentric forms [7].
This is a retrospective study on three patients with histologically confirmed MCD hyaline vascular type who were evaluated by the Diagnostic Imaging Department of Tor Vergata for the period 2016-2017. Systemic pretreatment and post-treatment staging was performed by using CT and FDG PET-CT. Total body CT examinations of case 1 were performed using a 64 row scanner (LightSpeed VCT, General Electric Medical Systems), before and after the injection of iodinate contrast medium (Iomeron 350 mg/mL, Bracco Imaging). FDG PET/CT examinations of cases 2 and 3 were performed using a Discovery ST Integrated PET-CT System (General Electric Medical Systems).
Case 1
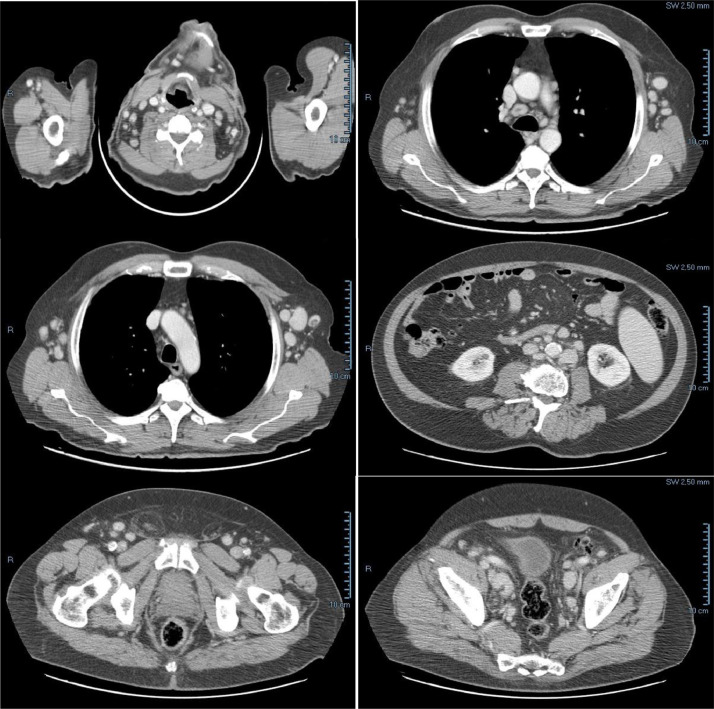
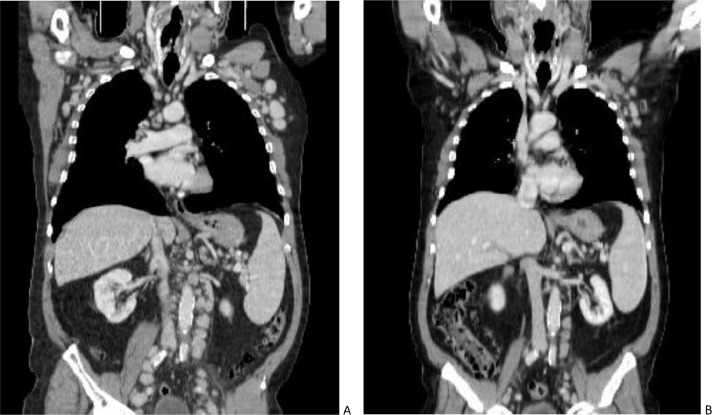
A 70- year-old man with a 3 month history of fever, night sweats, asthenia, and weight loss was referred to a hematologist by his general practitioner for suspected leukemia or lymphoproliferative disorder. Physical examination revealed bilateral cervical, axillary and inguinal lymphadenopathy with mild palpable splenomegaly. Routine investigations were found to be within normal range except for a polyclonal increase in gamma-globulins. A contrast-enhanced CT performed in our department confirmed widespread lymphadenopathy (Fig. 1). Biopsy of a right axillary lymph node was collected with the diagnosis of MCD hyaline vascular type. After treatment with rituximab (Anti-CD20 mAb) and steroid therapy, the patient performed a contrast enhanced CT for evaluation of treatment response. A reduction in size of lymph nodes was observed (Fig. 2). Unfortunately response has been short lived and treatment required a combination chemotherapy regimen (CHOP).
Fig. 1.
Case 1. Contrast-enhanced CT showing multiple, hyperenhancing, enlarged lymph nodes.
Fig. 2.
Case 1. Contrast-enhanced CT before (A) and after (B) therapy. Mediastinal, axillary, para-aortic and iliac swollen lymph nodes have reduced in size but multiple lymphadenopathies still persist on CT.
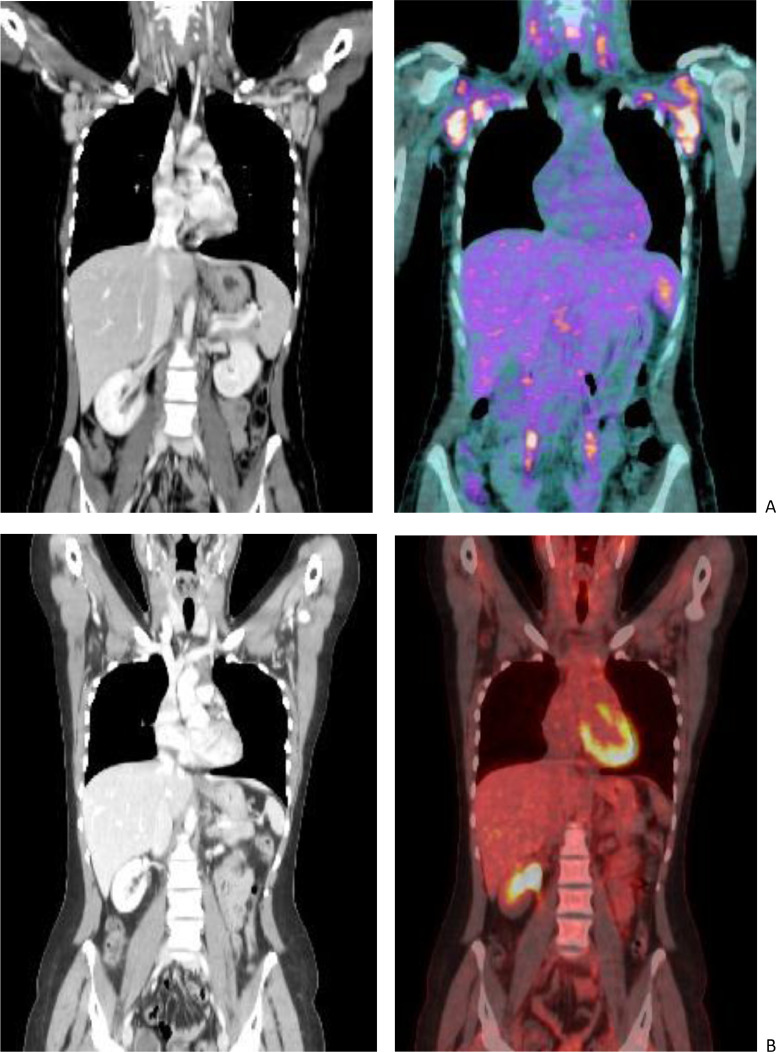
Case 2
A 27-year-old woman, with flu-like symptoms and bilateral axillary lymph node enlargement, was referred to our department for an FDG PET/CT scan that confirmed multiple swollen lymph nodes with high FDG uptake value in cervical and axillary regions (Fig. 3A). The PET/CT scan obtained some weeks after steroid treatment showed a complete disappearance of MCD lesions (Fig. 3B).
Fig. 3.
Case 2. Evaluation with FDG PET/contrast-enhanced CT before and after therapy. (A) High FDG uptake observed in enlarged axillary lymph nodes. (B) Complete regression of disease.
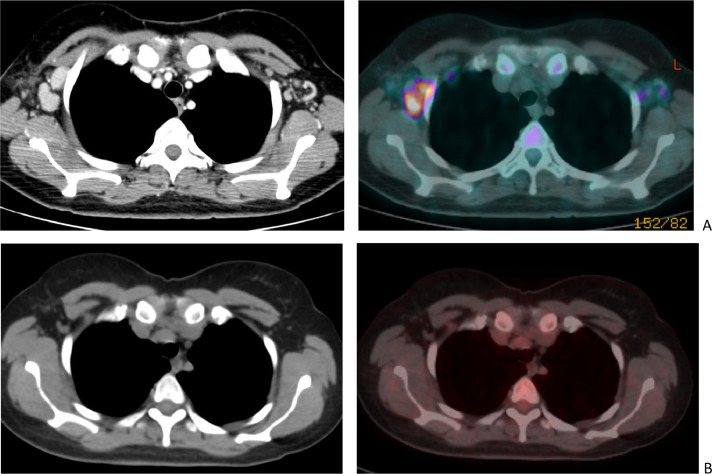
Case 3
We evaluated another case of MCD in a 40-year-old woman with medical history of fever, asthenia, and diffuse superficial lymphadenopathy. She performed an FDG PET/CT scan before and after steroid therapy. Even in this case, PET/CT evaluation demonstrated morphologic and metabolic regression of disease (Fig. 4).
Fig. 4.
Case 3. Evaluation with FDG PET/CT before and after therapy. (A) FDG-avid, enlarged and hyperenhancing axillary lymph nodes before therapy. (B) MCD lesions show complete metabolic response to steroid treatment.
Discussion
MCD can present with multiple enlarged lymph nodes with FDG avidity on whole body PET/CT and can mimic lymphoma [8, 9]. Even if PET/CT is not specific for the differential diagnosis of MCD from other benign or malignant lymphoproliferative diseases, we want to emphasize the role of PET/CT for evaluation of this uncommon condition. Compared to conventional contrast-enhanced CT, FDG PET/CT scan shows a better correlation with the extent and severity of disease. PET/CT allows accurate analysis of anatomic and/or morphologic and metabolic and/or functional informations and results more sensitive for the diagnosis of MCD lesions. Furthermore, the degree of FDG uptake in MCD lesions is well correlated with symptoms and response to therapy, suggesting that FDG PET/CT might be better than CT for clinical decisions and treatment evaluation in patients with MCD.
Footnotes
No conflicts of interest to disclose.
References
- 1.Sarrot-Reynauld F. 2001. http://www.orpha.net/data/patho/GB/uk-castleman.pdf Castleman's disease; Orphanet encyclopaedia, August.
- 2.Herrada J., Cabanillas F., Rice L., Manning J., Pugh W. The clinical behaviour of localized and multicentric Castleman disease. Ann Intern Med. 1998;128:657–662. doi: 10.7326/0003-4819-128-8-199804150-00010. [DOI] [PubMed] [Google Scholar]; PubMed.
- 3.Cronin D.M., Warnke R.A. Castleman disease: an update on classification and the spectrum of associated lesions. Adv Anat Pathol. 2009;16:236–246. doi: 10.1097/PAP.0b013e3181a9d4d3. [DOI] [PubMed] [Google Scholar]; PubMed.
- 4.Liu A.Y., Nabel C.S., Finkelman B.S., Ruth J.R., Kurzrock R., van Rhee F. Idiopathic multicentric Castleman's disease: a systematic literature review. Lancet Haematol. 2016;3(4):e163–e175. doi: 10.1016/S2352-3026(16)00006-5. [DOI] [PubMed] [Google Scholar]
- 5.Castleman B., Iversonl L., Menendez V.P. Localized mediastinal lymphnode hyperplasia resembling thymoma. Cancer. 1956;9:822–830. doi: 10.1002/1097-0142(195607/08)9:4<822::aid-cncr2820090430>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]; PubMed.
- 6.Gaba A.R., Stein R.S., Sweet D.L. Multicentric giant lymph node hyperplasia. Am J Clin Pathol. 1978;69:86–90. doi: 10.1093/ajcp/69.1.86. [DOI] [PubMed] [Google Scholar]; PubMed.
- 7.Sarrot-Reynauld F., Morand P., Buisson M. Groupe francais d'etude de la maladie de Castleman. Maladie de Castleman et infection par le virus HHV-8. Rev Med Interne. 1998;19:413. [Google Scholar]
- 8.Bonekamp D., Horton K.M., Hruban R.H., Fishman E.K. Castleman disease: the great mimic. Radiographics. 2011;31:1793–1807. doi: 10.1148/rg.316115502. [DOI] [PubMed] [Google Scholar]
- 9.Lee E.S., Paeng J.C., Park C.M., Chang W., Lee W.W., Kang KW. Metabolic characteristics of Castleman disease on 18F-FDG PET in relation to clinical implication. Clin Nucl Med. 2013;38:339–342. doi: 10.1097/RLU.0b013e3182816730. PubMed] [Cross Ref. [DOI] [PubMed] [Google Scholar]