Abstract
Fetus in fetu is a rare condition which most often presents as a fetiform calcified mass in the abdomen of its host, fetus or newborn. We report a case of 8-month-old girl with history of abdominal distension. Ultrasonography and computed tomography scan revealed a mass in which the contents favor a fetus in fetu rather than a teratoma. She underwent surgery and the mass was resected in toto. Radiograph of the resected specimen showed the presence of rudimentary vertebral column which was later confirmed by pathologist.
Keywords: Fetus in fetu (FIF)
Introduction
Fetus in fetu (FIF) is a rare pathological condition presenting as foetoid tumor within the body of an individual, usually as an abdominal mass in infants.
Fetus in fetu is a condition associated with abnormal embryogenesis, with two possible mechanisms one is a twinning theory [1] and the other highly differentiated teratoma. It is often overlooked in the differential diagnosis of intra-abdominal mass and should be differentiated from a teratoma because of teratomas malignant potential. Preoperative diagnosis is based on radiologic findings. Other reported locations include cranial cavity, mediastinum, and scrotum [2]. There is a report on antenatal detection of FIF within the abdomen of 34-week fetus using 3-dimensional ultrasound [16].
Here we report a case of 8-month-old baby with abdominal distension due to a foetoid tumor like mass which was confirmed as FIF.
Case report
An 8-month-old baby girl with complaints of abdominal distension was referred to our department for computed tomography (CT) examination. Physical examination revealed a well-developed and well-nourished girl. No family history of twinning was present. No significant prenatal history. It was a normal term vaginal delivery, postnatal period was uneventful. Abdominal distension was noticed by the parents.
Abdomen was grossly distended; on local examination a nontender mass of variable consistency was palpated. No abnormal sounds auscultated over the swelling. Ultrasound of the abdomen was performed from outside which showed large heterogeneous solid-cystic mass in the abdomen. Linear calcified areas with dense posterior acoustic shadowing was evident. Minimal vascularity was appreciated on color Doppler examination.
Plain and postcontrast CT scan of abdomen was performed with 64 slice multiple detector CT scanner after intravenous sedation. CT scan showed a 13 × 12 × 9 cm sized well-circumscribed retroperitoneal mass lesion with bulk toward left side (Fig. 1). Mass contained predominantly fatty tissue surrounding a central bony structure having foetoid morphology (Fig. 2).
Fig. 1.
CECT coronal image showing large retroperitoneal mass with fatty and calcified internal components. Note mass effect on adjacent organs.
Fig. 2.
CECT axial section at the level of kidneys showing a well-defined retroperitoneal mass with internal fat and calcified components.
It also had fluid density areas, enhancing solid areas, and nodular calcifications. Lesion was producing mass effect on the nearby organs without any features of infiltration (Figs. 1 and 2). Blood supply to the lesion was from abdominal aorta.
Laparotomy and surgical exploration was done and a large retroperitoneal mass was resected in toto.
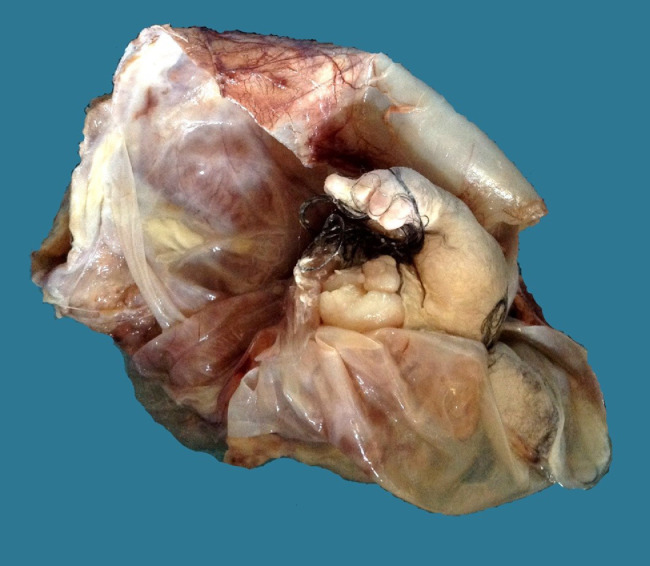
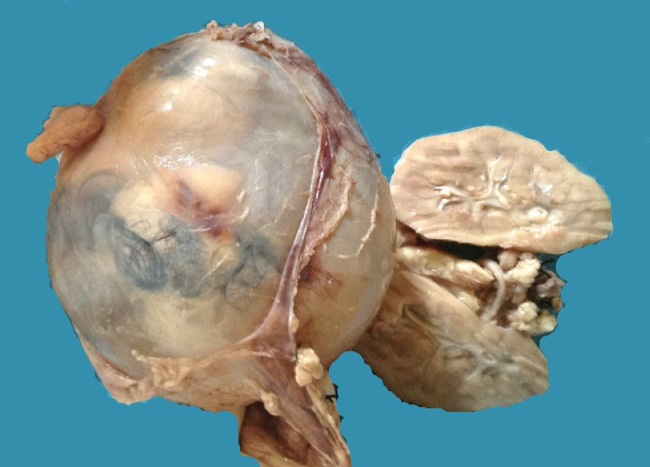
The gross pathology specimen revealed membrane covered mass having areas of foetoid differentiation. It contained partly formed limbs fully covered with skin partly formed vertebrae, cartilaginous tissue, hair, fat, and also showed a reniform structure (Figs. 3 to 5).
Fig. 4.
Gross specimen showing cartilage and hairs.
Fig. 3.
Gross specimen showing fetiform presentation of the mass. Structures represent malformed limbs with fingers, hairs, and the ruptured sac.
Fig. 5.
Gross specimen showing unruptured sac containing the malformed fetus.
Specimen radiograph confirmed the presence of limb bones and vertebrae (Fig. 6).
Fig. 6.
Radiograph of the gross specimen shows malformed vertebral column (arrows).
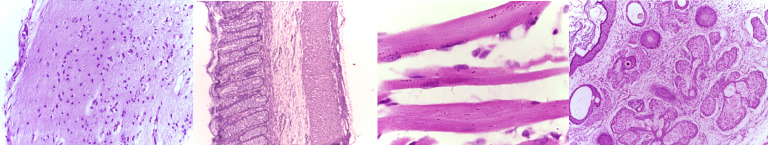
Microscopy revealed bone, skeletal and smooth muscles, and glandular elements (Fig. 7).
Fig. 7.
Histopathology images showed glial tissue, intestinal epithelium, skeletal muscles, and skin-sebaceous glands (from left-right).
The hallmark of FIF is the presence of vertebra along with appendicular bones and formed organs. And our case correctly matches the criteria.
Discussion
The term “fetus in fetu” was first described by Johann Friedrich Meckel during the late 18th century [3]. Later Willis described it as a rare condition where a parasitic twin resides in the body of its host usually the abdominal cavity [4]. Incidence is approximately one in 500,000 births with 2:1 male predominance [5].
Exact embryogenesis is controversial. There are two proposed theories, one describing FIF as a variant in the spectrum of monozygotic twinning and the other a highly differentiated teratoma. The presence of a complete or partial vertebral column plus other appropriately situated axial or appendicular bones or organs is the hallmark of FIF [6].
FIF is described as development of high organotypic type [7] with formation of vertebra and arrangement of tissues around it. Usual presentation of FIF is as a solitary mass. Multiple foetoid elements have also been reported [8]. The condition usually presents in infants and children. There are a few reports of the condition occurring in adult life [9].
Main differentiating feature FIF from teratoma is the identification of vertebral bodies or limbs [6].
The presence of vertebral bodies is a clue to postulate FIF having gone through that particular stage of embryogenesis known as gastrulation, indirectly reflecting its derivation from primitive streak developing during the third week in a normal embryo. This theory states that FIF likely arises from a zygote at a primitive-streak stage. In other words mass formation follows normal fatal development up to a particular phase. There are studies demonstrating the mass and host infant sharing the same genotype [10] further supporting the theory. A teratoma consists of pluripotent cells but organogenesis or vertebral segmentation is unusual. One observation pointing toward the teratoma theory is the occurrence of a mass in the expected locations of teratoma in an infant like retroperitoneum and ovaries [11]. Occasionally, it can occur even in a cryptorchidism testis [17]. Another observation holding against a twin fetus theory is the occasional teratoma formation after the FIF resection in the same surgical site. But reported incidences stating co-existence of FIF and teratoma is controversial.
Some times teratomas contain well-developed fetiform structures like brain and spinal cord [12]. But the occurrence of vertebral segments is never reported. Features highlighted by spencer to differentiate teratoma from FIF are lesser organization of microscopically identifiable tissues in the former and broader attachment site with multiple smaller blood vessels.
From a radiological and surgical perspective making a preoperative diagnosis and differentiating it from the usual and more common congenital mass that is teratoma is important. This is because of the fact that there is an associated 10% chance of malignancy developing in a teratoma whereas FIF is a benign condition. There has been only one report that showed malignant transformation of FIF, to our knowledge [13].
Imaging plays a role in accurate preoperative diagnosis. Visualization of the vertebral column and limbs forms the key differentiating feature to aid diagnosis. The Willis criterion stresses much emphasis on the development of axial skeleton and vertebral axis [4].
CT scans especially with multiplanar and volume rendering capabilities can correctly identify the vertebral column and other skeletal elements. It is useful in correctly detecting fat and soft tissues. Possible pressure effect on the adjacent organs as well as the feeding arteries and draining veins can be correctly identified. Initial CT appearance reported by Nocera et al. describes a mass that consisting of peripheral collection of fat surrounding a central bony structure [14]. Our case had a similar appearance with a foetaoid mass surrounded by a collection of fat.
Surgical excision is the recommended treatment. Usually the tumor derives its blood supply from the rich capsular vascular network, usually derived from the plexus where the sac is attached to abdominal wall. A few cases had definite vascular connections from major vessels [15]. Postsurgical follow-up imaging is the recommendation to rule out recurrence.
References
- 1.Gangopadhyay A.N., Srivastava A., Srivastava P. Twin fetus in fetu in a child: a case report and review of the literature. J Med Case Reports. 2010;4:96. doi: 10.1186/1752-1947-4-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang S.T., Leow S.W. Intracranial fetus in fetu: CT diagnosis. AJNR Am J Neuroradiol. 1992;13:1326–1329. [PMC free article] [PubMed] [Google Scholar]
- 3.Senyüz O.F., Rizalar R., Celayir S., Oz F. Fetus in fetu or giant epignathus protruding from the mouth. J Pediatr Surg. 1992;27:1493–1495. doi: 10.1016/0022-3468(92)90480-u. [DOI] [PubMed] [Google Scholar]
- 4.Willis R.A. Butterworths; Washington, DC: 1962. The borderland of embryology and pathology, 2; pp. 442–462. [PMC free article] [PubMed] [Google Scholar]
- 5.Thakral C.L., Maji D.C., Sajwani M.J. Fetus-in-fetu: a case report and review of the literature. J Pediatr Surg. 1998;33:1432–1434. doi: 10.1016/s0022-3468(98)90029-x. [DOI] [PubMed] [Google Scholar]
- 6.Magnus K.G., Millar A.J., Sinclair-Smith C.C., Rode H. Intrahepatic fetus-in-fetu: a case report and review of the literature. J Pediatr Surg. 1999;34:1861–1864. doi: 10.1016/s0022-3468(99)90333-0. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Crussi F. Armed Forces Institute of Pathology; Washington, DC: 1982. Atlas of tumor pathology. [Google Scholar]
- 8.Gerber R.E., Kamaya A., Miller S.S., Cronin D.M., Dwyer B., Chueh J. Fetus in fetu: 11 fetoid forms in a single fetus. J Ultrasound Med. 2008;27:1381–1387. doi: 10.7863/jum.2008.27.9.1381. [DOI] [PubMed] [Google Scholar]
- 9.Dagradi A.D., Mangiante G.L., Serio G.E., Musajo F.G., Menestrina F.V. Fetus in fetu removal in a 47-year-old man. Surgery. 1992;112:598–602. [PubMed] [Google Scholar]
- 10.Miura S., Miura K., Yamamoto T., Yamanaka M. Origin and mechanisms of formation of fetus-in-fetu: two cases with genotype and methylation analyses. Am J Med Genet A. 2006;140(16):1737–1743. doi: 10.1002/ajmg.a.31362. [DOI] [PubMed] [Google Scholar]
- 11.Derniaux E., Zachar D., Bory J.P., Gaillard D., Favre R., Graesslin O. Detection of a prenatal mature tumor arising from the external genitalia in a female fetus: fetus-in-fetu or teratoma? Prenat Diagn. 2010;30(11):1110-. doi: 10.1002/pd.2629. [DOI] [PubMed] [Google Scholar]
- 12.Weiss J.R., Burgess J.R., Kaplan K.J. Fetiform teratoma (homunculus) Arch Pathol Lab med. 2006;130(10):1552. doi: 10.5858/2006-130-1552-FTH. [DOI] [PubMed] [Google Scholar]
- 13.Hopkin K.L., Dickson P.K., Ball T.I., Ricketts R.R., O?Shea P.A., Abramovosky C.R. Fetus in fetu with malignant recurrence. J Pediatr Syrg. 1997;32:1476–1479. doi: 10.1016/s0022-3468(97)90567-4. [DOI] [PubMed] [Google Scholar]
- 14.Nocera R.M., Davis M., Hayden C.K., Jr, Schwartz M., Swischuk L.E. Fetus in fetu. AJR Am J Roentgenol. 1982;138:762–764. doi: 10.2214/ajr.138.4.762. [DOI] [PubMed] [Google Scholar]
- 15.Heifetz S.A., Alrabeeah A., Brown B.S., Lau H. Fetus in fetu: a fetiform teratoma. Pediatr Pathol. 1988;8:215–226. doi: 10.3109/15513818809022299. [DOI] [PubMed] [Google Scholar]
- 16.Jones D.C., Reyes-Múgica M., Gallagher P.G., Fricks P., Touloukian R.J., Copel J.A. Three-dimensional sonographic imaging of a highly developed fetus in fetu with spontaneous movement of the extremities. J Ultrasound Med. 2001;20(12):1357–1363. doi: 10.7863/jum.2001.20.12.1357. [DOI] [PubMed] [Google Scholar]
- 17.Landmann A., Calisto J.L., Reyes-Múgica M., Thomas D., Malek M.M. Fetus-in-Fetu presenting as a cryptorchid testis and abdominal mass: a report of a case and review of the literature. J Pediatr Surg Case Reports. 2016;13:38–40. [Google Scholar]