ABSTRACT
Each year in the UK, it is estimated that more than 100,000 people are admitted to hospital with sepsis and around 37,000 people will die as a result of the condition. We present an audit, re-audit and the implications these have had on the management of severe sepsis using the Sepsis Six, ultimately through actively promoting teamwork to initiate the protocol. This led to a significant improvement in management, decreasing admissions to the intensive care unit (ITU), length of stay in hospital and the number of patient deaths.
The initial audit and re-audit were done over 2-month periods. All clerking notes of patients with a medical consultant diagnosis of ‘sepsis’ on post-take ward round were analysed and further screened for presence of severe sepsis according to national guidelines.
There was significant improvement from only 1% of patients being appropriately managed (according to the existing guidelines) to 67% of eligible subjects adhering to the protocol (p<0.0001). Initially, 19% were admitted to the ITU (6% died), improving to 7% on re-audit (with no deaths). Length of hospital stay reduced from 10 to 7 days (p<0.0001).
There was a complete change in the management of severe sepsis with trust-wide updated protocols, resulting in a decrease in hospital morbidity and mortality.
KEYWORDS: Morbidity and mortality, sepsis, Sepsis Six, severe sepsis, teamwork
Introduction
Across many acute medicine units (AMUs), there is variable awareness of local and national guidelines for the optimal management of sepsis. A 24-month improvement programme in 30 countries measuring the delivery of the severe sepsis resuscitation bundle was unreliable, with compliance rising from 10% to 21% in self-selected centres.1
Through reflective practice, we present a quality improvement project, which demonstrates the key to success in timely management of severe sepsis, with significant and dedicated use of appropriate teamwork.
NHS England has established sepsis as a future indicator of the national outcomes framework.6
In the UK, sepsis causes approximately 37,000 deaths and 100,000 hospital admissions per year, with an overall mortality rate for admissions with severe sepsis of 35% (five times higher than for ST elevation myocardial infarction (STEMI) and stroke).2,3
Sepsis is a physiological response to infection and inadequate treatment may result in tissue damage, leading to multi-organ failure and, ultimately, death.4 This is manifested by the presence of two or more systemic inflammatory response syndrome (SIRS) criteria (Box 1).5 Sepsis is classified as severe when organ failure occurs.6
Box 1.
Systemic inflammatory response syndrome (SIRS) criteria6
Sepsis is confirmed if any two of the following are present:
|
Lactate levels in sepsis are highly predictive of death (Table 1).7 An initial elevation is a strong predictor of survival.
Table 1.
The relationship between lactate levels and mortality in sepsis patients7
| Lactate (mmol/L) | Mortality (%) |
|---|---|
| <2 | 15 |
| 2–4 | 25 |
| >4 | 38 |
Severe sepsis is time sensitive. Crucially, for every hour delay in antibiotic administration, there is an 8% increase in mortality.8
The Sepsis Six is an initial resuscitation bundle that offers basic intervention within the first hour: a prospective observational study has shown that it was independently associated with survival, suggesting that if it alone were responsible for outcome differences, the number needed to treat (NNT) to prevent one death is 4.6.9 Comparatively, the NNT is 42 for aspirin in a major heart attack and 45–90 for percutaneous coronary intervention in STEMI.6
We propose two questions:
Have we fulfilled the definition of audit, ie repeating analysis with a view to change in practice in accordance with national standards?
Have our measures lead to a significant change in morbidity and mortality?
Methods
Patients were audited over a 2-month period, from the middle of September to the middle of November 2014. All clerking notes of patients with a medical consultant diagnosis of ‘sepsis’ on post-take ward round were analysed and further screened for presence of severe sepsis according to national guidelines.
This was re-audited from the middle of April to the middle of June 2015, after presenting our findings to departmental and clinical hospital committees (specifically the accident and emergency clinical governance group), and updating of the online blood requesting system to show a ‘sepsis’ tab – which would show the protocol and request appropriate bloods automatically (Fig 1). This was an instrumental step.
Fig 1.
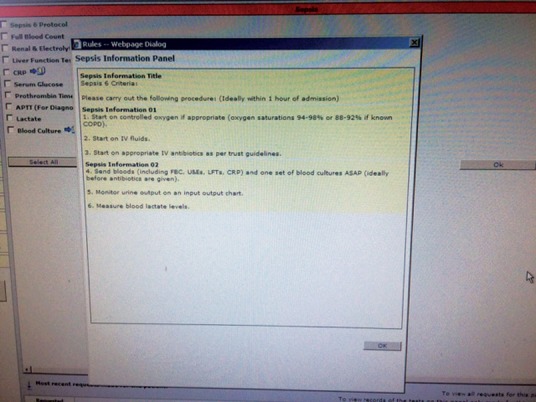
Online initiation of the Sepsis Six – ‘sepsis’ tab.
Morbidity and mortality were assessed by reviewing the number of intensive care unit (ITU) admissions, number of deaths and the average length of hospital stay.
Data management and analysis
Date and time of admission coupled with details of administration of intravenous fluids, antibiotics and high flow oxygen, and the taking of blood cultures, monitoring of urine output and lactate measurement were collated. The information gathered was then statistically analysed using the Fisher’s exact test (Tables 2 and 3).10,11
Table 2.
Sepsis Six outcomes
| Sepsis Six outcomes | Audit year | Appropriately managed, n (%) | p-value |
|---|---|---|---|
| All Sepsis Six completed within 1 hour | 2014 | 1 (1) | <0.0001 |
| 2015 | 36 (67) | ||
| All Sepsis Six completed | 2014 | 1 (1) | <0.0001 |
| 2015 | 46 (85) | ||
| Antibiotics given within 1 hour | 2014 | 6 (9) | <0.0001 |
| 2015 | 44 (81) | ||
| Fluids given within 1 hour | 2014 | 6 (9) | <0.0001 |
| 2015 | 40 (74) | ||
| Oxygen given within 1 hour | 2014 | 39 (58) | <0.0001 |
| 2015 | 53 (98) | ||
| Blood cultures taken within 1 hour | 2014 | 45 (67) | <0.0001 |
| 2015 | 54 (100) | ||
| Blood lactate checked within 1 hour | 2014 | 39 (58) | <0.0001 |
| 2015 | 50 (93) | ||
| Urine output measured within 1 hour | 2014 | 45 (67) | 0.0175 |
| 2015 | 47 (87) |
For 2014, n=67 and for 2015, n=54. Two-tailed Fisher's exact test was used to calculate statistical significance.
Table 3.
Mortality and morbidity outcomes
| Morbidity and mortality outcomes | Audit year | p-value | |
|---|---|---|---|
| 2014 | 2015 | ||
| ITU admissions, n (%) | 13 (19) | 4 (7) | 0.0695 |
| 0.0498 | |||
| Deaths, n (%) | 4 (6) | 0 (0) | 0.1274 |
| LOS, days | 10 | 7 | <0.0001 |
For 2014, n=67 and for 2015, n=54.
ITU = intensive care unit; LOS = length of stay
With the help of the clinical coding department, notes of all the patients were reviewed again later, when they were either discharged or had died, and at this stage the length of hospital stay was determined and whether they were admitted to ITU. This information was also collated as previously, using the same methods and statistical analyses. However, the unpaired t test was used to calculate statistical significance between the mean length of hospital stay in 2014 and in 2015 (Table 3).10
A p-value of less than 0.05 was considered statistically significant.10
Results
The audit included 67 patients in 2014 and 54 patients in 2015. As presented in Table 2, the initial audit demonstrated that only 1% of appropriate patients (n=1) had been managed according to the existing guidelines, whereas, the re-audit emphatically showed a significant improvement with 85% of eligible subjects (n=46) having all of the Sepsis Six criteria met (p<0.0001), and 67% (n=36) adhering strictly to the protocol (p<0.0001).
In the 2014 audit, a mere 9% of patients (n=6) were managed appropriately – with administration of antibiotics and fluids – within the ‘golden hour’; however, there was a significant improvement to 81% (n=44, p<0.0001) and 74% (n=40, p<0.0001), respectively, on re-audit in 2015. Only 58% of patients (n=39) had both oxygen given and blood lactate levels checked appropriately on initial audit, which improved significantly to 98% (n=53, p<0.0001) and 93% (n=50, p<0.0001), respectively, on re-audit. In the 2014 audit, 67% of patients (n=45) had both blood cultures taken and urine output measured appropriately within the hour, which, once again, showed a significant improvement to 100% (n=54, p<0.0001) and 87% (n=47, p=0.0175), respectively, on re-audit.
On initial audit, many of the patients were found to have continued high lactate levels over time, due to either fluids not being given on time or being given too slowly. This prompted admission to the ITU. 19% of patients (n=13) were admitted to ITU on initial audit, which improved to 7% (n=4) on re-audit (two-tailed Fisher's exact test p=0.0695, one-tailed Fisher's exact test p=0.0498). The number of deaths was reduced from 6% (n=4) on initial audit to no deaths on re-audit (p=0.1274). Length of hospital stay was reduced, from an initial audit average of 10 days, to 7 days on re-audit (p<0.0001) (Table 3).
Discussion
Sepsis is one of the leading causes of preventable morbidity and mortality in hospitals today.11,12 However, we have demonstrated that simple measures, if consistently performed, save lives.
Our methods during presentation included assessment of prior knowledge by using questionnaires and reviewing these for pre- and post-improvement by using the same questionnaires after the presentation.13 The audit findings emphatically demonstrate improvements as a result of using visual, auditory and readable aids.14 The ‘sepsis’ tab, as mentioned, directed stepwise management of sepsis, prompting immediate diagnosis and initiation of the protocol (Fig 1).15
Our work has undoubtedly enhanced the recognition and management of severe sepsis using the Sepsis Six bundle. This has led to considerable reduction in cost to the NHS, particularly in length of stay – as demonstrated in the re-audit.
Based on the one-tailed p-value, there was a significant decrease in the number of ITU admissions and an overall decrease in morbidity and mortality, with no deaths on re-audit. This is likely to be related to the improved outcome on fluid resuscitation through enhanced lactate and urine output measurements.
Following dissemination of our data to the hospital, the emergency department staff have devised their own protocol, which has been shown to significantly improve multidisciplinary assessment of patients with severe sepsis and initiating the Sepsis Six (S1).
Conclusion
There was significant improvement and complete change in management of severe sepsis, resulting in trust-wide updated protocols and teamwork practice to guide timely initiation of the Sepsis Six. This led to a significant decrease in length of hospital stay, and a decrease in morbidity and mortality.
Food for thought
We hope this will be an eye opener to many national and international medical organisations. We have used multiple modality tools to present the key to success in multidisciplinary management of severe sepsis using the Sepsis Six, and making it as simple a task as checking vital observations to prompting action.
Supplementary material
Additional supplementary material may be found in theonline version of this article at www.clinmed.rcpjournal.org/:
S1 – Emergency department sepsis screening tool.
Author contributions
MA and GR have been involved in data collection. AB has been involved in data collection, performing statistical analysis and wrote the manuscript. AM had overview of the whole quality improvement project and edited the submitted manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgements
The authors would like to acknowledge Dr Lee and Dr Touma for their contribution in making the ED sepsis screening tool (adapted from Wexham Park Hospital local trust guidelines).
This quality improvement project has been nominated for the Lancet Research Prize and was awarded the Royal College of Physicians Research Poster Prize at the Royal College of Physicians Medicine 2016 conference.
References
- 1.Rivers E. Nguyen B. Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 2.Daniels R. Surviving the first hours in sepsis: getting the basics right (an intensivist's perspective) J Antimicrob Chemother. 2011;66(suppl ii):11–23. doi: 10.1093/jac/dkq515. [DOI] [PubMed] [Google Scholar]
- 3.Vincent JL. Sakr Y. Sprung CL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–53. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 4.Sepsis Alliance Definition of sepsis. San Diego:: Sepsis Alliance; Available online at www.sepsis.org/sepsis/definition/ [Accessed 1 July 2016]. [Google Scholar]
- 5.Levy MM. Fink MP. Marshall JC, et al. SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Int Care Med. 2003;29:530–8. doi: 10.1007/s00134-003-1662-x. 2001. [DOI] [PubMed] [Google Scholar]
- 6.Royal College of Physicians Acute care toolkit 9: Sepsis. London:: RCP; 2014. [Google Scholar]
- 7.Trzeciak S. Chansky ME. Dellinger PR, et al. Operationalising the use of serum lactate measurement for identifying high risk of death in a clinical practice algorithm for suspected severe sepsis. Acad Emerg Med. 2006;13:150–1. [Google Scholar]
- 8.Kumar A. Roberts D. Wood KE, et al. Duration of hypotension prior to initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 9.Daniels R. Nutbeam I. McNamara G, et al. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J. 2011;28:507–12. doi: 10.1136/emj.2010.095067. [DOI] [PubMed] [Google Scholar]
- 10.Peacock JL. Peacock PJ. Oxford Handbook of Medical Statistics. Oxford:: Oxford University Press; 2011. [Google Scholar]
- 11.Daniels R. Sepsis/Severe Sepsis Screening Tool. Retrieved Survive SEPSIS. 2007 www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/PHW_Sepsis_Screening_Leaflet_11.pdf. [Accessed 1 July 2016]. [Google Scholar]
- 12.NHS England Improving outcomes for patients with sepsis: a cross-system action plan. London:: NHS England; 2015. http://www.england.nhs.uk/wp-content/uploads/2013/12/spesis-brief.pdf . [Google Scholar]
- 13.Kaufman DM. Applying educational theory in practice. BMJ. 2003;326:213–6. doi: 10.1136/bmj.326.7382.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleming N. Bronwell C. How do I learn best? A student’s guide to improved learning. VARK; 2013. [Google Scholar]
- 15.Virtual College What is e-learning? www.virtual-college.co.uk/elearning/elearning.aspx. [Accessed 1 July 2016]. [Google Scholar]


