Introduction
Acrokeratosis paraneoplastica, also known as Bazex syndrome, is a paraneoplastic disorder of the skin characterized by an acral distribution of erythematous psoriasiform plaques that may also involve the nose and ears.1 Bazex syndrome typically affects patients older than 40 and is most commonly associated with squamous cell carcinomas of the upper aerodigestive tract. Bazex syndrome has also been reported in association with adenocarcinoma, genitourinary tumors, multiple myeloma, and lymphoma.2, 3 We report a case of Bazex syndrome correlating with peripheral T-cell lymphoma, an association that to the best of our knowledge has been identified only once before.4
Case report
A 56-year-old African-American man presented to the clinic with a 6-year history of unremitting pruritus overlying the arms, legs, neck, face, and dorsal hands and feet. Previous attempts to alleviate his symptoms with petroleum jelly and triamcinolone ointment had proven unsuccessful. Examination found erythematous papules coalescing into scaly plaques on the arms, legs, face, and neck with markedly lichenified plaques on the palmoplantar surfaces. His trunk was spared, and he exhibited no lymphadenopathy or hepatosplenomegaly. A short course of betamethasone and triamcinolone ointment was prescribed, and he was instructed to follow-up in 2 months.
Upon returning to clinic, he reported minimal improvement and was noted to have had an unintentional 10-pound weight loss. A punch biopsy of the right forearm found a spongiotic mixed dermatitis with eosinophils (Fig 1). Because of clinical concern for mycosis fungoides, T-cell gene rearrangement analysis was conducted but did not yield definitive evidence of clonality. Topical steroids were continued, and the patient was referred for patch testing, which also returned negative.
Fig 1.
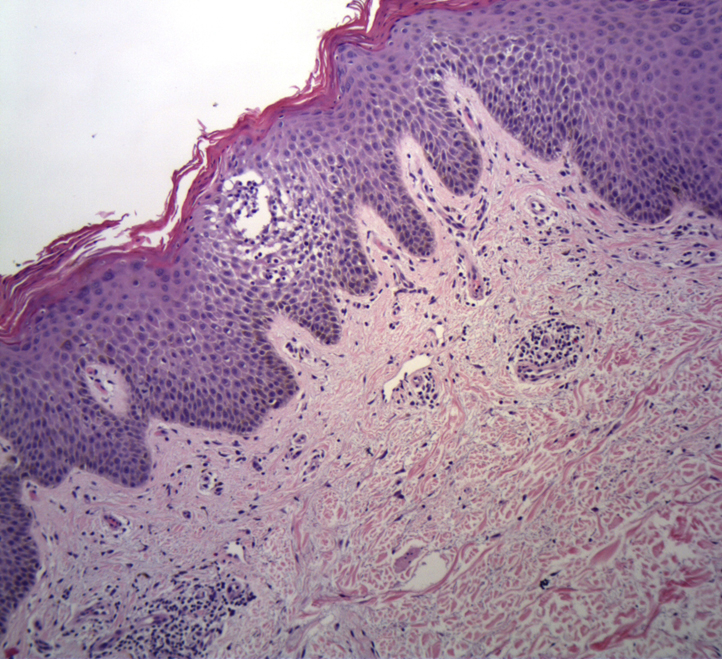
Hematoxylin-eosin stain of right forearm punch biopsy taken 7 months before hospitalization, showing spongiosis and a mixed dermal infiltrate. (Original magnification: ×10.)
Over the next several months, his symptoms continued to decline. In addition to topical steroids, serial courses of methotrexate and cyclosporine were given without improvement. On follow-up 9 months out from his initial presentation, examination found severe fissuring and scaling of the plantar feet, purulent drainage from the toes and right ear, and massive firm adenopathy of the cervical and inguinal nodes (Fig 2, A, B, and C). The patient was subsequently admitted to the hospital for intravenous antibiotics and further workup.
Fig 2.
Clinical image taken at time of hospitalization. A, Hyperkeratotic plaques and fissuring of left palm. B, Hyperkeratotic plaques and fissuring of right plantar foot. C, Hyperpigmented plaque over right ear.
An excisional biopsy of the right inguinal lymph node was taken at the time of admission to the hospital and found a peripheral T-cell lymphoma positive for CD2, CD3, CD5, CD7, and dim CD8 and T-cell receptor-α/β. Bone marrow biopsy found an aberrant T-cell population of similar immunophenotype. Based on these results, a diagnosis of peripheral T-cell lymphoma not otherwise specified was made. His skin symptoms were attributed to a paraneoplastic disorder, most consistent with Bazex syndrome. After treatment with topical steroids under occlusion and systemic antibiotics, the patient was discharged with arrangements to start outpatient chemotherapy.
At his next dermatology follow-up visit, shortly after his first chemotherapy treatment, the patient exhibited mild improvement to the lesions on his palms but not those on his soles. He did not show up to his next appointment, and the hospital was later notified that he had died.
Discussion
The diagnosis of Bazex syndrome can be clinically challenging because of the frequent onset of cutaneous lesions before a malignancy is identified, the lack of specificity on histopathologic examination, and the overlap with more common diseases such as dyshidrotic eczema or psoriasis. A recent systematic review of Bazex syndrome reported that in roughly 50% of cases, the skin manifestations preceded the diagnosis of malignancy.3 An earlier review estimated this finding to be as high as 75%.2 Histopathology is highly variable but in many reports includes hyperkeratosis, acanthosis, parakeratosis, spongiosis, and a mixed dermal infiltrate of leukocytes, neutrophils, eosinophils, or mononuclear cells.3 Treatment of Bazex syndrome requires treatment of the underlying malignancy. In fact, a lack of response to targeted dermatologic therapies such as topical corticosteroids provides support for the diagnosis.5 Given this constellation of nonspecific findings, a high level of clinical suspicion is necessary when making a diagnosis of Bazex syndrome. Furthermore, if Bazex syndrome is suspected, workup for malignancy should be conducted with particular attention paid to the aerodigestive tract.6
The patient in this case was initially suspected to have palmoplantar eczema. The lack of clinical response to topical steroids, methotrexate, and cyclosporine were clues that this diagnosis was incorrect. An acquired palmoplantar keratoderma syndrome was also less likely given that the lesions were not only on his palms and soles but also included his ears, a more specific feature associated with Bazex.7 Finally, despite initial concern for mycosis fungoides, the lack of T-cell receptor clonality on skin biopsy, the presence of spongiosis, and the specific distribution of plaques were inconsistent with this.
This case represents only the second reported instance of Bazex syndrome associated with peripheral T-cell lymphoma and highlights the key clinical features that can direct clinicians in making this diagnosis.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Bolognia J.L., Jorizzo J.L., Schaffer J.V. Elsevier Health Sciences; London: 2012. Dermatology E-Book. [Google Scholar]
- 2.Bolognia J.L., Brewer Y.P., Cooper D.L. Bazex syndrome (acrokeratosis paraneoplastica). An analytic review. Medicine. 1991;70(4):269–280. doi: 10.1097/00005792-199107000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Räßler F., Goetze S., Elsner P. Acrokeratosis paraneoplastica (Bazex syndrome) - a systematic review on risk factors, diagnosis, prognosis and management. J Eur Acad Dermatol Venereol. 2017;31(4):1119–1136. doi: 10.1111/jdv.14199. [DOI] [PubMed] [Google Scholar]
- 4.Lin Y.C., Chu C.Y., Chiu H.C. Acrokeratosis paraneoplastica (Bazex's syndrome): unusual association with a peripheral T-cell lymphoma. Acta Derm Venereol. 2001;81(6):440–441. doi: 10.1080/000155501317208471. [DOI] [PubMed] [Google Scholar]
- 5.Karabulut A.A.A., Sahin S., Sahin M., Ekşioğlu M., Ustün H. Paraneoplastic acrokeratosis of Bazex (Bazex's syndrome): report of a female case associated with cholangiocarcinoma and review of the published work. J Dermatol. 2006;33(12):850–854. doi: 10.1111/j.1346-8138.2006.00194.x. [DOI] [PubMed] [Google Scholar]
- 6.Poligone B., Christensen S.R., Lazova R., Heald P.W. Bazex syndrome (acrokeratosis paraneoplastica) Lancet. 2007;369(9560):530. doi: 10.1016/S0140-6736(07)60240-2. [DOI] [PubMed] [Google Scholar]
- 7.Kleyn C.E., Lai-Cheong J.E., Bell H.K. Cutaneous manifestations of internal malignancy: diagnosis and management. Am J Clin Dermatol. 2006;7(2):71–84. doi: 10.2165/00128071-200607020-00001. [DOI] [PubMed] [Google Scholar]



