Abstract
Data suggest that disability prevalence among mid-aged populations is increasing in recent years; current prevalence estimates for mid-aged adults range from 20 to 40 %. The World Health Organization’s International Classification of Functioning (ICF) has provided a multi-dimensional biopsychosocial model to understand disability that is highly relevant to mid-aged populations. Under the ICF framework, mid-aged women experience high levels of work, non-work, and mobility-associated disability but very little difficulty with self care. Despite the high prevalence, evidence suggests that there is a large proportion of non-chronic disability and that mid-aged women can both worsen and improve their functioning. Thus, the mid-life period may represent a critical window during which interventions to improve disability may be most efficacious for the improvement of current and future functioning. Interventions that are initiated during the mid-life are highly relevant as a strategy to reduce disability during this life stage and prevent or forestall the onset of late life disability. Targets for intervention include improvement of depressive symptoms and increasing physical activity levels, both of which have shown to be efficacious in older populations and are correlates of mid-life functioning and disability.
Keywords: Women, Mid-life, Middle age, Physical functioning, Functional limitations, Disability
Introduction
Our world is in the midst of an epidemiologic transition whereby the burden of non-communicable diseases has now surpassed communicable diseases and injury as the leading cause of death and illness worldwide [1]. Globally, the rise in prevalence of obesity and adverse health behaviors including smoking, poor diet, and physical inactivity in concert with the overall rise in life expectancy has led to the exponential increase in chronic disease prevalence and multi-morbidity. Individuals are being diagnosed with chronic conditions earlier and have a greater number and more severe chronic conditions than ever before [2, 3]. In the United States, the average number of chronic conditions among midlife adults is increasing; the number of midlife adults with three or more chronic conditions increased by 9.7 % between 1996 and 2005 [4]. Thus, the burden of chronic disease and its effects on functioning and health is the major public health challenge of the 21st century.
The increase in chronic disease prevalence and severity is concerning because chronic diseases are the leading cause of disability in the United States [5] and globally [6], so it is expected that there will be a concomitant rise in disability. Current estimates from the World Health Survey and the Global Burden of Disease indicate that more than 1 billion people in the world (based upon 2010 world population estimates) live with some form of disability [7]. While different methodologies in the World Health Study and the Global Burden of Disease suggest slightly different prevalence estimates for adult disability, 15.6 and 19.4 %, respectively [7], both suggest that the global burden of disability is substantial. Similarly, in the United States, based upon data from the Survey of Income and Program Participation (SIPP), 18.7 % of non-institutionalized persons are living with a disability [8]. This number is expected to rise given the aging of the population [9, 10] and the high burden of chronic conditions including ischemic heart disease, stroke and HIV/AIDS [11].
Globally, women represent a rapidly growing proportion of the aging population given the projected increase in the life expectancy gender gap (reaching a gap of 4.4 years by 2050) in less developed countries [12]. The focus on contextual factors and their relevance for disability may be particularly important for the initiation of disability among women. The reported Male–female Health-Survival Paradox, whereby men have higher death rates but women fare worse in terms of disability and functioning [13–15] demonstrate that women are a particularly vulnerable group for disability problems as they age. The root causes of this paradox are unknown, but may include greater total disability burden among older women as compared to men [15], decreased likelihood of mortality among women with moderate to severe disability as compared to similarly-disabled men [15] or sex and gender differences in biological, behavioral and social factors across the lifespan. For example, research demonstrates that socioeconomic disadvantage is more strongly associated with disability risk among women as compared to men [16], and sex differences in body composition (higher total and subcutaneous fat mass and lower lean mass, muscle area and muscle density) translate to worse physical performance among women [17, 18] than among men. Among elderly populations, women experience more severe disability than men but it has been hypothesized that the combined impact of various social disadvantages such as lower income, less education, and higher prevalence of widowhood among older women may make them at greater risk for disability [19]. The male-to-female advantage in functioning is not, however, limited to elderly populations. Among mid-aged adults, women have 40 % lower levels of strength [20, 21], 20 % poorer balance times [20] and nearly twice the prevalence of self-reported difficulties with stair climbing activities [20] as compared to age-matched men. Further, women experience a more rapid decline in strength commencing in mid-life than do men; accelerations in strength loss begin between ages 40 and 55 in women whereas the loss of strength in men is linear across the lifespan [22–24]. The timing of this loss in strength has been noted to coincide with the timing of the menopausal transition [24–26] and some studies suggest that strength is preserved following menopause among women using exogenous hormone therapy [24, 25]. In addition to strength changes following menopause, data from cross-sectional studies show that postmenopausal women have 3.5 times higher odds of reporting substantial physical functioning limitations [26] and 17 % poorer balance times as compared to premenopausal women [27]. Given differences in functioning among pre- and post-menopausal women as well as among mid-aged men and women it has been hypothesized that ovarian function and the consequent decrease in estrogen levels during the menopausal transition may be associated with poor functioning.
What is disability and how do we measure it?
The traditional model of disability and the disablement process was first described by Nagi [28] and then updated by Verbrugge & Jette [29]. As shown in Fig. 1, this traditional disablement model contributed substantially to our understanding by conceptualizing disability as a process during which one may experience impairments and limitations before reaching a disabled state. However, utilization of this model was limited by the focus on medical pathologies as the initiating factor in the cascade toward disablement. Although underlying medical conditions are known to be a risk factor for disability, a growing appreciation for the complexities underlying disability including the contextual and environmental factors prompted an international collaboration to revise and restructure this model.
Fig. 1.
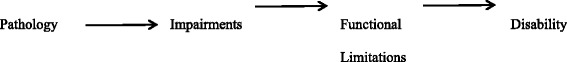
The disablement process by Verbrugge & Jette [17], adapted from Nagi [16]
In 2001, the World Health Organization (WHO) officially endorsed the International Classification of Functioning (ICF), Disability and Health as the prevailing framework for measuring health and disability within individuals and populations. The ICF conceptualizes disability as a general construct not only defined by underlying pathology but by the interaction of individuals with their environment and the mediation of that relationship by underlying contextual factors including genetic, biological, behavioral, social and economic factors. This biopsychosocial model, shown in Fig. 2, is structured on three levels of functioning: body functions and structure, activity, and participation. Importantly, disability is not a condition of an individual but one that occurs for a given individual in certain contexts. Unlike earlier disability models, the ICF model includes both disease-related and non-disease-related disability, the latter of which may be particularly relevant among middle-aged populations who may or may not yet have manifested overt disease. Scientific interest in functional limitations and disability as health outcomes are motivated by the fact that declines in physical performance and the presence of disability are associated with increased risk of death, morbidity, and reduced quality of life [12, 16, 30]. Preservation of functioning and prevention of disability is critical so that individuals can maintain independence and remain autonomous as they age.
Fig. 2.
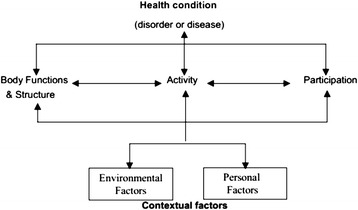
International Classification of Functioning disability framework
Disability is an increasingly relevant mid-life health issue
While there has been a large focus on the impending “silver tsunami” given the known relationship between age and disability [8], evidence from five national studies suggests that activities of daily living (ADL) or instrumental activities of daily living (IADL) disability rates among elderly individuals have remained constant in recent years [31] and even show 0.61–0.90 % improvement per year in ADLs and 0.3–1.41 % improvement per year in IADLs among the oldest old (85+ years) [31].
Among mid-aged adults, however, an emerging body of literature suggests a remarkably high prevalence of disability during this life stage. The prevalence of mid-life disability has been reported to range from 20 to 40 % [5, 11, 32, 33] and most common types of disability are mobility-based [5, 32]. Most concerning, however, are the growing number of studies reporting temporal increases in disability among middle-aged populations, suggesting that this problem is becoming more exacerbated. Odds of ADL, IADL, and mobility disability were 1.3–1.7 times higher among 60–64 year olds in the 1999–2004 National Health and Nutrition Examination Survey (NHANES) as compared to the 1988–1994 NHANES [34], independent of obesity and chronic health conditions. Similarly, among 50–64 year olds in the National Health Interview Survey (NHIS), there was a 6.8–12.1 % increase in the number of individuals reporting difficulty with lower extremity mobility including difficulty stooping, standing for 2 h, walking a quarter-mile, and climbing ten steps without resting from the 1997–99 versus 2005–07 data collection cycles [33]. Among 40–64 years old in NHIS, the odds for physical functioning limitations, ADLs and IADLs increased annually by 0.9, 0.9, and 2.7 %, respectively; the increase in ADLs was independent of increases in obesity and was greater for women as compared to men [35]. In the Health and Retirement Survey (HRS), 15 % of adults aged 55–64 years in 2000 reported having difficulty with ADLs and there was a 0.1–0.2 percentage point increase per year [31]. However, the prevalence of ADL or IADL-assessed disability in mid-aged populations is relatively quite low as compared to older adults, and so more evidence is needed to confirm temporal trends and individual trajectories in disability.
With respect to physical functioning, the mid-life period is well accepted as a critical window for the onset of self-reported functional limitations [26, 36, 37] and diseases which ultimately lead to poor functioning and disability. In the Study of Women's Health Across the Nation (SWAN), a longitudinal study of midlife women, nearly one third of women (aged 45–57 years) reported moderate functional limitations and 11 % reported severe limitations based upon the SF-36 physical functioning questionnaire [26]. Similarly, in a British cohort of middle-aged adults, the prevalence of upper (difficulty gripping or reaching) and lower (difficulty walking or stair climbing) body limitations was 21–28 %, respectively [37]; the majority of these limitations began during the mid-life. Findings from NHIS show that deficits in functioning, defined as restricted activity resulting from illness, injury, or impairment begin during the mid-life [38] and that the most common conditions causing the need for help with ADLs or IADLs later in life, including back or neck problems, arthritis or rheumatism, diabetes, depression, anxiety, or emotional problems, hypertension, and nervous system conditions most commonly onset between 30 and 49 years of age [33].
Issues of functional limitations and disability are particularly salient among mid-aged individuals who are still in the work force and often caring for both dependent children and grandchildren as well as aging parents. Data from SIPP suggest that more than 10 % of mid-aged adults reported having limitation in their ability to work at a job [5]. Lack of employment during the midlife years may further compound health status and quality of life, as one’s health insurance and ability to pay for medical care is often tightly linked to their employment.
Challenges to studying disability
While there is substantial interest in measuring and understanding functional limitations and disability, efforts are complicated by the multi-faceted nature of disability and the substantial diversity in the assessment methods used. To illustrate this point, please refer to Table 1 which was summarizes the variability in disability prevalence estimates and definitions used among studies reporting on mid-life disability. There is no consensus in the field as to how disability should be assessed or defined, and several different questionnaire and performance-based assessment tools are in operation, thereby resulting in highly variable prevalence estimates for disability. For example, two studies reporting disability rates among mid-aged women in Finland report wildly different estimates (7.8 % vs. 25.8 %) when using different definitions of disability [39, 40].
Table 1.
Midlife disability prevalence and disability definitions
| Reference | Study, year, geographic location | Midlife sample | Disability definition | Disability prevalence (95 % CI) |
|---|---|---|---|---|
| United States studies, national samples | ||||
| Altman & Gulley 2009 [45] | Joint Canada/United States Survey of Health, 2002–2003, United States and Canada national samples | 40–64 years | Disability in 4 question domains: Restriction of Activities Screener (reduction of activities at home, school, work); Health Utilities Index (functional abilities including vision, hearing, speech, mobility, dexterity, emotional well being, cognition, pain); Activity and Participation Screener (restriction caused by physical, mental or emotional problem); and Physical Functioning Limitation | |
| Men & women | • 40–49 years, Canada | 19.82 % (14.16, 25.48) | ||
| • 50–64 years, Canada | 25.32 % (19.17, 31.47) | |||
| • 40–49 years, United States | 16.80 % (12.47, 21.13) | |||
| • 50–64 years, United States | 28.59 % (23.67, 33.51) | |||
| Mitra et al. 2009 [46] | Medical Expenditure Panel Survey, 2004, United States national sample | 40–61 years | At least one of the following: limitations in work, housework, or school; walking limitations; cognitive limitation; limitations in seeing or hearing | |
| Men and women | • 40–49 years | 29.7 % | ||
| • 50–61 years | 45.4 % | |||
| Hottman et al. 2005 [5] | Survey of Income and Program Participation, 2005, United States national sample | 45–64 years | At least one of the following: (women only) | 25.9 % |
| Men & women | • Use of an assistive aid | 4.6 % (4.2, 5.0) | ||
| • Difficulty performing ADLs | 4.1 % (3.7, 4.5) | |||
| • Difficulty performing IADLs | 6.0 % (5.5, 6.5) | |||
| • Difficulty performing specified functional activities | 19.4 % (18.6, 20.2) | |||
| • Reported of selected impairments | 6.9 % (6.4, 7.4) | |||
| • Limitation in ability to work around house | 10.7 % (10.1, 11.3) | |||
| • Limitation in ability to work at Job/business | 11.3 % (10.7, 11.9) | |||
| Martin et al. 2010 [33] | National Health Interview Survey, 2005–2007, United States national sample | 50–64 years | Difficulty with physical functions due to a health problem | 42.0 % |
| Men & women | • Needing help with IADLs | 6.7 % | ||
| • Needing help with ADLs | 6.0 % | |||
| Zhao et al. 2009 [47] | Behavioral Risk Factor Surveillance System, 2005, United States national sample | 50–65 years | Self-reported limitations in participation in activities because of physical, mental, or emotional problems or whether health problems required use of special equipment | |
| Men & women | • 50–54 years | 22.9 % (21.3, 24.5) | ||
| • 55–59 years | 28.8 % (27.8, 29.8) | |||
| • 60–65 years | 28.8 % (27.8, 29.8) | |||
| United States studies, local samples | ||||
| Khoury et al. 2013 [69] | Female Medicaid beneficiaries, 2001–2005, Florida | 36–64 years | Presence of at least one physically disabling conditions but no use of a mobility assistive device | |
| Women | • 36–45 years | 35.79 % | ||
| • 46–55 years | 47.22 % | |||
| • 56–64 years | 53.30 % | |||
| Presence of at least one physically disabling conditions and use of a mobility assistive device | ||||
| • 36–45 years | 2.92 % | |||
| • 46–55 years | 5.59 % | |||
| • 56–64 years | 9.17 % | |||
| Brown et al. 2014 [41] | Patients admitted to San Francisco General Hospital, 2010–2011, San Francisco, California | 55–59 years | Needing help with at least one ADL 2 weeks before hospital admission | 28.9 % |
| Men & women | • Needing help with bathing | 21.1 % | ||
| • Needing help with dressing | 20.5 % | |||
| • Needing help with transferring | 14.5 % | |||
| • Needing help with eating | 9.0 % | |||
| • Needing help with toileting | 9.6 % | |||
| Needing help with at least 2 IADLs 2 weeks before hospital admission | 36.1 % | |||
| • Needing help with shopping | 32.5 % | |||
| • Needing help with light housework | 30.6 % | |||
| • Needing help with meal preparation | 30.1 % | |||
| • Needing help with transportation | 21.1 % | |||
| • Needing help with medication management | 20.7 % | |||
| • Needing help with money management | 16.9 % | |||
| • Needing help with using the telephone | 7.2 % | |||
| Mann et al. 2015 [48] | Behavioral Risk Factor Surveillance System (BRFSS), 2011, South Carolina | 45–64 years | Affirmative response to standard BRFSS disability questions: | |
| Men & women | Self-reported limitation in “activities because of physical, mental, or emotional problems” | |||
| Or | ||||
| Self-reported health problem that requires use of special equipment such as a cane, wheelchair, special bed, or special telephone. | ||||
| • 45–54 years | 22.1 % (20.0, 24.3) | |||
| • 55–64 years | 23.3 % (21.4, 25.2) | |||
| Karvonen-Gutierrez & Ylitalo 2013 [32] | Michigan Study of Women’s Health Across the Nation, 2011, Michigan | 55.9–67.7 years | 36-item World Health Organization Disability Assessment Schedule, severe-extreme disability: | |
| Women only | • Global score | 5.05 % (2.84, 7.26) | ||
| • Understanding and communicating | 5.05 % (2.84, 7.23) | |||
| • Getting around | 19.31 % (15.41, 23.41) | |||
| • Self-care | 4.26 % (2.22, 6.30) | |||
| • Getting along with people | 6.12 % (3.70, 8.54) | |||
| • Engaging in life activities, non-work | 43.16 % (35.07, 51.25) | |||
| • Engaging in life activities, work | 8.62 % (5.00, 12.23) | |||
| • Participation in society | 8.78 % (3.92, 11.64) | |||
| Arterburn et al. 2012 [52] | Group Health Plan enrollees, Washington | 40–65 years | Modified World Health Organization Disability Assessment Schedule, any disability: | |
| Women only | • Global score | Not reported | ||
| • Understanding and communicating | 26 % | |||
| • Getting around | 27 % | |||
| • Self-care | 7 % | |||
| • Getting along with people | 17 % | |||
| • Engaging in life activities, non-work | 46 % | |||
| • Engaging in life activities, work | 45 % | |||
| • Participation in society | 24 % | |||
| International studies | ||||
| Hosseinpoor et al. 2012 [16] | World Health Survey, 2002–2004, 57 countries | 50–59 years | World Health Organization Report on Disability definition, based upon Item Response Theory model using data from questions in multiple domains. | |
| Men & women | • 50–54 year old women | 27.3 % (25.1, 29.5) | ||
| • 55–59 year old women | 30.5 % (28.0, 33.0) | |||
| Europe | ||||
| Kattainen et al. 2004 [39] | Finland Health 2000 Survey, 2000–2001, Finland | 45–64 years | Blindness or being unable to perform without help or having marked difficulty at least one of | 7.8 % |
| Women | the following: moving about in the house, getting in/out of bed, dressing, carrying a 5-kg shopping bag, walking 500 m without rest, climbing a flight of stairs without rest, managing grocery shopping | |||
| Krishnan et al. 2004 [40] | Cross-sectional study in Central Finland District, 2000, Finland | 36–65 | Health Assessment Questionnaire (HAQ) disability index score >0. HAQ assesses difficulty with performing activities in 8 functional categories: dressing/grooming, arising, eating, walking, hygiene, reach, grip, and common daily activities. | |
| Women | • 36–40 years | 14.7 % (7.9, 21.4) | ||
| • 41–45 years | 17.4 % (10.4, 24.4) | |||
| • 46–50 years | 25.0 % (17.4, 32.6) | |||
| • 51–55 years | 25.6 % (17.7, 33.5) | |||
| • 56–60 years | 36.7 % (27.0, 46.4) | |||
| • 61–65 years | 33.1 % (24.4, 41.7) | |||
| Klijs et al. 2011 [81] | Dutch PLOS-survey (Permanent Onderzoek Leefsituatie), 2001–2007, the Netherlands | 55–59 years | Major difficulty doing or only able to do with help at least one of the following: walk up and down the stairs, walk outside, enter/leave the house, sit down/get up from a chair, move around on the same floor, get in/out of bed, eat/drink, get dressed/undressed, wash face/hands, wash completely | 6 % |
| Women | ||||
| Almazan-Isla et al. 2014 [60] | Residents from Cinco Villas, Spain, 2008–2009, Spain | 50–59 years | 36-item World Health Organization Disability Assessment Schedule, severe-extreme disability, women only | |
| Men & women | • Global score | 1.27 % | ||
| • Understanding and communicating | 1.27 % | |||
| • Getting around | 8.28 % | |||
| • Self-care | 2.55 % | |||
| • Getting along with people | 1.27 % | |||
| • Engaging in life activities, non-work | 12.74 % | |||
| • Engaging in life activities, work | 4.46 % | |||
| • Participation in society | 6.00 % | |||
| Africa | ||||
| Miszkurka et al. 2012 [54] | World Health Organization World Health Study, 2002–2003, Burkina Faso, Mali, and Senegal | 35–64 years | Mobility disability, defined as self-reported mild, moderate, severe or extreme difficulty or unable to move around. | |
| Men and women | • 35–44 years, Burkina Faso, women | 21 % (16, 28) | ||
| • 35–44 years, Mali, women | 22 % (19, 26) | |||
| • 35–44 years, Senegal, women | 36 % (28, 44) | |||
| • 45–54 years, Burkina Faso, women | 25 % (19, 32) | |||
| • 45–54 years, Mali, women | 31 % (24, 39) | |||
| • 45–54 years, Senegal, women | 41 % (23, 63) | |||
| • 55–64 years, Burkina Faso, women | 52 % (40, 64) | |||
| • 55–64 years, Mali, women | 48 % (38, 58) | |||
| • 55–64 years, Senegal, women | 56 % (38, 72) | |||
| Payne et al. 2013 [55] | Malawi Longitudinal Study of Families and Health, 2010, Malawi | 45–64 years | Having any health problem that limits ability to carry out culturally-relevant moderate activities or strenuous activities. | |
| Men & women | • Moderately disabled (‘somewhat limited’ in either moderate or strenuous activities) | 22.4 % | ||
| • Severely disabled (‘limited a lot’ in either moderate or strenuous activities) | 5.3 % | |||
| Wandera et al. 2014 [56] | Uganda National Household Survey, 2010, Uganda | 50–59 years | Having a lot of difficulty or being unable to perform at least one of the following OR having some difficulty with at least two of the following: difficulty seeing, even if wearing glasses; difficulty hearing, even if wearing a hearing aid; difficulty walking or climbing steps; difficulty remembering or concentrating; difficulty washing all over or dressing, feeding and toileting; difficulty communicating because of a physical, mental or emotional health condition. | 24.8 % |
| Women | ||||
| Asia | ||||
| Zheng et al. 2011 [57] | China National Survey, 2006, China | 45–64 years | Doctor-diagnosed disability following positive screen for self-reported visual, hearing, speech, physical, intellectual or mental disability | |
| Men and women | • 45–54 years | 11.0 % | ||
| • 55–64 years | 13.2 % | |||
| Peng et al. 2010 [58] | China National Sample Survey on Disability, 2006 | 35–64 years | Visual, intellectual, mental or physical disability assessed from an impairment-based examination | |
| Women | • 35–39 years | 3.48 % (3.41, 3.55) | ||
| • 40–44 years | 4.18 % (4.10, 4.26) | |||
| • 45–49 years | 5.32 % (5.21, 5.34) | |||
| • 50–54 years | 6.38 % (6.27, 6.49) | |||
| • 55–59 years | 8.77 % (8.62, 8.92) | |||
| • 60–64 years | 12.35 % (12.15, 12.55) | |||
| Hairi et al. 2010 [59] | Alor Gajah Older People Health Survey, 2007–2008, Malaysia | 60–64 years | Level of independence in ADLs. 5-item scale included feeding, dressing, bathing, toileting and transferring. 6-item scale additionally included walking. 10-item scale additionally included grooming, bladder control, bowel control, and stair climbing. | |
| Women | • 10 item ADL dependence | 5.3 % (2.6, 10.1) | ||
| • 6 item ADL dependence | 4.7 % (2.2, 9.4) | |||
| • 5 item ADL dependence | 2.9 % (1.1, 7.9) | |||
As shown in Table 1, many United States studies use either ADLs or IADLs as a disability measure. While these measures are relevant among elderly cohorts, the focus on self-care and ability to live independently may not be adequate to capture early deficits in functioning experienced by younger populations. As evidenced in Table 1, midlife disability prevalence estimates are lowest among studies using ADL or IADL definitions of disability among the general population where the prevalence ranges from 4.1 to 6.7 % [5, 33]. Notably, pre-admission ADL and IADL disability is much higher among a midlife sample of hospitalized patients (29–36 %) [41], suggesting the importance of ADLs and IADLs as a marker of poor health status.
Instead, studies among midlife populations often focus on physical functioning assessment with the assumption that deficits in physical functioning are a predictor of incident disability. The integrated nature of disability, rooted in the interaction between an individual and their environment, cannot be fully measured based upon physical functioning because variability in physical functioning does not full capture the full spectrum of limitations described by the ICF, particularly those that are contextual in nature and particularly relevant to mid-aged cohorts. For example, limitations in physical functioning may not lead to disability given one’s access to and use of adaptive strategies or resources. Further, one may be considered disabled for reasons other than limitations in physical functioning.
When physical functioning is used as a proxy for disability, it is assessed either based upon self-report using a variety of standardized and non-standardized questionnaires or based upon objective, performance-based measures which are often mobility-based. Evidence supports that self-reported and performance-based assessments measure distinct, yet related domains of physical functioning [42–44] but little work has been done to understand the correlation between physical functioning and ICF-based disability among community-based populations. Because physical functioning is only one aspect of an individual’s overall health and functioning, caution should be used when using physical functioning as a proxy for disability.
Many studies have considered self-reported limitation in (work, home, leisure, functioning) activities as a measure of disability. This paradigm is more closely aligned with the ICF framework by consideration of not only functioning but individual context. As shown in Table 1, disability prevalence using definitions based upon activity limitation are higher than those for ADL or IADL disability and increase by 40 % from early- to late-middle age in some [45, 46] but not all [47, 48] studies.
In many countries, work disability claims represent a potentially valuable resource for quantifying and studying the burden of disability among mid-life adults, as they are of working age. While such studies have contributed substantially to the literature and identified the importance of musculoskeletal functioning and mental health as major factors related to work-related disability, there are limitations in utilizing such databases for population research. First, work-related functioning and disability is often assessed in the context of one’s diagnosis and physical health and do not fully capture the impact of the psychosocial domains of disability [49]. Second, in occupational databases, there is often limited individual-level information about important causes, correlates, or consequences of disability such as that which is available from epidemiologic studies. This type of data is critical to identify potential strategies to prevent disability or to alleviate the individual burden of such limitations.
To support assessment of ICF-conceptualized disability, the WHO developed the Disability Assessment Schedule (WHO-DAS). The WHO-DAS questionnaire assesses disability in 6 domains including (a) understanding and communicating, (b) getting around, (c) self-care, (d) getting along with people, (e) engaging in life activities, and (f) participation in society, in addition to a global disability score. It is recognized and promoted as a universal and standardized measure of disability, suitable for national and international comparisons of disability prevalence and determinants across populations and age groups [50, 51]. While the WHO-DAS has been used to examine disability and its correlates in several clinical populations including those with mental health conditions, migraine, Parkinson’s Disease, multiple sclerosis, and traumatic brain injury, only two United States studies have examined WHO-DAS assessed disability in a general population of midlife adults. In the Michigan Study of Women’s Health Across the Nation (SWAN), WHO-DAS assessed disability prevalence was 25 % overall and at least 1 in 5 women reported moderate, severe or extreme problems with the understanding and communicating, getting around, getting along with people, work-related life activities and participation in society domains [32]. Data from a sample of women aged 40–65 years recruited from Group Health, a health insurance and care delivery system in the state of Washington, found that 45 % of women reported disabilities with work and non-work (i.e., household) activities and 27 % reported mobility disability [52]. Unlike studies among elderly cohorts [53] where the prevalence of self-care associated disability is nearly 40 %, only 1 in 10 midlife women in Michigan SWAN or the Group Health cohorts reported disability in the self-care domain [32, 52]. While WHO-DAS disability prevalence estimates (based upon the summary score) are similar to those published in the literature using other definitions of disability [5, 32, 33], the wide variation in domain-specific prevalence [33, 52] demonstrate the strength of the ICF framework in understanding the scope of disability during the mid-life.
Given national differences in medical care, support systems, and acceptability of aging, it is expected that international comparisons of disability prevalence would yield global variability. Unfortunately, cross-national comparisons of disability rates are complicated by variations in assessment method and definitions. As shown in Table 1, most disability work among midlife populations from Africa has focused on mobility disability or activity limitations and so prevalence rates range from 20 to 56 % [54–56]. While disability prevalence in Asia is appreciably lower (3–13 %), definitions are more conservative, based upon doctor diagnosis [57, 58] or ADL dependence [59]. The WHO-DAS has been used to assess disability among mid-life populations in the United States [32, 52] and Spain [60]. Disability prevalence rates were higher in the United States populations as compared to the Spanish population. However, the Spanish population included both men and women whereas the United States studies were among women only.
Differences in disability definitions, assessment strategies, and data sources can make it difficult to make comparisons between different studies, including national surveys, census-based data, and international agreements. Evaluation of trends in disability must be undertaken within longitudinal or panel studies using consistent measures and definitions. When synthesizing the literature and data regarding disability prevalence, incidence, and correlates, and particularly when making comparisons between studies, one must be careful to be cognizant of the constructs used to define disability.
Functioning and disability are dynamic processes
Further complicating the consideration of disability among mid-life populations is that unlike elderly populations, mid-aged individuals may be more likely to experience disability due to acute, non-chronic events. Using data from NHIS of adults ≥18 years of age from 1988 to 2011, Iezzoni et al. [61] found a high proportion of non-chronic disability among respondents, ranging from 1 % for non-chronic social limitation disability to 40 % for non-chronic sensory difficulties. Similarly, data from SWAN has demonstrated that the presence of functional limitations during the mid-life is a highly dynamic process. While most SWAN women maintained their physical functioning level over a two-year period, 6–22 % of women worsened to a poorer level of functioning and 11–30 % of women actually improved their functioning [36]. Older adults also exhibit dynamic patterns of disability transitions, but unlike midlife populations, the vast majority exhibit worsening disability. In the Leiden 85-plus Study, a prospective cohort study of adults age 85 years and older, the prevalence of worsening disability after 5-years was 86 % [62], nearly 4 times greater than that among midlife women in SWAN [36]. Thus, the mid-life may be a highly malleable period during which interventions may be most efficacious because individuals may be more likely to have a propensity for improvement rather than deterioration. Consideration of the dynamic, non-chronic nature of disability status among mid-life populations is critical because most assessments are not designed to capture transient difficulties; estimates suggest that up to 40 % of disability complaints are missed among mid-aged populations because discordance between measurement window and timing of disability [61]. Thus, in mid-aged populations, repeated assessment and data collection is critical to fully understand the burden of disability during this life stage.
Improving disability among mid-life women
Mid-life factors including stress, low social support, decreased social activity, physical inactivity, poor physical functioning, smoking, obesity and diabetes [63–65] are known to predict old age disability. The high prevalence of disability during the mid-life period [5, 11, 32, 33], however, raises the urgent need to intervene to prevent not only future disability but also present disability. The mid-life period is a time of dynamic changes in physical functioning and mid-aged individuals have a high capacity for improvement [36], so there is an imperative need to understand correlates of mid-age disability so that we may develop appropriate and efficacious interventions. Correlates of mid-age disability include obesity [52, 66, 67], depression symptoms [32, 52, 68], economic strain [32] and chronic disease comorbidity [69] and burden [47] including knee osteoarthritis and peripheral neuropathy [32]. Further, incident disability later in life is predicted by mid-life depression [70], increased body mass index [70–72], poor physical functioning performance [68, 73], low levels of physical activity [71, 73] and smoking [72].
As chronic conditions are the leading causes of disability in the United States [5] and globally [6], efforts to prevent disease or reducing symptomatology at earlier ages is one critical strategy to prevent or forestall disability. Many of the conditions which are major correlates of disability emerge or are more bothersome during the mid-life, including osteoarthritis [74], heart trouble [75], low back pain [76] and mental and emotional health problems [77] and are further exacerbated by obesity [78–80]. Among mid-life women, arthritis and back pain have the largest contribution to disability prevalence [81]. Thus, while much work has been done to intervene on disease-specific conditions in older adults as an effort to improve functioning and reduce disability, evidence suggests that interventions starting in midlife or earlier may be most beneficial in reducing disability risk among both midlife and older adults [47].
Individuals may be most amenable to interventions during the mid-life, as evidenced by the success of ergonomic, vocational rehabilitation, and strength training work-place interventions shown to reduce back and upper limb pain-associated work disability [82–84]. However, there has been a dearth of intervention studies among mid-life adults beyond work-place interventions to reduce sick leave or work-related disability. One potential reason for this is the belief that a prohibitively long follow-up period will be needed to observe any effects of an intervention. While recommendations for high-impact interventions for disability reductions among late-life adults have been published [85], no such statement has been issued for mid-life adults. However, given the high prevalence of disability and functional limitations among mid-life populations, this concern is mitigated by the opportunity to improve functioning and disability during the midlife. Given increasing trends in disability prevalence [31] and chronic conditions [2, 3] among mid-life adults, efforts to improve the health and functioning during this life stage is highly needed to appropriately address the unique health needs this population. Additionally, to fully understand how to prevent disability and improve health for late-life individuals, we must identify interventions that, when implemented early, have the ability for sustained benefit as one ages.
Studies among older adults, however, do provide insight to interventions that may be efficacious among mid-life populations. Multi-component exercise interventions [86] including the Lifestyle Interventions and Independence for Elders (LIFE) study [87, 88] and interventions to reduce depression symptoms [89] have showed promising results in reducing incident disability among older adults. Depressive symptoms and decreased physical activity are predictors of mid-life incident disability. This knowledge – the utility of depression and physical activity interventions among older adults and the importance of these factors for predicting mid-life disability suggest that they may be relevant areas for mid-life intervention studies. Further, a simulation study using data from the Nurses’ Health Study suggest that midlife weight loss and physical activity interventions would be most efficacious in preventing chronic disease incidence, reducing risk by up to 10 percentage points [90]. The current pressing challenge, however, is to develop and implement interventions that, when begun during the mid-life, have the capacity for long-term adherence and effectiveness so as to impact long-term health, functioning and wellness trajectories.
Another challenge to intervention studies among mid-life populations is the highly dynamic nature of mid-life functioning and disability, thereby signaling a need for different frameworks and interventions to impact the onset and recovery from functional limitations and disability. In HRS among adults age 51–61 years, recovery from mobility disability over 2 years was predicted by lack of diabetes, lung disease and pain whereas onset of mobility disability was predicted by being female, less educated, obese, and having frequent pain [91]. Among women SWAN, highly dynamic patterns of functioning, characterized as both worsening and improving over time, were observed among obese women and women who had arthritis [36]. Therefore, different intervention programs and paradigms may need to be considered which target mid-life factors to prevent old age disability versus those that can prompt recovery from current mid-life disability.
Conclusion
Disability prevalence is high during the mid-life, yet domains of disability among younger populations differ substantially from those among older adults. Despite a high burden, evidence suggests that the presence of mid-life disability does not inevitably worsen. Instead, encouraging data suggests that mid-aged individuals are highly capable of recovering from non-chronic disability. This observation, combined with the known detrimental effect of poor functioning and disability on current and further health should prompt a concentrated public health effort to target interventions to improve functioning and prevent disability among mid-aged adults. Focused efforts on treatment of depression and physical activity interventions to reduce obesity and prevent mobility disability may be most efficacious during this life stage.
Abbreviations
- SIPP
Survey of Income and Program Participation
- WHO
World Health Organization
- ICF
International Classification of Functioning
- ADL
Activities of daily living
- IADL
Instrumental activities of daily living
- WHO-DAS
World Health Organization Disability Assessment Schedule
- SWAN
Study of Women’s Health Across the Nation
- NHANES
National Health and Nutrition Examination Survey
- NHIS
National Health Interview Survey
- HRS
Health and Retirement Survey
- BRFSS
Behavioral Risk Factor Surveillance System
Footnotes
Competing interests
The author declares that she has no competing interests.
Authors’ contributions
CKG conceived of the manuscript, drafted and revised the manuscript, has approved the final version of the manuscript and is accountable for all aspects of work associated with this manuscript.
Authors’ information
CKG is an Assistant Research Professor whose research focuses on the impact of chronological and reproductive aging and obesity as risk factors for the development of knee osteoarthritis, functional limitations and disability.
References
- 1.World Health Organization . World Health Report 2003. Geneva: World Health Organization; 2003. [Google Scholar]
- 2.Crimmins E, Saito Y. Change in the prevalence of diseases among older Americans: 1984–1994. Demogr Res. 2000;3:9. doi: 10.4054/DemRes.2000.3.9. [DOI] [Google Scholar]
- 3.Freedman VA, Schoeni RF, Martin LG, Cornman JC. Chronic conditions and the decline in late-life disability. Demography. 2007;44(3):459–477. doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- 4.Paez KA, Zhao L, Hwang W. Rising out-of-pocket spending for chronic conditions: a ten-year trend. Health Aff (Millwood) 2009;28:15–25. doi: 10.1377/hlthaff.28.1.15. [DOI] [PubMed] [Google Scholar]
- 5.Hootman JM, Brault MW, Helmick CG, Theis KA, Armour BS. Prevalence and most common causes of disability among adults-United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58(16):421–426. [PubMed] [Google Scholar]
- 6.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UN World Health Organization (WHO). World Report on Disability: Summary. 2011. WHO/NMH/VIP/11.01, available at: http://www.refworld.org/docid/50854a322.html [accessed 29 April 2015].
- 8.Brault MW. Americans With Disabilities: 2010. Washington (DC): U.S. Census Bureau; 2012 Jul. (Current Population Reports; 70-131).
- 9.Centers for Disease Control and Prevention (CDC) Trends in aging – United States and worldwide. MMWR Morb Mortal Wkly Rep. 2003;52(6):101–106. [PubMed] [Google Scholar]
- 10.United Nations, Department of Economic and Social Affairs, Population Division, 2013. World Population Ageing 2013. ST/ESA/SER.A/348, available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf [accessed 29 April 2015].
- 11.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 12.United Nations, Department of Economic and Social Affairs, Population Division, 2001. World Population Ageing 1950–2050. ST/ESA/SER.A/207, available at: http://www.un.org/esa/population/publications/worldageing19502050/ [accessed 29 April 2015].
- 13.Romero-Ortuno R, Fouweather T, Jagger C. Cross-national disparities in sex differences in life expectancy with and without frailty. Age Ageing. 2014;43(2):222–228. doi: 10.1093/ageing/aft115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oksuzyan A, Bronnum-Hansen H, Jeune B. Gender gap in health expectancy. Eur J Ageing. 2010;7:213–218. doi: 10.1007/s10433-010-0170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill TM, Gahbauer EA, Lin H, Han L, Allore HG. Comparisons between older men and women in the trajectory and burden of disability over the course of nearly 14 years. J Am Med Dir Assoc. 2013;14(4):280–286. doi: 10.1016/j.jamda.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hosseinpoor AR, Williams JS, Jann B, Kowal P, Officer A, Posarac A, Chatterji S. Social determinants of sex differences in disability among older adults: a multi-country decomposition analysis using the World Health Survey. Int J Equity Health. 2012;11:52. doi: 10.1186/1475-9276-11-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tseng LA, Delmonico MJ, Visser M, Boudreau RM, Goodpaster BH, Schwartz AV, et al. Body composition explains sex differential in physical performance among older adults. J Gerontol A Biol Sci Med Sci. 2014;69(1):93–100. doi: 10.1093/gerona/glt027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yount KM, Hoddinott J, Stein AD. Disability and self-rated health among older women and men in rural Guatemala: the role of obesity and chronic conditions. Soc Sci Med. 2010;71:1418–1427. doi: 10.1016/j.socscimed.2010.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammond JM. Multiple jeopardy or multiple resources? The intersection of age, race, living arrangement and education level and the health of older women. J Women Aging. 1995;7(3):5–24. doi: 10.1300/J074v07n03_02. [DOI] [Google Scholar]
- 20.Kuh D, Bassey EJ, Butterworth S, Hardy R, Wadsworth ME. Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol A Biol Sci Med Sci. 2005;60(2):224–231. doi: 10.1093/gerona/60.2.224. [DOI] [PubMed] [Google Scholar]
- 21.Bassey EJ, Mockett SP, Fentem PH. Lack of variation in muscle strength with menstrual status in healthy women aged 45–54 years: data from a national survey. Eur J Appl Physiol Occup Physiol. 1996;73(3–4):382–386. doi: 10.1007/BF02425503. [DOI] [PubMed] [Google Scholar]
- 22.Danneskiold-Samsoe B, Bartels EM, Bulow PM, Lund H, Stockmarr A, Holm CC, et al. Isokinetic and isometric muscle strength in a healthy population with special reference to age and gender. Acta Physiol (Oxf) 2009;197(Suppl 673):1–68. doi: 10.1111/j.1748-1716.2009.02022.x. [DOI] [PubMed] [Google Scholar]
- 23.Samson MM, Meeuwsen IB, Crowe A, Dessens JA, Duursma SA, Verhaar HJ. Relationships between physical performance measures, age, height and body weight in healthy adults. Age Ageing. 2000;29(3):235–242. doi: 10.1093/ageing/29.3.235. [DOI] [PubMed] [Google Scholar]
- 24.Phillips SK, Rook KM, Siddle NC, Bruce SA, Woledge RC. Muscle weakness in women occurs at an earlier age than in men, but strength is preserved by hormone replacement therapy. Clin Sci (Lond) 1993;84(1):95–98. doi: 10.1042/cs0840095. [DOI] [PubMed] [Google Scholar]
- 25.Greeves JP, Cable NT, Reilly T, Kingsland C. Changes in muscle strength in women following the menopause: a longitudinal assessment of the efficacy of hormone replacement therapy. Clin Sci (Lond) 1999;97:79–84. doi: 10.1042/cs0970079. [DOI] [PubMed] [Google Scholar]
- 26.Tseng LA, El Khoudary SR, Young EA, Farhat GN, Sowers M, Sutton-Tyrrell K, Newman AB. The association of menopause status with physical function: the Study of Women’s Health Across the Nation. Menopause. 2012;19(11):1186–1192. doi: 10.1097/gme.0b013e3182565740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumari M, Stafford M, Marmot M. The menopausal transition was associated in a prospective study with decreased health functioning in women who report menopausal symptoms. J Clin Epidemiol. 2005;58:719–727. doi: 10.1016/j.jclinepi.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54(4):439–467. doi: 10.2307/3349677. [DOI] [PubMed] [Google Scholar]
- 29.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 30.Nuru-Jeter AM, Thorpe RJ, Jr, Fuller-Thomson E. Black-white differences in self-reported disability outcomes in the U.S.: early childhood to older adulthood. Public Health Rep. 2011;126(6):834–843. doi: 10.1177/003335491112600609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freedman VA, Spillman BC, Andreski PM, Cornman JC, Crimmins EM, Kramarow E, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50(2):661–671. doi: 10.1007/s13524-012-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karvonen-Gutierrez CA, Ylitalo KR. Prevalence and correlates of disability in a late middle-aged population of women. J Aging Health. 2013;25(4):701–717. doi: 10.1177/0898264313488165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin LG, Freedman VA, Schoeni RF, Andreski PM. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Aff (Millwood) 2010;29:725–731. doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988–1994 and 1999–2004. Am J Public Health. 2010;100(1):100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin LG, Schoeni RF. Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disabil Health J. 2014;7(1 suppl):S4–S14. doi: 10.1016/j.dhjo.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ylitalo KR, Karvonen-Gutierrez CA, Fitzgerald N, Zheng H, Sternfeld B, El Khoudary SR, Harlow SD. Relationship of race-ethnicity, body mass index, and economic strain with longitudinal self-report of physical functioning: the Study of Women’s Health Across the Nation. Ann Epidemiol. 2013;23(7):401–408. doi: 10.1016/j.annepidem.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murray ET, Hardy R, Strand BH, Cooper R, Guralnik JM, Kuh D. Gender and life course occupational social class differences in trajectories of functional limitations in midlife: findings from the 1946 British birth cohort. J Gerontol A Biol Sci Med Sci. 2011;66(12):1350–1359. doi: 10.1093/gerona/glr139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adams PF, Marano MA. Current estimates from the National Health Interview Survey, 1994. Vital Health Stat 10. 1995;193(Pt1):1–260. [PubMed] [Google Scholar]
- 39.Kattainen A, Reunanen A, Koskinen S, Martelin T, Knekt P, Sainio P, Harkanen T, Aromaa A. Secular changes in disability among middle-aged and elderly Finns with and without coronary heart disease from 1978–1980 and 2000–2001. Ann Epidemiol. 2004;14(7):479–485. doi: 10.1016/j.annepidem.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 40.Krishnan E, Sokka T, Hakkinen A, Hubert H, Hannonen P. Normative values for the Health Assessment Questionnaire disability index: benchmarking disability in the general population. Arthritis Rheum. 2004;50(3):953–960. doi: 10.1002/art.20048. [DOI] [PubMed] [Google Scholar]
- 41.Brown RT, Pierluissi E, Guzman D, Kessell ER, Goldman LE, Sarkar U, Schneidermann M, Critchfield JM, Jushel MB. Functional disability in late-middle-aged and older adults admitted to a safety-net hospital. J Am Geriatr Soc. 2014;62(11):2056–2063. doi: 10.1111/jgs.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, Harris T, Health ABC Study Group Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2011;56(10):M644–649. doi: 10.1093/gerona/56.10.M644. [DOI] [PubMed] [Google Scholar]
- 43.Wittink H, Rogers W, Sukiennik A, Carr DB. Physical functioning: self-report and performance measures are related but distinct. Spine. 2003;28(20):2407–2413. doi: 10.1097/01.BRS.0000085304.01483.17. [DOI] [PubMed] [Google Scholar]
- 44.Bean JF, Olveczky DD, Kiely DK, LaRose SI, Jette AM. Performance-based versus patient-reported physical function: what are the underlying predictors? Phys Ther. 2011;91(12):1804–1811. doi: 10.2522/ptj.20100417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Altman BM, Gulley SP. Convergence and divergence: differences in disability prevalence estimates in the United States and Canada based on four health survey instruments. Soc Sci Med. 2009;69(4):543–552. doi: 10.1016/j.socscimed.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 46.Mitra S, Findley PA, Sambamoorthi U. Health care expenditures of living with a disability: total expenditures, out-of-pocket expenses, and burden, 1996 to 2004. Arch Phys Med Rehabil. 2009;90(9):1532–1540. doi: 10.1016/j.apmr.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 47.Zhao G, Ford ES, Li C, Crews JE, Mokdad AH. Disability and its correlates with chronic morbidities among US adults aged 50-<65 years. Prev Med. 2009;48(2):117–121. doi: 10.1016/j.ypmed.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 48.Mann J, Balte P, Clarkson J, Nitchea D, Graham CL, McDermott S. What are the specific disability and limitation types underlying responses to the BRFSS disability questions? Disability Health J. 2015;8:17–28. doi: 10.1016/j.dhjo.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Schellekens JM, Abma FI, Mulders HP, Brouwer S. Measuring clients’ perception of functional limitations using the Perceived Functioning & Health questionnaire. J Occup Rehabil. 2010;20(4):512–525. doi: 10.1007/s10926-010-9236-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garin O, Ayuso-Mateos JL, Almansa J, Nieto M, Chatterji S, Vilagut G, et al. Validation of the World Health Organization Disability Assessment Schedule, WHODAS-2 in patients with chronic diseases. Health Qual Life Outcomes. 2010;8:51. doi: 10.1186/1477-7525-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ustun TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, et al. WHO/NIH joint project: developing the world health organization disability assessment schedule 2.0. Bull World Health Organ. 2010;88(11):815–823. doi: 10.2471/BLT.09.067231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arterburn D, Westbook EO, Ludman EJ, Operskalski B, Linde JA, Rohde P, et al. Relationship between obesity, depression and disability in middle-aged women. Obes Res Clin Pract. 2012;6(3):e197–206. doi: 10.1016/j.orcp.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Pedro-Cuesta J, Alberquilla A, Virues-Ortega J, Carmona M, Alcalde-Cabero E, Bosca G, et al. ICF disability measured by WHO-DAS II in three community diagnostic groups in Madrid, Spain. Gac Sanit. 2011;25(Suppl 2):21–28. doi: 10.1016/j.gaceta.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 54.Miszkurka M, Zunzunegui MV, Langlois EV, Freeman EE, Kouanda S, Haddad S. Gender differences in mobility disability during young, middle and older age in West African adults. Glob Public Health. 2012;7(5):495–508. doi: 10.1080/17441692.2011.630676. [DOI] [PubMed] [Google Scholar]
- 55.Payne CF, Mkandawire J, Kohler HP. Disability transitions and health expectancies among adults 45 years and older in Malawi: a cohort-based model. PLoS Med. 2013;10(5):e1001435. doi: 10.1371/journal.pmed.1001435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wandera SO, Notzi J, Kwagala B. Prevalence and correlates of disability among older Ugandans: evidence from the Uganda National Household Survey. Glob Health Action. 2014;7:25686. doi: 10.3402/gha.v7.25686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zheng X, Chen G, Song X, Liu J, Yan L, Du W, Pang L, Zhang L, Wu J, Zhang B, Zhang J. Twenty-year trends in the prevalence of disability in China. Bull World Health Organ. 2011;89(11):788–797. doi: 10.2471/BLT.11.089730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Peng X, Song S, Sullivan S, Qiu J, Wang W. Ageing, the urban–rural gap and disability trends: 19 years of experience in China – 1987 to 2006. PLoS One. 2010;5(8):e12129. doi: 10.1371/journal.pone.0012129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hairi NN, Bulgiba A, Cumming RG, Naganathan V, Mudla I. Prevalence and correlates of physical disability and functional limitation among community dwelling older people in rural Malaysia, a middle income country. BMC Public Health. 2010;10:492. doi: 10.1186/1471-2458-10-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Almazan-Isla J, Comin-Comin M, Damian J, Alcalde-Cabero E, Ruiz C, Franco E, Martin G, Larrosa-Montanes LA, de Pedro-Cuesta J. Analysis of disability using WHODAS 2.0 among middle-aged and elderly in Cinco Villas, Spain. Disabil Health J. 2014;7(1):78–87. doi: 10.1016/j.dhjo.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 61.Iezzoni LI, Kurtz SG, Rao SR. Trends in US adult chronic disability rates over time. Disabil Health J. 2014;7(4):402–412. doi: 10.1016/j.dhjo.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van Houwelingen AH, Cameron ID, Gussekloo J, Putter H, Kurrle S, de Craen AJ, et al. Disability transitions in the oldest old in the general population; The Leiden 85-plus study. Age (Dordr) 2014;26(1):483–493. doi: 10.1007/s11357-013-9574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kulmala J, von Bonsdorff MB, Stenholm S, Tormakangas T, von Bonsdorff ME, Nygard CH, et al. Perceived stress symptoms in midlife predict disability in old age: a 28-year prospective cohort study. J Gerontol A Biol Sci Med Sci. 2013;68(8):984–991. doi: 10.1093/gerona/gls339. [DOI] [PubMed] [Google Scholar]
- 64.Agahi N, Lennartsson C, Kareholt I, Shaw BA. Trajectories of social activities from middle age to old age and late-life disability: a 36-year follow-up. Age Ageing. 2013;42(6):790–793. doi: 10.1093/ageing/aft140. [DOI] [PubMed] [Google Scholar]
- 65.Deshpande N, Metter EJ, Guralnik J, Bandinelli S, Ferrucci L. Predicting 3-year incident mobility disability in middle-aged and older adults using physical performance tests. Arch Phys Med Rehabil. 2013;94(5):994–997. doi: 10.1016/j.apmr.2012.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Imai K, Gregg EW, Chen YJ, Zhang P, de Rekeneire N, Williamson DF. The association of BMI with functional status and self-rated health in US adults. Obesity. 2008;16:40240–8. doi: 10.1038/oby.2007.70. [DOI] [PubMed] [Google Scholar]
- 67.Nosek MA, Robinson-Whelen S, Hughes RB, Petersen NJ, Taylor HB, Bryne MM, Morgan R. Overweight and obesity in women with physical disabilities: Associations with demographic disability characteristics and secondary conditions. Disabil Health J. 2008;1:89–98. doi: 10.1016/j.dhjo.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 68.Wolinsky FD, Miller TR, Malmstrom TK, Miller JP, Schootman M, Andresen EM, Miller DK. Four-year lower extremity disability trajectories among African American men and women. J Gerontol A Biol Sci Med Sci. 2007;62:525–530. doi: 10.1093/gerona/62.5.525. [DOI] [PubMed] [Google Scholar]
- 69.Khoury AJ, Hall A, Andresen E, Zhang J, Ward R, Jarjoura C. The association between chronic disease and physical disability among female Medicaid beneficiaries 18–64 years of age. Disabil Health J. 2013;6(2):141–148. doi: 10.1016/j.dhjo.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 70.Dunlop DD, Manheim LM, Song J, Lyons JS, Chang RW. Incidence of disability among preretirement adults: the impact of depression. Am J Public Health. 2005;95(11):2003–2008. doi: 10.2105/AJPH.2004.050948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Clarke P, Latham K. Life course health and socioeconomic profiles of Americans aging with disability. Disabil Health J. 2014;7(1 Suppl):S15–22. doi: 10.1016/j.dhjo.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wong E, Stevenson C, Backholer K, Woodward M, Shaw JE, Peeters A. Predicting the risk of physical disability in old age using modifiable mid-life risk factors. J Epidemiol Community Health. 2015;69(1):70–76. doi: 10.1136/jech-2014-204456. [DOI] [PubMed] [Google Scholar]
- 73.den Ouden ME, Schuurmans MJ, Brand JS, Arts IE, Mueller-Schotte S, van der Schouw YT. Physical functioning is related to both an impaired physical ability and ADL disability: a ten year follow-up study in middle-aged and older persons. Maturitas. 2013;74(1):89–94. doi: 10.1016/j.maturitas.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 74.Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38:1134–1141. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 75.Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, Sutton-Tyrrell K. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009;54(25):2366–2373. doi: 10.1016/j.jacc.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 77.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: results from the Baltimore Epidemiological Catchment Area study. JAMA Psychiatry. 2014;71(3):273–280. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Koonce RC, Bravman JT. Obesity and osteoarthritis: more than just wear and tear. J Am Acad Orthop Surg. 2013;21(3):161–169. doi: 10.5435/JAAOS-21-03-161. [DOI] [PubMed] [Google Scholar]
- 79.Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res. 2015;8:399–408. doi: 10.2147/JPR.S55598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 81.Klijs B, Nusselder WJ, Looman CW, Mackenback JP. Contribution of chronic disease to the burden of disability. PLoS One. 2011;6(9):e25325. doi: 10.1371/journal.pone.0025325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sundstrup E, Jakobsen MD, Andersen CH, Jay K, Persson R, Aagaard P, Andersen LL. Effect of two contrasting interventions on upper limb chronic pain and disability: a randomized controlled trial. Pain Physician. 2014;17(2):145–154. [PubMed] [Google Scholar]
- 83.Linton SJ, Boersma K, Traczyk M, Shaw W, Nicholas M. Early workplace communication and problem solving to prevent back disability: results of a randomized controlled trial among high-risk workers and their supervisors. J Occup Rehabil. 2015. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 84.Del Pozo-Cruz B, Adsuar JC, Parraca J, Del Pozo-Cruz J, Moreno A, Gusi N. A web-based intervention to improve and prevent low back pain among office workers: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42(10):831–841. doi: 10.2519/jospt.2012.3980. [DOI] [PubMed] [Google Scholar]
- 85.Freedman VA, Hodgson N, Lynn J, Spillman B, Waidmann T, Wilkinson A, Wold DA. US Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy. A framework for identifying high-impact interventions to promote reductions in late-life disability. 2006. Available at http://aspe.hhs.gov/daltcp/reports/2006/prodecl.htm, [accessed 29 April 2015].
- 86.Daniels R, van Rossum E, de Witte L, Kempen GI, van den Heuvel W. Interventions to prevent disability in frail community-dwelling elderly: a systematic review. BMC Health Serv Res. 2008;8:278. doi: 10.1186/1472-6963-8-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cesari M, Vellas B, Hsu FC, Newman AB, Doss H, King AC, et al. A physical activity intervention to treat the frailty syndrome in older persons – results from the LIFE-P study. J Gerontol A Biol Sci Med Sci. 2015;70(20):216–222. doi: 10.1093/gerona/glu099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gitlin LN, Szanton SL, Huang J, Roth DL. Factors mediating the effects of a depression intervention on functional disability in older African Americans. J Am Geriatr Soc. 2014;62(12):2280–2287. doi: 10.1111/jgs.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Danaei G, Pan A, Hu FB, Hernan MA. Hypothetical midlife interventions in women and risk of type 2 diabetes. Epidemiology. 2013;24(1):122–128. doi: 10.1097/EDE.0b013e318276c98a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Clark DO, Stump TE, Wolinsky FD. Predictors of onset and recovery from mobility difficulty among adults age 51–61 years. Am J Epidemiol. 1998;148(1):63–71. doi: 10.1093/oxfordjournals.aje.a009561. [DOI] [PubMed] [Google Scholar]


