Abstract
This study sought to characterize depressive symptoms among mothers in Latino farmworker families, determine if maternal depression increases children's risk of obesity, and ascertain whether relevant risk factors such as physical activity, diet, and feeding style mediate this relationship. Mothers from 248 families completed the 10‐item Center for Epidemiologic Studies Depression Scale 9 times over a 2‐year period. Four distinct patterns were used to describe mothers: few symptoms, moderate episodic symptoms, severe episodic symptoms, and chronic symptoms. Approximately two‐thirds of women experienced moderate symptoms of depression at least once. Children of mothers fitting each pattern were compared. At the end of the study, children of mothers with severe episodic and chronic symptoms were significantly more likely to be overweight and obese than children of mothers with few symptoms (p < .05). After controlling for covariates, differences in weight status for children of mothers with severe episodic symptoms remained significant. Children of mothers with either moderate episodic or chronic symptoms were fed in a less responsive fashion (p < .05), and children of chronically symptomatic mothers had lower diet quality (p < .01). Although nonresponsive feeding has been linked to childhood obesity, in this analysis, feeding style did not mediate the relationship between maternal depression and diet quality. Elevated levels of depressive symptoms are common in this population, and those symptoms, especially when severe or chronic in nature, may increase children's risk of obesity. Additional research is needed to characterize the pathways through which maternal depression influences children's weight.
Keywords: childhood obesity, depression patterns, feeding style, Latino farmworker, maternal depression, mediation analysis
Key messages.
Depressive symptoms are highly prevalent among mothers in the Latino farmworker community, but relatively few women are persistently symptomatic.
Children of mothers with severe episodic or chronic depressive symptoms were significantly more likely to be overweight/obese after 2 years of follow‐up.
Children of mothers with severe episodic and chronic symptoms had a lower diet quality, and children of mothers with moderate episodic and chronic symptoms were fed in a less responsive manner.
Depression significantly predicted feeding responsiveness and diet quality but the indirect path on diet quality as mediated by responsiveness could not be established overall or for any pattern.
Adequate screening and treatment of maternal depression may translate to improved child weight outcomes.
1. INTRODUCTION
Mounting evidence points to the pivotal role parents, and mothers especially, have in shaping the physical growth trajectories of their young children. According to Skouteris et al. (2011), parents shape the weight of their young children through their behaviours, beliefs, attitudes, and perceptions. Parenting practices related to physical activity, screen viewing, and feeding are especially relevant for children's risk of obesity (Lloyd, Lubans, Plotnikoff, Collins, & Morgan, 2014; Ventura & Birch, 2008).
Many variables, including financial resources, social supports, upbringing, culture, education, and neighbourhood resources, influence the way in which mothers care and provide for their children. Another important characteristic influencing the mother–child interaction is maternal psychopathology, including depression. Maternal depression has long been known to have important effects on children in multiple domains ranging from behavioural problems to academic performance (Lovejoy, Graczyk, O'Hare, & Neuman, 2000; Zimmer & Minkovitz, 2003). In light of the obesity epidemic, there is mounting concern regarding the effects of maternal depression on children's weight. Young children who become overweight or obese suffer not only immediate health consequences, such as hypertension, insulin resistance, dyslipidemia, and psychosocial effects; they are also put at risk for lifelong struggles with overweight and obesity and the associated complications (Kelsey, Zaepfel, Bjornstad, & Nadeau, 2014). In early childhood, dietary and activity patterns are established that may persist throughout the life course (Birch & Fisher, 1998; Trost, Sirard, Dowda, Pfeiffer, & Pate, 2003); therefore, from a public health standpoint, directing obesity prevention efforts toward young children and their families is a necessary prevention effort.
In a recent systematic review of the relationship between maternal depression and preschool‐aged children's overweight and obesity, a positive relationship was found in 15 of the 19 included studies (Benton, Skouteris, & Hayden, 2015). A separate review of nine studies including children from the ages of 2–18 concluded that chronic depression, but not episodic, was linked to children being overweight (Lampard, Franckle, & Davison, 2014). However, in both reviews, not all studies supported this relationship, and results varied depending on children's age and gender.
Both maternal depression and childhood obesity are common, especially in certain demographics. Understanding the relationship between these two conditions could prove pivotal for promoting healthy weight outcomes in young children. Although screening and treatment of maternal depression are important in their own right, if there is a causal link between these two phenomena, then broadening obesity prevention efforts to include reduction in maternal depression burden, in the context of providing more support to mothers, could be instrumental in addressing childhood overweight and obesity.
The Latino farmworker community is one population that has high prevalence of both childhood obesity and maternal depression. Given that this population is also understudied and resource deprived, exploring the relationship between mothers' mood and children's weight is especially important.
Depressive symptoms among women in Latino farmworker families may be substantially more common relative to the general population of U.S. women, for which the 12‐month prevalence of depression is reported to be 8.2% (Center for Behavioral Health Statistics and Quality, 2015). De Leon Siantz (1990) surveyed 100 Mexican–American migrant farmworker mothers with young children, and found 41% met screening criteria for depression. Structured interviews with 68 Mexican farmworker women in North Carolina revealed that approximately 40% endorsed significant symptoms (Hiott, Grzywacz, Arcury, & Quandt, 2006). In the Niños Sanos study, which supplies data for the present analysis, 31% of 248 mothers in farmworker families reported significant depressive symptoms at baseline (Pulgar et al., 2016).
The social stress paradigm argues that elevated levels of depression seen in some groups may be attributable to socio‐economic disadvantages (Aneshensel, Rutter, & Lachenbruch, 1991), which in this population would include discrimination, poverty, limited education, language barriers, acculturative stress, and lack of social supports (Hovey & Magaña, 2000; Pulgar et al., 2016). This hypothesis is consistent with findings reported in large national studies such as the 2006–2008 Behavioral Risk Factor Surveillance Study and other studies that have examined the relationship between poverty and depression (Lorant et al., 2003; Lorant et al., 2007). For example, not finishing high school and not having health insurance were both associated with significantly higher rates of depressive symptoms based on responses to the PHQ‐8 questionnaire (CDC 2010). Latina farmworkers also may have increased risk due to gender‐related discrimination and inequality and gender‐related role conflict (having to manage employment and household responsibilities simultaneously; Pulgar et al., 2016).
As with depression, childhood obesity is thought to be disproportionately common in Latino farmworker families. A recent study of 495 Latino children, ages 3–16, in a migrant farmworker community found 27% were obese (Rosado, Johnson, McGinnity, & Cuevas, 2013). Another study of 52 predominately Latino migrant farmworker children, ages 6–11, found 41% were obese (Kilanowski & Ryan‐Wenger, 2007). In contrast, among the total U.S. population of children ages 2–5, 8.9% were obese in 2011–2014 (Ogden, Carroll, Fryar, & Flegal, 2015). Latino farmworker families in the United States include an estimated 800,000 children (Mines, 1999). Given that Latino immigrants often enter the United States through the portal of agriculture, better understanding of determinants of obesity in the farmworker community is likely to benefit the broader Latino community (Quandt et al., 2016).
In the present study, the relationship between maternal depression and children's weight outcomes is explored in a sample of 248 Latino farmworker families. Although depression is characterized by certain key symptoms such as depressed mood and loss of interest in usual activities, depression represents a continuum in terms of symptom presence, severity, and persistence (Musliner, Munk‐Olsen, Eaton, & Zandi, 2016), and different patterns of depression have been shown to have different effects on children (Lampard et al., 2014). Therefore, we attempt to capture variation in the experience of depression by using repeated assessment of symptoms and classifying women into different patterns based on (a) chronicity and (b) severity. Thus, women who experience persistent symptoms of depression can be examined separately from women who experience episodic symptoms, and women who experience moderate symptoms can be examined separately from those with more severe symptoms. Subsequently, we report whether certain patterns are associated with increased body mass index (BMI) and overweight/obesity in children.
A second objective of the present study is to determine how maternal depression may be contributing to unhealthy increases in children's weight. Although a growing body of evidence points to the fact that maternal depression and children's weight status are linked, the pathways through which depression influences weight have not been fully elucidated, with mixed evidence to support various theories (Benton et al., 2015). Nonetheless, recent evidence from at least one longitudinal study indicates that maternal depression may influence young children's TV viewing time and time spent sedentary. Fernald, Jones‐Smith, Ozer, Neufeld, and DiGirolamo (2008) found that 4–5 year‐old children in low SES Latino families, whose mothers exhibited depressive symptoms when the children were 15 months old, had overall low activity levels and high TV viewing time (10+ hr per week). Given that excess energy intake relative to energy expenditure is known to drive weight gain, and that poor dietary intake as well as sedentary activity patterns can both contribute to overweight, we compare a variety of dietary and activity risk factors that may differ for children with depressed mothers, such as time spent active or sedentary each day, daily screen time, diet quality, total energy intake, and feeding style.
Feeding style, the manner in which mothers interact with children in feeding situations, is one of the most plausible candidates for linking maternal depression, diet quality, and children's weight (Lindsay, Mesa, Greaney, Wallington, & Wright, 2017). As with parenting style, feeding style is often described in terms of the underlying dimensions of demandingness and responsiveness. In the context of feeding style, demandingness may be thought of as the amount or degree to which parents encourage eating, whereas responsiveness refers to how the parents encourage eating (Tovar et al., 2012). A responsive feeding style encourages and attends to the satiety of the child in an emotionally supportive way, whereas a nonresponsive style is characterized by a lack of reciprocity between the parent and child (Black & Aboud, 2011). A nonresponsive feeding style may be overly indulgent, allowing the child to control selection and intake of food, or overly demanding, in which case the child's own sense of fullness may be disregarded. Mothers with depressive symptoms such as low energy or lack of motivation may gravitate toward a feeding style that is less responsive, which may in turn have negative effects on the quality of the child's diet (Goulding et al., 2014; Hughes, Power, Liu, Sharp, & Nicklas, 2015). Another possibility is that depressed mothers may be less motivated to spend time shopping for healthy foods or preparing healthy meals. Indeed, Gross, Velazco, Briggs, and Racine (2013) found children of mildly depressed mothers consumed more sweetened beverages, were more likely to eat out at restaurants, and were more likely to skip breakfast. Specific feeding practices, as opposed to feeding style, may also mediate the relationship between maternal depression and childhood obesity. Detailed measures of feeding practices were not collected in our study.
The third and final objective is to test whether differences in risk factors for obesity such as feeding style mediate the relationship between maternal depression and children's weight outcomes. Mediation analysis is only indicated and will only be performed for those variables which differ significantly between mother–child pairs with different patterns of depressive symptoms.
Determining the relationship between maternal depression and childhood obesity could clarify the effects of maternal depression on children's health. If maternal depression and excess weight gain are indeed correlated, this further supports the importance of depression screening and treatment of mothers' affective disorders. We hypothesize that, as maternal depression increases in severity and occurs more consistently, children's weight will increase in response, and that this increase can be explained at least in part by variation in modifiable risk factors for obesity. This study aims to (a) characterize depression among Latino farmworker mothers using four distinct depression symptom patterns; (b) determine if depression pattern can predict differences in BMI status of children and various risk factors for obesity; and (c) determine if depression pattern influences dietary and weight outcomes through both a direct pathway as well as an indirect pathway for which feeding or activity differences may serve as mediators.
2. METHODS
This analysis included 248 families enrolled in the Niños Sanos study, a longitudinal 2‐year study of dietary and physical activity patterns of young children of Latino farmworkers in North Carolina. Eligible participants were self‐identified Latinas with a coresident child aged 2.5–3.5 years and at least one member of the household engaging in farm work during the previous year.
2.1. Sampling and recruitment
A site‐based sampling plan with a large contact base was developed to recruit participants. This approach was chosen due to the narrow age range of children and lack of sampling frame. “Sites” are organizations or locations with which members of the target community are associated. Sites used in this study include Head Start and Migrant Head Start programmes (n = 7), migrant education programmes (n = 15), community health centres (n = 4), Special Supplemental Nutrition Program for Women, Infants, and Children (n = 1), community partner nonprofit organizations (n = 2), and stores, churches, and events serving predominantly farmworkers (n = 7). Community data collectors also conducted door‐to‐door recruitment in multiple Latino neighbourhoods and farmworker camps, and previous participants in Latino health studies were contacted regarding participation.
A bilingual female data collector contacted potential participants, either in person or by phone, depending on the site. Organizations subject to privacy regulations (i.e., Head Start) used staff members to solicit permission to contact parents. After making contact, the data collector introduced the study and screened for inclusion criteria, explained study procedures and incentives of study participation, and invited eligible families to participate. All participants provided signed informed consent. The Wake Forest School of Medicine Institutional Review Board approved the study, and a certificate of confidentiality was obtained from the National Institutes of Health.
Given the multipronged nature of the sampling strategy, precise rates of participation and refusal could not be determined. The study eligibility of persons who declined to participate is unknown. Sites may have provided incomplete lists of potential participants, and potential participants may have avoided contact at events.
2.2. Data collection
Nine trained study staff interviewed participants at baseline and during each quarter of the study (nine total measurement points). All interviews were conducted in Spanish in participants' homes or another preferred location between April 19, 2011 and July 30, 2014. Compensation of 10 dollars was given for each interview. Participants were administered a survey designed to determine demographic, family, household characteristics, their level of current depressive symptoms, and other information. Children's weight was measured using a Tanita model BSB800 digital scale capable of determining weight to the nearest 0.1 kg. Height was determined using a portable stadiometer without shoes.
Children's dietary data were collected using three 24‐hr recalls during a 7‐day period, including one weekend day and two weekdays. Nutrition Data System for Research software (Version 11) was used (Johnson, 2002). The first recall was conducted face‐to‐face, and subsequent interviews were conducted in person when possible or by telephone. Mothers were given a printed serving size guide, and the interviewer measured the size or volume of their child's usual bowl, plate, and cup to help calculate serving sizes. For children enrolled in preschools or daycares, food intake data were collected directly from those caregivers.
The Revised Children's Diet Quality Index (Kranz, Hartman, Siega‐Riz, & Herring, 2006), specifically developed for use among preschoolers, was used to evaluate quality of children's dietary intake using data from the three 24‐hr recalls. This index uses 13 dietary components, such as added sugar and fat intake, to determine diet quality. The range of possible total scores extends from 0 to 90, with higher values indicating higher quality. Points are deducted for each component according to the degree of deviation from the ideal, determined using professional recommendations (Kranz et al., 2006). Energy intake was calculated as the mean of the total kilo‐calories per day from the three 24‐hr recalls. Dietary data collected at baseline, end of Year 1 and end of Year 2, are used in this analysis.
Children's physical activity was measured using Actical accelerometers (Mini Mitter Company, Inc., Bend OR). Each device was attached to an elastic belt positioned above the child's iliac crest per usual protocols. Children were asked to wear the belt for 7 days and only remove the device for swimming, bathing, and sleeping. Mothers and children were compensated for completing the accelerometer protocol.
Accelerometers, initialized with 15‐s epochs, provided data to determine minutes children spent performing activities of varying intensity. Following the protocol used by Dolinksy, Brouwer, Evenson, Siega‐Riz, and Ostbye (2011), epochs with fewer than 12 counts were labelled sedentary, and epochs with more than 714 counts were classified as moderate/vigorous activity. Values between 12 and 714 represented light activity. The total number of epochs in each category was divided by the number of observation days to derive average minutes per day for each activity. Accelerometer data collected at baseline, end of Year 1 and end of Year 2, are used in this analysis.
2.3. Measures
2.3.1. Center for Epidemiologic Studies Depression Scale short form (CES‐D)
A 10‐item version of the CES‐D (Kohout, Berkman, Evans, & Cornoni‐Huntley, 1993), which measures symptoms of depression over the previous week, was administered to participants at baseline and every quarter (3 months) of the study. The short version has a factor structure similar to the full version and has been shown to have high concordance with measures of clinical depression (Zich, Attkisson, & Greenfield, 1990). Scores for each item, rated 0 (rarely or never) to 3 (most of the time or always), were summed to determine level of depressive symptoms. Two cut‐off scores were chosen to indicate intensity of depressive symptoms: 10 for moderate and 16 for severe. Although the 10‐item CES‐D was designed to use 10 as a single cut‐off score, several studies in diverse populations have suggested higher cut‐off scores are ideal in terms of sensitivity and specificity (Cho & Kim, 1998; Haringsma, Engels, Beekman, & Spinhoven, 2004). The ideal cut‐off score for Latino farmworkers is unknown, given the many ways in which this population differs from the mostly middle class white samples used to derive the original CES‐D (Cheng & Chan, 2005). Given current understanding of the stressful conditions in which farmworkers live and work, the standard cut‐off of 10 may misidentify people who are transiently stressed as depressed. The use of two cut‐off scores enables the identification of a subset of the population with more severe symptoms and can provide additional insight into the burden of depression.
Women were classified as having either few symptoms of depression or belonging to one of three depression patterns based on CES‐D scores over the nine time points of the study (Figure 1). Any woman who reported significant depressive symptoms (≥10) on four or more occasions, at which point symptoms were present at least half of the study quarters, was considered to have chronic depression. Any woman who was depressed on one to three occasions was considered to have episodic depression. The women in this group were further subdivided as having either moderate symptoms (maximum score < 16) or severe symptoms (maximum score ≥ 16). Further categorization (i.e., chronic moderate or chronic severe) was not pursued due to small size of the groups.
Figure 1.
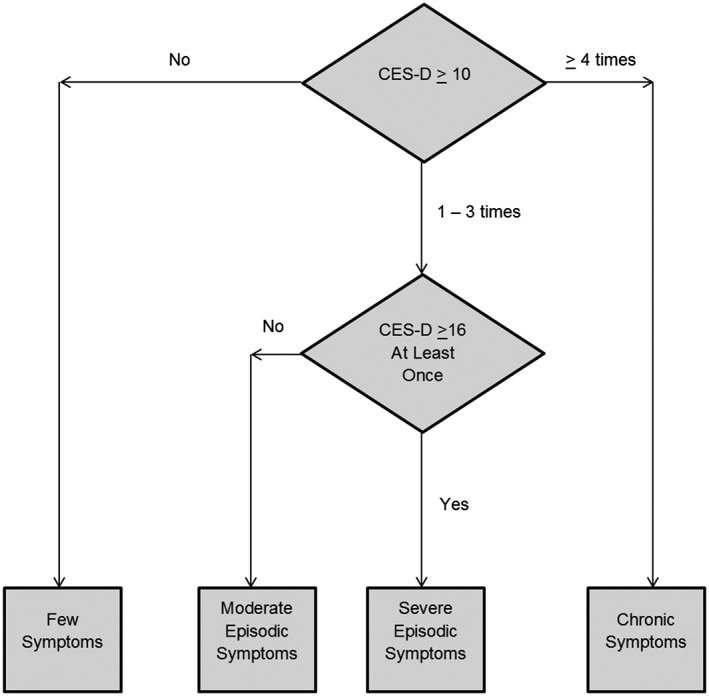
Classification of women using four patterns of depression. The few symptoms pattern includes women who never endorsed significant symptoms of depression (defined as ≥10 on the 10‐item CES‐D). The chronic symptoms group scored ≥10 on four or more occasions. The moderate episodic symptoms group includes women who scored 10 to 15 on one to three occasions but never greater than 15, and the severe episodic symptoms group includes women who scored ≥16 at least once but did not meet criteria for chronic depression
2.3.2. Caregiver's Feeding Style Questionnaire (CFSQ)
Parental feeding style was measured at baseline, 12 months and 24 months, using the CFSQ (Hughes et al., 2006). The CFSQ was designed specifically for use among low‐income African Americans and Hispanics, and reliability and validity have been demonstrated (Hughes et al., 2006). Each of the 13 items is rated on a 5‐point Likert scale ranging from 1 (never) to 5 (always). Items measure use of strategies that are either “parent centred” or “child centred” in nature. The mean score of all items constitutes the level of demandingness and has a range from one to five. Responsiveness is determined by dividing the mean of the child‐centred items by the demandingness score, and has a range 0.2–5.0.
2.4. Child BMI percentile
Standard CDC growth charts were used to determine age‐ and gender‐specific BMI percentiles for children (Kuczmarski, Ogden, & Grummer‐Strawn, 2000). Normal BMI was defined as BMI ≥ 5th percentile and <85th percentile. Overweight was defined as BMI ≥ 85th percentile, but <95th percentile, and obese as ≥95th percentile. A BMI < 5th percentile was considered underweight.
2.5. Other measures
Mothers reported their own age and the child's age and gender. Mothers reported their current employment and marital status and education in years completed. If the mother reported either parent moved from place to place to perform farm work, the family was classified as migrant; otherwise, they were classified as seasonal. Each mother reported whether she and her spouse/partner had documents allowing legal residence in the United States; if either had documents, the family was classified as documented. Each mother noted whether or not she set limits on children's television and video game usage using a 5‐point scale (1 = never and 5 = always), how often she took her child to play spaces such as parks (0–6 scale, higher number indicates greater frequency), and whether she was concerned about her child's level of activity (dichotomized as 0 [no concern] or 1 [any degree of concern]). Women were not asked if they had sought or received treatment for depression.
2.6. Statistical analysis
Descriptive statistics were used to describe the characteristics of the sample by depression pattern. Depression pattern was determined using observations from baseline and all eight quarters. Analyses involving other variables were conducted using data from baseline and the end of Years 1 and 2, because not all data were collected at all quarters. Depending on the outcome variable, bivariate analyses between an outcome variable and depression patterns were performed using chi‐square tests, Fisher's Exact Tests, and one‐way analyses of variance. At both baseline and the 24‐month follow‐up, several measures of child weight status were compared across depression patterns. We also tested for differences across depression pattern by child characteristics that were averaged over the course of the study. Longitudinal mixed effects models were constructed using PROC MIXED for continuous outcomes and PROC GLIMMIX for categorical outcomes. PROC MIXED is a generalization of ordinary linear regression to longitudinal data; and PROC GLIMMIX can be considered a generalization of logistic linear regression to longitudinal data. The outcome measures grouped by child were treated as repeated measures. Longitudinal mediational analysis, when indicated, was conducted to test if risk factors mediated the effect of depression pattern on dietary behaviour. Covariates used in testing differences between child characteristics and mediational analyses were mother's age and education level, employment, status as a migrant versus seasonal farmworker, documentation status, mother's weight, and time. The longitudinal mediational models assumed an unstructured covariance matrix and included repeated measures that were clustered by participant. All analyses were performed using SAS v. 9.4 (Cary, NC).
3. RESULTS
Retention of subjects was high (89.1%), with only 12 subjects withdrawn and 15 lost to follow‐up out of 248. Twenty‐one families that provided data at fewer than three observations were excluded from this analysis, which resulted in a final sample size of 227. Approximately, two‐thirds of women scored ≥10 on the 10‐item CES‐D at least once over the 2‐year study period. Ninety‐three women (41.0%) comprised the moderate episodic symptoms pattern and 35 women (15.4%) the severe episodic symptoms pattern. Twenty‐six women (11.5%) comprised the chronic depression pattern and the remaining 73 women (32.2%) constituted the few symptoms pattern (seven of whom actually reported no symptoms of depression at any time point).
Women were similar across patterns in terms of age, education, employment status, marital status, farmworker status, and documentation status (Table 1). The only significant group differences pertained to BMI, with more depressed mothers more likely to be overweight or obese.
Table 1.
Maternal characteristics by depression pattern
| Few symptoms (n = 73) | Moderate episodic symptoms (n = 93) | Severe episodic symptoms (n = 35) | Chronic symptoms (n = 26) | ||
|---|---|---|---|---|---|
| Age | 18–25 | 36% | 25% | 29% | 23% |
| 26–35 | 53% | 58% | 57% | 54% | |
| ≥36 | 11% | 17% | 14% | 23% | |
| Education | 0–6 years | 32% | 48% | 43% | 50% |
| 7–9 years | 32% | 31% | 34% | 23% | |
| 10+ years | 37% | 20% | 23% | 27% | |
| Employment status | Farmwork | 34% | 45% | 34% | 19% |
| Other employment | 19% | 19% | 14% | 27% | |
| Not working | 47% | 35% | 51% | 54% | |
| Marital status | Single/never married | 4% | 5% | ||
| Married/living as married | 93% | 89% | 89% | 92% | |
| Divorced/separated/widowed | 3% | 5% | 11% | 8% | |
| Farmworker status | Migrant | 16% | 26% | 29% | 31% |
| Seasonal | 84% | 74% | 71% | 69% | |
| Documentation | Anyone documented | 21% | 12% | 9% | 15% |
| Everyone undocumented | 79% | 88% | 91% | 85% | |
| Maternal BMI (SD)* | 29.2 (7.7) | 30.3 (4.8) | 30.9 (6.4) | 33.0 (6.6) | |
| Maternal BMI status* | Normal/underweight | 27% | 8% | 18% | 13% |
| Overweight | 38% | 48% | 41% | 29% | |
| Obese | 35% | 44% | 41% | 58% | |
Note. BMI = body mass index; SD = standard deviation.
Denotes significant group difference, p < .05.
Median BMI percentile is reported for children of mothers by depression pattern at baseline and the end of the study (24 months later) in Table 2 and Figure 2. Median BMI percentile was favoured over mean BMI percentile due to the possibility of skewed data distribution and outliers in the sample, and favoured over Z score due to ease of interpretability. At baseline, children of mothers with severe episodic or chronic symptoms had higher median BMI percentile than children of mothers with either moderate episodic or few symptoms. At the end of the study, the median was higher for all three symptomatic patterns compared with few symptoms. In fact, the median BMI percentile decreased for children of mothers with few symptoms and increased for the other three patterns, although the differences were not significant. The percentage of children with a normal weight fell slightly for children of mothers with few symptoms or moderate episodic symptoms over the course of the study (2% and 3%, respectively); the decline was much steeper for children of mothers with severe episodic or chronic symptoms (17% and 25%, respectively). Correspondingly, the percentage of children who were overweight or obese increased markedly for these two subgroups, rising from 55% to 61% (severe episodic) and from 56% to 69% (chronic). Interestingly, the percentage of underweight children increased for both groups as well. The overall distribution of weight status differed significantly for both (p < .05) compared with the few symptoms subgroup.
Table 2.
Weight differences of children by mother's depression pattern
| Baseline | Few symptoms (n = 73) | Moderate episodic symptoms (n = 93) | Severe episodic symptoms (n = 35) | Chronic symptoms (n = 26) |
|---|---|---|---|---|
| Median BMI percentile | 77.9 | 72.3 | 87.4 | 89.4 |
| Weight Status | ||||
| Underweight | 4% | 3% | 0% | 0% |
| Normal weight | 59% | 60% | 46% | 44% |
| Overweight | 16% | 17% | 26% | 20% |
| Obese | 21% | 20% | 29% | 36% |
| 24 Months | ||||
|
Median BMI percentile |
74.3 | 81.0 | 89.5 | 94.1 |
| Weight status | ||||
| Underweight | 4% | 0% | 9% | 4% |
| Normal weight | 57% | 57% | 29% | 27% |
| Overweight | 13% | 20% | 29% | 19% |
| Obese+ | 26% | 23% | 32%* | 50%* |
Note. BMI = body mass index.
Denotes significant difference, p < .05.
Distribution of weight status (% underweight, normal weight, overweight, and obese) was significantly different at 24 months with a higher proportion of children being overweight or obese in the severe episodic and chronic symptoms patterns compared with few symptoms (p = .031 and p = .040, respectively).
Figure 2.
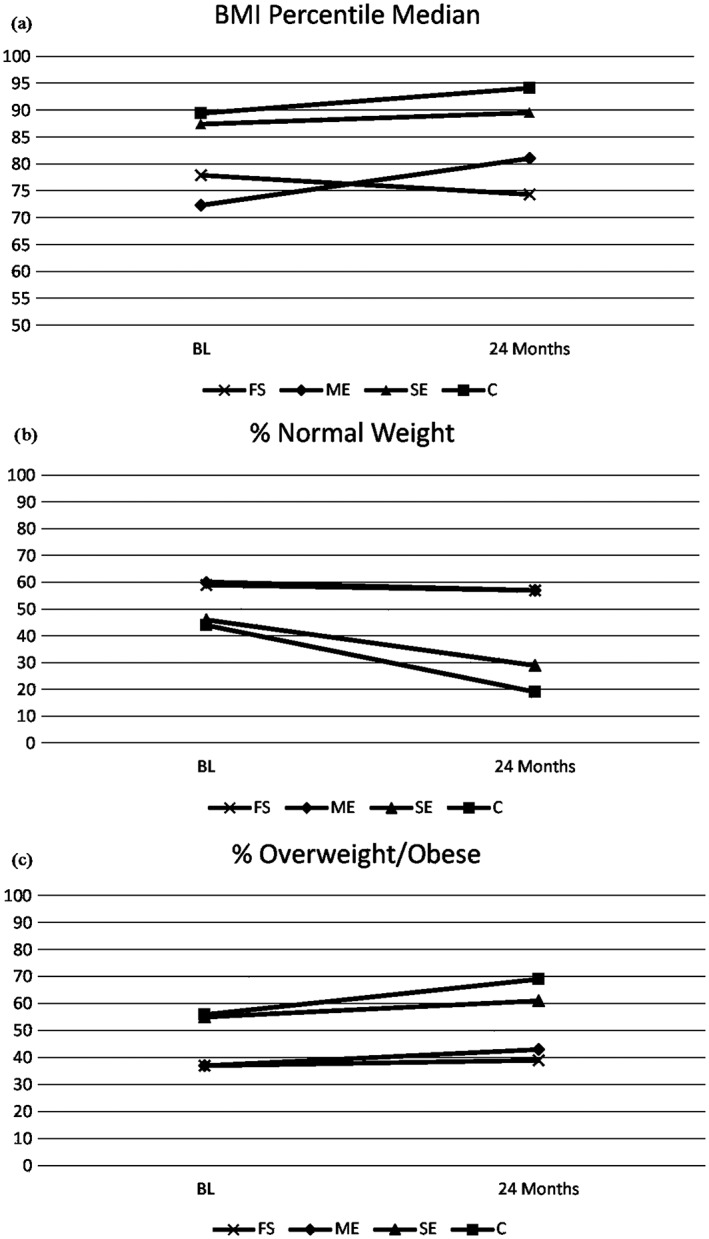
(a) Median BMI percentile, (b) % normal weight, and (c) % overweight or obese shown at baseline and 24‐months later for children of mothers with four patterns of depressive symptoms; FS = few symptoms, ME = moderate episodic, SE = severe episodic, and C = chronic
Children whose mothers were in the chronic pattern were slightly older (p < .05), and children whose mothers had severe episodic symptoms were more likely to be male (p < .05; Table 3). Children whose mothers had chronic symptoms had lower average diet quality per the DQI (p < .01). Children in the moderate episodic and chronic symptoms patterns were fed in a less responsive manner (p < .001 and p < .05, respectively). Other differences were not significant.
Table 3.
Child characteristics by mother's depression pattern
| Few symptoms (n = 73) | Moderate episodic symptoms (n = 93) | Severe episodic symptoms (n = 35) | Chronic symptoms (n = 26) | |
|---|---|---|---|---|
| Age | 2.45 (0.50) | 2.37 (0.48) | 2.60 (0.50) | 2.69* (0.47) |
| Gender (% male) | 37% | 52% | 63%* | 38% |
| Minutes sedentary per day | 420 (114) | 427 (115) | 414 (115) | 459 (111) |
| Minutes light activity per day | 403 (47) | 382 (71) | 398 (67) | 398 (65) |
| Minutes MVPA activity per day | 7 (6) | 6 (5) | 8 (7) | 6 (3) |
| TV viewing minutes per day | 76 (41) | 69 (41) | 67 (41) | 71 (40) |
| Screen time limit | 1.63 (0.75) | 1.87 (0.75) | 1.71 (0.75) | 1.98 (1.21) |
| Frequency taken to play spaces | 1.53 (0.89) | 1.48 (1.10) | 1.32 (0.86) | 1.31 (0.92) |
| Parent is concerned regarding activity level of child | 0.60 (0.83) | 0.90 (1.02) | 0.57 (0.78) | 0.54 (0.86) |
| DQI total score | 60.97 (5.61) | 61.34 (6.30) | 58.73 (6.57) | 56.30** (6.84) |
| Kcal per day | 1250 (321) | 1163 (220) | 1194 (240) | 1185 (253) |
| Feeding demandingness | 1.96 (0.38) | 2.07 (0.56) | 2.06 (0.52) | 2.09 (0.54) |
| Feeding responsiveness | 1.22 (0.10) | 1.17*** (0.10) | 1.21 (0.09) | 1.17* (0.07) |
Note. Few symptoms = reference group. Standard deviation is shown in parentheses.
Denotes significant difference p < .05.
Denotes p < .01.
Denotes p < .001.
For the mediational analysis, although depression pattern significantly predicted responsiveness (overall p < .01) as well as diet quality (overall p < .001), the indirect path of the effect on diet quality as mediated by responsiveness could not be established. In addition, each of the three depressive symptoms subgroups were tested individually to determine if feeding style mediated the relationship between maternal depressive symptoms and children's diet quality and weight. Although chronic depression pattern significantly predicted feeding style, diet quality, and weight status, responsiveness did not qualify as a mediator in this analysis. The mediation results for all three patterns are shown in Figure 3. Other potential mediators such as physical activity or screen time were not tested due to the lack of significant differences across patterns.
Figure 3.
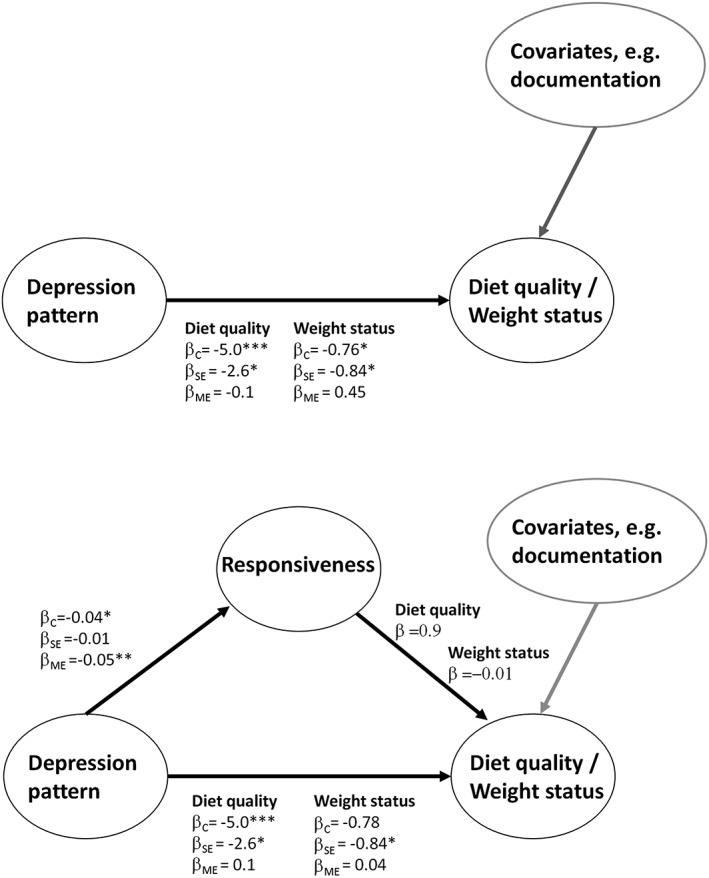
Path diagrams for mediational analysis of the direct pathway (above) and the mediated pathway (below). β indicates the regression coefficient and the subscript indicates depression group (C = chronic, SE = severe episodic, and ME = moderate episodic); * for p < .05, ** for p < .01, and *** for p < .001
In the multivariable analysis, children of mothers with severe episodic depression were significantly more likely to be overweight after adjusting for mother's age and education level, employment, status as a migrant versus seasonal farmworker, documentation status, and mother's BMI (β = −0.84, SE = 0.38, p = .028). After adjustment, the difference was no longer significant for children with mothers in the chronically depressed pattern (β = −0.76, SE = 0.43, p = .075). Also, after adjustment, diet quality remained significantly lower for children whose mothers reported chronic depression (β = −5.01, SE = 1.41, p = .005) and was also significantly lower for children whose mothers reported severe episodic symptoms (β = −2.58, SE = 1.23, p = .037). Mothers belonging to the moderate episodic and chronic symptoms pattern also fed their children in a less responsive manner after adjustment (β = −0.044, SE = 0.016, p = .005 and β = −0.060, SE = 0.023, p = .008, respectively).
4. DISCUSSION
Fewer than one‐third of women would have screened positive for depression using a single measure applied at baseline. Longitudinal examination over a 2‐year period revealed that two‐thirds of women experienced significant depressive symptoms at least once. This would suggest “snapshots” are likely to underestimate the true prevalence of depression, which is characterized by periods of relapse, recovery, and remission (Richards, 2011). Moreover, among affected women, there was significant heterogeneity in terms of duration and severity of symptoms. These results are consistent with and even exceed the high burden of depressive symptoms reported in other studies of Latino farmworkers.
At the end of the study, the median BMI percentile exceeded 75% for all children, reflective of the high degree to which Latino farmworker children experience undesirable weight outcomes (Rosado et al., 2013). Nonetheless, children whose mothers exhibited either severe episodic symptoms or chronic symptoms of depression were even more likely to be overweight or obese (children of mothers in the severe episodic symptom pattern, but not chronic pattern, remained significantly more likely to be overweight or obese after controlling for covariates, although we suspect both differences would have been significant with a moderately larger sample). Indeed, the number of children with normal weights in these categories was surprisingly low (less than 30%), and their median BMI percentile corresponds to overweight status (between 85% and 95%). These children also consumed a lower quality diet (both significant after controlling for covariates). These findings suggest the severity or duration of mother's depressive symptoms, and not just the presence of symptoms, may be important, as suggested in the review by Lampard et al. (2014).
Most obesity risk factors such as level of activity or screen time did not differ between children of mothers with different patterns, perhaps because most children in the sample were highly sedentary (Ip et al., 2016). The two exceptions were diet quality and responsiveness of feeding style. A mediation analysis was performed with feeding style as the mediator for all three patterns. Less responsive feeding did not mediate the relationship between depression, diet quality, and BMI status for any pattern.
Though statistically significant, the magnitude of difference in responsiveness across patterns was small, and patterns were overall similar to one another in terms of feeding style. All four patterns could be characterized as practicing a feeding style that is overall low in terms of demandingness and borderline in terms of high/low responsiveness (Ip et al., 2017). Following standard typology, this suggests that mothers in the study on average tended to feed their children in a manner in‐between “indulgent” and “uninvolved”. Because mothers in all four patterns were on average low in terms of demandingness, mothers in the less responsive patterns (moderate episodic and chronic symptoms) were relatively more “uninvolved”. Maternal depression may operate through additional pathways to influence children's weight and further research is warranted.
Despite our null finding, a difference in feeding style is one of the most compelling explanations for the increased risk of obesity of children of depressed mothers put forth in the literature. Several studies have noted that depressed mothers tend to feed their children in a less responsive fashion compared with mothers with normal mood (Goulding et al., 2014; Gross et al., 2013; Haycraft, Farrow, & Blissett, 2013; McCurdy, Gorman, Kisler, & Metallinos‐Katsaras, 2014; Mitchell, Brennan, Hayes, & Miles, 2009). In a systematic review (Lindsay et al., 2017), two of three studies reported mothers with increased depressive symptoms were less likely to feed their children in a responsive manner. A nonresponsive feeding style may take several forms, being either forceful (strictly controlling the child's intake), indulgent (acquiescing to the child's wishes with little parental guidance), or uninvolved (allowing the child significant autonomy in making eating decisions; Hurley, Black, Papas, & Caufield, 2008). An unsupervised child may choose to eat calorically dense foods and larger portions, while a child whose eating is controlled too tightly may learn to ignore satiety cues and consume excess calories (Birch, 1987; Johnson & Birch, 1993). A recent review linked child overweight and obesity to such nonresponsive practices (Hurley, Cross, & Hughes, 2011).
The nonresponsive feeding style that appears to be more prevalent among depressed mothers may stem largely from the symptoms of the depressive illness. Key symptoms of depression, such as fatigue, low energy, impaired concentration, and loss of interest in usual activities may impair the quality of mothers' interactions with their children. Mothers may be less able or less inclined to reason with their children, offer compliments, and model or encourage healthy eating.
Children did not differ in terms of weight status at the beginning of the study. Perhaps weight differences only emerge after a sustained period of exposure to obesity risk factors. Additionally, as children age and their eating habits change, depressive symptoms affect the mother–child relationship differently as compared with the first years of life. Evidence suggests very young children (<2) of mothers with depressive symptoms may actually be at increased risk of short stature and being underweight (Surkan, Ettinger, Ahmed, Minkovitz, & Strobino, 2012; Wojciki, Holbrook, Lustig, et al., 2011). Mothers with depressive symptoms are reportedly less likely to breastfeed their infants (Grigoriadis et al., 2013) and continue breastfeeding for the recommended period of time (McLearn, Minkovitz, Strobino, Marks, & Hou, 2006). Preschool‐age children are fed very differently and have much greater potential to engage in a variety of activities, so the divergence of obesity risk around this time is perhaps not surprising. As noted in the results, although they did not differ at baseline, there was a slight uptick in the percentage of underweight children in the two most symptomatic patterns over time, a finding that deserves consideration in future studies.
While this study has implications for treatment of depression in mothers of young children generally, it has specific implications for mothers in Latino farmworker families. Although farmworker health programmes in federally qualified health centres currently have a mandate to screen for depression in all patients, such programmes should consider extending this to the mothers of children being seen. In addition, many farmworkers do not live where they can access such clinics and other farmworker service providers (e.g., Migrant Head Start programmes) should consider means to screen mothers and refer them to treatment.
This study has several limitations. First, characterization of depression was based on the response to a 10‐item CES‐D self‐report questionnaire. The CES‐D is not a diagnostic tool but rather a screening measure intended to identify symptoms associated with depression. As such, study findings reference severity and chronicity of depressive symptoms rather than depression diagnoses. Second, some of the comparison groups were quite small, and the study may have been underpowered. For example, although the higher percentage of overweight and obesity seen in children of mothers with chronic symptoms (69%), compared with mothers with few symptoms (39%), appears meaningful, the difference was not significant after adjustment. Third, if persons who refused to participate in the study or were unable to be contacted by study staff had higher levels of depressive symptoms or at least more risk factors for depression, the true prevalence of depressive symptoms may be underestimated. Fourth, more detailed surveys on mother's feeding practices in addition to the feeding style questionnaire could have provided additional insight into how maternal depression may specifically lead to obesity. Lastly, though not a limitation, the study population included Latino farmworkers from North Carolina, and as such, the generalizability of the findings may be constrained. A strength of the study was the high retention, which may be due to the use of a single interviewer working with the woman throughout the study. This was analogous to a case manager approach and facilitates rapport building and the establishment of trust. Some women proactively called the interviewer to report a change in phone number or address. Future studies would benefit from longer duration, increased sample size, diagnostic assessment of maternal depression, and examination of additional mediators and proximal outcomes that may link maternal depression and weight outcomes.
Study results suggest maternal depressive symptoms are common and can affect children's weight, a relationship that has not been previously examined in the understudied and at‐risk Latino farmworker population. Depression is a heterogeneous illness that impacts women and their families differently, with some effects, such as increased rates of obesity, appearing only to emerge in those families with the greatest burden of depression. Given the short‐ and long‐term detriments associated with childhood obesity, study findings further highlight the importance of screening for maternal depression and for making appropriate treatment referrals. Childhood obesity prevention efforts that acknowledge maternal depression and help depressed mothers engage more effectively with their children to foster a healthy weight may be especially effective.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
CONTRIBUTIONS
SAM conceptualized the analysis of depression by pattern, interpreted the results, and drafted the first version of the manuscript. EHI designed the analytic procedures and interpreted the results. CKS performed statistical analysis including the longitudinal and mediation analyses. TAA designed the survey approach, supervised sample accrual, and critically evaluated the manuscript. SS conducted general data management, data cleaning, and analysis of the depression data. SSD critically evaluated the manuscript. SAQ oversaw the project, including data collection, provided crucial support, and critically evaluated the manuscript. All authors approved the final version of the manuscript.
Marshall SA, Ip EH, Suerken CK, et al. Relationship between maternal depression symptoms and child weight outcomes in Latino farmworker families. Matern Child Nutr. 2018;14:e12614 10.1111/mcn.12614
REFERENCES
- Aneshensel, C. S. , Rutter, C. M. , & Lachenbruch, P. A. (1991). Social structure, stress, and mental health: Competing conceptual and analytic models. American Sociological Review, 56, 166–178. [Google Scholar]
- Benton, P. M. , Skouteris, H. , & Hayden, M. (2015). Does maternal psychopathology increase the risk of pre‐schooler obesity? A systematic review. Appetite, 87, 259–282. [DOI] [PubMed] [Google Scholar]
- Birch, L. , & Fisher, J. (1998). Development of eating behaviors among children and adolescents. Pediatrics, 101, 539–549. [PubMed] [Google Scholar]
- Birch, L. L. (1987). The acquisition of food acceptance patterns in children In Boakers R. A., Popplewell D. A., & Burton M. J. (Eds.), Eating habits: Food, physiology and learned behavior. London: Wiley. [Google Scholar]
- Black, M. M. , & Aboud, F. E. (2011). Responsive feeding is embedded in a theoretical framework of responsive parenting. Journal of Nutrition, 141(3), 490–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality . (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H‐50). Retrieved from http://www.samhsa.gov/data/
- Centers for Disease Control and Prevention (CDC) . (2010). Current depression among adults—United States, 2006 and 2008. MMWR. Morbidity and Mortality Weekly Reports Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5938a2.htm?s_cid=mm5938a2_e%0d%0a. [PubMed]
- Cheng, S. T. , & Chan, A. C. (2005). The Center for Epidemiologic Studies Depression Scale in older Chinese: Threshold for long and short forms. International Journal of Geriatric Psychiatry, 20(5), 465–470. [DOI] [PubMed] [Google Scholar]
- Cho, M. J. , & Kim, K. H. (1998). Use of the Center for Epidemiologic Studies Depression (CES‐D) Scale in Korea. Journal of Nervous and Mental Disease, 186(5), 304–310. [DOI] [PubMed] [Google Scholar]
- De Leon Siantz, M. (1990). Correlates of maternal depression among Mexican‐American migrant farmworker mothers. Journal of Child and Adolescent Psychiatric and Mental Health Nursing, 3(1), 9–13. [PubMed] [Google Scholar]
- Dolinsky, D. H. , Brouwer, R. J. , Evenson, K. R. , Siega‐Riz, A. M. , & Ostbye, T. (2011). Correlates of sedentary time and physical activity among preschool‐aged children. Preventing Chronic Disease, 8(6), A131. [PMC free article] [PubMed] [Google Scholar]
- Fernald, L. C. , Jones‐Smith, J. C. , Ozer, E. J. , Neufeld, L. M. , & DiGirolamo, A. M. (2008). Maternal depressive symptoms and physical activity in very low‐income children. Journal of Developmental and Behavioral Pediatrics, 29(5), 385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulding, A. N. , Rosenblum, K. L. , Miller, A. L. , Peterson, K. E. , Chen, Y. P. , Kaciroti, N. , & Lumeng, J. C. (2014). Associations between maternal depressive symptoms and child feeding practices in a cross‐sectional study of low‐income mothers and their young children. The International Journal of Behavioral Nutrition and Physical Activity, 11, 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoriadis, S. , VonderPorten, E. H. , Mamisashvili, L. , Tomlinson, G. , Dennis, C. L. , Koren, G. , … Ross, L. E. (2013). The impact of maternal depression during pregnancy on perinatal outcomes: A systematic review and meta‐analysis. Journal of Clinical Psychiatry, 74(4), e321‐e341. [DOI] [PubMed] [Google Scholar]
- Gross, R. S. , Velazco, N. K. , Briggs, R. D. , & Racine, A. D. (2013). Maternal depressive symptoms and child obesity in low‐income urban families. Academic Pediatrics, 13(4), 356–363. [DOI] [PubMed] [Google Scholar]
- Haringsma, R. , Engels, G. I. , Beekman, A. T. , & Spinhoven, P. (2004). The criterion validity of the Center for Epidemiological Studies Depression Scale (CES‐D) in a sample of self‐referred elder with depressive symptomatology. International Journal of Geriatric Psychiatry, 19(6), 558–563. [DOI] [PubMed] [Google Scholar]
- Haycraft, E. , Farrow, C. , & Blissett, J. (2013). Maternal symptoms of depression are related to observations of controlling feeding practices in mothers of young children. Journal of Family Psychology, 27(1), 159–164. [DOI] [PubMed] [Google Scholar]
- Hiott, A. , Grzywacz, J. G. , Arcury, T. A. , & Quandt, S. A. (2006). Gender differences in anxiety and depression among immigrant Latinos. Families, Systems & Health, 24(2), 137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey, J. D. , & Magaña, C. (2000). Acculturative stress, anxiety, and depression among Mexican immigrant farmworkers in the Midwest United States. Journal of Immigrant Health, 2(3), 119–131. [DOI] [PubMed] [Google Scholar]
- Hughes, S. O. , Anderson, C. B. , Power, T. G. , Micheli, N. , Jaramillo, S. , & Nicklas, T. A. (2006). Measuring feeding in low‐income African–American and Hispanic parents. Appetite, 46(2), 215–223. [DOI] [PubMed] [Google Scholar]
- Hughes, S. O. , Power, T. G. , Liu, Y. , Sharp, C. , & Nicklas, T. A. (2015). Parent emotional distress and feeding styles in low‐income families. The role of parent depression and parenting stress. Appetite, 92, 337–342. [DOI] [PubMed] [Google Scholar]
- Hurley, K. M. , Black, M. M. , Papas, M. A. , & Caufield, L. E. (2008). Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. The Journal of Nutrition, 138(4), 799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley, K. M. , Cross, M. B. , & Hughes, S. O. (2011). A systematic review of responsive feeding and child obesity in high‐income countries. The Journal of Nutrition, 141(3), 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip, E. H. , Marshall, S. A. , Arcury, T. A. , Suerken, C. K. , Trejo, G. , Skelton, J. A. , & Quandt, S. A. (2017). Child feeding style and dietary outcomes in a cohort of Latino farmworker families. Journal of the Academy of Nutrition and Dietetics. 10.1016/j.jand.2017.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip, E. H. , Saldana, S. , Trejo, G. , Marshall, S. A. , Suerkan, C. K. , Lang, W. , … Quandt, S. A. (2016). Physical activity states of pre‐school aged children in farmworker families: Predictive factors and relationship with BMI percentile. Journal of Physical Activity and Health, 13(7), 726–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, R. K. (2002). Dietary intake—How do we measure what people are really eating? Obesity Research, 10(Supply 1), 63S–68S. [DOI] [PubMed] [Google Scholar]
- Johnson, S. , & Birch, L. (1993). Parenting style and regulation of food intake in children. Abstracts of the biennial meeting for the society for research in children development. Chicago, IL: University of Chicago Press. [Google Scholar]
- Kelsey, M. M. , Zaepfel, A. , Bjornstad, P. , & Nadeau, K. J. (2014). Age‐related consequences of childhood obesity. Gerontology, 60(3), 222–228. [DOI] [PubMed] [Google Scholar]
- Kilanowski, J. F. , & Ryan‐Wenger, N. A. (2007). Health status in an invisible population: Carnival and migrant worker children. Western Journal of Nursing Research, 29(1), 100–120. [DOI] [PubMed] [Google Scholar]
- Kohout, F. J. , Berkman, L. F. , Evans, D. A. , & Cornoni‐Huntley, J. (1993). Two shorter forms of the CES‐D (Center for Epidemiological Studies Depression) depression symptoms index. Journal of Aging and Health, 5(2), 179–193. [DOI] [PubMed] [Google Scholar]
- Kranz, S. , Hartman, T. , Siega‐Riz, A. M. , & Herring, A. H. (2006). A diet quality index for American preschoolers based on current dietary intake recommendations and an indicator of energy balance. Journal of the American Dietetic Association, 106(10), 1594–1604. [DOI] [PubMed] [Google Scholar]
- Kuczmarski, R. J. , Ogden, C. L. , & Grummer‐Strawn, L. M. (2000). CDC growth charts: United States. Advance Data, 314, 1–27. [PubMed] [Google Scholar]
- Lampard, A. M. , Franckle, R. L. , & Davison, K. K. (2014). Maternal depression and childhood obesity: A systematic review. Preventive Medicine, 59, 60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay, A. C. , Mesa, T. , Greaney, M. L. , Wallington, S. F. , & Wright, J. A. (2017). Associations between maternal depressive symptoms and nonresponsive feeding styles and practices in mothers of young children: A systematic review. JMIR Public Health Surveillance, 3(2), e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd, A. B. , Lubans, D. R. , Plotnikoff, R. C. , Collins, C. E. , & Morgan, P. J. (2014). Maternal and paternal parenting practices and their influence on children's adiposity, screen‐time, diet and physical activity. Appetite, 79, 149–157. [DOI] [PubMed] [Google Scholar]
- Lorant, V. , Croux, C. , Weich, S. , Deliege, D. , Mackenbach, J. , & Ansseau, M. (2007). Depression and socio‐economic risk factors: 7‐Year longitudinal population study. The British Journal of Psychiatry, 190(4), 293–298. [DOI] [PubMed] [Google Scholar]
- Lorant, V. , Deliege, D. , Eaton, W. , Robert, A. , Philippot, P. , & Ansseau, M. (2003). Socioeconomic inequality in depression: A meta‐analysis. American Journal of Epidemiology, 157, 98–112. [DOI] [PubMed] [Google Scholar]
- Lovejoy, M. C. , Graczyk, P. A. , O'Hare, E. , & Neuman, G. (2000). Maternal depression and parenting behavior: A meta‐analytic review. Clinical Psychology Review, 20(5), 561–592. [DOI] [PubMed] [Google Scholar]
- McCurdy, K. , Gorman, K. S. , Kisler, T. , & Metallinos‐Katsaras, E. (2014). Associations between family food behaviors, maternal depression, and child weight among low‐income children. Appetite, 79, 97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLearn, K. T. , Minkovitz, C. S. , Strobino, D. M. , Marks, E. , & Hou, W. (2006). Maternal depressive symptoms at 2 to 4 months post‐partum and early parenting practices. Archives of Pediatrics and Adolescent Medicine, 160(3), 279–284. [DOI] [PubMed] [Google Scholar]
- Mines, R. (1999). Children in immigrant and nonimmigrant farmworker families In Hernandez D. J. (Ed.), Children of immigrants: Health, adjustment and public assistance. Washington: National Academy Press. [PubMed] [Google Scholar]
- Mitchell, S. , Brennan, L. , Hayes, L. , & Miles, C. L. (2009). Maternal psychosocial predictors of controlling parental feeding styles and practices. Appetite, 53(3), 384–389. [DOI] [PubMed] [Google Scholar]
- Musliner, K. L. , Munk‐Olsen, T. , Eaton, W. W. , & Zandi, P. P. (2016). Heterogeneity in long‐term trajectories of depressive symptoms: Patterns, predictors and outcomes. Journal of Affective Disorders, 192, 199–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden, C. L. , Carroll, M. D. , Fryar, C. D. , & Flegal, K. M. (2015). Prevalence of obesity among adults and youth: United States, 2011‐2014. NCHS Data Brief, 219, 1–8. https://www.cdc.gov/nchs/data/databriefs/db219.pdf [PubMed] [Google Scholar]
- Pulgar, C. A. , Trejo, G. , Suerken, C. , Ip, E. H. , Arcury, T. A. , & Quandt, S. A. (2016). Economic hardship and depression among women in Latino farmworker families. Journal of Immigrant and Minority Health, 18(3), 505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quandt, S. A. , Trejo, G. , Suerken, C. K. , Pulgar, C. A. , Ip, E. H. , & Arcury, T. A. (2016). Diet quality among preschool‐age children of Latino migrant and seasonal farmworkers in the United States. Journal of Immigrant and Minority Health, 18(3), 505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, D. (2011). Prevalence and clinical course of depression: A review. Clinical Psychology Review, 31(7), 1117–1125. [DOI] [PubMed] [Google Scholar]
- Rosado, J. I. , Johnson, S. B. , McGinnity, K. A. , & Cuevas, J. P. (2013). Obesity among Latino children within a migrant farmworker community. American Journal of Preventive Medicine, 44(3), S274–S281. [DOI] [PubMed] [Google Scholar]
- Skouteris, H. , McCabe, M. , Swinburn, B. , Newgreen, V. , Sacher, P. , & Chadwick, P. (2011). Parental influence and obesity prevention in pre‐schoolers: A systematic review of interventions. Obesity Reviews, 12(5), 315–328. [DOI] [PubMed] [Google Scholar]
- Surkan, P. J. , Ettinger, A. K. , Ahmed, S. , Minkovitz, C. S. , & Strobino, D. (2012). Impact of maternal depressive symptoms on growth of preschool and school‐aged children. Pediatrics, 130(4), e847–e3855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tovar, A. , Hennessy, E. , Pirie, A. , Must, A. , Gute, D. M. , Hyatt, R. R. , … Economos, C. D. (2012). Feeding styles and child weight status among recent immigrant mother‐child dyads. International Journal of Behavioral Nutrition and Physical Activity, 9, 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trost, S. G. , Sirard, J. R. , Dowda, M. , Pfeiffer, K. A. , & Pate, R. R. (2003). Physical activity in overweight and nonoverweight preschool children. International Journal of Obesity, 27, 834–839. [DOI] [PubMed] [Google Scholar]
- Ventura, A. K. , & Birch, L. L. (2008). Does parenting affect children's eating and weight status? Internal Journal of Behavioral Nutrition and Physical Activity, 5, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojciki, J. M. , Holbrook, K. , Lustig, R. H. , Epel, E. , Caughey, A. B. , Muñoz, R. F. , … Heyman, M. B. (2011). Chronic maternal depression is associated with reduced weight gain in Latino infants from birth to 2 years of age. PLoS One, 6(2), e16737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zich, J. M. , Attkisson, C. C. , & Greenfield, T. K. (1990). Screening for depression in primary care clinics: The CES‐D and the BDI. International Journal of Psychiatry in Medicine, 20(3), 259–277. [DOI] [PubMed] [Google Scholar]
- Zimmer, K. P. , & Minkovitz, C. S. (2003). Maternal depression: An old problem that merits increased recognition by child healthcare practitioners. Current Opinion in Pediatrics, 15(6), 636–640. [DOI] [PubMed] [Google Scholar]


